Abstract
Posterior cervical laminoforaminotomy is an effective treatment for cervical radiculopathy due to disc herniations or spondylosis. Over the last decade, minimally invasive (i.e., percutaneous) procedures have become increasingly popular due to a smaller incision size and presumed benefits in postoperative outcomes. We performed a systematic review of the literature and identified studies of open or percutaneous laminoforaminotomy that reported one or more perioperative outcomes. Of 162 publications found by our initial screening, 19 were included in the final analysis. Summative results indicate that patients undergoing percutaneous cervical laminoforaminotomy have lower blood loss by 120.7 mL (open: 173.5 mL, percutaneous: 52.8 mL, n = 670), a shorter surgical time by 50.0 minutes (open: 108.3 minutes, percutaneous: 58.3 minutes, n = 882), less inpatient analgesic use by 25.1 Eq (open: 27.6 Eq, percutaneous: 2.5 Eq, n = 356), and a shorter hospital stay by 2.2 days (open: 3.2 days, percutaneous: 1.0 days, n = 1472), compared with patients undergoing open procedures. However, the heterogeneous nature of published data calls into question the reliability of these summative results. Further structured trials should be conducted to better characterize the risks and benefits of percutaneous laminoforaminotomy.
Keywords: cervical spine, laminoforaminotomy, minimally invasive spine surgery, percutaneous spine surgery, spine surgery outcomes
Posterior laminoforaminotomy is a well-established technique for cervical radiculopathy, first described in the mid-20th century by Spurling and Scoville,1 and soon after by Frykholm.2 For over five decades, the traditional posterior foraminotomy relied on an open “keyhole” approach performed through a midline incision. In 2001, Adamson published the first report of microendoscopic laminoforaminotomy.3 Since then, multiple reports of similar procedures have been published.4–11 Percutaneous laminoforaminotomy is appealing due to a smaller incision size and presumed benefits in blood loss, hospital stay, and pain medication use. However, percutaneous procedures may also be associated with longer surgical time, increased risk of intraoperative and postoperative complications, and a longer surgeon learning curve.12
In this systematic review, we compare published blood loss, surgical time, pain medication use, and postoperative hospital stay in open and percutaneous laminoforaminotomy.
Materials and Methods
The PubMed and Cochrane library databases were searched in April of 2011 to find English-language publications reporting outcomes from percutaneous or open cervical laminoforaminotomy ( Table 1 ). An initial search found 162 papers published between January 1990 and April 2011. Titles and abstracts of these papers were examined to identify reports that contained objective surgical outcomes. Studies that contained pooled open and percutaneous data, case reports, procedures related to the atlantoaxial junction, and laminoforaminotomy with laminoplasty were excluded. The remaining 29 publications received a full review. Nine of these failed to report data regarding blood loss, surgical time, pain medication use, and postoperative hospital stay. One was excluded because it reported follow-up outcomes on the same cohort. The remaining 19 publications ( Fig. 1 ) were assigned an evidence class based upon the standards established by Matz et al.13
Table 1. Literature Results.
| Search Term | PubMed | Cochrane Library |
|---|---|---|
| Cervical foraminotomy | 128 | 6 |
| Cervical foramenotomy | 5 | 0 |
| Tubular retractor foraminotomy | 3 | 1 |
| Tubular retractor foramenotomy | 0 | 0 |
| Endoscopic foraminotomy | 20 | 1 |
| Endoscopic foramenotomy | 1 | 0 |
| Microendoscopic foraminotomy | 7 | 0 |
| Microendoscopic foramenotomy | 0 | 0 |
| Percutaneous foraminotomy | 8 | 0 |
| Percutaneous foramenotomy | 0 | 0 |
| Laminoforaminotomy | 29 | 0 |
| Laminoforamenotomy | 0 | 0 |
| Total (unambiguous) | 162 | 6 |
Figure 1.
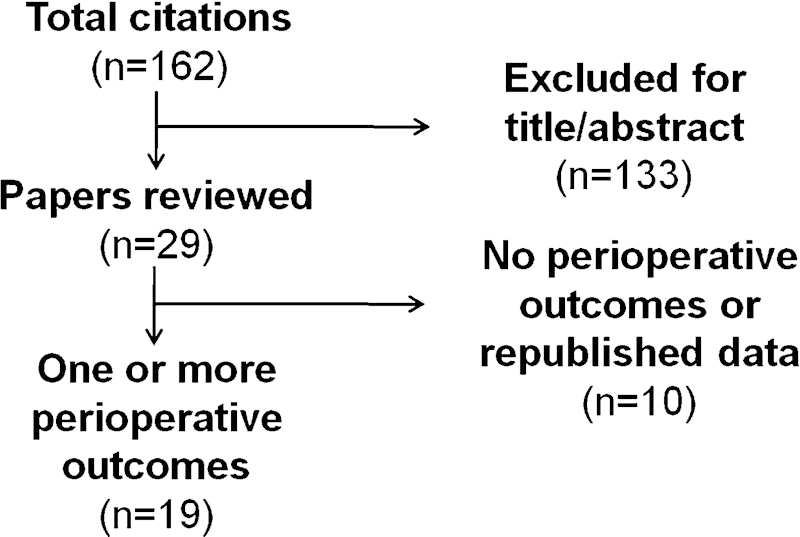
Identification of papers reporting perioperative outcomes.
The following assumptions were made to standardize the data for quantitative comparison. Blood loss that could not be measured (too minimal) was assumed to be 10 mL (two reports). Surgical time was defined to include anesthesia time if that was the only reported outcome (one report). Pain medication use was reported as postoperative pain medication use or postdischarge pain medication use. Only the five publications that reported pain treatments in equivalents were included in the overall analysis of analgesic use. Hospital stay was standardized to patient days. Publications that only reported the day on which patients left were recorded as follows: same day (0.5 patient days), next day (1.0 patient days), second day (2.0 patient days). In the infrequent case that a study only reported a median for any data point, this was estimated to be the mean for the purpose of our analysis. All data were averaged on a per-patient basis rather than a per-study basis.
Results
Summative Results
Of the 18 publications identified, 17 were classified as class III evidence due to lack of an adequate comparison group or substantial limitations in the cohort design. The remaining trial by Kim and Kim10 was a randomized clinical trial that was classified as class II evidence (as opposed to class I) due to the small number of patients in the study (n = 41). Each publication reported one or more perioperative outcomes related to blood loss (n = 8), surgical time (n = 10), pain medication use (n = 7), and hospital stay (n = 17; Table 2 , Table 3 ). The heterogeneous nature of the reported procedures and outcomes made strict meta-analysis impossible. However, data aggregated from these reports found that patients undergoing percutaneous cervical laminoforaminotomy have lower blood loss by 120.7 mL (open: 173.5 mL, percutaneous: 52.8 mL, n = 670), a shorter surgical time by 50.0 minutes (open: 108.3 minutes, percutaneous: 58.3 minutes, n = 882), less inpatient analgesic use by 25.1 Eq (open: 27.6 Eq, percutaneous: 2.5 Eq, n = 356), and a shorter hospital stay by 2.2 days (open: 3.2 days, percutaneous: 1.0 days, n = 1472), compared with patients undergoing open procedures ( Fig. 2 ).
Table 2. Publications Reporting Perioperative Outcomes from Open Laminoforaminotomy.
| Author(s) | Year | n | Blood Loss (mL) | Surgical Time (min) | Pain Medication Use | Hospital Stay (d) |
|---|---|---|---|---|---|---|
| Winder and Thomas11 | 2011 | 65 | 233 | 93.8 | 26.6 Eqa
9.9 Eqb |
2.4 |
| Kim and Kim10 | 2009 | 19 | NR | 76.5 | 3.6 wkb | 6.7 |
| Jagannathan et al14 | 2009 | 162 | NR | NR | NR | 1.9 |
| Cağler et al15 | 2007 | 84 | NR | NR | NR | 2 |
| Korinth et al16 | 2006 | 168 | NR | 94.1 | NR | 4.5 |
| Fessler and Khoo4 | 2002 | 26 | 246 | 177 | 40 Eqa | 2.8 |
| Grieve et al17 | 2000 | 62 | NR | NR | NR | 2 |
| Wirth et al18 | 2000 | 22 | NR | 139 | 15.9 Eqa | 4.3 |
| Grundy et al19 | 2000 | 11 | NR | NR | NR | 1 |
| Silveri et al20 | 1998 | 84 | 105 | 126 | NR | 3.3 |
| Tomaras et al21 | 1998 | 183 | NR | NR | NR | 0.5 |
| Kumar et al22 | 1998 | 89 | NR | NR | NR | 7 |
| Woertgen et al23 | 1997 | 54 | NR | NR | NR | 9 |
NR, not reported in this study.
aInpatient pain medication use.
bPostdischarge pain medication use.
Table 3. Publications Reporting Perioperative Outcomes from Percutaneous Laminoforaminotomy.
| Author(s) | Year | n | Blood Loss (mL) | Surgical Time (min) | Pain Medication Use | Hospital Stay (d) |
|---|---|---|---|---|---|---|
| Winder and Thomas11 | 2011 | 42 | 96 | 92.2 | 8.8 Eqa
6.0 Eqb |
1.1 |
| Kim and Kim10 | 2009 | 22 | NR | 78.5 | 2.6 wkb | 4.1 |
| Ruetten et al9 | 2008 | 89 | Not measureable | 28 | None required | NR |
| Scheufler and Kirsch8 | 2007 | 11 | 45.5 | 157 | NR | 5.7 |
| Ruetten et al7 | 2007 | 87 | Not measureable | 27 | None required | NR |
| Hilton6 | 2007 | 222 | 71 | 63 | NR | 0.6 |
| Holly et al5 | 2007 | 21 | 35 | NR | NR | 0.7 |
| Fessler and Khoo4 | 2002 | 25 | 138 | 115 | 9–11 Eqa | 0.8 |
| Adamson3 | 2001 | 100 | NR | NR | 84%<1 wkb | 0.6 |
NR, not reported in this study.
aInpatient pain medication use.
bPostdischarge pain medication use.
Figure 2.
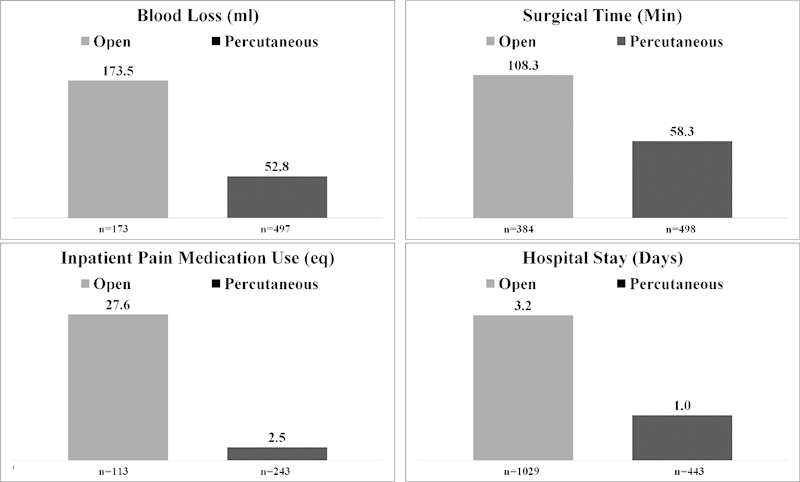
Summative perioperative results.
Retrospective and Prospective Cohort Studies Comparing Procedures
Two cohort studies directly compared open and percutaneous cervical laminoforaminotomy. The first, by Fessler and Khoo,4 was a small prospective cohort study of patients who underwent open (n = 26) or percutaneous (n = 25) laminoforaminotomy by a single surgeon. This study reported that percutaneous cases had lower blood loss by 108 mL (open: 246 mL, percutaneous: 138 mL), a shorter surgical time by 62 minutes (open: 177 minutes, percutaneous: 115 minutes), less analgesic use by 29 to 31 Eq (open: 40 Eq, percutaneous: 9 to 11 Eq), and a shorter hospital stay by 48 hours (open: 68 hours, percutaneous: 20 hours) compared with open controls. The patient was placed in a prone position in all controls and 13 of the cases, and in a sitting position in 12 percutaneous cases. The seated percutaneous cases had notably lower blood loss (27 mL), operative time (90 minutes), and hospital stay (8.1 hours) than the prone percutaneous cases. In addition, the 26 controls underwent decompression at 42 levels, and the 25 percutaneous cases underwent decompression at 33 levels. No significant difference was found in hospital stay among single- and multilevel procedures. Complications included three durotomies, with two leaks and one partial thickness violation.
Winder and Thomas11 describe retrospective results from a cohort study of 65 open and 42 microscopic tubular-assisted posterior laminoforaminotomies. They reported that percutaneous cases had lower blood loss by 137 mL (open: 233 mL, percutaneous: 96 mL), less recovery room analgesic use by 17.78 Eq (open: 26.57 Eq, percutaneous: 8.79 Eq), less discharge analgesic use by 3.87 Eq (open: 9.88 Eq, percutaneous: 6.01 Eq), and a shorter hospital stay by 31.7 hours (open: 58.6 hours, percutaneous: 26.9 hours) compared with open controls. There was insufficient evidence to conclude that surgical time was different between cases and controls (open: 103.7 minutes, percutaneous: 100.7 minutes). There were seven complications in the open group and three in the percutaneous group with specific complications not reported. In the open group, 3 three-level, 8 two-level, and 11 bilateral procedures were performed compared with 1 three-level, 2 two-level, and 2 bilateral cases in the percutaneous group.
Randomized Trials
Kim and Kim10 is the only reported randomized clinical trial of open verses percutaneous laminoforaminotomy. Forty-one patients were randomized to open (n = 19) or percutaneous (n = 22) procedures. The percutaneous cases had less postoperative analgesic use by 1 week (open: 3.6 weeks, percutaneous: 2.6 weeks), and a shorter hospital stay by 2.6 days (open: 6.7 days, percutaneous: 4.1 days) compared with open controls. Open surgical time was 76.5 minutes and percutaneous, 78.5 minutes. Blood loss was not reported. However, skin incision size was reported to be smaller in the percutaneous group by 4 mm (open: 3.6 ± 0.4 cm, percutaneous 3.2 ± 0.2 cm, p < 0.05). No complications were reported for any of these surgeries.
Discussion
Posterior laminoforaminotomy is an effective treatment for cervical radiculopathy in appropriately selected patients. These patients typically have radiculopathy due to cervical nerve root compression secondary to spondylosis or lateral displacement of a cervical disk. Due to the growing adoption of percutaneous procedures in the cervical spine, we aimed to identify published benefits and risks associated with percutaneous laminoforaminotomy.
We identified 19 publications that reported perioperative outcomes from open (n = 13) or percutaneous procedures (n = 9). Our analysis identified a total of 1029 open procedures and 619 percutaneous procedures with at least one reported perioperative outcome. To our knowledge, this is the first systematic review of these procedures. Data aggregated from the published literature suggest that blood loss, pain medication use, and hospital stay were reduced in patients who underwent percutaneous rather than open procedures. Surprisingly, surgical time in percutaneous procedures was reported to be shorter than in open procedures. However, it was also clear from our analysis that significant heterogeneity exists within the reported data. Surgical technique, standard hospital procedure, patient selection, and nonstandardized outcome measures all contributed to the variability seen within these outcomes. Although these results accurately report what has been published in the literature, they may not accurately represent the actual outcomes that are seen in everyday practice.
Analysis of a study by Tomaras et al provides insight as to whether perioperative outcomes from open laminoforaminotomy might be similar to outcomes from percutaneous laminoforaminotomy in an appropriately selected patient.21 In this report, 200 patients underwent open laminoforaminotomy. All patients went home the same day, and the range of incision sizes was reported to be only 1.2 to 3 cm. This incision size would likely be correlated with minimal blood loss, although that outcome was not reported. Postoperative pain medication use would also be relatively low in patients from this study. This theory is supported by Fessler and Khoo’s observation that hospitalization time might explain a substantial portion of postoperative pain medication use.4 Although these hypotheses cannot be generalized to all patients, it is clear that outstanding perioperative outcomes can occur in many open laminoforaminotomy procedures.
In the cohort studies we analyzed, there is a possibility that less complicated patients may have been more likely to undergo percutaneous laminoforaminotomy. One possible measure of complexity is the proportion of patients who undergo multilevel and bilateral procedures. In the cohort study by Winder and Thomas, there are a substantially higher number of multilevel and bilateral procedures in the open cohort compared with the percutaneous cohort.11 However, their analysis of single-level laminoforaminotomies alone still revealed that patients who underwent the percutaneous procedure had statistically significant improvements in blood loss, analgesic use, and hospital stay compared with patients who underwent single-level open procedures. Time is another potential confounder, as the proportion of patients who underwent open laminoforaminotomies decreased over the 10-year period of the study, introducing the possibility that other changes in surgical and medical practice may have accounted for some of the difference between cohorts. In summary, the retrospective nature of this study makes it unclear whether improved outcomes in percutaneous cases come as a result of surgical technique or some other underlying variable. Fessler and Khoo attempted to control for selection bias by performing open and then percutaneous procedures on consecutive patients. However, their results become even more difficult to interpret due to a major change in operative practice midway through the percutaneous cohort.4
Of particular importance is the small randomized clinical trial conducted by Kim and Kim.10 Although this study did not report blood loss, it did report significant decreases in hospital stay and postoperative pain medication use. Surgical time and the proportion of patients receiving single-level laminoforaminotomy were similar in both groups. The only reported differences between the two surgical groups are the percutaneous surgical incision, which is shorter by a statistically significant 4 mm over the 3.6 cm opening made during open procedures, and an acknowledgment that periosteal dissection is more extensive in open procedures. These differences may have some clinical relevance. The more extensive exposure may be the reason open procedure patients remained hospitalized for 2.6 days longer and used analgesics for an additional week compared with the percutaneous group. However, there is still the possibility that some other factors may have contributed to the magnitude of improvement in hospital stay and analgesic use.
Large randomized trials are beneficial to the understanding of expected outcomes among well-selected patients. Investigations of this kind have proven to be valuable in the lumbar spine. In 2010, Teli et al published the results of a randomized controlled trial of microendoscopic, microscopic, and open discectomy in 240 patients. Although most clinical outcome measures were comparable in all three groups, the microendoscopic group had longer surgical time (microendoscopic: 56 minutes, microscopic: 43 minutes, open: 36 minutes) and increased hospital stay (microendoscopic: 54 hours, microscopic: 49 hours, open: 49 hours) compared with the other two groups.24 Arts et al also performed a randomized controlled trial of 328 patients who underwent open or tubular discectomy. The tubular group had similar blood loss (tubular: 92% < 50 mL, open: 85% < 50 mL), longer surgical time (tubular: 47 minutes, open: 36 minutes), and equivalent hospital stay (3.3 days) compared with the open group.25 These large-scale clinical trials model how similar studies of both perioperative and long-term outcomes could be done in the cervical spine.
As with all systematic reviews, we are aware that less favorable results in percutaneous or open laminoforaminotomy have not been published. In addition, few of these studies take into account the time it takes a surgeon to learn the endoscopic technique. This learning curve is difficult to account for given the nature of surgical reporting; namely, a surgeon may wait until a technique is mastered before reporting outcomes. Additionally, our analysis has ignored differences in long-term outcomes between open and percutaneous laminoforaminotomy. However, we do note that long-term outcomes were observed to be grossly similar in the limited number of studies (only three) that directly compared open and percutaneous procedures.
In conclusion, the data describing open and percutaneous laminoforaminotomy are very heterogeneous, making it difficult to recommend one procedure over the other. As has taken place in the lumbar spine, it is important that more structured and thorough trials be designed to clarify the risks and benefits associated with each of these procedures.
References
- 1.Spurling R, Scoville W. Lateral rupture of the cervical intervertebral discs: a common cause of shoulder and arm pain. Surg Gynecol Obstet. 1944;78:350–358. [Google Scholar]
- 2.Frykholm R Cervical nerve root compression resulting from disc degeneration and root-sleeve fibrosis Acta Chir Scand 1951160(Suppl):1–149. [Google Scholar]
- 3.Adamson TE Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: results of a new technique in 100 cases J Neurosurg 2001951, Suppl):51–57. [DOI] [PubMed] [Google Scholar]
- 4.Fessler RG Khoo LT Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience Neurosurgery 2002515, Suppl):S37–S45. [PubMed] [Google Scholar]
- 5.Holly LT, Moftakhar P, Khoo LT, Wang JC, Shamie N. Minimally invasive 2-level posterior cervical foraminotomy: preliminary clinical results. J Spinal Disord Tech. 2007;20:20–24. doi: 10.1097/01.bsd.0000211254.98002.80. [DOI] [PubMed] [Google Scholar]
- 6.Hilton DL Jr. Minimally invasive tubular access for posterior cervical foraminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imaging. Spine J. 2007;7:154–158. doi: 10.1016/j.spinee.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Ruetten S, Komp M, Merk H, Godolias G. A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg. 2007;50:219–226. doi: 10.1055/s-2007-985860. [DOI] [PubMed] [Google Scholar]
- 8.Scheufler KM, Kirsch E. Percutaneous multilevel decompressive laminectomy, foraminotomy, and instrumented fusion for cervical spondylotic radiculopathy and myelopathy: assessment of feasibility and surgical technique. J Neurosurg Spine. 2007;7:514–520. doi: 10.3171/SPI-07/11/514. [DOI] [PubMed] [Google Scholar]
- 9.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine. 2008;33:940–948. doi: 10.1097/BRS.0b013e31816c8b67. [DOI] [PubMed] [Google Scholar]
- 10.Kim KT, Kim YB. Comparison between open procedure and tubular retractor assisted procedure for cervical radiculopathy: results of a randomized controlled study. J Korean Med Sci. 2009;24:649–653. doi: 10.3346/jkms.2009.24.4.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winder MJ, Thomas KC. Minimally invasive versus open approach for cervical laminoforaminotomy. Can J Neurol Sci. 2011;38:262–267. doi: 10.1017/s0317167100011446. [DOI] [PubMed] [Google Scholar]
- 12.Epstein NE. Minimally invasive/endoscopic vs “open” posterior cervical laminoforaminotomy: do the risks outweigh the benefits? Surg Neurol. 2009;71:330–331. doi: 10.1016/j.surneu.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Matz PG, Anderson PA, Kaiser MG. et al. Introduction and methodology: guidelines for the surgical management of cervical degenerative disease. J Neurosurg Spine. 2009;11:101–103. doi: 10.3171/2009.1.SPINE08712. [DOI] [PubMed] [Google Scholar]
- 14.Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine. 2009;10:347–356. doi: 10.3171/2008.12.SPINE08576. [DOI] [PubMed] [Google Scholar]
- 15.Cağlar YŞ, Bozkurt M, Kahilogullari G. et al. Keyhole approach for posterior cervical discectomy: experience on 84 patients. Minim Invasive Neurosurg. 2007;50:7–11. doi: 10.1055/s-2007-970138. [DOI] [PubMed] [Google Scholar]
- 16.Korinth MC Krüger A Oertel MF Gilsbach JM Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy Spine 2006311207–1214.; discussion 1215–1216 [DOI] [PubMed] [Google Scholar]
- 17.Grieve JP, Kitchen ND, Moore AJ, Marsh HT. Results of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathy. Br J Neurosurg. 2000;14:40–43. doi: 10.1080/02688690042898. [DOI] [PubMed] [Google Scholar]
- 18.Wirth FP Dowd GC Sanders HF Wirth C Cervical discectomy. A prospective analysis of three operative techniques Surg Neurol 200053340–346.; discussion 346–348 [DOI] [PubMed] [Google Scholar]
- 19.Grundy PL Germon TJ Gill SS Transpedicular approaches to cervical uncovertebral osteophytes causing radiculopathy J Neurosurg 2000931, Suppl):21–27. [DOI] [PubMed] [Google Scholar]
- 20.Silveri CP, Simpson JM, Simeone FA, Balderston RA. Cervical disk disease and the keyhole foraminotomy: proven efficacy at extended long-term follow up. Orthopedics. 1997;20:687–692. doi: 10.3928/0147-7447-19970801-07. [DOI] [PubMed] [Google Scholar]
- 21.Tomaras CR, Blacklock JB, Parker WD, Harper RL. Outpatient surgical treatment of cervical radiculopathy. J Neurosurg. 1997;87:41–43. doi: 10.3171/jns.1997.87.1.0041. [DOI] [PubMed] [Google Scholar]
- 22.Kumar GR, Maurice-Williams RS, Bradford R. Cervical foraminotomy: an effective treatment for cervical spondylotic radiculopathy. Br J Neurosurg. 1998;12:563–568. doi: 10.1080/02688699844448. [DOI] [PubMed] [Google Scholar]
- 23.Woertgen C Holzschuh M Rothoerl RD Haeusler E Brawanski A Prognostic factors of posterior cervical disc surgery: a prospective, consecutive study of 54 patients Neurosurgery 199740724–728.; discussion 728–729 [DOI] [PubMed] [Google Scholar]
- 24.Teli M, Lovi A, Brayda-Bruno M. et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443–450. doi: 10.1007/s00586-010-1290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arts MP Brand R van den Akker ME et al. Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial Neurosurgery 201169135–144.; discussion 144 [DOI] [PubMed] [Google Scholar]


