Abstract
Objective To demonstrate that preservation of all posterior structures during open-door laminoplasty (ODL) is associated with a significant preservation of motion.
Methods Fifteen patients underwent cervical ODL by one surgeon for treatment of cervical spondylotic myelopathy. An open-door technique was employed, and the laminae on the open side were reconstructed using miniplates with allograft strut bone graft. All spinous processes and interspinous and supraspinous ligaments were preserved within the operative levels and between supra- and subjacent levels in all patients. Postoperative radiographs were obtained 1.5, 3, 6, and 12 months. Computed tomography scans were obtained at 12 months.
Results There were no significant intraoperative or perioperative complications. Postoperatively, the neutral angle was 6.8 ± 11.5 degrees (95% confidence interval: 0.5 to 13.1), representing a loss of lordosis of 3 degrees (not significant). The difference between the preoperative and postoperative arc range of motion was 5.96 ± 11.9 degrees (confidence interval: −0.62 to 12.5). The average percent loss of motion was 3.5% ± (0.1 to 6.9%). Four patients had an increased range of motion postoperatively.
Conclusion Open-door laminoplasty with preservation of all posterior structures provides greater preservation of motion than has been previously described.
Keywords: laminoplasty, open-door laminoplasty, cervical spondylotic myelopathy, range of motion, alignment
Although open-door laminoplasty (ODL) is a well-known and frequently utilized technique for the treatment of cervical myelopathy, long-term follow-up studies demonstrate results consistent with significant postoperative loss of motion.1 2 3 A critical review by Ratliff and Cooper in 2003 reported a mean decrease of 50% range of motion (ROM), with losses between 17% and 80% across 23 studies.4 Furthermore, it has been shown that laminoplasty causes a loss of lordosis and loss of sagittal alignment. Despite the multitude of approaches to ODL for the treatment of cervical myelopathy, no studies have shown the clinical and radiographic results of ODL with preservation of all posterior structures. We hypothesize that the preservation of all structures will result in maintenance of sagittal alignment and range of subaxial motion. Here we present the results of 15 patients who underwent ODL with preservation of all posterior structures with mean 12.9-month follow-up that to our knowledge provides the first report of this technique.
Materials and Methods
Surgical Technique
Fifteen consecutive patients underwent cervical ODL by one surgeon (T.E.M.) for the treatment of cervical spondylotic myelopathy. In each patient, a 3-mm carbide bur was used on the side to be opened to transect the laminae at the laminae–lateral mass junction (Fig. 1). Next, the ligamentum flavum along this trough was meticulously ligated, as was the ipsilateral ligamentum flavum between the supra- and subjacent levels to facilitate opening. Next, the hinge side was then drilled and each surgical-level lamina was elevated in the typical fashion for an ODL. No grafting substrate was applied to the hinged levels. All spinous processes and supraspinous ligaments were preserved within the operative levels and between supra- and subjacent levels in all patients with the exception of the most caudal and rostral aspects of the exposure ipsilateral to the open side (where the ligamentum flavum was transected to facilitate the opening of the laminae). This includes preservation of the ligamentum nuchae throughout the cervical spine. The interspinous muscles were preserved as well. From the surgeon's clinical experience, the presence of these structures did not hinder or prevent adequate opening of the laminae as compared with expansion without preservation of the posterior elements. The interspinalis muscles are likely denervated during the exposure. The extensor muscles are elevated (but not removed) and then allowed to fall back after the exposure. In all patients but one, the laminae on the open side were reconstructed using miniplates with either an 8-mm or a 10-mm cortical allograft strut bone graft affixed to the plate. The laminar portion of the plate was secured with two 5-mm screws, and the lateral mass portion of the plate was secured with one 7-mm (cranial) and one 5-mm (caudal) screw. Although the patients' spines were placed in a neutral to slightly flexed alignment to facilitate the procedure, great care was taken to avoid placing the plate too far rostrally on the lateral mass to ensure there would be no abutment with the rostral lateral mass during subaxial extension. Once to the ward where soft collars are available, they are transitioned to a soft collar. On postoperative day 1, the surgical team (i.e., residents, fellows, attendings, or physician assistants) instructed the patient on active lateral bending, rotation, flexion, and extension. The patients were instructed to perform these exercises at least three times a day during the hospital stay and a minimum of ten times per day upon discharge. The soft cervical collar was discontinued as soon as possible, typically by postoperative day 3.
Figure 1.
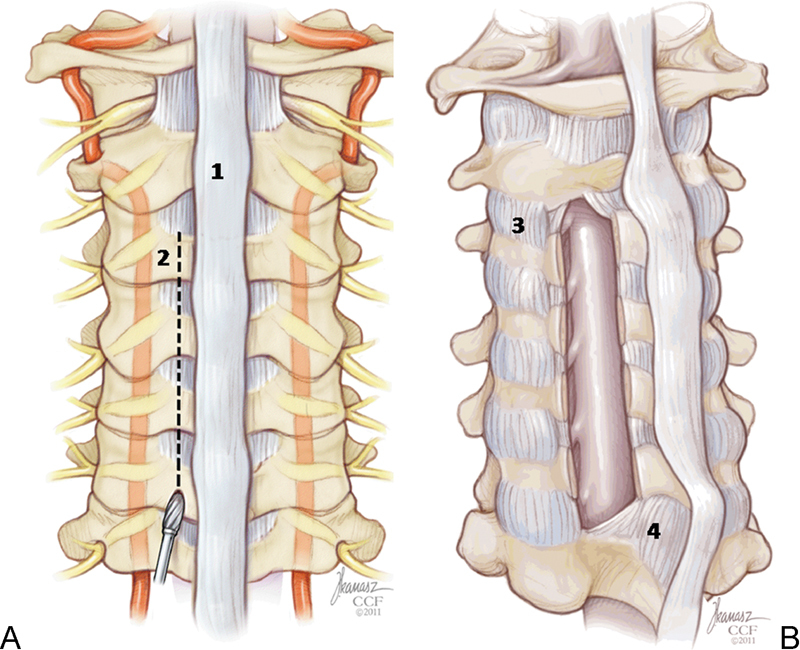
Anatomic diagram of the posterior ligamentomuscular structures. (A) Posterior exposure of the spine showing the ligamentum nuchae (1) and the burr path on the open side (2). (B) An oblique view of the spine with an idealized exposure of the cord demonstrating the interspinous muscles, which remain intact where possible (3), and the terminal end of the construct with an intact ligamentum nuchae (4).
Analysis
The primary measure was the radiographic assessment. Preoperative radiographs were taken in neutral, flexion, and extension positions. Postoperative radiographs were taken at 1.5, 3, 6, and 12 months with an average terminal follow-up of 41.2 months and included neutral, flexion, and extension positions. Postoperative measurements were based on the final follow-up radiograph at a mean of 12.9 months, and preoperative measurements were based on radiographs taken closest to the date of surgery. Two independent observers (K.G.A., T.Y.) utilized the posterior tangent method to estimate preoperative and postoperative angles in the neutral, flexion, and extension positions electronically using Sienet MagicView 1000 VE 42 (Siemens Medical Systems, Erlangen, Germany). The posterior tangent method involves the measurement of the angle created by the vertex of two lines: the posterior body of C2 and the posterior body of C7 (Fig. 2). This method was originally described by Gore et al5 and has since been reported to provide good reliability and a lower standard error of measurement than that of the Cobb angle.6 After assessment, intraclass correlation coefficients (ICC) were calculated to determine agreement between raters.7 ICC for all measurements ranged from 0.85 to 0.93, indicating that there was excellent correlation between observers. Computerized tomography (CT) scans with sagittal reconstructions and 2-mm axial CT images of each surgical level were obtained at a mean of 12.9 months (range: 9 to 26) in all patients to assess the construct integrity, hinge healing, and bone graft consolidation on the open side. On the open side, grafts were deemed “consolidated” if there was (1) bridging bone on both sides of the graft to the lamina and lateral mass, and (2) absence of instrumentation loosening. A hinge was deemed to be “healed” if bridging bone was evident on axial images. All statistics were calculated using JMP 8.0 (2008, SAS Institute, Carey, NC). Descriptive statistics including mean, standard deviation, standard error, and confidence intervals were computed for all measurements. p values were calculated using Student t test and were considered nominally significant at <0.05. Bivariate analysis of continuous variables was performed to determine all potential correlations between differences in ROM and other variables. When referring to sagittal pre- and postoperative values, we defined positive values as lordosis, and negative values as kyphosis. When examining overall changes in ROM, a positive value indicates a gain of motion and a negative value indicates a loss of motion.
Figure 2.
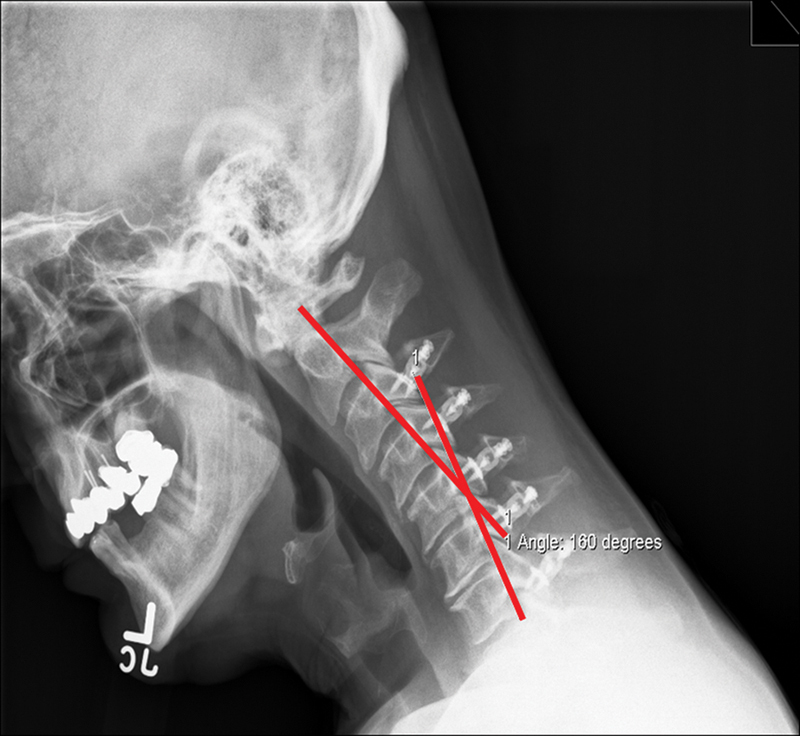
Posterior tangent method. The posterior tangent method involves the measurement of the angle created by the vertex of two lines shown here in red: the posterior body of C2 and the posterior body of C7.
Results
The cohort consisted of 15 male subjects with a mean age of 51.2 years with a mean follow-up of 14.8 months. There were no intraoperative or perioperative complications such as dural injuries or neurological deterioration. There was one postoperative infection that was treated with two serial debridements and maintenance of the instrumentation. Of the 15 patients who underwent ODL with preservation of all posterior structures, five underwent ODL from C4 to C7, seven from C3 to C7, and four from C3 to C6. Overall, eight underwent four-level laminoplasty and seven underwent five-level laminoplasty (Table 1, Fig. 3). When examining these patients separately, the average change in arc ROM was 13.4 ± 12.37 degrees in those undergoing five-level laminoplasty, and 0.53 ± 6.95 degrees in those patients undergoing four-level laminoplasty at a mean 14.8-month follow-up. The greatest change in arc ROM for any patient undergoing four-level laminoplasty was 11.95 degrees. The average preoperative neutral angle, as determined radiographically utilizing the posterior tangent method, was 9.8 ± 9.75 degrees (95% confidence interval [CI]: 4.4 to 15.2; i.e., 9.8 degrees of lordosis). Postoperatively, the neutral angle was 6.8 ± 11.5 degrees (95% CI: 0.5 to 13.1), representing a loss of lordosis of 3 degrees that was not statistically significant (p > 0.05). The preoperative angle of the patient in full extension was 20.5 ± 7.3 degrees (CI: 16.4 to 24.6) and at postoperative analysis was 17.2 ± 11 degrees (CI: 11.2 to 23.3). This was not a statistically significant change. The preoperative angle of the patient in full flexion was −19.2 ± 8.0 degrees (CI: 14.7 to 23.6), and analysis postoperatively was −16.4 ± 10.4 degrees (CI: 10.7 to 22.2), p > 0.05. The arc ROM (measure of extension subtracted by flexion) was 39.6 ± 7.5 degrees (CI: −33.3 to 43.8) preoperatively and 33.7 ± 12.3 degrees (CI: 26.9 to 40.5) postoperatively (p = 0.004). The difference between the preoperative and postoperative arc ROM was 5.96 ± 11.9 degrees (CI: −0.62 to 12.5). The average percentage loss of motion was 3.5% ± (0.1 to 6.9%). Overall, four patients had an increased ROM postoperatively, and 11 patients had a decreased ROM as determined by changes in arc ROM.
Table 1. Pre- and Postoperative Range of Motion Values.
| Position | Preoperative | Postoperative | p Value |
|---|---|---|---|
| Neutral | 9.8 ± 9.75 (4.4–15.2) | 6.8 ± 11.5 (0.5–13.1) | NS |
| Extension | 20.5 ± 7.3 (16.4–24.6) | 17.2 ± 11 (11.2–23.3) | NS |
| Flexion | −19.2 ± 8 (−14.7–23.6) | −16.4 ± 10.4 (−10.7–22.2) | NS |
| Arc ROM | 39.6 ± 7.5 (33.3–43.8) | 33.7 ± 12.3 (26.9–40.5) | 0.004 |
ROM, range of motion; NS, not significant.
Figure 3.

Case example: Pre- and postoperative range of motion. This 52-year-old man presented with a several-year history of progressive bilateral arm pain and numbness, along with gait and fine motor skills difficulties over the past year. Postoperatively, he had complete resolution of pain, numbness, and motor symptoms. (A–C) Plain films demonstrating preoperative neutral, flexion, and extension views, and (D–F) postoperative comparison films.
Bivariate analysis showed no significant correlations between the age of patients and their ROM. Additionally, there were no significant correlations between any preoperative values of the neutral, flexion, or extension positions and ROM outcomes. Based upon the review of all radiographs and CT scans, there were no cases of construct failure. Specifically, there was no lucency or migration of the screws or plate fracture or migration, and all laminae were maintained in the open position at terminal radiographic follow-up (average 14.8 months). The strut allograft consolidation rate was 54.5%, and the hinge healing rate was 87.2%.
Discussion
Cervical ODL is a well-characterized procedure used to treat cervical myelopathy. It is typically associated with loss of ROM, and certain studies have documented loss of sagittal alignment.1 2 3 8 9 10 The precise reason for the loss of motion remains elusive; however, there are several potential causes including postoperative axial pain, facet joint arthrosis/facet joint autofusion, and paraspinal muscle dysfunction. Similarly, it is not entirely clear why many patients lose sagittal alignment to varying degrees postoperatively. Most published studies on ODL suggest that there is disruption of the posterior tension band (i.e., removal of intervening supraspinous and interspinous ligaments, spinous processes, etc.).1 2 3 8 9 10 It is most logical to presume that removal or disruption of the posterior tension band during laminoplasty underlies the kyphogenic potential of cervical laminoplasty. Therefore, the hypothesis of this study was that preservation of all posterior structures would positively influence postoperative alignment (i.e., preservation) and possibly ROM (i.e., smaller loss).
ODL with preservation of all posterior structures provided greater mean preservation of motion than has been previously described. Additionally, this is the first report showing that an increased mean ROM is also possible following ODL, as was seen in 4 of the 15 patients in the study. The average 3.5% loss of motion (5.96 degrees) that was identified in the present study is less than previously reported estimates, which include a study from 2009 that reported a loss ranging between 17% and 80%,11 and a study by Kang et al in 200712 that reported a mean loss of 9.54 degrees of motion (Table 2). Several studies have shown that preserving the ligamentous structures in the cervical spine can potentially reduce postoperative pain levels.13 14 15 16 It follows from these studies that preserving posterior structures may possibly assist in the maintenance, and potentially even a gain, of physiological ROM.
Table 2. Range of Motion Preservation Reported Since 2003.
| Study | Technique | No. of Patients | Follow-Up | Postoperative Range of Motion |
|---|---|---|---|---|
| Chiba et al, 20061 | ODL | 80 | 14 y | −36% |
| Kang et al, 200712 | ODL | 20 | 19.45 mo | −31.8% |
| Takeuchi et al, 200716 | ODL | 70/41 | 19/30 mo | −47.4%/−19.2% |
| Hyun et al, 200911 | ODL | 23 | 26.78 mo | −31.66% |
| Kotani et al, 200914 | ODL | 42/42 | 43 mo | Not given |
| Otani et al, 20092 | ODL | 13 | 5 y | −13.3% |
| Sakaura et al, 201017 | ODL | 36 | >24 mo | −24.3%/26% |
ODL, open-door laminoplasty.
Recently, Sakaura et al17 reported that preservation of muscles attached to C2 and C7 spinous processes was more important than preserving the subaxial deep extensors in reducing unfavorable outcomes after laminoplasty. Particularly with regard to ROM, they showed no statistical difference between those patients with deep muscle preservation versus those undergoing traditional ODL (−26% versus −24.3%, respectively). The authors concluded that the temporally demanding preservations of deep structures were unnecessary when preserving superficial attachments from C2 to C7. The study by Sakaura et al is not necessarily in conflict with the present study data, as the presented technique preserves both deep extensors and more superficial muscle groups.17 The preservation of the extensor muscles is accomplished by elevating, instead of ligating, them during the procedure. The interspinalis muscles are likely denervated during this procedure, yet the clinical implication of this is not known. It is difficult to tease out the necessity of the deep extensors, but when provided with the preservation of ROM found in the present study, it can be argued that some combination of both approaches may facilitate better outcomes.
In the present study, the loss of ROM in four-level laminoplasty (0.53 degrees) was significantly lower than that of five-level laminoplasty (13.4 degrees). When taking into account that many previously reported ROM values are done on the analysis of surgeries involving four levels or less, these results are particularly salient. The value we obtained for the five-level laminoplasty matches that of at least one other study by Kang et al in 2007.12 The nearly 13-degree difference in loss of ROM between these two procedures may be due to the fact that the five-level laminoplasty often involves C7, which is thought to play an important role maintaining cervical spine stability and preserving muscle/ligament attachments. As there is limited research on this area, further studies to examine the use of this technique in four- and five-level laminoplasty will be necessary. Although lateral radiographs have comprised the basis of these results, we have utilized CT and magnetic resonance imaging in a subset of patients to determine the results of laminoplasty in regard to distribution and settling of posterior tissues. It was found that the paraspinal muscle attachment occurred in an apparent anatomical manner.
It is important to note that a study by Tani et al in 200218 reported a loss of ROM of only 7.26 degrees among patients undergoing laminoplasty for cervical myelopathy. Discretion should be used when attempting to draw parallels to this study. First, only 3 of their 30 patients underwent five-level laminoplasty, and the majority underwent three- and four-level laminoplasty.19 None of their patients underwent laminoplasty to C7. Ceramic spacers were only placed at two levels and then fixed. In the present study, allografts were applied to all levels and then fixed by miniplates. These differences may have significant effects on the outcome of both studies.
Several important factors must be considered in the interpretation of our results. The first is the value of loss of ROM between the preoperative and postoperative period. This study presents a loss of only 5.96 ± 11.9 degrees. Initially, the standard deviation presented seems abnormally broad. However, it is necessary to include the four patients who gained motion in the analysis. The large standard deviation is due to these patients who had greater ROM postoperatively. The authors are also aware of the inherent difficulty in interpreting pre- and postoperative images in the flexion and extension positions. These images may be affected by patient compliance with the radiographic technician and the presence of neurological symptoms with neck motion and neck pain. The postoperative activity regimen of choice may also influence eventual retention of ROM. All patients in this study transitioned to a soft collar and started on active flexion, extension, and rotation exercises on postoperative day 1. This decision may have also impacted the results. Not all surgeons utilize this postoperative regimen, and currently there is limited literature of the effects of perioperative motion on the eventual ROM following cervical laminoplasty. Although this rehabilitative aspect is not the main focus of this study, it may have a substantial bearing on the patients' eventual outcomes. The lack of literature on this subject leads to a surgeon-dependant movement regimen postoperatively, and it is difficult to tease out the benefits of motion preservation techniques that are emphasized in the operating room versus those conducted on the surgical ward and in the perioperative period.
The limitations of this study are well recognized. It is a retrospective review of a small number of male patients, with no control group, treated by one surgeon. The results, however, indicate that this variation of ODL may have merit, especially in the context of the preservation of motion reported when compared with previous studies. A prospective study is indicated to further assess the clinical and radiographic outcomes of this procedure.
Disclosures
Kalil G. Abdullah, None
Takayuki Yamashita, None
Michael P. Steinmetz, Consulting: Biomet Spine
Daniel Lubelski, None
Jeffrey C. Wang, Royalties: Medtronics, Stryker, Seaspine, Osprey, Aesculap, Biomet, Amedica, Zimmer, Synthes; Stock Ownership: Fziomed; Private Investments: Promethean Spine, Paradigm Spine, Benevenue, NexGen, K2 Medical, Pioneer, Amedica, Vertiflex, Electrocore, Surgitech, Axiomed; Board of Directors: North American Spine Society, Cervical Spine Research Society, AO Spine/AO Foundation; Scientific Advisory Board: VG Innovations, Corespine, Expanding Orthopaedics, Syndicom, Osprey, Amedica, Bone Biologics, Curative Biosciences, PearlDiver, Inc., Pioneer, Seaspine
Edward C. Benzel, None
Thomas E. Mroz, Stock Option: PearlDiver, Inc.; Consultant: Globus Medical; Speaking Honorarium: AO Spine: Fellowship Support: OREF, NREF, AO Spine
References
- 1.Chiba K, Ogawa Y, Ishii K. et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine. 2006;31:2998–3005. doi: 10.1097/01.brs.0000250307.78987.6b. [DOI] [PubMed] [Google Scholar]
- 2.Otani K, Sato K, Yabuki S, Iwabuchi M, Kikuchi S. A segmental partial laminectomy for cervical spondylotic myelopathy: anatomical basis and clinical outcome in comparison with expansive open-door laminoplasty. Spine. 2009;34:268–273. doi: 10.1097/BRS.0b013e318195b27a. [DOI] [PubMed] [Google Scholar]
- 3.Wang M Y Green B A Open-door cervical expansile laminoplasty Neurosurgery 200454119–123.; discussion 123–124 [DOI] [PubMed] [Google Scholar]
- 4.Ratliff J K, Cooper P R. Cervical laminoplasty: a critical review. J Neurosurg. 2003;98(3, Suppl):230–238. doi: 10.3171/spi.2003.98.3.0230. [DOI] [PubMed] [Google Scholar]
- 5.Gore D R, Sepic S B, Gardner G M. Roentgenographic findings of the cervical spine in asymptomatic people. Spine. 1986;11:521–524. doi: 10.1097/00007632-198607000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Harrison D E, Harrison D D, Cailliet R, Troyanovich S J, Janik T J, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000;25:2072–2078. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 7.Shrout P E, Fleiss J L. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 8.Lee T T, Manzano G R, Green B A. Modified open-door cervical expansive laminoplasty for spondylotic myelopathy: operative technique, outcome, and predictors for gait improvement. J Neurosurg. 1997;86:64–68. doi: 10.3171/jns.1997.86.1.0064. [DOI] [PubMed] [Google Scholar]
- 9.Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine. 1994;19:507–510. doi: 10.1097/00007632-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Satomi K, Ogawa J, Ishii Y, Hirabayashi K. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J. 2001;1:26–30. doi: 10.1016/s1529-9430(01)00008-0. [DOI] [PubMed] [Google Scholar]
- 11.Hyun S J, Rhim S C, Roh S W, Kang S H, Riew K D. The time course of range of motion loss after cervical laminoplasty: a prospective study with minimum two-year follow-up. Spine. 2009;34(11):1134–1139. doi: 10.1097/BRS.0b013e31819c389b. [DOI] [PubMed] [Google Scholar]
- 12.Kang S-H, Rhim S-C, Roh S-W, Jeon S-R, Baek H-C. Postlaminoplasty cervical range of motion: early results. J Neurosurg Spine. 2007;6:386–390. doi: 10.3171/spi.2007.6.5.386. [DOI] [PubMed] [Google Scholar]
- 13.Hosono N, Sakaura H, Mukai Y, Yoshikawa H. The source of axial pain after cervical laminoplasty-C7 is more crucial than deep extensor muscles. Spine. 2007;32:2985–2988. doi: 10.1097/BRS.0b013e31815cda83. [DOI] [PubMed] [Google Scholar]
- 14.Kotani Y, Abumi K, Ito M. et al. Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle-preserving approach: impact on cervical spine function and quality of life. Eur Spine J. 2009;18:663–671. doi: 10.1007/s00586-009-0892-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sakaura H, Hosono N, Mukai Y, Oshima K, Iwasaki M, Yoshikawa H. Preservation of the nuchal ligament plays an important role in preventing unfavorable radiologic changes after laminoplasty. J Spinal Disord Tech. 2008;21:338–343. doi: 10.1097/BSD.0b013e3181453de4. [DOI] [PubMed] [Google Scholar]
- 16.Takeuchi K, Yokoyama T, Ono A. et al. Cervical range of motion and alignment after laminoplasty preserving or reattaching the semispinalis cervicis inserted into axis. J Spinal Disord Tech. 2007;20:571–576. doi: 10.1097/BSD.0b013e318046363a. [DOI] [PubMed] [Google Scholar]
- 17.Sakaura H, Hosono N, Mukai Y, Fujimori T, Iwasaki M, Yoshikawa H. Preservation of muscles attached to the C2 and C7 spinous processes rather than subaxial deep extensors reduces adverse effects after cervical laminoplasty. Spine. 2010;35:E782–E786. doi: 10.1097/BRS.0b013e3181d34614. [DOI] [PubMed] [Google Scholar]
- 18.Tani S Isoshima A Nagashima Y Tomohiko Numoto R Abe T Laminoplasty with preservation of posterior cervical elements: surgical technique Neurosurgery 20025097–101.; discussion 101–102 [DOI] [PubMed] [Google Scholar]
- 19.Geck M J, Eismont F J. Surgical options for the treatment of cervical spondylotic myelopathy. Orthop Clin North Am. 2002;33:329–348. doi: 10.1016/s0030-5898(02)00002-0. [DOI] [PubMed] [Google Scholar]


