Abstract
While intraoperative three-dimensional fluoroscopy does not possess the resolution and image quality of computed tomography (CT), it may provide adequate information about screw placement to guide intra- and postoperative decision making. We compared the accuracy of intraoperative three-dimensional fluoroscopy visualization of proper screw placement with that of postoperative CT. We retrospectively reviewed spinal instrumentation procedures done using the O-arm (Medtronic, Minneapolis, MN, USA) that also had postoperative CT. All screws were assessed for placement accuracy on O-arm and CT images on a 4-point scale. In this study, 20 cases met the inclusion criteria. Thirteen breaches (11 grade 1 and 2 grade 2) were identified on O-arm images, and 14 breaches (10 grade 1, 3 grade 2, and 1 grade 3) were identified on CT. Sensitivity, specificity, and positive and negative predictive values were 93, 99, 99, and 98%, respectively. The Kappa value (0.96) suggested a very high degree of agreement between three-dimensional fluoroscopy and CT in determining accuracy of screw placement. These findings may allow less frequent use of postoperative CT scans, improving cost effectiveness in patients who require spinal instrumentation procedures and potentially decreasing the number of patients who require replacement of an inappropriately positioned screw.
Keywords: O-arm, three-dimensional fluoroscopy, computed tomography scan, accuracy, spinal instrumentation
Introduction
The O-arm™ Surgical Imaging System first received clearance from the U.S. Food and Drug Administration in 2005 for use as an intraoperative imaging system able to produce both two-dimensional and three-dimensional anatomical views. The O-arm has proven to play a valuable role in neurosurgical, orthopedic, and otolaryngologic procedures by providing rapid, quality views of bony anatomy. In particular, three-dimensional fluoroscopy performed intraoperatively is often used as a means to evaluate screw placement during spinal instrumentation.1 In a prospective interventional case study of 94 patients in 2009, the rate of screw misplacement with the use of intraoperative three-dimensional fluoroscopy was 4.8%, compared with 10% without the use of intraoperative three-dimensional fluoroscopy.1
An O-arm image of the appropriate levels can be obtained before or after placement of spinal instrumentation, and the images are then transferred to the computer workstation where they are reconstructed into axial, sagittal, and coronal views of the spinal anatomy.2 In addition, the O-arm allows for intraoperative navigation, further increasing the accuracy of screw placement.3 This has important ramifications as the use of three-dimensional fluoroscopy with or without surgical navigation may help decrease the number of patients who require additional surgery for repositioning of a misplaced screw.4 Finally, three-dimensional fluoroscopy also has the advantage of decreasing radiation exposure to both surgical staff and patients compared with that resulting from a standard computed tomography (CT) scan.5 6 7 8
At our institution, the O-arm is used for a wide variety of cases, including cervical, thoracic, and lumbar spinal instrumentation, thoracic disk herniations, spinal trauma, spinal deformity, and spinal tumors. Although postoperative imaging is often not routinely performed at every institution in the absence of a new neurological deficit, it is our standard to obtain a CT scan after instrumented spine surgery unless the procedure solely entails placement of cervical lateral mass screws. The goal of our study was to compare the images obtained using three-dimensional fluoroscopy intraoperatively with the images obtained on postoperative CT scan for equivalent visualization of instrumentation placement.
Methods
We retrospectively reviewed all neurosurgical spinal instrumentation procedures done at our institution by the senior authors using the O-arm from June 2009 to May 2010. Neither senior author evaluated their own cases. The primary author, who was not involved in any of the cases in this study, evaluated each procedure independently. All surgical approaches and instrumentation systems were included in this study. Cases in which no postoperative CT was obtained were excluded.
The placement of all screws was assessed on both the O-arm and CT images using the method described by Rao et al9 (Table 1) to determine the number of violations of the pedicle (breaches) and their severity. The imaging data were obtained directly from the O-arm workstation, and screw placement was assessed independently by each author at separate times and locations to help avoid bias. Any discrepancies were reviewed by all three authors together, and the majority decision was used. The sensitivity, specificity, positive and negative predictive values, and Kappa value of the measurements were calculated. The Kappa value is a reliability test used to determine observed agreement between different measuring techniques.10 Our aim was to determine how these two methods for determining the accuracy of screw placement compared with one another.
Table 1. Rao Grading Scale for Assessment of Screw Placement7 .
| 0 | No perforation of the pedicle (no breach) |
| 1 | <2 mm perforation with one screw thread out of the pedicle |
| 2 | 2–4 mm perforation of the pedicle |
| 3 | >4 mm perforation |
Results
Of the 47 posterior spinal fusions done at our institution during the study period, 26 cases performed with O-arm fluoroscopic guidance were identified. We identified 20 cases in which both postinstrumentation O-arm images and postoperative CT images were available. These included eight cervical, four cervicothoracic, two thoracic, three thoracolumbar, and three lumbosacral cases. Six cases were identified in which no postoperative CT scan was obtained or the O-arm images could not be located for analysis and were excluded. Fifteen, 36, and 22 screws were placed in the cervical, thoracic, and lumbosacral spine, respectively, for a total of 73 screws. Cervical lateral mass screws were not included. We identified a total of 11 breaches (9 grade 1, 2 grade 2) on the O-arm, and 11 breaches (7 grade 1, 3 grade 2, and 1 grade 3) on postoperative CT scan (Figs. 1 and 2). These data were then grouped for statistical analysis evaluating accuracy of the O-arm in identifying screw breach compared with postoperative CT scan. Sensitivity and specificity for the use of three-dimensional fluoroscopy were 85 and 97%, respectively. Positive and negative predictive values were calculated to be 82 and 98%, respectively. The Kappa value was 0.79, suggesting a substantial degree of agreement between three-dimensional fluoroscopy and CT scan in determining accuracy of screw placement.
Figure 1.
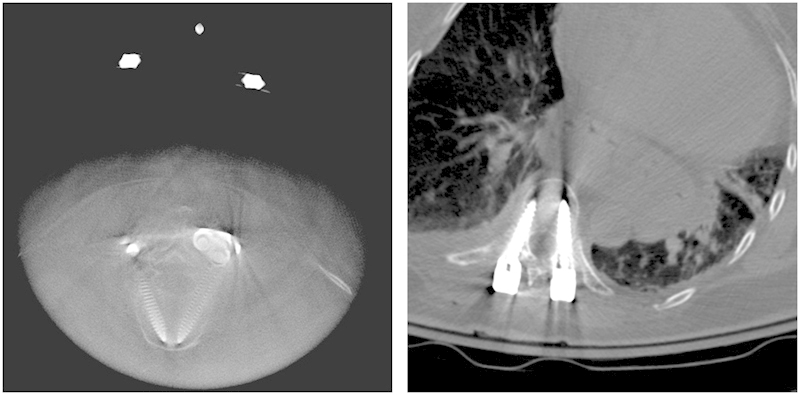
(Left) O-arm fluoroscopic image showing breach of a T9 pedicle screw in a patient with a thoracic fusion. The breach was identified as grade 0. (Right) Computed tomography scan showing the same pedicle screw breach, which was identified as a grade 1 breach on this image.
Figure 2.
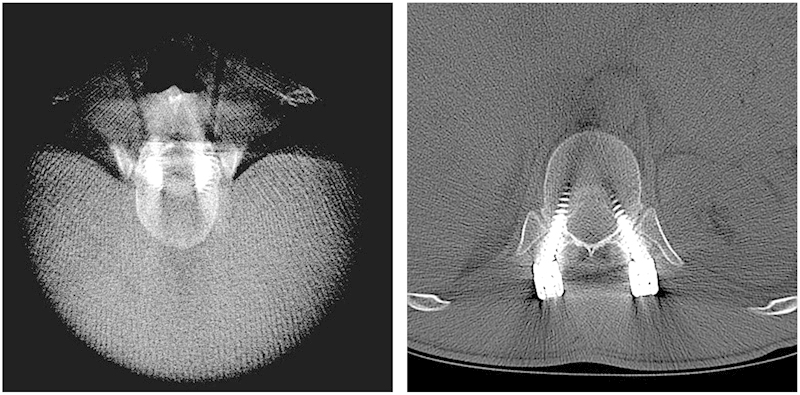
O-arm (left) and computed tomography scan (right) showing no breach (grade 0) in a patient with a thoracolumbar fusion.
Discussion
Our results indicate that three-dimensional fluoroscopy was highly accurate in evaluating screw placement during neurosurgical spine procedures. Furthermore, there was a high level of agreement between the findings obtained using the O-arm and those obtained using CT scan. The discrepancies between the grades imply that CT scan may have been slightly more accurate than the O-arm at picking up a subtle breach of the cortex; however, none of the patients in this study required a return trip to the operating room for repositioning of a misplaced screw, and therefore the discrepancy in visualized grade did not appear to be clinically significant. These data suggest that intraoperative fluoroscopy may be used to analyze the accuracy of screw placement.
This study is not the first to evaluate the accuracy of CT images to determine appropriate screw placement. Rao et al9 evaluated pedicle screw placement performed freehand or using virtual fluoroscopy in eight cadaver spines. A CT scan was then performed after the instrumentation was placed, and screw position was graded based on the CT images and direct visual inspection of each specimen. Using their grading scale, the authors found that there were 32 grade 1 breaches on CT scan and 23 using direct visualization. There were 13 grade 2 breaches on CT scan compared with 10 using direct visualization. There were no grade 3 breaches using either method. The calculated negative predictive value of this study was 62%, indicating that when CT scan showed a breach of the pedicle it was correct only 62% of the time. These numbers would indicate that screw breach evaluated by CT scan had false positives (i.e., overreported the number of misplaced screws) when compared with direct visualization.
In our study, we assumed that CT scan is the gold standard for assessing accurate screw placement as it is still the most common imaging modality used to visualize spinal instrumentation postoperatively. However, we hypothesized that intraoperative three-dimensional fluoroscopy would be equally accurate in identifying a malpositioned screw and would enable correction of the screw trajectory before the end of the operative case.4 11 This could reduce the number of patients who require return trips to the operating room to adjust a malpositioned screw. This has important implications for patient safety as return trips to the operating room increase both cost and morbidity in patients undergoing spinal instrumentation procedures. In addition, visualizing screw placement intraoperatively could decrease the number of postoperative CT scans required and therefore decrease cost and radiation exposure to patients undergoing screw placement. With sensitivity and specificity of 85 and 97%, respectively, intraoperative fluoroscopy is highly accurate in determining correct screw placement in the operating room. In addition, a negative predictive value of 98% suggests that when intraoperative fluoroscopy showed that a screw was correctly placed, it was wrong only 2% of the time. These data are encouraging since proper screw placement is vital both for structural stability and to avoid crucial anatomical structures.
Another important benefit of the use of intraoperative three-dimensional fluoroscopy for evaluation of screw placement is that it potentially exposes the patient to less radiation than a postoperative CT scan. In a 2010 study done at a university hospital in England, Richards et al12 calculated radiation dosage of lumbar and thoracic CT scans in mSv (estimated effective dose). Their results showed that imaging the thoracic spine exposed the patient to 10 mSv, while imaging the lumbar spine exposed the patient to 5.6 mSv. In a 2002 study, Rybicki et al13 reported that imaging the cervical spine exposed the patient to 3.45 mSv. Zhang et al8 investigated patient radiation dose using an O-arm imaging system versus a 64-slice CT imaging system. The Richards et al and Zhang et al studies both evaluated the use of these systems using synthetic spines instead of actual patients. Zhang et al showed that when using the same scan length and identical radiographic techniques, the three-dimensional O-arm imaging system delivered approximately half the radiation dose of a 64-slice CT scanner, which is similar to the one used at our institution. The results of these two studies imply that using intraoperative three-dimensional imaging does impart less radiation to the patient than conventional CT.
A limitation of our study is the small number of patients at our institution for whom both intraoperative three-dimensional fluoroscopy and a postoperative CT scan were available. As stated earlier, postoperative CT scans are routinely obtained at our institution after instrumented spine surgery. One potential bias with a retrospective study such as this one is that cases that did not have a postoperative CT scan may have been considered safely performed surgical procedures, and therefore CT scan was only performed when the surgeon was concerned about a malpositioned screw. A diligent chart review was performed to determine that this was not the case based on postoperative notes and discharge summaries. However, as three-dimensional fluoroscopy grows in popularity, we hope to undertake a prospective comparative analysis that would eliminate this bias and lead to larger case series available for analysis.
Another limitation of this study is the difference in the number of posterior spinal fusions done during the study period (47) and the number of cases in which the O-arm was used intraoperatively (26). Of these 26 cases, 20 used both intraoperative O-arm and postoperative CT scan for evaluation of screw placement. It is quite possible that in some of the 20 cases, both intraoperative O-arm and postoperative CT scan were used because of a concern by the operating surgeon for a pedicle screw breach; this would account for the positive correlation between O-arm and CT scan in picking up a violation of the cortex. The degree of pedicle rupture was independently evaluated by three neurosurgeons (the authors of this study), so it is doubtful that error in pedicle breach grade could have made a significant contribution to the results obtained. Certainly, a prospective study whereby patients undergoing posterior spinal fusions were randomized to either intraoperative O-arm imaging or postoperative CT imaging to evaluate accuracy in screw placement would be valuable to help eliminate operating surgeon bias and establish whether one modality is superior to another in evaluating pedicle screw placement.
Conclusion
The results of our study show that intraoperative three-dimensional fluoroscopy was highly accurate in the evaluation of screw placement during neurosurgical spine procedures. We believe that this allows for the ability to correct screw trajectory intraoperatively, potentially decreasing the number of patients who might have to return to the operating room for repositioning of a misplaced screw identified on postoperative CT scans. In addition, our data may enable a decreased use of postoperative CT scans and further ensure both quality and safety in patients who require spinal instrumentation.
Acknowledgment
We thank Kristin Kraus, M.Sc., for editorial assistance.
Disclaimer
None of the authors involved in this study is affiliated with Medtronic, and no funding was received from Medtronic for use in this project.
Disclosures
Sarah T. Garber, None
Erica F. Bisson, None
Meic H. Schmidt, None
References
- 1.Zausinger S, Scheder B, Uhl E, Heigl T, Morhard D, Tonn J C. Intraoperative computed tomography with integrated navigation system in spinal stabilizations. Spine (Phila Pa 1976) 2009;34(26):2919–2926. doi: 10.1097/BRS.0b013e3181b77b19. [DOI] [PubMed] [Google Scholar]
- 2.Holly L T Foley K T Image guidance in spine surgery Orthop Clin North Am 2007383451–461., abstract viii [DOI] [PubMed] [Google Scholar]
- 3.Geerling J, Gösling T, Gösling A. et al. Navigated pedicle screw placement: experimental comparison between CT- and 3D fluoroscopy-based techniques. Comput Aided Surg. 2008;13(3):157–166. doi: 10.3109/10929080802102110. [DOI] [PubMed] [Google Scholar]
- 4.Sugimoto Y, Ito Y, Tomioka M. et al. Clinical accuracy of three-dimensional fluoroscopy (IsoC-3D)-assisted upper thoracic pedicle screw insertion. Acta Med Okayama. 2010;64(3):209–212. doi: 10.18926/AMO/40014. [DOI] [PubMed] [Google Scholar]
- 5.Kim C W, Lee Y P, Taylor W, Oygar A, Kim W K. Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J. 2008;8(4):584–590. doi: 10.1016/j.spinee.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Rampersaud Y R, Foley K T, Shen A C, Williams S, Solomito M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 2000;25(20):2637–2645. doi: 10.1097/00007632-200010150-00016. [DOI] [PubMed] [Google Scholar]
- 7.Smith H E, Welsch M D, Sasso R C, Vaccaro A R. Comparison of radiation exposure in lumbar pedicle screw placement with fluoroscopy vs computer-assisted image guidance with intraoperative three-dimensional imaging. J Spinal Cord Med. 2008;31(5):532–537. doi: 10.1080/10790268.2008.11753648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang J, Weir V, Fajardo L, Lin J, Hsiung H, Ritenour E R. Dosimetric characterization of a cone-beam O-arm imaging system. J XRay Sci Technol. 2009;17(4):305–317. doi: 10.3233/XST-2009-0231. [DOI] [PubMed] [Google Scholar]
- 9.Rao G, Brodke D S, Rondina M, Dailey A T. Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg. 2002;97(2, Suppl):223–226. doi: 10.3171/spi.2002.97.2.0223. [DOI] [PubMed] [Google Scholar]
- 10.Rao G, Brodke D S, Rondina M, Bacchus K, Dailey A T. Inter- and intraobserver reliability of computed tomography in assessment of thoracic pedicle screw placement. Spine (Phila Pa 1976) 2003;28(22):2527–2530. doi: 10.1097/01.BRS.0000092341.56793.F1. [DOI] [PubMed] [Google Scholar]
- 11.Nottmeier E W, Young P M. Image-guided placement of occipitocervical instrumentation using a reference arc attached to the headholder. Neurosurgery. 2010;66(3, Suppl Operative):138–142. doi: 10.1227/01.NEU.0000346264.66833.B3. [DOI] [PubMed] [Google Scholar]
- 12.Richards P J, George J, Metelko M, Brown M. Spine computed tomography doses and cancer induction. Spine (Phila Pa 1976) 2010;35(4):430–433. doi: 10.1097/BRS.0b013e3181cdde47. [DOI] [PubMed] [Google Scholar]
- 13.Rybicki F, Nawfel R D, Judy P F. et al. Skin and thyroid dosimetry in cervical spine screening: two methods for evaluation and a comparison between a helical CT and radiographic trauma series. AJR Am J Roentgenol. 2002;179(4):933–937. doi: 10.2214/ajr.179.4.1790933. [DOI] [PubMed] [Google Scholar]


