Abstract
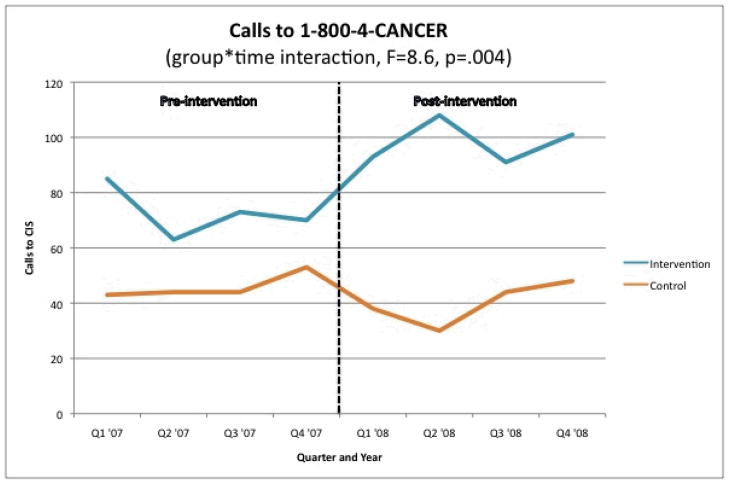
This study tested the feasibility of promoting 1-800-4-CANCER through partnerships with organizations serving African American and Hispanic communities. Small media and client reminders about HPV vaccination were made available through local agents to 28 community organizations. Organizations ordered 79,932 resources and distributed them to young women and parents of girls – African Americans in St. Louis, MO and Hispanics in the Lower Rio Grande Valley of Texas. Pre-to post-intervention calls to 1-800-4-CANCER increased 38% in these communities, while declining 15% in comparison communities of Kansas City, MO and El Paso, TX (F=8.6, p=.004) and 1.4% in the U.S. as a whole.
Keywords: Health disparities, HPV vaccination, African American, Hispanic, community health
Low levels of awareness and use of the National Cancer Institute’s (NCI) Cancer Information Service (CIS) among African Americans and Hispanics have been documented for over two decades.1,2 Recent findings from the Health Information National Trends Survey (HINTS) indicated that 45% of African Americans and 51% of Hispanics were aware of either the Cancer Information Service or its 1-800-4-CANCER telephone service,3 but awareness and use are much lower in surveys of low-income minority populations.4 Effective and sustainable promotion strategies are needed to assure that all Americans benefit from this important cancer information resource.
To date, most efforts to promote the use of NCI resources among African Americans and Hispanics have involved targeted mass media campaigns. These campaigns have generally been successful in increasing call activity to 1-800-4-CANCER,5–7 though some effects have been modest. Success of media-based promotion of CIS depends largely on intensity and duration of campaign exposure, both of which are maximized with paid advertising. But those costs are hard to sustain,5 and call volume in these campaigns returns to baseline levels when the campaign ends.6
In a 2004 review of 28 campaigns and 24 review articles, Randolph & Viswanath concluded that failure to address campaign sustainability is “one of the biggest gaps in the literature.”8 This may be a particular challenge for reaching certain population sub-groups. A 2008 review of 18 studies found that campaigns to promote smoking cessation and use of a telephone quitline were commonly less effective in low-income populations.9 To overcome these limitations, recommendations include involving community organizations as intermediaries and distribution channels for CIS information, and increasing interpersonal outreach in community settings.10,11
The CIS Partnership Program was established with these recommendations in mind, aiming to increase cancer knowledge and awareness in medically underserved populations by working collaboratively with established organizations that shared similar goals.12 The Partnership Program (recently replaced by NCI’s National Outreach Network13) developed long-term relationships with local, regional and national organizations for the purposes of sharing information and networking, jointly developing projects using evidence-based approaches to increase cancer prevention and control in minority and medically underserved populations, and increasing the capacity of partners to move science into practice.
This approach is consistent with the Integrated System Framework (ISF) for dissemination and implementation of prevention services.14 The ISF model proposes that there are three systems needed to carry out the functions of translating research evidence into prevention practice. The Prevention Synthesis and Translation System helps make research products more easily accessible and usable for practitioners. The Prevention Support System provides general and intervention-specific support to build capacity for implementation in adopting organizations. The Prevention Delivery System executes the activities needed to implement evidence-based programs. Community partnerships such as those cultivated by the CIS Partnership Program are particularly important in this third system.
In this study, a team of CIS Research Program and Partnership Program staff worked collaboratively with academic researchers to test the feasibility of promoting awareness and use of 1-800-4-CANCER through partnerships with community-based organizations that serve African American and Hispanic populations. Specifically, the research team and community partners worked together to develop a range of information resources (e.g., letters, posters, pamphlets, quizzes, referral cards, photonovellas, PowerPoint presentations) that promote 1-800-4-CANCER as a source of information about HPV vaccination. Such small media and patient reminder interventions are evidence-based approaches to cancer control.15,16 These resources were then made available through CIS’s Partnership Program to community organizations that served members of the target populations eligible for the vaccine - young African American and Hispanic women ages 18 to 26, and parents of African American and Hispanic girls ages 9 to 17. We tested this approach among organizations in St. Louis, MO (for African Americans) and the Lower Rio Grande Valley of Texas (for Hispanics), with comparison communities in Kansas City, MO and El Paso, TX.
Feasibility testing conducted in real world settings is an essential step in building practice-based evidence17 and identifying interventions worthy of evaluation in efficacy and effectiveness studies.18 Bowen and colleagues propose eight types of outcomes that can be addressed in feasibility studies – acceptability, demand, implementation, practicality, adaptation, integration, expansion and limited-efficacy.18 The present study addresses three of these: (1) demand (Is the intervention needed and used by minority-serving community organizations?); (2) acceptability (Is the intervention perceived as appropriate, attractive and useful to community organizations and those they serve?); and (3) limited efficacy (Does the intervention lead to increased calls to 1-800-4-CANCER?). The Institutional Review Boards at Saint Louis University and The University of Texas Health Science Center at Houston, approved this study.
Methods
Study settings
In St. Louis, MO, the study area included 26 contiguous ZIP codes in north St. Louis City and County, where 60.3% of adults are African American and residents have disproportionately low levels of income and education relative to the metropolitan area.19 Cancer mortality rates for African Americans are higher in this region than state and national averages.20 The Lower Rio Grande Valley study area included 19 ZIP codes in Hidalgo and Cameron Counties on the Texas-Mexico border. The populations of these counties are predominantly Hispanic (89.6% and 86.3% respectively),16 with high levels of poverty and low access to health care services.21 Hispanic women in the Lower Rio Grande Valley have higher rates of cervical cancer and lower rates of cervical cancer screening than White or Hispanic women in Texas and the U.S.22–25 The target populations for the intervention in these communities were African American and Hispanic young women (ages 18 to 26) and parents of girls ages 9 to 17. Community organizations that served this population of African Americans in the St. Louis study area or this population of Hispanics in the Lower Rio Grande Valley were eligible to participate in the study.
Research design
The study used a quasi-experimental design. Interventions were delivered to organizations serving African Americans in north St. Louis, MO and Hispanics in two counties in the Lower Rio Grande Valley on the Texas-Mexico border. Call volume to 1-800-4-CANCER from these study areas was compared pre- and post-intervention launch to geographically proximal areas with similar demographic composition – Kansas City, MO (for African Americans) and El Paso, TX (for Hispanics). In Kansas City, the comparison area included 12 contiguous ZIP codes where 38% of adults are African American and the proportion of residents living below the poverty level (19.4%) is higher than the surrounding metropolitan area.19 In El Paso, the comparison area included 22 contiguous ZIP codes where 87% of residents are Hispanic and 25% live below the poverty level. 16
Intervention
The intervention tested in this study was a menu of information resources that community organizations could choose from, obtain for free, and distribute or display to those they serve. Organizations accessed these resources through a local coordinator in NCI’s Cancer Information Service Partnership Program. Although the resources available in St. Louis and the Lower Rio Grande Valley differed, all shared three common elements: (1) a development process guided by community preferences and with community involvement; (2) a specific call-to-action to contact 1-800-4-CANCER for more information about the HPV vaccine and cervical cancer prevention; and (3) resource types – small media and client reminders – that are recommended for cancer control by the Community Guide.26
Intervention development and delivery in St. Louis
To inform development of HPV information resources for African American young women and parents of girls, we interviewed a community-based convenience sample of 30 women from the target population, as well as five clinical and educational staff members from local Federally Qualified Health Centers (FQHCs) and leaders of six non-clinical community-based organizations that serve the target audiences. The broad goal of these interviews was to identify types of resources and core content that would be interesting to these audiences and effective in prompting information seeking about HPV vaccine. Five types of resources emerged from this process: (1) posters; (2) patient reminder letters; (3) referral cards (i.e., to call 1-800-4-CANCER); (4) conversation cards (providing model questions that could be used to start a conversation about HPV topics commonly raised by the target audience); and (5) self-scoring quizzes (modeled after those in women’s magazines and designed to distinguish between those who will be more passive or active in an encounter with a health care provider).
We created several prototype versions of each resource type and met again with community partners and women in the target audiences to get their reactions. Enthusiasm for the resource types was high and nearly universal, but there was little agreement on which versions of the prototypes (i.e., specific images, designs and messages) were most preferred. In response, we altered the basic intervention approach. Instead of creating a single version of each resource, we created a standard template for each resource, and allowed community partners to select from a discrete set of images, designs and messages to make their own unique version of each resource. We branded this system MIYO© (Make It Your Own), and created a product brochure and order form to allow community partners to designate their choices for image, design and message for each available resource. These choices were used to custom design each resource for each community organization.
From December 2007 to July 2008, the St. Louis Coordinator of the CIS Partnership Program offered MIYO resources to organizations that: (1) served one or both of the target audiences in the target ZIP codes; (2) provided programs or services in settings where women and parents could be exposed to and attend to the resources; and (3) had a mission that was compatible with the project’s health improvement objectives and/or its focus on African American young women, parent and girls. Candidate organizations were identified from existing community partners in the local Cancer Prevention and Control Research Network,27 the Cancer Information Service Partnership Portfolio Database,12 recommendations of CIS, trusted stakeholders from past community partnerships, and attendees at community forums, public health practitioner training events and local health fairs. Priority was given to organizations that belonged to larger systems (e.g., Federally Qualified Health Centers, local public health departments, middle and high schools, community colleges and universities) and non-traditional partners (e.g., trade schools) because they could potentially expand the adoption and reach of the intervention if it was found to be effective.
The Partnership Program Coordinator phoned potential partners to determine whether MIYO resources might be useful to them. Interested organizations were sent sample materials and order forms. When organizations completed and returned an order form, the project team generated each customized resource, printed the desired quantity and delivered the resources to the partner organization. With each delivery of resources, we also gave community partners a standardized tracking form to help them record when, where and how each resource was distributed. From the time of receiving an order, this delivery process took 3–4 weeks.
Intervention development and delivery in the Lower Rio Grande Valley
To inform development of HPV information resources for Hispanic young women and parents of girls, we conducted small group interviews with young women ages 18 to 26 (n=15), women over age 26 (n=16), mothers and fathers of girls ages 9 to 17 (n=28), and promotoras, or lay health workers (n=9). We also interviewed 10 representatives from community organizations including health clinics and service centers, and a health education advocacy coalition. Interviews with the young women and parents yielded valuable information about content that should be included in the HPV resources. For example, knowledge about HPV, the HPV vaccine and the link between HPV and cervical cancer was very low, and many were skeptical about calling 1–800 numbers. Interviews with promotoras and community organization representatives revealed that the type of resources needed to deliver HPV information varied based on three factors: (1) the availability and capacity of computers to deliver the information; (2) the number and type of encounters they had with community members; and (3) the amount of time they could spend in each encounter. Some promotoras, for example, indicated that their programs had recently acquired laptop and tablet computers to facilitate educational outreach, but they did not yet have material available to put on those computers. The prospect of having PowerPoint slides or digital video was appealing to them. The promotoras requested training so that they would be prepared to discuss HPV and the vaccine with the community even though their primary role was to encourage people to call CIS for more information.
Based on this information, we developed five resources: (1) a print photonovella (brief, illustrated, soap opera-like narrative with a storyline built through dialog among characters); (2) an electronic version of the photonovella in PowerPoint, with photographs and text; (3) an electronic version of the photonovella in PowerPoint, with video; (4) a video available in DVD or VHS formats; and (5) conversation cards. The content of these resources addressed HPV-related knowledge gaps, issues and concerns emerging from audience research with young women and parents. To further customize these resources, we created different versions of the photonovella for young women and parents, and in English and Spanish. We also created a training program for promotoras that included a lesson plan, handouts and PowerPoint presentations. These resources were branded Vivir Sin Cancer (“Live without cancer”).
From February to September 2008, the Partnership Program Coordinator for the Lower Rio Grande Valley presented these resources to community partners and made them available for adoption and use. Partners included health care organizations, lay health worker programs, and the Hispanic Health Research Center media campaign Tu Salud Si Cuenta (“Your Health Matters”). The partnership coordinator in the region had established relationships with these organizations when the project started, and contacted them to gauge their interest in participating in the development process, delivering the materials once available, or both. While all CIS Partnership Program contacts expressed interest in participating at some level, organizations serving neighborhoods located in and near the city of Brownsville in Cameron County were the most active during the study period. This county is the poorest in the country and contains unincorporated neighborhoods called “colonias” such as Cameron Park that often lack basic infrastructure.
The CIS Partnership program coordinator visited organizations and described the materials to outreach coordinators, promotoras, and health center decision-makers (e.g., medical directors, health educators). The selection of types of resources depended on the delivery mechanisms available (i.e., whether or not they had DVD players in the waiting room; whether or not they had laptop computers). The CIS Partnership Program Coordinator delivered print photonovellas and question cards to all partners, and contacted partners weekly to restock materials as requested and collect encounter forms and clinic logs.
Measures
The three outcomes of interest in the study are demand for the intervention by minority-serving community organizations, acceptability of the intervention to community organizations, and limited efficacy in increasing calls to 1-800-4-CANCER. Given differences in intervention approaches used in St. Louis and the Lower Rio Grande Valley, some measures varied by study area.
Demand
In both study areas we tracked how many organizations ordered resources, which type of resources they ordered and how many of each resource type they ordered. In St. Louis, we also tracked each organization’s choices of image, message and design for each resource they ordered to determine whether the customization feature of MIYO was necessary. These data were used to determine the proportion of orders that selected a unique combination of image, message and design. In the Lower Rio Grande Valley we delivered all types of material to CIS partners and tracked which were used. When organizations had delivered almost all copies of a resource, they ordered more and the CIS coordinator tracked these orders. Most organizations used promotoras to deliver print photonovellas and conversation cards. Photonovellas were used most often in group settings while conversation cards were used when promotoras went door to door.
Acceptability/use
Distribution and display of the intervention resources was viewed as an indicator that the community partners deemed the materials to be appropriate, attractive and useful to their organization and those they serve. In St. Louis and the Lower Rio Grande Valley, we conducted telephone interviews with each community partner that had ordered any intervention resource. These interviews took place after resources from their final order had been delivered, and asked how many of the resources they received were displayed or distributed, and where and when they were distributed or displayed. We also asked them to describe the populations they intended to receive the resources, and whether they had heard positive or negative comments about the resources from members of that population.
In the Lower Rio Grande Valley, community partners that ordered any intervention resources also used a standardized encounter form to record each educational session in which a promotora presented the resources to an individual or group. Health clinics used a similar form to record the number of times the video played. These forms were collected monthly and tabulated by the project team.
Limited efficacy
The primary study outcome was number of calls to 1-800-4-CANCER originating from the geographically defined study areas for one year prior to intervention launch and one year during intervention delivery. Call data were collected by the CIS using its standard Electronic Call Record Form (ECRF) and made available to the research team for statistical analyses. Time, date, and ZIP code are recorded for each call, and provide the basis for matching call volume to study areas and classifying calls as pre- or post-intervention launch. We also examined ECRF data related to the intervention topic, intervention delivery and target population. These included subject of interaction (HPV vaccine), cancer type (cervical) and how the caller found out about 1-800-4-CANCER (“other printed material”); callers’ sex and race/ethnicity (African American, Hispanic) are collected from a subset of approximately 25% of callers.
Statistical analysis
Descriptive statistics are reported for demand and acceptability/use outcomes. Counts are reported for number and type of intervention resources ordered and distributed or presented by community partners. Proportions are reported for unique combinations of MIYO resources ordered by St. Louis partners, and for responses to selected items from follow-up interviews.
To examine pre-post differences in call volume between targeted ZIP codes in the intervention (St. Louis, Lower Rio Grande Valley) and comparison (Kansas City, El Paso) communities, we used linear regression to test for a time (pre-post) x study condition interaction. Separate models were used for each intervention community and for a pooled analysis.
Descriptive statistics are used to present the proportion of calls from women, African American and Hispanic, about HPV vaccine or cervical cancer, and from callers reporting they heard about 1-800-4-CANCER from “other printed sources.” Because the CIS collects these data from only a 25% subset of callers, the resulting small sample size diminishes the meaning of statistical test results for these outcomes.
Findings
Demand
In St. Louis, 19 community organizations were approached and offered the intervention, and all placed at least one order for HPV information resources targeting either young women (n=19, 100%) or parents (n=16, 84%). Participating organizations included 7 educational institutions (universities, community and trade colleges, public school districts), 4 neighborhood health centers, 4 community- and faith-based organizations, 2 public health departments, an Area Health Education Center and a local health foundation. Collectively, these organizations ordered 56,096 resources, and every type of resource available. On average, each organization ordered 5.1 different types of resources.
In the Lower Rio Grande Valley, resources were offered to and accepted by nine community organizations - 3 clinics, 3 community health centers, and 3 lay health advisor programs. Collectively, these organizations received 23,836 resources of every type available. Table 1 shows the quantity of each resource ordered or received for both study sites.
Table 1.
Community partners’ demand for HPV information resources, by resource type and study site
| Type of resource (audience) | Partners orderinga | Quantity ordered |
|---|---|---|
| St. Louis, MO | ||
| Poster (young women) | 15 | 367 |
| Poster (parents) | 13 | 329 |
| Conversation card (young women) | 16 | 15,350 |
| Conversation card (parents) | 15 | 12,100 |
| Self scoring quiz (young women & parents) | 12 | 10,250 |
| Referral cards (young women & parents) | 14 | 17,700 |
| Patient reminder letter (young women) | 1 | na |
| Patient reminder letter (parents) | 2 | na |
|
| ||
| Total | 19 | 56,096 |
|
| ||
| Lower Rio Grande Valley, TX | ||
| Photonovella, printed (young women) | 9b | 1,140 |
| Photonovella, printed (parents) | 9b | 1,530 |
| Photonovella, PowerPoint (young women) | 9b | 30 |
| Photonovella, PowerPoint (parents) | 9b | 30 |
| Conversation card (young women) | 9b | 12,470 |
| Conversation card (parents) | 9b | 8,520 |
| Video/DVD (young women) | 9b | 17 |
| Video/DVD (parents) | 9b | 23 |
|
| ||
| Total | 9 | 23,836 |
|
| ||
| Total both sites | 28 | 79,932 |
n=19 for St. Louis; n=9 for Lower Rio Grande Valley
For Lower Rio Grande Valley, all resource types were given to each partner, not “ordered”
A secondary indicator of demand applicable only in the St. Louis sample was the extent to which different organizations created different versions of each customizable resource. If most organizations chose the same images, messages and designs when creating their own version of a resource, customization would be an unnecessary feature. Table 2 shows each customizable resource (n=6) available in the study, how many versions could possibly be made, the number of community partners (out of 19) that ordered the resource, and the number of different versions of the product that were actually created by all partners combined. The last column, “value added”, is a measure of the benefit of offering community partners choice in creating their own version of that resource. It indicates the percentage of all partners ordering a resource that created a version different from the most commonly selected version. It is thus a conservative estimate of the percent of partners whose preferences would not have been met had only one version of that product been available. In short, the proportion of organizations that benefited from available customization was high for those ordering posters (77%–87%), conversation cards (73%–81%) and self-scoring quizzes (67%), but less so for referral cards (50%).
Table 2.
Community partners’ demand for customizable HPV information resources, St. Louis site only.
| Type of resource (audience) | Different versions possible | Different partners ordering | Partner versions chosen | Value addeda |
|---|---|---|---|---|
| Poster (young women) | 64 | 15 | 13 | 87% |
| Poster (parents) | 36 | 13 | 11 | 77% |
| Conversation card (young women) | 18 | 16 | 7 | 81% |
| Conversation card (parents) | 18 | 15 | 8 | 73% |
| Self scoring quiz (young women & parents) | 8 | 12 | 5 | 67% |
| Referral cards (young women & parents) | 3 | 14 | 3 | 50% |
percent of partners creating a version of the resource different from the most commonly selected version
Acceptability/use
In St. Louis, follow-up interviews were completed with 17 of 19 community partners that ordered intervention resources. These partners reported distributing or displaying 52,279 of the 56,099 resources they ordered (93%). This percentage varied by type of resource: 100% for posters, 86% for conversation cards, 100% for self-scoring quizzes and 99% for referral cards. Four partners ordered additional copies of resources after their original order had been distributed.
All partners reported delivering resources through direct contact with young women and parents at their physical location. Other distribution strategies varied by partner. Educational institutions reported distributing resources at parent-teacher conferences, in classrooms, in nurses’ offices, and at student health, counseling and campus recreation centers. Neighborhood health centers distributed or displayed resources in waiting rooms, exam rooms and at health fairs. Community- and faith-based organizations delivered resources at community events, open houses and public presentations. Half of the partners (n=10; 59%) reported that they had heard feedback about the resources from their clients, and most reported that comments were “all” (50%) or “mostly” (40%) positive; one respondent reported that comments were “evenly positive and negative.”
In the Lower Rio Grande Valley, partners reported distributing all of the 23,836 resources they had received. One of the major distribution strategies was through educational sessions conducted by the lay health advisor programs. Lay health advisors in these programs used the resources in 2,149 distinct encounters with community members at churches, schools, health fairs and through door-to-door contact. Encounter logs tracking these sessions showed that conversation cards were used 2,074 times (97% of encounters), printed photonovellas 1,192 times (55%), PowerPoint photonovellas 138 times (6%) and the video photonovella 10 times (<1%). Clinics and community health centers made the resources available in exam rooms and showed the video in waiting areas. In addition, an outreach program at the Hispanic Health Research Center in Brownsville, TX distributed monthly newsletters containing conversation cards (n=2,500) to community residents.
Limited efficacy
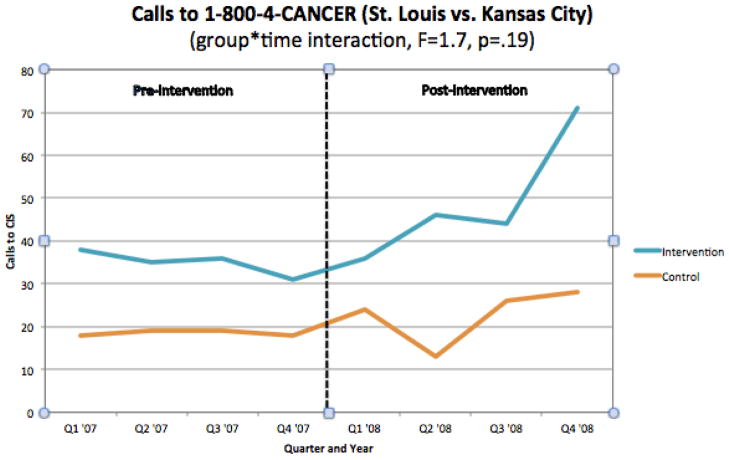
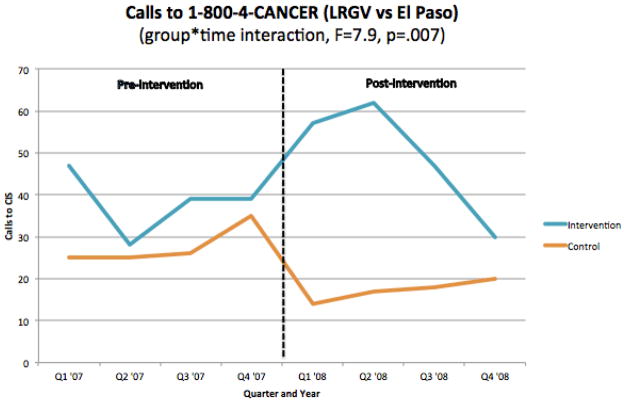
As shown in Figure 1, calls to 1-800-4-CANCER from the designated ZIP codes in St. Louis and the Lower Rio Grande Valley increased from an average of 24 calls per month in the year prior to the intervention to 33 calls per month in the year following intervention launch (+38%). During the same pre- and post-intervention time periods, calls to 1-800-4-CANCER from designated ZIP codes in the comparison communities of Kansas City and El Paso averaged 15.3 and 13.3 per month, respectively (−15%). This study group X time interaction was significant (β=168.01, F=8.6, p=.004). Both intervention sites experienced similar increases in call volume (Figures 2 and 3). In St. Louis, volume rose from an average of 9.2 to 13.5 calls per month (+47%) vs. change from 6.2 to 7.6 calls per month in Kansas City (+23%; β =33.33, F=1.7, p=.19). In the Lower Rio Grande Valley, call volume rose from an average of 12.6 to 16.3 calls per month (+29%) vs. a decline from 9.2 to 5.8 calls per month in El Paso (−59%; β =157.69, F=7.9, p=.007). By comparison, total U.S. calls to 1-800-4-CANCER (including those from ZIP codes in our four study communities) declined from 88,377 to 87,163 (−1.4%) during this period.
Figure 1.
Calls to 1-800-4-CANCER by study group and time.
Figure 2.
Calls to 1-800-4-CANCER by study group and time, Missouri site.
Figure 3.
Calls to 1-800-4-CANCER by study group and time, Texas site.
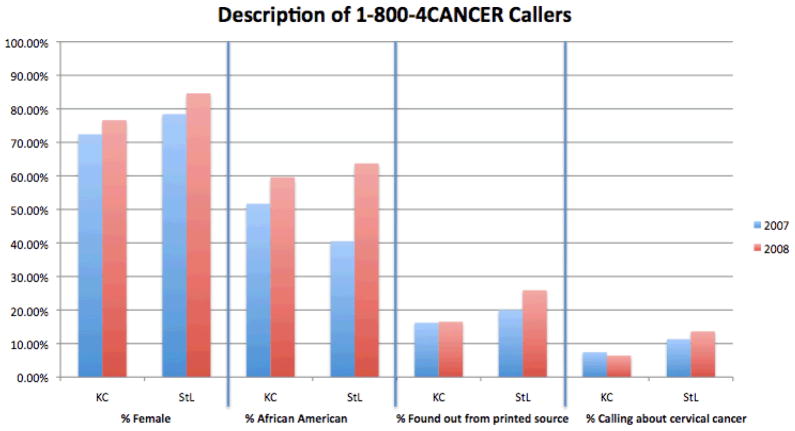
In addition to changes in call volume, we observed changes in caller characteristics and subject of call interactions. In St. Louis, the proportion of calls received from African Americans increased from pre- to post-intervention launch (40% to 64%), as did calls from women (78% to 85%), calls about HPV or cervical cancer (11% to 14%), and calls from those who reported finding out about 1-800-4-CANCER from “other printed sources” (20% to 26%). In each instance, the same changes over time were smaller in magnitude or in the reverse direction in Kansas City. In the Lower Rio Grande Valley, the proportion of calls received from Hispanic or Latino callers decreased from pre- to post-intervention launch (84% to 81%), as did calls from women (80% to 77%). Calls about HPV or cervical cancer increased (7% to 12%), as did calls from those who reported finding out about 1-800-4-CANCER from “other printed sources” (12% to 17%). Due to the small sample size for these analyses, none of these differences are statistically significant. Figures 4 and 5 show these findings for St. Louis and the Lower Rio Grande Valley, respectively.
Figure 4.
Proportion of calls to 1-800-4-CANCER by caller characteristics and subject of interaction.
Figure 5.
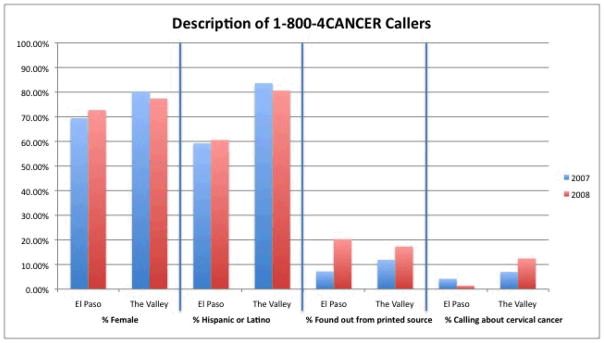
Proportion of calls to 1-800-4-CANCER by caller characteristics and subject of interaction (LRGV and El Paso).
DISCUSSION
This study evaluated the feasibility of disseminating cancer information resources to minority-serving community partners through an intermediary, the Cancer Information Service’s Partnership Program. Findings suggest that: (1) the Partnership Program can integrate this function into its standard practice; (2) its community partners will request a range of different resources and customize them in unique ways when that feature is available; (3) these partners will distribute the resources through a variety of channels and settings consistent with their missions and activities; and (4) availability of these resources within a community increases cancer information seeking by its members, as measured by calls to 1-800-4-CANCER.
This approach to disseminating cancer information resources is consistent with new thinking about the importance of building infrastructure to support dissemination efforts and using existing systems to facilitate distribution.14,28 The Partnership Program’s network of community contacts and staff members imbedded in the two intervention communities made it possible to reach many organizations in a short period of time. The research teams’ long history of conducting collaborative community-based research in the intervention communities also helped in this regard. Because building and maintaining these relationships lies at the heart of the Program, local staff were also well suited to develop new relationships with non-traditional partners (e.g., schools) to better reach populations for whom HPV vaccination is most relevant.
Study activities not only were consistent with the Program’s mission to increase cancer control activities in minority and medically underserved populations, they actually helped to advance it. Program staff reported that providing a range of high quality and population-specific cancer resources helped enhance the Program’s reputation among existing partners, increase awareness among others in the community, and change the perception that CIS only provided resources for cancer patients. While it is true that these resources might not have been developed in the absence of research funding, it is also true that the development costs were quite modest given the project’s large scope (16 distinct information products in two languages) and moderate budget (NIH R21).
In addition, 13 new community partnerships were formed as a result of the project. While the study did not formally assess the extent to which the intervention became integrated into Partnership Program activities, anecdotal evidence indicates this was happening. The Programs in both St. Louis and the Lower Rio Grande Valley continued using the HPV materials after the study ended, and continued training community partners to use them.
The widespread acceptance of these HPV resources and materials by organizations serving African American and Hispanic populations suggests they were deemed to be appropriate for the target audiences. Population-specific resources made by and for a particular sub-group may help reinforce positive cultural identity and cultural values in ways that enhance attention and processing of health information.29
Offering community partners the option of choosing among many types of HPV resources was also well received. In St. Louis, community partners could create customized cancer information resources by selecting the images, messages and designs to be used in their materials. This system, called MIYO (Make It Your Own), integrates core principles of Community-Based Participatory Research, including building partnerships in which community organizations and those they serve are actively involved in planning and designing interventions, have real decision making authority, and share resources in order to build capacity to address their priorities.30–34 Using MIYO, partner input determines what products MIYO will offer and what image, design and message choices will be available for making each resource. In addition, MIYO users have complete control over what resources they make, how they make them, and how they distribute them. In short, they shape the system to meet their own needs and use the system to create their own unique products for the specific populations they serve. Because MIYO gives users choice and control, they may feel more ownership of the products they create and be more committed to using them. Ongoing research with MIYO is testing these propositions.
The intervention increased call volume to 1-800-4-CANCER from targeted ZIP codes in St. Louis and the Lower Rio Grande Valley relative to pre-intervention levels and to comparison ZIP codes in Kansas City and El Paso. The patterns of increase were different for St. Louis and the Lower Rio Grande Valley in ways that may have reflected the distribution strategies of these sites. In St. Louis, where resources were distributed in a multi-step process from Partnership Program staff to organizations to their constituents, call volume built steadily over the follow-up period, perhaps reflecting the time needed for this process to play out. In the Lower Rio Grande Valley, there was a large and immediate increase in call volume, followed by a large decline in the final quarter of the project period. This may reflect the impact of promotoras interacting directly with the target population from day one, with intervention fatigue or diminished novelty of the approach accounting for later declines.
While the comparison communities and ZIP codes were determined a priori to maximize geographic and demographic similarity to the intervention sites, it is possible that they differed in other, unmeasured, ways that also could have been related to cancer information seeking. As a feasibility study with few sites and without random assignment, this must be considered in interpreting findings. The pattern of data reported in Figure 4 seem to support intervention effects, at least in St. Louis, where the proportions of African American callers, women callers and callers who learned about CIS from other printed sources all increased over the previous year and relative to Kansas City. For the Lower Rio Grande Valley, these data were less conclusive, although differences in call volume between this region and El Paso were actually greater.
The observed increase from pre- to post-intervention in call volume from ZIP codes in St. Louis and the Lower Rio Grande Valley (+38%) was quite different from the decline in call volume (−1.4%) observed in the entire U.S. over the same time period. While the observed increase in call volume may appear modest in absolute numbers, when projected to the U.S. population of African Americans and Hispanics from the 2000 census, these increases would translate to over 30,000 additional calls. It is not known whether or how long the observed increases were sustained beyond the 12-month follow-up period.
There are many variables unmeasured in this feasibility study that would be important to include in an efficacy trial evaluating this type of intervention. For example, in the current study, only the crudest measure of exposure was used (i.e., geographic area). While it would be logistically challenging and far more costly, the ideal approach would be to measure the number and type of people reached by each different distribution strategy employed by each community partner, how many of those exposed actually paid attention to the HPV informational resources, and in turn the proportion of those paying attention who called 1-800-4-CANCER. It would be equally important to expand the range of dependent variables measuring cancer information seeking. By focusing solely on calls to a telephone information system, the current study almost certainly missed other information seeking behaviors. For example, people exposed to information resources in the study may have asked their doctor about HPV vaccination, looked up information about it on the Internet, or talked to friends and family members about it. The Health Information National Trends Survey (HINTS)35 has consistently found that these are among the first places that people look for cancer information, while calling telephone information lines is comparatively less common. Finally, it would be important to determine effects of the intervention on HPV knowledge, as well as vaccination decisions and use.
For cancer information to help in eliminating racial and ethnic health disparities, it must be designed specifically for priority populations and reach members of those groups in large numbers.36,37 Effective and sustainable strategies that can achieve these dual goals are needed. The current study evaluated the feasibility of using an existing system with access to a network of community-based partner organizations to distribute HPV vaccination resources within African American and Hispanic communities. Three different indicators of feasibility – demand, acceptability and limited efficacy – were observed or measured, and all suggest that this approach is promising. The study also produced two innovative models – MIYO and Vivir Sin Cancer – for providing community partners with choices to maximize the fit between these resources and the specific populations they serve. Testing the effects of this approach in a larger study with a stronger design is an appropriate next step.
Acknowledgments
This project was supported by grants from the National Cancer Institute (R21-CA126326; P50-CA095815) and Centers for Disease Control and Prevention (5U48DP0000060). The authors thank the many community partner organizations that participated in developing and delivering the study intervention, and Jennifer Morgan for assistance in preparing the manuscript.
Contributor Information
Matthew W. Kreuter, Email: mkreuter@wustl.edu, Professor and Director of the Health Communication Research Laboratory, George Warren Brown School of Social Work, Washington University, St. Louis, MO.
Maria E. Fernandez, Email: maria.e.fernandez@uth.tmc.edu, Associate Professor of Health Promotion and Behavior Sciences; University of Texas School of Public Health, Center for Health Promotion and Prevention Research, University of Texas Health Science Center, Houston, TX.
Melissa Brown, Email: Melissa.brown@jeffcohealth.org, Jefferson County Health Department, Arnold, MO.
Ludmila Cofta-Woerpel, Email: lcwoerpel@mdanderson.org, Department of Behavioral Science, Division of OVP, Cancer Prevention and Population Sciences, University of Texas MD Anderson Cancer Center.
Debbie Pfeiffer, Email: dpfeiffer@wustl.edu, Health Communication Research Laboratory, George Warren Brown School of Social Work, Washington University, St. Louis, MO.
Brandie Adams-Piphus, Email: badamspiphus@yahoo.com, East Central Missouri Area Health Education Centers, St. Louis, MO.
Hope Krebill, Email: hkrebill@kumc.edu, Midwest Cancer Alliance, University of Kansas Medical Center, Kansas City, KS.
Dora Alice Gonzalez, Email: gonzalezda@uthscsa.edu, Epidemiology and Biostatistics, University of Texas Health Science Center at San Antonio, Institute for Health Promotion Research, San Antonio, TX.
Daisy Morales Campos, Email: moralescampo@athscsa.edu, Epidemiology and Biostatistics, University of Texas Health Science Center at San Antonio, Institute for Health Promotion Research, San Antonio, TX.
Ginny Thompson Kirklin, Email: gkirklin@komen-houston.org, Houston Affiliate of Susan G. Komen for the Cure, Houston, TX.
Sarah Betsworth, Email: sarah@transtria.com, Transtria LLC, St. Louis, MO.
Chris Casey, Email: ccasey@wustl.edu, Health Communication Research Laboratory, Gerorge Warren Brown School of Social Work, Washington University, St. Louis, MO.
Doug Luke, Email: dluke@wustl.edu, George Warren Brown School of Social Work, Washington University, St. Louis, MO.
References
- 1.Demark-Wahnefried W, McClelland J, Campbell M, et al. Awareness of cancer-related programs and services among rural African Americans. J Natl Med Assoc. 1998;90(4):197–202. [PMC free article] [PubMed] [Google Scholar]
- 2.Ward J, Baum S, Ter Maat J, Thomsen C, Maibach E. The value and impact of the Cancer Information Service telephone service. Part 4. J Health Commun. 1998;3(3 Suppl):50–70. doi: 10.1080/108107398127256. [DOI] [PubMed] [Google Scholar]
- 3.Squiers L, Rutten L, Atienza A, Treiman K, Moser R, Hesse B. Awareness of the National Cancer Institute’s Cancer Information Service: Results from the Health Information National Trends Survey (HINTS) J Health Commun. 2006;11(Suppl):117–133. doi: 10.1080/10810730600637517. [DOI] [PubMed] [Google Scholar]
- 4.Kreuter MW. Paper presented at the Consumer Health Informatics Summit; November 5, 2009; Bethesda, MD. Consumer Health Informatics for Cancer Prevention and Control: An Academic Research Perspective. [Google Scholar]
- 5.Arkin E, Romano R, Van Nevel J, McKenna J. Effect of the mass media in promoting calls to the Cancer Information Service. Natl Cancer I Monogr. 1993;(14):35–43. [PubMed] [Google Scholar]
- 6.Boyd N, Sutton C, Orleans C, et al. Quit Today! A targeted communications campaign to increase use of the Cancer Information Service by African American smokers. Prev Med. 1998;27(5 Pt 2):S50–S60. doi: 10.1006/pmed.1998.0383. [DOI] [PubMed] [Google Scholar]
- 7.Cummings K, Sciandra R, Davis S, Rimer B. Response to anti-smoking campaign aimed at mothers with young children. Health Educ Res. 1989;4(4):429–437. [Google Scholar]
- 8.Randolph W, Viswanath K. Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annu Rev Publ Health. 2004;25:419–437. doi: 10.1146/annurev.publhealth.25.101802.123046. [DOI] [PubMed] [Google Scholar]
- 9.Niederdeppe J, Kuang X, Crock B, Skelton A. Media campaigns to promote smoking cessation among socioeconomically disadvantaged populations: What do we know, what do we need to learn, and what should we do now? Soc Sci Med. 2008;67(9):1343–1355. doi: 10.1016/j.socscimed.2008.06.037. [DOI] [PubMed] [Google Scholar]
- 10.Freimuth V. Narrowing the cancer knowledge gap between whites and African Americans. Natl Cancer I Monogr. 1993;(14):81–91. [PubMed] [Google Scholar]
- 11.Sciandra R, Stein J. In: Mettlin C, Murphy G, editors. Applying marketing techniques to promotion of the Cancer Information Service; Progress in Cancer Control IV: Proceedings of the Progress in Cancer Control Meeting; Bethesda, Maryland. January 21–22, 1983; New York, NY: Alan R. Liss; 1983. pp. 153–160. [PubMed] [Google Scholar]
- 12.La Porta M, Hagood H, Kornfeld J, Treiman K. Evaluating the NCI’s Cancer Information Service Contact Centers: Meeting and Exceeding the Expectations of the Public. J Cancer Educ. 2007;22(S1):18–25. doi: 10.1007/BF03174342. [DOI] [PubMed] [Google Scholar]
- 13.Robinson B. NCI plans to expand outreach through community-based research programs. NCI Cancer Bulletin. 2009;6(16):9. [Google Scholar]
- 14.Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: The Interactive Systems Framework for Dissemination and Implementation. Am J Commun Psychol. 2008;41:171–181. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 15.Task Force on Community Preventive Services. Recommendations for client- and provider-directed interventions to increase breast, cervical, and colorectal cancer screening. Am J Prev Med. 2008;35(1s):S21–S25. doi: 10.1016/j.amepre.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Census Bureau. [Accessed November 11, 2009];State & County QuickFacts, 2008 Estimates. http://quickfacts.census.gov.
- 17.Green LW, Ottoson JM. Paper presented at the From Clinical Trials to Community: The Science of Translating Diabetes and Obesity Research; 2004. From efficacy to effectiveness to community and back: evidence-based practice vs. practice-based evidence. [Google Scholar]
- 18.Bowen D, Kreuter M, Spring B, et al. How we design feasibility studies. Am J of Prev Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Census Bureau. Census 2000 redistributing data (public law 94–171) summary file. Washington, DC: U.S. Department of Commerce, Economics and statistics administration, U.S. Census Bureau; 2001. [Google Scholar]
- 20.Missouri Department of Health and Senior Services. [Accessed March 21, 2006];Missouri Information for Community Assessment (MICA) Cancer Registry, 1996–2002. http://www.dhss.mo.gov/CancerMICA/index.html.
- 21.Bureau of Primary Health Care. [Accessed April 17, 2006];US-Mexico border health. http://bphc.hrsa.gov/bphc/borderhealth/default.htm.
- 22.Randolph W, Freeman D, Jr, Freeman J. Pap smear use in a population of older Mexican-American women. Women Health. 2002;36(1):21–31. doi: 10.1300/J013v36n01_02. [DOI] [PubMed] [Google Scholar]
- 23.Ries L, Eisner M, Kosary C, et al. SEER cancer statistics review, 1975–2002. Bethesda, MD: National Cancer Institute; 2005. [Google Scholar]
- 24.Texas Cancer Registry CEaSB. Cervical cancer incidence: Lower Rio Grande Valley females, 1998–2000 and other Texas females, 1998–2000. Austin, TX: Texas Department of State Health Services; 2000. [Google Scholar]
- 25.Wu Z, Black S, Freeman J, Markides K. Older Mexican-American women and cancer screening: Progress toward targets for healthy people 2000. Ethnic Dis. 2001;11(4):645–651. [PubMed] [Google Scholar]
- 26.Task Force on Community Preventive Services. The Guide to Community Preventive Services: What Works to Promote Health? New York: Oxford University Press; 2005. [Google Scholar]
- 27.Hannon P, Fernandez M, Williams R, et al. Cancer Control Planners’ Perceptions and Use of Evidence-Based Interventions. J Public Health Man. 2010;16(3):E1–E8. doi: 10.1097/PHH.0b013e3181b3a3b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kreuter M, Bernhardt J. Reframing the dissemination challenge: A marketing and distribution perspective. Am J Public Health. 2009;99(12):2123–2127. doi: 10.2105/AJPH.2008.155218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Publ Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 30.Goodman R, Speers M, McLeroy K, et al. Identifying and defining the dimensions of community capacity to provide a basis for measurement. Health Educ Behav. 1998;25(3):258–278. doi: 10.1177/109019819802500303. [DOI] [PubMed] [Google Scholar]
- 31.Green L, George M. Review and recommendations for the development of participatory research in health promotion in Canada. Vancouver, BC: The Royal Society of Canada; 1994. [Google Scholar]
- 32.Israel B, Eng E, Schulz A, Parker E. Methods in community-based participatory research for health. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- 33.Israel B, Schulz A, Parker E, Becker A. A review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Publ Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 34.Minkler M, Wallerstein N. Introduction to community based participatory research. In: Minkler M, Wallerstein N, editors. Community based participatory research for health. San Francisco: Jossey Bass; 2003. pp. 3–26. [Google Scholar]
- 35.Nelson D, Kreps G, Hesse B, et al. The Health Information National Trends Survey (HINTS): Development, design, and dissemination. J Health Commun. 2004;9(5):443–460. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 36.Kreuter M, Alcaraz K, Pfeiffer D, Christopher K. Using dissemination research to identify optimal community settings for tailored breast cancer information kiosks. J Public Health Man. 2008;14(2):160–169. doi: 10.1097/01.PHH.0000311895.57831.02. [DOI] [PubMed] [Google Scholar]
- 37.Kreuter M, Lukwago S, Bucholtz D, Clark E, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]