Abstract
Objectives
The aim of this study was to analyse inequalities in the use of dental care services according to socio-economic position (SEP) in individuals aged ≥50 years in European countries in 2006, and to examine the association between the degree of public coverage of dental services and the extent of inequalities, and specifically to determine whether countries with higher public health coverage show lower inequalities.
Methods
We carried out a cross-sectional study of 12,364 men and 14,692 women aged ≥50 years from 11 European countries. Data were extracted from the second wave of the Survey of Health, Ageing and Retirement in Europe (SHARE 2006). The dependent variable was use of dental care services within the previous year, and the independent variables were education level as a measure of SEP, whether services were covered to some degree by the country’s public health system, and chewing ability as a marker of individuals’ need for dental services. Age-standardised prevalence of the use of dental care as a function of SEP was calculated, and age-adjusted indices of relative inequality (RII) were computed for each type of dental coverage, sex, and chewing ability.
Results
SEP inequalities in the use of dental care services were higher in countries where no public dental care cover was provided than in countries where there was some degree of public coverage. For example, men with chewing ability from countries with dental care coverage had a RII of 1.39 (95%CI:1.29–1.51), while those from countries without coverage had a RII of 1.96 (95%CI:1.72–2.23). Women without chewing ability from countries with dental care coverage had a RII of 2.15 (95%CI:1.82–2.52), while those from countries without coverage had a RII of 3.02 (95%CI:2.47–3.69).
Conclusions
Dental systems relying on public coverage seem to show lower inequalities in their use, thus confirming the potential benefits of such systems.
Keywords: Socio-economic Factors, Dental Health Care, Public coverage
INTRODUCTION
Oral health is a condition in which people can speak, eat and socialize without active (oral) disease, discomfort or embarrassment (1). While having good levels of oral health is important in itself, it has also been linked to general health (2). However, levels of oral health are not equally distributed throughout the population, as there are inequalities in terms of socio-economic position (SEP), with people of disadvantaged SEP being more likely to have poorer outcomes in all oral health conditions (1,3). These inequalities are mediated by certain health-related behaviours such as having a balanced diet, smoking or alcohol consumption (1,4). In contrast, the role attributable to dental services in these inequalities is not entirely clear.
Dentist visits seem to be a determinant of oral health, at least when carried out on a regular basis (5,6). However, SEP inequalities in the use of dental care services have also been described, with socio-economically advantaged people being more likely to have seen a dentist (7,8). Thus, socio-economically disadvantaged people not only have greater needs of dental care, but also make less use of it, exacerbating existing inequalities.
In terms of oral health, older people are also a particularly vulnerable group, since the incidence of oral diseases increases with age and has a disproportionate effect in older age groups (1). In addition, their ability to pay is usually reduced and the costs of dental treatment, which are usually high, may represent an unacceptable burden for them.
In general, access to dental care services seems to be limited by the high costs of care and treatment, and in this regard, public funding of dental care provides a means of overcoming the divergence between ability to pay and need for care (9). However, it appears that health care systems are increasingly excluding dental care from their benefits packages (10). Within Europe the degree of public coverage of dental care in the adult population varies, with countries like Spain covering only tooth extractions, whereas in Sweden all types of treatment are subsidized and a special high-cost protection system is in place for individuals aged ≥65 years (11). The variability that exists in Europe with regard to coverage of public dental services provides the opportunity to assess whether or not inequalities in the use of dental care services are lower in countries that have higher levels of public dental coverage. This issue is currently highly relevant because the present financial situation has led governments to make cuts in public health care systems, even though many families are suffering impoverishment, particularly the more socioeconomically deprived. As mentioned by McKee et al. (12), the argument for public investment applies now more than ever.
The aim of this study was to analyse SEP-related inequalities in the use of dental care services among individuals aged 50 years or older in European countries in 2006, and to examine the association between the degree of public coverage of dental services and the extent of inequalities, and specifically to determine whether countries with public dental care services present lower inequalities.
MATERIALS AND METHODS
Design, study population and information sources
A cross-sectional study was performed. The study population consisted of 12,364 men and 14,692 women aged ≥50 years who were living in 11 European countries (Austria, Belgium, Denmark, France, Germany, Greece, Italy, Netherlands, Spain, Sweden and Switzerland) in 2006.
Data were extracted from the second wave of the Survey of Health, Ageing and Retirement in Europe (SHARE 2006) (13), a cross-national panel database on health, socio-economic status and social and family networks of European individuals aged ≥50 years. The individuals included in this analysis consisted of a baseline sample drawn in the first wave (SHARE 2004) plus a refreshment sample drawn in the second wave; to deal with problems of unit non-response and sample attrition, SHARE provides calibrated weights (which depend on the household design weight and the respondent’s calibration variables). In the latest version of the SHARE database (Release 2.5.0: May 24th, 2011), these weights were still not available for Ireland, so this country was excluded from the study.
Variables
Dependent variable
The dependent variable was use of dental care services, assessed using the question, ‘During the last twelve months, have you seen a dentist or a dental hygienist? (visits for routine controls, dentures and stomatology consultations included): Yes; No’.
Independent individual variables
The main individual independent variable was socio-economic position, assessed through the maximum education level achieved and coded according to the 1997 International Standard Classification of Education (ISCED-97), which facilitates international comparisons (14). The categories of this variable were: Pre-primary education (0); Primary or first stage of basic education (1); Lower secondary or second stage of basic education (2); Upper secondary education (3); Post-secondary, non-tertiary education (4); First stage of tertiary education (5); and Second stage of tertiary education (6). In order to have sufficient numbers in each category and country, some categories were combined, as follows: Lower secondary education or lower (0,1,2); Upper secondary or Post-secondary education (3,4) and Tertiary education (5,6).
Other individual-level variables analysed as possible confounders were: age (as a continuous variable, or grouped into 5-year categories for the purposes of standardising); and chewing ability, assessed using the question, ‘Can you bite and chew on hard foods, such as a firm apple, without difficulty? (Yes; No)’. This variable was used to account for differences in dental care needs between socio-economic groups.
Independent contextual variable
Data on the degree of public dental care coverage in each country during 2006 (the year for which survey data is available) were obtained by a review of the literature. Principally, we used the WHO/Europe Health system reviews (HiTs) (15–27), which are country-based reports created by the European Observatory on Health Systems and Policies that provide a detailed description of each European health care system. To cover gaps in the information on dental care, we also used a review on Oral Healthcare Systems published in 2004 (11). Three of the authors (LP, MCO and CB) independently reviewed all documents and classified each country according to the degree of public dental care coverage. Dental care was considered to be partially covered if curative services were covered by the public health system, either through coinsurance or reimbursement, and not covered if none of the services, or only emergencies, were covered by the public health system. None of the countries considered had complete coverage of dental care services (see appendix 1). After sharing and discussing the findings of this review, some discrepancies persisted regarding coverage in Eastern European countries, probably because a transition from the old public dental care system to an insurance-based dental care model was underway, and resources available for the new health care sector were relatively limited compared to the treatment needs of the populations (28,29). Thus, the two Eastern European countries that participated in SHARE (Czech Republic and Poland) were excluded from the analysis.
Data analysis
All analyses were performed separately for men and women and weights derived from the sample design and from the non-response pattern were used in all calculations.
For each country, the age-standardised prevalence of visits to the dentist was calculated for each educational level using the direct method (30). The age-standardised prevalence of visits to the dentist was also calculated according to educational level and chewing ability. The Relative Index of Inequality (RII) and the Slope Index of Inequality (SII) (31) were computed as measures of SEP inequality. This required previous conversion of the SEP marker variable (educational level) to a scale variable (values from 0 to 1) measuring, for each category, the cumulative proportion of the population that has a lower position in the hierarchy (31). Age-adjusted robust Poisson regression models (32) were fitted to test for association between having visited the dentist and the SEP scale variable, which was introduced as a continuous variable. The RII corresponds to the exponent of the coefficient for education, while the SII corresponds to the difference in the estimated proportion of use between the highest and lowest educational levels. These indices can be interpreted as the prevalence ratio and the prevalence difference at the two extremes of the education level spectrum, respectively (33).
These models were first fitted separately for each country, including an interaction term between educational level and chewing ability, to assess whether the association between SEP and the use of dental services differed as a function of the need for dental services. Inequalities between levels of education in each category of chewing ability were inferred from the models. To check whether there was a relationship between public coverage and inequalities, a model including all the countries was fitted. In these models, in addition to the interaction between educational level and chewing ability, we assessed the interaction between educational level and type of coverage to assess whether the magnitude of inequalities in use of dental care services differed according to the degree of public coverage. In these models the country was introduced as a categorical variable to adjust for its potential confounding effect.
RESULTS
Seventy-one percent of men and 63% of women were under 70 years of age and approximately 22% of men and 16% of women had tertiary level education. Approximately 17% of men and 22% of women had reduced chewing ability.
Almost 55% of respondents had visited the dentist in the previous year (table 1), and this percentage was systematically higher in better educated groups in all the countries under study and in both sexes (table 2). This effect was most marked in the Netherlands, for example, where 76.3% of men in the highest educational level group had visited the dentist in the previous year compared to 50.3% in the lowest educational group. In women the corresponding figures were 84.8% and 56.0%. This gradient in prevalence of visits to the dentist was independent of other covariates; for example, in men with poor chewing ability from countries without dental care coverage these percentages were 31.3%, 43.7% and 54.3% for the lowest to highest educational levels, respectively; conversely, in women with normal chewing ability from countries with some degree of coverage the corresponding percentages were 56.3, 66.1 and 73.2% (table 3).
Table 1.
Gender distribution of the study sample in relation to the variables under study
| Men | Women | |||
|---|---|---|---|---|
| N | % | N | % | |
| Age | ||||
| 50–59 | 5,021 | 40.6 | 5,136 | 34.9 |
| 60–69 | 3,775 | 30.5 | 4,124 | 28.1 |
| 70–79 | 2,542 | 20.6 | 3,364 | 22.9 |
| 80 or + | 1,027 | 8.3 | 2,068 | 14.1 |
| Educational level | ||||
| Lower secondary | 5,113 | 41.4 | 7,877 | 53.6 |
| Upper secondary | 4,172 | 33.7 | 4,040 | 27.5 |
| Tertiary | 2,768 | 22.4 | 2,396 | 16.3 |
| Missing | 311 | 2.5 | 379 | 2.6 |
| Chewing ability | ||||
| Normal | 10,184 | 82.4 | 11,369 | 77.4 |
| Reduced | 2,136 | 17.3 | 3,263 | 22.2 |
| Missing | 44 | 0.3 | 60 | 0.4 |
| Visits to the dentist | ||||
| No | 5,508 | 44.5 | 6,467 | 44.0 |
| Yes | 6,783 | 54.9 | 8,154 | 55.5 |
| Missing | 73 | 0.6 | 71 | 0.5 |
| Total | 12,364 | 100.0 | 14,692 | 100.0 |
Table 2.
Number of study participants and age-standardized prevalence (%) of dental visits according to country, sex and educational level (LS=Lower Secondary, US= Upper Secondary, T=Tertiary), stratified by country and type of dental care coverage.
| Type of coverage and country |
Total | Men | Women | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LS | US | T | LS | US | T | ||||||||
| N | N | % | N | % | N | % | N | % | N | % | N | % | |
| Partially covered | |||||||||||||
| Austria | 1,278 | 96 | 44.1 | 314 | 51.7 | 160 | 54.4 | 296 | 42.7 | 310 | 54.6 | 103 | 65.3 |
| Belgium | 2,979 | 608 | 39.2 | 368 | 54.5 | 384 | 63.7 | 847 | 42.0 | 394 | 52.9 | 378 | 67.1 |
| Denmark | 2,478 | 167 | 60.3 | 571 | 79.8 | 427 | 86.4 | 404 | 66.2 | 442 | 83.4 | 467 | 89.0 |
| France | 2,779 | 528 | 39.1 | 444 | 44.4 | 280 | 58.3 | 858 | 44.1 | 394 | 61.7 | 276 | 63.4 |
| Germany | 2,454 | 64 | 62.2 | 672 | 69.1 | 374 | 80.5 | 380 | 65.0 | 697 | 76.3 | 268 | 83.7 |
| Greece | 2,922 | 771 | 30.8 | 358 | 34.2 | 237 | 41.1 | 1,085 | 37.1 | 335 | 48.9 | 136 | 48.7 |
| Sweden | 2,630 | 604 | 74.5 | 366 | 81.3 | 262 | 87.3 | 688 | 77.7 | 403 | 84.8 | 307 | 86.6 |
| Total* | 17,520 | 2,838 | 49.4 | 3,093 | 58.5 | 2,124 | 67.9 | 4,558 | 53.7 | 2,975 | 65.8 | 1,935 | 72.2 |
| Not covered | |||||||||||||
| Italy | 2,873 | 861 | 29.9 | 320 | 49.4 | 114 | 46.9 | 1,227 | 30.7 | 288 | 51.0 | 64 | 38.5 |
| Netherlands | 2,499 | 510 | 50.3 | 319 | 68.5 | 340 | 76.3 | 793 | 56.0 | 284 | 73.3 | 252 | 84.8 |
| Spain | 2,102 | 767 | 23.0 | 82 | 49.7 | 106 | 49.8 | 964 | 28.2 | 87 | 35.4 | 96 | 43.3 |
| Switzerland | 1,372 | 161 | 63.3 | 376 | 69.3 | 96 | 86.7 | 306 | 65.0 | 390 | 81.1 | 43 | 78.4 |
| Total* | 8,846 | 2,299 | 39.5 | 1,097 | 58.4 | 656 | 61.9 | 3,290 | 43.3 | 1,049 | 58.3 | 455 | 59.0 |
standardised by age and country
Table 3.
Age standardized prevalence (%) of dental visits according to sex, chewing ability and educational level (LS=Lower Secondary, US= Upper Secondary, T=Tertiary), stratified by country and type of dental care coverage.
| Type of coverage and country |
Men | Women | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal chewing ability | Reduced chewing ability | Normal chewing ability | Reduced chewing ability | |||||||||
| LS | US | T | LS | US | T | LS | US | T | LS | US | T | |
| % | % | % | % | % | % | % | % | % | % | % | % | |
| Partially covered | ||||||||||||
| Austria | 57.9 | 54.7 | 55.5 | 12.8 | 38.3 | 51.7 | 46.0 | 55.3 | 59.5 | 36.4 | 52.9 | 63.2 |
| Belgium | 42.7 | 57.6 | 64.9 | 32.1 | 42.7 | 58.3 | 46.6 | 53.2 | 70.2 | 31.8 | 48.8 | 57.3 |
| Denmark | 62.5 | 82.1 | 88.9 | 46.1 | 68.4 | 75.3 | 68.8 | 85.5 | 92.5 | 59.6 | 77.6 | 73.9 |
| France | 40.1 | 44.7 | 59.8 | 26.5 | 46.4 | 42.7 | 47.0 | 63.3 | 63.7 | 34.8 | 54.1 | 66.8 |
| Germany | 66.1 | 68.8 | 80.5 | 41.3 | 58.8 | 83.6 | 68.7 | 74.9 | 86.6 | 56.2 | 74.8 | 83.4 |
| Greece | 32.8 | 35.9 | 43.8 | 25.7 | 36.1 | 27.7 | 37.4 | 45.9 | 51.1 | 40.5 | 51.9 | 52.1 |
| Sweden | 75.1 | 83.0 | 87.7 | 71.1 | 50.4 | 46.8 | 80.4 | 85.5 | 86.5 | 58.7 | 71.0 | 80.3 |
| Total* | 52.3 | 60.6 | 69.2 | 38.0 | 49.0 | 55.1 | 56.3 | 66.1 | 73.2 | 45.4 | 61.9 | 68.0 |
| Not covered | ||||||||||||
| Italy | 32.0 | 50.0 | 44.8 | 24.2 | 39.1 | 55.2 | 29.7 | 56.2 | 37.1 | 32.8 | 43.3 | 48.5 |
| Netherlands | 53.7 | 71.0 | 78.7 | 29.2 | 49.8 | 63.7 | 58.2 | 76.4 | 81.0 | 48.6 | 60.4 | 79.7 |
| Spain | 22.9 | 45.8 | 45.7 | 27.3 | 40.0 | 54.4 | 28.7 | 33.9 | 49.1 | 31.3 | 37.6 | 28.0 |
| Switzerland | 66.5 | 70.9 | 87.4 | 54.6 | 52.8 | 33.2 | 67.8 | 81.5 | 79.1 | 46.3 | 78.8 | 47.4 |
| Total* | 41.8 | 58.9 | 61.0 | 31.3 | 43.7 | 54.3 | 43.9 | 60.6 | 58.6 | 39.4 | 51.8 | 53.3 |
standardised by age and country
The age- and country-standardised prevalence of dental visits appeared to be higher in countries where dental care was covered to some degree than in countries were dental care was not covered, in each of the educational levels with the exception of men in the middle category of education (table 2). Age-and country-standardised prevalence of dental visits was also higher in individuals with normal chewing ability, compared to those with reduced chewing ability, in both sexes and all levels of education (table 3).
Our results confirmed the existence of inequalities in the use of dental care services between educational levels in 35 out of 44 combinations of country, sex and chewing ability. In fact, inequalities were found for all countries, in at least one of the two categories of chewing ability, and in most cases in both (table 4). For example, relative inequalities in men with poor chewing ability in countries with dental care coverage ranged from 1.11 in Sweden to 5.43 in Austria, while in countries without coverage these values ranged from 1.90 in Switzerland to 8.77 in Spain. Statistically significant interactions between educational level and public coverage, and between educational level and chewing ability were found (p-value<0.001 in both cases and both sexes). Inequalities between educational levels were higher in countries where dental care was not covered than in countries where dental care was covered to some degree. For example, men with normal chewing ability who lived in countries with dental care coverage had a RII of 1.39 (95%CI: 1.29–1.51) while those from countries without coverage had a RII of 1.96 (95%CI: 1.72–2.23). Women with poor chewing ability who lived in countries with dental care coverage had a RII of 2.15 (95%CI: 1.82–2.52), while those from countries without coverage had a RII of 3.02 (95%CI: 2.47–3.69). Nonetheless, confidence intervals overlapped in individuals with poor chewing ability. In addition, socio-economic inequalities were statistically significantly higher in individuals with decreased chewing ability than in those with normal chewing ability (table 4, figure 1). For example, in countries where dental care was not covered, women with normal chewing ability and a higher SEP were 1.93 times (95%CI: 1.70–2.18) more likely to have seen a dentist than those with lower SEP, while women with poor chewing ability and a higher SEP were 3.02 times (95%CI: 2.47–3.69) more likely to have seen a dentist than those with lower SEP.
Table 4.
Relative Index of Inequality (RII) of dental visits (highest education level compared to lowest) and 95% confidence intervals according to sex and chewing ability, stratified by country and type of dental care coverage.
| Type of coverage and country |
Relative inequalities | |||
|---|---|---|---|---|
| Men | Women | |||
| Normal chewing ability |
Reduced chewing ability |
Normalchewing ability |
Reduced chewing ability |
|
| RII (95% CI) | RII (95% CI) | RII (95% CI) | RII (95% CI) | |
| Partially covered | ||||
| Austria | 0.97 (0.69–1.37) | 5.43 (2.14–13.73) | 1.55 (1.17–2.07) | 4.08 (1.87–8.91) |
| Belgium | 1.85 (1.49–2.30) | 2.65 (1.62–4.33) | 1.85 (1.50–2.27) | 3.09 (1.97–4.86) |
| Denmark | 1.35 (1.20–1.53) | 1.74 (1.19–2.53) | 1.45 (1.29–1.63) | 1.61 (1.17–2.22) |
| France | 1.78 (1.25–2.55) | 2.06 (0.89–4.78) | 1.64 (1.26–2.13) | 2.81 (1.58–4.99) |
| Germany | 1.31 (1.11–1.54) | 2.03 (1.34–3.06) | 1.28 (1.08–1.52) | 2.43 (1.58–3.73) |
| Greece | 1.47 (1.06–2.04) | 1.66 (0.60–4.65) | 1.32 (0.96–1.79) | 1.75 (0.87–3.52) |
| Sweden | 1.24 (1.09–1.42) | 1.11 (0.47–2.60) | 1.17 (1.05–1.30) | 1.79 (1.08–2.94) |
| Total* | 1.39 (1.29–1.51) | 2.18 (1.77–2.69) | 1.38 (1.28–1.48) | 2.15 (1.82–2.55) |
| Not covered | ||||
| Italy | 2.23 (1.52–3.26) | 3.93 (1.91–8.08) | 2.79 (1.93–4.04) | 1.92 (0.86–4.26) |
| Netherlands | 1.66 (1.40–1.96) | 3.21 (1.54–6.69) | 1.62 (1.38–1.91) | 2.55 (1.54–4.22) |
| Spain | 3.51 (2.03–6.07) | 8.77 (3.55–21.66) | 2.52 (1.61–3.95) | 2.74 (0.83–9.06) |
| Switzerland | 1.39 (1.14–1.68) | 1.90 (0.82–4.40) | 1.43 (1.19–1.73) | 3.35 (1.71–6.56) |
| Total* | 1.96 (1.72–2.23) | 3.07 (2.42–3.89) | 1.93 (1.70–2.18) | 3.02 (2.47–3.69) |
age and country-adjusted
Figure 1.
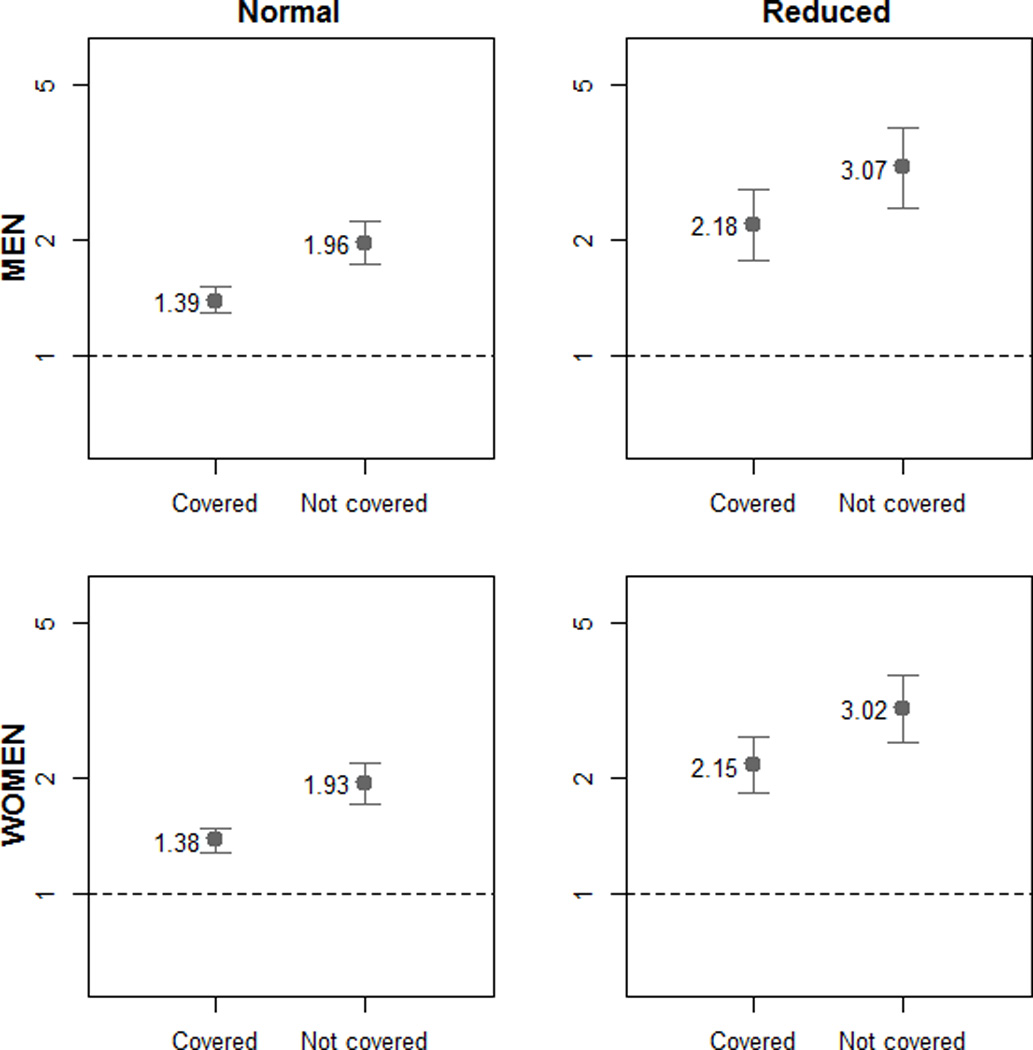
Relative Index of Inequality (RII) (highest education level compared to lowest) and 95% confidence intervals stratified by type of dental care coverage (partially covered and not covered), chewing ability (normal and reduced) and sex.
The absolute inequalities given by the SII showed the same pattern as relative inequalities (see appendix 2).
DISCUSSION
Socio-economically advantaged older adults are more likely to have seen the dentist, independently of their chewing ability. When the degree of public dental care is taken into account, socio-economic inequalities are more pronounced in countries where dental care is not covered by the public health system than in those where it is partially covered.
Socio-economic inequalities in use of dental care services
SEP inequalities in oral health are well documented (3,34). These inequalities are mediated by certain health-related behaviours such as smoking, alcohol consumption or diet, and are also partly determined by others, such as access to healthy food, and to dental products and dental services (1,4). The role of dental services in those inequalities is unclear, with some authors finding that it has an important role (2,35) and others finding that it has no role at all (36).
Socio-economically disadvantaged people not only have worse oral health, but also make less use of dental services, which is consistent with previous studies that have used educational level (37) or other indicators of socioeconomic position (37–39). In this regard, several multi-country studies have found strong socio-economic inequalities in most of the countries under study (7,40). Moreover, a study that was also based on SHARE data found income-related inequalities in all European countries involved in the study (8). Our study goes one step further, in that we have measured the role of public dental care on inequalities, and have assessed the relationship between chewing ability, dental attendance and socio-economic status.
Interaction between socio-economic position and chewing ability
A health system is equitable if it matches access or, more pragmatically, use to need, regardless of ability to pay (41), and for this reason the use of services across different socio-economic groups must be considered in relation to their differing levels of need. Some studies of the use of dental care services have standardised or adjusted the use of these services by oral health status; however, this implies the assumption that the relationship between the use of dental care services and socio-economic position does not vary with level of need. In this study, however, we have observed an interaction between socio-economic position and chewing ability that shows that the relationship between the use of dental services and socio-economic position is stronger among individuals with greater health care needs. A previous study observed an interaction between disadvantaged socio-economic status and seeking dental care in relation to self-rated oral health (38), and as both studies are cross-sectional, the conclusions would be similar. We have hypothesised that this may occur because individuals with reduced chewing ability may also have fewer teeth and thus be less likely to perceive a need for dental services (42). This may be particularly true among socio-economically disadvantaged groups.
Association between public dental care coverage and SEP inequalities
As far as we are aware, no studies have been published that have specifically evaluated the association between public dental care coverage and socio-economic inequalities in dental attendance. It has been found that being covered by a dental care model is related to dental care use in children (43), and in fact we also saw in our study that the prevalence of dental care use was higher in countries where dental care was covered to some extent. Regarding inequalities, several Spanish studies have found that dental care, the only service not covered by the Spanish public health system, had the highest inequalities (44,45). A study based on data simulations found that providing the poorest people with dental insurance would substantially reduce (although not eliminate, due to the gradient in the association) inequity in the use of dental care services (39,45). Additionally, a study measuring inequalities after the introduction of universal coverage in Thailand (46) found that inequalities persisted mainly because of the limited scope of benefit packages in covering treatment costs, and also due to the presence of the private sector in dental care.
Health care coverage provides financial security against the costs of unexpected illness and facilitates access to treatments and preventive services (47). In contrast, out-of pocket payments fall more on those who use these services more often, and have a disproportionate effect on people from disadvantaged socioeconomic groups (41) due to their increased health care needs. Some systems opt for protecting the most deprived, but as already discussed, the gradient of socio-economic position affects the whole of society, so this does not entirely eliminate the problem. The most equitable systems are those that offer universal care, which are financed by progressive taxes, with sufficiently high quality benefits to discourage people, especially those from the middle classes, from seeking private healthcare options, thus reducing the tendency for, in the famous words of Richard Titmuss, “a service for the poor” to inevitably become “a poor service” (48). Within health care systems, socio-economic inequalities in dental care seem to have become more acceptable than in other branches of medicine (2). In addition, there is a tendency in many countries for public dental care funding to be reduced (28). In a service in which the private sector has such an important role, and which is used mainly in a preventive way, the financial crisis and the consequent impoverishment of families, mainly the socio-economically deprived, can have devastating effects in term of inequalities. For this reason, socio-economic inequalities in oral health and the use of dental care services need to be monitored and kept in consideration.
Limitations
One of the limitations of this study is the fact that the measure of need for dental care was self-reported. However, self-reported chewing ability has been established as an important dimension of oral health and has been associated with oral health-related quality of life (49). Better educated older Europeans appear to be more likely to rate a given health state negatively (50), but this would only reassert the presence of inequalities. Another limitation of the study is its cross-sectional nature and the fact that it is subject to reverse causality. The use of health care services during the previous few months cannot have an effect on the maximum education level achieved, but having used dental services reduces the onset of chewing difficulties (51). However, we presented socio-economic inequality according to chewing ability and the relationship between socio-economic position and the use of dental services was seen in both groups. Socio-economic position is a complex construct and educational level is one way of measuring it, although it has its own limitations. However, it is among the most widely used indicators and reasons for its popularity include: ease of measurement, relevance to people regardless of age or working circumstances, applicability to persons not in the active labour force (homemakers, the unemployed and retired) and association with numerous health outcomes (52,53). For both men and women with poor chewing ability the confidence intervals of the RIIs in countries with coverage overlapped with those of countries without coverage. In the four strata studied (men and women with normal and poor chewing ability), the RIIs in countries without coverage were approximately 1.4 times higher than the RIIs in countries with coverage. For this reason we hypothesise that the smaller sample sizes in people with poor chewing ability could make intervals wider and thus overlap. Finally, multilevel models could not be used due to the limited number of countries in the study.
CONCLUSIONS
Socio-economic inequalities in the use of dental care services exist throughout Europe but are less marked in countries with some degree of public coverage. These results indicate the potential benefits of dental systems that rely on public coverage.
Acknowledgements
This paper uses data from SHARE release 2.5.0, as of May 24th 2011. The SHARE data collection has been primarily funded by the European Commission through the 5th framework programme (project QLK6-CT-2001- 00360 in the thematic programme Quality of Life), through the 6th framework programme (projects SHARE-I3, RII-CT-2006-062193, COMPARE, CIT5-CT-2005-028857, and SHARELIFE, CIT4-CT-2006-028812) and through the 7th framework programme (SHARE-PREP, 211909 and SHARE-LEAP, 227822). Additional funding from the U.S. National Institute on Aging (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, Y1-AG-4553-01 and OGHA 04-064, IAG BSR06-11, R21 AG025169) as well as from various national sources is gratefully acknowledged (see http://www.share-project.org for a full list of funding institutions).
Appendix 1
Coverage of oral health services for adults and older people in the countries under study around 2006
| Country | Coverage | Degree of coverage |
|---|---|---|
| Austria | Partially covered | Restorative and some surgical treatments are fully covered by the sickness insurance. For some treatments and within some sickness insurances patients contribute 10% to 20% (depending on the region). For removable prostheses patients have to pay between 25% and 50% of the costs (11). The cost of fixed dentures is only reimbursed in exceptional cases (15). |
| Belgium | Partially covered | Preventive dental care and extractions are fully reimbursed (16). Patients pay the dentist and are then reimbursed at 75% of the nationally agreed fees for restorative care, removable dentures, minor oral surgery and limited preventive care (11). Periodontal treatment, fixed prostheses and oral implants are not covered (11). For insured people with preferential reimbursement, all dental services are free (16). |
| Denmark | Partially covered | Most adults obtain oral healthcare from the private sector and a proportion of the cost of this care is refunded. The refund rates vary from 30–65% depending on the patient’s age and the category of treatment (11). Some of the payments, in particular the curative services, are covered by the regions (18). |
| France | Partially covered | Patients pay full fees to the dentist. The mandatory insurance system reimburses about 70% of these fees on a fee-per-item basis for all standard treatments such as extractions, conservative dentistry and prostheses as well as scaling and sealing. About 5% of the population belonging either to low-income groups or to groups without any income, benefit from free care. Most prosthodontic treatment is paid for entirely by patients (11). |
| Germany | Partially covered | The sick funds pay 100% of costs for examinations, radiographic investigations, fillings, oral surgery, preventive treatments for defined groups, periodontal care and endodontic treatment. Prosthetic care such as dentures, crown and bridge work attract a subsidy of 50% to 60%. Implants are not covered at all (11). |
| Greece | Partially covered | Three ways of receiving oral health care: dental departments of those SIFs (Social Insurance Funds) that operate polyclinics where treatment is provided free of charge; private dental practitioners contractors with a SIF that provide some treatments free of charge and some with co-payments; independent dental practitioner without any contract with a SIF, in which case patients claim back 20–30% of the costs from the SIF. The third option (reimbursement) is common practice (11). |
| Italy | Not covered | 95% of dentistry is provided by private practitioners. Private practise is in the most part outside any existing insurance schemes and patients pay dentists directly for their care and treatment (11). Dental health care is guaranteed by the government for specific populations such as children (0–16 years old), vulnerable people (disabled, people with HIV, people with rare diseases) and individuals who need dental health care in some urgency/emergency cases (22). |
| Netherlands | Not covered | Cover is limited to dental care for children and preventive dental care for adults, in addition to specialist surgical treatment. People with a specific dental complaint, or a physical or mental handicap resulting from medical treatment, are entitled (under specific circumstances and if required) to integral dental care (23). |
| Spain | Not covered | Dental care for adults is excluded from public funding (25). The public sector offers free tooth extractions (10). |
| Sweden | Partially covered | Within general dental insurance all types of treatment are subsidized, including prosthetics and orthodontics (11), the subsidies being fixed according to the type of treatment involved. For certain extensive dental procedures, there is a special high- cost protection system for those aged 65 years or over (26). |
| Switzerland | Not covered | Dental treatment is covered by the compulsory health insurance only in the case of very severe and unavoidable diseases. As a result, most dental services are funded privately either by the patient or through supplementary health insurance (27). |
Appendix 2
Slope Index of Inequality (SII) (highest education level compared to lowest) and 95% confidence intervals according to sex and chewing ability, stratified by country and type of dental care coverage.
| Type of
coverage and country |
Absolute inequalities | |||
|---|---|---|---|---|
| Men | Women | |||
| Normal chewing ability |
Reduced chewing ability |
Normal chewing ability |
Reduced chewing ability |
|
| SII (95% CI) | SII (95% CI) | SII (95% CI) | SII (95% CI) | |
| Partially covered | ||||
| Austria | −1.4 (−20.3–17.5) | 70.8 (26.6–115.0) | 22.5 (8.2–36.9) | 62.3 (25.8–98.7) |
| Belgium | 32.2 (20.8–43.5) | 42.2 (19.6–64.7) | 32.0 (21.2–42.8) | 46.8 (26.9–66.8) |
| Denmark | 24.4 (14.8–34.0) | 37.9 (11.8–63.9) | 29.7 (20.6–38.8) | 32.5 (10.4–54.7) |
| France | 26.3 (10.3–42.3) | 31.0 (−6.4–68.4) | 26.7 (12.8–40.5) | 48.8 (22.3–75.2) |
| Germany | 19.9 (7.9–31.9) | 47.1 (19.3–74.8) | 18.3 (6.1–30.5) | 62.0 (31.2–92.9) |
| Greece | 13.7 (2.2–25.2) | 12.9 (−14.2–39.9) | 10.5 (−1.3–22.4) | 20.9 (−5.6–47.4) |
| Sweden | 17.3 (6.8–27.7) | 6.2 (−47.0–59.5) | 12.6 (3.8–21.5) | 40.1 (4.6–75.6) |
| Total* | 17.9 (13.4–22.4) | 35.0 (24.8–45.1) | 16.3 (12.6–20.1) | 34.8 (26.6–43.0) |
| Not covered | ||||
| Italy | 30.2 (15.6–44.7) | 45.2 (18.2–72.3) | 36.5 (23.0–50.0) | 23.4 (−6.7–53.5) |
| Netherlands | 32.6 (22.0–43.2) | 50.9 (16.8–85.0) | 30.5 (20.4–40.6) | 51.5 (23.5–79.5) |
| Spain | 34.5 (19.2–49.8) | 77.3 (40.3–114.3) | 28.4 (14.3–42.5) | 30.4 (−7.6–68.4) |
| Switzerland | 23.6 (10.0–37.1) | 36.3 (−13.8–86.4) | 27.0 (13.3–40.6) | 81.0 (35.5–126.5) |
| Total* | 48.2 (38.6–57.7) | 67.6 (51.8–83.3) | 48.8 (39.8–57.9) | 73.6 (59.5–87.8) |
age and country-adjusted
REFERENCES
- 1.Kwan S, Petersen PE. Equity, social determinants and public health programmes. WHO; 2010. Oral health: equity and social determinants. [DOI] [PubMed] [Google Scholar]
- 2.Spencer J, Harford J. Inequality in oral health in Australia. In: Symposium: Is it Time for a Universal Dental Scheme in Australia? Australian Review of Public Affairs. 2007 [Google Scholar]
- 3.Marmot M, Bell R. Social determinants and dental health. Adv Dent Res. 2011;23(2):201–206. doi: 10.1177/0022034511402079. [DOI] [PubMed] [Google Scholar]
- 4.Sisson KL. Theoretical explanations for social inequalities in oral health. Community Dent Oral Epidemiol. 2007;35(2):81–88. doi: 10.1111/j.1600-0528.2007.00354.x. [DOI] [PubMed] [Google Scholar]
- 5.Thomson WM, Williams SM, Broadbent JM, et al. Long-term dental visiting patterns and adult oral health. J Dent Res. 2010;89(3):307–311. doi: 10.1177/0022034509356779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richards W, Ameen J. The impact of attendance patterns on oral health in a general dental practice. Br Dent J. 2002;193(12):697–702. doi: 10.1038/sj.bdj.4801664. [DOI] [PubMed] [Google Scholar]
- 7.Hosseinpoor AR, Itani L, Petersen PE. Socio-economic Inequality in Oral Healthcare Coverage: Results from the World Health Survey. J Dent Res. 2012;91(3):275–281. doi: 10.1177/0022034511432341. [DOI] [PubMed] [Google Scholar]
- 8.Listl S. Income-related inequalities in dental service utilization by Europeans aged 50+ J Dent Res. 2011;90(6):717–723. doi: 10.1177/0022034511399907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leake JL, Birch S. Public policy and the market for dental services. Community Dent Oral Epidemiol. 2008;36(4):287–295. doi: 10.1111/j.1600-0528.2008.00438.x. [DOI] [PubMed] [Google Scholar]
- 10.Mossialos E, Dixon A, Figueras J, Kutzin J, editors. European Observatory on Health Care Systems Series. Europe: WHO; 2002. Funding health care: options for Europe. [Google Scholar]
- 11.Widstrom E, Eaton KA. Oral healthcare systems in the extended European union. Oral Health Prev Dent. 2004;2(3):155–194. [PubMed] [Google Scholar]
- 12.McKee M, Basu S, Stuckler D. Health systems, health and wealth: the argument for investment applies now more than ever. Soc Sci Med. 2012;74(5):684–687. doi: 10.1016/j.socscimed.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 13.SHARE - Survey of Health, Ageing and Retirement in Europe. Available at: http://share-dev.mpisoc.mpg.de/index.php?id=642.
- 14.International Standard Classification of Education (ISCED) 1997. Available at: http://www.uis.unesco.org/Education/Pages/international-standard-classification-of-education.aspx.
- 15.Hofmarcher MM, Rack H-M. Austria: Health system review. Health Systems in Transition. 2006;8(3):1–247. [PubMed] [Google Scholar]
- 16.Corens D. Health system review: Belgium. Health Systems in Transition. 2007;9(2):1–172. [Google Scholar]
- 17.Rokosová M, Háva P, Schreyögg J, Busse R. Health care systems in transition: Czech Republic. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2005 [Google Scholar]
- 18.Strandberg-Larsen M, Nielsen MB, Vallgårda S, Krasnik A, Vrangbæk K, Mossialos E. Denmark: Health system review. Health Systems in Transition. 2007;9(6):1–164. [Google Scholar]
- 19.Sandier S, Paris V, Polton D. Health care systems in transition: France. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2004 [Google Scholar]
- 20.Busse R, Riesberg A. Health care systems in transition: Germany. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2004 [Google Scholar]
- 21.Economou C. Greece: Health system review. Health Systems in Transition. 2010;12(7):1–80. [PubMed] [Google Scholar]
- 22.Lo Scalzo A, Donatini A, Orzella L, Cicchetti A, Profili S, Maresso A. Italy: Health system review. Health Systems in Transition. 2009;11(6):1–216. [Google Scholar]
- 23.Exter A, Hermans H, Dosljak M, Busse R. Health care systems in transition: Netherlands. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2004 [Google Scholar]
- 24.Kuszewski K, Gericke C. Health Systems in Transition: Poland. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2005 [Google Scholar]
- 25.Durán A, Lara JL, van Waveren M. Spain: Health system review. Health Systems in Transition. 2006;8(4):1–208. [PubMed] [Google Scholar]
- 26.Glenngård AH, Hjalte F, Svensson M, Anell A, Bankauskaite V. Health Systems in Transition: Sweden. WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies. 2005 [Google Scholar]
- 27.European Observatory on Health Care Systems. Health care systems in transition: Switzerland. European Observatory on Health Systems. 2000 [Google Scholar]
- 28.Kossioni AE. Is Europe prepared to meet the oral health needs of older people? Gerodontology. 2012;29(2):e1230–e1240. doi: 10.1111/j.1741-2358.2010.00445.x. [DOI] [PubMed] [Google Scholar]
- 29.Widstrom E, Van Den Heuvel J. More attention to public health in the European Union - implications for dentistry? Int Dent J. 2005;55(3):157–161. doi: 10.1111/j.1875-595x.2005.tb00313.x. [DOI] [PubMed] [Google Scholar]
- 30.Rué M, Borrell C. Los métodos de estandarización de tasas. Revisiones de Salud Pública. 1993;3:263–295. [Google Scholar]
- 31.Shaw M, Galobardes B, Lawlor DA, Lynch J, Wheeler B, Davey Smith G. The Handbook of Inequality and Socioeconomic Position: Concepts and Measures. The Policy Press. 2007 [Google Scholar]
- 32.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 33.Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 34.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83(9):661–669. [PMC free article] [PubMed] [Google Scholar]
- 35.Wamala S, Merlo J, Bostrom G. Inequity in access to dental care services explains current socioeconomic disparities in oral health: the Swedish National Surveys of Public Health 2004–2005. J Epidemiol Community Health. 2006;60(12):1027–1033. doi: 10.1136/jech.2006.046896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behaviour in oral health inequalities. Community Dent Oral Epidemiol. 2006;34(1):71–79. doi: 10.1111/j.1600-0528.2006.00261.x. [DOI] [PubMed] [Google Scholar]
- 37.Pavi E, Karampli E, Zavras D, Dardavesis T, Kyriopoulos J. Social determinants of dental health services utilisation of Greek adults. Community Dent Health. 2010;27(3):145–150. [PubMed] [Google Scholar]
- 39.Grignon M, Hurley J, Wang L, Allin S. Inequity in a market-based health system: Evidence from Canada's dental sector. Health Policy. 2010;98(1):81–90. doi: 10.1016/j.healthpol.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 40.Van Doorslaer E, Masseria C. OECD Health Equity Research Group Members. Income-Related Inequality in the Use of Medical Care in 21 OECD Countries. OECD Health Working Papers No 14 OECD. 2004 [Google Scholar]
- 41.Hanratty B, Zhang T, Whitehead M. How close have universal health systems come to achieving equity in use of curative services? A systematic review. Int J Health Serv. 2007;37(1):89–109. doi: 10.2190/TTX2-3572-UL81-62W7. [DOI] [PubMed] [Google Scholar]
- 42.Exley C. Bridging a gap: the (lack of a) sociology of oral health and healthcare. Sociol Health Illn. 2009;31(7):1093–1108. doi: 10.1111/j.1467-9566.2009.01173.x. [DOI] [PubMed] [Google Scholar]
- 43.Barriuso Lapresa L, Sanz Barbero B. Multilevel analysis of the use of oral health services by the pediatric population. Gac Sanit. 2011;25(5):391–396. doi: 10.1016/j.gaceta.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 44.Palència L, Espelt A, Rodríguez-Sanz M, Rocha KB, Pasarín MI, Borrell C. Trends in social class inequalities in the use of health care services within the Spanish National Health System, 1993–2006. Eur J Health Econ. 2011 doi: 10.1007/s10198-011-0362-7. [DOI] [PubMed] [Google Scholar]
- 45.Garrido-Cumbrera M, Borrell C, Palència L, Espelt A, Rodríguez-Sanz M, Pasarín MI, et al. Social class inequalities in the utilization of health care and preventive services in Spain, a country with a national health system. Int J Health Serv. 2010;40(3):525–542. doi: 10.2190/HS.40.3.h. [DOI] [PubMed] [Google Scholar]
- 46.Somkotra T, Detsomboonrat P. Is there equity in oral healthcare utilization: experience after achieving Universal Coverage. Community Dent Oral Epidemiol. 2009;37(1):85–96. doi: 10.1111/j.1600-0528.2008.00449.x. [DOI] [PubMed] [Google Scholar]
- 47.De Looper M, Lafortune G. Measuring Disparities in Health Status and in Access and Use of Health Care in OECD Countries. OECD Health Working Papers No. 43. OECD. 2009 [Google Scholar]
- 48.McKee M, Stuckler D. The assault on universalism: how to destroy the welfare state. BMJ. 2011;343:d7973. doi: 10.1136/bmj.d7973. [DOI] [PubMed] [Google Scholar]
- 49.Inukai M, John MT, Igarashi Y, Baba K. Association between perceived chewing ability and oral health-related quality of life in partially dentate patients. Health Qual Life Outcomes. 2010;8:118. doi: 10.1186/1477-7525-8-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.D'Uva TB, O'Donnell O, van Doorslaer E. Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. Int J Epidemiol. 2008;37(6):1375–1383. doi: 10.1093/ije/dyn146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shelton BJ, Gilbert GH, Lu Z, Bradshaw P, Chavers LS, Howard G. Comparing longitudinal binary outcomes in an observational oral health study. Stat Med. 2003;22(12):2057–2070. doi: 10.1002/sim.1469. [DOI] [PubMed] [Google Scholar]
- 52.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 53.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey SG. Indicators of socioeconomic position (part 1) J Epidemiol Community Health. 2006;60(1):7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]


