Abstract
A multi-antigen multi-peptide vaccine, targeting proteins expressed in pre-invasive breast lesions, can stimulate Type I CD4+ T-cells which have been shown to be deficient in both breast cancer patients and mice that develop mammary tumors. Transgenic mice (TgMMTV-neu) were immunized with a multi-antigen peptide vaccine specific for neu, IGFBP-2 and IGF-IR at a time when some of the animals already had pre-invasive lesions (18 weeks of age). While immunization with each individual antigen was partially effective in inhibiting tumor growth, immunization with the multi-antigen vaccine was highly effective, blocking development of palpable lesions in 65% of mice and slowing tumor growth in the infrequent palpable tumors which did arise. Protection was mediated by CD4+ T-cells and the few slow-growing tumors that did develop demonstrated a significant increase in intratumoral CD8+ T-cells as compared to controls (p=0.0007). We also combined the vaccine with agents that were, by themselves, partially effective inhibitors of tumor progression in this model; lapatinib and the RXR agonist bexarotene. While the combination of lapatinib and vaccination performed similarly to vaccination alone (p=0.735), bexarotene and vaccination significantly enhanced disease free survival (p<0.0001) and approximately 90% of mice showed no pathologic evidence of carcinomas at 1 year. The vaccine also demonstrated significant clinical efficacy in an additional transgenic model of breast cancer (TgC3(I)-Tag). Chemo-immunoprevention combinations may be an effective approach to breast cancer prevention even when the vaccine is administered in the presence of subclinical disease.
Keywords: Vaccine, bexarotene, breast cancer, prophylactic, T-cell
Introduction
Vaccination targeting immunogenic proteins expressed by pre-invasive or proliferative breast lesions offers a unique approach to breast cancer prevention. Vaccines can elicit memory T-cells that remain in lymph nodes until exposed to the target antigen. After stimulation, T-cells migrate to the site of antigen expressing lesions regardless of location and will proliferate and destroy those lesions. HER-2/neu (HER2), insulin like growth factor binding protein 2 (IGFBP-2), and insulin like growth factor receptor-1 (IGF-IR) are overexpressed in multiple types of breast cancer and are associated with a poor prognosis.(1–4) Likewise, these proteins are immunogenic and elicit both humoral and cellular immunity in breast cancer patients.(5, 6) All three proteins are up regulated in high risk and pre-invasive breast lesions and expression of each is associated with an increased risk of developing invasive breast cancer. We examined whether prophylactic immunization against these proteins could prevent the development of palpable breast cancer in a preclinical model where pre-invasive lesions already exist in the preponderance of mice. This approach approximates the patient population of Phase III breast cancer prevention trials with SERMs and aromatase inhibitors which evaluated treatment over 3–5 years to a cancer endpoint. The short period of time needed to meet that endpoint implies that a significant proportion of the women who progressed were enrolled with incipient lesions.
The FVB/N-TgN (MMTVneu)-202Mul mouse (TgMMTV-neu) develop spontaneous mammary cancer. These cancers express neu, IGF-IR and IGFBP-2 and investigations have shown that growth of syngeneic implanted tumors can be significantly delayed by vaccinating mice with peptides, derived from each of these proteins, designed to elicit antigen specific CD4+ T-cells.(6–8) The mice are tolerant to their tumors and T-cells derived from tumor draining lymph nodes do not secrete interferon (IFN)-gamma (γ) when challenged with antigen.(9) The lack of Type I IFN-γ secreting tumor antigen specific T-cells has also been well described in breast cancer patients.(10) IFN-γ is needed for tumor recognition through activating antigen presenting cells (APC) to engage T-cells. Several prophylactic vaccine approaches employing immunization against a single antigen, neu, have been evaluated in TgMMTV-neu mice. The extent of protection in these studies was variable and vaccine efficacy decreased significantly with age at immunization.(11–13)
The multi-antigen multi-peptide vaccine, described here, was designed to preferentially stimulate CD4+ T-cells. Our goal was to determine if the vaccine could generate protective Type I immunity in the TgMMTV-neu and prevent the development of palpable breast cancer destined to occur in mice with pre-existing lesions. We immunized older mice to model the clinical translation of such an approach to mature adult women, with high risk of developing breast cancer, who would likely be the target population for preventative vaccination. We also questioned whether combining the vaccine with agents which are themselves partially effective in this model in inhibiting tumor progression, lapatinib and bexarotene, might enhance the anti-tumor efficacy of the approach.
Materials and Methods
Mice
Female TgMMTV-neu (FVB/N-TgN (MMTVneu)-202Mul) (Charles River Laboratory) and TgC3(I)-Tag mice (Dr. J Green, NCI) were used. Procedures were in compliance with the University of Washington Institutional Animal Care and Use Committee guidelines. Age-matched mice were used in experiments.
Expression of antigens in mammary lesions
Pre-invasive lesions were identified by a veterinary pathologist (PMT). Immunohistochemistry (IHC) was performed on pre-invasive and invasive tumors and cell lines. Paraffin embedded tissues were sectioned to 5 μm thickness. The sections were deparaffinized by washing in xylene twice for 5 minutes, dehydrated via ethanol dilutions (100%, 95%, 70%) for 3 minutes each and washed in distilled water. Tumor cells were processed via cytospin and stained similarly. Antigen retrieval was performed by microwave heating with odium citrate (pH 6) for 8 minutes. Tissue sections were cooled and rinsed with PBS. After blocking with 3% H2O2 for 5 minutes, sections were incubated with normal goat serum (10% in PBS) for one hour at room temperature. Primary antibodies against IGF-IR (C-20, Santa Cruz Biotechnology), IGFBP-2 (C-18, Santa Cruz) or neu (clone 7.16.4)(14) were applied (1:500 dilution (10% goat serum in PBS)) and the slides were incubated overnight at 4°C. Isotype control IgG included; rabbit IgG (sc-2027, Santa Cruz), goat IgG (sc-2053, Santa Cruz), and rat IgG (2A3, University of California San Francisco (UCSF)). Sections were washed three times for 5 minutes and incubated (1: 500) with a biotinylated anti-rabbit antibody for IGF-IR (BA-1000), a biotinylated anti-goat antibody for IGFBP-2 (BA-9500), or a biotinylated anti-rat antibody for neu (BA 9401) for one hour at room temperature (Vector Laboratories). After washing, slides were incubated with avidin-conjugated peroxidase (DAKO) at room temperature for 30 minutes, washed and treated with 3,3′-diaminobenzidine before counterstaining with hematoxlin (DAKO). Images were captured using Nikon 80i Eclipse microscope with digital camera with NIS Elements Basic research imaging software.
Vaccination and tumor protection or inhibition
Eighteen week old female TgMMTV-neu mice, without palpable lesions, were immunized with single antigen (2–3 peptides/antigen) or a multiple antigen (total 8 peptides) vaccine derived from the human HER2, IGF-IR, and IGFBP-2 proteins (Genemed Synthesis) (Supplemental Table 1). Peptides ranged from 10 to 18 amino acids in length and were 70% or more homologous with the mouse homologue (median 97%, range 70–100%). Vaccines were administered as previously described.(6) Animals received vaccines consisting of 50μg/each peptide admixed in either Freund’s (priming dose) or incomplete Freund’s (boosters) adjuvant sq every 2 weeks for 3 immunizations. Monthly boosters were then administered until experiments were terminated at 44–52 weeks. The mean number of vaccinations received was 6, range 5–7. Controls received adjuvant in PBS. Mice were evaluated for tumors via palpation as previously described.(6) Disease free survival (DFS) was defined as no evidence of palpable tumor. Overall survival (OS) was defined as the time period from birth to death regardless of cause; either the maximum tumor volume requiring euthanasia or termination of the experiment (n=15 mice/group).
To determine vaccine efficacy in a different mammary cancer phenotype, 6–8 week old TgC3(I)-Tag mice were vaccinated as described above with either the multi-antigen vaccine in adjuvant or adjuvant alone every 10–14 days for three immunizations. Two weeks following the last immunization, 1×106 cells of a syngeneic tumor cell line, M6, generated from a spontaneous tumor (Dr. J Green, NCI), was injected orthotopically into the mammary fat pads. The line was tested for antigen expression, as described above, 2 weeks prior to implant. Tumor growth was measured every 3 days until termination (n=5/group). Experiments were repeated with similar results.
Primary effector characterization and T-cell response
To standardize both tumor size and time from last vaccine prioir to cell depletions, blocking studies were performed using a tumor implant model with a cell line syngeneic to TgMMTV-neu, MMC.(14) Similar to M6, MMC was characterized for antigen expression 2 weeks prior to the described experiments. Mice were vaccinated three times, 14 days apart with the multi-antigen vaccine. MMC cells, 1×106, were implanted, two weeks from the last vaccine. Monoclonal antibodies were used for in vivo depletion (CD4+ and CD8+ T-cells, NK and B cells) via intraperitoneal (i.p.) injection of the specific antibody every other day (3X) during the week before MMC was implanted and twice per week until the experiment was terminated. Doses used for T-cell depletion were 300μg of anti-CD4 clone GK1.5 and 100μg of anti CD8 clone 2.43 (UCSF). The depletion of B cells and NK cells was performed using 100μg of an anti-CD22 clone CY34.1.2 and anti-CD56 clone PK136 (UCSF). Rat IgG2b and IgG2a were used as controls. Data is shown as the mean and SEM of 5 mice/group. Experiments were repeated once with similar results. IFN-γ ELISPOT assays were performed as published.(6) Antigens tested included the pools of peptides contained in the vaccine (10μg/ml/each peptide), an irrelevant Class II peptide, HIV Gag p17(15) (10μg/ml) or phytohemagglutinin (PHA) (1μg/ml), a nonspecific T-cell mitogen. Data is reported as mean absolute spots/well (SPW) ± SEM for 5 mice/group.
T-cell purification and adoptive transfer
CD3+ T-cells were purified from cells pooled from spleens of vaccinated and control mice using a Pan T-cell Isolation Kit (Miltenyi Biotec Inc). Purity of the CD3+ cells prior to infusions was an average of 92% (range 90–94%). Naïve TgMMTV-neu mice were injected subcutaneously on the mid-dorsum with 1×106 of MMC 24 hours prior to an intravenous tail vein infusion of 10×106 CD3+ T-cells derived from the experimental groups. Tumor growth was measured every other day (n=6 mice/group).
Evaluation of tumor infiltrating T-cells (TIL)
Tumors were frozen in Tissue-Tek OCT (16) and stored at −80°C. Frozen tumors were then sectioned (8μm), fixed in 75%/25% acetone/methanol for 5 min, and washed using PBS. Slides were incubated with normal goat serum (10% in PBS) for 1 hour at room temperature, washed, and incubated with rat anti-mouse CD8 (AbD Serotec) at 1:100 dilution in 10% goat serum/PBS overnight at 4°C. After washing, Alexa Fluor 488 goat anti-rat secondary antibody (Invitrogen) was added to the slides (1:1000) for one hour at room temperature. Prolong Gold antifade with DAPI mounting media (Invitrogen) was added after an additional wash and cover slips were attached. Positive cells and DAPI stained nuclei were counted in three random high powered microscopic fields per slide and expressed as a mean. The number of positive cells over the total number of nuclei in the field was expressed as %CD8+. Data is shown as the mean and SEM for 5 mice/group.
Cancer incidence and pathologic evaluation
Age at the time of first palpable tumor was determined in 50 female TgMMTV-neu mice. Fifteen mice, 18 weeks old, with no palpable disease, were subject to microscopic examination of mammary fat pads. Tissues were processed routinely, stained with hematoxylin and eosin, and examined for the presence of hyperplasia and neoplasia using published methods.(17) Similar methods were used to evaluate tissues from treated mice (Fig. 4C).
Figure 4. Bexarotene, but not lapatinib, in combination with a multi-antigen polyepitope vaccine significantly enhances vaccine efficacy.
(A) Percent of mice with disease free survival after vaccination (y-axis) by weeks from birth (x-axis); solid gray line, adjuvant controls; solid black line, multi-antigen vaccinated mice; dotted black line, lapatinib alone; dashed gray line, vaccine plus lapatinib, n=15 mice/group. Data is representative of 2 separate experiments. (B) Percent of mice with disease free survival after vaccination (y-axis) by weeks from birth (x-axis); solid gray line, adjuvant controls; solid black line, multi-antigen vaccinated mice; dotted black line, bexarotene alone; dashed gray line, vaccine plus bexarotene, n=15 mice/group. Data is representative of 2 separate experiments. (C) Percent specific disease states; adjuvant controls, bexarotene alone (B), vaccine (V), vaccine and bexarotene (V+B). Black bars, detectable cancer; gray bars, pre-invasive disease; white bars; histological NED.
Combination chemoprevention
Fifteen mice, aged 18 weeks, per group were assigned to; (1) adjuvant only; (2) 30mg/kg bexarotene (ONYX Scientific) administered for the duration of the experiment; (3) vaccine, administered as described above, with adjuvant, and (4) vaccine with adjuvant administered with 30mg/kg bexarotene for the duration of the experiment. Bexarotene, in 200μl sesame oil, was given by gavage 5 days/week. The adjuvant control group was gavaged with 200μl sesame oil alone. Tumor growth was measured. For experiments using lapatinib (Dr. C. Grubbs, University of Alabama), the same groups were repeated but in place of bexarotene, lapatinib was administered at 75mg/kg. One group received the vaccine with concurrent lapatinib and another received lapatinib alone. For administration of lapatinib, mice were gavaged 5 days/week with the drug in 200μl of sesame oil. The adjuvant control group was gavaged with 200μl of sesame oil alone. Lapatinib or oil control treatment was given for the duration of the experiment. The doses of agents used were those that have been shown to induce shown antiproliferative activity in mice. Each experimental group was composed of 15 mice.
Statistical analysis
Kaplan-Meier curves were generated to show the probability of disease free survival (DFS) and overall survival (OS). Curve comparisons were performed by the Gehan-Breslow-Wilcoxon test. The Student’s t test or Mann Whitney test was used to evaluate significance. Krukal Wallis test was used to assess equivalence across multiple groups. In all cases, a p value of <0.05 was considered significant. All statistical analyses were performed using GraphPad Prism version 3.02 (GraphPad Software).
Results
A prophylactic multi-antigen vaccine, targeting proteins expressed in pre-invasive mammary lesions, can inhibit cancer development and increase survival in TgMMTV-neu mice
The mouse homologues of all three proteins, IGFBP-2, IGF-IR and neu, demonstrated expression in hyperplastic mammary lesions in TgMMTV-neu mice (Supplemental Fig. 1). Fifty percent of multi-antigen immunized mice did not develop breast cancer as compared with 0% of controls (p<0.0001). The median DFS of vaccinated animals was significantly longer than those mice receiving adjuvant alone, 46 vs. 30 weeks (HR 3.959, CI 2.018 to 7.768) (Fig. 1A). At experiment termination, OS was also significantly different between the two groups (p<0.0002). The median OS of the vaccinated animals had not been reached while the median OS of the adjuvant control group was 40 weeks (HR 4.335, CI 1.886–9.962) (Fig. 1B).
Figure 1. A prophylactic multi-antigen vaccine, targeting proteins expressed in pre-invasive mammary lesions, can inhibit cancer development and increase survival in TgMMTV-neu mice.
(A) Percent of mice with DFS (y-axis) and (B) OS (y-axis) after vaccination by weeks (x-axis) from birth; solid gray line, adjuvant controls; solid black line, multi-antigen vaccinated mice, n=15/group. Data is representative of 3 separate experiments. (C) Percent of mice with DFS after vaccination (y-axis) by age (x-axis); solid gray line, controls; solid black line multi-antigen vaccine, dashed black line, neu specific vaccine; dotted gray line, IGF-IR specific vaccine; and dashed gray line, IGFBP-2 specific vaccine. (D) Tumor volume (y-axis) by day after MMC implant (x-axis) is shown for mice depleted of CD4 -◆- and CD8 -▼- T-cells, B-cells-x-, NK cells -▲-, and isotype controls IgG2a
 and IgG2b
and IgG2b
 . Animals receiving vaccine alone, -■-, as well as adjuvant controls, -●- are depicted. Data is representative of 2 separate experiments.
. Animals receiving vaccine alone, -■-, as well as adjuvant controls, -●- are depicted. Data is representative of 2 separate experiments.
The DFS of mice immunized with the multi-antigen vaccine was statistically higher than that mediated by any single antigen vaccine. Mice immunized with a neu-specific vaccine demonstrated a median DFS of 38 weeks as compared to 28 weeks in adjuvant controls (p=0.251 between groups) (Fig. 1C). The DFS was 38 weeks for IGF-IR immunized mice (p=0.367) and 37 weeks for IGFBP-2 vaccinated animals (p=0.251) compared to adjuvant controls. In the multi-antigen vaccinated cohort, 80% of the mice remained tumor free and the median DFS for the multi-antigen vaccinated mice was not reached at the time of experiment termination (p=0.0013 compared to adjuvant control). In addition, while the DFS of the single antigen vaccinated animals was not different from each other (p=0.965) the multi-antigen vaccine significantly prolonged DFS compared to any of the single antigen approaches (p=0.018).
Tumor protection was mediated by CD4+ T-cells (Fig. 1D). Splenocytes from immunized mice were tested for their ability to facilitate rejection of the graft tumor cells derived from TgMMTV-neu mice. Elimination of CD8+ T-cells, NK cells or B cells had no impact on the anti-tumor response elicited by the multi-antigen vaccine without T-cell depletion (p=0.99 all groups compared to vaccination alone). Similarly, isotype controls administered after vaccination were not significantly different from vaccine alone (p>0.1). Depletion of CD4+ T-cells within 2 weeks of completing immunizations, however, resulted in a significant loss of the tumor inhibitory effect of the multi-antigen vaccine (p=0.013 compared to vaccinewithout depletion). Indeed, vaccination followed by depletion of CD4+ T-cells resulted in an anti-tumor effect similar to administration of adjuvant alone (p=0.450).
To evaluate whether antigen coverage provided by the vaccine would effectively inhibit the growth of additional mammary cancer phenotypes, TgC3(I)-Tag mice, a model with mammary tumors that are neu− and estrogen receptor−-, were immunized and then challenged with syngeneic tumor. Tumor growth was significantly inhibited (p<0.00001) in the multi-antigen vaccinated mice as compared to the adjuvant controls (Supplemental Fig. 2A). Indeed, tumor inhibition occurred despite the fact spontaneous tumors in these mice show expression of only IGF-IR and IGFBP-2 but not neu (Supplemental Fig. 2B).
Multi-antigen vaccine induced T-cells, from both protected and unprotected mice, demonstrate significant antitumor activity
As vaccine efficacy was mediated by CD4+ T-cells, to determine a mechanism for vaccine failure, we first evaluated potential differences in the cellular immune response between groups. For those mice protected by multi-antigen vaccination (protected), the mean IFN-γ secreting cell response to the mix of epitopes was 591 spots/well (SPW) compared to 33 SPW for the HIV peptide (p<0.0001) (Fig. 2A). Animals who were immunized, but developed tumors (unprotected) demonstrated a mean IFN-γ secreting cell response to immunizing peptides of 450 SPW, significantly higher than the response to the HIV peptide (24 SPW) (p<0.001), but not as robust as the protected group (p=0.006) (Fig. 2B). In both groups, single antigen specific responses were greater than the adjuvant controls (p<0.0001). Animals immunized with the adjuvant alone did not develop antigen specific immunity to either the epitope mix or single antigen pools (Fig. 2C) with the mean IFN-γ response similar to the HIV peptide (p=0.621). There was no significant difference in PHA response in animals receiving vaccines (p=0.319).
Figure 2. Multi-antigen vaccine induced T-cells, from both protected and unprotected mice, demonstrate significant antitumor activity.
IFN-γ secreting cells quantified as spots per well (SPW) +/− SEM (x-axis) for (A) vaccinated mice protected from mammary cancer development, (B) vaccinated mice not protected from mammary cancer development, and (C) adjuvant control mice. For all groups (y-axis) white bars are the negative controls (no antigen (No Ag) and irrelevant HIV peptide (HIVp17), gray bars; responses to single antigen peptide pools (neu, IGFBP-2, IGF-IR), or to the pool of all antigen vaccinating peptides (Mix), and black bars; PHA response, n=5mice/group, assayed in quadruplicates. (D) Representative immunofluorescence for intratumoral CD8+ T-cells. I; adjuvant control tumor, II; vaccinated/unprotected tumor. (E) Percent of CD8+ cells in relation to the total number of nuclei/400X HPF (y-axis). Gray bar; controls, black bar; multi-antigen vaccinated tumors (x-axis), mean and SEM of 5 mice/group, ***p<0.001. (F) Mean and SEM for tumor growth (mm2) (y-axis) days (x-axis) after adoptive transfer of CD3+ cells from experimental groups.-●- denotes naïve, -■- adjuvant control vaccinated, -▲- vaccinated/protected, and -▼- vaccinated/unprotected derived T-cells (6 mice/group). The data is representative of two separately executed experiments.
Vaccine induced CD4+ T-cells have the capability of indirectly eliciting antigen specific CD8+ T-cells via the activation of tumor localized APC(18). The activated APC stimulate CD8+ T-cells, through a process called cross-priming resulting in CD8+ T-cells of multiple antigenic specificities responding to the tumor. An evaluation of the tumors of mice that developed mammary cancer after multi-antigen vaccination demonstrated that adjuvant vaccinated controls contained significantly less intratumoral CD8+ T-cells (mean 0.520+/−0.12%) (Figs. 2DI, 2E) compared with vaccinated mice (mean 5.8+/−1.1%), p=0.0007 (Figs. 2DII, 2E). This observation infersthat vaccine induced T-cells could traffic to tumor. Moreover, the kinetics of tumor growth in vaccine failures was significantly slower than adjuvant controls at both 20 days (p=0.021) and 40 days (p=0.007) after tumor detection. The mean rate of tumor growth in control animals was 16-mm3/day as compared to 8-mm3/day in vaccinated but unprotected animals.
To assess the functionality of the entire T-cell compartment, CD3+ T-cells derived from either protected or unprotected animals were adoptively transferred to tumor bearing mice. The tumors in mice treated with naïve cells were no different in size (509.5+/−37.9-mm2) than those animals treated with cells derived from adjuvant only group (506.67+/−32.7-mm2), p=0.749 (Fig. 2F). The tumors from mice treated with T-cells derived from the vaccinated animals were significantly smaller than either control, whether cells were derived from protected (134.4+/6.1-mm2), p=0.004, or unprotected (212.1+/−13.6-mm2), p=0.027, mice. T-cells obtained from the protected animals behaved similarly to T-cells from unprotected mice in inhibiting tumor growth (p=0.425).
Vaccine failure may be due to the presence of subclinical disease at the time immunizations are initiated
As significant levels of T-cells were generated by immunization and appeared to be functional, we questioned whether mice administered vaccines at 18 weeks of age had existing pre-invasive lesions. We evaluated the natural history of tumor development in 50 consecutive TgMMTV-neu mice born in our colony, contemporaneous to the experiments described here, and determined that 16% of animals were found to have palpable mammary cancers between 16–20 weeks; similar to the time we initiated immunizations (Fig. 3A). We next examined selected serial sections of the mammary tissue harvested from 18 week old mice that didn’t appear to have evidence of palpable mammary masses and determined only half of the mice (53%) were histologically free of any mammary disease (Fig. 3B). Forty seven percent of 18 week old animals had histological evidence of subclinical mammary lesions (Fig. 3B); 13% demonstrated focal hyperplasia, 27% multifocal hyperplasia, and 7% bore adenomas. Thus, many of the mice had lesions or presumably developed lesions early during the vaccination process.
Figure 3. Vaccine failure may be due to the presence of subclinical disease at the time immunizations are initiated.
(A) The number (y-axis) of TgMMTV-neu mice at specific age ranges (x-axis) at the time of first palpable mammary tumor (n=50). (B) Histological evaluation of resected mammary tissue at age 18 weeks (n=15) showing the percent of mice (y-axis) with no evidence of disease (NED), focal hyperplasia (Focal), multifocal hyperplasia (Multifocal), or adenoma (x-axis).
Bexarotene, but not lapatinib, in combination with a multi-antigen polyepitope vaccine significantly enhances vaccine efficacy
We hypothesized combining vaccination with known chemoprevention agents, lapatinib and bexarotene, that have been shown to inhibit progression of pre-invasive to invasive disease in the TgMMTV-neu mouse would increase vaccine efficacy(19, 20) Vaccination in combination with lapatinib was no more effective than vaccination alone (Fig. 4A). Detectable disease was present in 53% of the group that received lapatinib/vaccine as compared to 60% with vaccination alone (p=0.735). Both groups had a significantly improved DFS (not reached) vs. adjuvant controls (p=0.022). Twenty seven percent of mice treated with lapatinib alone were disease free (median DFS 40 weeks) as compared to 13% of adjuvant control mice (p=0.386).
In contrast, vaccine combined with bexarotene was highly effective (Fig. 4B). At study termination, the group that received combination prophylaxis had not yet reached a median DFS as compared to a median DFS of 25 weeks in the adjuvant control (p<0.0001, HR 20.14, CI 6.420–63.19). Vaccination alone was significantly better than adjuvant control with a median DFS of 49 weeks (p=0.016). The addition of bexarotene to vaccine significantly enhanced DFS vs. vaccine alone (p=0.024) (Fig. 4B). The DFS outcome of the bexarotene alone treated group was similar to the adjuvant controls (p=0.307).
One hundred percent of adjuvant control animals, 87% of bexarotene treated mice, and 66% of vaccine treated animals but only 13% of mice who received a combination of bexarotene and multi-antigen vaccination had palpable disease at study termination (Fig. 4C). We analyzed the mammary tissue from representative surviving mice with no evidence of palpable tumors. The highest proportion of mice without histological evidence of mammary cancer or pre-invasive disease, i.e. no evidence of disease (NED) was in the group that received combination prophylaxis, all mice evaluated (5/5) were NED (Fig. 4C).
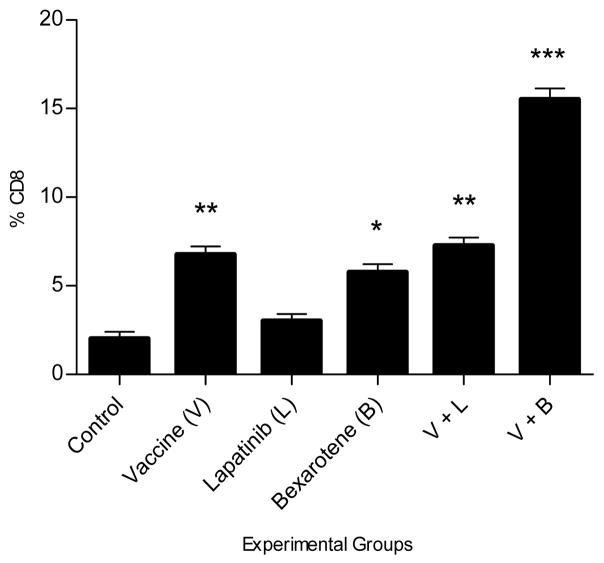
Oral bexarotene increases the number of CD8+ tumor infiltrating lymphocytes (TIL) in treated animals
We evaluated the number of CD8+ TIL from representative mice in each group that developed mammary cancer (Fig. 5). Both the vaccine alone (p=0.003) and the bexarotene alone groups (p=0.015) significantly increased the number of intratumoral T-cells over adjuvant controls while there was no difference between the controls and animals treated with lapatinib (p=0.100). Indeed, the addition of lapatinib to vaccination had no effect on the number of tumor infiltrating CD8+ T-cells and was equivalent to vaccination alone (p=0.604). The combination of the multi-antigen vaccine and bexarotene, however, resulted in a significant increase in the level of intratumoral CD8+ T-cells over vaccine alone (p=0.0014, p=0.0006 compared to adjuvant control) nearly doubling the relative number of tumor infiltrating CD8+ cells (Fig. 5).
Figure 5. Oral bexarotene increases the number of tumor infiltrating CD8+ T-cells in treated animals.
Percent of CD8+ cells in relation to the total number of nuclei (y-axis). Black bars (x-axis) represent the mean and SEM of the mice/experimental group; adjuvant control, vaccine (V), lapatinib alone (L), bexarotene alone (B), vaccine +lapatinib (V+L), vaccine+bexarotene (V+B). *, p<0.05, **p<0.01, ***p<0.001
Discussion
Data presented here demonstrate that vaccines stimulating antigen specific T-helper (Th) cells, and composed of a limited number of immunogenic proteins expressed in high risk lesions, can inhibit the development/progression of mammary cancer. Furthermore, vaccination may be an effective strategy for breast cancer prophylaxis, even in high risk and older women who may be bearing occult pre-invasive disease. Finally, our data suggests that some chemoprevention agents may act synergistically with vaccines. The synergistic effect of bexarotene with immunization may be due to the inherent immune stimulatory properties of RXR modulation.
HER2, one of the most commonly studied breast cancer antigens, is expressed in ductal carcinoma in situ (DCIS) and expression of the protein has been associated with a higher risk of the development of subsequent invasive disease.(21, 22) In addition, HER2+ DCIS is more likely to be estrogen receptor (ER)−.(23) Investigators have immunized patients with DCIS against HER2, prior to definitive resection, and demonstrated some resolution of lesions at the time of surgery.(24) Remaining lesions, however, were antigen negative either due to the generated immune response eliminating antigen expressing cells or immunity having no effect on cells which were HER2 negative. To mitigate the limited efficacy of single antigen vaccination we focused on both extending antigenic coverage and formulating a vaccine to stimulate CD4+ T-cells.(25) The insulin like growth factor (IGF) family of proteins has been shown to play a role in the progression of normal mammary tissue to pre-invasive lesions.(26) We have previously published that IGFBP-2 is immunogenic in breast cancer patients and over 40% of patients have an increased level of expression of IGFBP-2 in their tumors.(3, 6) IGFBP-2 has also been shown to have increased expression in atypical hyperplasia and DCIS as compared to normal glandular cells.(27) Increased expression of IGF-IR in normal breast tissue has been linked with a greater risk of developing breast cancer.(28, 29) Moreover, increased IGF-IR expression is correlated with non-invasive high risk breast lesions that are hormonally driven such as atypical ductal hyperplasia.(30) We have recently demonstrated that breast cancer patients have pre-existent immunity to IGF-IR.(8) We reasoned a vaccine targeting both HER2 and IGF family members may give broad phenotypic coverage of ER+ and ER− pre-invasive and high risk lesions. The observation that transgenic mouse models express similar proteins in pre-invasive mammary lesions provided a stringent model in which to evaluate immune prophylactic approaches for breast cancer prevention.
Vaccines designed to stimulate CD4+ T-cells may also function to enhance antigenic coverage. Type I cytokine secretion by Th, particularly IFN-γ, up regulates MHC class I expression on tumor cells, as well as APC, facilitating tumor recognition by CD8+ T-cells.(31) Tumor localized Th, secreting IFN-γ (Th1), will enable cross-presentation of tumor associated antigens by APC or dendritic cells to both CD4+ and CD8+ T-cells.(18) Our data showing depletion of CD4+ T-cells immediately after vaccine priming, resulting in the abrogation of an anti-tumor effect, suggests that the long term tumor inhibition observed in the TgMMTV-neu was due to an initial vaccine induced CD4+ T-cell response. The significant increase in intratumoral CD8+ T-cells, documented in vaccinated unprotected animals suggests that endogenous priming of tumor specific CD8 T-cells occurred. The ability of vaccine induced Th1 to modulate the tumor environment may have important consequences for breast cancer prophylaxis. A Type II T-cell (Th2) signature has been reported in DCIS.(32) Studies indicate Th2 may dominate the immune infiltration in breast cancer, secreting cytokines such as IL-13 and IL-4, which are conducive to breast cancer progression.(33) Thus, induction of a Th1 response may partially overcome the immunoinhibitory signature observed in progressing pre-invasive lesions.
The target population for a prophylactic breast cancer vaccine includes high risk and post menopausal women. Furthermore, the standard Phase III breast cancer prevention trial has used a cancer endpoint within 3–5 years implying many individuals may have pre-existing lesions. For this reason we immunized older, mature mice many of which have pre-invasive disease. Routinely, therapeutic vaccination has been marginally effective in eradicating established tumors. Analysis of prophylactic mastectomies, derived from women with a high risk of developing breast cancer, suggests a significant incidence of subclinical breast disease in many populations. A prospective evaluation of 67 women, almost 70% with known genetic mutations, demonstrated 57% harbored a high risk lesion or cancer with some women having multiple lesions.(34) A similar study found the incidence of occult carcinoma in situ or invasive disease to be almost 20%.(35) In over 200 post-mortem examinations in women with no known breast cancer risk, the incidence of both breast hyperplasia and carcinoma in situ was nearly 15%.(36) Further, we hoped that the multi-antigen approach would be effective against a variety of subtypes of breast cancer. We show activity in neu overexpressing and neu−/ER− mammary tumors. We are presently testing the vaccine in an ER+ model of breast cancer in rats.
We determined co-administration of agents, which were themselves partially effective in this model, could improve vaccine efficacy. The agents we combined with vaccination were lapatinib and bexarotene. Lapatinib is a dual tyrosine kinase inhibitor which blocks the activation of both HER2 and EGFR. Using the same dose we employed for this study, investigators have demonstrated lapatinib could significantly delay progression of hyperplastic lesions to invasive disease in TgMMTV-neu mice.(20) Similarly, bexarotene, an RXR-selective ligand has been shown to delay tumor progression when used as a chemoprevention agent in the model.(19) Treatment with either lapatinib or bexarotene alone delayed the development of tumors in mice however DFS was not statistically different between the agents and controls when initiated in 18-week old mice. Concurrent vaccination and oral bexarotene increased the number of disease free mice at 1 year by almost 50% compared to vaccination alone, suggesting bexarotene acts synergistically to enhance immune function. Lapatinib plus vaccination was not significantly different than vaccination alone.
There is evidence to indicate that treatment with bexarotene can both activate T-cells as well as prevent activation induced apoptosis. In vitro studies, incubating T-cell lymphoma lines with bexarotene, demonstrated a significant increase in IL-2 receptor (R) α and β on the surface of treated cells.(37) Th1, secreting IL-2, may activate other T-cells via IL-2R. This activation could be augmented by bexarotene treatment. In addition, RXR agonists have been shown enhance the survival of T-cells in vivo potentially preventing the “activation induced cell death” T-cells undergo when exposed to chronic amounts of cancer associated antigens.(38, 39) Examination of tumors from mice who failed prophylaxis with concurrent vaccination and bexarotene show a marked 2-fold increase of tumor infiltrating CD8+ T-cells vs. vaccination alone. Indeed, oral bexarotene, on its own, increased CD8+ TIL to the level of what was present in animals receiving vaccination alone implying that immune stimulation may be a significant contributor to the efficacy of bexarotene in multiple models of breast cancer. Lapatinib appeared to have little impact on the influx of CD8+ TIL.
A vaccine for breast cancer prevention could offer a significant advantage over other types of chemoprevention as, if effective, will generate lifelong protective immunity potentially requiring only occasional booster vaccines. The identification of antigens expressed in pre-invasive breast disease has allowed the development of a multi-antigen vaccine immunizing against early tumor promoting proteins in a manner analogous to vaccinating against the most important strains of a virus to prevent infection. Combination immune-chemoprophylaxis may significantly improve the protective efficacy of vaccines designed to prevent breast cancer in high risk populations and postmenopausal women.
Supplementary Material
Acknowledgments
Grant support: M. Disis is supported by a National Cancer Institute grant (N01-CN-53300/WA#10, U01 CA141539, P50 CA083636), and the Ovarian Cancer Research Fund. M. Disis is supported by the Athena Distinguished Professorship of Breast Cancer Research.
Footnotes
COI: MLD is an inventor on patents held by University of Washington that pertain to data presented in this manuscript.
References
- 1.Dawood S, Hu R, Homes MD, Collins LC, Schnitt SJ, Connolly J, et al. Defining breast cancer prognosis based on molecular phenotypes: results from a large cohort study. Breast Cancer Res Treat. 2010 doi: 10.1007/s10549-010-1113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nielsen TO, Andrews HN, Cheang M, Kucab JE, Hsu FD, Ragaz J, et al. Expression of the insulin-like growth factor I receptor and urokinase plasminogen activator in breast cancer is associated with poor survival: potential for intervention with 17-allylamino geldanamycin. Cancer Res. 2004;64:286–91. doi: 10.1158/0008-5472.can-03-1242. [DOI] [PubMed] [Google Scholar]
- 3.Probst-Hensch NM, Steiner JH, Schraml P, Varga Z, Zurrer-Hardi U, Storz M, et al. IGFBP2 and IGFBP3 protein expressions in human breast cancer: association with hormonal factors and obesity. Clin Cancer Res. 2010;16:1025–32. doi: 10.1158/1078-0432.CCR-09-0957. [DOI] [PubMed] [Google Scholar]
- 4.So AI, Levitt RJ, Eigl B, Fazli L, Muramaki M, Leung S, et al. Insulin-like growth factor binding protein-2 is a novel therapeutic target associated with breast cancer. Clin Cancer Res. 2008;14:6944–54. doi: 10.1158/1078-0432.CCR-08-0408. [DOI] [PubMed] [Google Scholar]
- 5.Disis ML, Knutson KL, Schiffman K, Rinn K, McNeel DG. Pre-existent immunity to the HER-2/neu oncogenic protein in patients with HER-2/neu overexpressing breast and ovarian cancer. Breast Cancer Res Treat. 2000;62:245–52. doi: 10.1023/a:1006438507898. [DOI] [PubMed] [Google Scholar]
- 6.Park KH, Gad E, Goodell V, Dang Y, Wild T, Higgins D, et al. Insulin-like growth factor-binding protein-2 is a target for the immunomodulation of breast cancer. Cancer Res. 2008;68:8400–9. doi: 10.1158/0008-5472.CAN-07-5891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai VP, Gad E, Bigdeli L, Dang Y, Stannard C, Disis ML. Antigen-specific T cells cultured in IL-21 demonstrate superior antitumor efficacy secondary to the secretion of IL-17 and TNF-a. J Immunother. 2009;32:954. [Google Scholar]
- 8.Cecil D, Park KH, Gad E, Higgins D, Childs J, Disis ML. IGF-IR peptide-based vaccines inhibit tumor growth in a murine model of breast cancer. J Immunother. 2009;32:954. [Google Scholar]
- 9.Kurt RA, Whitaker R, Baher A, Seung S, Urba WJ. Spontaneous mammary carcinomas fail to induce an immune response in syngeneic FVBN202 neu transgenic mice. Int J Cancer. 2000;87:688–94. [PubMed] [Google Scholar]
- 10.Inokuma M, dela Rosa C, Schmitt C, Haaland P, Siebert J, Petry D, et al. Functional T cell responses to tumor antigens in breast cancer patients have a distinct phenotype and cytokine signature. J Immunol. 2007;179:2627–33. doi: 10.4049/jimmunol.179.4.2627. [DOI] [PubMed] [Google Scholar]
- 11.Saha A, Chatterjee SK. Dendritic cells pulsed with an anti-idiotype antibody mimicking Her-2/neu induced protective antitumor immunity in two lines of Her-2/neu transgenic mice. Cell Immunol. 2010;263:9–21. doi: 10.1016/j.cellimm.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Manjili MH, Wang XY, Chen X, Martin T, Repasky EA, Henderson R, et al. HSP110-HER2/neu chaperone complex vaccine induces protective immunity against spontaneous mammary tumors in HER-2/neu transgenic mice. J Immunol. 2003;171:4054–61. doi: 10.4049/jimmunol.171.8.4054. [DOI] [PubMed] [Google Scholar]
- 13.Pupa SM, Invernizzi AM, Forti S, Di Carlo E, Musiani P, Nanni P, et al. Prevention of spontaneous neu-expressing mammary tumor development in mice transgenic for rat proto-neu by DNA vaccination. Gene Ther. 2001;8:75–9. doi: 10.1038/sj.gt.3301360. [DOI] [PubMed] [Google Scholar]
- 14.Knutson KL, Almand B, Dang Y, Disis ML. Neu antigen-negative variants can be generated after neu-specific antibody therapy in neu transgenic mice. Cancer Res. 2004;64:1146–51. doi: 10.1158/0008-5472.can-03-0173. [DOI] [PubMed] [Google Scholar]
- 15.Ramduth D, Day CL, Thobakgale CF, Mkhwanazi NP, de Pierres C, Reddy S, et al. Immunodominant HIV-1 Cd4+ T cell epitopes in chronic untreated clade C HIV-1 infection. PLoS One. 2009;4:e5013. doi: 10.1371/journal.pone.0005013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagahama M, Otsuka A, Oda M, Singh RK, Ziora ZM, Imagawa H, et al. Effect of unsaturated bonds in the sn-2 acyl chain of phosphatidylcholine on the membrane-damaging action of Clostridium perfringens alpha-toxin toward liposomes. Biochim Biophys Acta. 2007;1768:2940–5. doi: 10.1016/j.bbamem.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Cardiff RD, Anver MR, Gusterson BA, Hennighausen L, Jensen RA, Merino MJ, et al. The mammary pathology of genetically engineered mice: the consensus report and recommendations from the Annapolis meeting. Oncogene. 2000;19:968–88. doi: 10.1038/sj.onc.1203277. [DOI] [PubMed] [Google Scholar]
- 18.Matsuo M, Nagata Y, Sato E, Atanackovic D, Valmori D, Chen YT, et al. IFN-gamma enables cross-presentation of exogenous protein antigen in human Langerhans cells by potentiating maturation. Proc Natl Acad Sci U S A. 2004;101:14467–72. doi: 10.1073/pnas.0405947101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Y, Zhang Y, Hill J, Kim HT, Shen Q, Bissonnette RP, et al. The rexinoid, bexarotene, prevents the development of premalignant lesions in MMTV-erbB2 mice. Br J Cancer. 2008;98:1380–8. doi: 10.1038/sj.bjc.6604320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strecker TE, Shen Q, Zhang Y, Hill JL, Li Y, Wang C, et al. Effect of lapatinib on the development of estrogen receptor-negative mammary tumors in mice. J Natl Cancer Inst. 2009;101:107–13. doi: 10.1093/jnci/djn436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerlikowske K, Molinaro AM, Gauthier ML, Berman HK, Waldman F, Bennington J, et al. Biomarker expression and risk of subsequent tumors after initial ductal carcinoma in situ diagnosis. J Natl Cancer Inst. 2010;102:627–37. doi: 10.1093/jnci/djq101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roses RE, Paulson EC, Sharma A, Schueller JE, Nisenbaum H, Weinstein S, et al. HER-2/neu overexpression as a predictor for the transition from in situ to invasive breast cancer. Cancer Epidemiol Biomarkers Prev. 2009;18:1386–9. doi: 10.1158/1055-9965.EPI-08-1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nofech-Mozes S, Spayne J, Rakovitch E, Kahn HJ, Seth A, Pignol JP, et al. Biological Markers Predictive of Invasive Recurrence in DCIS. Clin Med Oncol. 2008;2:7–18. [PMC free article] [PubMed] [Google Scholar]
- 24.Czerniecki BJ, Roses RE, Koski GK. Development of vaccines for high-risk ductal carcinoma in situ of the breast. Cancer Res. 2007;67:6531–4. doi: 10.1158/0008-5472.CAN-07-0878. [DOI] [PubMed] [Google Scholar]
- 25.Disis ML, Gooley TA, Rinn K, Davis D, Piepkorn M, Cheever MA, et al. Generation of T-cell immunity to the HER-2/neu protein after active immunization with HER-2/neu peptide-based vaccines. J Clin Oncol. 2002;20:2624–32. doi: 10.1200/JCO.2002.06.171. [DOI] [PubMed] [Google Scholar]
- 26.Kleinberg DL, Wood TL, Furth PA, Lee AV. Growth hormone and insulin-like growth factor-I in the transition from normal mammary development to preneoplastic mammary lesions. Endocr Rev. 2009;30:51–74. doi: 10.1210/er.2008-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Busund LT, Richardsen E, Busund R, Ukkonen T, Bjornsen T, Busch C, et al. Significant expression of IGFBP2 in breast cancer compared with benign lesions. J Clin Pathol. 2005;58:361–6. doi: 10.1136/jcp.2004.020834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tamimi RM, Colditz GA, Wang Y, Collins LC, Hu R, Rosner B, et al. Expression of IGF1R in normal breast tissue and subsequent risk of breast cancer. Breast Cancer Res Treat. 2011;128:243–50. doi: 10.1007/s10549-010-1313-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Furstenau DK, Mitra N, Wan F, Lewis R, Feldman MD, Fraker DL, et al. Ras-related protein 1 and the insulin-like growth factor type I receptor are associated with risk of progression in patients diagnosed with carcinoma in situ. Breast Cancer Res Treat. 2011;129:361–72. doi: 10.1007/s10549-010-1227-y. [DOI] [PubMed] [Google Scholar]
- 30.Bhargava R, Beriwal S, McManus K, Dabbs DJ. Insulin-like growth factor receptor-1 (IGF-1R) expression in normal breast, proliferative breast lesions, and breast carcinoma. Appl Immunohistochem Mol Morphol. 2011;19:218–25. doi: 10.1097/PAI.0b013e3181ffc58c. [DOI] [PubMed] [Google Scholar]
- 31.Zhou F. Molecular mechanisms of viral immune evasion proteins to inhibit MHC class I antigen processing and presentation. Int Rev Immunol. 2009;28:376–93. doi: 10.1080/08830180903013034. [DOI] [PubMed] [Google Scholar]
- 32.Kristensen VN, Vaske CJ, Ursini-Siegel J, Van Loo P, Nordgard SH, Sachidanandam R, et al. Integrated molecular profiles of invasive breast tumors and ductal carcinoma in situ (DCIS) reveal differential vascular and interleukin signaling. Proc Natl Acad Sci U S A. 2012;109:2802–7. doi: 10.1073/pnas.1108781108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pedroza-Gonzalez A, Xu K, Wu TC, Aspord C, Tindle S, Marches F, et al. Thymic stromal lymphopoietin fosters human breast tumor growth by promoting type 2 inflammation. J Exp Med. 2011;208:479–90. doi: 10.1084/jem.20102131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoogerbrugge N, Bult P, de Widt-Levert LM, Beex LV, Kiemeney LA, Ligtenberg MJ, et al. High prevalence of premalignant lesions in prophylactically removed breasts from women at hereditary risk for breast cancer. J Clin Oncol. 2003;21:41–5. doi: 10.1200/JCO.2003.02.137. [DOI] [PubMed] [Google Scholar]
- 35.Leunen K, Drijkoningen M, Neven P, Christiaens MR, Van Ongeval C, Legius E, et al. Prophylactic mastectomy in familial breast carcinoma. What do the pathologic findings learn us? Breast Cancer Res Treat. 2008;107:79–86. doi: 10.1007/s10549-007-9525-8. [DOI] [PubMed] [Google Scholar]
- 36.Bhathal PS, Brown RW, Lesueur GC, Russell IS. Frequency of benign and malignant breast lesions in 207 consecutive autopsies in Australian women. Br J Cancer. 1985;51:271–8. doi: 10.1038/bjc.1985.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gorgun G, Foss F. Immunomodulatory effects of RXR rexinoids: modulation of high-affinity IL-2R expression enhances susceptibility to denileukin diftitox. Blood. 2002;100:1399–403. doi: 10.1182/blood-2002-01-0300. [DOI] [PubMed] [Google Scholar]
- 38.Rasooly R, Schuster GU, Gregg JP, Xiao JH, Chandraratna RA, Stephensen CB. Retinoid x receptor agonists increase bcl2a1 expression and decrease apoptosis of naive T lymphocytes. J Immunol. 2005;175:7916–29. doi: 10.4049/jimmunol.175.12.7916. [DOI] [PubMed] [Google Scholar]
- 39.Lu B, Finn OJ. T-cell death and cancer immune tolerance. Cell Death Differ. 2008;15:70–9. doi: 10.1038/sj.cdd.4402274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.