Abstract
Background
Latinas in the U.S. are less physically active than non-Latino white women, and also report higher levels of diabetes, obesity, and other conditions related to inactivity. Interventions are needed to address disparities in this high-risk group.
Purpose
To evaluate the efficacy of a culturally adapted, Spanish-language, individually tailored, computer expert system–driven physical activity print-based intervention for adult Latinas.
Design
RCT.
Setting/participants
Participants were 266 inactive adult Latinas who participated between 2009 and 2012.
Intervention
Participants were randomized to one of two treatment arms: a 6-month tailored physical activity intervention condition or wellness contact control. For both conditions, print materials were delivered by mail.
Main outcome measures
The main outcome measure was change in weekly moderate to vigorous physical activity (MVPA) measured by the 7-Day Physical Activity Recall interview, which was administered at baseline and post-intervention (6 months). Participants also wore accelerometers for a week at baseline and follow-up. Analyses were conducted in 2013.
Results
Increases in minutes/week of MVPA measured by the 7-Day PAR were significantly greater in the intervention group compared to the control group (mean difference=41.36, SE=7.93, p<0.01). This difference was corroborated by accelerometer readings (rho=0.44, p<0.01). Further, results indicate that intervention participants had greater increases in self-efficacy, cognitive processes and behavioral processes at 3 months compared to control paricipants (p’s<0.05).
Conclusions
The tailored Spanish-language intervention was effective in increasing MVPA among predominantly low-income, less-acculturated Latinas. Such print-based interventions are poised for widespread dissemination, and thus may help address health disparities.
Introduction
Regular physical activity (PA) is associated with lower morbidity and mortality from heart disease, diabetes, obesity, hypertension, and other chronic diseases.1–3 Yet PA rates in the U.S. are markedly low.4,5 Latinos in particular report the highest rates of inactivity (44%) and also suffer disproportionately from conditions linked to sedentary lifestyle, including diabetes, obesity, and metabolic syndrome.5–7 These disparities represent a significant public health concern and are especially pronounced among Latino women.5 Thus, interventions to increase PA in Latinas are especially needed.
Several PA interventions have targeted Latinas by providing materials and site-based programs in Spanish and/or delivering such interventions through bicultural clinicians or researchers.8 However, retention of and adherence to site-based interventions with Latinas has been challenging,9–11 along with a number of barriers to participating in PA (e.g., limited transportation, lack of personal free time).12–14 In one study, 151 Latinas were randomized to Spanish-language dance classes in “store-front” locations near a community clinic or to a safety education control.12 While the women in the aerobic dance group reported more vigorous exercise and improved fitness compared to those in the control group, the authors noted that continuous rigorous outreach from study staff was necessary to maintain attendance at classes. To be both effective and sustainable, then, PA interventions with this population will likely need to allow for flexibility in time and location of activity, in addition to addressing other unique cultural barriers such as the expectation to put the needs of one’s family before oneself.9,14
Additionally, few interventions have directly targeted psychosocial constructs shown to predict PA adoption in Latinas, signaling a need for interventions that are both culturally adapted to Latinas and targeted to population-specific theory-based predictors of PA. Previous research has shown that computer expert system–driven, individually tailored, theory-based print interventions (based on the Transtheoretical Model and Social Cognitive Theory) can significantly increase PA in predominantly non-Hispanic white individuals.15,16 These interventions have potential for increasing PA in Latinas, as they can be delivered through the mail, allowing individuals to exercise wherever and whenever it is convenient for them.
In addition, these interventions incorporate theoretic constructs, such as social support and self-efficacy, shown to predict greater activity in Latinas.17–19 Therefore, formative research was conducted to culturally and linguistically adapt this intervention for Latinas,20 and the adapted intervention was tested (N=93) in a pilot study.21 Results supported the feasibility and acceptability of using such an approach to promote PA in Latinas.21 The objective of the current study was to conduct a fully powered RCT (Seamos Saludables) to test the efficacy of the culturally adapted PA intervention for Latinas.20 It was hypothesized that, after 6 months, women randomized to the intervention arm would report significantly greater increases in weekly moderate-to-vigorous physical activity (MVPA) than those randomized to a wellness contact control condition.
Methods
Design
The Seamos Saludables study is an RCT of a 6-month culturally and linguistically adapted, individually tailored PA print intervention for Latinas versus a wellness contact control condition. Data were collected between 2009 and 2012. The primary dependent variable is self-reported weekly PA at baseline and 6 months as measured by the 7-Day Physical Activity Recall (7-Day PAR; for more detailed information on the design, see Pekmezi et al.20).
Setting and Sample
The study was conducted at the Institute for Community Health Promotion at Brown University. Human subjects’ approval was obtained from the Brown University IRB. Participants meeting inclusion criteria were adult women (aged 18–65 years) who self-identified as Hispanic or Latina (or of a group defined as Hispanic/Latino by the Census Bureau); could read and write in Spanish; and were underactive, which was defined as participating in MVPA ≤ 2 days per week for ≤ 30 minutes each day. Recruitment involved advertising in local Spanish-language newspapers, radio and TV stations, and recruiting at Latino churches, festivals, and events.
Exclusion criteria included being positive for any item on the Physical Activity Readiness Questionnaire (PAR-Q),22 a screening tool recommended by the American College of Sports Medicine (ACSM) to determine safety of adopting unsupervised physical activity. Exclusion items included a history of coronary heart disease, diabetes, stroke, osteoarthritis, osteoporosis, orthopedic problems, or any other serious medical condition that could make PA unsafe, as well as current or planned pregnancy, planning to move from the area within the next 12 months, hospitalization due to a psychiatric disorder in the past 3 years, BMI >45, and/or taking medication that may impair PA tolerance (e.g., beta blockers).
Protocol
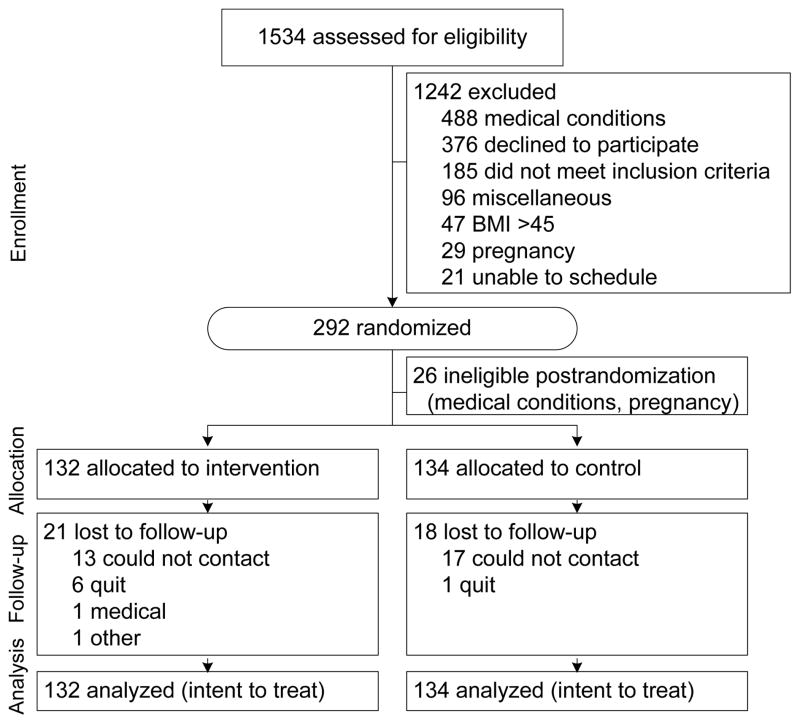
After a telephone screening interview to determine initial eligibility, participants attended an orientation session and completed the informed consent process. At the next session, participants were measured (anthropometry, blood pressure, percentage body fat) and received ActiGraph GT3X accelerometers, with instructions to wear the accelerometer during waking hours for 7 consecutive days. On return of the accelerometers, participants completed baseline PA measures and were randomly assigned to one of two Spanish-language print-based mail-delivered intervention conditions: PA or wellness. Group assignment was determined by a list of random numbers (using a permuted block-randomization procedure implemented in MATLAB), which was stratified by stage of change to ensure an equal distribution of various levels of motivational readiness for PA across groups. Research staff was blind to the randomization schedule. All participants received regular mailings over the next 6 months (four mailings in Month 1, two in Months 2–3, and one in Months 4–6) and then returned to the research center for post-intervention assessments (Figure 1).
Figure 1.
Study flow diagram
Measures
Demographics assessed at baseline included age, education, income, occupation, race, ethnicity, history of residence, and marital status. Acculturation and health literacy were assessed using the Brief Acculturation Scale (BrAS), a four-item measure that asks about language use across various life contexts,23 and the Short Test of Functional Health Literacy in Adults (STOFHLA), a measure designed to evaluate adult literacy in the healthcare setting.24 For a more detailed account of the measures used, see Pekmezi et al.20
The primary outcome measure, the 7-Day PAR,25,26 was completed at baseline and 6-month assessments. The 7-Day PAR is an interviewer-administered measure of MVPA performed during the prior week across contexts (e.g., leisure, occupation) in a minimum of 10-minute bouts. It has consistently demonstrated acceptable reliability, internal consistency, and congruent validity with other more objective measures of PA (e.g., accelerometers).27–35 It is sensitive to changes in moderate-intensity PA over time36,37 and has good test–retest reliability among Latino participants.38 To corroborate the self-report 7-Day PAR data, participants also wore ActiGraph GT3X accelerometers for 7 days prior to the baseline and 6-month assessments (overlapping with the 7-Day PAR recall period). Accelerometers were used to measure both movement and intensity of activity and have been validated with heart rate telemetry39 and total energy expenditure.40 Accelerometer data was processed using ActiLife 5 software, with a cutpoint of 1952 as the minimum threshold for moderate-intensity activity and minimum activity duration of 10 minutes.
Three psychosocial measures—stage of change, self-efficacy for PA, and the processes of change—were administered face-to-face at baseline and 6 months and via mail at 3 months. Intervention participants also completed these measures at 2, 4, and 5 months to generate the tailored expert-system feedback reports and assess for changes in theoretic constructs directly targeted by the intervention. The four-item stage-of-change measure has demonstrated reliability as well as shown acceptable concurrent validity with measures of self-efficacy and current activity levels.41 Self-efficacy, or confidence in one’s ability to persist with exercising in various situations (e.g., when feeling fatigued, during inclement weather) was measured with a five-item instrument41 developed by Marcus and colleagues (alpha=0.82). The 40-item processes measure contains ten subscales that address a variety of processes of PA behavior change. Internal consistency of the subscales ranged from 0.62 to 0.96.42
Tailored Intervention
The intervention is based on Social Cognitive Theory and the Transtheoretical Model and therefore emphasizes behavioral strategies for increasing PA (e.g., goal-setting, self-monitoring, problem-solving barriers, increasing social support, rewarding oneself for meeting PA goals). The intervention includes regular mailings of PA manuals matched to the participant’s current stage of motivational readiness for PA, individually tailored feedback reports, and tip sheets on selected topics (e.g., stretching, measuring heart rate). These reports are generated by a computer expert system and draw from a library of approximately 296 messages regarding motivation, self-efficacy, and cognitive and behavioral strategies for PA adoption based on participants’ responses to questionnaires.
The expert system also provides feedback on progress over time and compared to other individuals who have successfully adopted and maintained PA. Participants received pedometers and PA logs to encourage self-monitoring of PA behavior. To better meet the PA intervention needs and preferences of Latinas, the program was provided in Spanish and addressed PA barriers identified by Latinas in focus groups and in the literature review (lack of time, lack of motivation, childcare, partner support, personal empowerment, costs, inclement weather, gender roles, body-size ideals; see Pekmezi et al.20 for further details).
Wellness Contact Control Condition
The attention control condition received Spanish-language pamphlets on heart-healthy behaviors (other than PA) developed by the National Heart, Lung, and Blood Institute (NHLBI) for Latinos.43 The pamphlets focus on diet, smoking, and other factors associated with cardiovascular disease risk and were specifically targeted to Latinos aged 18–54 years with low levels of acculturation, SES, and education.
Data Analysis
Differences between conditions on baseline demographics, anthropometric and psychosocial measures were assessed using Wilcoxon rank-sum tests, t-tests, and chi-square tests as appropriate. For the primary outcome, minutes/week of MVPA, unadjusted M, range, and SD were examined and summarized overall and by intervention arm at baseline and 6-month follow-up.
Using a mixed-effects longitudinal regression model,44 between-group differences in minutes/week of MVPA were assessed at follow-up, controlling for baseline values, as well as potential covariates (variables not balanced by randomization). Models included random intercepts to account for within-subject correlation between repeated outcomes over time, and SEs were adjusted to account for clustering. All analyses were conducted on the intent-to-treat sample, including all participants randomized at baseline. Mixed-effects models use a likelihood-based approach to estimation and therefore made use of all available data without directly imputing missing outcome values. As a subsequent step, any occupational activity reported by participants was removed to specifically assess between-group differences in changes in leisure-time MVPA.
Using a longitudinal regression model implemented with generalized estimating equations (GEE’s)45,46 with robust SEs, the effect of treatment assigned was examined on the probability of meeting ACSM guidelines for PA (defined as reporting ≥ 150 minutes/week of MVPA47) at follow-up, controlling for potential confounders (in this case, variables not balanced by randomization). Specifically, binary indicators of meeting criteria on treatment assigned (intervention versus control); baseline level of PA; and potential covariates (as listed previously), were regressed using binomial errors, a logit link function and a working unstructured correlation to accommodate within-subject correlations. The correlation between the 7-day PAR and the ActiGraph was examined using Spearman rank correlations. The primary analysis (testing between-group differences in minutes/week of MVPA at follow-up) was repeated using data collected from the ActiGraph at baseline and 6-month follow-up.
Finally, as an exploratory step, between-group differences were assessed in intermediate variables targeted by the intervention, including self-efficacy, behavioral and cognitive processes. A series of generalized linear models assessed between-group differences in each of these constructs at 3-month follow-up, controlling for baseline values and potential confounders of the intervention effect. Intermediate variables were assessed at 3 months, as they were proposed a priori as potential mediators of the intervention effect and thus were measured earlier to guarantee that the temporal precedence assumption was met. All analyses were conducted in 2013 using SAS 9.3; significance level was set a priori at 0.05.
Results
Table 1 presents baseline characteristics of the sample, both overall and by intervention arm. Among the 266 women randomized at baseline, the average age was 40.67 years (SD=9.98) and mean BMI was 29.40 (SD=4.70). More than 90% were first-generation immigrants to the U.S., and >81% spoke only Spanish or more Spanish than English, suggesting that the group was low in acculturation. The majority were of Caribbean or South-American descent, with the largest groups being Dominican (37%) and Colombian (26%). Participants were also of limited financial means, with nearly half (47%) being unemployed and 54% reporting a family income below $20,000. A full description of the sample is provided in Table 1 and has been presented in detail elsewhere.20 Significant between-group differences at baseline were found for generation status and blood pressure (systolic and diastolic), p’s<0.05; hence, these variables were included as covariates in all final models. Follow-up was 87% at 6 months (no differential loss to follow-up between treatment arms).
Table 1.
Baseline Descriptives of Study Sample, M (SD) unless otherwise indicated
| Intervention n=132 | Wellness contact control n=134 | |
|---|---|---|
|
| ||
| BMI | 29.59 (4.34) | 29.21 (5.03) |
|
| ||
| Age, years | 41.61 (10.07) | 39.75 (9.84) |
|
| ||
| Generation, % * | ||
| First | 90.9 | 96.3 |
| Second | 6.8 | 3.7 |
| Third | 2.3 | 0 |
|
| ||
| Speak only Spanish or more Spanish than English at home, % | 79.5 | 83.4 |
|
| ||
| Country of Origin, % | ||
| Puerto Rican | 10.6 | 10.5 |
| Dominican | 34.1 | 40.6 |
| Mexican, Mexican-American, Chicana | 5.3 | 4.5 |
| Cuban | 0 | 0 |
| Guatemalan | 6.8 | 11.3 |
| Columbian | 30.3 | 21.8 |
| Other | 12.9 | 11.3 |
|
| ||
| Education, % at least some college) | 47.73 | 44.78 |
|
| ||
| Employment, % unemployed | 45.80 | 48.12 |
|
| ||
| Income (N=254), $ (%) | ||
| <20,000 | 52.8 | 54.4 |
| 20,000–29,999 | 15.0 | 15.7 |
| 30,000–39,999 | 11.0 | 6.3 |
| 40,000–49,999 | 7.1 | 3.9 |
| >=50,000 | 6.3 | 4.7 |
| Don’t Know | 7.9 | 15.0 |
|
| ||
| Marital status (% married/partnered) | 62.12 | 51.88 |
|
| ||
| Waist (inches) | 34.78 (4.34) | 34.16 (4.70) |
|
| ||
| Hips (inches) | 42.21(3.49) | 41.82 (4.06) |
|
| ||
| Systolic blood pressure* | 116.68 (11.16) | 120.07 (10.63) |
|
| ||
| Diastolic blood pressure* | 72.92 (8.53) | 75.83 (8.14) |
|
| ||
| Health literacy | 31.84 (5.19) | 31.81 (5.37) |
|
| ||
| Baseline self-efficacy | 2.19 (0.81) | 2.14 (0.76) |
|
| ||
| Baseline cognitive processes | 2.54 (0.83) | 2.48 (0.83) |
|
| ||
| Baseline behavioral processes | 2.00 (0.63) | 2.01 (0.64) |
p<0.05 for between-group differences
The median minutes/week of MVPA was zero for both PA intervention and control conditions at baseline (range was 0–35 in the intervention and 0–60 in control). Intervention participants (n=132) increased their self-reported mean minutes/week of MVPA from 1.87 (SD=6.86) at baseline to 73.36 minutes/week (SD=89.73) at 6-month follow-up. Control participants (n=134) increased their minutes/week of MVPA from a mean of 3.02 (SD=10.30) at baseline to 32.98 (SD=82.82) at 6 months.
The longitudinal regression model showed a significant treatment effect such that at 6 months, intervention participants reported an average of 41.36 (SE=7.93) minutes more MVPA compared to control participants, p<0.01, when controlling for baseline values, blood pressure and generation status. Model results are summarized in Table 2. There was no significant change in the estimated treatment effect when reported occupational activity was removed from total minutes/week of MVPA. Among participants randomized to the intervention arm, 15 (or 11.36%) reported meeting ACSM guidelines for PA at 6 months, versus only eight (or 5.97%) control participants. When controlling for blood pressure and generation status, there was a nearly significant treatment effect on the odds of meeting PA guidelines at 6-month follow-up (OR=2.34, p=0.07).
Table 2.
Estimated Fixed Effects from Longitudinal Model of Minutes/Week of moderate-to-vigorous physical activity
| Parameter estimate | SE | p-value | |
|---|---|---|---|
| Intervention effect | −0.03 | 7.17 | 0.99 |
| Indicator of 6-month follow-up | 29.82 | 7.35 | <0.01 |
| Intervention X 6- month follow-up | 41.39 | 10.57 | <0.01 |
Note: Model controlled for baseline PA, blood pressure and whether or not participants were born outside of the U.S.
Results also indicate a significant correlation between self-reported MVPA and objectively measured activity level at both baseline and 6 months (rho=0.26, p<0.01 at baseline and rho=0.44, p<0.01 at the 6-month follow-up). Note that correlations at 6 months correspond to the subsample of participants who both completed the 7-Day PAR and had available accelerometer data for the corresponding 7 days (n=198, 74% at 6 months). Results from a regression model suggest a significant effect of treatment on objectively measured MVPA at 6-month follow-up such that at 6 months, intervention participants were reporting an average of 35.64 (SE=7.37) more minutes of objectively measured MVPA than control participants, p<0.01, when controlling for baseline values, blood pressure and nativity.
Finally, initial exploration suggested significant associations between treatment assignment and potential mediators of the intervention effect (psychosocial variables at 3-month follow-up). Unadjusted effects have been summarized in Table 3. Regression models indicate that intervention participants had higher mean self-efficacy scores (b=0.52, SE=0.11, p<0.01); cognitive processes (b=0.37, SE=0.09, p<0.01); and behavioral processes (b=0.66, SE=0.08, p<0.01) at 3 months compared to control participants.
Table 3.
Unadjusted Mean Values of Potential Mediators by Group at Baseline and 3 Months
| Baseline | 3-Month Follow-up | |
|---|---|---|
|
| ||
| Self-Efficacy | ||
| Intervention | 2.19 (0.81) | 2.76 (0.98) |
| Wellness Contact Control | 2.14 (0.76) | 2.24 (0.78) |
|
| ||
| Behavioral Processes | ||
| Intervention | 2.00 (0.63) | 2.96 (0.75) |
| Wellness Contact Control | 2.01 (0.64) | 2.33 (0.73) |
|
| ||
| Cognitive Processes | ||
| Intervention | 2.54 (0.83) | 3.14 (0.80) |
| Wellness Contact Control | 2.48 (0.83) | 2.72 (0.82) |
Discussion
Findings support the efficacy of this technology-based approach to promoting physical activity in Latinas. As hypothesized, both self-report and objective data show that women randomized to the intervention group reported significantly greater increases in weekly MVPA after 6 months than those randomized to the wellness control condition. Effect sizes were relatively unchanged after removing occupational activity, suggesting that changes were primarily in leisure-time PA. The increase in physical activity produced by the intervention (approximately 70 minutes per week) may appear modest, but these changes have high potential clinical significance. Even small increases in PA can produce health benefits, especially for those who are initially inactive.48 Moreover, the current study achieved greater increases in PA than other interventions with this target population.8,49
Significant group differences were also found in the theoretic mediators directly targeted by the intervention. After 3 months, those in the intervention group reported significantly greater self-efficacy and cognitive and behavioral processes of change compared to control participants. These psychosocial constructs have been shown to predict PA adoption and maintenance, but there is a paucity of research examining the theoretic mechanisms of action behind PA behavior change in Latinas.50 Thus, the current study corroborates past results and extends these findings to a new population.
Limitations and Strengths
Limitations of the current study include the fact that the participants were self-selected, in that only individuals interested in joining a PA research program were recruited. Participants were also screened for health problems that would limit their ability to engage safely in a PA program. Therefore, this sample consisted of relatively motivated, healthy women with some degree of health literacy and advanced education, who may not be representative of the larger Latina population.
Additionally, while the materials utilized in the study were written at a basic reading level to accommodate individuals varying in levels of education, the print- based nature of the intervention may also limit its generalizability to participants with low reading and writing literacy. Overall, the sample was particularly low-income, with more than half reporting a yearly household income of <$20,000, suggesting that study protocols did not selectively exclude those of limited means, and less than 3% of screened participants were excluded due to low literacy. This finding is consistent with data from the focus groups, in which Latinas indicated that a print-based intervention was their preferred mode of delivery, as it would allow them to share materials with family and friends, suggesting that literacy was not a primary concern for this particular population.
This study has a number of strengths, including the RCT design and the diverse sample of Latinas from varying countries of origin. The majority of PA interventions with Latinos have focused on Mexican Americans, yet they may not be representative for all Latino subgroups, which differ in a number of health behaviors including PA.51,52 While Mexican Americans are the largest Latino subgroup in the U.S., other subgroups are growing at a faster rate,53 and may suffer from a higher prevalence of chronic diseases than Mexican Americans.54,55 Therefore, the inclusion of participants from diverse countries of origin is particularly important. Additionally, the participants in the current study were generally low in acculturation, representing a hard-to-reach group that often reports lower leisure-time PA than more highly acculturated Latinos.56 An additional strength is that the current study used both subjective and objective measures of activity, which demonstrated similar results.
Conclusion
Latinos now constitute the largest (and fastest-growing) ethnic minority group in the U.S. and are projected to constitute nearly one third of the population by 2050.57 Thus, health promotion programs for this population that are both effective and poised for widespread dissemination have the potential to positively affect public health and reduce health disparities. As the current intervention is automated and mail-delivered, it could have broad reach, particularly for individuals with limited financial or transportation resources. Past research has shown similar programs to be relatively low cost58 given that facilities and instructors are not required. In fact, high retention rates were achieved in the current study (87%) with minimal staff contact. Future studies should assess the longer-term effects of such interventions beyond the 6-month mark, and evaluate the potential of delivery via other media channels, such as the Internet or text messaging, which could further increase reach and decrease costs.
Acknowledgments
This research was supported by the National Institute of Nursing Research at the NIH (Grant NR011295). The authors thank collaborators Drs. Christina Lee, Charles Neighbors, Ernestine Jennings, and Ronnesia Gaskins for earlier contributions to this study. The authors thank Susan Carton-Lopez, Viveka Ayala-Heredia, Susan Pinheiro, Jane Wheeler, Jamie Longval, Jacqueline Parra, Joshua Marcus-Blank, and Rebecca Levenson of Brown University, as well as Raul Fortunet and Rachelle Edgar of the University of California, San Diego for their valuable assistance with this project. Most importantly, the authors thank the study participants for their time.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–9. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauman AE. Updating the evidence that physical activity is good for health: an epidemiological review 2000–2003. J Sci Med Sport. 2004;7(1 Suppl):6–19. doi: 10.1016/s1440-2440(04)80273-1. [DOI] [PubMed] [Google Scholar]
- 3.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carlson S, Densmore D, Fulton J, Your M, Kore Hr. Differences in physical activity prevalence and trends from 3 US surveillance systems: NHIS, NHANES, and BRFSS. J Phys Act Health. 2009;6(S1):S18–S27. doi: 10.1123/jpah.6.s1.s18. [DOI] [PubMed] [Google Scholar]
- 5.Pleis J, Ward B, Lucas J. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. Vital Health Stat 10. 2010;10(249) [PubMed] [Google Scholar]
- 6.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 7.Caballero AE. Type 2 diabetes in the Hispanic or Latino population: challenges and opportunities. Curr Opin Endocrinol Diabetes Obes. 2007;14(2):151–7. doi: 10.1097/MED.0b013e32809f9531. [DOI] [PubMed] [Google Scholar]
- 8.Staten LK, Gregory-Mercado KY, Ranger-Moore J, et al. Provider counseling, health education, and community health workers: the Arizona WISEWOMAN project. J Womens Health (Larchmt) 2004;13(5):547–56. doi: 10.1089/1540999041281133. [DOI] [PubMed] [Google Scholar]
- 9.Hovell MF, Mulvihill MM, Buono MJ, et al. Culturally tailored aerobic exercise intervention for low-income Latinas. Am J Health Promot. 2008;22(3):155–63. doi: 10.4278/ajhp.22.3.155. [DOI] [PubMed] [Google Scholar]
- 10.Keller CS, Cantue A. Camina por Salud: walking in Mexican-American women. Appl Nurs Res. 2008;21(2):110–3. doi: 10.1016/j.apnr.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harralson TL, Emig JC, Polansky M, Walker RE, Cruz JO, Garcia-Leeds C. Un Corazon Saludable: factors influencing outcomes of an exercise program designed to impact cardiac and metabolic risks among urban Latinas. J Community Health. 2007;32(6):401–12. doi: 10.1007/s10900-007-9059-3. [DOI] [PubMed] [Google Scholar]
- 12.Yancey A, Ory M, Davis S. Dissemination of physical activity promotion interventions in underserved populations. Am J Prev Med. 2006;31(4):82–91. doi: 10.1016/j.amepre.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 13.King A, Castro C, Eyler A, Wilcox S, Sallis J. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of U.S. middle-aged and older-aged women. Health Psychol. 2000;19(4):354–64. doi: 10.1037//0278-6133.19.4.354. [DOI] [PubMed] [Google Scholar]
- 14.Eyler AA, Baker E, Cromer L, King AC, Brownson RC, Donatelle RJ. Physical activity and minority women: a qualitative study. Health Educ Behav. 1998;25(5):640–52. doi: 10.1177/109019819802500510. [DOI] [PubMed] [Google Scholar]
- 15.Marcus B, Bock B, Pinto B, Forsyth L, Roberts M, Traficante R. Efficacy of an individualized, motivationally-tailored physical activity intervention. Ann Behav Med. 1998;20(3):174–80. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 16.Marcus B, Lewis B, Williams D, et al. Step into Motion: a randomized trial examining the relative efficacy of Internet vs. print-based physical activity interventions. Contemp Clin Trials. 2007;28(6):737–47. doi: 10.1016/j.cct.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Marquez DX, McAuley E. Social cognitive correlates of leisure time physical activity among Latinos. J Behav Med. 2006;29(3):281–9. doi: 10.1007/s10865-006-9055-6. [DOI] [PubMed] [Google Scholar]
- 18.Marquez DX, McAuley E, Overman N. Psychosocial correlates and outcomes of physical activity among Latinos: A review. Hisp J Behav Sci. 2004;26:195–229. [Google Scholar]
- 19.Hovell M, Sallis J, Hofstetter R, Barrington E, Hackley M, Castro F. Identification of correlated of physical activity among Latino adults. J Community Health. 1991;16:23–36. doi: 10.1007/BF01340466. [DOI] [PubMed] [Google Scholar]
- 20.Pekmezi DW, Dunsiger S, Gans K, et al. Rationale, design, and baseline findings from Seamos Saludables: a randomized controlled trial testing the efficacy of a culturally and linguistically adapted, computer- tailored physical activity intervention for Latinas. Contemp Clin Trials. 2012;33(6):1261–71. doi: 10.1016/j.cct.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pekmezi DW, Neighbors CJ, Lee CS, et al. A culturally adapted physical activity intervention for Latinas: a randomized controlled trial. Am J Prev Med. 2009;37(6):495–500. doi: 10.1016/j.amepre.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Whaley MH, editor. American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 7. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 23.Norris AE, Ford K, Bova CA. Psychometrics of a brief acculturation scale for Hispanics in a probability sample of urban Hispanic adolescents and young adults. Hisp J Behav Sci. 1996;18(1):29–38. [Google Scholar]
- 24.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 26.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 27.Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sloane R, Snyder DC, Demark-Wahnefried W, Lobach D, Kraus WE. Comparing the 7-day physical activity recall with a triaxial accelerometer for measuring time in exercise. Med Sci Sports Exerc. 2009;41(6):1334–40. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc. 2003;35(5):801–9. doi: 10.1249/01.MSS.0000064941.43869.4E. [DOI] [PubMed] [Google Scholar]
- 30.Irwin ML, Ainsworth BE, Conway JM. Estimation of energy expenditure from physical activity measures: Determinants of accuracy. Obes Res. 2001;9(9):517–25. doi: 10.1038/oby.2001.68. [DOI] [PubMed] [Google Scholar]
- 31.Johnson-Kozlow M, Sallis JF, Gilpin EA, Rock CL, Pierce JP. Comparative validation of the IPAQ and the 7-Day PAR among women diagnosed with breast cancer. Int J Behav Nutr Phys Act. 2006;3:7. doi: 10.1186/1479-5868-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leenders NYJM, Sherman WM, Nagaraja HN, Kien CL. Evaluation of methods to assess physical activity in free-living conditions. Med Sci Sport Exer. 2001;33(7):1233–40. doi: 10.1097/00005768-200107000-00024. [DOI] [PubMed] [Google Scholar]
- 33.Leenders NYJM, Sherman WM, Nagaraja HN. Comparisons of four methods of estimating physical activity in adult women. Med Sci Sport Exer. 2000;32(7):1320–6. doi: 10.1097/00005768-200007000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):S1–205. [PubMed] [Google Scholar]
- 35.Wilkinson S, Huang CM, Walker LO, Sterling BS, Kim M. Physical activity in low-income postpartum women. J Nurs Scholarship. 2004;36(2):109–14. doi: 10.1111/j.1547-5069.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 36.Dunn AL, Garcia ME, Marcus BH, Kampert JB, Kohl HW, Blair SN. Six-month physical activity and fitness changes in Project Active, a randomized trial. Med Sci Sports Exerc. 1998;30(7):1076–83. doi: 10.1097/00005768-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, 3rd, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281(4):327–34. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 38.Rauh MJ, Hovell MF, Hofsetter CR, Sallis JF, Gleghorn A. Reliability and validity of self-reported physical activity in Latinos. Int J Epidemiol. 1992;21(5):966–71. doi: 10.1093/ije/21.5.966. [DOI] [PubMed] [Google Scholar]
- 39.Janz KF. Validation of the CSA accelerometer for assessing children’s physical activity. Med Sci Sports Exerc. 1994;26(3):369–75. [PubMed] [Google Scholar]
- 40.Melanson EL, Jr, Freedson PS. Validity of the Computer Science and Applications, Inc. (CSA) activity monitor. Med Sci Sports Exerc. 1995;27(6):934–40. [PubMed] [Google Scholar]
- 41.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–6. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 42.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11(6):386–95. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 43.Alcalay R, Alvarado M, Balcazar H, Newman E, Huerta E. Salud para su Corazon: a community-based Latino cardiovascular disease prevention and outreach model. J Community Health. 1999;24(5):359–79. doi: 10.1023/a:1018734303968. [DOI] [PubMed] [Google Scholar]
- 44.Laird N, Ware J. Random-effects models for longitudinal data. Biometrics. 1982;38:963. [PubMed] [Google Scholar]
- 45.Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrics. 1986;73:12. [Google Scholar]
- 46.Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–3. [PubMed] [Google Scholar]
- 47.Haskell WL, Lee IM, Pate RR, et al. Physical Activity and Public Health: Updated Recommendation for Adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 48.DHHS. 2008 Physical Activity Guidelines for Americans. Washington, DC: DHHS; 2008. [Google Scholar]
- 49.Leeman-Castillo B, Beaty B, Raghunath S, Steiner J, Bull S. LUCHAR: using computer technology to battle heart disease among Latinos. Am J Public Health. 2010;100(2):272–5. doi: 10.2105/AJPH.2009.162115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–71. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 51.Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Soc Sci Med. 2005;61(1):53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 52.Neighbors CJ, Marquez DX, Marcus BH. Leisure-time physical activity disparities among Hispanic subgroups in the U. S Am J Public Health. 2008;98(8):1460–4. doi: 10.2105/AJPH.2006.096982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.U.S. Census Bureau. Statistical Abstract of the US: 2012. Washington DC: 2012. [Google Scholar]
- 54.Ai AL, Appel HB, Huang B, Lee K. Overall health and healthcare utilization among Latino American women in the U. S. J Womens Health (Larchmt) 2012;21(8):878–85. doi: 10.1089/jwh.2011.3431. [DOI] [PubMed] [Google Scholar]
- 55.Ai AL, Noel LT, Appel HB, Huang B, Hefley WE. Overall health and health care utilization among latino american men in the U.S. Am J Mens Health. 7(1):6–17. doi: 10.1177/1557988312452752. [DOI] [PubMed] [Google Scholar]
- 56.Crespo CJ, Smit E, Carter-Pokras O, Andersen R. Acculturation and leisure-time physical inactivity in Mexican American adults: results from NHANES III, 1988–1994. Am J Public Health. 2001;91(8):1254–7. doi: 10.2105/ajph.91.8.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Passel J, Cohn D. U.S. Population Projections: 2005–2050. Pew Research Hispanic Center. 2008 www.pewhispanic.org/2008/02/11/us-population-projections-2005-2050/
- 58.Sevick MA, Napolitano MA, Papandonatos GD, Gordon AJ, Reiser LM, Marcus BH. Cost-effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Prev Med. 2007;45(1):54–61. doi: 10.1016/j.ypmed.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]