ABSTRACT
Background: Pulmonary arterial hypertension (PAH) represents an emerging pathology in modern medicine. Transthoracic echocardiography is an inexpensive and reproducible method and it is the most commonly used non-invasive diagnostic tool to asses pulmonary artery pressure (PAP) and the function of the right ventricle. Although, the right heart catheterization is still considered as the standard for the diagnosis, according to the last guidelines, the new echocardiographic methods may offer an improved value in the PAH evaluation.
Aim: To evaluate if cardiac ultrasonography data correlate with catheterization results in patients with PAH (Group I Dana Point 2008), and to compare the ultrasonography evaluation of PAH patients with that of normal.
Methods: 15 consecutive patients (pts) (52±15 yrs, 5 men, time from onset of symptoms 1.6±1.7 years) with PAH of different aetiologies (12 pts with idiopathic PAH, 2 pts with PAH associated with scleroderma and one with persistent PAH after atrial septal defect (ASD) closure) were evaluated through: 1. clinical examination (NYHA class); 2. exercise capacity (6 minute walking test – 6MWT); 3. conventional echocardiography (diameter of right ventricle – RVD and right atrium, fractional area shortening – FAS, TAPSE, pulmonary ascension time – PA, systolic and mean PAP -sPAP, mPAP, tricuspid E/A ratio, cardiac index-CI) and 4. Tissue Doppler Imaging – TDI (systolic and diastolic myocardial velocities at the tricuspid annulus – S, D, A); 5. right heart catheterization (sPAP, mPAP, CI, pulmonary vascular resistance – PVR)
We compared classical and TDI echo parameters with those obtained from 15 normal subjects, matched in age and sex.
Results: PAH patients had high sPAP and mPAP with right heart dilation (RV - 44.8±7.3 mm), depressed TAPSE (16.2±5.9 mm) and cardiac index and low TDI systolic velocities at tricuspid level (7.3±2.9 cm/s). All parameters differed statistically significant from normal. There were no significant correlations between ultrasonography and catheterization (cath) parameters (sPAP 92±28.2 echo vs. 106.4±25.8 mmHg cath; mPAP 47.9±8.4 echo vs. 65.8±17.3 mmHg cath), excepting for CI 2.3±1.2 l/min/m2 vs. 2.08±0.3 ml/min/m2) and PVR (16.5 ± 15.3 Wood U echo, vs. 19.6 ± 7.9 cath).
Conclusion: Classic and TDI cardiac ultrasonography represents a good screening and monitoring tool for PAH patients, but tends to underestimate the severity of the disease, leaving right heart catheterization as the essential diagnostic method for this rare disease.
Keywords: pulmonary arterial hypertension, echocardiography, Tissue Doppler Imaging, right heart catheterization
INTRODUCTION
Pulmonary hypertension (PH) is a hemodynamic and pathophysiological condition defined as an increase in mean pulmonary arterial pressure (mPAP) ≥25 mmHg at rest as assessed by right heart catheterization (RHC). It includes various clinical conditions, grouped by the Dana Point 2008 classification (1,2). Pulmonary arterial hypertension (PAH, group 1 Dana Point) is a clinical condition characterized by the presence of pre-capillary PH (pulmonary wedge pressure PWP <15 mmHg), in absence of other causes such as PH due to lung diseases, chronic thromboembolic PH, or other rare diseases (1). PAH includes different forms that share a similar clinical picture and virtually identical pathological changes of the lung microcirculation (1).
As suggested by current guidelines, the assessment of a patient with suspected PH requires a series of investigations necessary to confirm the diagnosis, establish the clinical group of PH and, determine the degree of functional and hemodynamic impairment and finally to evaluate the prognosis. The workup includes: electrocardiogram, chest radiograph, echocardiography, pulmonary function tests and arterial blood gases, ventilation/perfusion lung scan, computed tomography (high-resolution and contrast-enhanced), cardiac magnetic resonance imaging, pulmonary angiography, blood tests and immunology, abdominal echocardiography and right heart catheterization (1).
Among these, for the hemodynamic evaluation, two are widely used in clinical practice: echocardiography, as screening and monitoring tool, reliable and non-invasive, and right heart catheterization, indispensable for establishing a final diagnosis. Both assessments are well correlated with prognosis (1).
Presently, the echocardiographic parameters recommended by the European guidelines as being useful to quantify PH are the following: the peak velocity of the tricuspid regurgitation jet, the right atrial pressure (estimated based on the diameter and respiratory variation of the inferior vena cava), the pulmonary regurgitation velocity, pulmonary acceleration time, dimensions of the right heart and of the pulmonary artery, RV thickness, and the shape and movement of the ventricular septum (1,3). The estimation of PAP based on Doppler transthoracic echocardiography measurements is not suitable for screening for mild, asymptomatic PH according to are several studies (3).
Modern echocardiographic techniques have penetrated into clinical practice during the last ten years. Among them, Tissue Doppler Imaging (TDI) plays a very important role, using Doppler principles to quantify the velocity of myocardial contraction (4) and being the first imaging method to determine in real time the movement velocities in solid tissue (5,6), therefore allowing an accurate evaluation of both systolic and diastolic function (7,8). In contrast to conventional Doppler ultrasound, which detects high velocities of small amplitude, TDI can detect low myocardial velocities, with high amplitude. For the assessment of right ventricular function, ultrasonographers use presently colour guided TDI, with real time analysis of tricuspid annular velocities and offline analysis of other RV wall segments. The method is simple and validated, but different studies have established different cut off values for RV dysfunction (between 9,5 and 11,5 cm/s for the tricuspid annular velocities) (8-11).
The 2010 guidelines for the echocardiographic assessment of the right heart in adults suggest systolic velocities S at the level of the lateral tricuspid annulus to be very useful for the evaluation of right heart function (12). A tricuspid annular systolic velocity S below <11.5 cm/s predicts RV dysfunction with a sensitivity of 90% and a specificity of 85% (8).
Due to the fact that echocardiography is a non-invasive, feasible, cost efficient imaging method, easy accessible for patients, we aimed to evaluate the correlations of cardiac ultrasonography data with catheterization results in patients with PAH, in a medical system where frequently RHC has limited availability. To further emphasise the role of classical and modern ultrasonography parameters in PAH diagnosis, we compared the ultrasonography evaluation of PAH patients with that of normal. ❑
METHODS
Study groups
We studied prospectively 15 consecutive patients (52±15 yrs, 5 men, time from onset of symptoms 1.6±1.7 years) addressed to our clinic for the evaluation and treatment of PAH of different etiologies (12 patients with idiopathic PAH, 2 patients with PAH associated with scleroderma and one persistent PAH after ASD surgical closure). Also, we examined 15 healthy controls (age and sex matched), recruited from the local population, without history of significant cardiovascular disease or risk factors and with normal physical examinations. All subjects were completely informed about the procedures and gave their informed consent.
Subjects from both study groups underwent a clinical examination and were referred to the cardiac ultrasonography laboratory, where they were evaluated by conventional and Tissue Doppler echocardiography. In PAH patients we also assessed exercise capacity (through 6MWT) and they were referred to the catheterization laboratory, where a RHC was performed.
Echocardiography
All individuals underwent an extensive echocardiographic examination using a commercially available ultrasonography machine equipped with TDI software, using a 2-4 MHz transducer (Vivid 7 Dimensions, GE Medical System, Horten, Norway). Heart rate and blood pressure were measured just before the study. The electrocardiogram was recorded simultaneously. All measurements were done in accordance with the current guidelines of the American Society of Echocardiography by the same well trained ultrasonographer (13).
Through conventional echocardiography the following parameters were assessed: right heart dimensions, right ventricular fractional area shortening (calculated in the apical 4 chamber view as the ratio : {RVTD area- RVTS area}/RVTD area), tricuspid annular plane systolic excursion (TAPSE), tricuspid regurgitation flow velocity and right ventricular-right atrial gradient, tricuspid diastolic E/A ratio, pulmonary ascension time (PA), systolic pulmonary artery pressure (based on the transtricuspid pressure gradient and the right atrial pressure estimated from the inferior vena cava dimensions) and mean pulmonary artery pressure (calculated based on the PA, using the formula: mPAP=79-0,45*PA) as well as cardiac index (calculated based on the LV outflow tract area and the aortic time velocity time integral, using the formula CI={(LVOT area* aortic VTI)*HR}/BSA). Pulmonary vascular resistance was determined using the formula PVR = mPAP/cardiac output (14).
Off-line pulsed-wave tissue velocity measurements at the level of the lateral tricuspid annulus were made in order to assess longitudinal right ventricular function. We determined: systolic velocities S and diastolic velocities ETri and ATri.
Right heart catheterization
All PAH subjects underwent invasive right heart catheterization at rest, using a Siemens AXIOM Sensis XP system. A Swan-Ganz catheter was inserted via brachial or femoral venous access in order to assess right chambers and pulmonary artery pressures (mPAP, sPAP and dPAP) and to obtain oximetry samples. Additionally, for all the patients, left heart catheterization was performed using a Pig-tail catheter and pressures and oximetry measurements were obtained from the left ventricle (LV) and aorta. For excluding a postcapillary pulmonary hypertension, both pulmonary wedge pressure (PWP) and LV end-diastolic pressure (LVEDP) were determined.
Cardiac output (CO) was determined by the Fick method, using the oxygen consumption. Cardiac index (CI) was calculated with the formula: CI (l/min/m2) = CO (l/min)/body surface (m2) and pulmonary vascular resistance (PVR) was calculated as: PVR (Wood units) = mPAP (mmHg)/ CO(l/min).
All the parameters were expressed as mean value of three different measurements, according to current recommendations (15,16). Heart rate and systemic blood pressure were measured just before the study. The electrocardiogram was recorded simultaneously.
Statistical analysis
Statistical analysis was performed with SPSS software (version 13.0) (SPSS Inc. Chicago, Illinois). Results are presented as mean value ± standard deviation or as absolute number (percentage). Differences between groups were tested for significance using the independent samples t-test for continuous variables. Univariate Pearson correlation was used to investigate the relation between cardiac ultrasonography and RHC parametric variables in the PAH group. A p <0.05 for a two-tailed test was considered significant. Bland-Altman analysis was used for calculating the relative mean differences (which reflect any systematic change between examinations) and their standard deviation (which reflects the degree of random variation in the measurements) between paired measurements through ultrasonography or RHC. Ninety-five percent confidence limits of a single estimate of the measurements were calculated as 2*SD/√2, and reported as absolute values and percentages from the mean value (17). ❑
RESULTS
Subjects
Baseline characteristics of the study groups are showed in Table 1. There were no significant differences between the two groups for age or body mass index, but as expected, PAH patients had a lower arterial blood pressure and a higher heart rate than controls. In the PAH group, mean NYHA class was 3, and mean 6MWT was 407.1 meters. PAH patients had no specific treatment at the enrolment in our study, our examination being part of the diagnostic algorithm.
Table 1.
Demographical characteristics of the study groups.
| PAH | Controls | P value | |
|---|---|---|---|
| Age (yrs) | 52.0 ± 15.0 | 60.4 ± 7.6 | NS |
| BMI (kg/m2) | 27.9 ± 5.3 | 27.0 ± 5.2 | NS |
| Systolic BP (mmHg) | 105 ± 15 | 127 ± 19 | 0.05 |
| Diastolic BP (mmHg) | 67 ± 7 | 73 ± 11 | 0.05 |
| Heart rate (bpm) | 94 ± 9 | 67 ± 8 | 0.05 |
* BP = blood pressure; BMI = body mass index.
Conventional echocardiography
Conventional right heart parameters are showed in Table 2. As expected, all parameters assessed were statistically significant different between the 2 study groups, with parameters in the PAH group way out of reference values suggested by current guidelines (8). PAH patients had high sPAP and mPAP with right heart dilation; also they had a depressed TAPSE and a low cardiac index.
Table 2.
Right heart structural and functional parameters (standard echocardiography, mean ± SD).
| Parameter | PAH | Controls | P value |
|---|---|---|---|
| RV transversal diameter (mm) | 44.8 ± 7.3 | 30.9 ± 3.2 | 0.01 |
| RA transversal diameter (mm) | 42.8 ± 6.2 | 35.0 ± 4.1 | 0.01 |
| RV free wall (mm) | 6.4 ± 2.3 | 4.0 ± 1.3 | 0.05 |
| TAPSE (mm) | 16.2 ± 5.9 | 23.9 ± 2.3 | 0.01 |
| FAS (%) | 42.8 ± 5.6 | 31.7 ± 6.5 | 0.01 |
| PA (mm) | 71.8 ± 42.9 | 107.8 ± 17.5 | 0.01 |
| mPAP (mmHg) | 47.9 ± 8.4 | 16.8± 9.1 | 0.01 |
| sPAP (mm Hg) | 92.6 ± 28.1 | 22.7 ± 7.7 | 0.01 |
| Tricuspid E/A ratio | 1.2 ± 0.5 | 0.8 ± 0.2 | 0.05 |
| Cardiac index (ml/min/m2) | 2.3 ± 1.2 | 3.0 ± 0.9 | 0.05 |
* RV = right ventricle; RA = right atrium; TAPSE = tricuspid annular plane systolic excursion; sPAP = systolic pulmonary artery pressure; mPAP = mean pulmonary artery pressure.
Tissue Doppler Imaging
Myocardial velocities at the level of the tricuspid annulus, assessed through Tissue Doppler imaging and interpreted offline are shown in Table 3. Systolic myocardial velocities were significantly lower in the PAH group, suggesting right heart systolic dysfunction in these patients. Also diastolic velocities were lower in the PAH group, with a modified E/A ratio, indicating the alteration of the right ventricular diastolic function.
Table 3.
RV myocardial velocities (TDI echocardiography, mean ± SD).
| Parameter | PAH | Controls | P value |
|---|---|---|---|
| STDI tricuspid annulus (cm/s) | 7.4 ± 3.0 | 10.2 ± 1.8 | 0.01 |
| ETDI lateral tricuspid annulus (cm/s) | 4.7 ± 2.9 | 8.7 ± 1.8 | 0.01 |
| ATDI lateral tricuspid annulus (cm/s) | 8.7 ± 3.9 | 9.9 ± 2.2 | 0.01 |
| ETDI/ATDI ratio | 0.6 ± 0.2 | 0.9 ± 0.5 | 0.05 |
Right heart catheterization and correlations with cardiac ultrasonography
Parameters determined through right heart catheterization had the following values: mPAP 65.8 ± 17.3 mmHg, sPAP 106.4 ± 2 5.8 mmHg, PVR 19.6 ± 7.9 Wood Units, CI 2.08 ± 0.3 ml/min/m2. All patients had a PWP and/or LVEDP <15 mmHg.
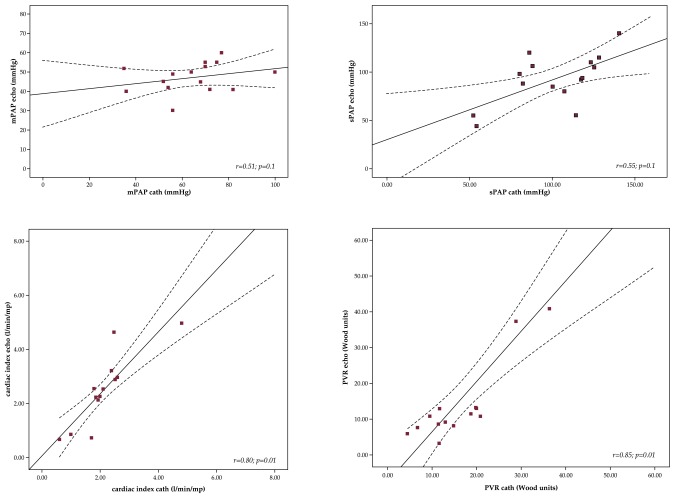
Using univariate analysis we investigated the correlations between some of the cardiac ultrasonography and RHC parameters. No statistically significant correlation was observed for mPAP and sPAP between values determined through the two methods: for mPAP r=0.55, p=0.1, and for sPAP r=0.51, p=0.1 (Table 4, Figure 1). Cardiac ultrasonography tends to underestimate PAP values. Cardiac index determined echocardiographically had a good correlation index with cardiac index through RHC: 2.3 ± 1.2 for cardiac ultrasonography, vs. 2.1 ± 0.3 for RHC, r=0.80, p=0.01 (Table 4, Figure 1). Also, PVR, determined echocardiographically using the formula mPAP/cardiac output, had significant correlation with PVR determined through RHC: 16.5 ± 15.3 for cardiac ultrasonography, vs. 19.6 ± 7.9 for RHC, r=0.85, p=0.01 (Table 4, Figure 1). Variability between ultrasonography and RHC measurements, calculated through Bland Altman analysis was very high for sPAP and mPAP (sPAP ±37 mmHg, ±36%, mPAP ±21 mmHg, ±38%), but was satisfactory for CI (±14%, ±0.3 l/min/m2) and PVR (±12.5%, ±2.3 Wood U). ❑
Table 4.
Correlations between echocardiographic and RHC parameters.
| Parameter | Echo | Cath | Correlation index | P value |
|---|---|---|---|---|
| sPAP (mmHg) | 92.6 ± 28.1 | 106.4 ± 25.8 | 0.55 | 0.1 |
| mPAP (mm Hg) | 47.9 ± 8.4 | 65.8 ± 17.3 | 0.51 | 0.1 |
| Cardiac index (ml/min/m2) | 2.3 ± 1.2 | 2.1 ± 0.3 | 0.80 | 0.01 |
| PVR (Wood U) | 16.5 ± 15.3 | 19.6 ± 7.9 | 0.85 | 0.01 |
Figure 1. Statistical correlations for mPAP, sPAP, cardiac index and PVR, echocardiography vs right heart catheterization (Pearson correlations).
DISCUSSION
Pulmonary arterial hypertension is a rare condition, but with high morbidity and mortality if untreated, comparatively with PH, a rather common hemodynamic condition. After a clinical suspicion, the steps towards final diagnosis include multiple imaging techniques, among which cardiac ultrasonography is the most feasible and cost efficient (1). Nevertheless, there are several studies suggesting the fact that echocardiography doesn't have the necessary accuracy in calculating both systolic and mean pulmonary artery pressure, with diagnostic errors in up to 20% of cases and that RHC remains unavoidable for the definitive diagnosis and for establishing therapeutic indications (3, 18-20). In addition, RHC remains the investigation of choice for excluding the post-capillary PH, perhaps the most important diagnostic challenge, by measuring the PWP.
Cardiac ultrasonography seems to be very useful in monitoring pulmonary hypertension patients and especially their cardiac function (21-23). Modern techniques allow a more extensive assessment of right ventricular function (24-26). Until the last decade, RV function had as gold standard for its evaluation cardiac MRI, which remains inaccessible and with high costs. The use of emerging ultrasonography techniques, such as TDI and lately Speckle tracking or 3D echocardiography, have introduced into clinical practice new parameters for the direct and indirect quantification of the right heart function, despite its complex anatomy (26,27). These are good news for patients with right heart pathology, especially PAH, due to the fact that therapeutic effects can be now monitored comprehensively noninvasively (27).
In our country the access to RHC is limited thus the importance of good case-selection for RHC indication. Also, the use of RHC for monitoring PAH therapy, as recommended by current guidelines, is limited to a few difficult cases. That is why, a complex echocardiographical approach of PAH and its impact on the right heart becomes mandatory. Our study had as main purpose to compare classical and modern TDI parameters in PAH patients to those of controls, in order to confirm their sensitivity for diagnosis and also, as an additional aim, we wanted to compare ultrasonographic pulmonary hemodynamic measurements to those obtained through RHC, in order to re-evaluate the usefulness of the latter in PAH diagnosis.
The Romanian National Program for the Treatment of PAH became available in 2008. Patients with idiopathic PAH, PAH associated with congenital heart diseases, connective tissue diseases, HIV and inoperable or residual chronic thromboembolic PH are treated with sildenafil or bosentan in monotherapy and severe patients receive double oral combination therapy. 5 centers for adult patients and 4 centers for pediatric patients are included in the PAH program with a total number of patients treated in 2012 of 254.
The treatment indication requires right heart catheterization with measurements of mPAP, PWP and cardiac output for all patients. Echocardiography remains the most utilized investigation for disease monitoring since RHC is limited to a few centers and cardiac MRI is practically inaccessible.
Our clinical findings, combining data from all subjects, confirmed the fact that ultrasonography is a very useful tool for the determination of systolic and mean pulmonary artery pressures as well as for the assessment of RV function, with values significantly modified in PAH patients compared to controls age and sex matched. Unfortunately, when compared to RHC, echocardiography had very different results concerning mPAP and sPAP measurements (variability of over 35%), with satisfactory measurement agreement only for CI (variability of 14%). Cardiac ultrasonography tends to underestimate PAP values. Also, RHC, through the detection of PVR and PWP offers a more complete hemodynamic profile of the PAH patient.
Clinical implications
The present study has been designed to provide additional information that may accelerate PAH diagnosis and may quantify PAH-targeted treatment effects on RV structure and function, without the use of costly or invasive methods. In the future we intend to provide data from follow-up (every six months), further investigating the association between echocardiography and RHC and, if possible providing data about RV function during therapy and about correlations between RV function and changes in functional class and exercise capacity.
For now, our study results confirm other data from literature, demonstrating the usefulness of echocardiographic tools – conventional and modern, such as TDI – for the non-invasive and rapid detection of PAH and right heart dysfunction (1,22-27). The limited correlation between echocardiographic and RHC measurements suggest once more that RHC is mandatory for a definitive diagnosis in PAH patients and that cardiac ultrasonography should remain a screening and monitoring method (3,16,20,21). Both methods may offer important prognostic parameters, for RHC - CI, PVR and RA pressure and for echocardiography - RA diameter, TAPSE, presence of pericardial effusion which together with exercise tolerance tests and NYHA class have a major impact on PAH treatment management. Follow up data are needed and other echocardiographic parameters, such as Speckle Tracking or 3D echocardiography should be evaluated extensively.
Study limitations
The limits of our study are given first of all by the used methods (conventional echocardiography, TDI, and RHC) - but measurements were made according to the current guidelines, the methods are validated and have a good intra - and inter - observer agreement. Also, we have a small number of patients (rare pathology, patients benefit from cardiac ultrasonography and RHC in various laboratories, enrolment includes only subjects with a standardized protocol), but this is a pilot study, with results already statistically significant, and enrolment on going. The patients have severe forms of PAH; therefore we couldn't evaluate the impact of echocardiography in the diagnosis of borderline pulmonary hypertension values. ❑
CONCLUSION
The present study confirms the utility of modern echocardiographic parameters for the non-invasive evaluation of the right heart in PAH. Regarding the correlations between echocardiography and RHC measurements, cardiac ultrasound is less reliable for assessing pressures in severe PAH but seems to offer correct data for cardiac index and PVR.
Nevertheless RHC offers a more accurate and complete hemodynamic profile of the PAH patient and remains mandatory for the final diagnosis.
We intend to further evaluate the association between echocardiography and RHC extending our study group also to "border-line" PAH and testing as well more cardiac ultrasound parameters.
CONFLICT OF INTEREST
none declared.
FINANCIAL SUPPORT
none declared.
References
- 1.Galie N. Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension. The Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), Endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J. 2009;30:2493–2537. doi: 10.1093/eurheartj/ehp297. [DOI] [PubMed] [Google Scholar]
- 2.Simonneau G, Robbins IM, Beghetti M, et al. Updated Clinical Classification of Pulmonary Hypertension. J Am Coll Cardiol. 2009;54:S43–S54. doi: 10.1016/j.jacc.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Fisher MR, Forfia PR, Chamera E, et al. Accuracy of Doppler Echocardiography in the Hemodynamic Assessment of Pulmonary Hypertension. Am J Resp Crit Care Med. 2009;179:615–621. doi: 10.1164/rccm.200811-1691OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho CY, Solomon SD. A Clinician's Guide to Tissue Doppler Imaging. Circulation. 2006;113:e396–e398. doi: 10.1161/CIRCULATIONAHA.105.579268. [DOI] [PubMed] [Google Scholar]
- 5.Gherghinescu CL. Editura Infomedica; Bucuresti: 2008. Elemente practice de ecocardiografie tisulara miocardica. [Google Scholar]
- 6.Sutherland GR, Steward MJ, Groundstroem KWE, et al. Color Doppler Myocardial Imaging: a New Technique for the Assessment of Myocardial Function. J Am Soc Echocardiogr. 1994;7:441–458. doi: 10.1016/s0894-7317(14)80001-1. [DOI] [PubMed] [Google Scholar]
- 7.Kjaergaard J, Sogaard P, Hassager C. Quantitative Echocardiographic Analysis of the Right Ventricle In Healthy Individuals. J Am Soc Echocardiogr. 2006;19:1365–372. doi: 10.1016/j.echo.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 8.Meluzin J, Spinarova L, Bakala J, et al. Pulsed Doppler Tissue Imaging of the Velocity of Tricuspid Annular Systolic Motion; A New, Rapid and Non-invasive Method of Evaluating Right Ventricular Systolic Function. Eur Heart J. 2001;22:340–348. doi: 10.1053/euhj.2000.2296. [DOI] [PubMed] [Google Scholar]
- 9.De Castro S, Cavarretta E, Milan A, et al. Usefulness of Tricuspid Annular Velocity in Identifying Global Rv Dysfunction in Patients with Primary Pulmonary Hypertension: A Comparison with 3D Echo Derived Right Ventricular Ejection Fraction. Echocardiography. 2008;25:289–293. doi: 10.1111/j.1540-8175.2007.00587.x. [DOI] [PubMed] [Google Scholar]
- 10.Miller D, Farah MG, Liner A, et al. The Relation Between Quantitative Right Ventricular Ejection Fraction and Indices of Tricuspid Annular Motion And Myocardial Performance. J Am Soc Echocardiogr. 2004;17:443–447. doi: 10.1016/j.echo.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 11.Saxena N, Rajagopalan N, Edelman K, et al. Tricuspid Annular Systolic Velocity: A Useful Measurement in Determining Right Ventricular Systolic Function Regardless of Pulmonary Artery Pressures. Echocardiography. 2006;23:750–5. doi: 10.1111/j.1540-8175.2006.00305.x. [DOI] [PubMed] [Google Scholar]
- 12.Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the Echocardiographic Assessment of The Right Heart in Adults: A Report From the American Society of Echocardiography. Endorsed by the European Association of Echocardiography, a Registered Branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 13.Ginghina C, Popescu BA, Jurcut R. Editura Medicala Antaeus; Bucuresti: 2005. Esentialul in ecocardiografie. [Google Scholar]
- 14.Davidson CJ, Bonow RO. In: Bonow RO, Mann DL, Zipes DP, Libby P, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; Philadelphia: 2011. chapter 20.Cardiac catheterization. [Google Scholar]
- 15.Kern M. In: Goldman L, Schafer AI, eds. Cecil Medicine. 24th ed. Saunders Elsevier; Philadelphia: 2011. chap 55.Catheterization and angiography. [Google Scholar]
- 16.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 17.Currie P, Seward J, Chan K, et al. Continuous Wave Doppler Determination of Right Ventricular Pressure: a Simultaneous Doppler-catheterization Study in 127 patients. J Am Coll Cardiol. 1986;6:750–756. doi: 10.1016/s0735-1097(85)80477-0. [DOI] [PubMed] [Google Scholar]
- 18.Selby VN, Scherzer R, Barnett CF, et al. Doppler Echocardiography Does Not Accurately Estimate Pulmonary Artery Systolic Pressure in HIV-Infected Patients. AIDS. 2012;26:1967–1969. doi: 10.1097/QAD.0b013e3283579653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Attaran RR, Ramaraj R, Sorrell VL, et al. Poor Correlation of Estimated Pulmonary Artery Systolic Pressure between Echocardiography and Right Heart Catheterization in Patients Awaiting Cardiac Transplantation: Results from The Clinical Arena. Transplant Proc. 2009;41:3827–3830. doi: 10.1016/j.transproceed.2009.06.201. [DOI] [PubMed] [Google Scholar]
- 20.Fitzgerald M, Fagan K, Herbert DE, et al. Misclassification of Pulmonary Hypertension in Adults with Sickle Hemoglobinopathies Using Doppler Echocardiography. South Med J. 2012;105:300–305. doi: 10.1097/SMJ.0b013e318256b55b. [DOI] [PubMed] [Google Scholar]
- 21.Hinderliter AL, Willis PW, Long WA, et al. Frequency and Severity of Tricuspid Regurgitation Determined By Doppler Echocardiography in Primary Pulmonary Hypertension. Am J Cardiol. 2003;91:1033–1037. doi: 10.1016/s0002-9149(03)00136-x. [DOI] [PubMed] [Google Scholar]
- 22.Eysmann SB, Palevsky HI, Reichek N, et al. Two-Dimensional Doppler-Echocardiographic and Cardiac Catheterization Correlates of Survival in Primary Pulmonary Hypertension. Circulation. 1989;80:353–360. doi: 10.1161/01.cir.80.2.353. [DOI] [PubMed] [Google Scholar]
- 23.Raymond RJ, Hinderliter AL, Willis PW, et al. Echocardiographic Predictors of Adverse Outcomes in Primary Pulmonary Hypertension. J Am Coll Cardiol. 2002;39:1214–1219. doi: 10.1016/s0735-1097(02)01744-8. [DOI] [PubMed] [Google Scholar]
- 24.Gupta H, Ghimire G, Naeije R. The Value of Tools to Assess Pulmonary Arterial Hypertension. Eur Respir Rev. 2011;20:222–235. doi: 10.1183/09059180.00006911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borges A, Knebel F, Eddicks S, et al. Right Ventricular Function Assessed by Two-Dimensional Strain and Tissue Doppler Echocardiography in Patients with Pulmonary Arterial Hypertension and Effect of Vasodilator Therapy. Am J Cardiol. 2006;98:530–534. doi: 10.1016/j.amjcard.2006.02.060. [DOI] [PubMed] [Google Scholar]
- 26.Sato T, Tsujino I, Ohira H, et al. Validation Study on the Accuracy of Echocardiographic Measurements of Right Ventricular Systolic Function in Pulmonary Hypertension. J Am Soc Echocardiogr. 2012;25:280–286. doi: 10.1016/j.echo.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 27.Rajaram S, Swift AJ, Capener D, et al. Comparison of the Diagnostic Utility of Cardiac Magnetic Resonance Imaging, Computed Tomography, and Echocardiography in Assessment of Suspected Pulmonary Arterial Hypertension in Patients With Connective Tissue Disease. J Rheumatol. 2012;39:1265–1274. doi: 10.3899/jrheum.110987. [DOI] [PubMed] [Google Scholar]