Abstract
Plague, initiated by Yersinia pestis infection, is a rapidly progressing disease with a high mortality rate if not quickly treated. The existence of antibiotic-resistant Y. pestis strains emphasizes the need for the development of novel countermeasures against plague. We previously reported the generation of a recombinant Y. pestis strain (Kim53ΔJ+P) that over-expresses Y. enterocolitica YopP. When this strain was administered subcutaneously to mice, it elicited a fast and effective protective immune response in models of bubonic, pneumonic and septicemic plague. In the present study, we further characterized the immune response induced by the Kim53ΔJ+P recombinant strain. Using a panel of mouse strains defective in specific immune functions, we observed the induction of a prompt protective innate immune response that was interferon-γ dependent. Moreover, inoculation of mice with Y. pestis Kim53ΔJ+P elicited a rapid protective response against secondary infection by other bacterial pathogens, including the enteropathogen Y. enterocolitica and the respiratory pathogen Francisella tularensis. Thus, the development of new therapies to enhance the innate immune response may provide an initial critical delay in disease progression following the exposure to highly virulent bacterial pathogens, extending the time window for successful treatment.
Introduction
Plague is a fatal disease that has caused millions of deaths in three world pandemics, and it remains a public health concern in some regions of the world [1] [2]. The disease, initiated by infection with the bacterial pathogen Yersinia pestis, is manifested in two main forms: pneumonic plague and bubonic plague. Primary pneumonic plague is the more fatal form of the disease, although it is less frequent in nature; it results from the inhalation of Y. pestis-containing droplets or aerosols. Bubonic plague develops following transmission of the pathogen from rodent reservoirs to humans by infected fleas [1]. Bacteria migrate through the cutaneous lymphatics to regional lymph nodes, where they multiply rapidly, followed by colonization of the spleen and liver and, finally, bacteremia and systemic dissemination to other tissues. Nonspecific symptoms start several days after infection and are followed by the development of swollen lymph nodes, which are termed buboes [3].
The medical treatment of plague should be initiated as early as possible to be effective. Antibiotic administration is the well-established first-line therapy against plague. However, the existence of antibiotic-resistant Y. pestis strains highlights the need for the development of new therapeutic tools [4]. Three main strategies have been adopted to achieve this goal: a. Search for anti-infective agents that can inhibit the activity of specific essential virulence systems or virulence factors. These agents include small molecules that target the type III secretion system (T3SS) apparatus and specific T3SS effectors [5]–[8]. b. Development of subunit vaccine candidates that extend the spectrum of the immune response generated by the F1/LcrV-based vaccines are also promising [9], [10]. c. Attenuated Y. pestis strains have been used in an effort to reveal potential targets for new therapeutic measures or to elucidate elements of the host immune system that are required for the generation of protective immunity against plague [11]–[16]
We have recently shown that a newly engineered strain of Y. pestis, Kim53ΔJ+P, is dramatically attenuated in a mouse model of bubonic plague (LD50>107 cfu), whereas its virulence is retained in mouse models of pneumonic and systemic plague [17]. This strain was generated by the over-expression of the Y. enterocolitica 0:8 T3SS effector YopP in the virulent yopJ-deleted Kimberley53 Y. pestis strain. YopP is homologous to the endogenous Y. pestis YopJ; both are known to inhibit the pro-inflammatory response in target host cells [18]–[20]. However, the recombinant YopP-expressing strain was found to induce cell death more effectively than the wild-type strain, most likely due to differences in YopJ/YopP translocation efficiency and allelic variations among the genes encoding these effectors [17], [21]. These results are similar to the findings of Brodsky et al., who demonstrated that the ectopic expression of YopP from Y. enterocolitica in Y. pseudotuberculosis led to attenuation following the oral infection of mice [22]. Interestingly, the Y. pestis Kim53ΔJ+P strain induced a rapid and effective systemic immune response that provided protection against subcutaneous (s.c.), intranasal (i.n.) and intravenous challenges with a fully virulent Y. pestis strain [17].
In the present study, we further characterized the rapid immune response induced by the Kim53ΔJ+P recombinant Y. pestis strain in an effort to uncover a potential new avenue for the development of protective measures against plague. Using immunodeficient mouse strains, we observed the induction of a prompt but transient protective innate immune response that was interferon-γ dependent. This response appeared to postpone disease progression and allow the development of adaptive immunity. Consistent with the relatively low specificity characterizing the rapid induction of the innate response, Kim53ΔJ+P-infected wild-type mice were also protected from a lethal challenge with the enteropathogen Y. enterocolitica and furthermore with a non-related respiratory pathogen, Francisella tularensis subspecies holarctica LVS.
Materials and Methods
Bacterial strains
The bacterial strains used in this study are listed in Table 1. Yersinia strains were routinely grown on brain heart infusion agar (BHIA, Difco) for 48 hours at 28°C. Ampicillin-resistant Y. pestis strains (Kim53pGFP, Kim53ΔJ+P) were grown on BHIA supplemented with 100 µg/ml ampicillin (Sigma, Israel). Live F. tularensis vaccine strain (ATCC 29684) stocks were plated on GCHI agar (GC Medium base [Difco Laboratories] supplemented with 1% hemoglobin and 1% Iso-VitaleX [BD, France]).
Table 1. Bacterial strains used in this study.
| Strains | Relevant characteristics | Reference |
| Yersinia pestis | ||
| Kimberley53 (Kim53) | Fully virulent Y. pestis strain (biovar Orientalis) | [11], [49] |
| Kim53pGFP | Kim53 carrying pGFPuv (Clontech) | [50] |
| Kim53ΔyopJ+pyopP | yopJ-deleted Kim53 over-expressing YopP of Y. enterocolitica WA 0:8 | [17] |
| Kim53ΔpCD1ΔpPCP1 | Spontaneously pPCP1 and pCD1-cured Kim53 | [17] |
| EV76 | pgm- (Girard's strain) | [49] |
| Yersinia enterocolitica | ||
| WA O:8 | Virulent Y. enterocolitica strain | [51] |
| Francisella tularensis | ||
| Holarctica LVS | Live vaccine strain (ATCC 29684) | [52] |
Ethics statement
This study was carried out in strict accordance with the recommendation in the Guide for the Care and Use of Laboratory Animals of the National Institute of Health. All animal experiments were performed in accordance with Israeli law and were approved by the Ethics Committee for animal experiments at the Israel Institute for Biological Research. (Permit Number: IACUC-IIBR M-32-2-09, IACUC-IIBR M-57-09, IACUC-IIBR M-58-11 and IACUC-IIBR M-62-11, IACUC-IIBR M-23-12, IACUC-IIBR M-26-13). During the experiments mice were monitored daily. Humane endpoints were used in our survival studies. Mice exhibiting loss of the righting reflex were euthanized by cervical dislocation. Analgesics were not used as they may have affected the experimental outcomes of the studies.
Animals
Five- to six-week-old female OF1 mice were purchased from Charles River Laboratories (IFFA CREDO S.A., France). Female C67BL/6J, µMT (B6.129S2-Ighmtm1Cgn/J), RAG1-/- (B6;129S7-Rag1tmMom/J), Kitwsh -/- (B6.CgKitWsh/HNih rLae BsmJ), IFNγ-/- (B6.129S7-Ifng tm1Ts/J), TCRbd-/- (B6.129P2-Tcrbtm1MomTcrdtm1Mom/J), and CD4-/- (B6.129S2-Cd4tm1Mak/J) mice (6 to 8 weeks old) were purchased from Jackson Laboratories (ME, USA) and randomly assigned into cages in groups of 6 animals. The mice were allowed free access to water and rodent diet (Harlan, Israel).
Animal studies
Yersinia strains were grown on BHIA plates (Difco) for 48 hours at 28°C. Several colonies were suspended in a sterile saline solution, diluted to the desired infectious dose and used for the challenge. Mice (6/group, unless stated otherwise), were injected with 0.1 ml of suspension containing the indicated amount of bacterial cells s.c. in their lower or upper back or intraperitoneally (i.p.). Bacterial cell counts were performed by serial dilution plating on BHIA. Unless otherwise indicated, the challenged animals were monitored daily for 35 days. The F. tularensis LVS strain was grown at 37°C to the mid-log phase (optical density of 0.1–0.2 at 660 nm) in TSBC (TSB [Difco] supplemented with 0.1% cysteine). The bacteria were washed and then re-suspended at the desired concentration in PBS. The bacteria were instilled i.n. (25 µl) to ketamine/xylazine-anesthetized mice or injected i.p. (0.5 ml). Experiments evaluating the ability of Y. pestis Kim53ΔJ+P to protect against Y. enterocolitica and F. tularensis were performed with OF1 outbred mice. Results from animal studies were obtained from at least two repeats.
Antibody titer analysis
Titers of anti-F. tularensis antibodies in serum samples were determined by ELISA in 96-well microtiter plates coated with 100 µl of 108 CFU/ml formalin-inactivated LVS. Antibody titers were expressed as reciprocal geometric mean titers (GMTs). The limit of detection for this assay was the reciprocal GMT value of 40.
Statistical analyses
GraphPad statistical software was used for the statistical analyses. Survival curves were compared using the log-rank test. In all analyses, P values equal to 0.05 served as the limit of significance.
Results and Discussion
Y. pestis over-expressing YopP activates a transient innate protective response
In mice, the s.c. administration of Kim53ΔJ+P induces a highly rapid systemic resistance against Y. pestis strains [17]. To characterize the contribution of innate immunity to the Kim53ΔJ+P-activated protective response, we used immunodeficient RAG1-/- mice, which lack the capacity to mount an adaptive immune response.
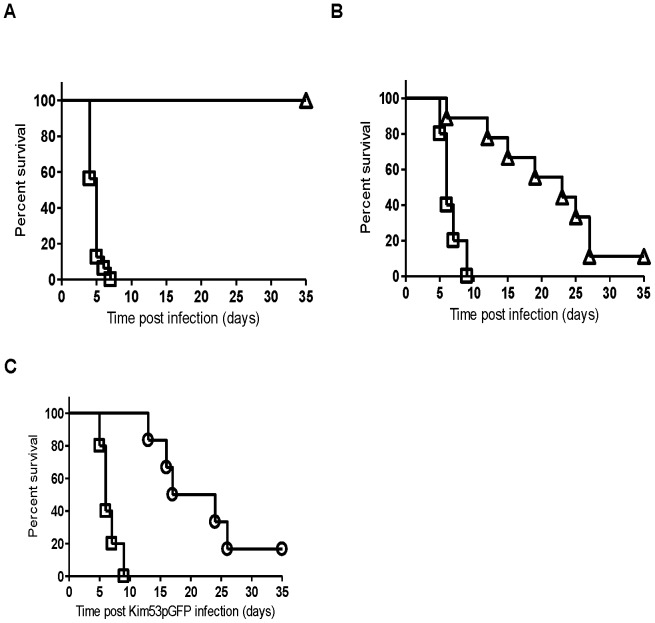
Parental C57BL/6J mice and their isogenic RAG1-/- mice were infected s.c. with Kim53ΔJ+P (104 cfu) or with the fully virulent Y. pestis strain Kim53pGFP (102 cfu) as a control. As expected, all wild-type C57BL/6J mice survived the Kim53ΔJ+P infection, whereas those infected with Kim53pGFP succumbed to the disease within seven days (Figure 1A). All immunodeficient RAG1-/- mice infected with Kim53pGFP succumbed to the disease within nine days, whereas high survival rates of 100-89% were observed for Kim53ΔJ+P-infected RAG1-/- mice during the initial nine days post-infection (Figure 1B). This result suggests that following the s.c. infection of RAG1-/- mice with Kim53ΔJ+P, a rapid protective innate immune response was evoked. However, the protective response was transient as the survival rate declined gradually to 14% by day 35 post-infection (mean time to death of 19 days in the Kim53ΔJ+P-infected mice compared with 6.6 days in the RAG1-/- mice infected with Kim53pGFP).
Figure 1. Transient protective immunity induced by Kim53ΔJ+P in immunodeficient RAG1-/- mice.
C57BL/6J mice (A) and their isogenic RAG1-/- mice (B) were infected s.c. with either 100 cfu of Kim53pGFP strain (square, five mice/group) or 1×104 cfu of Kim53ΔJ+P (triangle, nine mice/group). (C) RAG1-/- mice were either only infected s.c. with 100 cfu of Kim53pGFP (square) or infected with 1×104 cfu of Kim53ΔJ+P and challenged s.c. with Kim53pGFP three days later (circle, six mice/group).
In a subsequent cross-protection experiment, we assessed the ability of the innate immune response induced by Kim53ΔJ+P to provide rapid systemic protection against the challenge with a fully virulent Y. pestis strain inoculated s.c. at a different remote site. RAG1-/- mice were infected s.c. with 104 cfu of Kim53ΔJ+P and were challenged s.c. with a lethal dose of 102 cfu of the virulent Kim53pGFP strain three days later. Indeed, the Kim53ΔJ+P-induced protective response in the RAG1-/- mice was also effective in postponing the time to death following Kim53pGFP infection (Figure 1C). Importantly, the survival curve of co-infected mice was statistically indistinguishable from that of mice infected with Kim53ΔJ+P alone (P = 0.97 by the log-rank test, Figures 1B and 1C). These results indicate that a potent protective innate response can delay mouse mortality following infection with a highly virulent Y. pestis strain and even cure a small but distinct proportion of Y. pestis-infected mice. One may speculate that in wild-type mice this initial delay in disease progression provides the host with the time needed to develop an effective adaptive response against Y. pestis infection.
In an effort to characterize the distinct innate immune response induced rapidly following infection with Kim53ΔJ+P, we compared the levels of various classes of innate immune cells in the draining inguinal lymph node (ILN) and spleen at 24 and 48 hours post-infection with Kim53ΔJ+P and the virulent Kim53pGFP strain using flow cytometry. However, no significant differences in the levels of neutrophils, macrophages and dendritic cells were observed between mice infected with Kim53ΔJ+P and Kim53pGFP (data not shown). Mast cells (MCs) are another type of pro-inflammatory cell located throughout the skin, and they are considered to be among the first cells encountered by invading pathogens. MCs can induce rapid innate immune responses through the release of mediators [23]–[25]. Interestingly, histamine, which is one of these MC mediators, has been shown to be important for controlling Y. enterocolitica infection in mice [26]. These mast cell features led us to evaluate their involvement in the specific immunity induced by s.c. infection with Kim53ΔJ+P. However, the infection of MC-deficient mice (Kitwsh -/-) with 104 cfu of Kim53ΔJ+P via the s.c. route resulted in 100% survival. Furthermore, all Kim53ΔJ+P–infected Kitwsh -/- mice were protected against the challenge with a lethal dose of the virulent Kim53pGFP strain, which was administered s.c. three days later. These results indicate that MC activation is dispensable for the rapid induction of protective immunity by Kim53ΔJ+P.
Interferon-gamma is essential for the rapid induction of the Kim53ΔJ+P-mediated protective response
Interferon-gamma (IFNγ) is a pleiotropic cytokine that modulates the development of both the innate and adaptive immune responses [27]. Based on the key role that IFNγ plays in the immune system and its previously demonstrated role in the defense against Yersinia species [28]–[35], we evaluated the contribution of IFNγ to Kim53ΔJ+P-mediated immunity. All mice infected s.c. with 104 cfu of Kim53ΔJ+P succumbed to the disease within four days, which was similar to mice infected with the fully virulent Y. pestis strain (Figure 2). Restoration of the virulent phenotype was unique to Kim53ΔJ+P, as IFNγ-deficient mice infected with other attenuated Y. pestis strains, such as the vaccine strain EV76 or the pCD1−/pPCP1− derivative of Kim53, did not develop any disease symptoms (Figure 2). These observations clearly indicate that IFNγ is a key element of Kim53ΔJ+P-mediated immunity. Moreover, the rapid kinetics of disease progression and mortality of all Kim53ΔJ+P-infected IFNγ-/- mice within four days post-infection suggests that IFNγ is important for the induction of protective innate responses by Kim53ΔJ+P prior to the development of adaptive immunity.
Figure 2. IFNγ is essential for the Kim53ΔJ+P-mediated rapid protective response.
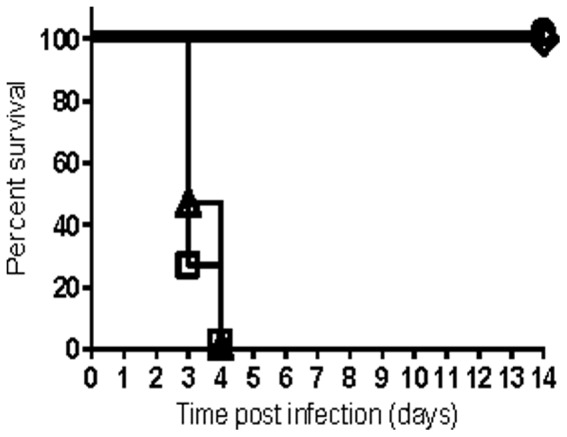
IFNγ-deficient mice (IFNγ-/-) were infected with 1×104 cfu of the following strains: Kim53ΔJ+P (triangle, twelve mice/group), Kim53pGFP (square, four mice/group), EV76 (circle, four mice/group) and Kim53ΔpCD1ΔpPCP1 (diamond, four mice/group).
Numerous studies have demonstrated that IFNγ can activate innate immune cells to exert a potent antimicrobial effect against intracellular pathogens, including Legionella pneumophila [36], F. tularensis [37], [38] and Mycobacterium tuberculosis [39]. However, in the case of Y. pestis, the ripA gene located within the pgm locus was shown to contribute to pathogen survival in macrophages activated by IFNγ in vitro following infection [40]. Recent in vivo studies have shown that neutralization of tumor necrosis factor alpha (TNFα) and IFNγ increases the lethality and bacterial burden of pgm −negative Y. pestis strain D27 in naïve mice infected i.n. [41]. In addition, these cytokines were found to play a role in the F1/LcrV-mediated protective response in various mouse models of plague and are proposed to be released from T cells primed following vaccination [31], [34], [41]. In the present study, we further extend the observations regarding the contribution of IFNγ to host defense against plague and demonstrate that this cytokine plays an essential role in the rapid development of protective immunity against s.c. infection with the pgm-positive Kim53ΔJ+P Y. pestis strain in naïve mice (Figure 2). The rapid time course of disease progression in Kim53ΔJ+P-infected IFNγ-/- mice suggests that adaptive cellular immunity, which typically requires a longer duration to develop, is not involved in the IFNγ-mediated early protective response against Kim53ΔJ+P. To further address this assumption, TCRbd-/- mice, which lack functional T cells, were infected s.c. with 104 cfu of Kim53ΔJ+P, and survival was monitored for 35 days. All TCRbd-/- mice survived for two weeks after s.c. infection with 104 cfu of Kim53ΔJ+P, suggesting that T cells are not required for the IFNγ-mediated early protective response against Kim53ΔJ+P (Figure 3A). However, by day 35 post-infection, 50% of the TCRbd-/--infected mice succumbed to the infection (Figure 3A), indicating that T cell activity is required to augment the early protective innate response against Kim53ΔJ+P and that this activity makes an important contribution to host defense against Kim53ΔJ+P infection. Notably, the ability of T cells to help B cells produce antibodies appears to play a minor role in the Kim53ΔJ+P-mediated defense response, as 90% of µMT B cell-deficient mice (Figure 3B) and all CD4 T cell-deficient mice survived for 35 days following s.c. infection with 104 cfu of Kim53ΔJ+P.
Figure 3. Contributions of T cells and B cells to the protective immunity induced by Kim53ΔJ+P.
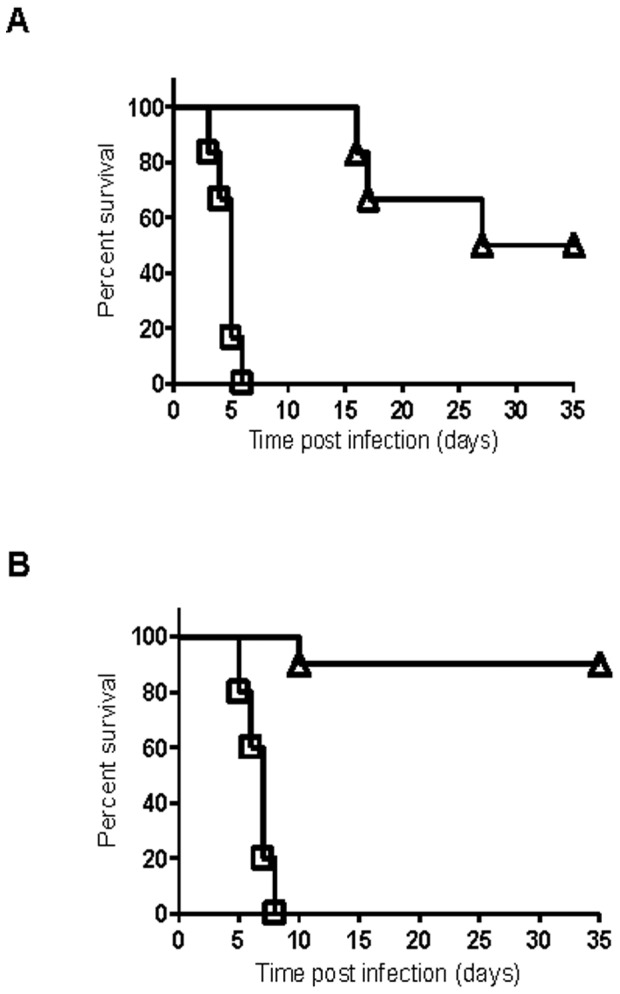
TCRbd-/- mice lacking functional T cells (A) and µMT mice lacking functional B cells (B) were infected s.c. with 104 cfu of Kim53ΔJ+P (triangle, ten mice/group) or 100 cfu of Kim53 (square, five mice/group). Survival was monitored for 35 days.
Currently, the exact mechanism by which IFNγ is involved in the Kim53ΔJ+P-mediated early innate immune response is unclear, and requires further studies. It should be noted, however, that the levels of IFNγ measured in the spleens of mice during the first 72 hours after infection with Kim53ΔJ+P were similar to their levels in mice infected with the virulent Kim53pGFP strain [17], suggesting that IFNγ might act locally following s.c. infection with Kim53ΔJ+P. Another possibility is that the expression of IFNγ is necessary, but not sufficient for Kim53ΔJ+P-mediated rapid protective response, and that the ability of the host to overcome the infection depends on another, yet unknown, factor(s).
Kim53ΔJ+P activates cross-protection against other bacterial pathogens
Non-specific protective responses against secondary infection with heterologous bacterial pathogens have previously been described in the pioneering studies of Mackaness and Henderson in the 1960s [42], [43], and in later publications by Killar [44] and Elkins [45]. Additional work by Elkin et al., also described rapid induction of non-specific, IFN-γ-mediated protection against F. tularensis infection using bacterial DNA [46]. The rapid activation of innate immunity by Kim53ΔJ+P raised the intriguing question of whether s.c. infection with Kim53ΔJ+P would also elicit heterologous protective immunity against other bacterial pathogens.
We first evaluated whether Kim53ΔJ+P-mediated cross-protection could be induced against another member of the Yersinia genus, the food-born pathogen Y. enterocolitica, which causes gastroenteritis [47]. Mice were infected s.c. with 105 cfu of Kim53ΔJ+P and were challenged i.p. three days later with a lethal dose of 2×103 cfu of Y. enterocolitica WA O:8 strain. Although all mice infected with 2×103 cfu of Y. enterocolitica alone succumbed to the disease within 11 days, a high survival rate of 80% was observed when the mice were challenged with Y. enterocolitica three days after infection with Kim53ΔJ+P (Figure 4A). This result indicated that the Kim53ΔJ+P-activated response can indeed provide rapid and effective cross-protection against another pathogen. However, because Y. enterocolitica and Y. pestis belong to the same genus and may share common antigenic determinants, we extended the evaluation of the protective immunity induced by Kim53ΔJ+P toward a non-related Gram-negative pathogen, F. tularensis, the etiologic agent of tularemia. Mice were infected i.p. and i.n. with a lethal dose of the F. tularensis subspecies holarctica LVS attenuated strain (500 cfu and 5,000 cfu, respectively). All infected mice exhibited disease symptoms (weight loss), and succumbed within ten days (Figures 4B and 4C). However, when the mice were first infected s.c. with Kim53ΔJ+P and challenged three days later with F. tularensis LVS, high survival rate of 70% was observed following the i.p. challenge and most notably, 63% survived the i.n. challenge (Figures 4B and 4C). In addition, substantial anti-LVS titers (103–105) were measured in the sera of mice surviving the infection with Kim53ΔJ+P and secondary challenge with F. tularensis LVS. These findings suggest that the initial non-specific immune response evoked by Y. pestis Kim53ΔJ+P delayed disease progression, allowing the development of a slower adaptive immune response against the F. tularensis LVS.
Figure 4. Kim53ΔJ+P induces cross-protection against Y. enterocolitica and F. tularensis.
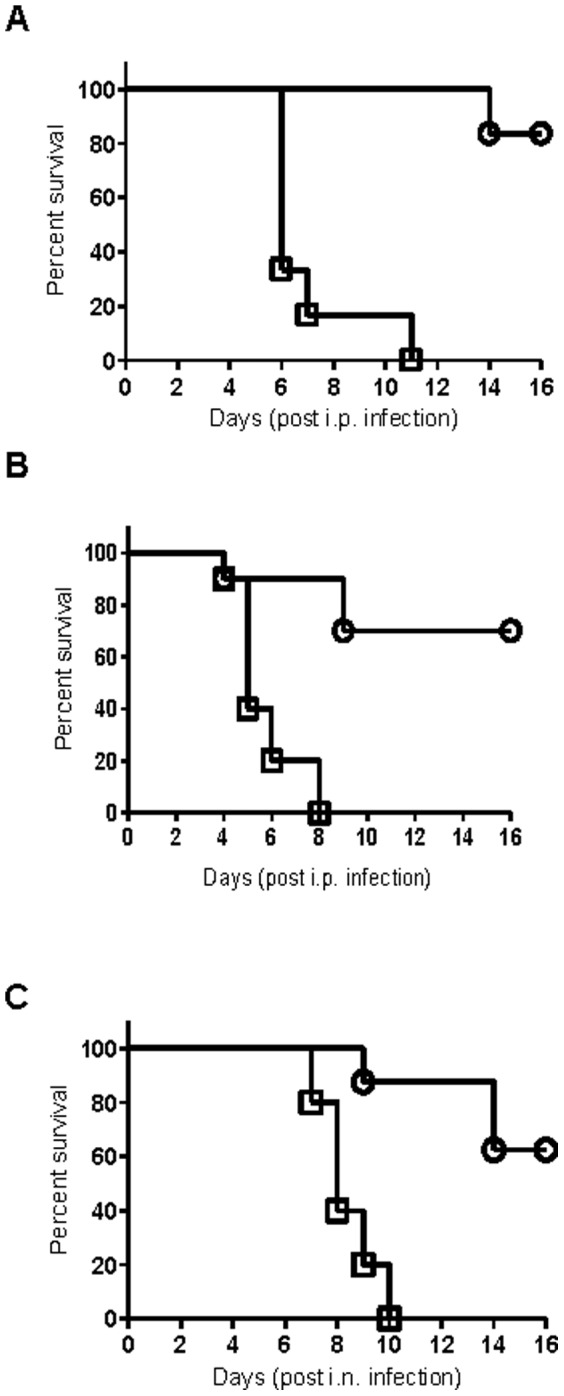
(A) Mice were either only infected i.p. with 1×103 cfu of Y. enterocolitica WA (square, six mice/group) or infected s.c. with 1×104 cfu of Kim53ΔJ+P and challenged i.p. with 1×103 cfu of Y. enterocolitica WA three days later (circle, six mice/group). (B) Mice were either only infected either i.p. with 500 cfu of F. tularensis LVS (square, ten mice/group) or infected s.c. with 1×104 cfu of Kim53ΔJ+P and challenged i.p. with 500 cfu of F. tularensis LVS three days later (circle, ten mice/group). (C) Mice were either only infected i.n. with 5000 cfu of F. tularensis LVS (square, eight mice/group) or infected s.c. with 1×104 cfu of Kim53ΔJ+P and challenged i.n. with 5000 cfu of F. tularensis LVS three days later (circle, ten mice/group). Mortality was monitored for 16 days post-challenge.
Notably, s.c. infection with the facultative intracellular pathogen Y. pestis Kim53ΔJ+P induced a prompt protective response against an unrelated intracellular pathogen that can replicate in the lung, spleen and liver. One can speculate that IFNγ, which was suggested in this study to be essential for the development of rapid protection against Kim53ΔJ+P, might also provide initial antigen-independent cross-protection against F. tularensis LVS due to its ability to activate macrophages. Indeed, it has been reported that rapid generation of a strong innate immune response mediated by macrophages and NK cells and dependent on IFNγ and TNFα, protects naïve mice against lethal infection with F. tularensis LVS [48].
Taken together, the present data indicate that the s.c. infection of mice with Kim53ΔJ+P activates an extremely rapid and potent protective response in which innate immunity appears to play a critical although transient role. IFNγ was found to be a key player in mediating this early, effectively induced protective response. Consistent with the relatively low specificity characterizing the rapid induction of the innate response, Kim53ΔJ+P-infected wild-type mice were also protected from a lethal challenge with other bacterial pathogens, including the enteropathogen Y. enterocolitica and the respiratory pathogen F. tularensis LVS. Thus, the development of new therapies to enhance the innate immune response may provide an initial critical delay in disease progression following the exposure to highly virulent bacterial pathogens such as Y. pestis, extending the time window for successful treatment.
Acknowledgments
We wish to thank Mrs. H. Cohen for her excellent technical assistance.
Funding Statement
This work was supported by the Israel Institute for Biological Research funds, grand number SB/5112-50. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Perry R, Fetherston J (1997) Yersinia pestis-etiologic agent of plague. Clin Microbiol Rev 10: 35–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kool JL (2005) Risk of person-to-person transmission of pneumonic plague. Clin Infect Dis 40: 1166–1172. [DOI] [PubMed] [Google Scholar]
- 3.Butler T (1983) Plague and other Yersian infections. New York: Plenum press.
- 4. Galimand M, Carniel E, Courvalin P (2006) Resistance of Yersinia pestis to antimicrobial agents. Antimicrob Agents Chemother 50: 3233–3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Swietnicki W, Carmany D, Retford M, Guelta M, Dorsey R, et al. (2011) Identification of small-molecule inhibitors of Yersinia pestis Type III secretion system YscN ATPase. PLoS One 6: e19716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pan N, Lee C, Goguen J (2007) High throughput screening for small-molecule inhibitors of type III secretion in Yersinia pestis . Adv Exp Med Biol 603: 367–375. [DOI] [PubMed] [Google Scholar]
- 7. Garrity-Ryan LK, Kim OK, Balada-Llasat JM, Bartlett VJ, Verma AK, et al. (2010) Small molecule inhibitors of LcrF, a Yersinia pseudotuberculosis transcription factor, attenuate virulence and limit infection in a murine pneumonia model. Infect Immun 78: 4683–4690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eriksson J, Grundstrom C, Sauer-Eriksson AE, Sauer UH, Wolf-Watz H, et al. (2012) Small molecule screening for inhibitors of the YopH phosphatase of Yersinia pseudotuberculosis . Adv Exp Med Biol 954: 357–363. [DOI] [PubMed] [Google Scholar]
- 9. Lin JS, Szaba FM, Kummer LW, Chromy BA, Smiley ST (2011) Yersinia pestis YopE contains a dominant CD8 T cell epitope that confers protection in a mouse model of pneumonic plague. J Immunol 187: 897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williamson ED, Oyston PC (2013) Protecting against plague: towards a next-generation vaccine. Clin Exp Immunol 172: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tidhar A, Flashner Y, Cohen S, Levi Y, Zauberman A, et al. (2009) The NlpD lipoprotein is a novel Yersinia pestis virulence factor essential for the development of plague. PLoS One 4: e7023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smiley ST (2008) Current challenges in the development of vaccines for pneumonic plague. Expert Rev Vaccines 7: 209–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Feodorova VA, Motin VL (2012) Plague vaccines: current developments and future perspectives. Emerging Microbes & Infections 1: e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rosenzweig JA, Jejelowo O, Sha J, Erova TE, Brackman SM, et al. (2011) Progress on plague vaccine development. Appl Microbiol Biotechnol 91: 265–286. [DOI] [PubMed] [Google Scholar]
- 15. Dentovskaya SV, Kopylov PK, Ivanov SA, Ageev, Anisimov AP (2013) Molecular Bases of Vaccine Prevention of Plague. Molecular Genetics, Microbiology and Virology 28: 87–98. [Google Scholar]
- 16. Wang X, Zhang X, Zhou D, Yang R (2013) Live-attenuated Yersinia pestis vaccines. Expert Rev Vaccines 12: 677–686. [DOI] [PubMed] [Google Scholar]
- 17. Zauberman A, Tidhar A, Levy Y, Bar-Haim E, Halperin G, et al. (2009) Yersinia pestis endowed with increased cytotoxicity is avirulent in a bubonic plague model and induces rapid protection against pneumonic plague. PLoS One 4: e5938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Monack D, Mecsas J, Ghori N, Falkow S (1997) Yersinia signals macrophages to undergo apoptosis and YopJ is necessary for this cell death. Proc Natl Acad Sci U S A 94: 10385–10390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ruckdeschel K, Machold J, Roggenkamp A, Schubert S, Pierre J, et al. (1997) Yersinia enterocolitica promotes deactivation of macrophage mitogen-activated protein kinases extracellular signal-regulated kinase-1/2, p38, and c-Jun NH2-terminal kinase. Correlation with its inhibitory effect on tumor necrosis factor-alpha production. J Biol Chem 272: 15920–15927. [DOI] [PubMed] [Google Scholar]
- 20. Zhang Y, Ting AT, Marcu KB, Bliska JB (2005) Inhibition of MAPK and NF-kappaB pathways is necessary for rapid apoptosis in macrophages infected with Yersinia. J Immunol 174: 7939–7949. [DOI] [PubMed] [Google Scholar]
- 21. Zauberman A, Cohen S, Mamroud E, Flashner Y, Tidhar A, et al. (2006) Interaction of Yersinia pestis with macrophages: limitations in YopJ-dependent apoptosis. Infect Immun 74: 3239–3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brodsky IE, Medzhitov R (2008) Reduced secretion of YopJ by Yersinia limits in vivo cell death but enhances bacterial virulence. PLoS Pathog 4: e1000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Urb M, Sheppard DC (2012) The role of mast cells in the defence against pathogens. PLoS Pathog 8: e1002619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dawicki W, Marshall JS (2007) New and emerging roles for mast cells in host defence. Curr Opin Immunol 19: 31–38. [DOI] [PubMed] [Google Scholar]
- 25. Abraham SN, St John AL (2010) Mast cell-orchestrated immunity to pathogens. Nat Rev Immunol 10: 440–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Handley SA, Dube PH, Miller VL (2006) Histamine signaling through the H(2) receptor in the Peyer's patch is important for controlling Yersinia enterocolitica infection. Proc Natl Acad Sci U S A 103: 9268–9273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schroder K, Hertzog PJ, Ravasi T, Hume DA (2004) Interferon-gamma: an overview of signals, mechanisms and functions. J Leukoc Biol 75: 163–189. [DOI] [PubMed] [Google Scholar]
- 28. Autenrieth IB, Heesemann J (1992) In vivo neutralization of tumor necrosis factor-alpha and interferon- gamma abrogates resistance to Yersinia enterocolitica infection in mice. Med Microbiol Immunol 181: 333–338. [DOI] [PubMed] [Google Scholar]
- 29. Nakajima R, Brubaker RR (1993) Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect Immun 61: 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bohn E, Heesemann J, Ehlers S, Autenrieth IB (1994) Early gamma interferon mRNA expression is associated with resistance of mice against Yersinia enterocolitica . Infect Immun 62: 3027–3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Elvin SJ, Williamson ED (2004) Stat 4 but not Stat 6 mediated immune mechanisms are essential in protection against plague. Microb Pathog 37: 177–184. [DOI] [PubMed] [Google Scholar]
- 32. Pujol C, Bliska JB (2005) Turning Yersinia pathogenesis outside in: subversion of macrophage function by intracellular yersiniae. Clin Immunol 114: 216–226. [DOI] [PubMed] [Google Scholar]
- 33. Parent MA, Wilhelm LB, Kummer LW, Szaba FM, Mullarky IK, et al. (2006) Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect Immun 74: 3381–3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lin JS, Park S, Adamovicz JJ, Hill J, Bliska JB, et al. (2010) TNFalpha and IFNgamma contribute to F1/LcrV-targeted immune defense in mouse models of fully virulent pneumonic plague. Vaccine 29: 357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang Y, Bliska JB (2010) YopJ-promoted cytotoxicity and systemic colonization are associated with high levels of murine interleukin-18, gamma interferon, and neutrophils in a live vaccine model of Yersinia pseudotuberculosis infection. Infect Immun 78: 2329–2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bhardwaj N, Nash TW, Horwitz MA (1986) Interferon-gamma-activated human monocytes inhibit the intracellular multiplication of Legionella pneumophila . J Immunol 137: 2662–2669. [PubMed] [Google Scholar]
- 37. Lindgren H, Stenman L, Tarnvik A, Sjostedt A (2005) The contribution of reactive nitrogen and oxygen species to the killing of Francisella tularensis LVS by murine macrophages. Microbes Infect 7: 467–475. [DOI] [PubMed] [Google Scholar]
- 38. Edwards JA, Rockx-Brouwer D, Nair V, Celli J (2010) Restricted cytosolic growth of Francisella tularensis subsp. tularensis by IFN-gamma activation of macrophages. Microbiology 156: 327–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Herbst S, Schaible UE, Schneider BE (2011) Interferon gamma activated macrophages kill mycobacteria by nitric oxide induced apoptosis. PLoS One 6: e19105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pujol C, Grabenstein JP, Perry RD, Bliska JB (2005) Replication of Yersinia pestis in interferon gamma-activated macrophages requires ripA, a gene encoded in the pigmentation locus. Proc Natl Acad Sci U S A 102: 12909–12914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kummer LW, Szaba FM, Parent MA, Adamovicz JJ, Hill J, et al. (2008) Antibodies and cytokines independently protect against pneumonic plague. Vaccine 26: 6901–6907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mackaness GB (1964) The Immunological Basis of Acquired Cellular Resistance. J Exp Med 120: 105–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Henderson DW (1964) Mixed populations in vivo and in vitro. Symp Soc Gen Microbiol 14: 241–256. [Google Scholar]
- 44. Killar LM, Eisenstein TK (1985) Immunity to Salmonella typhimurium infection in C3H/HeJ and C3H/HeNCrlBR mice: studies with an aromatic-dependent live S. typhimurium strain as a vaccine. Infect Immun 47: 605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Elkins KL, MacIntyre AT, Rhinehart-Jones TR (1998) Nonspecific early protective immunity in Francisella and Listeria infections can be dependent on lymphocytes. Infect Immun 66: 3467–3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Elkins KL, Rhinehart-Jones TR, Stibitz S, Conover JS, Klinman DM (1999) Bacterial DNA containing CpG motifs stimulates lymphocyte-dependent protection of mice against lethal infection with intracellular bacteria. J Immunol 162: 2291–2298. [PubMed] [Google Scholar]
- 47. Brubaker RR (1991) Factors promoting acute and chronic diseases caused by Yersiniae. Clin Microbiol Rev 4: 309–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Elkins KL, Rhinehart-Jones TR, Culkin SJ, Yee D, Winegar RK (1996) Minimal requirements for murine resistance to infection with Francisella tularensis LVS. Infect Immun 64: 3288–3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ben-Gurion R, Shafferman A (1981) Essential virulence determinants of different Yersinia species are carried on a common plasmid. Plasmid 5: 183–187. [DOI] [PubMed] [Google Scholar]
- 50. Ber R, Mamroud E, Aftalion M, Tidhar A, Gur D, et al. (2003) Development of an improved selective agar medium for isolation of Yersinia pestis . Appl Environ Microbiol 69: 5787–5792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mamroud E, Flashner Y, Tidhar A, Ber R, Gur D, et al. (2003) Evaluation of protective immunity induced by Yersinia enterocolitica type-III secretion system mutants. Adv Exp Med Biol 529: 425–430. [DOI] [PubMed] [Google Scholar]
- 52. Bar-Haim E, Gat O, Markel G, Cohen H, Shafferman A, et al. (2008) Interrelationship between dendritic cell trafficking and Francisella tularensis dissemination following airway infection. PLoS Pathog 4: e1000211. [DOI] [PMC free article] [PubMed] [Google Scholar]