Abstract
Social and demographic trends are placing an increasing number of adults at risk for loneliness, an established risk factor for physical and mental illness. The growing costs of loneliness have led to a number of loneliness reduction interventions. Qualitative reviews have identified four primary intervention strategies: 1) improving social skills, 2) enhancing social support, 3) increasing opportunities for social contact, and 4) addressing maladaptive social cognition. An integrative meta-analysis of loneliness reduction interventions was conducted to quantify the effects of each strategy and to examine the potential role of moderator variables. Results revealed that single group pre-post and non-randomized comparison studies yielded larger mean effect sizes relative to randomized comparison studies. Among studies that used the latter design, the most successful interventions addressed maladaptive social cognition. This is consistent with current theories regarding loneliness and its etiology. Theoretical and methodological issues associated with designing new loneliness reduction interventions are discussed.
The formation of meaningful social connections is an integral part of human nature (Baumeister & Leary, 1995; Cacioppo & Patrick, 2008). Some individuals have difficulty forming meaningful social connections whereas others form such social connections but lose them through separation, widowhood, or other vagaries of life. Individuals without meaningful social connections are at risk for loneliness, an aversive experience that all humans experience at one time or another. Although the health consequences of persistent loneliness are on par with that of many psychiatric illnesses, our understanding of the origins and treatment of loneliness is still limited (O’Luanaigh & Lawlor, 2008). To properly treat loneliness, a better understanding of the nature and mechanisms underlying loneliness is needed. Therefore, the goals of this paper are to review the definitions, prevalence, health effects, and current theories regarding loneliness, to describe the relationship between these theories and previous studies of loneliness reduction strategies, and to use meta-analytic techniques to quantify the loneliness-reducing effects of studies which meet our analysis criteria.
Definitions
Loneliness is typically defined as the discrepancy between a person’s desired and actual social relationships (Russell, Peplau, & Cutrona, 1980). Although sometimes considered synonymous with social isolation, loneliness and social isolation are related but distinct concepts. The latter reflects an objective measure of social interactions and relationships, whereas loneliness reflects perceived social isolation or outcast. Accordingly, loneliness is more closely associated with the quality than the number of relationships (Peplau & Perlman, 1982; Wheeler, Reis, & Nezlek, 1983). The importance of relationship quality takes origin in the fundamentally social nature of the human species. Both phylogenetically and ontogenetically, humans require not simply the presence of others but the presence of others who value them, whom they can trust, and with whom they can communicate, plan, and work together to survive, prosper, and care for our offspring sufficiently long that they too reproduce (Cacioppo & Patrick, 2008). As a result, an individual may be lonely in a crowd or socially contented while alone.
Loneliness was traditionally thought to be a gnawing sensation or chronic distress without redeeming features (Weiss, 1973), but more recently loneliness has been conceptualized as a biological construct, a state that has evolved as a signal to change behavior – very much like hunger, thirst, or physical pain – that serves to help one avoid damage and promote the transmission of genes to the gene pool (Cacioppo et al., 2006). That is, loneliness has been posited to be an aversive signal that motivates us to become sensitive to potential social threats and to renew the connections needed to survive and prosper. Like hunger, thirst, and pain, loneliness is typically mild and transient because it contributes to the maintenance or repair of meaningful social connections – as occurs when a child is reunited with his or her parent following separation or a spouse returns home following a trip. When meaningful social connections are perceived as severed or unavailable, however, loneliness can produce deleterious effects on cognition and behavior (Cacioppo & Hawkley, 2005) that, in turn, increase the likelihood that loneliness becomes chronic (Cacioppo & Hawkley, 2009; Young, 1982). Interventions to reduce loneliness have been developed because the chronic form of loneliness is highly aversive (Peplau & Perlman, 1982; Weiss, 1973), is a significant risk factor for mental and physical health problems (Danese et al., 2009; Hawkley & Cacioppo, 2007), and adversely affects others around them (Berscheid & Reis, 1998; Cacioppo, Fowler, & Christakis, 2009).
Weiss distinguished between emotional and social loneliness on theoretical grounds (Weiss, 1973). Various factor analytic studies have provided some evidence that the experience of loneliness can be partitioned into separable dimensions (Hawkley, Browne, & Cacioppo, 2005; Knight, Chisholm, Nigel, & Godfrey, 1988; McWhirter, 1990a), but these factors have also been found to be highly correlated and their antecedents and consequences have been found to be sufficiently overlapping that loneliness is generally conceptualized and measured as a unidimensional construct (Hawkley, Browne, & Cacioppo, 2005; Russell, 1996; Russell, Peplau, & Cutrona, 1980).
Prevalence
Research reveals a significant prevalence of loneliness among both children and adults. In a study of kindergarteners and first graders, 12% reported feeling lonely at school (Cassidy & Asher, 1992). Among third through sixth-grade children, 8.4% scored in the lonely range using the Asher et al. Loneliness Scale (Asher, Hymel, & Renshaw, 1984; Asher & Wheeler, 1985). Among middle-aged and older adults, from five to seven percent report feeling intense or persistent loneliness (Steffick, 2000; Victor, Scambler, Bowling, & Bondt, 2005) and up to 32% of adults over age 55 report feeling lonely at any given time (De Jong Gierveld & van Tilburg, 1999). According to the 2002 Health and Retirement Survey, 19.3% of U.S. adults over age 65 reported feeling lonely for much of the previous week (Theeke, 2009). Several factors suggest the prevalence of loneliness could increase in the coming decades. One is the aging of the U.S. population. In 1900, 4.1% of Americans were 65 years or older. By 2006, that percentage had increased to 12.4%, representing 37.3 million Americans (Administration on Aging, 2008). Older age is associated with disability-related obstacles to social interaction as well as with longer periods of time living as widows or widowers. Moreover, delayed marriage (Goldstein & Kenney, 2001), increased dual career families (Schneider & Waite, 2005), increased single-residence households (U.S. Bureau of Labor Statistics, 2003), and reduced fertility rates (Taylor et al., 2010) may also contribute to an increased prevalence of loneliness and its associated health effects.
Health Effects
The associations between loneliness and physical and mental health indicate that loneliness influences virtually every aspect of life in our social species. For example, loneliness not only involves painful feelings of isolation, disconnectedness from others and not belonging (Hawkley, Browne, & Cacioppo, 2005) but it is also a risk factor for myriad health conditions, including increased vascular resistance in young adults (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley, Burleson, Berntson, & Cacioppo, 2003), elevated systolic blood pressure in older adults (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley, Masi, Berry, & Cacioppo, 2006; Hawkley, Thisted, Masi, & Cacioppo, 2010), less restorative sleep (Cacioppo, Hawkley, Berntson et al., 2002; Hawkley, Preacher, & Cacioppo, 2010), increased hypothalamic pituitary adrenocortical activity (Adam, Hawkley, Kudielka, & Cacioppo, 2006), diminished immunity (Kiecolt-Glaser et al., 1984; Pressman et al., 2005), under-expression of genes bearing anti-inflammatory glucocorticoid response elements (Cole et al., 2007), and abnormal ratios of circulating white blood cells (e.g., neutrophils, lymphocytes, and monocytes) (Cole, 2008). In addition, longitudinal analysis reveals that adults who were socially isolated as children are more likely to have risk factors for cardiovascular disease, including overweight, high blood pressure, high total cholesterol, low high-density lipoprotein cholesterol, high glycated hemoglobin, and low maximum oxygen consumption (Caspi, Harrington, Moffitt, Milne, & Poulton, 2006), as well as elevated high sensitivity C-reactive protein (hsCRP) (Danese et al., 2009).
Compared to non-lonely individuals, lonely people are also more likely to suffer from cognitive decline (Tilvis et al., 2004) and progression of Alzheimer’s disease (Wilson et al., 2007). Animal studies are beginning to shed light on the mechanism by which these effects may occur. Among mice, social isolation reduces central anti-inflammatory responses and increases infarct size following induction of stroke (Karelina et al., 2009). In addition, socially isolated animals demonstrate less dendritic arborization in the hippocampus and prefrontal cortex (Silva-Gomez, Rojas, Juarez, & Flores, 2003) as well as decreased production of brain-derived neurotropic factors (Barrientos et al., 2003). Whereas it is unknown whether similar effects occur in humans, experimental manipulation that leads people to believe they face a future of social isolation has been shown to impair executive functioning. Compared to controls, the “future alone” group performed similarly on a rote memorization task but consumed more delicious but unhealthy foods (Baumeister, DeWall, Ciarocco, & Twenge, 2005) and were more aggressive toward others (Twenge, Baumeister, Tice, & Stucke, 2001). Therefore, perceived future isolation did not reduce routine mental ability but rather impaired higher order executive functioning related to food consumption and social interaction.
Loneliness impairs executive functioning in part because it triggers implicit hypervigilance for social threats (Cacioppo & Hawkley, 2009). Heightened sensitivity to social threats results in biases in attention and cognition toward negative aspects of the social context. These social cognitions subtly influence behaviors, social interactions, and affect in a confirmatory fashion that exacerbates feelings of sadness and loneliness. Maladaptive social cognitions have consequences for mental health and well-being. Loneliness has been shown to predict depressive symptoms (Cacioppo, Hawkley, & Thisted, in press; Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006) and suicidal ideation and behavior (Rudatsikira, Muula, Siziya, & Twa-Twa, 2007). The impact of loneliness on such diverse aspects of physical and mental health provides justification for interventions to mitigate this experience.
Theories of Loneliness
As described above, loneliness can be a fleeting, unpleasant mood for some individuals or a persistent, aversive experience for others. Most people are capable of feeling loneliness acutely, but some are unable to escape the grip of loneliness. Research indicates that loneliness is approximately 50% heritable and 50% environmental (Boomsma, Willemsen, Dolan, Hawkley, & Cacioppo, 2005; McGuire & Clifford, 2000). For a species to survive, not only must one generation procreate, but the offspring of that generation must procreate as well. Human offspring have the longest period of dependency of any species and rely upon their parents to feed and protect them for many years. During hunter-gatherer times, survival of children to reproductive age would have depended on parents sharing food and resources with their children even if at cost to themselves. Parents who felt no ‘pangs’ of loneliness when parted from their children would have been less likely to maintain nurturing and protective parental connections compared to parents who experienced distress when separated from the family and tribe. Thus, whereas loneliness is unpleasant for the individual, it may be essential for species survival (Cacioppo et al., 2006). Because infant attachment is not predictive of adult attachment and adult attachment can change, childhood attachment appears not to be a major determinant of loneliness in most adults (Cacioppo & Patrick, 2008; Shaver, Furman, & Buhrmester, 1985).
Of course, having a gene or genes for loneliness does not mean an individual will be lonely. What appears to be inherited is the level of distress aroused by social disconnection. For individuals of all ages, loneliness may arise upon moving to a new city, losing a friend, or losing a loved one. Analysis of data from a population-based, racially diverse sample of men and women aged 50 through 68 revealed several factors were positively associated with loneliness. These included number of physical symptoms, chronic stress from employment, and chronic stress from social life and recreation. Factors negatively associated with loneliness included social network size, satisfaction with social network, and having a spousal confidant (Hawkley et al., 2008). These results suggest that the success of interventions to reduce loneliness may hinge upon the degree to which one’s social environment and social interactions are improved.
Research over the past several decades has shaped our understanding of the nature of loneliness. Early studies focused on individual differences between lonely and non-lonely people. This research demonstrated that compared to the non-lonely, lonely individuals approach social encounters with greater cynicism and interpersonal mistrust (Brennan & Auslander, 1979; Jones, Freemon, & Goswick, 1981; Moore & Sermat, 1974), rate others and themselves more negatively, and are more likely to expect others to reject them (Jones, 1982). In addition, lonely people have lower feelings of self-worth (Peplau, Miceli, & Morasch, 1982), tend to blame themselves for social failures (Anderson, Horowitz, & French, 1983), are more self-consciousness in social situations (Cheek & Busch, 1981), and adopt behaviors that increase, rather than decrease, their likelihood of rejection (Horowitz, 1983). This “individual differences” model of loneliness has influenced loneliness reduction interventions to date. Specifically, these interventions have attempted to correct deficits in social skills, social support, opportunities for social interaction, and/or maladaptive social cognition.
More recent research suggests that loneliness is not an immutable trait but rather can be exacerbated or ameliorated by social interactions. In an illustrative study, hypnosis was successfully used to induce participants to feel high and low levels of loneliness (Cacioppo et al., 2006). Increasing feelings of loneliness also increased feelings of shyness, anxiety and anger, and decreased feelings of social skills, optimism, self-esteem, and social support, suggesting that loneliness is syndrome-like in carrying with it a range of attributions, expectations, and perceptions that reinforce feelings of loneliness (Cacioppo et al., 2006). Conversely, these findings suggest that interventions that enhance a feeling of social connectedness can alter self-and other-perceptions along dimensions that have the potential to improve the quality of social interactions and relationships and keep loneliness at bay.
To examine the role of the social context in loneliness, investigators studied loneliness in the Framingham Heart Study (Cacioppo, Fowler, & Christakis, 2009). Using social network analysis and self-reported data from over 6,000 participants between 1983 and 2001, the authors identified several unique phenomena. Specifically, they found that lonely people tend to be linked to other people who are lonely, an effect that is stronger for geographically proximal friends but extends to three degrees of separation. In addition, non-lonely individuals who are around lonely individuals tend to grow lonelier over time. This suggests that loneliness can be induced and operates not unlike a biological contagion. Finally, analysis revealed that lonely individuals were consistently moved to the periphery of social networks, as if they had been metaphorically pushed there by others in the network. From an evolutionary perspective, such marginalization may protect the structural integrity of the network. These findings also go beyond the individual differences model of loneliness and demonstrate the power not only of social networks but the ability of people who become lonely to have a negative effect on non-lonely people.
A mechanism for the contagion of loneliness may lie in the reciprocal effects of social interaction quality and affect. In an experience sampling study, 134 undergraduates were queried regarding their psychosocial and behavioral states at nine random times during the day on seven consecutive days (Hawkley, Preacher, & Cacioppo, 2007). Information regarding the positivity or negativity of their affect and their interactions (if they were interacting with someone at the time their programmable watched beeped) was collected via diary entries. Of primary interest was the ability of loneliness to predict variability in affect and interaction quality and their interrelationship. Using multilevel modeling, the authors found that loneliness was associated with decreased positivity and increased negativity in affect and interaction quality across all measurement occasions. In longitudinal analysis, positive and negative interaction quality predicted subsequent positive and negative affect, and in a reciprocal causal fashion, positive and negative affect predicted subsequent interaction quality. Moreover, the influence of interaction negativity on negative affect persisted over a longer duration than the influence of interaction positivity on positive affect. In addition, negative affect influenced subsequent interaction positivity and negativity, whereas positive affect influenced only subsequent interaction positivity. Finally, loneliness was characterized by greater negative affect and more negative interactions. Together, this pattern of results suggests that lonely individuals not only communicate negativity to others but also elicit it from others and transmit it through others. This perpetuates a cycle of negative interactions and affect in the lonely individual and also transmits negativity to others to affect their interactions as well. These results may explain the mechanism by which lonely individuals increase feelings of loneliness among those with whom they interact. The authors concluded that interventions that reduce perceptions of negativity in interactions or affect have the potential to break the cycle of negativity that people experience when lonely.
Taken together, these studies suggest that when individuals feel lonely, they think and act differently than when they do not feel lonely. Accordingly, their perceptions of the social environment, their social cognitions, and their interpersonal actions have all been targeted in interventions to reduce loneliness.
Previous Reviews of Loneliness Interventions
Since 1984, six papers have reviewed the literature regarding strategies to reduce loneliness, social isolation, or both. Of these reviews, all are qualitative, rather than quantitative, and most explicitly or implicitly discuss four primary strategies of loneliness reduction interventions: 1) improving social skills, 2) enhancing social support, 3) increasing opportunities for social interaction, and 4) addressing maladaptive social cognition. Because the number of friends or social interactions is not as predictive or loneliness as the quality of their relationships, increasing opportunities for social interaction and enhancing social support may address social isolation more than loneliness. In contrast, improving social skills and addressing maladaptive social cognition focus on quality of social interaction and therefore address loneliness more directly. All of the reviews identified both successful and unsuccessful loneliness reduction strategies, and five of the six reviews concluded that loneliness can be mitigated with specific interventions. However, all of the reviews concluded that questions remain regarding the efficacy of interventions and that more rigorous research is needed in this area.
The earliest review cited over 40 loneliness reduction interventions dating back to the 1930’s (Rook, 1984). Most of these interventions fell into the four categories described above. Depending upon the study, interventions to improve social skills emphasized one or several of the following: conversational skills, speaking on the telephone, giving and receiving compliments, handling periods of silence, enhancing physical attractiveness, nonverbal communication methods, and approaches to physical intimacy. In one study, a social skills intervention among lonely college students was associated with decreased loneliness, self-consciousness, and shyness compared to two control groups (Jones, Hobbs, & Hockenbury, 1982). Among interventions that enhanced social support, professionally-initiated interventions for the bereaved (Vachon, Lyall, Rogers, Freedman-Letofsky, & Freeman, 1980), for the elderly whose personal networks had been disrupted by relocation (Kowalski, 1981), and for children whose parents had divorced (Wallerstein & Kelly, 1977) all demonstrated loneliness reductions. Increasing opportunities for social interaction also reduced loneliness in some studies. An example is a blood pressure evaluation program conducted in the lobbies of single-room occupancy hotels that housed older individuals. Although the residents tended to stay in their rooms due to physical disability and fear of crime, the program increased social interaction in the lobbies, and over time, helped participants identify shared interests (Pilisuk & Minkler, 1980). Another example involved isolated seniors working together to collect and distribute food for the needy. As the study progressed, the seniors formed informal support networks (Pilisuk & Minkler, 1980). Finally, programs that focused on maladaptive social cognition through cognitive behavioral therapy (CBT) appeared somewhat successful in reducing loneliness (Young, 1982). The cornerstone of this intervention was to teach lonely individuals to identify automatic negative thoughts and regard them as hypotheses to be tested rather than facts. Rook (1984) acknowledged that many of the studies in her review were not successful or lacked experimental rigor but indicated that interventions that focused on social skills, social support, opportunities for social interaction, and social cognition held promise for reducing loneliness.
A 1990 review also identified social skills training, opportunities for social interaction, and CBT as potentially effective in reducing loneliness (McWhirter, 1990b). The author noted that whereas social skills training was initially developed to reduce anxiety and shyness, it has been successfully adapted to treat loneliness (Twentyman & Zimering, 1979). Other programs have achieved success by providing individuals with opportunities to find others with common goals and by arranging activities of interest for small groups of lonely individuals (Cutrona & Peplau, 1979). McWhirter (1990b) referred to several CBT-based studies that succeeded in reducing loneliness (Anderson & Arnoult, 1985; Anderson, Horowitz, & French, 1983; Young, 1982). Some studies even showed that combining CBT with social skills training was more effective in treating lonely and socially anxious adults than either treatment alone (Glass, Gottman, & Shmurak, 1976; Rook & Peplau, 1982).
A third review examined twenty-one interventions designed to reduce loneliness among older individuals (Cattan & White, 1998). Although references to the specific interventions were not provided, the authors grouped them into four categories: 1) group activities, 2) one-to-one interventions 3) service delivery, and 4) whole community approaches. Taking design quality into consideration, the authors concluded that the most effective interventions included group activities, self-help, or bereavement support, targeted specific groups (e.g., women and widowers), used more than one intervention strategy, had an evaluation that coincided with the intervention, and gave participants some level of control. The lone study that evaluated a community approach was deemed inconclusive due to poor study design.
A subsequent review identified 17 loneliness reduction interventions published between 1982 and 2002 (Findlay, 2003). This report used a classification scheme similar to that of Cattan & White (1998) (e.g., group interventions, one-to-one interventions, service provision, and Internet usage). Although this typology does not perfectly match that of Rook (1984) or McWhirter (1990), most of the studies addressed social skills, social support, opportunities for social interaction, or social cognition. For example, the one-to-one interventions included telephone-based and gatekeeper programs designed to enhance social interaction and social support, respectively. Similarly, the group interventions included teleconferencing, support groups, and friendship enrichment training, which were also designed to improve social interaction and social skills. The service provision interventions focused on social support whereas the Internet programs represented an approach to increasing opportunities for social interaction. Whereas some of the programs in this review showed benefit, Findlay (2003) noted that many were flawed by weak study design. For example, only six of the 17 studies were randomized controlled trials. As a result, this review concluded there was little evidence to support the notion that interventions can reduce loneliness among older people.
Cattan et al. (2005) conducted a qualitative review of studies published between 1970 and 2002 and found 30 papers that evaluated loneliness prevention interventions among older adults (Cattan, White, Bond, & Learmouth, 2005). In this review, the authors used their previous typology (e.g., group activities, one-to-one counseling, service provision, and community development). These categories were further refined to include group activities with an educational component; group interventions to provide social support; home visits to provide assessment, information, or social services; home visits or telephone contact to provide directed support or problem solving; and one-on-one interventions to provide social support. As in previous reviews, these interventions addressed social skills, social support, opportunities for social interaction, and social cognition. Because only 16 of the 30 studies were randomized controlled trials, Cattan et al. (2005) also highlighted the dearth of methodological rigor among loneliness reduction interventions. Nonetheless, of the 13 studies considered to be of high quality, six were considered effective, one was considered partially effective, five were considered ineffective, and one was considered inconclusive. Consistent with their previous review, Cattan et al. (2005) concluded that the most effective programs were group interventions that included an educational component or a targeted activity, targeted specific groups (e.g., women, care-givers, the widowed, the physically inactive, or people with serious mental health problems), tested a representative sample of the intended target group, and enabled some level of participant and/or facilitator control.
The final review examined 36 studies and focused on persons with severe mental illness, a population whose prevalence of loneliness is approximately twice that of the general population (Perese & Wolf, 2005). Interventions to reduce loneliness in this group were similar to those developed for the general population, including social skills training, enhanced social support, increased opportunities for social interactions, and cognitive behavioral training. Support groups were noted to be the primary method for social skills training in this population. In one study, this approach was associated with a decline in unmet needs for friends (Perese, Getty, & Wooldridge, unpublished). In contrast, mutual-help groups represented the primary strategy for enhancing social support among those with mental illness. Although few studies have evaluated this approach, one study found mutual-help groups reduced psychiatric symptoms, hospitalizations, and social isolation among the mentally ill (Galanter, 1988).
According to Perese & Wolfe (2005), one way to increase opportunities for social interaction is befriending, which “aims to develop a relationship between individuals that is distinct from professional/client relationships”(Cox, 1993). Originally developed to reduce loneliness, its goals have grown to include improving quality of life, reducing social isolation, helping people meet emotional needs, and promoting and maintaining mental health (Andrews, Gavin, Begley, & Brodie, 2003). Although befriending appears to reduce social isolation, studies to date have not assessed the effect of befriending on loneliness among individuals with mental illness or the general population. Finally, deficits in social cognition were addressed through self-help groups, which attempted to change thinking from negative and fearful to positive and self-supportive (Murray, 1996). The self-help groups in this review focused on problems brought up by members and on coping techniques taught by professional group leaders. The review noted that little research has assessed the efficacy of this approach. However, one study found that family members who attended self-help groups reported improvements in their relationships with mentally ill family members (Heller, Roccoforte, Hsieh, Cook, & Pickett, 1997).
In summary, six previous qualitative reviews of loneliness reduction studies identified both successful and unsuccessful interventions. Five of the reviews concluded loneliness could be reduced with certain interventions but one concluded there was little evidence that current techniques can reduce loneliness, especially among lonely elders (Findlay, 2003). In three of the reviews, interventions were explicitly classified as addressing social skills, social support, opportunities for social interaction, or impairments in social cognition (McWhirter, 1990b; Perese & Wolf, 2005; Rook, 1984). In the other three reviews, this classification was implicit, although not all reviews included studies that addressed impaired social cognition (Cattan & White, 1998; Cattan, White, Bond, & Learmouth, 2005; Findlay, 2003). All of the reviews noted a dearth of randomized controlled trials and all called for increased rigor in evaluating loneliness reduction interventions.
Purpose of the Meta-Analysis
The goal of this meta-analysis is to provide the rigor called for by previous reviews and quantify the efficacy of the primary intervention strategies. Although previous reviews suggested that certain interventions can reduce loneliness, the results were mixed and a significant number of interventions were not associated with loneliness reduction. It may be that the success of certain interventions was due more to study design than to the quality of the intervention. For example, pre-post studies, non-randomized group comparison studies, and randomized group comparison studies are inequivalent designs in terms of comparing effect sizes (Lipsey & Wilson, 2001). Using meta-analysis, mean effect sizes can be compared across study designs and within groups of studies of the same design. Within study design, heterogeneity of effect sizes can be assessed and, when evident, examined to determine whether efficacy varies as a function of intervention format (group-based versus individual-based), intervention mode (technology-based versus non-technology-based), the type of loneliness measure used, the frequency and duration of the intervention, and the age and sex of the study participants. Each of these variables has the potential to influence intervention efficacy and the studies we reviewed provided data regarding these characteristics. We did not evaluate marital status as a potential moderator because very few studies provided data on this variable.
Interventions to date have relied upon an “individual differences” model, in which the lonely were considered to have deficits in social skills, social support, opportunities for social interaction, and/or social cognition. Given recent insights regarding the centrality of social cognition to loneliness (Cacioppo, Fowler, & Christakis, 2009; Cacioppo et al., 2006; Hawkley, Preacher, & Cacioppo, 2007), we hypothesized that interventions that address maladaptive social cognition will have a greater impact than those which address social skills, social support, or opportunities for social interaction.
Method
Selection of Studies Included in the Meta-Analysis
Applying recently published guidelines for meta-analysis (APA Publications and Communications Board Working Group on Journal Article Reporting Standards, 2008), the literature review identified trials that specifically targeted loneliness among adults, adolescents, and/or children. PubMed and PsycINFO were searched for relevant studies using combinations of the following keywords: loneliness, intervention, treatment, prospective, medication, and pharmacology. Eligible studies had to be published from 1970 through September 2009, in English, in a peer-reviewed journal or doctoral dissertation, designed as an intervention specifically to lower loneliness, and had to measure loneliness quantitatively.
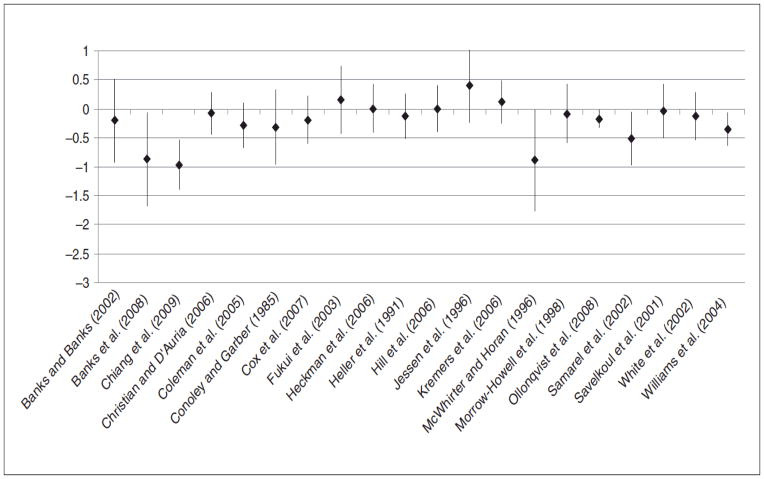
The initial search produced a total of 818 references in Medline and 777 references in PsycINFO, with significant duplication in references between the sources. As shown in Figure 1, the abstracts of 928 unique references were reviewed and 772 were excluded for lack of relevance based upon the abstract. The remaining 156 studies were reviewed in detail. Of these, 12 studies were excluded because they were descriptive reviews that did not assess loneliness interventions either qualitatively or quantitatively. However, two additional studies were identified in these reviews. This resulted in 146 studies that were further evaluated. Of these, 78 did not meet our initial inclusion criteria. A request for relevant studies posted on the listserv for the Society for Personality and Social Psychology (spsp-announce-l@list.cornell.edu) failed to generate any additional eligible studies. E-mail requests to individual authors in North America and Europe known to conduct research on loneliness elicited only one positive response. T. Fokkema indicated that a paper had been published in 2007, in the Dutch language, that reported the results of 18 loneliness interventions conducted among older adults in the Netherlands (Fokkema & van Tilburg, 2007). The authors forwarded an English version of the manuscript (Fokkema & van Tilburg, unpublished) and nine of the studies described met our initial inclusion criteria. Adding these studies to the others that met our initial criteria yielded 77 studies, which were then evaluated to determine whether they met established meta-analytic criteria.
Figure 1.
Identification of eligible studies for meta-analysis
Meta-Analytic Criteria
The first criterion for inclusion in the meta-analysis was that the intervention had to directly target loneliness. Seven studies were excluded because the interventions were directed at stress relief (Whitehouse et al., 1996), anxiety and/or depression (Mynatt, Wicks, & Bolden, 2008; Ransom et al., 2008), or health behaviors (de Craen, Gussekloo, Blauw, Willems, & Westendorp, 2006; Hedberg, Wikstrom-Frison, & Janlert, 1998; Hopman-Rock & Westhoff, 2002; Soholt Lupton, Fonnebo, Sogaard, & Fylkesnes, 2005). One study (Hu, 2009) examined the effect of an intervention on an induced state of loneliness, and was excluded from the analysis because induced loneliness is not comparable to the loneliness targeted in other included studies. In addition, the Wish Fulfillment study (Fokkema & van Tilburg, 2007) was excluded for lack of adequate information regarding the nature of the intervention. The second criterion was that the intervention effect had to be measured and reported quantitatively to enable the calculation of effect size. Although twelve studies originally failed to meet this criterion (Andersson, 1985; Brown, Allen, Dwozan, Mercer, & Warren, 2004; Clarke, Clarke, & Jagger, 1992; Evans & Jaureguy, 1982; Evans, Smith, Werkhoven, Fox, & Pritzl, 1986; Jones, Hobbs, & Hockenbury, 1982; McLarnon & Kaloupek, 1988; Routasalo, Tilvis, Kautiainen, & Pitkala, 2009; Seepersad, 2005; Stewart, Reutter, Letourneau, & Makawarimba, 2009; van Kordelaar, Stevens, & Pleiter, 2004; van Rossum et al., 1993), attempts to recover quantitative data from the authors were successful in two cases (Evans, Smith, Werkhoven, Fox, & Pritzl, 1986; Seepersad, 2005). The third criterion was that each study had to report original data not reported in another paper to avoid inflating effect sizes. Two studies were excluded based on this criterion. One study (Stevens, Martina, & Westerhof, 2006) was excluded because it duplicated data and because more complete results were reported in Martina and Stevens (2006), which was already included as an eligible study. Similarly, the other study (Add LUSTRE to your life, in Fokkema & van Tilburg, 2007) was excluded because a more detailed data of the same intervention was reported in Kremers, Steverink, Albersnagel, & Slaets (2006), which was already included. The fourth criterion was that the intervention had to involve a treatment group, not individual cases. On this basis, one study was excluded because the study focused on only two participants (Guevremont, MacMillan, Shawchuck, & Hansen, 1989). A total of 50 studies ultimately qualified for meta-analysis.
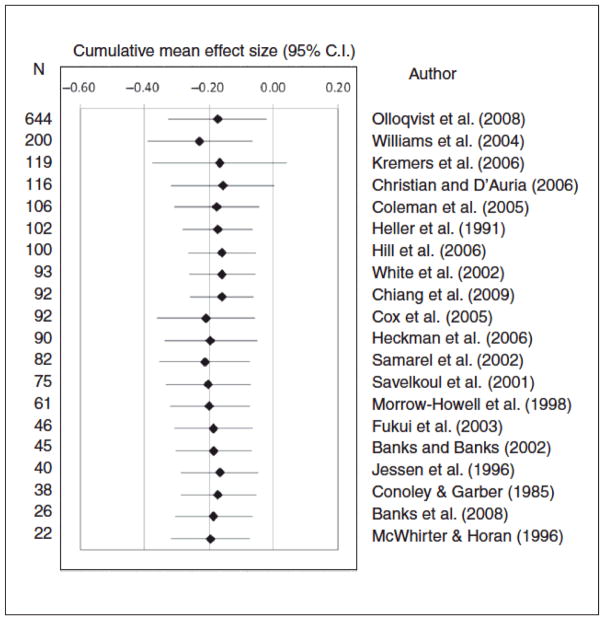
Because the effect size obtained from a single group pre-post study has a different meaning than the effect size calculated as the difference between two separate groups (Lipsey & Wilson, 2001), and because the effect size from a non-randomized group comparison often provides a less satisfactory estimate of the true effect size than a randomized group comparison study, the studies were categorized based on research design and a meta-analysis was conducted within each research design type. Of the 50 interventions, 12 were single group pre-post studies, 18 were non-randomized group comparison studies, and 20 were randomized group comparison studies.
Coded Variables
Key characteristics of the included studies are provided, by design type, in Tables 1–3. These tables provide effect sizes and information employed in moderator analyses, including mean age of the sample (as reported1 or as inferred when means were not reported2), gender composition (percent females, as reported or calculated3), intervention duration (in weeks, available for all but four studies4), intervention frequency (which was converted to total number of sessions for analysis purposes, and was calculable for all but fourteen studies5), type of loneliness measure (e.g., UCLA Loneliness Scale, DeJong Gierveld Loneliness Scale, other6), intervention format and mode (e.g., individual- or group-based and non-technology or technology-based, respectively), and intervention type (social skills training, enhanced social support, increased opportunity for social interaction, or social cognitive training). Intervention format was categorized as individual-based if the intervention was implemented on a one-on-one basis, and as group-based if more than one person participated in the intervention at the same time or if the intervention involved asynchronous interactions such as Internet-based chat room exchanges. Intervention mode was classified as technology-based if a telephone or computer was used to facilitate the intervention. Intervention type was categorized as 1) social skills training if the intervention focused on improving participants’ interpersonal communication skills, 2) as enhancing social support if the intervention offered regular contacts, care, or companionship, 3) as social access if the intervention increased opportunities for participants to engage in social interaction (e.g., online chat room or social activities), and 4) as social cognitive training if the intervention focused on changing participants’ social cognition. Importantly, intervention type was not confounded with study design: each intervention type was represented in each study design group (with the one exception that pre-post studies did not include a social skills intervention).
TABLE 1.
Single Group, Pre-Post Studies (N = 12)
| Authors | Enrollment Eligibility and Sample Size | Intervention Type and Duration | Effect Size (95% CI) | Intervention format | Intervention mode | Sample age | Sample % female | Loneliness Measure |
|---|---|---|---|---|---|---|---|---|
| (Battles & Wiener, 2002) | Seriously ill children visiting the National Institutes of Health for treatment of chronic medical conditions. Participants recruited from NIH playrooms by a recreation therapist, principal investigator, or research assistant. N=32. | Social access: Virtual environment designed to provide an interactive online community in which children played games, learned about their medical condition, or talked with other chronically ill children. Participants completed four 1-hour sessions over a period of 6 to 9 months. | −0.43 (−0.72, −0.14) | Individual | TECH | 8–19 yrs; mean=14 | 47% | 8 item UCLA Loneliness Scale. |
| (Bauminger, 2007) | Children who attended schools in middle-class, large urban areas and who had a prior clinical diagnosis of either high functioning autism or Asperger’s Syndrome. Schools and children were recruited through the Special Education Department in the Israeli Ministry of Education. N=19. | Social cognitive training: Cognitive-behavioral-ecological program conducted in each child’s school, implemented by the child’s main teacher, and involved one typically developing older peer and the child’s parents. Each child completed a cognitive behavioral-educational program, met with their assigned peer twice weekly, and the parents completed social tasks with their children over a 7 month period. | 0.12 (−0.23, 0.47) | Individual | NON-TECH | 7–11 yrs; mean= 9 | 5% | 16 item Asher Loneliness Scale. |
| (Collins & Benedict, 2006) | Using newsletters and promotional flyers, participants were recruited from senior centers and senior housing developments in Las Vegas and rural Clark County Virginia. N=339. | Social support: Small-group class led by paraprofessionals, volunteer peer educators, and on-site staff. Topics included nutrition and food, personal safety, reducing accidents in the home, financial strategies to manage limited resources, general wellness, and productive aging. Class met weekly for 4 months. | −0.45 (−0.54, −0.36) | Group | NON-TECH | 52–93 yrs; mean= 73 | 80% | 4 item UCLA Loneliness Scale. |
| (de Vries et al., 1997) | Eligibility required a histologically-confirmed diagnosis of malignant neoplasm, measurable disease with documented progression prior to protocol therapy, no options for further medical treatment, an acceptable clinical condition (Karnofsky at least 80), and no concomitant somatic disease which might influence length of survival and physical or psychosocial functioning. N=35. | Social support: Patients were offered 12 sessions of individual psychosocial counseling once a week, each session lasting 1.5 to 2 hours. Patients also participated in fortnightly group meetings. These group sessions were guided by two psychotherapists and lasted 2.5 hours. Partners of the patients were also invited to participate in the individual and group sessions. | −0.14 (−0.46, 0.18) | Group | NON-TECH | 27–73 yrs; mean= 55 | 54% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Kraut et al., 1998) | 1995 cohort comprised of families with teenagers participating in journalism classes in four Pittsburgh high schools. 1996 cohort comprised of families in which an adult was on the Board of Directors of one of four community development organizations. Households with active Internet connections were excluded and children younger than 10 years of age were excluded. N=169. | Social access: Families received a personal computer and software, a free telephone line, and free access to the Internet. Program lasted 2 years for the 1995 cohort and 1 year for the 1996 cohort. | −0.14 (−0.26, −0.02) | Individual | TECH | Not reported | 56% | 3 items from the UCLA Loneliness Scale. |
| (Marshall, Bryce, Hudson, Ward, & Moth, 1996) | Non-familial male child molesters incarcerated in a medium security Canadian penitentiary participated in the study. They had volunteered for treatment in the Bath Institution Sex Offenders’ Program, a comprehensive cognitive-behavioral program. N=32. | Social cognitive training: Topics discussed in group meetings were benefits of being in a relationship, sexual relations, jealousy, development of relationship skills, and dealing with loneliness. This curriculum was part of an overall treatment package offered as a group therapy program. Duration of program not described. | −1.46 (−1.91, −1.01) | Group | NON-TECH | 24–53 yrs; mean= 37 | 0% | 20 item UCLA Loneliness Scale. |
| (McAuley et al., 2000) | Sedentary, older, U.S. community-dwelling adults were recruited using fliers, advertisements in the local newspapers and announcements on local radio shows and local television news programs. N=174. | Social access: Aerobic intervention group classes were conducted by trained exercise specialists and employed brisk walking for up to 40 minutes 3 times per week for 6 months. Stretching and toning intervention group exercised under supervision for 40 minutes 3 times per week for 6 months. | −0.08 (−0.25, 0.08) | Group | NON-TECH | Range not reported; mean=67 | 72% | 20 item UCLA Loneliness Scale. |
| (Petryshen, Hawkins, & Fronchak, 2001) | Community-dwelling adults who were socially isolated and living with a serious and persistent mental health problem and were eligible for a social recreation program within a Canadian community mental health center. N=36. | Social access: Social recreation intervention, which included information sessions about opportunities and resources in the community, workshops on relationship development, workshops on healthy lifestyles, self-help groups, weekly community walks, and community forums on mental illness. Approximately 200 group activities were offered per year. Participation varied considerably. The median number of activities completed by participants was 18. | −0.59 (−0.88, −0.30) | Group | NON-TECH | 18–65 yrs; mean=43 | 61% | 4 item UCLA Loneliness Scale. |
| (Sorenson, 2003) | Women who reported significant psychological disruption after a traumatizing provider interaction during a birth experience unrelated to the baby’s physical outcome. Sample was recruited in conjunction with an International Cesarean Awareness Network (ICAN) state affiliate, ICAN referral agencies and midwifery practices in a U.S. metropolitan area. N=9. | Social cognitive training: 5 monthly group cognitive behavioral therapy sessions, each lasting 4 hours. Group leader was a psychiatric mental health clinical nurse specialist who encouraged the development of positive interpersonal relationships and provided support to confront issues and develop new cognitive and relationship skills. | −4.81 (−7.09, −2.53) | Group | NON-TECH | 26–45 yrs; mean=33 | 100% | 20 item UCLA Loneliness Scale. |
| (Stewart, Craig, MacPherson, & Alexander, 2001) | Canadian widows over age 55 with no neurological deficits who spoke and wrote English and who were not currently attending a bereavement self-help or support group. N=23. | Social support: Four support groups comprised of 5–9 participants met for 1–1.5 hours weekly for a maximum of 20 weeks. Each group was led by a peer (widow) and a professional facilitator. Participants were invited to discuss their priority needs and relevant issues. Discussions were augmented by guest lecturers, case studies, audiovisual aids, and role-playing exercises. | −0.27 (−0.60, 0.06) | Group | NON-TECH | 54–77 yrs; mean=66 | 100% | 15 item Emotional/Social Loneliness Inventory. |
| (Stewart, Reutter, Letourneau, & Makawarimba, 2009) | Homeless youths in Edmonton were referred from employment programs, drop-in centers, and a Community Advisory Committee. N=14. | Social support: 20 week intervention program consisting of 4 support groups, which included one-on-one support, group recreational activities, and meals. | −0.34 (−0.77, 0.08) | Group | NON-TECH | 16–24 yrs; mean=19 | 46% | 20 item UCLA Loneliness Scale. |
| (Yarnoz, Plazaola, & Etxeberria, 2008) | Long-term separated or divorced adults with children. N=7. | Social support: Attachment-based intervention, encouraging people to elaborate, through shared narratives with peers and the therapists, a representation of the events, the self, the other, and the relationships that contribute to a better adjustment to the situation of divorce. Participants met for a two-hour session each week for 8 months. Each session was led by a psychoanalyst and an attachment-oriented professional on an alternating basis. | −0.09 (−0.66, 0.49) | Group | NON-TECH | 50–60 yrs; mean=54 | 43% | 15 item Social and Emotional Loneliness Scale. |
TABLE 3.
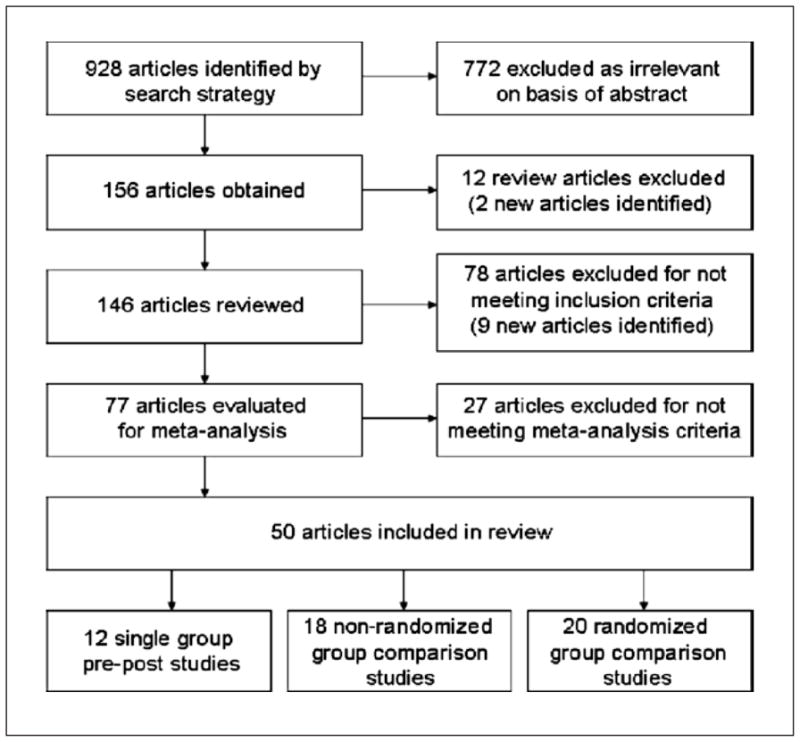
Randomized Group Comparison Studies (N = 20)
| Authors | Enrollment Eligibility and Sample Size | Intervention Type and Duration | Effect Size (95% CI) | Intervention format | Intervention mode | Sample age | Sample % female | Loneliness Measure |
|---|---|---|---|---|---|---|---|---|
| (Banks & Banks, 2002) | Recruited from three nursing homes in a city in southern Mississippi. Inclusion criteria included no cognitive impairment, no history of psychiatric disorder, and a score of 30 or greater on the UCLA Loneliness Scale. N=45. | Social support: Animal-Assisted Therapy (AAT) consisted of an attendant bringing a leashed dog to the participant’s room for 30 minutes. Participants were allowed to hold, stroke, groom, talk to, play with, or walk the dog in the hallway. Interaction with attendant was minimized. AAT-1 group members had one session per week while AAT-3 members had three sessions per week. Control group received no AAT sessions. Duration of study was 6 weeks. | −0.20 (−0.92, 0.52) | Individual | NON-TECH | Range not reported; mean inferred=78 | 80% | 20 item UCLA Loneliness Scale. |
| (Banks, Willoughby, & Banks, 2008) | Recruited from three nursing homes in St. Louis, Missouri. Inclusion criteria included no cognitive impairment, no history of psychiatric disorder, and a score of 30 or greater on the UCLA Loneliness Scale. N=26. | Social support: Animal-Assisted Therapy (AAT) consisted of a weekly 30 minute visit from either a living dog or a robot dog (AIBO) for 8 weeks. Sessions occurred in the resident’s room and consisted of the resident sitting in his or her chair or upright in bed with the dog or AIBO next to the resident. Control group received no AAT sessions. | −0.88 (−1.68, −0.07) | Individual | NON-TECH | Range not reported; mean inferred=75 | Inferred as 80% | 20 item UCLA Loneliness Scale. |
| (Chiang et al., 2009) | Participants were recruited from a nursing home in the Taipei area. Inclusion criteria were 1) conscious and able to speak Mandarin or Taiwanese, 2) aged 65 years or over, and 3) scored greater than 20 on the Mini Mental State Examination. N=92. | Social cognitive training: Intervention consisted of 8 weekly sessions of individual reminiscence therapy. Each session focused on a different topic, including sharing memories and greeting each other, increasing participant awareness of their feelings and helping them to express their feelings, and identifying positive relationships from their past and how to apply positive aspects of past relationships to present relationships. | −0.97 (−1.40, −0.54) | Individual | NON-TECH | Range not reported; mean=77 | 0% | 20 item UCLA Loneliness Scale. |
| (Christian & D’Auria, 2006) | Recruited from four university-based cystic fibrosis centers in North Carolina. N=116. | Social skills training: Educational problem-solving and social skills intervention designed to help children with cystic fibrosis (CF) deal with specific problems, including finding out about their CF diagnosis, explaining their CF related differences, dealing with teasing about CF, and keeping up with peers during physical activity. Intervention included an individual home visit and a structured, small-group (4 children) session approximately two weeks later. Control group did not receive intervention. | −0.08 (−0.44, 0.29) | Group | NON-TECH | 8–12 yrs; mean=9 | 49% | 16 item Asher Loneliness Scale. |
| (Coleman et al., 2005) | Women referred from hospitals in urban and rural communities in Arkansas and from the Arkansas Division of the American Cancer Society who were English-speaking and diagnosed with TNM stage 0, I, II, or III non-metastatic breast cancer, had no major underlying medical problems or previous history of cancer (except for non-melanoma skin cancer) and who entered the study two to four weeks post-surgery. N=106. | Social support: In Phase I, oncology nurses provided weekly telephone social support from 2–3 weeks post-surgery through 3 months. In Phase II, weekly calls were continued through 5 months post-surgery and participants received a resource kit regarding adaptation to disease and treatment. In Phase III, calls were decreased to twice per month through 8 months post-surgery. In Phase IV, calls decreased to once per month until the one year anniversary of diagnosis. Control group received the same resource kit but no telephone social support. | −0.29 (−0.67, 0.09) | Individual | TECH | Range not reported: mean=57 | 100% | 20 item UCLA Loneliness Scale. |
| (Conoley & Garber, 1985) | U.S. undergraduate students who scored one SD above the mean on UCLA Loneliness Scale and scored as moderately depressed on the Beck Depression Inventory. N=38. | Social cognitive training: Two 30-minute individual counseling sessions (1 week apart) which emphasized either reframing perception of loneliness or self-control (i.e., trying harder to overcome loneliness). Control group did not receive counseling sessions. | −0.32 (−0.96, 0.32) | Individual | NON-TECH | Range not reported; mean inferred=20 | 100% | 20 item UCLA Loneliness Scale. |
| (Cox, Green, Hobart, Jang, & Seo, 2007) | Community-dwelling older adults from the Denver area who were 55 years or older and required a minimum of 6 hours of personal care per week due to stroke, heart disease, osteoporosis, mild dementia, cancer, or severe arthritis. N=92. | Social support: 10 biweekly sessions of 1.5 to 2 hours related to specific themes and 2 review sessions. The goal was to increase the capacity of elderly care receivers to effectively manage their own care, including optimizing the relationship with their caregiver. Comparison group received needs assessment, referral and assistance, monthly follow-up and ongoing telephone assistance at the request of the participant. | −0.19 (−0.60, 0.22) | Individual | NON-TECH | 51–96 yrs; mean=79 | 77% | Philadelphia Geriatric Morale Scale on Lonely Dissatisfaction. |
| (Fukui, Koike, Ooba, & Uchitomi, 2003) | Recruited from a group of outpatients with breast cancer who were surgically treated at a national cancer center hospital in Japan. All patients were younger than 65 years old, had surgery within the previous 4–18 months, and had no chemotherapy or had completed chemotherapy. N=46. | Social support: 3 intervention groups of 6–10 patients met for 1.5 hours weekly for six weeks. Intervention consisted of health education, coping skills training, stress management, and psychological support. Goals of the intervention were to provide within-group support by professionals and peers, lessen the psychological distress associated with having cancer, and assist patients in learning effective coping methods for cancer related concerns. Control group did not receive intervention. | 0.15 (−0.43, 0.73) | Group | NON-TECH | Range not reported; mean=54 | 100% | 20 item UCLA Loneliness Scale. |
| (Heckman & Barcikowski, 2006) | Eligibility criteria included 50 years of age or older, HIV infected or had AIDS by self report, diagnosed with major depressive disorder, partial remission of major depression, dysthymia, or minor depressive disorder, and score of 75 or higher on the Modified Mini-Mental State Examination. N=90. | Social support: Twelve weekly 90 minute telephone conference calls emphasizing coping strategies to reduce psychological distress. Each group was comprised of 6–8 participants and 2 leaders. Topics included sharing personal histories, identifying life stressors, sharing personal coping strategies, a discussion of adaptive problem-focused coping, adaptive emotion focused coping, and ways to increase social resources. Intervention duration was 3 months. Control group did not participate in conference calls. | 0 (−0.41, 0.41) | Group | TECH | Range not reported; mean=54 | 32% | 10 item UCLA Loneliness Scale. |
| (Heller, Thompson, Trueba, Hogg, & Vlachos-Weber, 1991) | Telephone calls were made to a random sample of residences in low-income housing tracts in three Indiana communities to identify women living alone or with one other person in the household. Selection criteria were annual household income below median for Indiana senior citizens and either below median perceived support or above median loneliness. N=102. | Social support: Initial randomization was to either 10 weeks of friendly staff telephone contact or control group. Staff called twice a week for 5 weeks then once a week for 5 weeks. Staff inquired about participant’s health and well-being, events of the week, and stressful life events. After 10 weeks, those receiving the staff contact were randomly assigned to continue that contact or were paired in dyads to continue phone contact with one another. Control group received no intervention. | −0.12 (−0.51, 0.27) | Individual | TECH | Range not reported; median=74 | 100% | 7 item Paloutzian and Ellison Loneliness Scale. |
| (Hill, Weinert, & Cudney, 2006) | Community-living, chronically ill women living in rural western U.S. Recruitment occurred through mass media, agency and service organization newsletters, and word of mouth. N=100. | Social access: 22 weeks of participation in an online, asynchronous, peer-led support group, and a health teaching unit. Participants received in-home Internet access to e-mail and an asynchronous chat room in which they exchanged feelings, expressed concerns, provided support, and shared life experiences. Intervention also included web-based health education modules. In addition, participants also engaged in expert-facilitated chat room discussions related to the health teaching unit activities. Control group did not receive intervention. | 0.004 (−0.39, 0.40) | Group | TECH | 35–65 yrs; mean inferred=52 | 100% | 20 item UCLA Loneliness Scale. |
| (Jessen, Cardiello, & Baun, 1996) | Men and women ages 65 or older admitted to two Midwestern skilled rehabilitation units. All newly admitted persons were approached but participation was voluntary. N=40. | Social support: Caged bird (budgerigar) placed in participant’s room for 10 days. Participants received verbal and written instructions regarding the bird but participants did not provide care to the bird. Control group did not receive the intervention. | 0.40 (−0.23, 1.02) | Individual | NON-TECH | 65–91 yrs; mean=76 | 68% | 20 item UCLA Loneliness Scale. |
| (Kremers, Steverink, Albersnagel, & Slaets, 2006) | Participants recruited through advertisement in local newspapers in two regions of the Netherlands. Single, community-dwelling women, 55 years and older, were asked by phone if they missed having people around them, wished to have more friends, participated in very few leisure activities, or had trouble initiating activities. N=119. | Social skills training: Intervention consisted of six weekly group meetings which included 8–12 participants and two facilitators. Each meeting lasted 2.5 hours and focused on one or more techniques, including taking initiative in making friends, investing in friendships, having a positive frame of mind, finding and maintaining multifunctionality in friendship, and having more than one friend. Control group did not participate in group meetings. | 0.12 (−0.25, 0.49) | Group | NON-TECH | Range not reported; mean=64 | 100% | 11 item De Jong Gierveld loneliness questionnaire. |
| (McWhirter & Horan, 1996) | U.S. university students who responded to a publicized program at a university counseling center were accepted if they scored one standard deviation above the mean on the UCLA Loneliness Scale for college age populations, reported experiencing loneliness within the four week period prior to intake, and presented no clinical evidence of suicidal behavior or severe depression. N=22. | Social cognitive training: A counselor led each structured, small group (3–5 participants) experience, which met for two hours each week for 6 weeks. Intimate condition group used cognitive and behavioral techniques to focus on establishing and maintaining intimate relationships. Social condition group combined cognitive restructuring with modeling, role play, and homework assignments for developing better communication skills in social settings. Combined condition group included all elements of the intimate and social condition groups. Control condition met to express feelings and share experiences but counselor did not suggest ways to reduce loneliness. | −0.89 (−1.77, −0.01) | Group | NON-TECH | 18–38 yrs; mean=25 | 48% | 20 item UCLA Loneliness Scale from which intimate and social loneliness subscales were derived. |
| (Morrow-Howell, Becker-Kemppainen, & Lee, 1998) | Older U.S. adults in the St. Louis area who either called a suicide crisis hotline or were referred from family members, friends, or professionals due to depression, social isolation, or unmet needs in activities of daily living. N=61. | Social support: Social worker made weekly telephone calls to administer three components of the program: multidimensional psychosocial evaluation, assistance with social services, and supportive therapy, through which the social worker encouraged the client to articulate problems, explore possible solutions, and take action. Median length of contact was 8 months. Control group did not receive intervention. | −0.09 (−0.59, 0.41) | Individual | TECH | 61–92 yrs; mean=76 | 85% | OARS Social Resource Rating Scale regarding loneliness frequency. |
| (Ollonqvist et al., 2008) | Working in collaboration with seven independent rehabilitation centers and 41 municipalities throughout Finland, the goal was to recruit a representative sample of frail older persons over age 65 who were living at home but faced a risk of institutionalization within two years due to progressively decreasing functional capacity. N=644. | Social support: Intervention consisted of a network-based group rehabilitation program which consisted of three separate inpatient periods at a rehabilitation center within eight months. Participants had individual visits with the physician, physiotherapist, social worker, and occupational therapist. In addition, participants engaged in group activities which focused on various exercises, as well as group discussions and lectures. Topics included promotion of self-care, psychological counseling, medical issues, social services, and recreational activities. | −0.17 (−0.33, −0.02) | Group | NON-TECH | 65–96 yrs; mean=78 | 86% | Do you feel yourself lonely? 0 = never, 1 = seldom, 2 = sometimes, 3 = often, 4 = always. |
| (Samarel, Tulman, & Fawcett, 2002) | English-speaking U.S. women who had had surgery for non-metastatic (TNM stage 0, I, II, or III) breast cancer within 4 weeks prior to study participation, had no previous cancer diagnosis except for non-melanoma skin cancer, and had no other major medical problems. N=82. | Social support: Experimental group received weekly 2-hour, group social support and education (topics included stress management, communication techniques, problem solving skills, and understanding emotions and needs) as well as weekly individual telephone social support and education over 13 months. Control group 1 received weekly individual telephone social support and education over 13 months. Social support and education were provided by either oncology nurse-clinicians or social workers. Control group 2 received educational resource kit via a one-time mailing. | −0.51 (−0.97, −0.05) | Group | TECH | 30–83 yrs; mean=54 | 100% | 20 item UCLA Loneliness Scale. |
| (Savelkoul, de Witte, Candel, Van Der Tempel, & Van Den Borne, 2001) | Patients of rheumatology clinics in 2 regional hospitals in the Netherlands. Final sample was selected on the basis of chronic rheumatologic condition, duration of more than 1 year, age between 35 and 65 years, higher than median score on impact of rheumatic disease on functional health status, and a higher than median score on at least 1 of the following: loneliness, lack of social support, or impact of rheumatic disease on social behavior. N=75. | Social support: Aim of coping intervention group was to increase action-oriented directed coping and coping by seeking social support. Emphasized 4 steps: describe the problem, think about possible solutions, choose 1 or more solutions, implement the solution and evaluate the results. Aim of mutual support group was to exchange information, experiences, feelings, and emotions. No coping skills were taught. There were 10 weekly two-hour sessions in each intervention and each group was comprised of 10–12 participants. Control group did not receive the intervention. | −0.04 (−0.49, 0.41) | Group | NON-TECH | 35–65 yrs; mean=51 | 68% | 11 item De Jong Gierveld Loneliness questionnaire. |
| (White et al., 2002) | Residents of four U.S. congregate housing sites and two nursing facilities. Volunteers were solicited during information sessions open to all residents at each site. N=93. | Social access: 9 hours of training over a two week-period. Training covered basic computer operation, use of e-mail, and introduction to accessing the Internet. Each participant also received a training manual. Subsequently, the trainer was available at each site for about two hours per week for technical support. Trainer was also available by phone and e-mail. Duration of program was 5 months. Control group did not receive the intervention. | −0.13 (−0.54, 0.27) | Individual | TECH | Range not reported; mean=71 | 76% | 20 item UCLA Loneliness Scale. |
| (Williams et al., 2004) | Recruits at basic training at the Naval Recruit Training Command at Great Lakes, Illinois. Those who scored 18 or higher on the Beck Depression Inventory of 30 or higher on the Perceived Stress Scale were classified as at-risk recruits. N=200. | Social cognitive training: Cognitive behavioral intervention consisted of 10–15 at-risk recruits meeting for 45 minutes each week for 9 weeks. Groups were facilitated by a psychologist. Participants read a manual each week, then discussed and practiced strategies for coping, increasing one’s sense of belonging, decreasing thought distortion, and stress management. Non-intervention and comparison groups participated in weekly meetings which focused on other topics, such as swimming skills and personal hygiene. | −0.36 (−0.64, −0.08) | Group | NON-TECH | Range not reported; mean=20 | 28% | 20 item UCLA Loneliness Scale. |
Effect Size Calculation
Established procedures were used to calculate the effect size for each of the qualified studies (Lipsey & Wilson, 2001). The standard error of each effect size was calculated in order to derive the inverse variance that served as our weighting unit for the mean effect size across studies. For a better depiction of the relative weight given to each study, the percentage of weight was calculated by dividing each individual weight by the sum of weights from each group of studies.
For single group pre-post studies, effect sizes were calculated by taking the difference between pre- and post-treatment loneliness scores and dividing by the pooled standard deviation of the two scores. Correlations between pre- and post-treatment loneliness values were required to calculate standard errors of the pre-post effect sizes using the formula:
where SE = standard error of the effect size, r = the correlation between pre- and post-treatment loneliness values, n = the sample size, and ES = effect size. With two exceptions (Christian & D’Auria, 2006; Cox, Green, Hobart, Jang, & Seo, 2007), these correlations were not provided by study authors. These correlations were estimated to be 0.7, which approximates the test-retest reliability for loneliness over periods of a year or more, and is consistent with test-retest correlations reported in the literature (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Russell, 1996).
For randomized and non-randomized group comparison studies, effect sizes were calculated as the loneliness difference between the treatment and control group divided by the pooled standard deviation of the two scores. Standard errors of the effect sizes were calculated by multiplying the pooled standard deviation with the square root of the sum of the inverse of each sample size.
If a study didn’t provide enough information regarding the means and standard deviations of the post-treatment loneliness scores but provided chi-square, F, or t test results on the difference between the treatment and control group after the intervention, an online effect size calculator was accessed to determine the effect sizes from those test results (Wilson, 2002).7
When the authors reported the effect sizes but not other statistics for their intervention (Banks & Banks, 2002; Savelkoul, de Witte, Candel, Van Der Tempel, & Van Den Borne, 2001), those effect sizes were used.8 If the author reported subscale loneliness scores separately (McWhirter & Horan, 1996; Stewart, Craig, MacPherson, & Alexander, 2001), effect sizes were calculated for all sub-scales and their mean was reported as the effect size for the given study.
Effect sizes based on post-treatment group differences and their pooled standard deviations are known as Cohen’s g, which is said to be upwardly biased especially for small samples (Hedges & Olkin, 1985). To adjust for this bias, g was multiplied by a correction term of [1 – 3/(4N-9)] where N equals the sample size to get an unbiased estimator known as Hedge’s d (Hedges & Olkin, 1985), and this adjusted effect size was used for our analyses.
Studies were evaluated for baseline differences in loneliness between the treatment and control groups, especially studies with non-randomized group comparison designs. Four of the studies reported baseline differences in loneliness between the treatment and control groups: (Cohen et al., 2006; Hartke & King, 2003; Martina & Stevens, 2006; White et al., 1999). To avoid misleading effect sizes that would result from comparing only the post-treatment scores, the effect size was calculated as the difference between the changes of the treatment and the control groups. In addition, in one study (Kolko, Loar, & Sturnick, 1990), baseline differences in loneliness were not reported but were determined to be present because confidence intervals around treatment and control group loneliness means at baseline did not overlap. These groups were treated as statistically different at baseline and effect size was calculated accordingly.
Primary Effect Size
Effect sizes included in Tables 1–3 are “primary” effect sizes, which were calculated from the first available post-treatment measurement time point. In addition, in studies with more than one intervention group, the primary effect size was calculated for the intervention group that reflected the key feature of each intervention, or that incorporated the fewest design flaws. In studies with more than one control group, the control group that was theoretically expected to exhibit the greatest difference from the treatment group was used to calculate the primary effect size.
Five studies had more than one intervention group. For three of these studies, the primary effect size was based on the intervention that best represented the key features of the intervention. In Allen-Kosal (2008), the three intervention groups received, respectively, a pre-training session, an eight-week class, or both a pre-training session and a class. The group with both the pre-training and the eight-week class was selected to calculate the primary effect size. In Banks et al. (2008), animal-assisted therapy was provided to one intervention group with a robotic dog, and to a second group with a real dog. A sizeable literature documents the benefits of owning “real” pets (Keil, 1988), so the real dog intervention was included as the primary intervention. In McWhirter & Horan (1996), the three intervention groups—intimate condition, social condition, and combined condition—focused on a different set of skills and techniques for improving intimate, social, or both types of relationships, respectively. The combined condition included both the intimate and social components of the intervention and was therefore treated as the primary effect.
In two additional studies with more than one intervention group, the intervention with the fewest implementation failures was selected to calculate the primary effect size. In Cox et al. (2007), a small group-based version and an individual-based version of the “Care-Receiver Efficacy Intervention” were compared with a standard individual-based case management group. Randomization wasn’t fully implemented because only participants who were able to access and participate in the group-based intervention were eligible for the small-group treatment, and all eligible participants were assigned to the small-group treatment. All individual-eligible participants were randomly assigned to individual-based treatment or the case management control group condition. The effect size from the individual intervention group was therefore treated as the primary intervention. In Heller et al. (1991), the effect on loneliness and psychological well-being of telephone call support from staff was compared to that of telephone support from peers. Participants were first randomized into treatment or control groups. The treatment group received 10 weekly staff phone calls whereas the control group received no intervention. After 10 weeks of regular staff phone calls, participants in the treatment group were randomly assigned to one of three intervention conditions. In one intervention, staff phone calls continued. In the second and third intervention types, participants were assigned to either receive or initiate regular phone calls with a peer in the study. The frequency of phone calls was held constant across all intervention types. However, since 27 out of the 125 participants (22%) in the second and third intervention groups declined to participate after the randomization and all of the participants in the staff contact group remained, the staff contact group was used to calculate the primary effect size to avoid the potential self-selection problem in the other two groups. The control group used for the calculation of the primary effect size was the group that received nothing throughout the study.
Three studies included more than one control group. In Samarel et al. (2002), the treatment included telephone support and group social support along with a mailed education kit; one control group received telephone support with mailed materials, and the other control group received only the mailed materials. The primary effect size was calculated using the control group that received the mailed materials only (i.e., the group that was expected to exhibit the greatest difference relative to the treatment group). Conoley & Garber (1985) administered cognitive reframing as the main intervention. In addition to the control group that received no intervention, this study had another comparison group whose members were instructed “to try harder” to overcome loneliness. The primary effect size was calculated using the control group that received no intervention. Heckman & Barcikowski (2006) had two time-lagged intervention groups (immediate and delayed) serving as control groups for each other; effect sizes were calculated for both interventions but the immediate condition was treated as the primary intervention because its control group didn’t receive any intervention and thus was more comparable to the control groups of other included studies.
Analyses
The meta-analytical procedure demonstrated in Borenstein et al. (2009) was used to calculate the mean effect size, identify the level of heterogeneity, and perform the subsequent moderator analyses. Due to the wide range of interventions included in this meta-analysis, a random-effects model was selected. In contrast with the fixed-effect model, which assumes that all studies have the same true effect size, the random-effects model assumes that the true effect size varies across studies and follows a normal distribution around the mean. The summary effect size is thus an estimation of the mean of a distribution of effects, not the single true effect assumed and estimated by the fixed-effect model. The random-effects model takes two sources of variance into consideration: within-study error in the estimate of the effect size, and between-study variation in the true effect size. The Q-statistic and p-value were calculated to test the assumption of homogeneity in effect sizes. The T2 statistic was calculated to estimate the magnitude of the between-study variance of the true effect sizes. The I2 statistic was calculated to estimate the proportion of total observed variance attributable to between-study variation in effect size as opposed to random error. The more I2 deviates from zero, the greater the justification for follow-up moderator analyses that explore reasons for the between-study variation. As benchmark values, Higgins et al. (2003) suggest that between-study variance of 25% is low, 50% is moderate, and 75% is high (Higgins, Thompson, Deeks, & Altman, 2003). Using procedures described by Borenstein et al. (2009), the influence of categorical moderator variables was assessed using subgroup analyses analogous to ANOVAs that partition the total effect size variance into variance within and between groups (Borenstein, Hedges, Higgins, & Rothstein, 2009). Within-study variance is removed from the total variance, and the remaining between group variance (Qb) was used to test whether effect sizes differed among categories of a given moderator. The influence of continuous moderator variables was assessed using weighted regression analyses.
Ancillary analyses were used to determine whether meta-analytic results differed if the primary effect size was replaced with the alternative effect size calculated from delayed post-treatment measures. A total of thirteen studies had delayed post-treatment measures. Three used a single group pre-post design (McAuley et al., 2000; Stewart, Craig, MacPherson, & Alexander, 2001; Stewart, Reutter, Letourneau, & Makawarimba, 2009); two used a non-randomized group comparison design (Allen-Kosal, 2008; Martina & Stevens, 2006); and eight used a randomized group comparison design (Chiang et al., 2009; Christian & D’Auria, 2006; Coleman et al., 2005; Conoley & Garber, 1985; Cox, Green, Hobart, Jang, & Seo, 2007; Fukui, Koike, Ooba, & Uchitomi, 2003; Heller, Thompson, Trueba, Hogg, & Vlachos-Weber, 1991; Kremers, Steverink, Albersnagel, & Slaets, 2006; McWhirter & Horan, 1996). Also examined was the effect of using the largest effect size in each study. This decision resulted in six new effect sizes9: One was a single group pre-post design (Stewart, Craig, MacPherson, & Alexander, 2001); one was a non-randomized group comparison design (Allen-Kosal, 2008); and four fused a randomized group comparison design (Christian & D’Auria, 2006; Fukui, Koike, Ooba, & Uchitomi, 2003; Heckman & Barcikowski, 2006; Kremers, Steverink, Albersnagel, & Slaets, 2006). Results of the ancillary analyses did not differ substantively from those reported in our primary analyses below.
Results
Studies with a Single Group Pre-Post Design
Twelve studies met our criteria for single group pre-post interventions to reduce loneliness. In terms of the target population, two of the studies focused on children, seven had sample age ranges between 19 and 55 years old, and three focused on individuals aged 65 years or older. With the exception of two studies, the gender composition of the studies in this group consisted of more female than male participants. There was no social skills training intervention in this group but the remaining three types of interventions were equally presented. The majority of the interventions in this group were group-based with no utilization of technology. UCLA loneliness measures were used in eight of the twelve studies. The details of these studies are summarized in Table 1.
The effect sizes in this group differed across studies, ranging from −4.81 to 0.12. As is shown in Table 4, the mean effect size for these twelve studies was −0.367 (95% CI: −0.55, −0.18; p < .001). The distribution of effect sizes is displayed in Figure 2. The degree of dispersion as indicated by the between-study variance statistic, T2, was 0.18. A significant Q statistic (28.52, p < .01) indicated a heterogeneous distribution of effect sizes. The I2 showed that 61% of the variance could be attributed to between-study variation. To examine whether heterogeneity was caused by the presence of an outlier, Sorenson (2003) was removed and the same analysis was conducted again. The mean effect size of the remaining eleven studies was −0.333 (95% CI: −0.51, −0.16; p < .001), with a Q score of 16.95 (p = .075), indicating that removal of Sorenson (2003) decreased the level of heterogeneity to nonsignificance. However, because the Q statistic is influenced by the number of studies and/or large within-study variance, a nonsignificant p value does not mean that the effect sizes are homogeneous across studies (Borenstein, Hedges, Higgins, & Rothstein, 2009). The I2 statistic showed that a large proportion of variance (41%) remained attributable to between-study variation. Sorenson (2003) was therefore included in the subsequent moderator analyses. Results of moderator analyses conducted without this study did not differ substantively from results of analyses that included this study.
TABLE 4.
Summary Statistics Regarding Loneliness Interventions
| Study Type | N | Mean effect size (SE) | 95% C.I. of effect size | Z-score | Q test for homogeneity (p value) | I2 (95% C.I.) | Characteristic |
|---|---|---|---|---|---|---|---|
| Single group, pre-post studies | 12 | −0.367 (0.096) | −0.55, −0.18 | −3.781 | 28.52 (< .01) | 61.43% (27.7%, 79.4%) | High between-study variance |
| Non-randomized group comparison studies | 18 | −0.459 (0.135) | −0.72, −0.20 | −3.400 | 20.89 (.23) | 18.63% (0, 53.6%) | Low between-study variance |
| Randomized group comparison studies | 20 | −0.198 (0.062) | −0.32, −0.08 | −3.182 | 21.65 (.30) | 12.25% (0, 47.53%) | Approaching no between-study variance |
Figure 2. Effect size distribution: Single-group pre-post design (n = 12).
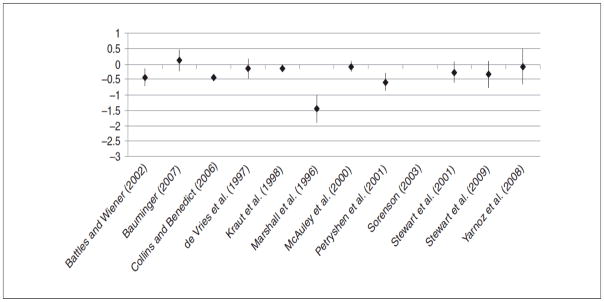
Note: To make the graphs comparable, the y-axis was set at (1.0 to −3.0). The result from one study with a larger effect size (−4.81) is therefore not fully demonstrated in this graph (Sorenson, 2003).
The first moderator examined was intervention type. Mean effect sizes were significant for all three types of intervention.10 The subgroup analyses indicated no difference in mean effect size (Qb= 2.65, df= 2, p> .2) among intervention types. Therefore, intervention type failed to explain the difference in effect size among the pre-post studies. Tests of moderation by intervention format and mode were not conducted because most of the single group pre-post studies implemented a group-based format (nine out of twelve studies) and a non-technological mode of delivery (ten out of twelve studies). A test of moderation by type of loneliness measure revealed a significant difference in mean effect size among loneliness measures (Qb= 6.62, df= 1, p= .01): studies using the UCLA Loneliness Scale showed a mean effect size of −0.499 (N=8; 95% CI: −0.74, −0.26; p < .001), whereas studies that used non-UCLA loneliness measures had a mean effect size of −0.103 (N=4; 95% CI: −0.28, 0.08; p > .2). The gender and age composition of the sample, number of intervention sessions, and the duration of the intervention did not moderate the effect size among the single group pre-post studies.11
In sum, meta-analysis of the single group pre-post studies revealed that the interventions appeared to be highly effective in reducing loneliness. Design features and sample characteristics did not moderate the effect size, but studies that measured loneliness with the UCLA Loneliness Scale on average reported greater effect sizes than studies that used other loneliness measures.
Studies with a Non-Randomized Group Comparison Design
Eighteen studies met our criteria for non-randomized group comparisons design. In terms of the target population, two of the studies focused on children, two focused on young adults, and the remaining fourteen focused on individuals aged 60 years or older. The majority of the samples in this group consisted of more female than male participants, with only one study focused mainly on a male population. All four types of interventions were present in this group. The majority of the interventions in this group had a group-based format, and about one-third of the studies utilized technology in their interventions. The UCLA Loneliness Scale and the De Jong Gierveld questionnaire were administered by about the same number of studies, whereas three studies used other loneliness measures. The details of these studies are summarized in Table 2.
TABLE 2.
Non-Randomized Group Comparison Studies (N = 18)
| Authors | Enrollment Eligibility and Sample Size | Intervention Type and Duration | Effect Size (95% CI) | Intervention format | Intervention mode | Sample age | Sample % female | Loneliness Measure |
|---|---|---|---|---|---|---|---|---|
| (Allen-Kosal, 2008) | Children were recruited from six third-grade classrooms from four different elementary schools in Knox County, Tennessee. N=72. | Social skills training: Group 1 received pre-training in cooperative behavior and completed 8 weeks of cooperative learning activities. Group 2 completed 8 weeks of cooperative learning activities but received no pre-training. Group 3 received pre-training in cooperative behavior but did not complete cooperative learning activities. Group 4 was comprised of three classrooms and served as the control group. Intervention lasted for eight weeks. | −0.49 (−1.10, 0.13 ) | Group | NON-TECH | Third grade; mean=8 | Not reported | 24 item Loneliness and Social Dissatisfaction Questionnaire. |
| (Cohen et al., 2006) | Recruitment notices sent to senior centers or retirement communities requesting volunteers for a study to assess physical and mental health as well as involvement in activities. One notice sought singers for a chorale group while the other notice did not mention that activity. N=166. | Social access: Participation in a professionally conducted chorale in which there were weekly singing rehearsals as well as public performances several times during the intervention period. Duration of intervention was 30 weeks. Control group did not receive the intervention. | 0.06 (−0.27, 0.39 ) | Group | NON-TECH | Range not reported; mean=79 | 78% | 20 item UCLA Loneliness Scale. |
| (Evans, Werkhoven, & Fox, 1982) | Legally blind adults randomly selected from a register of over 500 blind veterans in Washington state. N=84. | Social support: Groups of 3 participants plus a facilitator participated in 8 weekly 1-hour group conference calls. Goals were provision of information about resources, problem solving within the group, development of camaraderie, and building confidence among group members. Control group did not receive the intervention. | −1.42 (−1.90, −0.95 ) | Group | TECH | 53–78 yrs; mean=62 | 7% | 20 item UCLA Loneliness Scale. |
| (Fokkema & Knipscheer, 2007) | Volunteer home visitors recruited Dutch seniors with chronic illness or a handicap who lived alone, had few opportunities to leave the home, and did not have a computer or Internet access. N=30. | Social access: Participants received on loan, free of charge, a personal computer with Internet access, monitor, speakers and a printer for three years. Participants were given five two-hour lessons at home on how to e-mail and how to use the Internet. Participants continued to be supported and coached by volunteers who made home visits. Control group did not receive any intervention. | −0.52 (−1.30, 0.26) | Individual | TECH | Range not reported; mean=66 | 92% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Fokkema & van Tilburg, 2007) | Inactive adults living on their own. Experimental group recruited through brochures and local newspapers. Control group recruited by approaching random older adults. N=72. | Social skills training: Seen Through Other Eyes. 6 weekly group training courses (2.5 hours per week) aimed at improving social skills and promoting an active lifestyle, co-led by professionals. | 0 (−0.49, 0.49) | Group | NON-TECH | Range not reported; mean=71 | 74% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Fokkema & van Tilburg, 2007) | Adults with physical or mental health problems and living on their own. Experimental group recruited through brochures, local newspapers, and invited by helpers. Control group recruited by postal questionnaire among homosexual older adults. N=52. | Social support: Buddy Care for Homosexuals. Social and/or emotional support visits by volunteer homosexuals aimed at enlarging social network and participation and improving self-management abilities. Home-based intervention of variable duration. | 0 (−0.55, 0.55) | Individual | NON-TECH | Range not reported; mean=67 | 40% | 11 item De Jong Gierveld loneliness questionnaire. |
| (van den Elzen & Fokkema, 2006) as reported in (Fokkema & van Tilburg, 2007) | Elderly adults living on their own and making use of extramural care. Sample was from register of care receivers. Experimental group contains those who are willing to participate whereas control group comprised of those who refused. N=52. | Social support: Elderly support home visits. Volunteer visits to assess social needs, followed by social and/or emotional support provision. Home-based intervention of variable duration. | 0 (−0.55, 0.55) | Individual | NON-TECH | Range not reported; mean=79 | 71% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Fokkema & van Tilburg, 2007) | Adults in residential care for the elderly. Experimental group selected from list of interested residents and invited by caretakers. Control group recruited through self-selection (i.e., those who were not interested in the intervention). N=71. | Social support: Group Activities in Residential Homes. Network building encouraged through group trips and eight group meetings by new residents co-led by professionals. No information on the length of the intervention. | 0 (−0.56, 0.56) | Group | NON-TECH | Range not reported; mean=84 | 86% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Fokkema & van Tilburg, 2007) | Adults in residential homes for the elderly. Experimental group included all residents of two homes for the elderly. Control group included all resident of a different home for the elderly. N=116. | Social support: Institutional Interventions in Residential Homes. Network building encouraged through group training course for caregivers focused on topics related to loneliness and systematic information provision. Co-led by professionals. Duration of intervention was 6 months. | 0 (−0.39, 0.39) | Group | NON-TECH | Range not reported; mean=84 | 71% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Hartke & King, 2003) | Eligibility included 60 years or older, married or spousal equivalent and living with a stroke survivor as the primary caregiver for a minimum of 1 month, not currently in a caregiver support group, and had a telephone in the home. Recruitment occurred through review of spouse’s admission records, media advertisements, and community outreach. N=88. | Social cognitive training: Eight weekly 1-hour telephone conference calls with 2 clinician-facilitators. Each participant received a manual, which outlined 8 topics, including facts about stroke and care-giving, communicating with one’s spouse, dealing with spouse’s problematic feelings and behaviors, stress as a caregiver, taking care of oneself as a caregiver, community resources for caregivers, and goal setting. Manual also included an audiotape of a relaxation procedure and a publication on stress management. Control group received the same manual but did not participate in conference calls. Duration of intervention was 8 weeks. | −0.18 (−0.60, 0.24) | Group | TECH | Range not reported; mean=70 | 74% | 10 item UCLA Loneliness Scale. |
| (Hopps, Pepin, & Boisvert, 2003) | Community-living Canadian adults with physical disabilities were recruited via announcements posted on bulletin boards and placed in various mailings to associations for people with physical disabilities and neurological disease. N=19. | Social cognitive training: Using home computers or computers in rehabilitation center, each participant completed 12, two-hour group cognitive behavioral sessions via synchronous, text-based Inter Relay Chat. During each session, participants examined the nature of and factors involved in their loneliness, determined ways of reducing loneliness, assessed various loneliness-reducing actions, and shared experiences in learning from others. Control group did not receive the intervention initially. | −1.84 (−2.92, −0.77) | Group | TECH | Range not reported; mean=34 | 53% | 20 item UCLA Loneliness Scale. |
| (Kolko, Loar, & Sturnick, 1990) | Children with conduct or developmental disorders admitted to a 24-bed child psychiatric unit in a U.S. hospital. Eligibility based upon scores from a four-item social problems screen for interpersonal difficulties (e.g. rejection, social skill deficiencies). Children who received a score of at least 7, with at least one maximum rating were eligible. N=56. | Social skills training: Intervention consisted of 15 one-hour, small group sessions which emphasized skill development in gaze, physical space, voice volume and inflection, compliments, conversational openers, assertive requests, appropriate responses to provocation, and appropriate play and sharing with others. Control consisted of 15 one-hour, small group sessions which offered semi-structured opportunities for socialization in the context of age- and developmentally appropriate group activities, games, and tasks. | −1.49 (−2.10, −0.88) | Group | NON-TECH | Range not reported; mean=10 | 32% | 24 item Asher Loneliness Scale. |
| (Martina & Stevens, 2006) | Recruited by senior service agencies in four Dutch communities using local newspaper articles and publicly distributed printed material. N=60. | Social skills training: 12 weekly small group lessons with a mean of 10 participants per group. Investigator-led lessons focused on theory of friendship enrichment, practice in skills important in friendship, and role playing. Control group was placed on an intervention waiting list and received no intervention during the initial study period. | −0.06 (−0.42, 0.31) | Group | NON-TECH | 53–86 yrs; mean=63 | 100% | 11 item De Jong Gierveld loneliness questionnaire. |
| (Rosen & Rosen, 1982) | Directors of six senior centers in Georgia identified community-dwelling individuals who seemed depressed, had experienced recent traumas, gave evidence of approaching senility, or gave other indications that they might benefit from mental health counseling. Comparison group included seniors at two other senior centers who were in need of mental health services but did not have access to those services. N=68. | Social support: Meetings typically began with a discussion of happenings during the previous week. Intervention staff encouraged sharing of past experiences and current feelings as well as interactions among members between group sessions. In total, there were 40 to 49 two-hour weekly sessions over a period of 12 to 15 months. | −0.37 (−0.89, 0.15) | Group | NON-TECH | 65+ yrs; median=70 | 80% | Participants were asked if they were seldom/never lonely. |
| (Seepersad, 2005) | Students recruited on a college campus via fliers, brochures, and e-mails and who reported frequent loneliness, no severe current psychopathology, no unresolved trauma history, and who had a capacity to function as a group member. N=16. | Social skills training: Each week for 7 weeks, participants were given written educational materials and assignments regarding various theories and ideas associated with loneliness. Groups of 7–9 participants met weekly with a program facilitator for 2 hours. Meetings focused on developing and practicing listening and communication skills. Participants were also asked to keep a journal every week. Control group did not receive intervention. | −0.37 (−1.05, 0.31) | Group | NON-TECH | Range not reported; mean=21 | 74% | 20 item UCLA Loneliness Scale. |
| (Shapira, Barak, & Gal, 2007) | Community- and nursing home-dwelling Israeli seniors who had sufficient cognitive ability to participate in the offered activities. N=22. | Social access: Computers were placed in common rooms in outpatient senior centers and nursing homes. Participants received in-person, small group computer, Internet, and e-mail training and were encouraged to use the computers and Internet between training sessions. Program lasted 15 weeks and included one or two 60 minute lessons per week. Comparison group took part in other group activities, including painting, sewing, needlework, and ceramics. | −1.99 (−2.81, −1.17) | Group | TECH | 70–93 yrs; mean=82 | 82% | 20 item UCLA Loneliness Scale. |
| (White et al., 1999) | Recruited from a U.S. retirement community which included independent living, assisted living, and skilled nursing care facilities. Participants willing to commit 4–6 hours per week for 4 months were placed in the intervention group. Individuals who showed initial interest but declined to enroll due to scheduling conflicts were placed in the comparison group. N=23. | Social access: Computer consultant provided 9 hours of instruction on use of the computer, e-mail, and the Internet. Three computers were available to participants at all times in a common area. Help desk was available 3–4 hours/week for first 2 months then 1 hour/week for last 3 months. Duration of program was 5 months. Control group did not receive the intervention and did not use the computers during the study. | −0.51 (−1.39, 0.36) | Individual | TECH | Range not reported; mean=78 | 84% | 20 item UCLA Loneliness Scale. |
| (Winningham & Pike, 2007) | Institutionalized older adults were recruited from 6 U.S. assisted living facilities. | Social cognitive training: Intervention group participants attended 3 small group meetings per week for 3 months. Meetings were designed to educate participants about the brain and memory, stimulate memory and cognitive activity and focus on making new memories. Activities were designed and conducted in order to facilitate social interactions and develop social support networks. Control group did not participate in small group meetings. | −0.31 (−0.82, 0.21) | Group | NON-TECH | 61–98 yrs; mean=82 | Inferred as 80% | 20 item UCLA Loneliness Scale. |
Effect sizes ranged from −1.88 to 0.11 for this group of studies, with fourteen of the effect sizes having confidence intervals that included zero, whereas the remaining four appeared highly effective in reducing loneliness. As is shown in Table 4, the mean effect size for these eighteen studies was −0.459 (95% CI: −0.72, −0.20; p < .01). The distribution of effect sizes is displayed in Figure 3. The between-study variance in effect size was estimated as T2 = 0.08. The Q test did not reject the null hypothesis of homogeneity (Q = 20.89, p = .23), but the I2 showed that 19% of the variation was attributable to between-study variance. Because the Q statistic has low power to detect heterogeneity when the sample size is small, moderator analyses were conducted to prevent premature conclusions.
Figure 3. Effect size distribution: Nonrandomized group comparison design (n = 18).
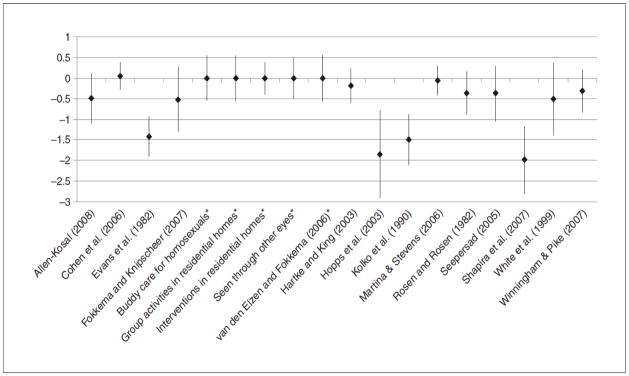
Note: Studies marked with an asterisk were listed in the unpublished English translation of C. M. Fokkema and van Tilburg (2007).
Subgroup analyses showed no difference among the four intervention types (Qb= 0.85, df= 3, p> .8). In addition, the four aforementioned highly effective studies fell into four distinct intervention types and thus confirmed that, among the non-randomized group comparison studies, the intervention type was not the dominant factor contributing to the difference in effect sizes. For intervention format, group-based interventions on average had larger effect sizes than individual-based interventions,12 but the difference was not statistically significant (Qb= 2.51, df= 1, p> .1). On the other hand, the utilization of technology showed a significant moderating effect (Qb= 5.71, df= 1, p= .02). The mean effect size of the interventions that used technology was −1.04 (N=6; 95% CI: −1.68, −0.40; p < .01), as opposed to an effect size of −0.21 (N=12; 95% CI: −0.43, 0.01; p = .05) in studies that didn’t use any kind of technology in the intervention. The instrument used to measure loneliness was significant in differentiating effect sizes (Qb= 9.64, df= 2, p< .01), with the De Jong Gierveld questionnaire producing the smallest mean effect size.13 Follow-up analysis revealed that studies that used the De Jong Gierveld questionnaire, for example (van den Elzen & Fokkema, 2006), reported significantly smaller effect sizes than studies with either UCLA or other loneliness measures (Qb= 9.65, df= 1, p< .01). The gender and age composition of the samples were also significant moderators of the effect size. Percentage of females in the sample was negatively correlated with the effect size (β=1.59, Z=3.15, p< .01): the more females in the sample, the less loneliness reduction was observed. Mean age of the sample was negatively correlated with the effect size (β=0.01, Z=1.93, p= .05), but the effect was small. Neither the intervention duration14 nor the number of sessions had a moderating influence on the effect size. Follow-up analysis with all the individually significant moderators (gender, age, technology, and loneliness measure) in one regression model showed that only the utilization of technology consistently showed a moderating effect (β=−5.60, Z=−2.28, p= .02).
In sum, meta-analysis of the non-randomized group comparison studies suggested a significant intervention effect on loneliness. Utilization of technology had a moderating effect on effect size independent of effect size differences associated with gender, age, and type of loneliness measure used.
Studies with a Randomized Group Comparison Design
Twenty studies met our criteria for randomized comparison design. In terms of the target population, one study focused on children, three focused on young adults, six studies focused on middle-aged adults, and the remaining eleven studies focused on individuals aged 60 years or older. Seven studies in this group included only female participants and one study included only male participants. Eight of the remaining thirteen studies had more female than male participants. All four types of interventions were present in this group. An equal number of studies used group-based and individual-based formats, and about one-third of the studies utilized technology in their interventions. The UCLA Loneliness Scale was used in thirteen of the twenty studies, whereas two studies administered the De Jong Gierveld questionnaire and five used other loneliness measures. The details of these studies are summarized in Table 3.
The effect sizes in this group ranged from −0.79 to 0.40, with six studies reporting efficacy in reducing loneliness (Banks, Willoughby, & Banks, 2008; Chiang et al., 2009; McWhirter & Horan, 1996; Ollonqvist et al., 2008; Samarel, Tulman, & Fawcett, 2002; Williams et al., 2004). The remaining fourteen studies showed no change in loneliness as indicated by 95% confidence intervals that included zero. However, as is shown in Table 4, the mean effect size for these twenty studies was −0.198 (95% CI: −0.32, −0.08; p < .01). The distribution of effect sizes is displayed in Figure 4. A forest plot that includes the mean effect size with the addition of each successively smaller study (Figure 5) demonstrates that the smaller studies exerted little bias and shifted the effect size only somewhat to the left (i.e., a greater reduction in loneliness). Orwin’s (1983) fail-safe N indicated that 374 null studies would be required to reduce the effect size to −0.01 (an effect that is substantively equivalent to 0) (Orwin, 1983).
Figure 4.
Effect size distribution: Randomized group comparison design (n = 20)
Figure 5. Forest plot showing results of cumulative meta-analysis of randomized group studies.
Note: The mean effect size (and 95% CI) is recalculated with the addition of each successively smaller study.
The between-study variance in effect size in the group of randomized group comparison studies was estimated as T2 = 0.01. The Q test did not reject the null hypothesis of homogeneity (Q= 21.65, p = .30), and the I2showed that only 12.25% of the observed variance was attributable to between-study variance. However, because the upper confidence interval for I2 approached 48%, and for comparability with prior analyses, moderator analyses were conducted.
The analog to the ANOVA test revealed that the difference among intervention types was significant (Qb= 7.73, df= 3, p= .05), and the four social cognitive training interventions (Chiang et al., 2009; Conoley & Garber, 1985; McWhirter & Horan, 1996; Williams et al., 2004) yielded greater loneliness reduction (mean effect size = −0.598, p = 0.001) compared to the twelve interventions to enhance social support (mean effect size = −0.162, p = 0.003), the two interventions to improve social skills (mean effect size = 0.017, p = 0.90), and the two interventions to increase opportunities for social interaction (mean effect size = −0.062, p = 0.67). In addition, the mean effect size of the social support interventions did not differ significantly from the mean effect sizes of the social skills or social access interventions.
Neither group-based format nor the use of technology showed any moderating effects on the effect size.15 In addition, the instrument used to measure loneliness did not moderate the effect size (Qb= 3.60, df= 2, p> .1).16 The weighted regressions with each continuous moderator as the independent variable revealed that only gender composition had a moderating influence on the effect size.17 Studies with more females in the sample showed a smaller reduction in loneliness. In summary, meta-analysis of the randomized group comparison studies revealed a small but significant effect of the interventions on loneliness. Of note, interventions which addressed maladaptive social cognition had a sizeable mean effect compared to the other intervention types.
Discussion
Qualitative reviews of loneliness reduction interventions have identified diverse study designs (e.g., single group pre-post studies, non-randomized group comparisons, and randomized group comparisons) and intervention strategies (e.g., improving social skills, enhancing social support, increasing opportunities for social interaction, and addressing abnormal social cognition). Five of the six prior reviews, all of which were qualitative, concluded that certain interventions could reduce loneliness, although each review concluded that increased rigor was needed in evaluation of loneliness interventions.
The current study used meta-analytic techniques to determine quantitatively whether the outcomes of loneliness interventions varied based upon study design, intervention type, or other study characteristic. Compared to single group pre-post and non-randomized group comparison studies, randomized group comparison studies had a small but significant mean effect size (−0.198, p<0.05). Within this group, the mean effect size for interventions which addressed maladaptive social cognition was larger than that for intervention which attempted to improve social skills, enhance social support, or increasing opportunities for social interaction. A primary criterion for empirically supported therapies is that they demonstrate efficacy in randomized controlled trials (Chambless & Hollon, 1998). By this criterion, our meta-analysis suggests certain interventions, particularly those which use cognitive behavioral therapy, can reduce loneliness.
Although the single group pre-post studies and non-randomized group comparisons exhibited larger mean effect sizes compared to the mean effect of randomized group comparisons, our confidence in the former studies is tempered. One reason is that single group pre-post studies are vulnerable to regression toward the mean, in which individuals who have high scores on a loneliness measure on one occasion are likely to score less extremely on a second occasion even if no intervention had occurred (Weeks, 2007). A second reason why results of pre-post studies should be viewed with caution is that loneliness may serve its adaptive purpose and motivate reconnection with others such that the group, on average, improves over time without intervention. Our meta-analysis of these studies indicated there was indeed a lowering of loneliness as measured before and after the interventions, but whether this result was due to the interventions, regression toward the mean, or the adaptive function of loneliness cannot be determined.
Non-randomized group comparison studies also have important design flaws, including regression toward the mean and selection bias. Selection bias occurs when assignment of individuals to the experimental or control group is not random but is based upon convenience, participant preference, or some other factor. When this occurs, individuals in the treatment arms may differ from individuals in the control arms in ways that affect the outcome of the studies. For example, people who volunteer to be in the treatment arm of a loneliness reduction study may be more gregarious by nature and may be more likely to become less lonely over time regardless of their exposure to the intervention. As a result, although our results suggest that non-randomized group comparison interventions might be effective, it cannot be determined whether this finding is due to the interventions or to a combination of regression toward the mean and selection bias.
In contrast, randomized group comparison studies eliminate selection bias and minimize the effect of regression toward the mean. The plurality of the intervention studies in our meta-analysis were randomized group comparison studies and the mean effect size in this group (−0.198) was significantly different from zero. To interpret this effect size in familiar units, the 6 randomized studies that used the 20-item UCLA Loneliness Scale and reported loneliness means and SD’s were further evaluated (Chiang et al., 2009; Coleman et al., 2005; Conoley & Garber, 1985; Hill, Weinert, & Cudney, 2006; Jessen, Cardiello, & Baun, 1996; Samarel, Tulman, & Fawcett, 2002). Using formulas provided by Lipsey & Wilson (2001), the pooled mean (41.17) and SD (8.05) for the control groups were calculated. With an intervention effect size of −0.198, the average treatment group scored 0.198 SDs lower in loneliness, which is equivalent to 8.05*0.198 = 1.59 units on the UCLA Scale. Thus, with the control group mean at 41.17, the reduction in loneliness in the average treatment group was equivalent to a decrease from 41.17 to 39.58 on the UCLA Loneliness Scale. By comparison, a previous survey of 301 healthy, community-living individuals over age 65 yielded a mean UCLA Lonelines Score of 31.5 with a SD of 6.9 Because clinical significance is defined as “returning to normal functioning” (Jacobson, Roberts, Berns, & McGlinchey, 1999), a 1.59 point decrease in the UCLA Loneliness score clearly did not return study participants to the level of healthy, community-living individuals. Moreover, a meta-analysis of 302 social and behavioral intervention meta-analyses (reviewed in (Lipsey & Wilson, 2001)) showed that, on average, interventions in this field have generated a mean effect size of 0.50. A mean effect size of −0.198 falls in the bottom 15% of this distribution, suggesting that loneliness interventions to date have not attained the degree of efficacy achieved by interventions targeting other social and behavioral outcomes.
On the other hand, despite not returning to the level of healthy, community-living adults, the small reduction in loneliness score is consistent with the notion of “improved but not recovered” (Jacobson, Roberts, Berns, & McGlinchey, 1999). Additionally, the mean effect size of the four randomized group comparisons that addressed abnormal social cognition was −0.598, which is comparable to the mean effect size found by Lipsey & Wilson (2001) for over 300 social and behavioral meta-analyses. We did not convert the mean effect size of social cognition interventions to a reduction in the UCLA Loneliness Scale because there were only four studies of this type. Whereas well-designed loneliness reduction interventions achieved only modest success on average, interventions that address abnormal social cognition show promise in reducing loneliness. This result is consistent with the important role that social cognition plays in the development and persistence of loneliness (Cacioppo, Fowler, & Christakis, 2009; Cacioppo & Hawkley, 2009; Hawkley, Preacher, & Cacioppo, 2007). The surprisingly small effects of interventions to increase opportunities for social interaction or enhance social support suggests that reducing social isolation does not necessarily reduce loneliness. Nevertheless, the causes of loneliness are likely unique in each person and matching specific therapies with specific interventions is worth further investigation and may prove valuable in future studies.
The reliable change index (RCI) was used to determine the reliability of a 1.6 point change in the UCLA Loneliness Scale (Jacobson & Truax, 1991). This index ensures that the degree of change is of sufficient magnitude to exceed the margin of measurement error. As such the RCI is calculated as the post-test score minus the pre-test score, divided by the standard error of the difference between these two scores. Using this formula, as well as 8.1 as the standard deviation for the experimental group posttest and .7 as the test-retest reliability of the measure, the RCI of a 1.6 point reduction in the UCLA Loneliness Scale is 0.26. Values exceeding 1.96 are considered to be in the “recovered” zone, so with an RCI of 0.26, the most we can say is that these interventions achieve, at best only modest improvement but not recovery. Thus, there is a need for improvements in interventions to reduce loneliness if clinically significant improvements are to be achieved.
Are there particular intervention types, formats, modes, or population characteristics that make some interventions more likely to succeed than others? Authors have suggested that interventions that enhance opportunities for social interaction via group activities or group-based interventions tend to be more successful (Cattan & White, 1998; Cattan, White, Bond, & Learmouth, 2005). However, simply bringing lonely people together may not result in new friendships because the thoughts and behaviors of lonely individuals makes them less attractive to one another as relationship partners (Jerrome, 1983; Stevens, 2001). To determine whether group-based interventions or other interventions characteristics moderated study efficacy, effect sizes in each study design group were first subjected to a test of homogeneity. This analysis revealed that the percent of variance that could be attributed to between-study variation declined going from single group, to non-randomized comparison, to randomized comparison studies (61.43% to 18.63% to 12.25%). A significant Q statistic indicated heterogeneity of effect sizes among the single group pre-post studies. However, the Q statistic was not significant for the non-randomized and randomized group comparison studies. Because this statistic has low power to detect heterogeneity in small sample sizes, moderator analyses within each design type were conducted.
Intervention type as a moderator in single group pre-post studies was examined first. Although effect sizes varied widely in these studies, intervention type did not explain this difference. In other words, increasing opportunities for social interaction was not more effective than enhancing social support or addressing abnormal social cognition. Because none of the single group pre-post studies utilized social skills training, the hypothesis that this intervention can increase intervention success could not be tested. The effect sizes varied much less in the non-randomized and randomized comparison studies and moderator analyses revealed intervention type did not explain what little variation existed. These analyses therefore revealed that intervention type was not important to study outcome, even among the single group pre-post studies that differed widely in effect size. This result runs counter to previous speculation that increasing opportunities for social interaction may be more effect than other interventions. Moreover, these results also do not support the suggestion that social cognitive training or social skills training are more effective than social access or social support in reducing loneliness, at least in adults.
Most of the single group pre-post studies utilized a group-based format and did not include a technology-based component. Therefore moderator analyses were not performed using these variables in single group studies. In contrast, both the non-randomized and randomized group comparison studies utilized a greater variety of intervention formats and modes and were therefore subjected to moderator analyses using these variables. Among both the non-randomized and randomized group comparison studies, group-based interventions were no more effective than individual-based interventions. In contrast, the use of technology-based interventions was associated with greater efficacy among the non-randomized studies. The reason for this is not clear but may be due to selection bias. Specifically, when randomization is not present, those who receive the intervention may be more predisposed to loneliness reduction compared to those who do not. Results from the randomized studies support this hypothesis as the presence of a technology component did not enhance their effect size. Stated another way, random assignment effectively removed the apparent advantage of the technology component. This finding is somewhat disappointing as technology-based interventions have been helpful in managing other chronic diseases (Celler, Lovell, & Basilakis, 2003; Gaikwad & Warren, 2009). Our results indicate that loneliness reduction interventions have yet to harness the power of technology.
Of note, studies that used the UCLA Loneliness Scale showed greater reductions in loneliness compared to studies that used other loneliness measures. This was true for the single group pre-post studies and the non-randomized group comparison studies but not for the randomized group comparison studies. The reason for this may be uninteresting. Of the 50 studies analyzed, 6 were from the Fokkema & van Tilburg (2007) paper. All of these studies used the De Jong Gierveld Loneliness Questionnaire and all were solicited from diverse public and private organizations as pilot studies, in contrast with the more focused professionally-led studies that used the UCLA Loneliness Scale. Many of the latter found large effect sizes, especially among the single group pre-post studies. Other explanation are also possible, including a longer duration of the U.S. interventions (which primarily used the UCLA Loneliness Scale) compared to pilot studies in the Netherlands (which used the De Jong Gierveld Loneliness Questionnaire), as well as cultural differences in perceptions of loneliness treatment in the two countries. These explanations may be moot, however, as no differences in effect size were found as a function of loneliness measure in the randomized group comparison design.
In the non-randomized group comparison studies, participant age and proportion of female participants were inversely related to effect size whereas the intervention duration and number of sessions did not have a moderating effect. These relationships were generally not present in the single group pre-post test or the randomized group comparison studies. This inconsistency is difficult to explain but may be due to selection bias in which, for example, especially lonely older individuals volunteered to be in the treatment arm of the studies among elders, thereby blunting the effect of the treatment. The lack of association between effect sizes and age or intervention duration among the 20 randomized group comparison studies supports the notion of selection bias as an explanation among non-randomized studies. As shown in Table 3, there was significant variation in duration of intervention, ranging from ten days to 8 months.
On the other hand, the gender composition of the sample moderated the effect size in both the non-randomized and the randomized group comparison studies. The greater the proportion of males in the study, the greater the effect of the intervention. Said differently, males were more responsive to the interventions than females. In the case of the non-randomized studies, one could argue that women with more resistant forms of loneliness may have been drawn to studies with higher proportions of women. The fact that this gender difference was also observed in the randomized studies suggests a different interpretation. Females tend to be more self-reliant than males in finding and maintaining meaningful social relations, and interventions may therefore be more impactful in assisting males to forge a sense of connectedness and belonging. Conversely, the majority of participants in the randomized studies were older. Of the 20 randomized studies, 11 included adults aged 60 years and older, six included middle-aged adults, and only one included children. Given the disproportionate rates of widowhood among older women compared to older men, it is likely that many of the female study participants were widowed. Therefore loneliness among widowed females may be more intransigent if they have failed to meet their social needs despite their stereotypical advantage in forming meaningful social relationships. This issue requires further examination to determine whether marital status-or gender-specific therapies are indicated.
An important finding of the randomized group comparison studies is that the four interventions that addressed maladaptive social cognition yielded greater reductions in mean loneliness scores compared to the other intervention types. Although none of studies that addressed social cognition utilized precisely the same intervention, all included a form of cognitive behavioral therapy or psychological reframing. Therefore, these studies begin to fulfill the criterion that the intervention be replicated by independent research groups in order to be considered empirically supported (Chambless & Hollon, 1998). The twelve studies that enhanced social support were associated with a much smaller effect size and this effect did not differ from those of interventions that focused on social skills development (n = 2) or increased opportunities for social interaction (n = 2).
Limitations
The current study is at risk for the same limitations as other systematic reviews. Namely, despite a concerted effort, it is possible that our literature search failed to identify one or more interventions that met our study criteria. As mentioned above, this would only be important if such interventions were randomized group comparisons and showed non-significant treatment effects. Compared to studies with positive results, those with negative results are less likely to be published. Exclusion of studies due to the “file drawer” effect would weaken the conclusion that loneliness interventions have met with some success. However, our analyses indicated that as many as 374 null results would be needed to abolish the significant effect found here. A second potential limitation is our use of studies either published in English or described by an English translation of a Dutch review (Fokkema & van Tilburg, 2007). It is possible that randomized group interventions published in non-English journals demonstrated greater efficacy in reducing loneliness and that the intervention effect was therefore underestimated. Also, although our literature search did not exclude any age groups, only five studies evaluated interventions in children and only 19 studies evaluated interventions among adults less than age 60 years. Therefore, the extant literature on loneliness speaks most clearly to interventions among older adults.
In addition, studies in this meta-analysis did not distinguish between social and emotional loneliness. Although various studies have provided evidence that the experience of loneliness can be partitioned into separable dimensions, including social and emotional loneliness (Weiss, 1973), these features have also been found to be highly correlated and their antecedents and consequences have been found to be sufficiently overlapping that loneliness is generally conceptualized and measured as a unidimensional construct (Hawkley, Browne, & Cacioppo, 2005; Russell, 1996; Russell, Peplau, & Cutrona, 1980). Because measures of social and emotional loneliness were typically not provided by the studies in this meta-analysis, the effect of various interventions on these dimensions of loneliness was not evaluated. Measurement of these dimensions in future interventions may permit investigators to determine whether certain interventions are more successful in reducing social versus emotional loneliness.
Conclusion
This report is the first to analyze loneliness reduction strategies in a quantitative manner. Previous reviews noted the dearth of well-designed intervention studies but found evidence that specific interventions showed promise in reducing loneliness. These included programs to improve social skills, enhance social support, increase opportunities for social interaction, and address deficits in social cognition. Importantly, intervention type did not differ across study design; each of these strategies was implemented in each of various study design types, including single group pre-post evaluations, non-randomized group comparisons, and randomized group comparisons. A consensus existed in the literature that these interventions were successful across the array of study designs, and our meta-analysis revealed that success was achieved in all three study design types. Given their design superiority, our analysis focused primarily on randomized group comparison studies and found a small but statistically significant effect of loneliness reduction interventions in this group.
Moderator analysis demonstrated that, among the randomized studies, interventions that addressed maladaptive social cognition had a larger mean effect size compared to interventions that addressed social support, social skills, and opportunities for social intervention. This result is consistent with our model of loneliness as regulatory loop (Cacioppo & Hawkley, 2009), in which lonely individuals have increased sensitivity to and surveillance for social threats, preferentially attend to negative social information (Cacioppo, Norris, Decety, Monteleone, & Nusbaum, 2009), remember more of the negative aspects of social events (Duck, Pond, & Leatham, 1994), hold more negative social expectations (Cacioppo & Hawkley, 2005), and are more likely to behave in ways that confirm their negative expectations. This loop has short-term self-protective features but over the long-term, heightens cognitive load, diminishes executive functioning, and adversely influences physical and mental health and well-being. Among the four intervention types, addressing maladaptive social cognition most directly addresses this regulatory loop. Therefore, our results shed light on the nature and mechanisms underlying loneliness and are consistent with the latest theories regarding this condition.
As for future directions, the recommendation of previous review authors to improve study design should be heeded. However, while randomized group comparisons provide the most internally valid results, non-randomized studies can provide valuable insights. Investigators will have to consider whether randomized studies, which place lonely individuals into the usual care or wait-list group is ethical, especially given the potential negative health effects of untreated loneliness. Future interventions should also incorporate current understanding regarding the nature of loneliness. Of primary importance is an acknowledgment that loneliness is not equivalent to social isolation. Loneliness is the social equivalent of physical pain and, like physical pain, is functional in motivating individuals to alleviate the social pain by seeking out the connections they need to feel safe, secure, and content with life. For individuals who have a rich and forgiving social environment, loneliness has a high probability of accomplishing its purpose of motivating interactions and enhancing a sense of connectedness and belonging. For other individuals, however, loneliness becomes inescapable, and it is for these individuals that interventions are perhaps most necessary. Results from this meta-analysis suggest that correcting maladaptive social cognition offers the best chance for reducing loneliness. Given that temporal trends are placing an increasing number of individuals at risk for this condition, it is critical that results of this study be considered when designing interventions to address the potentially rising tide of loneliness.
Acknowledgments
We thank those primary article authors who provided us with the requested information for the meta-analysis. We also thank Benjamin Pomper for his assistance with the literature review. This work was supported by a National Institute on Aging Career Development Award K08 (AG027200, principal investigator C.M. Masi), a National Institute on Aging R01 (AG036433, principal investigator L.C. Hawkley), and a National Institute on Aging R01 (AG034052, principal investigator J.T. Cacioppo).
Financial Disclosure/Funding
The authors received no financial support for the research and/or authorship of this article.
Footnotes
For studies that reported sample age only as a threshold (e.g., 75 years or older), the threshold age was used as the mean age of the sample: Banks and Banks (2002).
Allen-Kosal (2008): sample was 3rd grade children, the mean age was inferred to be 8 years old. Banks et al. (2008): sample was institutionalized elderly people, the mean age was inferred to be 75 years old; Bauminger (2007): sample age ranged from 7 years and 7 month to 11 years and 6 month, the mean age was inferred to be 9 years old; Conoley and Garber (1985): sample was college students, the mean age was inferred to be 20 years old; Hill et al. (2006): sample age ranged from 35 to 65 years old with 92% over 40 years old, the mean age was inferred to be 52 years old. Kraut et al. (1998): sample was 93 families with both teens and adults, the mean age was not calculated due to the heterogeneous nature of the sample.
Banks et al. (2008) and Winningham and Pike (2007) did not report the gender composition of their samples. However, because their samples were both institutionalized older adults, we inferred the gender composition to be 80% female, the same as reported for an institutionalized sample in Banks and Banks (2002).
Marshall et al. (1996), and three studies listed in Fokkema (unpublished): (1) Buddy care for homosexuals, (2) Elderly support home visits, and (3) Group activities in residential homes.
Four studies did not provide information on intervention frequency: Marshall et al. (1996), and three studies listed in Fokkema (unpublished): (1) Buddy care for homosexuals, (2) Elderly support home visits, and (3) Good company in a big home. Five had interventions that provided computer/internet access thus no exact number of intervention sessions available: Fokkema and Knipscheer (2007), Hill et al. (2006), Kraut et al. (1998), White et al. (1999), White et al. (2002). Three studies had intervention frequencies that varied among participants: Stewart et al. (2009), due to the unpredictable nature of homeless youth; Petryshen et al. (2001), because participants were offered a choice from about 200 group activities; and Morrow-Howell et al. (1998), due to different level of needs and suicide risks of their sample. Two studies had interventions that were in effect continuously for a period of time and thus couldn’t be quantified into sessions: Jessen et al. (1996), who placed a caged bird in participants’ rooms for 10 days; Ollonqvist et al. (2008), who implemented an intervention that included three separate inpatient periods over eight months.
Other loneliness measure included: 1) 15 item Emotional/Social Loneliness Inventory (Vinconzi & Grabosky 1987) used in Stewart et al. (2001); 2) 15 item short version of the Social and Emotional Loneliness Scale for Adults (DiTommaso, Brannen, & Best 2004) used in Yárnoz et al. (2008); 3) 16 item Loneliness Scale (Asher et al. 1984) used in Bauminger (2007) and Christian & D’Auria (2006); 4) 24 item Loneliness Scale (Asher & Wheeler 1985) used in Kolko et al. (1990) and Allen-Kosal (2008); 5) 7 item loneliness scale (Paloutzian and Ellison 1982) used in Heller et al. (1991); 6) Philadelphia Geriatric Center Morale Scale (6 items on loneliness) used in Cox et al. (2007); 7) Frequency of loneliness (OARS Social Resource Rating Scale) used in Morrow-Howell et al. (1998); 8) Single question asking the participants if he/she feels lonely used in Rosen &Rosen (1982) and Ollonqvist et al. (2008).
Hopps et al. (2003) and Shapira et al. (2007) reported one-way ANOVA F statistics; Morrow-Howell et al. (1998), White et al. (2002), & Williams et al. (2004) reported t-test statistics; Rosen & Rosen (1982) reported Chi-Squared statistic;.
In Banks & Banks (2002), the effect size was obtained from a one-way ANCOVA with the pre-test loneliness score as a covariate, and in Savelkoul et al. (2001) the effect size was calculated by the authors from a multivariate regression model with pre-test loneliness and self-reported functional health as covariates.
Five of these six largest effect sizes were from the delayed post-treatment measures of the primary interventions reported in our analyses. In Allen-Kosal (2008), the largest effect size was from an alternative intervention which contains only the pre-training component of the full intervention.
There is no social skills training intervention in this group of studies. Mean effect size of the social cognitive training interventions is −1.58 (N=3; 95% CI: −3.18, 0.02; p= .053) as opposed to −0.340 (N=5; 95%CI: −0.49, −0.19; p< .001) for social support interventions, and −0.273 (N=4; 95% CI: −0.48, −0.07; p< .01) for social activity/access interventions.
Gender composition of the sample (β=−0.16, Z=−0.43, p> .6); mean age of the sample (β=−0.002, Z=−0.29, p> .7); intervention duration (β=−0.001, Z=−0.26, p> .7); number of intervention sessions (β=−0.007, Z=−1.30, p= .20).
Mean effect size for group-based interventions was −0.53 (N=14; 95% CI: −0.85, −0.21; p < .01); for individual-based interventions was −0.16 (N=4; 95% CI: −0.49, 0.16; p > .3).
Mean effect size for studies that used the UCLA scale was −0.75 (N=8; 95% CI: −1.27, −0.24; p < .01), for the De Jong Gierveld group was −0.04 (N=7; 95% CI: −0.23, 0.14; p > .6), and for other measures was −0.77 (N=3; 95% CI: −1.46, 0.08; p = .03).
Fokkema and Knipscheer (2007) was removed as an outlier in this analysis because their intervention lasted for three years as opposed to the average of 16.4 weeks for the rest of the group.
For group- versus individual-based comparison: Qb=0.87, df=1, p> .3. Mean effect size was −0.15 (N=10, 95% CI: −0.28, −0.02; p< .05) for the group-based intervention, and −0.27 (N=10, 95% CI: −0.50, −0.05; p< .05) for the individual-based intervention. For technology-based versus non-technological interventions: Qb=0.31, df=1, p> .5. Mean effect size was −0.16 (N=7, 95% CI: −0.31, 0; p= .5) for the technology-based interventions, and −0.23 (N=13, 95% CI: −0.41, −0.04; p= .01) for studies using no technology.
Mean effect size was −0.28 (N=13; 95% CI: −0.48, −0.08; p< .05) for the UCLA group, 0.05 (N=2; 95% CI: −0.23, 0.34; p> .7) for the De Jong Gierveld group, and −0.16 (N=5; 95% CI: −0.28, −0.03; p= .01) for other loneliness measures.
Gender composition of the sample (β=0.42, Z=2.16, p< .05); mean age of the sample (β=0.001, Z=0.16, p> .8); intervention duration (β=−0.004, Z=−0.81, p> .4); number of intervention sessions (β=−0.003, Z=−0.39, p> .6).
Declaration of Conflicting Interests
The authors declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
References
References included in the meta-analysis are marked by an *.
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience - cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Science USA. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Administration on Aging. A statistical profile of older Americans Aged 65+ Washington, D.C: Department of Health and Human Services; 2008. [Google Scholar]
- *.Allen-Kosal LM. Unpublished Dissertation. Central Michigan University; Mount Pleasant, Michigan: 2008. Cooperative Learning and Cooperative Pre-Training: An Intervention for Loneliness in Elementary Students. [Google Scholar]
- Anderson CA, Arnoult LH. Attributional style and everyday problems in living: Depression, loneliness, and shyness. Social Cognition. 1985;3(1):16–35. [Google Scholar]
- Anderson CA, Horowitz LM, French RD. Attributional style of lonely and depressed people. Journal of Personality and Social Psychology. 1983;45:127–136. doi: 10.1037//0022-3514.45.1.127. [DOI] [PubMed] [Google Scholar]
- Andersson L. Intervention against loneliness in a group of elderly women: An impact evaluation. Social Science & Medicine. 1985;20(4):355–364. doi: 10.1016/0277-9536(85)90010-3. [DOI] [PubMed] [Google Scholar]
- Andrews GJ, Gavin N, Begley S, Brodie D. Assisting friendships, combating loneliness: Users’ views on a “befriending” scheme. Ageing & Society. 2003;23(3):349–362. [Google Scholar]
- APA Publications and Communications Board Working Group on Journal Article Reporting Standards. Reporting standards for research in psychology: Why do we need them? What might they be? American Psychologist. 2008;63(9):839–851. doi: 10.1037/0003-066X.63.9.839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asher S, Hymel S, Renshaw PD. Loneliness in children. Child Development. 1984;55:1456–1464. [Google Scholar]
- Asher SR, Wheeler VA. Children’s loneliness: A comparison of rejected and neglected peer status. Journal of Consulting and Clinical Psychology. 1985;53(4):500–505. doi: 10.1037//0022-006x.53.4.500. [DOI] [PubMed] [Google Scholar]
- *.Banks MR, Banks WA. The effects of animal-assisted therapy on loneliness in an elderly population in long-term care facilities. Journal of Gerontology. 2002;57A(7):M428–M432. doi: 10.1093/gerona/57.7.m428. [DOI] [PubMed] [Google Scholar]
- *.Banks MR, Willoughby LM, Banks WA. Animal-assisted therapy and loneliness in nursing homes: Use of robotic versus living dogs. Journal of American Medical Directors Association. 2008;9(3):173–177. doi: 10.1016/j.jamda.2007.11.007. [DOI] [PubMed] [Google Scholar]
- Barrientos RM, Sprunger DB, Campeau S, Higgins EA, Watkins LR, Rudy JW, et al. Brain-derived neurotrophic factor mRNA downregulation produced by social isolation is blocked by intrahippocampal interleukin-1 receptor antagonist. Neuroscience. 2003;121(4):847–853. doi: 10.1016/s0306-4522(03)00564-5. [DOI] [PubMed] [Google Scholar]
- *.Battles HB, Wiener LS. Starbright world: effects of an electronic network on the social environment of children with life-threatening illnesses. Children’s Health Care. 2002;31(1):47–68. [Google Scholar]
- Baumeister RF, DeWall CN, Ciarocco NJ, Twenge JM. Social exclusion impairs self-regulation. Journal of Personality and Social Psychology. 2005;88(4):589–604. doi: 10.1037/0022-3514.88.4.589. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117(3):497–529. [PubMed] [Google Scholar]
- *.Bauminger N. Brief report: individual social-multi-modal intervention for HFASD. Journal of Autism and Developmental Disorders. 2007;27:1593–1604. doi: 10.1007/s10803-006-0245-4. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Reis HT. Attraction and close relationships. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. Vol. 2. New York: McGraw-Hill; 1998. pp. 193–281. [Google Scholar]
- Boomsma D, Willemsen G, Dolan C, Hawkley L, Cacioppo J. Genetic and environmental contributions to loneliness in adults: The Netherlands twin register Study. Behavior Genetics. 2005;35(6):745–752. doi: 10.1007/s10519-005-6040-8. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. West Sussex, UK: John Wiley & Sons, Ltc; 2009. [Google Scholar]
- Brennan T, Auslander N. Adolescent loneliness: An exploratory study of social and psychological predispositions and theory. Vol. 1. Washington, DC: National Institute of Mental Health, Juvenile Problems Division; 1979. [Google Scholar]
- Brown VM, Allen AC, Dwozan M, Mercer I, Warren K. Indoor gardening older adults: effects of socialization, activities of daily living, and loneliness. Journal of Gerontological Nursing. 2004;30(10):43–42. doi: 10.3928/0098-9134-20041001-10. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Fowler JH, Christakis NA. Alone in the crowd: The structure and spread of loneliness in a large social network. Journal of Personality and Social Psychology. 2009;97(6):977–991. doi: 10.1037/a0016076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC. People thinking about people: The vicious cycle of being a social outcast in one’s own mind. In: Williams KD, Forgas JP, von Hippel W, editors. The social outcast: Ostracism, social exclusion, rejection, and bullying. New York: Psychology Press; 2005. pp. 91–108. [Google Scholar]
- Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends in Cognitive Sciences. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Sciences. 2002;13(4):384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, et al. Loneliness and health: Potential mechanisms. Psychosomatic Medicine. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, et al. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40:1054–1085. [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: Five year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology & Aging. doi: 10.1037/a0017216. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Norris CJ, Decety J, Monteleone G, Nusbaum H. In the eye of the beholder: Individual differences in perceived social isolation predict regional brain activation to social stimuli. Journal of Cognitive Neuroscience. 2009;21:1–10. doi: 10.1162/jocn.2009.21007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Patrick W. Loneliness: Human Nature and the Need for Social Connection. New York: W.W. Norton & Company; 2008. [Google Scholar]
- Caspi A, Harrington H, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: Risk of cardiovascular disease. Archives of Pediatric and Adolescent Medicine. 2006;160(8):805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Asher SR. Loneliness and peer relations in young children. Child Development. 1992;63(2):350–365. doi: 10.1111/j.1467-8624.1992.tb01632.x. [DOI] [PubMed] [Google Scholar]
- Cattan M, White M. Developing evidence based health promotion for older people: A systematic review and survey of health promotion interventions targeting social isolation and loneliness among older people. Internet Journal of Health Promotion. 1998;13:1–9. [Google Scholar]
- Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing & Society. 2005;25:41–67. doi: 10.7748/nop.17.1.40.s11. [DOI] [PubMed] [Google Scholar]
- Celler BG, Lovell NH, Basilakis J. Using information technology to improve the management of chronic disease. Medical Journal of Australia. 2003;179:242–246. doi: 10.5694/j.1326-5377.2003.tb05529.x. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Cheek JM, Busch CM. The influence of shyness on loneliness in a new situation. Personality and Social Psychology Bulletin. 1981;7:572–577. [Google Scholar]
- *.Chiang KJ, Chu H, Chang HJ, Chung MH, Chen CH, Chiou HY, et al. The effects of reminiscence therapy on psychological well-being, depression, and loneliness among the institutionalized aged. International Journal of Geriatric Psychiatry. 2009 doi: 10.1002/gps.2350. e-published ahead of print. [DOI] [PubMed] [Google Scholar]
- *.Christian BJ, D’Auria JP. Building life skills for children with cystic fibrosis. Nursing Research. 2006;55(5):300–307. doi: 10.1097/00006199-200609000-00002. [DOI] [PubMed] [Google Scholar]
- Clarke M, Clarke SJ, Jagger C. Social intervention and the elderly: a randomized controlled trial. American Journal of Epidemiology. 1992;136(12):1517–1523. doi: 10.1093/oxfordjournals.aje.a116473. [DOI] [PubMed] [Google Scholar]
- *.Cohen GD, Perlstein S, Chapline J, Kelly J, Firth KM, Simmens S. The impact of professionally conducted cultural programs on the physical health, mental health, and social functioning of older adults. The Gerontologist. 2006;46(6):726–734. doi: 10.1093/geront/46.6.726. [DOI] [PubMed] [Google Scholar]
- Cole SW. Social regulation of leukocyte homeostasis: The role of glucocorticoid sensitivity. Brain, Behavior, and Immunity. 2008;22(7):1049–1055. doi: 10.1016/j.bbi.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Sung CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes. Genome Biology. 2007;8(9):R189.181–R189.113. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Coleman EA, Tulman L, Samarel N, Chamberlain-Wilmoth M, Rickel L, Rickel M, et al. The effect of telephone social support and education on adaptation to breast cancer during the year following diagnosis. Oncology Nursing Forum. 2005;32(4):822–829. doi: 10.1188/05.onf.822-829. [DOI] [PubMed] [Google Scholar]
- *.Collins CC, Benedict J. Evaluation of a community-based health promotion program for the elderly: Lessons from Seniors CAN. American Journal of Health Promotions. 2006;21(Sep–Oct):45–48. doi: 10.1177/089011710602100108. [DOI] [PubMed] [Google Scholar]
- *.Conoley CW, Garber RA. Effects of reframing and self-control directives on loneliness, depression, and controllability. Journal of Counseling Psychology. 1985;32(1):139–142. [Google Scholar]
- Cox AD. Befriending young mothers. British Journal of Psychiatry. 1993;163:6–18. doi: 10.1192/bjp.163.1.6. [DOI] [PubMed] [Google Scholar]
- *.Cox EO, Green KE, Hobart K, Jang LJ, Seo H. Strengthening the later-life care process: Effects of two forms of a care-receiver efficacy intervention. The Gerontologist. 2007;47(3):388–397. doi: 10.1093/geront/47.3.388. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Peplau LA. Loneliness and the process of social adjustment. Paper presented at the American Psychological Association; Toronto. 1979. [Google Scholar]
- Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Archives of Pediatrics & Adolescent Medicine. 2009;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Craen AJM, Gussekloo J, Blauw GJ, Willems CG, Westendorp RGJ. Randomised controlled trial of unsolicited occupational therapy in community-dwelling elderly people: The LOTIS trial. PLoS Clinical Trials. 2006:1–6. doi: 10.1371/journal.pctr.0010002. Vol. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong Gierveld J, van Tilburg T. Living arrangements of older adults in the Netherlands and Italy: Coresidence values and behaviour and their consequences for loneliness. Journal of Cross-Cultural Gerontology. 1999;14(1):1–24. doi: 10.1023/a:1006600825693. [DOI] [PubMed] [Google Scholar]
- *.de Vries MJ, Schilder JN, CLM, Vrancken AME, Remie ME, Garssen B. Phase II study of psychotherapeutic intervention in advanced cancer. Psycho-Oncology. 1997;6:129–137. doi: 10.1002/(SICI)1099-1611(199706)6:2<129::AID-PON264>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Duck S, Pond K, Leatham G. Loneliness and the evaluation of relational events. Journal of Social & Personal Relationships. 1994;11:253–276. [Google Scholar]
- Evans RL, Jaureguy BM. Phone therapy outreach for blind elderly. The Gerontologist. 1982;22(1):32–35. doi: 10.1093/geront/22.1.32. [DOI] [PubMed] [Google Scholar]
- Evans RL, Smith KM, Werkhoven WS, Fox HR, Pritzl DO. Cognitive telephone group therapy with physically disabled elderly persons. The Gerontological Society of America. 1986;26(1):8–11. doi: 10.1093/geront/26.1.8. [DOI] [PubMed] [Google Scholar]
- *.Evans RL, Werkhoven W, Fox HR. Treatment of social isolation and loneliness in a sample of visually impaired elderly persons. Psychological Reports. 1982;51:103–108. doi: 10.2466/pr0.1982.51.1.103. [DOI] [PubMed] [Google Scholar]
- Findlay RA. Interventions to reduce social isolation among older people: Where is the evidence? Ageing & Society. 2003;23(5):647–658. [Google Scholar]
- *.Fokkema CM, van Tilburg TG. Loneliness interventions among older adults: Sense or nonsense? Tijdschrift Voor Gerontologie en Geriatrie. 2007;38(4):185–203. [PubMed] [Google Scholar]
- *.Fokkema T, Knipscheer K. Escape loneliness by going digital: A quantitative and qualitative evaluation of a Dutch experiment in using ECT to overcome loneliness among older adults. Aging & Mental Health. 2007;11(5):496–504. doi: 10.1080/13607860701366129. [DOI] [PubMed] [Google Scholar]
- *.Fukui S, Koike M, Ooba A, Uchitomi Y. The effect of a psychosocial group intervention on loneliness and social support for Japanese women with primary breast cancer. Oncology Nursing Forum. 2003;30(5):823–830. doi: 10.1188/03.ONF.823-830. [DOI] [PubMed] [Google Scholar]
- Gaikwad R, Warren J. The role of home-based information and communications technology interventions in chronic disease management: A systematic literature review. Health Informatics. 2009;15(2):122–146. doi: 10.1177/1460458209102973. [DOI] [PubMed] [Google Scholar]
- Galanter M. Zealous self-help groups as adjuncts to psychiatric treatment: A study of Recovery, Inc. American Journal of Psychiatry. 1988;145:1248–1253. doi: 10.1176/ajp.145.10.1248. [DOI] [PubMed] [Google Scholar]
- Glass CR, Gottman JM, Shmurak SH. Response acquisition and cognitive self-statements modification approaches to dating skills training. Journal of Counseling Psychology. 1976;23:520–526. [Google Scholar]
- Goldstein JR, Kenney CT. Marriage delayed or marriage forgone? New cohort forecasts of first marriage for U.S. women. American Sociological Review. 2001:506–519. [Google Scholar]
- Guevremont DC, MacMillan VM, Shawchuck CR, Hansen DJ. A peer-mediated intervention with clinic-referred socially isolated girls. Behavior Modification. 1989;13(1):32–50. doi: 10.1177/01454455890131002. [DOI] [PubMed] [Google Scholar]
- *.Hartke RJ, King RB. Telephone group intervention for older stroke caregivers. Topics in Stroke Rehabilitation. 2003;9(4):65–81. doi: 10.1310/RX0A-6E2Y-BU8J-W0VL. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Browne MW, Cacioppo JT. How can I connect with thee? Let me count the ways. Psychological Science. 2005;16(10):798–804. doi: 10.1111/j.1467-9280.2005.01617.x. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality and Social Psychology. 2003;85:105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Cacioppo JT. Aging and loneliness: Downhill quickly? Current Directions in Psychological Science. 2007;16:187–191. [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology: Social Sciences. 2008;63B:S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging. 2006;21(1):152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Preacher KJ, Cacioppo JT. Multilevel modeling of social interactions and mood in lonely and socially connected individuals: The MacArthur social neuroscience studies. In: Ong AD, van Dulmen M, editors. Oxford handbook of methods in positive psychology. New York: Oxford University Press; 2007. pp. 559–575. [Google Scholar]
- Hawkley LC, Preacher KJ, Cacioppo JT. Loneliness impairs daytime functioning but not sleep duration. Health Psychology. 2010;29(2):124–129. doi: 10.1037/a0018646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: Five-year cross-lagged analyses in middle-aged and older adults. Psychology and Aging. 2010;25(1):132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Heckman TG, Barcikowski R. A telephone-delivered coping improvement group intervention for middle aged and older adults living with HIV/AIDS. Annals of Behavioral Medicine. 2006;32(1):27–38. doi: 10.1207/s15324796abm3201_4. [DOI] [PubMed] [Google Scholar]
- Hedberg GE, Wikstrom-Frison L, Janlert U. Comparison between two programmes for reducing the levels of risk indicators for heart diseases among male professional drivers. Occupational and Environmental Medicine. 1998;55:554–561. doi: 10.1136/oem.55.8.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando: Academic Press; 1985. [Google Scholar]
- *.Heller K, Thompson MG, Trueba PE, Hogg JR, Vlachos-Weber I. Peer support telephone dyads for elderly women: was this the wrong intervention? American Journal of Community Psychology. 1991;19(1):53–74. doi: 10.1007/BF00942253. [DOI] [PubMed] [Google Scholar]
- Heller T, Roccoforte JA, Hsieh K, Cook JA, Pickett SA. Benefits of support groups for families of adults with severe mental illness. American Journal of Orthopsychiatry. 1997;67(2):187–198. doi: 10.1037/h0080222. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Hill W, Weinert C, Cudney S. Influence of a computer intervention on the psychological status of chronically ill rural women: Preliminary results. Nursing Research. 2006;55(1):34–42. doi: 10.1097/00006199-200601000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopman-Rock M, Westhoff MH. Development and evaluation of “Aging well and healthily”: A health-education exercise program for community-living older adults. Journal of Aging and Physical Activity. 2002;10:364–381. [Google Scholar]
- *.Hopps SL, Pepin M, Boisvert JM. The effectiveness of cognitive-behavioral group therapy for loneliness via inter-relay-chat among people with physical disabilities. Psychotherapy: Theory, Research, Practice, Training. 2003;40(1/2):136–147. [Google Scholar]
- Horowitz LM. The toll of loneliness: Manifestations, mechanisms, and means of prevention. Washington, DC: National Institute of Mental Health, Office of Prevention; 1983. [Google Scholar]
- Hu M. Will online chat help alleviate mood loneliness. CyberPsychology & Behavior. 2009;12(2):219–223. doi: 10.1089/cpb.2008.0134. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB. Methods for defining and determining the clinical significance of treatment effects: description, application, and alternatives. Journal of Consulting and Clinical Psychology. 1999;67(3):300–307. doi: 10.1037//0022-006x.67.3.300. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jerrome D. Lonely women in a friendship club. British Journal of Guidance and Counseling. 1983;11(1):11–21. [Google Scholar]
- *.Jessen J, Cardiello F, Baun MM. Avian companionship in alleviation of depression, loneliness, and low morale of older adults in skilled rehabilitation. Psychological Reports. 1996;78:339–348. doi: 10.2466/pr0.1996.78.1.339. [DOI] [PubMed] [Google Scholar]
- Jones W. Loneliness and social behavior. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. [Google Scholar]
- Jones WH, Freemon JR, Goswick RA. The persistence of loneliness: Self and other determinants. Journal of Personality. 1981;49:27–48. [Google Scholar]
- Jones WH, Hobbs SA, Hockenbury D. Loneliness and social skill deficits. Journal of Personality and Social Psychology. 1982;42(4):682–689. doi: 10.1037//0022-3514.42.4.682. [DOI] [PubMed] [Google Scholar]
- Karelina D, Norman GJ, Zhang N, Morris JS, Peng H, DeVries AC. Social isolation alters neuroinflammatory response to stroke. Proceedings of the National Academy of Sciences. 2009;106:5895–5900. doi: 10.1073/pnas.0810737106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keil CP. Loneliness, stress, and human-animal attachment among older adults. In: Wilson CC, Turner DC, editors. Companion animals in human health. Thousand Oaks: Sage; 1988. pp. 123–134. [Google Scholar]
- Kiecolt-Glaser JK, Garner W, Speicher C, Penn GM, Holliday J, Glaser R. Psychosocial modifiers of immunocompetence in medical students. Psychosomatic Medicine. 1984;46(1):7–14. doi: 10.1097/00006842-198401000-00003. [DOI] [PubMed] [Google Scholar]
- Knight RG, Chisholm BJ, Nigel VM, Godfrey HPD. Some normative, reliability, and factor analytic data for the revised UCLA loneliness scale. Journal of Clinical Psychology. 1988;44:203–206. doi: 10.1002/1097-4679(198803)44:2<203::aid-jclp2270440218>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- *.Kolko DJ, Loar LL, Sturnick D. Inpatient social-cognitive skills training groups with conduct disordered and attention deficit disordered children. Journal of Child Psychology and Psychiatry. 1990;31(5):737–748. doi: 10.1111/j.1469-7610.1990.tb00814.x. [DOI] [PubMed] [Google Scholar]
- Kowalski NC. Institutional relocation: Current programs and applied approaches. Gerontologist. 1981;21:512–519. [Google Scholar]
- *.Kraut R, Patterson M, Lundmark V, Kiesler S, Mukopadhyay T, Scherlis W. Internet Paradox: A social technology that reduces social involvement and psychological well-being? American Psychologist. 1998;53(9):1017–1031. doi: 10.1037//0003-066x.53.9.1017. [DOI] [PubMed] [Google Scholar]
- *.Kremers IP, Steverink N, Albersnagel FA, Slaets JPJ. Improved self-management ability and well-being in older women after a short group intervention. Aging & Mental Health. 2006;10(5):476–484. doi: 10.1080/13607860600841206. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- *.Marshall WL, Bryce P, Hudson SM, Ward T, Moth B. The enhancement of intimacy and the reduction of loneliness among child molesters. Journal of Family Violence. 1996;11(3):219–235. [Google Scholar]
- *.Martina CMS, Stevens NL. Breaking the cycle of loneliness? Psychological effects of a friendship enrichment program for older women. Aging & Mental Health. 2006;10(5):467–475. doi: 10.1080/13607860600637893. [DOI] [PubMed] [Google Scholar]
- *.McAuley E, Blissmer B, Marquez DX, Jerome GJ, Kramer AF, Katula J. Social relations, physical activity, and well-being in older adults. Preventive Medicine. 2000;31:608–617. doi: 10.1006/pmed.2000.0740. [DOI] [PubMed] [Google Scholar]
- McGuire S, Clifford J. Genetic and environmental contributions to loneliness in children. Psychological Science. 2000;11:487–491. doi: 10.1111/1467-9280.00293. [DOI] [PubMed] [Google Scholar]
- McLarnon LD, Kaloupek DG. Psychological investigation of genital herpes recurrence: Prospective assessment and cognitive-behavioral intervention for a chronic physical disorder. Health Psychology. 1988;7(3):231–249. doi: 10.1037//0278-6133.7.3.231. [DOI] [PubMed] [Google Scholar]
- McWhirter BT. Factor analysis of the revised UCLA loneliness scale. Current Psychology: Research & Reviews. 1990a;9:56–58. [Google Scholar]
- McWhirter BT. Loneliness: A review of current literature, with implications for counseling and research. Journal of Counseling & Development. 1990b;68:417–422. [Google Scholar]
- *.McWhirter BT, Horan JJ. Construct validity of cognitive-behavioral treatments for intimate and social loneliness. Current Psychology. 1996;15(1):42–52. [Google Scholar]
- Moore JA, Sermat V. Relationship between self-actualization and self-reported loneliness. Canadian Counsellor. 1974;8(3):194–196. [Google Scholar]
- *.Morrow-Howell N, Becker-Kemppainen S, Lee J. Evaluating an intervention for the elderly at increased risk of suicide. Research on Social Work Practice. 1998;8(1):28–46. [Google Scholar]
- Murray P. Recovery, Inc as an adjunct to treatment in an era of managed care. Psychiatric Services. 1996;47(12):1378–1381. doi: 10.1176/ps.47.12.1378. [DOI] [PubMed] [Google Scholar]
- Mynatt S, Wicks M, Bolden L. Pilot study of INSIGHT therapy in African American women. Archives of Psychiatric Nursing. 2008;22(6):364–374. doi: 10.1016/j.apnu.2007.10.007. [DOI] [PubMed] [Google Scholar]
- O’Luanaigh C, Lawlor BA. Loneliness and the health of older people. International Journal of Geriatric Psychiatry. 2008;23:1213–1221. doi: 10.1002/gps.2054. [DOI] [PubMed] [Google Scholar]
- *.Ollonqvist K, Palkeinen H, Aaltonen T, Pohjolainen T, Puukka P, Hinkka K, et al. Alleviating loneliness among frail older people: Findings from a randomised controlled trial. The International Journal of Mental Health Promotion. 2008;10(2):26–34. [Google Scholar]
- Orwin RG. A fail-safe N for effect size in meta-analysis. Educational Statistics. 1983;8:157–159. [Google Scholar]
- Peplau LA, Miceli M, Morasch B. Loneliness and self-evaluation. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. [Google Scholar]
- Peplau LA, Perlman D. Loneliness: A sourcebook of current theory, research, and therapy. New York: Wiley; 1982. [Google Scholar]
- Perese EF, Wolf M. Combating loneliness among persons with severe mental illness: social network interventions’ characteristics, effectiveness, and applicability. Issues in Mental Health Nursing. 2005;26:591–609. doi: 10.1080/01612840590959425. [DOI] [PubMed] [Google Scholar]
- *.Petryshen PM, Hawkins JD, Fronchak TA. An evolution of the social recreation component of a community mental health program. Psychiatric Rehabilitation Journal. 2001;24(3):293–298. doi: 10.1037/h0095083. [DOI] [PubMed] [Google Scholar]
- Pilisuk M, Minkler M. Supportive networks: Life ties for the elderly. Journal of Social Issues. 1980;36:95–116. [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshman. Health Psychology. 2005;24(3):297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Ransom D, Heckman TG, Anderson T, Garske J, Holroyd K, Basta T. Telephone-delivered, interpersonal psychotherapy for HIV-infected rural persons with depression: A pilot trial. Psychiatric Services. 2008;59(8):871–877. doi: 10.1176/ps.2008.59.8.871. [DOI] [PubMed] [Google Scholar]
- Rook KS. Promoting social bonds: Strategies for helping the lonely and socially isolated. American Psychologist. 1984;39(12):1389–1407. [Google Scholar]
- Rook KS, Peplau LA. Perspectives on helping the lonely. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. [Google Scholar]
- *.Rosen CE, Rosen S. Evaluating an intervention program for the elderly. Community Mental Health Journal. 1982;18(1):21–33. doi: 10.1007/BF00757109. [DOI] [PubMed] [Google Scholar]
- Routasalo PE, Tilvis RS, Kautiainen H, Pitkala KH. Effects of psychosocial group rehabilitation on social functioning, loneliness and well-being of lonely, older people: Randomized controlled trial. Journal of Advanced Nursing. 2009;65(2):297–305. doi: 10.1111/j.1365-2648.2008.04837.x. [DOI] [PubMed] [Google Scholar]
- Rudatsikira E, Muula AS, Siziya S, Twa-Twa J. Suicidal ideation and associated factors among school-going adolescents in rural Uganda. BMC Psychiatry. 2007;67:1–6. doi: 10.1186/1471-244X-7-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980;39(3):472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- *.Samarel N, Tulman L, Fawcett J. Effects of two types of social support and education on adaptation to early-stage breast cancer. Research in Nursing and Health. 2002;25:459–470. doi: 10.1002/nur.10061. [DOI] [PubMed] [Google Scholar]
- *.Savelkoul M, de Witte L, Candel MJJM, Van Der Tempel H, Van Den Borne B. Effects of a coping intervention on patients with rheumatic diseases: Results of a randomized controlled trial. Arthritis Care & Research. 2001;45:69–76. doi: 10.1002/1529-0131(200102)45:1<69::AID-ANR86>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Schneider B, Waite LJ. Being together, working apart. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- *.Seepersad SS. Unpublished Dissertation. University of Illinois at Urbana-Champaign; Urbana: 2005. Understanding and Helping the Lonely: An Evaluation of the Luv Program. [Google Scholar]
- *.Shapira N, Barak A, Gal I. Promoting older adults’ well-being through Internet training and use. Aging & Mental Health. 2007;11(5):477–484. doi: 10.1080/13607860601086546. [DOI] [PubMed] [Google Scholar]
- Shaver P, Furman W, Buhrmester D. Transition to college: Network changes, social skills, and loneliness. In: Duck S, PD, editors. Understanding personal relationships: An interdisciplinary approach. London: Sage; 1985. pp. 193–219. [Google Scholar]
- Silva-Gomez AB, Rojas D, Juarez I, Flores G. Decreased dendritic spine density on prefrontal cortical and hippocampal pyramidal neurons in postweaning social isolation rats. Brain Research. 2003;983(1–2):128–136. doi: 10.1016/s0006-8993(03)03042-7. [DOI] [PubMed] [Google Scholar]
- Soholt Lupton BS, Fonnebo V, Sogaard AJ, Fylkesnes K. The Finnmark Intervention Study: Do community-based intervention programmes threaten self-rated health and well-being? Experiences from Batsfjord, a fishing village in North Norway. European Journal of Public Health. 2005;15(1):91–96. doi: 10.1093/eurpub/cki101. [DOI] [PubMed] [Google Scholar]
- *.Sorenson DS. Healing traumatizing provider interactions among women through short-term group therapy. Archives of Psychiatric Nursing. 2003;17(6):259–269. doi: 10.1053/j.apnu.2003.10.002. [DOI] [PubMed] [Google Scholar]
- Steffick DE. Documentation on affective functioning measures in the Health and Retirement Study (No DR-005) Ann Arbor: Survey Research Center, University of Michigan; 2000. [Google Scholar]
- Stevens N. Combating loneliness: A friendship enrichment programme for older women. Ageing and Society. 2001;21:183–202. [Google Scholar]
- Stevens NL, Martina CMS, Westerhof GJ. Meeting the need to belong: Predicting effects of a friendship enrichment program for older women. The Gerontologist. 2006;46(4):495–502. doi: 10.1093/geront/46.4.495. [DOI] [PubMed] [Google Scholar]
- *.Stewart M, Craig D, MacPherson K, Alexander S. Promoting positive affect and diminishing loneliness of widowed seniors through support intervention. Public Health Nursing. 2001;18(1):54–63. doi: 10.1046/j.1525-1446.2001.00054.x. [DOI] [PubMed] [Google Scholar]
- *.Stewart M, Reutter L, Letourneau N, Makawarimba E. A support intervention to promote health and coping among homeless youths. Canadian Journal of Nursing Research. 2009;41(2):55–77. [PubMed] [Google Scholar]
- Taylor P, Kochhar R, Livingston G, Cohn D, Wang W, Dockterman D. US Birth rate decline linked to recession. Washington, D.C: Pew Research Center; 2010. [Google Scholar]
- Theeke LA. Predictors of loneliness in U.S. adults over age sixty-five. Archives of Psychiatric Nursing. 2009;23(5):387–396. doi: 10.1016/j.apnu.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Tilvis RS, Kahonen-Vare MH, Jolkkonen J, Valvanne J, Pitkala KH, Strandberg TE. Predictors of cognitive decline and mortality of aged people over a 10-Year period. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2004;59(3):M268–274. doi: 10.1093/gerona/59.3.m268. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Baumeister RF, Tice DM, Stucke TS. If you can’t join them, beat them: Effects of social exclusion on aggressive behavior. Journal of Personality and Social Psychology. 2001;81(6):1058–1069. doi: 10.1037//0022-3514.81.6.1058. [DOI] [PubMed] [Google Scholar]
- Twentyman CT, Zimering RT. Behavioral training of social skills: A critical review. In: Hersen M, Eisler RM, Miller PM, editors. Progress in behavior modification. Vol. 7. New York: Academic Press; 1979. [Google Scholar]
- U.S. Bureau of Labor Statistics. Families and work in 12 countries 1980–2001. Washington, D.C: 2003. [Google Scholar]
- Vachon ML, Lyall W, Rogers J, Freedman-Letofsky K, Freeman S. A controlled study of a self-help intervention for widows. American Journal of Psychiatry. 1980;137:1380–1384. doi: 10.1176/ajp.137.11.1380. [DOI] [PubMed] [Google Scholar]
- *.van den Elzen AJ, Fokkema CM. Home visits to the elderly in Leiden: An investigation into the effect of loneliness. Tijdschrift Voor Gerontologie en Geriatrie. 2006;37(4):142–146. [PubMed] [Google Scholar]
- van Kordelaar KACM, Stevens NL, Pleiter A. Good Company in a Big Home described in Loneliness Interventions among older adults: Sense or nonsense? In: Fokkema CM, van Tilburg TG, editors. Tijdschrift Voor Gerontologie en Geriatrie. 4. Vol. 38. 2004. pp. 185–203. [PubMed] [Google Scholar]
- van Rossum E, Frederiks CMA, Philipsen H, Portengen K, Wiskerke J, Knipschild P. Effects of preventive home visits to elderly people. BMJ. 1993;307:27–32. doi: 10.1136/bmj.307.6895.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor CD, Scambler SJ, Bowling A, Bondt J. The prevalence of and risk factors for loneliness in later life: A survey of older people in Great Britain. Ageing & Society. 2005;25:357–375. [Google Scholar]
- Wallerstein JS, Kelly JB. Divorce counseling: A community service for families in the midst of a divorce. American Journal of Orthopsychiatry. 1977;47:4–22. doi: 10.1111/j.1939-0025.1977.tb03240.x. [DOI] [PubMed] [Google Scholar]
- Weeks DL. The regression effect as a neglected source of bias in nonrandomized intervention trials and systematic reviews of observational studies. Evaluation & the Health Professions. 2007;30:254–265. doi: 10.1177/0163278707304043. [DOI] [PubMed] [Google Scholar]
- Weiss RS. Loneliness: The experience of emotional and social isolation. Cambridge, MA: MIT Press; 1973. [Google Scholar]
- Wheeler L, Reis H, Nezlek J. Loneliness, social interaction, and sex roles. Journal of Personality and Social Psychology. 1983;45(4):943–953. doi: 10.1037//0022-3514.45.4.943. [DOI] [PubMed] [Google Scholar]
- *.White H, McConnell E, Clipp E, Branch LG, Sloane R, Pieper C, et al. A randomized controlled trial of the psychosocial impact of providing internet training and access to older adults. Aging & Mental Health. 2002;6(3):213–221. doi: 10.1080/13607860220142422. [DOI] [PubMed] [Google Scholar]
- *.White H, McConnell E, Clipp E, Bynum L, Teague C, Navas L, et al. Surfing the net in later life: A review of the literature and pilot study of computer use and quality of life. The Journal of Applied Gerontology. 1999;18(3):358–378. [Google Scholar]
- Whitehouse WG, Dinges DF, Orne EC, Keller SE, Bates BL, Bauer NK, et al. Psychological and immune effects of self-hypnosis training for stress management throughout the first semester of medical school. Psychosomatic Medicine. 1996;58:249–263. doi: 10.1097/00006842-199605000-00009. [DOI] [PubMed] [Google Scholar]
- *.Williams RA, Hagerty BM, Yousha SM, Horrocks J, Hoyle KS, Liu D. Psychosocial effects of the boot strap intervention in Navy recruits. Military Medicine. 2004;169(10):814–820. doi: 10.7205/milmed.169.10.814. [DOI] [PubMed] [Google Scholar]
- Wilson DB. ES Calculation xls. 2002 Retrieved October 5, 2009, from http://mason.gmu.edu/~dwilsonb/ma.html.
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;62(2):234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]
- *.Winningham RG, Pike NL. A cognitive intervention to enhance institutionalized older adults’ social support networks and decrease loneliness. Aging & Mental Health. 2007;11(6):716–721. doi: 10.1080/13607860701366228. [DOI] [PubMed] [Google Scholar]
- *.Yarnoz S, Plazaola M, Etxeberria J. Adaptation to divorce: An attachment-based intervention with long-term divorced parents. Journal of Divorce & Remarriage. 2008;49(3/4):291–307. [Google Scholar]
- Young JE. Loneliness, depression and cognitive therapy: Theory and application. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley; 1982. pp. 379–406. [Google Scholar]