Abstract
Background
Dietary fiber may decrease the risk of cardiovascular disease and associated risk factors. We examined trends in dietary fiber intake among diverse US adults between 1999 and 2010, and investigated associations between dietary fiber intake and cardiometabolic risks including metabolic syndrome, cardiovascular inflammation, and obesity.
Methods
Our cross-sectional analysis included 23,168 men and non-pregnant women aged 20+ years from 1999–2010 National Health and Nutrition Examination Survey. We used weighted multivariable logistic regression models to estimate predicted marginal risk ratios and 95% confidence intervals (CIs) for the risks of having the metabolic syndrome, inflammation, and obesity associated with quintiles of dietary fiber intake.
Results
Dietary fiber intake remained consistently below recommended adequate intake levels for total fiber defined by the Institute of Medicine. Mean dietary fiber intake averaged 15.7g–17.0g. Mexican-Americans (18.8 g) consumed more fiber than non-Hispanic Whites (16.3 g) and non-Hispanic Blacks (13.1 g). Comparing the highest to lowest quintiles of dietary fiber intake, adjusted predicted marginal risk ratios (95% CI) for the metabolic syndrome, inflammation, and obesity were 0.78 (0.69–0.88), 0.66 (0.61–0.72), and 0.77 (0.71–0.84), respectively. Dietary fiber was associated with lower levels of inflammation within each racial and ethnic group, though statistically significant associations between dietary fiber and either obesity or metabolic syndrome were seen only among whites.
Conclusions
Low dietary fiber intake from 1999–2010 in the US, and associations between higher dietary fiber and a lower prevalence of cardiometabolic risks suggest the need to develop new strategies and policies to increase dietary fiber intake.
Keywords: Dietary fiber, disparities, metabolic diseases, NHANES
INTRODUCTION
The benefits of dietary fiber on cardiovascular risk reduction have been documented.1–4 Specifically, epidemiologic data suggest a protective relationship between dietary fiber and risk factors for cardiovascular disease, including components of the metabolic syndrome,5, 6 and related risks such as cardiovascular inflammation.7, 8 Dietary fiber intake is thought to play a role in cardiometabolic and cardiovascular disease risk reduction by decreasing blood pressure,9 cholesterol levels,10, 11 and levels of biomarkers of inflammation.8, 12 Additionally, fiber intake is associated with an increased sensation of satiety thought to contribute to weight loss,9 and improved insulin sensitivity.13, 14 Based on large-scale prospective cohort studies and small-scale intervention studies that show reductions in coronary heart disease (CHD) risk, including lipid reduction associated with dietary and functional fiber intake from oat cereal and bean sources, the Institute of Medicine has established a recommended “adequate intake” level for total fiber intake by age and sex: 38g per day for men aged 19 to 50 years, 30g per day for men older than 50 years, 25g per day for women aged 19 to 50 years, and 21g per day for women older than 50 years.15 To date, recent studies have not fully investigated potential demographic and socioeconomic disparities in dietary fiber intake over time, or the relation between dietary fiber intake and cardiometabolic risk factors in diverse populations. Surveillance data from the National Health and Nutrition Examination Survey (NHANES) can assist in identifying vulnerable groups that may benefit from targeted dietary interventions, and, help estimate cardiometabolic risks associated with dietary fiber intake in diverse groups.16
The present study has three objectives: (1) to examine secular trends in dietary fiber intake among US adults from 1999 to 2010; (2) to investigate possible sex, age, racial/ethnic, and socioeconomic disparities in dietary fiber intake trends during this time period; and (3) to examine the association between dietary fiber intake and the prevalence of cardiometabolic risk factors, the metabolic syndrome, inflammation, and obesity in diverse groups of adults in the US, with attention to any racial/ethnic differences in associations between fiber intake and cardiometabolic risks.
METHODS
Study Population
Our study examines data from the 1999–2010 NHANES. The NHANES is a cross-sectional, nationally representative sample of the US non-institutionalized civilian population.17 The NHANES population was recruited using a multistage, stratified sampling design.17 Our study population included all non-pregnant participants, aged 20 years and older in the 1999 to 2010 NHANES cohorts (N=30,433). Those with complete data for all covariates including dietary fiber intake, C-reactive protein (CRP) and body mass index were included in the analysis of inflammation and obesity (N=23,168). Individuals who did not participate in the fasting subsample were excluded from the analysis of the metabolic syndrome (N=12,374). After limiting the cohort to participants with complete data for all covariates, there were 10,473 people included in the analysis of the metabolic syndrome. Human subject procedures for NHANES were approved by the National Center for Health Statistics Research Ethics Review Board. Our study was approved by the Partners Institutional Review Board.
Dietary fiber intake
Dietary intake data were assessed using 24-hour dietary recalls, administered during computer-assisted, in-person interviews by a trained interviewer at NHANES Mobile Examination Centers. Nutrient intakes were coded and analyzed using the United States Department of Agriculture (USDA) 1994–98 Survey Nutrient Database (1999–2001) and the USDA Food and Nutrient Databases for Dietary Studies (2001–2010).6, 17–19 From 1999–2002, NHANES assessed dietary intake with one 24-hour recall date. Beginning in 2003, NHANES collected two 24-hour dietary recalls for each participant. To facilitate comparability across all 12 survey years, our analysis used dietary intake data from the first 24-hour recall interview.
Clinical Outcomes
According to Adult Treatment Panel III criteria, we classified individuals with at least 3 of the following cardiometabolic components as having the metabolic syndrome: (1) abdominal obesity (waist circumference > 102 cm in males and > 88 cm in females); (2) elevated blood pressure (≥ 130/85 mmHg); (3) hypertriglyceridemia (≥ 150 mg/dL); (4) low high-density lipoprotein (HDL) cholesterol (< 40 mg/dL in males and < 50 mg/dL in females); and (5) elevated fasting plasma glucose (≥ 100 mg/dL).20, 21 We classified individuals with a CRP concentration > 3.0 mg/L as having elevated CRP.22, 23 We defined obesity as having a body mass index ≥ 30.0 kg/m2.24
Analytes were collected via venipuncture from fasting blood samples at the NHANES Mobile Examination Center. HDL cholesterol was measured by the heparin-manganese precipitation method (1999–2002) and the direct HDL cholesterol immunoassay method (2003–2010); we used the adjusted HDL measurements as reported by NHANES for the years that required correction due to assay-related bias.25 Across all 12 survey years, plasma glucose was determined using the hexokinase enzymatic assay. Fasting plasma glucose levels were only determined for those persons who participated in the morning fast. In 1999–2010, CRP concentrations were measured by high-sensitivity latex-enhanced nephelometry.
Blood pressure, waist circumference, and body mass index were measured at the Mobile Examination Center. Detailed descriptions about blood collection and processing and anthropometric measurements have been described.26
Demographic and other behavioral characteristics
The primary covariates included in this analysis were: age (20–50 years, ages 51 years and older), sex, race/ethnicity (Mexican American, non-Hispanic White, non-Hispanic Black), educational attainment (less than 9th grade, 9–12th grade and no diploma, high school diploma or GED, associate’s degree or some college, bachelor’s degree or higher), smoking status (current smoker: ≥ 100 cigarettes in life and currently smoking; former smoker; never smoker: < 100 cigarettes in life), and total energy intake (low: males < 2000 kcal/day, females < 1600 kcal/day; adequate: males 2000–3000 kcal/day, females 1600–2400 kcal/day; high: males > 3000 kcal/day, females >2400 kcal/day).27
Statistical analysis
Temporal trends in dietary fiber intake between 1999 and 2010 were estimated using weighted linear regression in SUDAAN to account for the complex sampling design. These temporal trends were estimated for the entire cohort and within categories for age, sex, racial/ethnicity, and educational attainment. Multivariable models were used to examine the association between quintiles of dietary fiber intake and cardiometabolic risks, while also adjusting for potential confounding factors. We used weighted multivariable logistic regression models to estimate the predicted marginal risk ratios and 95% confidence intervals (CIs) for the risk of having the metabolic syndrome, inflammation, and obesity associated with quintiles of dietary fiber intake.28 Models adjusted for age and total energy intake were compared to fully-adjusted models with the following covariates: age, sex, race/ethnicity, educational attainment, smoking status, and total energy intake.29, 30 Accounting for the complex sampling design in NHANES, all statistical analyses were conducted in a SAS-callable version of SUDAAN (version 9.0.1, Research Triangle Institute, Research Triangle Park, NC). Twelve-year fasting subsample weights were used for the analysis of the metabolic syndrome (N=10,473) and 12-year Mobile Examination Center weights were used for the analysis of inflammation and obesity (N=23,168). Statistical significance was based on two-tailed tests of statistical significance at an alpha level of 0.05.
A sensitivity analysis was performed to exclude outlier values with low and high dietary fiber intakes below the 5th and 1st percentile and above the 95th and 99th percentile ranges to determine their influence on the associations we report. Additionally, the recall period and the domains classifying physical activity changed substantially between survey cycles 2005–2006 and 2007–2008 limiting the ability to make direct comparisons across all years.31 We also conducted sensitivity analyses to estimate potential confounding effects of physical activity on the associations we report, and we estimated associations adjusted for physical activity measures separately in the 1999–2006 and 2007–2010 cohorts. Categories of physical activity (no activity; some/irregular activity; regular activity) were based on the United States Department of Health and Human Services 2008 Physical Activity Guidelines for Americans.32 These results are available in a supplemental appendix (Appendix 1 and Appendix 2).
RESULTS
Study Population Characteristics
Study population characteristics are listed in Table 1 by mean dietary fiber intake. Reported dietary fiber intake among all non-pregnant adults ranged between 6.3 grams per day (g/d) (10th percentile) and 29.0 g/d (90th percentile). Mean dietary fiber intake was 16.2 g/d (Table 1). In comparison to those who consumed lower amounts of dietary fiber, participants who consumed higher amounts of dietary fiber were more likely to be older (51 years and older), male, Mexican-American, highly educated (bachelor’s degree or greater), former smokers, and physically active.
Table 1.
Descriptive Characteristics for all Non-pregnant Adults 20+ Years by Dietary Fiber, NHANES 1999–2010.
| Unadjusted mean dietary fiber intake | ||
|---|---|---|
| Total N (%) | Dietary Fiber (g) ± SE | |
| Demographics | ||
| Total Population, % | 23,168 (100) | 16.2 ± 0.2 |
| Age | ||
| 20–50 years | 11,794 (59.8) | 16.1 ± 0.2 |
| 51+ years | 11,374 (40.2) | 16.2 ± 0.2 |
| Gender | ||
| Male | 11,761 (49.5) | 18.0 ± 0.2 |
| Female | 11,407 (50.5) | 14.3 ± 0.2 |
| Race/Ethnicity | ||
| Mexican-American | 5,257 (8.6) | 18.8 ± 0.2 |
| Non-Hispanic White | 13,009 (80.0) | 16.3 ± 0.2 |
| Non-Hispanic Black | 4,902 (11.5) | 13.1 ± 0.2 |
| Education | ||
| Less than 9th grade | 3,099 (5.8) | 16.1 ± 0.3 |
| 9–12th grade, but no HS diploma | 3,804 (12.5) | 14.4 ± 0.2 |
| HS diploma/GED | 5,670 (25.9) | 14.9 ± 0.2 |
| Some college, Associate’s degree | 6,194 (30.2) | 15.7 ± 0.2 |
| Bachelor’s degree or greater | 4,401 (25.6) | 18.8 ± 0.3 |
| Behaviors | ||
| Smoking Status | ||
| Current smoker | 5,232 (23.7) | 13.6 ± 0.2 |
| Former smoker | 6,266 (26.0) | 17.0 ± 0.2 |
| Never smoker | 11,670 (50.3) | 16.9 ± 0.2 |
| Physical Activity 1999–2006a | ||
| No activity | 6,106 (34.6) | 14.6 ± 0.2 |
| Some/Irregular activity | 3,279 (25.1) | 15.8 ± 0.2 |
| Regular activity | 4,989 (40.3) | 17.2 ± 0.3 |
| Physical Activity 2007–2010a | ||
| No activity | 4,812 (47.2) | 14.9 ± 0.2 |
| Some/Irregular activity | 1,326 (17.3) | 16.9 ± 0.5 |
| Regular activity | 2,635 (35.5) | 18.6 ± 0.4 |
| Energy Intake (kcal/day)b | ||
| Low (below guidelines) | 9,746 (36.6) | 12.1 ± 0.2 |
| Adequate (meets guidelines) | 4,892 (24.8) | 23.1 ± 0.5 |
| High (above guidelines) | 8,530 (38.6) | 16.9 ± 0.3 |
Data from National Health and Nutrition Examination Survey, 1999–2010.
Due to methodological changes in physical activity measurement between 2006 and 2007, physical activity was assessed separately in 1999–2006 and 2007–2010. Physical activity categories based on the US Department of Health and Human Services’ 2008 Physical Activity Guidelines for Americans. “No activity” includes participants with no moderate or vigorous physical activity. “Some/Irregular activity” includes participants with < 150 minutes/week of moderate activity or < 75 minutes/week of vigorous activity. “Regular activity” includes participants with ≥ 150 minutes/week of moderate activity, ≥ 75 minutes/week of vigorous activity, or ≥ 150 minutes/week of a combination of moderate and vigorous activity.
Energy intake categories based on the US Department of Health and Human Services’ 2010 Dietary Guidelines for Americans. “Low” includes males with < 2000 kcal/day and females with < 1600 kcal/day. “Adequate” includes males with 2000–3000 kcal/day and females with 1600–2400 kcal/day. “High” includes males with > 3000 kcal/day and females with >2400 kcal/day.
Trends in Dietary Fiber
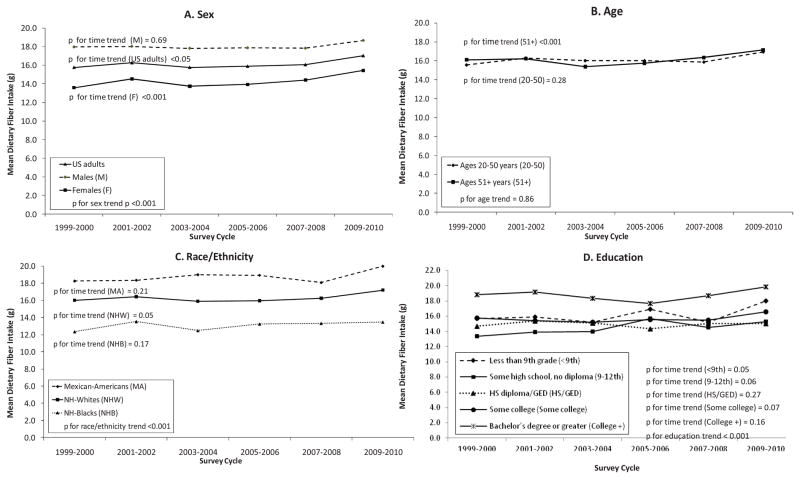
Figure 1 presents the trends in crude mean dietary fiber intake among non-pregnant US adults and crude mean dietary fiber intake by sex, age, educational attainment, and race/ethnicity across 12 survey years. The crude fiber intake among all US adults increased by approximately1.3 grams between 1999 and 2010. However, quantities of dietary fiber intake among US adults were below total recommended adequate intake levels, as recommended by the Institute of Medicine, across all 12 survey years.15 Mean dietary fiber intake was statistically different by sex (P < 0.001), with males consuming higher amounts of dietary fiber. Younger adults had mean dietary fiber intakes that were not statistically different across survey years (P = 0.28), while older adults had mean dietary fiber intakes that tended to increase across survey years (P < 0.001). College graduates had higher mean dietary fiber intakes than other groups (P < 0.001); though trends by education were not linear. Additionally, mean dietary fiber intake was statistically different by race/ethnicity (P < 0.001), with Mexican-Americans consuming higher amounts of dietary fiber and non-Hispanic Blacks consuming lower amounts of dietary fiber compared to non-Hispanic Whites. Young non-Hispanic Black men aged 20 to 50 had a mean fiber intake (14.7g) that was furthest from the recommended adequate intake for their age group (38g). Older Mexican-American (15.6g) and non-Hispanic White women (15.0g) aged 51 and older had fiber intake that was closest to recommended levels for their age group (21g). Mexican-Americans and non-Hispanic Blacks had mean dietary fiber intake patterns that were not statistically different across survey years (P = 0.21 and P = 0.17, respectively), while non-Hispanic Whites had mean dietary fiber intakes that increased marginally across survey years (P = 0.05).
Figure 1.
Trends in Mean Dietary Fiber Intake among Non-pregnant US Adults, by Sex, Age, Race/Ethnicity, and Education, in NHANES 1999–2010.
Data from National Health and Nutrition Examination Survey, 1999–2010.
Dietary Fiber and Cardiometabolic Risks
The prevalence estimates of the metabolic syndrome, elevated CRP and obesity are displayed in Table 2, by socio-demographic and behavioral characteristics. Overall, participants with the metabolic syndrome, elevated CRP, and obesity consumed lower amounts of dietary fiber, but also had lower reported energy intake.
Table 2.
Descriptive Characteristics for all Non-pregnant Adults 20+ Years by Presence of Metabolic Syndrome,a Inflammation,b and Obesity,b NHANES 1999–2010.
| Metabolic syndrome – Present a N =3,780 |
Metabolic syndrome – Absent a N =6,693 |
C-reactive protein > 3.0 mg/L N =8,877 |
C-reactive protein ≤ 3.0 mg/L N =14,291 |
Body mass index ≥ 30.0 kg/m2 N =8,158 |
Body mass index < 30.0 kg/m2 N =15,010 |
|
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Total Population, % | 32.3 | 67.7 | 34.9 | 65.1 | 33.5 | 66.5 |
| Age | ||||||
| 20–50 years | 23.9 | 76.1 | 31.4 | 68.6 | 31.7 | 68.3 |
| 51+ years | 45.0 | 55.0 | 40.1 | 59.9 | 36.1 | 63.9 |
| Gender | ||||||
| Male | 32.7 | 67.3 | 27.8 | 72.3 | 31.8 | 68.2 |
| Female | 31.9 | 68.1 | 42.0 | 58.1 | 35.2 | 64.8 |
| Race/Ethnicity | ||||||
| Mexican-American | 33.4 | 66.6 | 36.7 | 63.3 | 35.5 | 64.5 |
| Non-Hispanic White | 32.9 | 67.1 | 33.6 | 66.4 | 31.7 | 68.3 |
| Non-Hispanic Black | 27.0 | 73.0 | 42.5 | 57.5 | 44.3 | 55.7 |
| Education | ||||||
| Less than 9th grade | 40.7 | 59.3 | 40.4 | 59.6 | 34.8 | 65.2 |
| 9–12th grade, but no HS diploma | 38.7 | 61.3 | 41.3 | 58.7 | 36.6 | 63.4 |
| HS diploma/GED | 37.9 | 62.1 | 37.0 | 63.1 | 35.3 | 64.7 |
| Some college, Associate’s degree | 31.5 | 68.5 | 35.7 | 64.3 | 36.1 | 63.9 |
| Bachelor’s degree or greater | 22.6 | 77.4 | 27.5 | 72.5 | 26.7 | 73.3 |
| Behaviors | ||||||
| Smoking Status | ||||||
| Current smoker | 29.5 | 70.5 | 37.9 | 62.1 | 27.1 | 72.9 |
| Former smoker | 38.3 | 61.7 | 35.9 | 64.1 | 36.4 | 63.6 |
| Never smoker | 30.4 | 69.6 | 33.0 | 67.0 | 35.0 | 65.0 |
| Dietary Intake | ||||||
| Mean dietary fiber intake (g) (± SE) | 15.5 ± 0.2 | 16.3 ± 0.2 | 14.5 ± 0.2 | 17.0 ± 0.2 | 15.5 ± 0.2 | 16.5 ± 0.2 |
| Mean energy intakec (kcal) (± SE) | 2147.8 ± 21.4 | 2261.3 ± 15.5 | 2082.4 ± 14.4 | 2304.6 ± 11.8 | 2190.6 ± 16.0 | 2245.3 ± 11.7 |
| Physical Activity 1999–2006 d | ||||||
| No activity | 39.7 | 60.3 | 43.8 | 56.2 | 37.6 | 62.4 |
| Some/Irregular activity | 34.6 | 65.4 | 36.2 | 63.8 | 34.4 | 65.6 |
| Regular activity | 25.3 | 74.7 | 29.3 | 70.7 | 26.5 | 73.5 |
| Physical Activity 2007–2010 d | ||||||
| No activity | 40.2 | 59.8 | 40.1 | 59.9 | 42.1 | 57.9 |
| Some/Irregular activity | 28.3 | 71.7 | 32.2 | 67.9 | 34.3 | 65.7 |
| Regular activity | 22.7 | 77.3 | 23.6 | 76.4 | 27.8 | 72.3 |
Data from National Health and Nutrition Examination Survey, 1999–2010.
The ATPIII clinical criteria were used to define metabolic syndrome. Metabolic syndrome was defined as having at least 3 of the 5 following cardiometabolic risk factors: high waist circumference (waist circumference > 102 cm for males or > 88 cm for females); elevated blood pressure (blood pressure ≥ 130/85 mmHg); elevated triglycerides (triglyceride concentration ≥ 150 mg/dL); low HDL cholesterol (HDL cholesterol levels < 40 mg/dL for males or < 50 mg/dL for females); and elevated fasting glucose (fasting plasma glucose ≥ 100 mg/dL).
Inflammation was defined as having a CRP concentration > 3.0 mg/L, while obesity was characterized as having a BMI ≥ 30 kg/m2.
Energy intake categories based on the US Department of Health and Human Services’ 2010 Dietary Guidelines for Americans. “Low” includes males with < 2000 kcal/day and females with < 1600 kcal/day. “Adequate” includes males with 2000–3000 kcal/day and females with 1600–2400 kcal/day. “High” includes males with > 3000 kcal/day and females with >2400 kcal/day.
Due to methodological changes in physical activity measurement between 2006 and 2007, physical activity was assessed separately in 1999–2006 and 2007–2010. Physical activity categories based on the US Department of Health and Human Services’ 2008 Physical Activity Guidelines for Americans. “No activity” includes participants with no moderate or vigorous physical activity. “Some/Irregular activity” includes participants with < 150 minutes/week of moderate activity or < 75 minutes/week of vigorous activity. “Regular activity” includes participants with ≥ 150 minutes/week of moderate activity, ≥ 75 minutes/week of vigorous activity, or ≥ 150 minutes/week of a combination of moderate and vigorous activity.
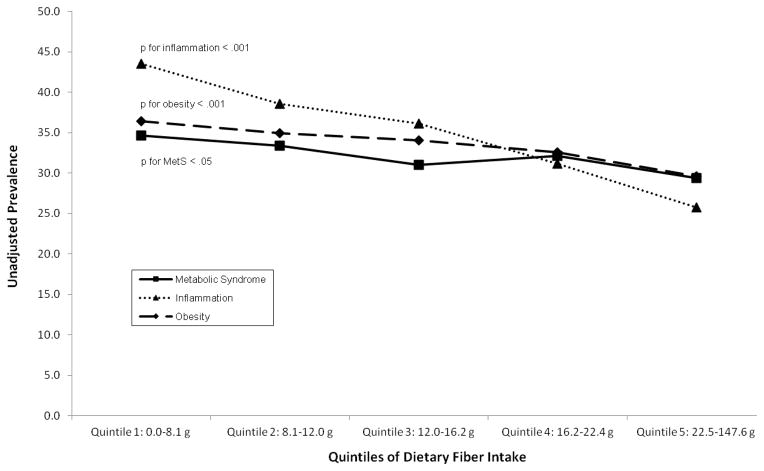
The unadjusted prevalence of cardiometabolic risks by quintiles of dietary fiber intake is presented in Figure 2. Overall, the prevalence of the metabolic syndrome, inflammation, and obesity each decreased with increasing quintiles of dietary fiber intake (P < 0.05, P < 0.001 and P < 0.001, respectively). The highest unadjusted prevalence of the metabolic syndrome (34.7%), inflammation (43.5%), and obesity (36.4%) was observed among participants in the lowest quintile of dietary fiber intake (0.0–8.1 g).
Figure 2.
Prevalence of Cardiometabolic Risks by Quintiles of Dietary Fiber Intake among Non-pregnant Adults 20+ Years, in NHANES 1999–2010.
Data from National Health and Nutrition Examination Survey, 1999–2010.
In Table 3, weighted multivariable regression models demonstrated an inverse association between dietary fiber intake and cardiometabolic risks. After adjusting for covariates, participants with higher intakes of dietary fiber were less likely to have the metabolic syndrome, inflammation, and be obese. This trend was consistent after adjusting for age, total energy intake, sex, race/ethnicity, educational attainment, and smoking status. Compared to participants in the lowest quintile of dietary fiber intake, participants in the highest quintile of dietary fiber intake had a statistically significant lower risk of having the metabolic syndrome (RR 0.78, 95% CI 0.70–0.88), inflammation (RR 0.66, 95% CI 0.61–0.72), and obesity (RR 0.77, 95% CI 0.71–0.84). Adding physical activity to the multivariable models produced similar results for adults in NHANES 1999–2006 and NHANES 2007–2010 (Appendix 1). Additionally, excluding participants with “extreme” dietary fiber intakes did not change our findings (Appendix 2).
Table 3.
Predicted Marginal Risk Ratios for Cardiometabolic Risk Factors, based on Quintiles of Dietary Fiber Intake and other Individual Covariates – Non-pregnant Adults 20+ Years in NHANES 1999–2010
| Predicted Marginal Risk Ratios (95% CI) a | |||
|---|---|---|---|
| Metabolic Syndrome | Inflammation | Obese | |
| Fully-Adj.b | Fully-Adj.b | Fully-Adj.b | |
| Quintiles of Dietary Fiber | |||
| 0.0–8.1 g | 1.00 | 1.00 | 1.00 |
| 8.1–12.0 g | 0.91 (0.82–1.00) | 0.90 (0.84–0.95) | 0.94 (0.88–1.00) |
| 12.0–16.2 g | 0.85 (0.76–0.93) | 0.86 (0.80–0.93) | 0.89 (0.83–0.95) |
| 16.2–22.4 g | 0.84 (0.75–0.93) | 0.76 (0.70–0.82) | 0.85 (0.80–0.92) |
| 22.5–147.6 g | 0.78 (0.70–0.88) | 0.66 (0.61–0.72) | 0.77 (0.71–0.84) |
Data from National Health and Nutrition Examination Survey, 1999–2010.
Estimates weighted to account for complex survey design in SUDAAN.
Fully-Adjusted - models adjusted for age, total energy intake, sex, race/ethnicity, educational attainment, and smoking status.
Associations stratified by racial/ethnic group differed by the cardiometabolic risk studied. Statistically significant decreases in the prevalence of inflammation were associated with increasing dietary fiber intakes for all groups. Statistically significant decreases in the risk of obesity and the metabolic syndrome were seen only among whites, though a protective trend was observed in all groups (Appendix 3).
DISCUSSION
Our findings indicate that among a nationally representative sample of non-pregnant US adults in NHANES 1999–2010, the consumption of dietary fiber was consistently below the recommended total adequate intake levels across survey years. Our study also confirms persistent differences in dietary fiber intake among sex, socioeconomic status, and racial/ethnic subpopulations over time.33 On average, young males consumed almost 20 grams less dietary fiber than recommended amounts, with particularly low consumption by young non-Hispanic Black men. Older women had dietary fiber intakes that were closest, yet, still an average of 6 grams below recommended amounts of fiber for their age group. Importantly, lower dietary fiber intake was associated with a higher prevalence of cardimetabolic risks among US adults.
Our findings are consistent with prior literature suggesting a lack of improvement in US dietary fiber intake trends over time, as well as socio-demographic differences in fiber intake.16, 19, 33 These data support prior recommendations to improve strategies that increase dietary fiber intake among US adults.34 To this end, the 2010 Scientific Statement from the American Heart Association on interventions to improve lifestyle changes in dietary intake and physical activity reviewed over 74 studies, and describe 18 interventions directed toward increasing fruit and vegetable intake; six of the studies focused on increasing fiber intake.35 Successful approaches to increase fiber intake included: (1) individual-based counseling from health educators using goal setting, problem solving, and telephone follow up for support and reinforcement; (2) group and individual sessions that employ reflective listening and self-monitoring techniques; as well as (3) community and internet based strategies, including interventions at point of sale in supermarkets.36–40 Additional research is needed to determine effective clinical and population-based strategies for improving fiber intake trends in diverse groups.
Our study has strengths and limitations that should be considered. We cannot infer causal interpretations of the relation between dietary fiber intake and cardiometabolic risks due to the cross-sectional design of the study. Moreover, we were unable to estimate separate associations between cardiometabolic risks and soluble or insoluble fiber, fiber supplements, or with specific sources of fiber which may have differential impacts on cardiovascular disease risks.2, 10, 41 Recent small-scale intervention studies have used dietary sources and psyllium supplements at high levels (at or in excess of 30g/day) to achieve reductions in inflammation, BMI, and other cardiometabolic risk factors.42, 43 Additional large scale epidemiologic and randomized intervention studies are needed to refine recommendations on the sources and quantities of dietary fiber, or fiber from supplemental sources, that may lower cardiometabolic risks in diverse groups.
Additional limitations include the fact that we reported dietary fiber intake, and did not report on functional or synthetic (supplemental) fiber intake, which may under-estimate total fiber intake of US adults. Moreover, we modeled dietary fiber intake based on a single 24-hour dietary recall survey, which may have led to misclassification of fiber intake. We also cannot exclude recall bias during the assessment of sources of fiber intake. Validation study data from Conway et al. suggests that the United States Department of Agriculture 5-step multiple pass dietary recall methodology used by NHANES provides self-reported macronutrient and energy intake that are within 10% of actual intakes among men and women.44,45 Additionally, we note that earlier nationally representative data collected between 1995 and 1996 from the National Institutes of Health AARP Diet and Health study provide a more complete assessment of fiber intake than the NHANES surveys by using 124-item food-frequency questionnaires to collect data on usual frequency of intake over 12 months, and with data from 2 nonconsecutive 24-hour recalls.1 Similar to the NHANES estimates, NIH AARP data also reported similarly low fiber intake, with energy-adjusted dietary fiber values ranging from 11 and 13 g/day for women and men, respectively, at the 10th percentile of intake, to 26 to 29 g/day at the 90th percentile. Such data are consistent with our results using a single 24-hour recall to assess fiber intake.
Despite above limitations, our study has important strengths, including the large nationally representative sample in NHANES that allows examination of trends in diverse groups. Additionally, our results are robust to the potential influence of extreme reporting of fiber intake.
In summary, our study shows that fiber consumption among US adults has remained consistently low between 1999 and 2010. There are also significant differences in dietary fiber intake by sex, racial/ethnicity, and socioeconomic status. Our findings underscore the need for additional randomized controlled trial data to shape recommendations for dietary fiber intake as a preventive strategy to reduce associated cardiometabolic risks. Additional nutritional policies may be needed to increase adequate consumption of dietary fiber, in order to reduce cardiometabolic risk factors in diverse US populations. Continued monitoring and surveillance of fiber intake trends are also warranted.
Dietary fiber intake has been consistently below recommended adequate intake levels for all US adults from 1999 to 2010.
Lower dietary fiber intake is found to be associated with a higher prevalence of cardiometabolic risks including metabolic syndrome, cardiovascular inflammation, and obesity among US adults.
Additional clinical and population-based strategies may be needed to increase recommended adequate fiber intake for US adults.
Acknowledgments
Financial support: Institutional financial support from Partners HealthCare and The Brigham and Women’s Hospital Center for Community Health and Health Equity
This research was supported by institutional support from the Center for Community Health and Health Equity at Brigham and Women’s Hospital and Partners HealthCare, Inc. The authors would like to acknowledge the kind intellectual and institutional support of Ms. Wanda McClain from the Community Health and Health Equity and Ms. Ronnie Sanders from Partners HealthCare. Dr. Cheryl Clark was supported by funding from the National Institute on Aging (NIH K08 AG 032357).
Footnotes
Authorship: All authors who had access to the study data and contributed to the findings and conclusions of this manuscript have been included in the authorship of this manuscript.
Conflict of interest: No authors have any conflict of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Park Y, Subar AF, Hollenbeck A, Schatzkin A. Dietary fiber intake and mortality in the NIH-AARP Diet and Health Study. Arch Intern Med. 2011;171(12):10611068. doi: 10.1001/archinternmed.2011.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erkkila AT, Lichtenstein AH. Fiber and cardiovascular disease risk: how strong is the evidence? J Cardiovasc Nurs. 2006;21(1):3–8. doi: 10.1097/00005082-200601000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Whelton SP, Hyre AD, Pedersen B, Yi Y, Whelton PK, He J. Effect of dietary fiber intake on blood pressure: a meta-analysis of randomized, controlled clinical trials. J Hypertens. 2005;23(3):475–481. doi: 10.1097/01.hjh.0000160199.51158.cf. [DOI] [PubMed] [Google Scholar]
- 4.Pereira MA, O’Reilly E, Augustsson K, et al. Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch Intern Med. 2004;164(4):370–376. doi: 10.1001/archinte.164.4.370. [DOI] [PubMed] [Google Scholar]
- 5.Cabello-Saavedra E, Bes-Rastrollo M, Martinez JA, et al. Macronutrient intake and metabolic syndrome in subjects at high cardiovascular risk. Ann Nutr Metab. 2010;56(2):152–159. doi: 10.1159/000280104. [DOI] [PubMed] [Google Scholar]
- 6.Carlson JJ, Eisenmann JC, Norman GJ, Ortiz KA, Young PC. Dietary fiber and nutrient density are inversely associated with the metabolic syndrome in US adolescents. J Am Diet Assoc. 2011;111(11):1688–1695. doi: 10.1016/j.jada.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Bo S, Durazzo M, Guidi S, et al. Dietary magnesium and fiber intakes and inflammatory and metabolic indicators in middle-aged subjects from a population-based cohort. Am J Clin Nutr. 2006;84(5):1062–1069. doi: 10.1093/ajcn/84.5.1062. [DOI] [PubMed] [Google Scholar]
- 8.Ajani UA, Ford ES, Mokdad AH. Dietary fiber and C-reactive protein: findings from national health and nutrition examination survey data. J Nutr. 2004;134(5):1181–1185. doi: 10.1093/jn/134.5.1181. [DOI] [PubMed] [Google Scholar]
- 9.Slavin JL. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2008;108(10):1716–1731. doi: 10.1016/j.jada.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Brown L, Rosner B, Willett WW, Sacks FM. Cholesterol-lowering effects of dietary fiber: a meta-analysis. Am J Clin Nutr. 1999;69(1):30–42. doi: 10.1093/ajcn/69.1.30. [DOI] [PubMed] [Google Scholar]
- 11.Marlett JA, McBurney MI, Slavin JL. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2002;102(7):993–1000. doi: 10.1016/s0002-8223(02)90228-2. [DOI] [PubMed] [Google Scholar]
- 12.King DE, Egan BM, Geesey ME. Relation of dietary fat and fiber to elevation of C-reactive protein. Am J Cardiol. 2003;92(11):1335–1339. doi: 10.1016/j.amjcard.2003.08.020. [DOI] [PubMed] [Google Scholar]
- 13.Schneeman BO. Dietary fiber and gastrointestinal function. Nutr Rev. 1987;45(7):129–132. doi: 10.1111/j.1753-4887.1987.tb06343.x. [DOI] [PubMed] [Google Scholar]
- 14.Liese AD, Schulz M, Fang F, et al. Dietary glycemic index and glycemic load, carbohydrate and fiber intake, and measures of insulin sensitivity, secretion, and adiposity in the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2005;28(12):2832–2838. doi: 10.2337/diacare.28.12.2832. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine. Report of the Panel on Macronutrients Staff, Subcommittees on Upper Reference Levels of Nutrients, Interpretation, Uses of Dietary Reference Intakes Staff, Standing Committee on the Scientific Evaluation of Dietary Reference Intakes Staff. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) Washington, DC: National Academies Press; 2005. Summary Tables, Dietary Reference Intakes; pp. 1319–1332. [Google Scholar]
- 16.King DE, Mainous AG, Lambourne CA. Trends in dietary fiber intake in the United States, 1999–2008. J Acad Nutr Diet. 2012;112(5):642–648. doi: 10.1016/j.jand.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 17.National Center for Health Statistics, National Health and Nutrition Examination Survey Data 1999–2010. [Accessed March 27, 2013.];Centers for Disease Control and Prevention Web Site. http://www.cdc.gov/nchs/nhanes.htm.
- 18.Kant AK, Graubard BI. 20-Year trends in dietary and meal behaviors were similar in U.S. children and adolescents of different race/ethnicity. J Nutr. 2011;141(10):1880–1888. doi: 10.3945/jn.111.144915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oza-Frank R, Cheng YJ, Narayan KM, Gregg EW. Trends in nutrient intake among adults with diabetes in the United States: 1988–2004. J Am Diet Assoc. 2009;109(7):1173–1178. doi: 10.1016/j.jada.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 20.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 21.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 22.Rifai N, Ridker PM. Population distributions of C-reactive protein in apparently healthy men and women in the United States: implication for clinical interpretation. Clin Chem. 2003;49(4):666–669. doi: 10.1373/49.4.666. [DOI] [PubMed] [Google Scholar]
- 23.Ford ES, Giles WH, Mokdad AH, Myers GL. Distribution and correlates of C-reactive protein concentrations among adult US women. Clin Chem. 2004;50(3):574–581. doi: 10.1373/clinchem.2003.027359. [DOI] [PubMed] [Google Scholar]
- 24.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics. National Health and Nutrition Examination Survey Laboratory/Medical Technologists Procedures Manual 2007–2008. US Dept of Health and Human Services, Centers for Disease Control and Prevention. National Center for Health Statistics (NCHS),Centers for Disease Control and Prevention; Apr, 2010. [Accessed 2013 Jul 24.]. [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) National Health and Nutrition Examination Survey Laboratory/Medical Technologists Procedures Manual. Hyattsville, MD: US Dept of Health and Human Services, Centers for Disease Control and Prevention; 2003–2004. [Google Scholar]
- 27.US Department of Health and Human Services. [Accessed March 27, 2013.];Dietary Guidelines for Americans. http://www.health.gov/dietaryguidelines.
- 28.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 29.Willett WC, Stampfer MJ. Implications of Total Energy Intake for Epidemiologic Analyses. In: Willett WC, editor. Nutritional Epidemiology. 2. New York, NY: Oxford University Press; 1998. pp. 273–301. [Google Scholar]
- 30.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65(4 Suppl):1220S–1228S. doi: 10.1093/ajcn/65.4.1220S. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics. National Health and Nutrition Examination Survey: Survey Questionnaires, Examination Components and Laboratory Components 2007–2008. National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention; May 14, 2010. [Accessed Aug 1, 2012.]. [Google Scholar]
- 32.US Department of Health and Human Services. [Accessed March 27, 2013.];Physical Activity Guidelines for Americans. 2008 http://www.health.gov/paguidelines/guidelines.
- 33.Lanza E, Jones DY, Block G, Kessler L. Dietary fiber intake in the US population. Am J Clin Nutr. 1987;46(5):790–797. doi: 10.1093/ajcn/46.5.790. [DOI] [PubMed] [Google Scholar]
- 34.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, et al. Diet and lifestyle recommendations revision 2006 A scientific statement from the American Heart Association nutrition committee. Circulation. 2006;114:82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 35.Artinian NT, Fletcher GF, Mozaffarian D, et al. American Heart Association Prevention Committee of the Council on Cardiovascular Nursing. Interventions to Promote Physical Activity and Dietary Lifestyle Changes for Cardiovascular Risk Factor Reduction in Adults A Scientific Statement From the American Heart Association. Circulation. 2010;122(4):406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glasgow RE, Toobert DJ. Brief, computer-assisted diabetes dietary self-management counseling: effects on behavior, physiologic outcomes, and quality of life. Med Care. 2000;38(11):1062–1073. doi: 10.1097/00005650-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Eakin EG, Bull SS, Riley KM, Reeves MM, McLaughlin P, Gutierrez S. Resources for health: a primary-care-based diet and physical activity intervention targeting urban Latinos with multiple chronic conditions. Health Psychol. 2007;26(4):392–400. doi: 10.1037/0278-6133.26.4.392. [DOI] [PubMed] [Google Scholar]
- 38.Howard BV, Van Horn L, Hsia J, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295(6):655–666. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- 39.Anderson ES, Winett RA, Wojcik JR, Winett SG, Bowden T. A computerized social cognitive intervention for nutrition behavior: direct and mediated effects on fat, fiber, fruits, and vegetables, self-efficacy, and outcome expectations among food shoppers. Ann Behav Med. 2001;23(2):88–100. doi: 10.1207/S15324796ABM2302_3. [DOI] [PubMed] [Google Scholar]
- 40.Delichatsios HK, Friedman RH, Glanz K, et al. Randomized trial of a “talking computer” to improve adults’ eating habits. Am J Health Promot. 2001;15(4):215–224. doi: 10.4278/0890-1171-15.4.215. [DOI] [PubMed] [Google Scholar]
- 41.Ma Y, Griffith JA, Chasan-Taber L, et al. Association between dietary fiber and serum C-reactive protein. Am J Clin Nutr. 2006;83(4):760–766. doi: 10.1093/ajcn/83.4.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.King DE, Egan BM, Woolson RF, Mainous AG, III, Al-Solaiman Y, et al. Effect of a high-fiber diet vs a fiber-supplemented diet on C-reactive protein level. Arch Intern Med. 2007;167:502. doi: 10.1001/archinte.167.5.502. [DOI] [PubMed] [Google Scholar]
- 43.Pal S, Khossousi A, Binns C, Dhaliwal S, Ellis V. The effect of a fibre supplement compared to a healthy diet on body composition, lipids, glucose, insulin and other metabolic syndrome risk factors in overweight and obese individuals. Brit J Nutr. 2011;105:90. doi: 10.1017/S0007114510003132. [DOI] [PubMed] [Google Scholar]
- 44.Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77:1171–8. doi: 10.1093/ajcn/77.5.1171. [DOI] [PubMed] [Google Scholar]
- 45.Conway JM, Ingwersen LA, Moshfegh AJ. Accuracy of dietary recall using the USDA five-step multiple-pass method in men: an observational validation study. J Am Diet Assoc. 2004;104(4):595–603. doi: 10.1016/j.jada.2004.01.007. [DOI] [PubMed] [Google Scholar]