Abstract
Aims: Although Russia has one of the highest rates of alcohol consumption and alcohol-attributable burden of disease, little is known about the existing research on prenatal alcohol exposure (PAE) and Fetal Alcohol Spectrum Disorders (FASDs) in this country. The objective of this study was to locate and review published and unpublished studies related to any aspect of PAE and FASD conducted in or using study populations from Russia. Methods: A systematic literature search was conducted in multiple English and Russian electronic bibliographic databases. In addition, a manual search was conducted in several major libraries in Moscow. Results: The search revealed a small pool of existing research studies related to PAE and/or FASD in Russia (126: 22 in English and 104 in Russian). Existing epidemiological data indicate a high prevalence of PAE and FASD, which underlines the strong negative impact that alcohol has on mortality, morbidity and disability in Russia. High levels of alcohol consumption by women of childbearing age, low levels of contraception use, and low levels of knowledge by health and other professionals regarding the harmful effects of PAE put this country at great risk of further alcohol-affected pregnancies. Conclusions: Alcohol preventive measures in Russia warrant immediate attention. More research focused on alcohol prevention and policy is needed in order to reduce alcohol-related harm, especially in the field of FASD.
INTRODUCTION
Russia has one of the highest rates of alcohol consumption in the world. According to the Global Burden of Disease Study (2010), alcohol use is the second leading risk factor contributing to the disease burden in Russia (Institute for Health Metrics and Evaluation, 2012). The World Health Organization (WHO) European and Global Status Report on Alcohol and Health reported that on average, for 2003–2005, the level of per capita consumption of pure alcohol in liters among adults older than 15 years of age reached 26.7 l (16.3 l for women and 35.4 l for men; WHO, 2010, 2011). In Russia, 5.8% of women and 22.1% of men are heavy episodic drinkers (i.e. consume at least 60 g or more of pure alcohol on at least one occasion weekly; WHO, 2010, 2011). The prevalence of alcohol use disorders is also high in Russia—2.6% for women and 16.3% for men (WHO, 2011). As a result, Russia is characterized as having the most risky pattern of drinking and the greatest alcohol-attributable burden of disease in the world.
A recent study conducted in Saint Petersburg and the Nizhnyi Novgorod region revealed that 89% of non-pregnant women reported consuming alcohol and 65% reported binge drinking in the past 3 months (Balachova et al., 2012a). Forty-seven percent of women in the Nizhny Novgorod region and 28% in Saint Petersburg reported at least one binge-drinking episode at least monthly. Women who might become pregnant consumed alcohol similar to women who were not likely to become pregnant, and 54% of women in the Nizhny Novgorod region and 32% of women in Saint Petersburg were considered to be at risk of having an alcohol-exposed pregnancy (Balachova et al., 2012a).
Popovitch et al. (2004) conducted a telephone-based behavioral risk factor surveillance survey in three Russian cities in 2000–2001. A random sample of 3032 residential telephone numbers was selected and 1693 interviews were conducted among adults 25–64 years of age in each selected household: 21% of women from Moscow, 8.2% of the women in Arkhangelsk and 10.8% of women in Murmansk abstain from alcohol. From 3 to 5% of women (and about 30% of men) in the above Russian cities consume >20 g of pure alcohol per day. Among women, about 30% of consumed beverages were spirits and 40% was beer. The highest level of hazardous alcohol consumption (>20 g of pure alcohol per day) among women was reported for those between 25 and 34 years of age, the most reproductive age group (Popovitch et al., 2004).
An article from the mid-1990s reported that 80–94% of high-school girls consumed alcohol and in major Russian cities, girls drank at the same level or higher than boys of the same age (Koshkina and Paronyan, 1995).
According to the official report of the Russian National Research Center on Addiction for 2011, the prevalence of alcoholism in the general population of Russia is estimated to be 1.4% (1402 per 100,000 persons), and ∼0.5% of women (505 per 100,000) have been diagnosed with alcoholism (Koshkina et al., 2012). A ratio of 1:5 (women:men) has been reported to exist between the genders (Altshuler, 2010). Given that the official figures are based on reported cases only, the actual number of cases of alcoholism among women in Russia may be higher (if unreported cases are considered; Kirganova, 2009). It has also been suggested that in Russia, from 1999 to 2003, the number of registered cases of alcoholism in women increased from 2.2 to 3.7% (Altshuler et al., 2006).
In addition to the alarming data on alcohol consumption by women in the general population, research indicates that there is a low level of contraception use. Only 49% of all women in Russia who have ever been sexually active use contraception, and that number increases to only 51% when women in the age group of 50–54 were excluded (Barden-O'Fallon et al., 2010). In another sample of 347 non-pregnant women 18–44 years of age recruited at women's clinics, 44% of women in Saint Petersburg and 70% in the Nizhny Novgorod region were sexually active and not using contraception consistently (Balachova et al., 2012a).
Due to high levels of alcohol consumption within the population, paired with low rate of contraceptive use, many Russian women of childbearing age are at risk of having an alcohol-exposed pregnancy, which may result in having a child with Fetal Alcohol Spectrum Disorder (FASD). FASD is a non-diagnostic umbrella term that is used to represent the full spectrum of birth defects that are caused by prenatal alcohol exposure (PAE), which encompasses four categorical diagnostic entities: fetal alcohol syndrome (FAS), partial FAS (pFAS), alcohol-related neurodevelopmental disorder (ARND) and alcohol-related birth defects (ARBD; Chudley et al., 2005). PAE is a leading preventable cause of the birth defects, which can include physical, mental, behavioral and/or learning disabilities with possible lifelong complications. In North America, the lifetime cost for some cases of FASD has been estimated to be more than one million dollars (Popova et al., 2011).
Despite the high risk of, and potentially high cost associated with, FASD in Russia, there are no official surveillance efforts targeting FASD and no social facilities for children and/or adults with FASD in the country. Furthermore, very little is known about the existing pool of research on PAE or FASD in Russia. Therefore, the purpose of this study was to perform a systematic literature review in order to locate published and unpublished studies related to any aspect of PAE and FASD that were conducted in Russia or used study populations from Russia.
METHODS
Systematic literature search
Participating researchers from Canada and from Russia simultaneously conducted a systematic literature search. The procedure varied due to the differences in the availability of sources of information. For detailed search strategy in both countries and results, see Supplementary material, File S1.
The search was not limited by language of publication and was conducted up to and including December 2012.
RESULTS
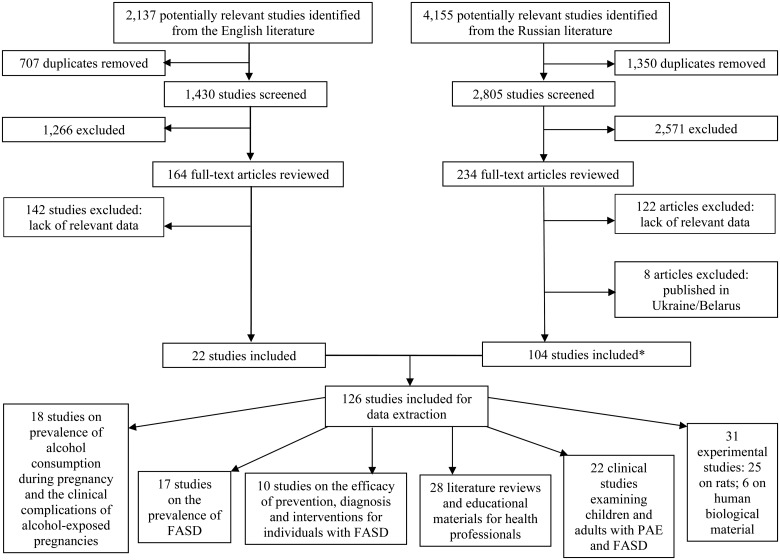
In total, 22 studies in English and 104 studies in Russian were included in the present review. The results of the search strategy are shown in Fig. 1.
Fig. 1.
Schematic diagram of the systematic search strategy. *Articles published in iteration are excluded from the total reported number of included studies.
The 126 examined studies were categorized into the following six major groups, those that:
assessed the prevalence of alcohol consumption during pregnancy and the clinical complications of alcohol-exposed pregnancies;
examined the prevalence of FASD in the general population, or other specific populations (e.g. orphanages);
assessed the efficacy of preventive measures, methods of diagnostics and interventions for individuals with FASD;
conducted literature reviews on FASD and developed educational materials for health professionals;
clinically examined children and adults and demonstrated the lifelong polysystemic teratogenic effects of alcohol on the fetus and
experimentally studied the teratogenic effects of alcohol on laboratory animals or human biological material.
A summary of all examined studies in chronological order is available in Supplementary material, Table S1.
Studies on the prevalence of alcohol consumption during pregnancy and the clinical complications of alcohol-exposed pregnancies
Some studies reported both the prevalence of alcohol consumption and clinical complications. Therefore, these studies have been categorized by the primary purpose of the study.
The prevalence of alcohol consumption during pregnancy
The search revealed 11 studies reporting the prevalence of alcohol consumption during pregnancy (see Supplementary material, Table S1). It was found that alcohol consumption during pregnancy in Russia varies from 3.1% (Talykova et al., 2007) to 83% (Kurianova et al., 2006) and heavy drinking during pregnancy varies from 0.2–1% (Radzinsky, 2002) to 9.2% (Shilko et al., 2011a). In a study by Kosyh et al. (2010) it was reported that 50% of females consumed seven or more alcoholic drinks during the 3 months prior to pregnancy. Chambers et al. (2006) conducted a longitudinal pregnancy outcome study in the Moscow Region of Russia and revealed that 52% used alcohol in their most recent month of pregnancy. Further, these authors reported that, of those ‘ever drinkers’, 4.8% had at least one episode of five or more standard drinks, and 10.5% had at least one episode of three or four standard drinks in the most recent month of pregnancy. The survey conducted by Kristjanson et al. (2007) in Saint Petersburg among 899 pregnant women revealed that 96% of them drank alcohol in the year before they became pregnant; of these women, 60% reported drinking when they knew they were pregnant, and 35% had reported drinking within the past 30 days. Among pregnant women who drank within the past 30 days, 7.4% reported having 5 or more drinks on at least 1 occasion. One recent study reported that 16% of pregnant women with disorders of the pancreas and liver practiced heavy drinking (Egorova et al., 2012). The drink of choice among pregnant Russian women was reported most commonly as wine, sparkling wine and beer (Kurianova et al., 2006; Kurianova, 2006; Sashchenko, 2007; Kalinina et al., 2012).
Several studies revealed that Russian women substantially reduce their alcohol consumption after pregnancy recognition, when compared with pre-pregnancy levels (Balachova et al., 2012a; Gaidukov et al., 2008); however, about 20% continued to consume alcohol after pregnancy recognition (Balachova et al., 2012a). Binge drinking after pregnancy recognition declined by a factor of 10, but did not disappear completely; ∼6% of women had at least one binge episode.
It is important to note that the levels of alcohol consumption during pregnancy within all of the reviewed studies were based on maternal self-reports, which are likely to be imprecise and most likely underreported due to bias (e.g. recall and social desirability biases). Furthermore, the term ‘standard drink’ is not a term commonly used in Russia; therefore, the respondents may have had difficulty understanding this concept. In addition, there were inconsistencies between studies in the definition of a ‘binge drinking’. For example, Balachova et al. (2012a) defined binging as ‘four or more standard drinks on a single occasion’, while Chambers et al. (2006) defined binge drinking as an episode of ‘five or more drinks’.
It should also be noted that Russia is geographically large and culturally diverse; therefore, regional variations are important. Thus, findings on the prevalence and patterns of alcohol consumption during pregnancy from individual studies may not be representative of all Russian women.
The clinical complications of alcohol-exposed pregnancies
There were seven studies describing the clinical complications of alcohol-exposed pregnancies in Russia (Supplementary material, Table S1). The research studies included in this analysis have reported that alcohol consumption during pregnancy increases the risk of miscarriage (Sashchenko, 2007; Komarova, 2008), fetoplacental insufficiency (Orazmuradov et al., 2007), premature or accelerated delivery (Komarova, 2008; Alekseeva, 2011a,b), pathology of amniotic fluid (Komarova, 2008; Alekseeva, 2011a,b) and disturbances in the mother's immune system (Kurianova et al., 2006; Sashchenko, 2007; Komarova, 2008). Several other research studies reported that alcohol consumption during pregnancy decreases the levels of zinc and copper in the blood stream of pregnant women, as well as the levels of cobalt, iodine, magnesium and phosphorus in pregnant women's hair (Ogotoeva and Borisova, 2008; Ogotoeva et al., 2009a,b; Alekseeva, 2011a,b). Furthermore, these studies reported that newborns of these mothers are deficient in certain essential minerals, such as cobalt, iron, iodine and zinc, and have increased levels of lithium and nickel. Shilko et al. (2010c, 2011c) stated that increased levels of transforming growth factor (TGF-β1), found in the blood of alcohol misusing pregnant women, might explain the growth retardation in newborns.
Due to the small sample sizes of the studies presented above (Orazmuradov et al., 2007; Ogotoeva and Borisova, 2008; Ogotoeva et al., 2009a,b; Uliyanovskaia and Solovev, 2010; Shilko et al., 2010c, 2011c; Kalinina et al., 2012), and the fact that the level of alcohol consumption during pregnancy was not defined, was based on self-reported data obtained via unstructured interviews, and the timing of alcohol use was not specified (i.e., first, second or third trimester; Shilko et al., 2010c, 2011c; Alekseeva, 2011a,b; Alekseeva and Ivanova, 2011; Kalinina et al., 2012), these results should be interpreted with caution.
Studies reporting on prevalence of FASD
In total, 17 studies reported the prevalence of FASD in different populations of Russia (see, for example, Warren et al., 2001; Riley et al., 2003; Grigovich et al., 2006; Miller et al., 2007; Malakhova et al., 2008; Konovalova et al., 2009) (Supplementary material, Table S1). The prevalence of FAS in the general population was estimated in one study to be 18–19 per 1000 live births (Malakhova, 2012). However, a study of 326 kindergarten-aged children of the same area did not report any cases of FAS (Bubnov, 2009, 2010). The prevalence of FAS in maternity hospitals in Saint Petersburg was reported from 0.79 to 3.62 per 1000 live births; however, in specialized neonatal clinics it was almost 10 times higher—ranging from 3 to 35 per 1000 during 2000–2009 (Palchik et al., 2006; Palchik and Legonkova, 2011).
The prevalence of FAS in orphanages ranged from 46 (Legonkova, 2011; Palchik and Legonkova, 2011) to 340 (Sofronova and Palchik, 2012) per 1000 live births by Russian researchers and from 55 (Stromland et al., 2005) to 330 (The St. Petersburg-USA Orphanage Research Team, 2005) per 1000 live births by international researchers. For comparison purposes, it is believed that the prevalence rate of FAS in the North American general population is ∼1 per 1000 live births (Roberts and Nanson, 2000; May and Gossage, 2001).
Studies by Marincheva et al. (2003) reported the prevalence of FAS to be 129 per 1000 in a boarding orphanage, 58 per 1000 in boarding schools, 49 per 1000 in regular orphanages and 164 per 1000 in a school of the social welfare system. The highest prevalence of FAS was found in ‘psycho-correctional’ orphanages for children with special needs, ranging from about 427–680 per 1000 (Legonkova, 2011; Palchik and Legonkova, 2011).
The prevalence of FAS among adopted children from Russia (or in some cases, from Eastern Europe, including Russia) currently living in the USA was estimated to range from 15 to 70 per 1000 live births (Aronson, 2003; Robert et al., 2009). Farina et al. (2004) reported that 34% of children adopted from Russia were diagnosed with ARND. However, the records of alcohol-exposed pregnancy were significantly higher and constituted 19% (Albers et al., 1997) to 41% (McGuinness et al., 2000) of the cases. Albers et al. (1997) stressed that the majority of prospective adopting parents are concerned about the high risk of FASD among children adopted from Russia, due to the widespread availability of alcohol and the limited public awareness of alcohol's detrimental effects on the fetus.
The existing FASD prevalence estimates in Russia vary greatly from population to population and study to study. These variations may reflect not only differences in maternal drinking behavior, but also different diagnostic criteria, methods of case ascertainment (i.e. surveillance method) and populations surveyed in the different studies.
The existing studies have a number of limitations due to (a) inadequate and/or unavailable diagnostic capacity across the country and (b) lack of nation-wide diagnostic guidelines and definitions. Further, the studies presented above have weak methodologies, small sample sizes that are restricted to sub-populations, used convenience sampling and had a low response rate. There are also inconsistencies in the use of the terms ‘incidence’ and ‘prevalence’ across the studies.
Studies on FASD prevention, diagnostics and interventions
There were five studies found on selective prevention measurement, two on interventions, and three on diagnostic procedures (Jones et al., 2006; Shilko et al., 2008a, 2009c, 2010b, 2011a; Kuznetsova et al., 2011). (Supplementary material, Table S1).
The studies by Balachova et al. (2007) and Isurina et al. (2009) demonstrated that, in Russia, with the exception of pediatricians, professionals such as physicians, psychologists, nurses and social workers have insufficient knowledge about FASD and usually do not discuss the negative effects of alcohol consumption during pregnancy with their female patients. These studies also demonstrated that gynecologists and pediatricians often had misinformed or inconsistent attitudes toward alcohol exposure during pregnancy such as ‘it is tolerable to consume low doses of alcohol in cases involving a healthy pregnancy’ (a misinformed attitude). Pediatricians, who were characterized as having inconsistent attitudes, assumed that it is important to convince a woman to abstain from alcohol consumption during pregnancy; however, good quality alcoholic beverages can be consumed during the late stage of pregnancy. Only medical doctors specializing in addiction treatment stated that complete abstinence from alcohol during pregnancy is necessary. Despite the small number of participants, these results (Balachova et al., 2007; Isurina et al., 2009) indicate a lack of knowledge regarding the detrimental effects of alcohol use during pregnancy, even among highly educated individuals in Russia.
In a brief PAE prevention intervention based on evidence-based interventions using techniques of motivational interviewing (Balachova et al., 2010a,b), women were counseled to choose safe contraception or complete abstinence from alcohol consumption. It was recommended that gynecologists of the maternity welfare centers conduct this intervention because Russian women considered them as a reliable source of information (Moskalenko 2002, 2008a,b; Balachova et al., 2010a,b).
Balachova et al. (2012b) also evaluated different types of informational leaflets with positive (positive visual images, list of positive outcomes for baby's health in case of abstinence from alcohol), negative (negative visual images, list of negative consequences of alcohol consumption during the pregnancy) and neutral information (general information about healthy life style during pregnancy). The study found that information about FASD increases the general awareness of woman of childbearing age regarding FASD, stimulates them to consider changing their behavior toward abstinence from alcohol in case of pregnancy planning or pregnancy and decreases the level of alcohol consumption among women, in general. It was also found that women who read the leaflets with positive information had better memories and were able to reproduce factual information about FASD. However, women who read negative information were more likely to develop a strong decision to abstain from alcohol during pregnancy (Balachova et al., 2012b; Regentova, 2012).
As can be seen from the above, there are few published studies on FASD prevention, diagnosis and interventions in Russia. Studies of prevention efforts targeting high-risk women are completely absent.
Only two studies concerning the treatment of individuals with FAS were found in the Russian literature. Transcranial direct current stimulation was reported to be beneficial in normalizing the altered sleep-wake cycle in 13 children with FAS (Malakhova and Bubnov, 2011; Malakhova et al., 2011). Another study reported that after implementing peptide-antiminotoxic therapy on 56 children with FAS, an improvement in psychomotor development was observed in 56–77% of cases, while a positive effect of standard therapy on psychomotor development was observed in 45% cases (Khasianova, 2010). These studies should be considered with caution due to (a) the absence of an appropriate control group, (b) the lack of a clear definition of the outcomes, (c) small sample sizes and (d) lack of appropriate statistical analyses.
Literature reviews and educational materials for health professionals
The search revealed 28 literature reviews that included information on FASD for health professionals (see, for example, Petrov-Maslakov, 1961; Lezhepekova, 1981; Bakanov, 1986, 1999; Mastiukova, 1986, 1989; Skalny and Skosyreva, 1987; Radzinsky and Kostin, 2009; Popova, 2010). (Supplementary material, Table S1). The reviews provided information on a variety of topics including: the evaluation of medical views on the FASD problem through the years, descriptions of the mechanisms of the damaging effects of alcohol on a fetus, descriptions of the clinical characteristics of children with FAS (e.g. growth retardation, birth defects/abnormalities, changes in phenotype, and neurodevelopmental and intellectual disorders) and strategies for FASD prevention (see, for example, Badalyan, 1986; Tabolin and Uryvchikov, 1986; Alipov and Korkhov, 1988; Lisitcyn and Sidorov, 1990; Akhmadeeva, 1997; Ramazanova and Semiatov, 2002; Palchik and Shabalov, 2009; Balachova et al., 2012c).
An educational trial was conducted to evaluate FASD training developed for obstetricians/gynecologists and pediatricians (Balachova et al., 2010a,b). This study claimed that the inclusion of a 3-h FASD education module in continued medical education led to significant changes in physicians' knowledge, attitudes and skills necessary for diagnosing FASD and conducting brief prevention interventions. Furthermore, this study implemented new technologies to disseminate developed FASD education materials and designed the first internet-based FASD educational resource in the Russian language for physicians and other health professionals (www.NetFAS.net; Balachova et al., 2010a,b).
Several studies discussed the ways in which alcohol influences the development of FASD such as the direct damage of alcohol on sex cells, genitals (Koshkina et al., 1998; Shilko et al., 2008b), indirect autoimmune effects (Shilko et al., 2008b) and metabolic disturbance (Lebedev, 1974; Bakanov, 1986; Anokhina and Moskalenko, 1987; Garmasheva and Konstantinova, 1988). The negative effect of alcohol on newborns through breastfeeding has also been reported (Bisiarina and Lisitcyna, 1987; Koshkina et al., 1998). Additionally, some studies discuss the role of acetaldehyde in fetal central nervous system damage (Bakanov, 1986; Anokhina and Moskalenko, 1987; Garmasheva and Konstantinova, 1988). These studies report that an increase in acetaldehyde, ethanol's metabolite, due to insufficient maternal alcohol dehydrogenase activity, is the leading damaging factor in FAS development.
Several studies underline the dose-dependent effect of alcohol on the fetus. Some studies suggest that consumption of 60–80 g of pure alcohol per day leads to FAS (Frolova and Nikolaeva, 1987), while others report that consumption of 150 g of pure alcohol per day increases the chance of FAS development by 50% (Koshkina et al., 1998).
Interestingly, in the older Russian sources from the 1980s, the detrimental effects of alcohol on the fetus were described and pregnancy termination for women with alcohol dependency was strongly recommended (Skosyreva, 1980; Kirushenkov, 1986).
As can be seen from the literature reviews listed above, the majority of them are outdated—70% were published before 2000. In addition, most of the existing reviews only provide general information on FAS. Information pertaining to the practical aspects of diagnostics, treatment, care and prevention are only touched on very briefly. Thus, they are extremely limited in their clinical applicability.
Clinical studies examining children and adults
There were 22 clinical studies conducted on children affected by FASD (Supplementary material, Table S1). These studies provide a description of neurodevelopmental, mental, cardiovascular, gastrointestinal, metabolic and other disorders presented in children with PAE and/or FASD. (Semenov et al., 1987; Donetc, 1992; Erokhova and Bozhenov, 1997; Grjibovski et al., 2002, 2004; Khatckel and Popov, 2005, 2009a,b, 2011; Miller et al., 2006; Ruchkin et al., 2008; Palchik et al., 2009, 2011; Kashirskaya, 2010; Khoroshkina and Krivtcova, 2010; Sheffer, 2012).
The majority of these studies have serious limitations, including: (a) small sample sizes (Shurygin, 1974; Usova et al., 1981; Grechany, 2002; Legonkova and Palchik, 2009), (b) lack of a control group (Usova et al., 1981; Gummel et al., 2007a,b; Khatckel and Popov, 2011) and (c) a failure to properly confirm PAE and thus, a failure to properly establish an FASD diagnosis (Shurygin, 1974; Kunikovskaia, 1980; Kornilov et al., 2005; Sokolovskaya et al., 2009). Most importantly, in all of the existing clinical studies examining children and adults a standardized diagnostic procedure was not used/indicated.
Experimental studies with laboratory animals or human embryos
The search revealed 25 experimental research studies conducted on rats (see, for example, Skosyreva, 1973; Skosyreva et al., 1973; Anokhina et al., 1989; Kolomeitceva et al., 1989; Maizelis et al., 1989; Nozdracheva et al., 1989; Zabludovsky et al., 1989; Zhulin and Bazyan, 1989; Chebotar and Konopistceva, 1993; Omelianchik et al., 1993; Kataeva et al., 2004; Kurch, 2004, 2011; Sverdlova, 2008; Vyatchanina and Skalny, 2009; Arzamasova, 2011; Pugach, 2012; Shabanov et al., 2012) and 6 studies using human biological material (Kovetcky et al., 1991a,b; Kuteneva et al., 2005; Solonsky, 2006, 2008; Shushpanova and Solonsky, 2012) (Supplementary material, Table S1). The majority of these studies reported polysystemic pathology due to PAE that affects growth, organ development, metabolism, micro- and macro-element balance and neurocognitive functioning. Experimental studies of rats further reinforce the knowledge on the negative effects of alcohol consumption during pregnancy, such as the possibility of depression-like symptoms or memory disorders in the newborns (Kolomeitceva and Levina, 1989). Furthermore, studies using human biological material demonstrated that when a mother consumes alcohol the embryo may develop many different deviations in brain development (Kovetcky et al., 1991a; Solonsky, 2006, Solonsky and Logvinov, 2008). The details of these studies can be found in the Supplementary material, Table S1.
Many experimental research studies have serious limitations; they used small sample sizes (Skalny et al., 2001; Shilko et al., 2009a,b, 2010a,c, 2011b,c), did not describe their sample(s) (Skalny et al., 2009; Morozova and Popova, 2010; Kurch, 2011) and did not present statistical significance (for example, Babenko and Skalny, 1986; Artiukhina et al., 1989).
DISCUSSION
Overall, in the last five decades (the first identified article is dated as 1961), 126 studies related to alcohol consumption during pregnancy and FASD were found that were published in Russia (or on Russian samples). This seems low considering Russia's large area and population [17.1 million km2; 143 million people as of 2012 according to the Federal State Statistics Service of Russian Federation (FSSS; FSSS, 2012)]. This is also surprising given that Russia has one of the highest rates of alcohol consumption in the world. This leaves us with the question ‘why is there such a low interest in this issue in the Russian research community?’
The reviewed studies suffer multiple methodological limitations and weaknesses outlined in the results section and thus, should be viewed with appropriate caution. Despite the limitations, these studies demonstrate a high level of alcohol consumption among Russian women of childbearing age, a low level of contraception usage and an especially high proportion of pregnant women with a pattern of heavy drinking. Based on these findings, it is conceivable that the prevalence of FASD is likely to be high in the general population of Russia.
The present systematic literature review revealed that only a few epidemiological studies reporting the prevalence of FASD exist. However, the reported figures are not generalizable to the general Russian population due to the methodological limitations of the studies (e.g. conducted in small communities with small sample sizes, or conducted among special populations). Valid population-based epidemiological studies are needed to examine the prevalence of FASD in both the general population and populations likely to be at high risk of PAE in Russia. Such information is crucial for understanding the magnitude of the problem and for initiating preventative measures at the country level.
The present review also revealed that the existing research on the negative effects of PAE and FASD available to health and other professionals is not only limited, but also outdated, as the majority of these studies have been published prior to 2000. Moreover, medical education rarely ever includes a course describing the negative consequences of alcohol consumption during pregnancy; most medical doctors are not trained to recognize the clinical features of FASD in Russia (Isurina et al., 2009).
Aside from medical doctors, other health and human services professionals (for example, social workers) are well positioned to help prevent FASD and to intervene with individuals and families affected by FASD. A major setback is that these professionals are also lacking appropriate knowledge and skills regarding the consequences of PAE in Russia (Balachova et al., 2007, 2010a,b). Given the exceptionally high prevalence of children with FASD in foster care, orphanages and other child welfare systems in Russia, there is a need for proper training for professionals in these systems in order to be able to recognize a child with behavioral and/or mental health problems that may be the result of PAE. It is important to make educational materials available to a variety of professionals—such as guidelines for diagnosing and working with individuals already affected, as well as their parents and caregivers.
As a result of the limited research and medical and other educational information, the awareness and knowledge of Russian medical professionals, psychologists, social workers and other professionals about harmful effects of alcohol consumption during pregnancy and FASD is extremely limited (Balachova et al., 2007, 2010a,b; Isurina et al., 2009). There is a large discrepancy between the number of individuals who need to be diagnosed with FASD and receive proper care and the number of available professionals able to provide a proper diagnosis, treatment and other support services.
There is an urgent need to reduce the harmful use of alcohol among women of childbearing age in Russia and initiate prevention strategies targeting pregnant women. Prevention efforts need to be widely spread and should target women of childbearing age and clearly state that there is no safe time to consume alcohol during pregnancy, nor is there a safe amount or type of alcohol. The present literature review presents some effective strategies that could be implemented in these types of FASD prevention programs. For instance, Moskalenko (2002, 2008a,b) advises that the main method of preventing alcohol intake during pregnancy should involve informing women through primary care physicians, and to use positive reinforcement rather than threats. Also, several studies point out that there are misconceptions about FASD, as well as lack of awareness of FASD symptomatology (Balachova et al., 2007). Improving awareness could be an effective way to minimize drinking in women of childbearing age. A randomized educational trial indicated that including FASD information in standard continuing medical education courses significantly improves physicians' knowledge, attitudes and skills (Balachova et al., 2010a). Another study suggests that simple interventions such as distributing leaflets containing both positive and negative information about the consequences of drinking during pregnancy increase the general awareness of women of childbearing age and their attitudes about FASD (Balachova et al., 2012b; Regentova, 2012). Thus, such research studies are a valuable tool for structuring FASD prevention programs that target women who may become pregnant.
As the literature indicates, the population of alcohol-dependent women in Russia is large; however, the principles of prevention measures and interventions for alcohol-dependent women are underrepresented in the Russian professional literature. This means that the at-risk women are unlikely to receive an intervention for FASD prophylaxis. System-wide screening strategies and targeted interventions for women of childbearing age with alcohol dependence need to be developed. These recommendations should be primary prevention priorities for substance abuse prevention programs.
To conclude, the existing PAE and FASD research underlines the strong negative impact that alcohol has on mortality, morbidity and disability in Russia (Institute for Health Metrics and Evaluation, 2012; Lim et al., 2012; Neufeld and Rehm, 2013). The regulations introduced within the last decade in Russia seem to show some positive effects on both drinking behavior and health outcomes (Neufeld and Rehm, 2013). However, there is an urgent need for further alcohol-control strategies to reduce alcohol-related harm, especially in the field of PAE and FASD.
Supplementary material
Supplementary material is available at Alcohol and Alcoholism online.
Funding
Funding to pay the Open Access publication charges for this article was provided by Social and Epidemiological Research Department, Centre for Addiction and Mental Health.
Conflict of interest statement
None declared.
Supplementary Material
Acknowledgements
The Canadian team acknowledges that support to the Centre for Addiction and Mental Health for the salaries of scientists and infrastructure has been provided by the Ontario Ministry of Health and Long-Term Care in Canada. The views expressed in this manuscript do not necessarily reflect those of the Ontario Ministry of Health and Long-Term Care. The Russian team thanks the National Research Center on Addiction and Moscow State University of Medicine and Dentistry named after A.I. Evdokimov, Russian Ministry of Health for the salaries of scientists and support on FASD-related initiative in Russia. They also thank all members of Russian International Coordination Council on Alcohol Damage on Health and Fetal Alcohol Spectrum Disorder for encouragement and support of FASD-related initiative in Russia. The views expressed in this manuscript do not necessarily reflect those of the Russian Ministry of Health. We also thank Dr Tatiana Balachova, Associate Professor, University of Oklahoma Health Sciences Center, USA for her helpful comments on the draft of this paper.
REFERENCES
- Akhmadeeva EN. Alkogolnyi sindrom ploda: obzor [Fetal alcohol syndrome: a review] Zdravookhranenie Bashkortostana [Healthcare of Bashkortostan] 1997;6:46–51. [Google Scholar]
- Albers LH, Johnson DE, Hostetter MK, et al. Health of children adopted from the former Soviet Union and Eastern Europe. JAMA. 1997;278:922–4. [PubMed] [Google Scholar]
- Alekseeva SN. Yakutsk, Russia: Nord-Ost Federal University named after M.K. Ammosov; 2011a. Osobennosti sostoianiia zdorovia i mikroelementnogo statusa novorozhdennykh, rodivshikhsia u materei, upotrebliaiushchikh alkogol (na primere g. Iakutska) [Health condition characteristics and micronutrient status of newborns to alcohol consuming mothers (an example of the city of Yakutsk)] Doctoral Dissertation. [Google Scholar]
- Alekseeva SN. Alkogolnyi sindrom ploda [Fetal Alcohol Syndrome]. V: XV Kongress pediatrov Rossii s mezhdunarodnym uchastiem ‘Aktualnye problemy pediatrii’ [In: XV Congress of Pediatricians of Russia with International Participation ‘Current Problems of Pediatrics’]; Moscow, Russia: 2011b. 14–17 Feb 2011, p. 17. [Google Scholar]
- Alekseeva SN, Ivanova ON. Abstinentnyi sindrom u novorozhdennogo ot materei, upotrebliaiushchikh alkogol vo vremia beremennosti [Withdrawal syndrome in neonates born to mothers who were consuming alcohol during pregnancy]. V: Resp. nauchno-prakt. konf., posv. 55-letiiu detskoi nevrologicheskoi sluzhby RS(Ia) [In: Scientific-Practical Conference Dedicated to the 55th Anniversary of Children's Neurological Services of Republic Sakha (Yakuty)]; Yakutsk, Russia: 2011. pp. 19–22. 14–15 Apr. 2011. [Google Scholar]
- Alipov VI, Korkhov VV. Alkogolizm i materinstvo [Alcoholism and Motherhood] Leningrad: Znanie; 1988. [Leningrad: Knowledge] [Google Scholar]
- Altshuler VB. Alkogolizm [Alcoholism] Moskva: GEOTAR Media; 2010. [Moscow: GEOTAR Media] [Google Scholar]
- Altshuler VB, Ivanets NN, Kravchenko SL. Zhenskij alkogolizm: klinicheskie aspekty [Female Alcoholism: Clinical Aspects] Moskva: Genius; 2006. [Moscow: Genius] [Google Scholar]
- Anokhina IP, Moskalenko VD. Alkogolizm v zerkale geneticheskoi nauki [Alcoholism in the mirror of Genetic Science]. V: Simpozium ‘Alkogolizm i nasledstvennost’—Mezhdunarodnye nauchnye sviazi (Vesti AN SSSR) [In: The Symposium ‘Alcoholism and Heredity’—International Scientific Relations (USSR Academy of Sciences)]; Moscow, USSR: 1987. pp. 103–8. [Google Scholar]
- Anokhina IP, Khristoliubova NA, Stanishevskaya AV, et al. Moskva: Nauka; 1989. pp. 3–8. Funktcionalnye narusheniia neiromediatornykh sistem u potomstva krys, podvergnutykh dlitelnoi alkogolnoi intoksikatcii. V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod. red. Airapetiantc MG [Functional disorders of neurotransmitter systems in the offspring of rats exposed to long-term alcohol intoxication. In Ayrapetyants MG (ed). The Consequences of Alcohol Intoxication for Posterity] [Moscow: Science] [Google Scholar]
- Aronson J. 2003. Fetal alcohol syndrome in Russian orphanages Orphan Doctor Available at http://www.orphandoctor.com/medical/commondiseases/fas/fas_russian.html. (15 January 2013, date last accessed)
- Artiukhina NI, Nozdracheva LV, Mikheeva TS. Moskva: Nauka; 1989. pp. 9–12. Postnatalnoe razvitie kory golovnogo mozga antenatalno alkogolizirovannykh krys. V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod. red. Airapetiantc MG [Postnatal development of the cerebral cortex of prenatally alcohol-exposed rats. In Ayrapetyants MG (ed). The Consequences of Alcohol Intoxication for Posterity] [Moscow: Science] [Google Scholar]
- Arzamasova OA. Omsk, Russia: 2011. pp. 21–8. Uglevod-belkovye kompleksy pecheni i syvorotki krovi prenatalno alkogolizirovannykh krys [Carbohydrate-protein complexes of liver and blood serums of prenatally alcohol-exposed rats]. V: Vseross. nauchn.-prakt. konf. biokhimikov i spetcialistov po laboratornoi meditcine ‘Meditcinskaia biokhimiia i klinicheskaia laboratornaia diagnostika v aspekte modernizatcii sistemy nauchnykh issledovanii’ [In: Russian Scientific-Practical Conference of Biochemistry Specialists and Specialists in Laboratory Medicine ‘Medical Biochemistry and Clinical Laboratory Diagnostics in the Perspective of Modernizing the System of Scientific Research’] 20–21 Sep 2011. [Google Scholar]
- Babenko GA, Skalny AV. Vliianie khronicheskoi alkogolnoi intoksikatcii na obmen tcinka u materi i potomstva [The influence of chronic alcohol intoxication on zinc metabolism in mother and offspring] Akusherstvo i Ginekologiia [Obstet Gynaecol] 1986;3:50–2. [PubMed] [Google Scholar]
- Badalyan LO. Sovremennye problemy alkogolnoi embrio- i fetopatii [Modern problems of alcohol embryo- and fetopathy] Zhurn Nevr i Psikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 1986;86:1443–9. [PubMed] [Google Scholar]
- Bakanov MI. Alkogol i metabolizm rebenka [Alcohol and metabolism of a child] Pediatriia [Pediatrics] 1986;10:52–4. [PubMed] [Google Scholar]
- Bakanov MI. Vliianie alkogolia na obmen veshchestv u detei i podrostkov (obzor literatury) [The influence of alcohol on the metabolism of children and adolescents (literature review)] Detskii Doktor [Pediatrician] 1999;3:40–1. [Google Scholar]
- Balachova TN, Bonner BL, Isurina GL, et al. Use of focus groups in developing FAS/FASD prevention in Russia. Subst Use Misuse. 2007;42:881–94. doi: 10.1080/10826080701202601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balachova T, Bonner B, Isurina G, et al. Changing physicians’ knowledge, skills and attitudes to prevent FASD in Russia. Proceedings of the 33rd Annual Scientific Meeting of the Research Society on Alcoholism. Alcohol Clin Exp Res. 2010a;34:210A. [Google Scholar]
- Balachova TN, Isurina GL, Grandilevskaya IV, et al. Profilaktika alkogolnogo sindroma ploda i narushenii neirorazvitiia u detei: tekhnologiia razrabotki profilakticheskoi programmy [Prevention of Fetal Alcohol Syndrome and neurodevelopmental disorders in children: Technology of prevention program developing]. V: Mezhdunarodnaia konferentciia po klinicheskoi psikhologii detstva ‘Rozhdenie i Zhizn’. [In: International Conference on Clinical Psychology of Childhood ‘Birth and Life’]; St. Petersburg, Russia: 2010b. pp. 233–8. 15–16 Oct 2010. [Google Scholar]
- Balachova T, Bonner BL, Chaffin M, et al. Women's alcohol consumption and the risk for alcohol-exposed pregnancies in Russia. Addiction. 2012a;107:109–17. doi: 10.1111/j.1360-0443.2011.03569.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balachova TN, Bonner BL, Isurina GL, et al. Izuchenie vlijanija informacionnyh materialov na otnoshenie zhenshhin k upotrebleniju alkogolja vo vremja beremennosti [Investigation of effects of informational materials on women's attitudes to alcohol consumption during pregnancy] Vestnik Sankt-Peterburgskogo Universiteta. Sankt-Peterburg: Sankt-Peterburgskij Gosudarstvennyj Universitet imeni M. Lomonosova [Bulletin of St. Petersburg State University. St. Petersburg: St. Petersburg State University named after M. Lomonosov] 2012b;12:101–8. [Google Scholar]
- Balachova TN, Volkova EN, Isurina GL, et al. Fetalnyi alkogolnyi sindrom [Fetal Alcohol Syndrome] Sankt-Peterburg: SPbGU; 2012c. [St. Petersburg: StPSU] [Google Scholar]
- Barden-O'Fallon J, Reynolds Z, Speizer IS. Chapel Hill: 2010. Women's health in the Russian Federation: the Russia Longitudinal Monitoring Survey 2010. [working paper WP-11–121] MEASURE Evaluation. [Google Scholar]
- Bisiarina VP, Lisitcyna NF. Omsk: 1987. Predupredit bedu: alkogolizm i deti [To prevent a disaster: alcoholism and children] Vsesoiuz. Dobrovol. Ob-vo Borby za Trezvost [Omsk: USSR's Voluntary Temperance Society] [Google Scholar]
- Bubnov AA. Tcirkadnyi ritm temperatury tela u detei s fetalnym alkogolnym sindromom [Circadian rhythm of the body temperature of children with Fetal Alcohol Syndrome]. V: Mezhregionalnaia nauchno-prakticheskaia konf. ‘Aktualnye Problemy Pediatrii’ [In: International Scientific-Practical Conference ‘Current Issues in Paediatrics’]; Ufa, Russia: 2009. pp. 168–71. 29 Oct 2009. [Google Scholar]
- Bubnov AA. Ekaterinburg, Russia: Ural's State Medical Academy; 2010. Morfo-funktcionalnaia diagnostika posledstvii vnutriutrobnogo alkogolnogo vozdeistviia u detei rannego vozrasta [Morpho-functional diagnostics of consequences of intrauterine alcohol exposure in infants] Doctoral Dissertation. [Google Scholar]
- Chambers CD, Kavteladze L, Joutchenko L, et al. Alcohol consumption patterns among pregnant women in the Moscow region of the Russian Federation. Alcohol. 2006;38:133–7. doi: 10.1016/j.alcohol.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Chebotar NA, Konopistceva LA. Mekhanizmy teratogennogo deistviia alkogolia [Mechanisms of the teratogenic effects of alcohol] Morfologiia [Morphology] 1993;105:19–26. [PubMed] [Google Scholar]
- Chudley A, Conry J, Cook J, et al. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ. 2005;172(5 suppl):S1–S21. doi: 10.1503/cmaj.1040302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donetc OY. Tomsk, Russia: Tomsk's Scientific Centre RAMS, SRIMH; 1992. Psikhicheskie narusheniia u potomstva materei, bolnykh khronicheskim alkogolizmom: (klinich. i immunolog. aspekty) [Mental disorders in the offspring of mothers with chronic alcoholism: clinical and immunological aspects] Doctoral Dissertation. [Google Scholar]
- Egorova AT, Kapitonov VF, Baraniuk NV, et al. Sotcialno-gigienicheskaia kharakteristika i reproduktivnoe zdorove zhenshchin s zabolevaniiami pankreo-biliarnoi sistemy [Social and hygienic characteristics and reproductive health of women with diseases of the pancreatobiliary system] Sovremennye Issledovaniia Sotcialnykh Problem [Curr Res Soc Probl] 2012;6:16. [Google Scholar]
- Erokhova ZN, Bozhenov Yu A. Osobennosti sostoianiia zdorovia detei rannego vozrasta s vnutriutrobnoi subklinicheskoi alkogolnoi intoksikatciei[Characteristics of the health status of young children with subclinical intrauterine alcohol intoxication] Ros Vestn Perinatologii i Pediatrii [Rus Bull Perinatology Paediatry] 1997;1:70. [Google Scholar]
- Farina L, Leifer M, Chasnoff IJ. Attachment and behavioural difficulties in internationally adopted Russian children. Adoption Fostering. 2004;28:38–49. [Google Scholar]
- Federal State Statistics Service of Russian Federation (FSSS) 2012. Available at http://www.gks.ru/wps/wcm/connect/rosstat/rosstatsite.eng/figures/population/ (15 March 2013, date last accessed)
- Frolova OG, Nikolaeva EI. Gigiena Beremennoi [Prenatal Hygeine] Moskva: Meditcina; 1987. [Moscow: Medicine] [Google Scholar]
- Gaidukov SN, Nekrasov KV, Atlasov VO. Rasprostranennost upotrebleniia zhenshchinami alkogolia do i vo vremia beremennosti i ee sotcialno-demograficheskie determinanty [Prevalence of alcohol consumption among women before and during pregnancy and its social-demographic determinants] Zhurnal Akusherstva i Zhenskikh Boleznei [J Obstet Gynecol] 2008;LVII:11–6. [Google Scholar]
- Garmasheva NL, Konstantinova NN. Povrezhdenie mozga v geneze alkogolnogo sindroma ploda [Brain damage in the genesis of fetal alcohol syndrome] Vestnik Akademii Meditcinskikh Nauk SSSR [Bull USSR Academy Med Sci] 1988;3:59–64. [PubMed] [Google Scholar]
- Grechany SV. Sankt-Peterburg: SPbGPMA; 2002. pp. 52–6. Psikhicheskoe razvitie detei rannego vozrasta, podvergshikhsia vnutriutrobnomu vozdeistviiu geroina i alkogolia.V Akusherstvo i ginekologiia.Dostizheniia i puti razvitiia v 21 veke. Sb. nauch. tr. pod red. prof. S.N. Gaidukova, posviashchennyi 75-letiiu kafedry akusherstva i ginekologii SPbGPMA [Mental development of children who were exposed to heroin and alcohol in utero. In Gaigukov SN (ed). Obstetrics and Gynaecology. Accomplishments and Ways of Development in 21 Century] [St. Petersburg: StPSMPA] [Google Scholar]
- Grigovich IN, Mebelova II, Nikula MZ. Alkogolnyi sindrom ploda [Fetal Alcohol Syndrome] Rossiiskii Vestnik Perinatologii i Pediatrii (Voprosy okhrany materinstva i detstva): Nauchno-prakticheskii retcenziruemyi zhurnal [Rus Bull Perinatalogy Paediatry (Issues of Protection of Mother and Child): Peer-Reviewed Journal] 2006;51:10–3. [Google Scholar]
- Grjibovski A, Bygren LO, Svartbo B. Socio-demographic determinants of poor infant outcome in North-West Russia. Pediatr Perinat Epidemiol. 2002;16:255–62. doi: 10.1046/j.1365-3016.2002.00429.x. [DOI] [PubMed] [Google Scholar]
- Grjibovski A, Bygren LO, Svartbo B, et al. Housing conditions, perceived stress, smoking, and alcohol: determinants of fetal growth in northwest Russia. Acta Obstet Gynecol Scand. 2004;83:1159–66. doi: 10.1111/j.0001-6349.2004.00443.x. [DOI] [PubMed] [Google Scholar]
- Gummel KK, Brzheskiy VV, Igge Y. Nekotorye kharakteristiki zritelnogo analizatora u detei s fetalnym alkogolnym sindromom [Characteristics of the visual analyzer in children with Fetal Alcohol Syndrome] Russkii Meditcinskii Zhurnal.Prilozhenie ‘Klinicheskaia Oftalmologiia’ [Rus Med J App ‘Clin Ophthalmol’] 2007a;8:25–8. [Google Scholar]
- Gummel KK, Brzheskiy VV, Igge Y. Sankt-Peterburg: Piastr; 2007b. pp. 5–8. Rezultaty vizometrii, refraktometrii i staticheskoi kompiuternoi perimetrii (RBP) u detei s fetalnym alkogolnym sindromom. V: Sovremennye Problemy Oftalmologii. Sb. Nauchnykh Statei [Results of optometry, refractometry, and statistical computerized compare rarebit perimetry (RBP) in children with fetal alcohol syndrome. In: Contemporary Problems of Ophthalmology: Collection of Scientific Articles] [St. Petersburg: Piastre] [Google Scholar]
- Institute for Health Metrics and Evaluation. Seattle, Washington DC, USA: Institute for Health Metrics and Evaluation; 2012. Global Burden of Disease Study Profile: Russia : Available at http://www.healthmetricsandevaluation.org/sites/default/files/country-profiles/GBD%20Country%20Report%20-%20Russia.pdf. (17 July 2013, date last accessed) [Google Scholar]
- Isurina GL, Pechenezhskaia MS, Regentova AYu. St. Petersburg, Russia: 2009. pp. 39–41. Profilaktika alkogolnogo sindroma ploda: izuchenie ustanovok v otnoshenii upotrebleniia alkogolia vo vremia beremennosti [Prevention of Fetal Alcohol Syndrome: study of attitudes towards alcohol consumption during pregnancy]. V: Nauchnii Simpozium ‘Nasilie i Prenebrezhdenie po Otnosheniiu k Detiam: Profilaktika, Vyiavlenie, Vmeshatelstvo’ [In: Scientific Symposium ‘Abuse and Neglect of Children: Prevention, Detection, Intervention’] 20–22 Oct 2009. [Google Scholar]
- Jones KL, Robinson LK, Bakhireva LN, et al. Accuracy of the diagnosis of physical features of fetal alcohol syndrome by pediatricians after specialized training. Pediatrics. 2006;118:1734–8. doi: 10.1542/peds.2006-1037. [DOI] [PubMed] [Google Scholar]
- Kalinina AG, Surkova LA, Zabirova IG, et al. Vliianie razlichnykh alkogolnykh napitkov, upotrebliaemykh zhenshchinami reproduktivnogo vozrasta na strukturu patologii i zdorove novorozhdennykh [Influence of different alcoholic beverages, consumed by women of child-bearing age, on the type of pathology and the state of health of neonates] Narkologiia [Narcology] 2012;3:43–51. [Google Scholar]
- Kashirskaya EI. Astrakhan, Russia: Astrakhan's State Medical Academy; 2010. Kliniko-biokhimicheskaia otcenka i prognozirovanie sostoianiia zdorovia detei, razvivaiushchikhsia pod vozdeistviem psikhoaktivnykh veshchestv [Clinical-biochemical evaluation and prognosis of the health status of children exposed to psychoactive substances] Doctoral Dissertation. [Google Scholar]
- Kataeva LN, Kataev SI, Krasnova TA. Vliianie alkogolnoi intoksikatcii belykh krys na eritropoez ikh potomstva [The effect of alcohol intoxication in white rats on erythropoiesis of their breed] Vestnik Ivanovskogo Gosudarstvennogo Universiteta. Seriia ‘Biologiia. Khimiia. Fizika. Matematika’ [Bull Ivanovo State University. Series ‘Biology, Chemistry, Physics, Mathematics’] 2004;3:33–7. [Google Scholar]
- Khasianova TA. Otcenka effektivnosti kompleksnoi terapii fetalnogo alkogolnogo sindroma [Evaluation of the effectiveness of complex treatment of fetal alcohol syndrome] Uspekhi Sovremennogo Estestvoznaniia [Success Mod Nat Sci] 2010;7:123–6. [Google Scholar]
- Khatckel SB, Popov IV. Malye anomalii razvitiia: prognosticheskii pokazatel neblagopoluchiia rebenka bolnoi alkogolizmom materi [Minor developmental anomalies: prognostic indicator of ill-being of a child to an alcohol-dependent mother] Morfologiia [Morphology] 2005;127:68–71. [PubMed] [Google Scholar]
- Khatckel SB, Popov IV. Alkogol - vazhneishii faktor fetalnogo programmirovaniia [Alcohol: the most important fetal programming factor]. V: 3ii Mezhdistciplinarnii Rossiiskii Kongress ‘Chelovek i Alkogol (Alkogolnye Bolezni)’. [In: 3rd Russian Interdisciplinary Congress ‘Human and Alcohol (Alcohol-Related Diseases)’]; St. Petersburg, Russia: 2009a. pp. 88–9. 23–24 Apr 2009. [Google Scholar]
- Khatckel SB, Popov IV. Vozrastnye aspekty fetalnogo programmirovaniia kardiovaskuliarnoi patologii pod vliianiem alkogolia [Age-related aspects of fetal programming of cardiovascular pathology under the influence of alcohol]. V: 3ii Mezhdistciplinarnii Rossiiskii Kongress ‘Chelovek i Alkogol (Alkogolnye Bolezni)’. [In: 3rd Russian Interdisciplinary Congress ‘Human and Alcohol (Alcohol-Related Diseases)’]; St. Petersburg, Russia: 2009b. pp. 89–90. 23–24 Apr. 2009. [Google Scholar]
- Khatckel SB, Popov IV. Analiz fenotipa u vospitannikov domov rebenka [Analysis of the phenotype of orphans] Terra Medica: Pediatriia [Terra Medica: Paediatrics] 2011;2:35–40. [Google Scholar]
- Khoroshkina LA, Krivtcova LA. Vliianie nikotinovoi i alkogolnoi zavisimosti zhenshchiny na zdorove novorozhdennogo [Effect of women's nicotine and alcohol dependence on newborn's health] Mat’ i Ditia v Kuzbasse [Mother and Child in Kuzbass] 2010;4:35–8. [Google Scholar]
- Kirganova VV. Moscow, Russia: NRCA; 2009. Mediko-sotsialniie posledstviia in'ektcionnogo upotrebleniia narkotikov v Rossii (metodi otsenki i preduprezhdeniia) [Medical and social outcomes of injected drug use in Russia (evaluation and prevention)] Doctoral Dissertation. [Google Scholar]
- Kiriushchenkov AP. Alkogolnyi sindrom ploda [Fetal Alcohol Syndrome] Akusherstvo i Ginekologiia [Obstet Gynaecol] 1986;8:5–7. [PubMed] [Google Scholar]
- Kolomeitceva IA, Levina OL. Vliianie alkogolnoi intoksikatcii v period vnutriutrobnogo razvitiia na funktcii TcNS potomstva [Effects of alcohol intoxication during intrauterine development on CNS functions in the offspring] Akusherstvo i Ginekologiia [Obstet Gynaecol] 1989;1:46–50. [PubMed] [Google Scholar]
- Kolomeitceva IA, Varmut R, Airapetiantc MG, et al. Moskva: Nauka; 1989. pp. 33–6. Potomstvo pri eksperimentalnom alkogolizme i substantciia P. V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod.red. Airapetiantc M.G. [Breed in experimental alcoholism and P-substance. In Ayrapetyants MG (ed). The Consequences of Alcohol Intoxication for Posterity] [Moscow: Science] [Google Scholar]
- Komarova EE. Moscow, Russia: People Friendship University of Russia; 2008. Sostoianie fetoplatcentarnoi sistemy pri upotreblenii psikhoaktivnykh veshchestv (geroin i alkogol) [The condition of the fetoplacental system during consumption of psychoactive substances (heroin and alcohol)] Doctoral Dissertation. [Google Scholar]
- Konovalova VV, Kupriyanova TA, Marincheva GS. Fetalnyi alkogolnyi sindrom u detei shkolnogo vozrasta [Fetal Alcohol Syndrome in school children]. V: IV Mezhdunarodnii Kongress ‘Molodoe Pokolenie XXI Veka: Aktualnye Problemy Sotcialno-psikhologicheskogo Zdorovia’ [In: International Congress IV ‘The Young Generation of the XXI Century: Actual Problems of Social and Mental Health’]; Kirov, Russia: 2009. pp. 106–7. 22–24 Sep 2009. [Google Scholar]
- Kornilov AA, Seledtcov AM, Maksimenko AV, et al. Alkogolizm roditelei i umstvennaia otstalost ikh detei [Parental alcoholism and children's mental retardation] Mat’ i Ditia v Kuzbasse [Mother and Child in Kuzbass] 2005;1:24–7. [Google Scholar]
- Koshkina EA, Paronyan ID. Moskva: Institut sociologii RAN; 1995. pp. 53–8. Dinamika upotrebleniia psihoaktivnih veschestv sredi podrostkov [Dynamics of psychoactive substance consumption among adolescents].VAktualnie problemi deviantnogo povedenia. Borba s sotsialnimi bolezniami [In: Actual Problems of Deviant Behavior. Combating Social Diseases] [Moscow: RAS Institute of Sociology] [Google Scholar]
- Koshkina EA, Gurtovenko VM, Paronyan ID, et al. Posledstviia potrebleniia alkogolia dlia zhenshchin, podrostkov, detei i semi [The consequences of alcohol consumption for women, adolescents, children and family] Novosti Nauki i Tekhniki. Ser. Med. Vyp. ‘Alkogolnaia Bolezn’. Razdel 4. Alkogolnyi Sindrom Ploda / VINITI [Scientific and Technical News. Set of Medical Volumes ‘Alcohol Disease’. Chapter ‘Fetal Alcohol Syndrome’/RISTI] 1998;3:9–22. [Google Scholar]
- Koshkina EA, Kirzhanova VV, Sidoryuk OV, et al. Moskva: NNTc Narkologii; 2012. Osnovniie pokazateli deiatelnosti narkologicheskoi sluzhbi v 2011g. [Report on the main performance indicators of narcology service in Russian Federation in 2011] [Moscow: National Research Center of Addiction]. Available at http://www.nncn.ru/datadepot/dd51/020371.pdf. (7 July 2013, date last accessed) [Google Scholar]
- Kosyh EA, Balachova T, Bonner B, et al. Alcohol consumption by pregnant women in the Nizhny Novgorod region, Russia. Alcohol Clin Exp Res. 2010;34:111A. [Google Scholar]
- Kovetcky NS, Konovalov GV, Orlovskaya DD, et al. Dizontogenez golovnogo mozga potomstva materei, upotrebliavshikh alkogol v period beremennosti [Dysontogenesis of brain developmentin the offspring of mothers who consumed alcohol during pregnancy] Zhurn Nevr i i Psikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 1991a;10:57–63. [PubMed] [Google Scholar]
- Kovetcky NS, Solonsky AV, Yarygina EG. Formirovanie sinapsov golovnogo mozga embrionov v norme i pri alkogolizme materi [Genesis of brain synapses in embryos in normal and in cases of alcoholic mothers] Zhurn Nevr iPsikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 1991b;2:91–3. [Google Scholar]
- Kristjanson AF, Wilsnack SC, Zvartau E, et al. Alcohol use in pregnant and non-pregnant Russian women. Alcohol Clin Exp Res. 2007;31:299–307. doi: 10.1111/j.1530-0277.2006.00315.x. [DOI] [PubMed] [Google Scholar]
- Kunikovskaia LS. Klinicheskaia kharakteristika oligofrenii alkogolno-embrioticheskogo geneza [Clinical characteristics of alcohol-embryonic origin oligophrenia] Zhurn Nevr i Psikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 1980;80:417–22. [PubMed] [Google Scholar]
- Kurch NM. Tomsk, Russia: Siberia's State Medical Academy; 2004. Morfofunktcionalnye osobennosti razvitiia podzheludochnoi zhelezy u krys, alkogolizirovannykh v prenatalnom periode [Special morphofunctional characteristics of pancreas development in prenatally alcohol exposed rats] Doctoral Dissertation. [Google Scholar]
- Kurch NM. Korrektciia narushenii metabolizma uglevod-belkovykh kompleksov soedinitelnoi tkani podzheludochnoi zhelezy u prenatalno alkogolizirovannykh krys [Correction of metabolic disturbances of carbohydrate-protein complexes of the pancreatic connective tissue of prenatally alcohol-exposed rats]. V: Vseross. Nauchn.-Prakt. Konf. Biokhimikov i Spetcialistov po Laboratornoi Meditcine ‘Meditcinskaia biokhimiia i klinicheskaia laboratornaia diagnostika v aspekte modernizatcii sistemy nauchnykh issledovanii’ [In: Russian Scientific-Practical Conference of Biochemists and Secialists of Lab Medicine ‘Medical Biochemistry and Clinical Laboratory Diagnostics in the Perspective of Modernization of System of Scientific Research’]; Omsk, Russia: 2011. pp. 171–4. 20–21 Sep 2011. [Google Scholar]
- Kurianova NN. Osobennosti khronicheskoi intoksikatcii etanolom zhenshchin v usloviiakh sotcialno-ekologicheskogo stressa[Characteristics of women with chronic alcohol intoxication under conditions of social and ecological stress] Uspekhi Sovremennogo Estestvoznaniia [Success Mod Nat Sci] 2006;2:37–8. [Google Scholar]
- Kurianova NN, Bolotnikova NI, Udodova LV. Kliniko-sotcialnaia kharakteristika zhenshchin, upotrebliavshikh vo vremia beremennosti alkogol [Clinical and social characteristic of women consuming alcohol during pregnancy] Uspekhi Sovremennogo Estestvoznaniia [Success Mod Nat Sci] 2006;2:36. [Google Scholar]
- Kuteneva NA, Solonsky AV, Daniletc AV, et al. Tomsk, Russia: 2005. Vliianie prenatalnoi alkogolizatcii na razvitie embrionalnykh kapilliarov golovnogo mozga [Effects of prenatal alcohol exposure on the development of embryonic capillaries of the brain] V: Biulleten sibirskoi meditciny. Prilozhenie 1. ‘Tezisy Dokladov V Sibirskogo Fiziologicheskogo Sezda’ [In: Bull of Siberia's Medicine. App. 1. ‘Theses of Reports of Siberia's Physiological Congress’] 29–30 Jun, 1 Jul 2005 3:163. [Google Scholar]
- Kuznetsova TA, Pavlikova AV, Sviridov AS. St. Petersburg, Russia: 2011. pp. 99–100. Otcenka litcevykh anomalii v diagnostike fetalnogo alkogolnogo sindroma ploda [Evaluation of facial anomalies in the diagnosis of Fetal Alcohol Syndrome].V; Rossiiskii Forum ‘Zdorove detei: profilaktika sotcialno-znachimykh zabolevanii. Sankt-Peterburg – 2011’ [In: Russian Forum ‘Children's health: prevention of socially significant diseases. St. Petersburg – 2011’] 12–13 May 2011. [Google Scholar]
- Lebedev BA. Alkogol i semia [Alcohol and Family] Leningrad: Meditcina; 1974. [Leningrad: Medicine] [Google Scholar]
- Legonkova SV. St. Peterburg, Russia: St. Peterburg's State Paediatric Medical Academy; 2011. Kliniko-funktcionalnaia kharakteristika fetalnogo alkogolnogo sindroma u detei rannego vozrasta [Clinical and functional characteristics of Fetal Alcohol Syndrome in early childhood] Doctoral Dissertation. [Google Scholar]
- Legonkova SV, Palchik AB. Vozrastnye osobennosti manifestatcii fetalnogo alkogolnogo sindroma [Special age-related manifestations of Fetal Alcohol Syndrome]. V: 3ii Mezhdistciplinarnii Rossiiskii Kongress ‘Chelovek i Alkogol (Alkogolnye Bolezni)’ [In: 3rd Russian Interdisciplinary Congress ‘Human and Alcohol (Alcohol-related Diseases)’]; St. Petersburg, Russia: 2009. p. 57. 23–24 Apr 2009. [Google Scholar]
- Lezhepekova LN. Chto nado znat pri lechenii alkogolizma? [What Is Necessary to Know for Treatment of Alcoholism?] Leningrad: Meditcina; 1981. [Leningrad: Medicine] [Google Scholar]
- Lim S, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisitcyn YP, Sidorov PI. Moskva: Meditcina; 1990. pp. 221–8. Meditcinskie posledstviia alkogolizma.Alkogolnyi sindrom ploda. V Alkogolizm. Mediko-sotcialnye aspekty, pod red. Lisitcyn YP [Medical consequences of alcohol. Fetal Alcohol Syndrome. In Lisitcyn YP (ed). Alcoholism. Medical and Social Aspects] [Moscow: Medicine] [Google Scholar]
- Maizelis MY, Zabludovsky AL, Shikhov NS. Moskva: Nauka; 1989. pp. 42–8. Eksperimentalnaia terapiia narushenii funktcii i metabolizma mozga, vyzvannykh prenatalnoi alkogolizatciei.V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod.red. Airapetiantc MG [Experimental therapy in the disruption of the function and metabolism of the brain induced by prenatal alcohol exposure. In Ayrapetyants MG (ed). The Consequences of Alcohol Intoxication for Posterity] [Moscow: Science] [Google Scholar]
- Malakhova ZL. Ekaterinburg, Russia: Ural's State Medical Academy; 2012. Kliniko-patogeneticheskie osnovy fetalnogo alkogolnogo sindroma u detei rannego vozrasta [Clinical and pathogenic basis of fetal alcohol syndrome in infants] Doctoral Dissertation. [Google Scholar]
- Malakhova ZL, Bubnov AA. Opyt ispolzovaniia transkranialnoi mikropoliarizatcii golovnogo mozga kak metoda abilitatcii detei rannego vozrasta s fetalnym alkogolnym sindromom [The experience of using transcranial micropolarization (TCMP) as a method of rehabilitation of infants with Fetal Alcohol Syndrome] Narkologiia [Narcology] 2011;12:61–3. [Google Scholar]
- Malakhova ZL, Bubnov AA, Efremov AV. Otcenka fenotipicheskikh i psikhologo-pedagogicheskikh kharakteristik detei v kontekste posledstvii alkogolnykh effektov ploda [Evaluation of phenotypical and psycho-educational characteristics of children in the context of the consequences of Fetal Alcohol Effects] Uralskii Meditcinskii Zhurnal [Ural's Med J] 2008;5:67–70. [Google Scholar]
- Malakhova ZL, Bubnov AA, Shukshina LA. Opyt primeneniia transkranialnoi mikropoliarizatcii golovnogo mozga u detei rannego vozrasta s fetalnym alkogolnym sindromom [The experience of applying transcranial micropolarization (TCMP) in infants with Fetal Alcohol Syndrome] Uralskii Meditcinskii Zhurnal [Ural's Med J] 2011;4:118–20. [Google Scholar]
- Marincheva GS, Riley EP, Konovalova VV, et al. Fetalnyi alkogolnyi sindrom v razlichnykh kontingentakh detei i podrostkov [Fetal Alcohol Syndrome in different groups of children and adolescents] Sotcialnaia i Klinicheskaia Psikhiatriia [Soc Clin Psychiatry] 2003;3:17–22. [Google Scholar]
- Mastiukova EM. Rol alkogolizma roditelei v etiologii nervno-psikhicheskikh rasstroistv u detei [The role of parents’ alcoholism in the etiology of psycho-neurological disorders in children] Defektologiia [Abnorm Psychol] 1986;2:77. [Google Scholar]
- Mastiukova EM. Defekty zreniia i intellekta pri alkogolnom sindrome ploda. [Defects of vision and intellect in fetal alcohol syndrome] Defektologiia [Abnorm Psychol] 1989;6:9–13. [Google Scholar]
- May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome: a summary. Alcohol Res Health. 2001;25:159–67. [PMC free article] [PubMed] [Google Scholar]
- McGuinness TM, McGuinness JP, Dyer JG. Risk and protective factors in children adopted from the former Soviet Union. Pediatr Health Care. 2000;14:109–16. [PubMed] [Google Scholar]
- Miller LC, Chan W, Litvinova A, et al. Fetal alcohol spectrum disorders in children residing in Russian orphanages: a phenotypic survey. Alcohol Clin Exp Res. 2006;30:531–8. doi: 10.1111/j.1530-0277.2006.00059.x. [DOI] [PubMed] [Google Scholar]
- Miller LC, Chan W, Litvinova A, et al. Medical diagnoses and growth of children residing in Russian orphanages. Acta Paediatr. 2007;96:1765–9. doi: 10.1111/j.1651-2227.2007.00537.x. [DOI] [PubMed] [Google Scholar]
- Morozova MV, Popova NK. Sochetannoe vliianie alkogolia i stressa v prentalnom periode na povedenie vzroslykh myshei [The combined effects of alcohol and stress in the prenatal period on the behaviour of adult mice] Rossiiskii Fiziologicheskii Zhurnal im I.M. Sechenova [Rus Physiolog J named after I.M. Sechenov] 2010;96:1114–21. [PubMed] [Google Scholar]
- Moskalenko VD. Moskva: ID Medpraktika; 2002. pp. 326–8. Profilaktika alkogolnogo sindroma u ploda i sindroma lisheniia narkotikov u novorozhdennykh. V Rukovodstvo po narkologii, pod red. NN Ivantca i dr. [Prevention of fetal alcohol syndrome in foetuses and drug withdrawal syndrome in neonates. In Ivanetc NN et al. (eds). Manual in Narcology] [Moscow: Medpraktika] [Google Scholar]
- Moskalenko VD. Moskva: GEOTAR-Media; 2008a. pp. 643–5. Profilaktika alkogolnogo sindroma u ploda i sindroma lisheniia narkotikov u novorozhdennykh. V Narkologiia: Natcionalnoe rukovodstvo, pod red. NN Ivantca i dr. [Prevention of fetal alcohol syndrome in foetuses and drug withdrawal syndrome in neonates. In Ivanetc NN et al. (eds). Narcology: National Manual] [Moscow: GEOTAR-Media] [Google Scholar]
- Moskalenko VD. Moskva: OOO Meditcinskoe Informatcionnoe Agenstvo; 2008b. pp. 818–20. Profilaktika alkogolnogo sindroma u ploda i sindroma lisheniia narkotikov u novorozhdennykh. V Rukovodstvo po narkologii, pod red. NN Ivantca i dr. [Prevention of Fetal Alcohol Syndrome in foetuses and drug withdrawal syndrome in neonates. In Ivanetc NN et al. (eds). Manual in Narcology] [Moscow: Medical News Agency] [Google Scholar]
- Neufeld M, Rehm J. Alcohol consumption and mortality in Russia since 2000: Are there any changes following the alcohol policy changes starting in 2006? Alcohol Alcohol. 2013;48:222–30. doi: 10.1093/alcalc/ags134. [DOI] [PubMed] [Google Scholar]
- Nozdracheva LV, Artyukhina NI, Kolomeitceva IA, et al. Moskva: Nauka; 1989. pp. 59–63. Korregiruiushchee deistvie dalargina na TcNS krys pri antenatalnoi alkogolnoi intoksikatcii. V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod.red. Airapetiantc MG [Corrective action of dalargin on the central nervous system of rats with antenatal alcohol intoxication. In Ayrapetyants MG (ed). The Consequences of Alcohol Intoxication for Posterity] [Moscow: Science] [Google Scholar]
- Ogotoeva SN, Borisova NV. Mikroelementnyi sostav krovi beremennykh zhenshchin pri upotreblenii alkogolia [Micronutrient blood count in pregnant women consuming alcohol] Mikroelementy v Meditsine [Microelements Med] 2008;9:61. [Google Scholar]
- Ogotoeva SN, Barashkova NN, Borisova NV. Vliianie ‘umerennogo’ upotrebleniia alkogolia vo vremia beremennosti na mikroelementnyi sostav krovi zhenshchin i sostoianie zdorovia novorozhdennykh detei [Effects of moderate alcohol consumption during pregnancy on maternal micronutrient blood count and the health status of the neonate] Iakutskii Meditcinskii Zhurnal [Yakuty's Med J] 2009a;3:68–70. [Google Scholar]
- Ogotoeva SN, Borisova NV, Tumusov PS, et al. Osobennosti techeniia rannego neonatalnogo perioda novorozhdennykh ot materei, stradaiushchikh khronicheskim alkogolizmom [Characteristics of early neonatal development of neonates born to chronic alcohol-dependent mothers] Nauka i Obrazovanie [Sci Educ] 2009b;2:49–51. [Google Scholar]
- Omelianchik MS, Artamonova VG, Selyavko AA. Asimmetriia v okostenenii nizhnei cheliusti kak rannii simptom alkogolnogo sindroma ploda [Asymmetry in the ossification of the lower jawbone as an early symptom of Fetal Alcohol Syndrome] Zdravookhranenie Belarusi [Healthc Belarus] 1993;8:45–9. [Google Scholar]
- Orazmuradov AA, Radzinsky VE, Ogurtcov PP, et al. Vliianie alkogolizma i tabakokureniia na techenie beremennosti i perinatalnyi iskhod rodov [The effects of alcoholism and cigarette smoking on the pregnancy and the perinatal outcome of labor] Narkologiia [Narcology] 2007;11:60–2. [Google Scholar]
- Palchik AB, Legonkova SV. Fetalnyi alkogolnyi sindrom: manifestatciia i dinamika [Fetal alcohol syndrome: manifestation and dynamic] Obozrenie Psikhiatrii i Med. Psikhologii im. V.M. Bekhtereva [Rev Psychiatry Med Psychology named after V.M. Bekhterev] 2011;3:17–20. [Google Scholar]
- Palchik AB, Shabalov NP. Toksicheskie entcefalopatii novorozhdennykh [Toxic Encephalopathy of Newborns] Moskva: MEDpress-inform; 2009. [Moscow: MEDpress-inform] [Google Scholar]
- Palchik AB, Fedorova LA, Legonkova SV. Fetalnyi alkogolnyi sindrom. Metodicheskie rekomendatcii [Fetal Alcohol Syndrome. Medical Recommendations] Sankt-Peterburg: OOO ANTT-Print; 2006. [St. Petersburg: ANTT-Print] [Google Scholar]
- Palchik AB, Nazdzhanova ZG, Legonkova SV. Osobennosti formirovaniia bioelektricheskoi aktivnosti u detei rannego vozrasta s antenatalnoi ekspozitciei toksichnykh veshchestv [Characteristics of the formation of bio-electrical activity in children with antenatal exposure to toxic substances]. V: 3ii Mezhdistciplinarnii Rossiiskii Kongress ‘Chelovek i Alkogol (Alkogolnye Bolezni)’ [In: 3rd Russian Interdisciplinary Congress ‘Human and Alcohol (Alcohol-related Diseases)’]; St. Petersburg, Russia: 2009. p. 62. 23–24 Apr 2009. [Google Scholar]
- Palchik AB, Legonkova SV, Sofronova GI. Etnicheskie osobennosti manifestatcii fetalnogo alkogolnogo sindroma [Ethnic characteristics of the manifestation of Fetal Alcohol Syndrome] Iakutskii Meditcinskii Zhurnal [Yakuty's Med J] 2011;2:22–5. [Google Scholar]
- Petrov-Maslakov MA. Moskva: MEDGIZ; 1961. p. 416. Gigiena zhenshchiny.V Istoricheskoe razvitie akusherstva i ginekologii. Embriogenez. Anatomiia i fiziologiia zhenskikh polovykh organov. Gigiena zhenshchiny, pod red.toma prof. FA Syrovatko. V Mnogotomnoe rukovodstvo po akusherstvu i ginekologii, otv.red. prof. LS Persianov. [Hygiene of women. In: Syrovatko FA (ed). Historical Development of Obstetrics and Gynecology. Embryogenesis. Anatomy and Physiology of the Female Genital Organs.Hygiene of Woman. In: Persianov LS (ed). Multivolume Manual on Obstetrics and Gynecology] [Moscow: Medical State Publisher] [Google Scholar]
- Popova EN. Ultrastruktura mozga.alkogol i potomstvo[Ultrastructure of the Brain, Alcohol and the Offspring] Moskva: Nauchnyi Mir; 2010. [Moscow: Scientifical World] [Google Scholar]
- Popova S, Stade B, Bekmuradov D, et al. What do we know about the economic impact of Fetal Alcohol Spectrum Disorder? A systematic literature review. Alcohol Alcohol. 2011;46:490–7. doi: 10.1093/alcalc/agr029. [DOI] [PubMed] [Google Scholar]
- Popovitch MV, Glazunov RA, Potemkin AD, et al. Potreblenie alkogolia v Rossii [Alcohol consumption in Russia] Demoskop Weekly [Demoskop Weekly] 2004 Available at: http://www.demoscope.ru/weekly/2004/0143/analit02.php. (15 January 2013, date last accessed) [Google Scholar]
- Pugach PV. St. Peterburg, Russia: St. Peterburg's State Paediatric Medical Academy; 2012. Vliianie dlitelnosti etanolovoi intoksikatcii na krys i immunnye organy ikh potomstva [The effects of time and duration of ethanol intoxication on rats and the immune organs of their breed] Doctoral Dissertation. [Google Scholar]
- Radzinsky VE. Moskva: RUDN; 2002. p. 545. Patologicheskoe akusherstvo. V Akusherstvo. Praktikum v 3-kh chastiakh [Pathological obstetrics. In Radzinsky VE (ed). Obstetrics. Practical Course in 3 Parts] [Moscow: People Friendship University of Russia] [Google Scholar]
- Radzinsky VE, Kostin IN. Moskva: Eksmo; 2009. pp. 81–6. Faktory perinatalnogo riska: vrednye privychki. V Akusherskii risk. Maksimum informatcii minimum opasnosti dlia materi i mladentca [Perinatal risk factors: addictions. In Obstetrical Risk. Maximum Information Minimum Danger for Mother and Newborn] [Moscow: Eksmo] [Google Scholar]
- Ramazanova LM, Semiatov SM. Alkogol i ego vliianie na plod [Alcohol and its effects on the foetus] Vestnik Rossiiskogo Universiteta Druzhby Narodov. Seriia: Meditcina [Bull of People Friendship University of Russia] 2002;1:274–81. [Google Scholar]
- Regentova AY. Informirovannost kak faktor vliianiia na otnoshenie zhenshchin k upotrebleniiu alkogolia vo vremia beremennosti [Awareness as a factor of influence on women's attitudes to alcohol consumption during pregnancy] Vestnik IuUrGU [Bull South Ural's State University] 2012;31:109–14. [Google Scholar]
- Riley EP, Mattson SN, Li T-K, et al. Neurobehavioral consequences of prenatal alcohol exposure: An international perspective. Alcohol Clin Exp Res. 2003;27:362–73. doi: 10.1097/01.ALC.0000052703.38558.B2. [DOI] [PubMed] [Google Scholar]
- Robert M, Carceller A, Domken V, et al. Physical and neurodevelopmental evaluation of children adopted from Eastern Europe. Can J Clin Pharmacol. 2009;16:432–40. [PubMed] [Google Scholar]
- Roberts G, Nanson J. Best Practices. Fetal Alcohol Syndrome/Fetal Alcohol Effects and the Effects of Other Substance Use During Pregnancy. Ottawa, ON: Canada's Drug Strategy Division, Health Canada; 2000. [Google Scholar]
- Ruchkin V, Gilliam WS, Mayes L. Developmental pathway modeling in considering behavior problems in young Russian children. Child Psychiatry Hum Dev. 2008;39:49–66. doi: 10.1007/s10578-007-0070-9. [DOI] [PubMed] [Google Scholar]
- Sashchenko AI. Moscow, Russia: People Friendship University of Russia; 2007. Fetoplatcentarnaia sistema pri alkogolizme i tabakokurenii [Fetoplacental system in women with alcoholism and tobacco consumption] Doctoral Dissertation. [Google Scholar]
- Semenov AS, Serganova TI, Skalny AV, et al. O vliianii alkogolizma roditelei na razvitie potomstva [The effect of alcoholic parents on the development of the offspring] Pediatriia [Paediatrics] 1987;4:49–53. [PubMed] [Google Scholar]
- Shabanov PD, Lebedev AA, Bychkov ER. Vliianie vnutriutrobnogo deistviia etanola na sozrevanie monoaminergicheskikh sistem v razvivaiushchemsia mozge krys [Effects of intrauterine alcohol exposure on the monoamiergic system maturation in the rat's developing brain] Ross Fiziol Zhurnal im I.M. Sechenova [Rus Physiol J named after I.M. Sechenov] 2012;98:202–11. [Google Scholar]
- Sheffer KK. St. Peterburg, Russia: St. Peterburg's State Paediatric Medical Academy; 2012. Funktcionalnoe sostoianie zritelnogo analizatora u detei podrostkovogo vozrasta s fetalnym alkogolnym sindromom [Functional conditions of the visual analyzer in adolescents with fetal alcohol syndrome] Doctoral Dissertation. [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA, et al. Fetalnyi alkogolnyi spektr narushenii sredi vospitannikov domov rebenka [Fetal Alcohol Spectrum Disorder in orphans] Narkologiia [Narcology] 2008a;11:53–6. [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA. Fetalnyi alkogolnyi sindrom [Fetal alcohol syndrome] Nizhegorodskii Meditcinskii Zhurnal [N Novgorod's Med J] 2008b;2:94–8. [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA, et al. Kliniko-eksperimentalnye sopostavleniia pri fetalnom alkogolnom sindrome [Clinical and experimental comparisons in fetal alcohol syndrome] Uralskii Meditcinskii Zhurnal: Pediatriia [Ural's Med J Paediatrics] 2009a;7:25–8. [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA, et al. Fetalnyi alkogolnyi sindrom: kliniko-eksperimentalnye sopostavleniia [Fetal alcohol syndrome: clinical and experimental comparisons] Narkologiia [Narcology] 2009b;8:38–40. [Google Scholar]
- Shilko VI, Malakhova ZL, Shukshina ZL. Fetalnyi alkogolnyi spektr narushenii sredi vospitannikov sotcialnykh uchrezhdenii [Fetal Alcohol Spectrum Disorder in children from foster homes] Kazanskii Meditcinskii Zhurnal [Kazan's Med J] 2009c;90:647–50. [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA. Porazhenie golovnogo mozga pri fetalnom alkogolnom sindrome [Brain damage in fetal alcohol syndrome] Biulleten Eksperimentalnoi Biologii i Meditciny [Bull Exp Biol Med] 2010a;150:100–3. doi: 10.1007/s10517-010-1077-y. [DOI] [PubMed] [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA, et al. Fetalnyi alkogolnyi spektr narushenii sredi vospitannikov domov rebenka [Fetal Alcohol Spectrum Disorder in orphans] Vestnik VolGMU [Bull Volgograd's State Med Academy] 2010b;4:108–11. [Google Scholar]
- Shilko VI, Zilber MY, Malakhova ZL. Transformiruiushchii faktor rosta u beremennykh zhenshchin stradaiushchikh alkogolizmom, i u detei s fetalnym alkogolnym sindromom [Transforming growth factor in pregnant alcohol dependent women and in children with fetal alcohol syndrome] Rossiiskii Vestnik Perinatologii i Pediatrii [Rus Bull Perinatalogy Paediatry] 2010c;6:20–2. [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA. Fetalnyi alkogolnyi sindrom: kliniko-patogeneticheskaia kharakteristika posledstvii u detei rannego vozrasta [Fetal Alcohol Syndrome: Clinical and Pathogenetic Characteristics of the Consequences in Infants] Ekaterinburg: UrGMA; 2011a. [Ekaterinburg, UrGMA] [Google Scholar]
- Shilko VI, Malakhova ZL, Bubnov AA. K patogenezu fetalnogo alkogolnogo sindroma [The pathogenesis of Fetal Alcohol Syndrome] Vestnik Uralskoi Meditcinskoi Akademicheskoi Nauki [Bull Ural's Med Acad Sci] 2011b;3:55–8. [Google Scholar]
- Shilko VI, Malakhova ZL, Zilber MY. O roli transformiruiushchego faktora rosta TGF-b1 v razvitii fetalnogo alkogolnogo sindroma [About the role of transforming growth factor TGF-b1 in the development of Fetal Alcohol Syndrome] Nauchno-prakticheskii Zhurnal ‘Kliniko-laboratornyi Konsilium’ [Sci Pract J ‘Clin Lab Concillium’] 2011c;1:46–8. [Google Scholar]
- Shurygin GI. Ob osobennostiakh psikhicheskogo razvitiia detei ot materei, stradaiushchikh khronicheskim alkogolizmom [About the characteristics of the mental development of children of mothers with chronic alcoholism] Pediatriia [Paediatrics] 1974;11:71–3. [PubMed] [Google Scholar]
- Shushpanova TV, Solonsky AV. Sinaptogenez i formirovanie benzodiazepinovykh retceptov mozga cheloveka v usloviiakh prenatalnoi alkogolizatcii [Synaptogenesis and Benzedrine receptor formation in human brain under prenatal alcohol exposure] Zhurn Nevr i Psikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 2012;1:60–7. [Google Scholar]
- Skalny AV, Skosyreva AM. Defitcit tcinka u materi, ploda i potomstva pri zloupotreblenii alkogolem [Zinc deficit in the mother, foetus and offspring when alcohol abuse is present] Akusherstvo i Ginekologiia [Obstet Gynaecol] 1987;4:51–6. [PubMed] [Google Scholar]
- Skalny AV, Kampov-Polevoi AB, Voronin AE. Vliianie tcinka na aktivnost etanolokisliaiushchikh fermentov potomkov alkogolizirovannykh krys [Effects of zinc on ethanol acidic activity in a breed of alcohol-exposed rats] Mikroelementy v Meditcine [Microelements Med] 2001;2:21–3. [Google Scholar]
- Skalny AV, Kin KL, Chembers KD, et al. Narushenie obmena tcinka pri prenatalnom vozdeistvii alkogolia [Zinc metabolism disturbances under prenatal alcohol exposure]. V: I Ross. Natcionalnii Kongress po Narkologii s Mezhdunarodnym Uchastiem [In: 1st Rus National Congress on Narcology with International Participation]; Moscow, Russia: 2009. pp. 18–9. 24–27 Nov 2009. [Google Scholar]
- Skosyreva AM. Vliianie etilovogo spirta na razvitie embrionov stadii organogeneza [Effects of alcohol on the development of embryos on the stage of organogenesis] Akusherstvo i Ginekologiia [Obstet Gynaecol] 1973;4:15–8. [PubMed] [Google Scholar]
- Skosyreva AM. Deistvie etilovogo spirta v period ontogeneza [Effects of alcohol during ontogenesis] Akusherstvo i Ginekologiia [Obstet Gynaecol] 1980;12:7–9. [PubMed] [Google Scholar]
- Skosyreva AM, Balika YuD, Kartasheva VE. Vliianie etilovogo spirta na razvitie embriona i ploda v eksperimente [Effects of alcohol on the development of the embryo and foetus in an experimental setting] Akusherstvo I Ginekologiia [Obstet Gynaecol] 1973;4:18–20. [Google Scholar]
- Sofronova GI, Palchik AB. Features of maternal alcohol consumption and fetal alcohol syndrome in the Sakha Republic. J Popul Ther Clin Pharmacol. 2012;19:e405–6. [Google Scholar]
- Sokolovskaya TA, Azarko AE, Dmitrieva OV. Vliianie alkogolizma roditelei na formirovanie invalidnosti u detei [Effects of parental alcohol-exposure on developmental disabilities in children] Informatcionno-analiticheskii vestnik ‘Sotcialnye Aspekty Zdorovia Naseleniia’ [Inf Anal J ‘Soc Aspects Popul Health’] 2009 Available at http://vestnik.mednet.ru/content/view/110/30/ (15 January 2013, date last accessed) [Google Scholar]
- Solonsky AV. Formirovanie krovenosnykh sosudov embrionalnogo mozga cheloveka v usloviiakh prenatalnoi alkogolizatcii [Formation of blood vessels in the human embryonic brain in conditions of prenatal alcohol exposure] Zhurn Nevr iPsikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 2006;12:71–3. [Google Scholar]
- Solonsky AV. Tomsk, Russia: Siberia's State Medical Academy; 2008. Morfologicheskie zakonomernosti rannikh stadii razvitiia golovnogo mozga v usloviiakh prenatalnoi alkogolizatcii [Morphological regularities of early stages of the brain developmentunder conditions of parental alcohol exposure] Doctoral Dissertation. [Google Scholar]
- Solonsky AV, Logvinov SV. Ultrastrukturnye i morfometricheskie osobennosti sinaptogeneza mozga embriona i plodov cheloveka v usloviiakh prenatalnogo vozdeistviia etanola [Ultrastructural and morphological characteristics of synaptogenesis of the brain in human embryos and foetuses during parental alcohol exposure] Biulleten Sibirskoi Meditciny [Bull Siberia Med] 2008;7:35–9. [Google Scholar]
- Stromland K, Mattson SN, Adnams CM, et al. Fetal alcohol spectrum disorders: an international perspective. Alcohol Clin Exp Res. 2005;29:1121–6. [Google Scholar]
- Sverdlova AV. Vliianie prenatalnoi etanolovoi khronicheskoi intoksikatcii na razvitie potomstva krys v rannie sroki postnatalnogo ontogeneza (po pokazateliam nefrogeneza) [Effects of prenatal chronic alcohol intoxication on the development of offsprings of rats in early stage of postnatal ontogenesis (based on the indicators of nephrogenesis)] Fundamentalnye Issledovaniia [Fundam Res] 2008;1:148–50. [Google Scholar]
- Tabolin VA, Uryvchikov GA. Alkogolnyi sindrom ploda: (Obzor literatury) [Fetal Alcohol Syndrome: literature review] Vopr Okhrany Materinstva i Detstva [Matern Child Prot Issues] 1986;5:48–54. [Google Scholar]
- Talykova LV, Vaktskjold A, Serebrjakova NG, et al. Pregnancy health and outcome in two cities in the Kola Peninsula, northwestern Russia. Int J Circumpolar Health. 2007;66:168–81. doi: 10.3402/ijch.v66i2.18249. [DOI] [PubMed] [Google Scholar]
- The St. Petersburg-USA Orphanage Research Team. Characteristics of children, caregivers, and orphanages for young children in St. Petersburg, Russian Federation. J Appl Dev Psychol. 2005;26:477–506. [Google Scholar]
- Uliyanovskaia TN, Solovev AG. Sotcialno-psikhologicheskie osobennosti beremennykh zhenshchin, upotrebliaiushchikh alkogol [Socio-psychological characteristics of pregnant women consuming alcohol] Ekologiia Cheloveka [Hum Ecol] 2010;4:42–5. [Google Scholar]
- Usova EV, Sazonova NS, Rassadina ZA. Sindrom alkogolnoi embriopatii [Alcohol embryopathy syndrome] Zhurn nevr i Psikhiatr im S.S. Korsakova [J Neur Psychiatry named after S.S. Korsakov] 1981;81:1552–6. [PubMed] [Google Scholar]
- Vyatchanina ES, Skalny AV. Izuchenie vliianiia upotrebleniia alkogolia materiu do beremennosti na elementnyi sostav kory golovnogo mozga potomstva (eksperimentalnoe issledovanie) [Research study on the influence of maternal alcohol consumption before pregnancy on the offspring's cortex structure (experimental study)]. V: I Ross. Natcionalnii Kongress po Narkologii s Mezhdunarodnym Uchastiem [In: 1st Rus National Congress on Narcology with International Participation]; Moscow, Russia: 2009. pp. 7–8. 24–27 Nov 2009. [Google Scholar]
- Warren KR, Calhoun FJ, May PA, et al. Fetal alcohol syndrome: an international perspective. Alcohol Clin Exp Res. 2001;25:202S–6S. doi: 10.1097/00000374-200105051-00033. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Geneva: WHO Regional Office for Europe; 2010. European Status Report on Alcohol and Health 2010. Available at: http://www.euro.who.int/en/what-we-do/health-topics/disease-prevention/alcohol-use/publications/2010/european-status-report-on-alcohol-and-health-2010. (7 July 2013, date last accessed) [Google Scholar]
- World Health Organization (WHO) Geneva: WHO; 2011. Global Status Report on Alcohol and Health. Available at: http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/rus.pdf. (7 July 2013, date last accessed) [Google Scholar]
- Zabludovsky AL, Shikhov NS, Maizelis MY. Moskva: Nauka; 1989. pp. 21–7. Osobennosti povedenie i uslovnoreflektornoi deiatelnosti zhivotnykh, podvergshikhsia vnutriutrobnym vozdeistviiam etanola.V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod.red. Airapetiantc MG [Characteristics of behaviour and conditioned reflex activity in animals exposed to ethanol in utero. In Ayrapetyants MG (ed). The Consequences of Alcohol Intoxication for Posterity] [Moscow: Science] [Google Scholar]
- Zhulin VV, Bazyan AS. Moskva: Nauka; 1989. pp. 15–9. Vliianie vnutriutrobnogo vliianiia etanola na nekotorye neiromediatornye sistemy kory mozga krys. V Posledstviia alkogolnoi intoksikatcii dlia potomstva, pod.red. Airapetiantc M.G. [Influence of prenatal ethanol exposure on several neurotransmitter systems of the cerebral cortex of rats]. Posledstviia alkogolnoi intoksikatcii dlia potomstva [In Ayrapetyants MG (ed). The consequences of alcohol intoxication for posterity] [Moscow: Science] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.