Abstract
Aims: The aim of the study was to assess the cumulative evidence on the effectiveness of brief alcohol interventions in primary healthcare in order to highlight key knowledge gaps for further research. Methods: An overview of systematic reviews and meta-analyses of the effectiveness of brief alcohol intervention in primary healthcare published between 2002 and 2012. Findings: Twenty-four systematic reviews met the eligibility criteria (covering a total of 56 randomized controlled trials reported across 80 papers). Across the included studies, it was consistently reported that brief intervention was effective for addressing hazardous and harmful drinking in primary healthcare, particularly in middle-aged, male drinkers. Evidence gaps included: brief intervention effectiveness in key groups (women, older and younger drinkers, minority ethnic groups, dependent/co-morbid drinkers and those living in transitional and developing countries); and the optimum brief intervention length and frequency to maintain longer-term effectiveness. Conclusion: This overview highlights the large volume of primarily positive evidence supporting brief alcohol intervention effects as well as some unanswered questions with regards to the effectiveness of brief alcohol intervention across different cultural settings and in specific population groups, and in respect of the optimum content of brief interventions that might benefit from further research.
INTRODUCTION
A range of interventions exist for the prevention and treatment of alcohol-related risk and harm, from health-promoting input aiming at reducing hazardous and harmful drinking, to more intensive and specialist treatment for severely dependent drinking. Primary healthcare is seen as an ideal context for the early detection and secondary prevention of alcohol-related problems, due to its high contact-exposure to the population (Lock et al., 2009), and the frequency with which higher-risk drinkers present (Anderson, 1985).
In particular, screening and brief intervention for alcohol has emerged as a cost-effective preventative approach (Hutubessy et al., 2003), which is relevant and practicable for delivery in primary healthcare (Raistrick et al., 2006), where patients tend to present with less acute conditions, return regularly for follow-up appointments (Bernstein et al., 2009) and build long-term relationships with their GP (Lock, 2004). These interventions are typically short in duration (5–25 min), designed to promote awareness of the negative effects of drinking and to motivate positive behaviour change (HoC Health Committee, 2010).
Despite considerable efforts over the years to persuade practitioners to adopt brief interventions in practice, most have yet to do so. Indeed, there is an international literature on barriers to brief alcohol intervention (Heather, 1996; Kaner et al., 1999; Babor and Higgins-Biddle, 2000; Aalto et al., 2003; Aira et al., 2003; Wilson et al., 2011), the majority focussing on primary healthcare. These barriers include: lack of time, training and resources; a belief that patients will not take advice to change drinking behaviour; and a fear amongst practitioners of offending patients by discussing alcohol. It has therefore been argued that today's challenge is more about how to encourage the uptake and use of brief alcohol intervention in routine practice (Anderson et al. 2004; Nilsen et al., 2006; Johnson et al., 2010; Kaner, 2010a; Gual and Sabadini 2011), and less about financing additional research on its effectiveness. It would seem timely, therefore, to evaluate the extent to which the primary healthcare brief alcohol intervention evidence base is now saturated, or whether there are any remaining knowledge gaps requiring further investigation.
This paper reports on the EU co-funded research BISTAIRS (brief interventions in the treatment of alcohol use disorders in relevant settings) project, which aims to intensify the implementation of brief alcohol intervention by identifying, systematizing and extending evidence-based good practice across Europe. Given the existence of several reviews in this field, and the overarching BISTAIRS timescale, the first phase of the project comprised a systematic overview of published reviews to provide a structured, comprehensive summary of the evidence base on the effectiveness of brief alcohol intervention in primary healthcare.
The focus on effectiveness (how an intervention performs in real world conditions) as opposed to efficacy (how an intervention performs under optimal or ideal world conditions) is deliberate. There is a well-established literature on the distinction between efficacy and effectiveness trials (Flay, 1986), although the terms explanatory or pragmatic trials are sometimes also used (Thorpe et al., 2009). However, placing trials into one category or other is challenging since there is wide agreement that they actually sit on a continuum from optimized to naturalistic conditions (Gartlehner et al., 2006). Moreover, efficacy must be demonstrated before effectiveness is assessed and the latter is a necessary pre-condition for wider dissemination (Flay et al., 2005). The US Society for Prevention Research (Flay et al., 2004, 2005) has outlined that efficacy testing requires at least two rigorous trials involving: tightly defined populations; psychometrically sound measures and data collection procedures; rigorous statistical analysis; consistent positive effects (without adverse effects); and at least one significant long-term follow-up. This requirement has been comprehensively established in a field where over 60 high-quality brief intervention trials have been reported in peer-reviewed journals, with over half based in primary healthcare (Kaner, 2010b).
This paper focuses on effectiveness, adding clinical breadth to methodological rigour by: extending the range of patients and delivery agents in trials; specifying details of necessary training and technical support; clarifying the nature of comparison or control conditions; assessing intervention fidelity; and conducting unbiased (generally intention to treat) analyses, which also considers effects on different sub-groups of patients and differing outcome exposures (Flay et al., 2005; Thorpe et al., 2009). To add to the brief alcohol intervention literature, we synthesize the findings from a rapidly growing number of systematic reviews to answer four questions: (a) does the cumulative evidence base continue to show that brief alcohol intervention is effective when delivered in primary healthcare settings? (b) is brief alcohol intervention equally effective across different countries and different healthcare systems? (c) is the brief alcohol intervention evidence base applicable across different population groups? and (d) what is the optimum length, frequency and content of brief alcohol intervention, and for how long is it effective?
METHODS
Standard systematic reviewing methods were tailored to identify existing reviews rather than primary research (CRD, 2001). Reporting was carried out according to PRISMA statement guidelines (Moher et al., 2009) (see Supplementary material, Appendix 1 for full details). The review team comprised international experts in the field of brief alcohol interventions (EK, PA) and in systematic reviewing methods (DNB).
One author (AO) searched MEDLINE, EMBASE, PsycInfo, The Cochrane Database, The Database of Abstracts of Reviews of Reviews and the Alcohol and Alcohol Problems Science Database between July and August 2012 using appropriate MeSH terms. The search was split into three core concepts: (a) setting: general practice, general practitioners, physician, family practice, primary health care, community health services and family physician; (b) intervention: alcohol, brief intervention, early intervention, alcohol therapy, counselling and intervention; and (c) study design: systematic review, review and meta-analysis (full details of database-specific search terms are available upon request from the corresponding author). Reference lists of selected reviews and relevant websites, including the National Institute for Health and Care Excellence and the World Health Organisation, were also searched and appropriate experts contacted in order to identify unpublished reviews. The title and abstract of all records were screened by a single reviewer (AO), with full text copies of potentially relevant papers retrieved for in-depth review against the inclusion criteria. Any queries were resolved through discussion with the wider review team (AO, DNB, EK, PA).
Full systematic reviews and meta-analyses of studies examining the effectiveness of brief alcohol intervention in comparison to control conditions in primary healthcare settings and published between 2002 and 2012 were eligible for inclusion. Primary healthcare was operationalized to include all immediately accessible general healthcare facilities but not emergency settings. Brief intervention was defined as a single session and/or up to a maximum of five sessions of engagement with a patient, and the provision of information and advice designed to achieve a reduction in risky alcohol consumption or alcohol-related problems. Primary outcomes of interest included changes in self- or other reports of drinking quantity and/or frequency, drinking intensity and drinking within recommended limits.
The methodological quality of eligible studies was assessed independently by two reviewers (AO and DNB) using the Revised Amstar tool (R-AMSTAR) (Kung et al., 2010). Data were extracted on: healthcare setting; characteristics of the target population; authors' conclusions; and any identified evidence gaps. Data were extracted against a data abstraction template by one author (AO) and checked by another (DNB) with reference to the full article text. Extracted data also included inclusion/exclusion criteria, reported analyses and analysis type. No statistical analyses or meta-analyses were conducted. Instead, the existing analyses reported in the articles reviewed were extracted systematically, with the findings reported in a structured narrative synthesis.
RESULTS
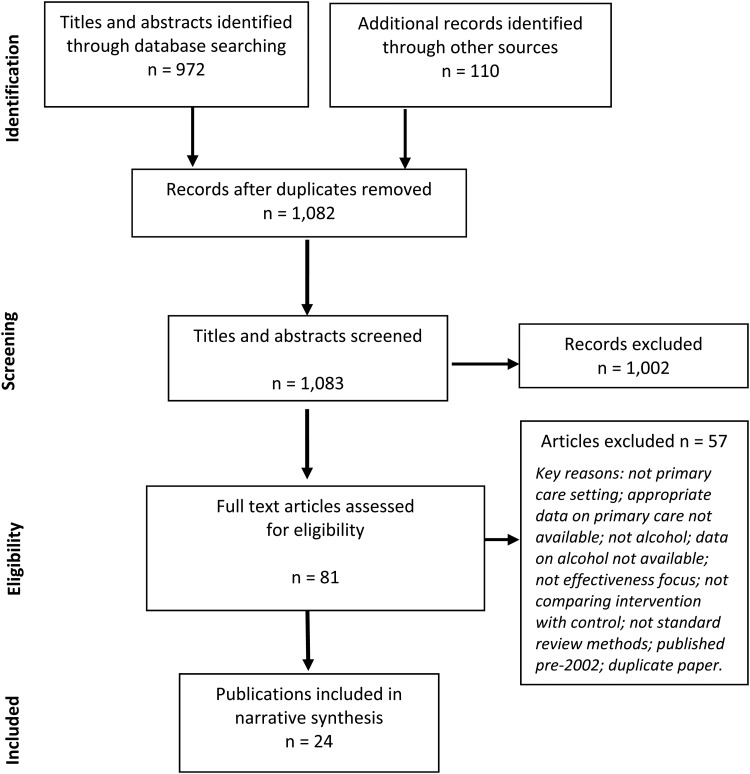
Twenty-four individual systematic reviews met the eligibility criteria (see Figure 1) (Chang, 2002; Moyer et al., 2002; Beich et al. 2003; Berglund et al. 2003; Huibers et al., 2003; Ballesteros et al., 2004a,b; Cuijpers et al., 2004; Whitlock et al., 2004; Bertholet et al., 2005; Littlejohn, 2006; Gordon et al., 2007; Kaner et al., 2007; Parkes et al., 2008; Solberg et al., 2008; Peltzer, 2009; Jackson et al., 2010; Latimer et al., 2010; Saitz, 2010; Bray et al., 2011; Gilinsky et al., 2011; Sullivan et al., 2011; Jonas et al., 2012; Babor et al., 2013). Establishing the precise number of unique trials covered by this evidence base is challenging due to the slightly different emphases of some reviews. Nevertheless, we identified 56 primary healthcare trials reported across 80 separate publications.
Fig. 1.
Flow chart showing the number of potentially relevant references identified by searches and number meeting inclusion criteria and included in the narrative review of systematic reviews.
The mean R-AMSTAR score for the 24 included reviews was 29 (median 30.5; range 13–44). These numeric scores translated into grades as follows: 13–20 = D; 21–28 = C; 29–36 = B; and 37–44 = A. Using R-AMSTAR scoring, five reviews were categorized as an ‘A’ grade publication (Huibers et al., 2003; Bertholet et al., 2005; Kaner et al., 2007; Sullivan et al., 2011; Jonas et al., 2012), eight were categorized as ‘B’ (Beich et al., 2003; Ballesteros et al., 2004a,b; Jackson et al., 2010; Latimer et al., 2010; Bray et al., 2011; Gilinsky et al., 2011; Babor et al., 2013), seven as ‘C’ (Cuijpers et al., 2004; Whitlock et al., 2004; Littlejohn, 2006; Gordon et al., 2007; Parkes et al., 2008; Solberg et al., 2008; Saitz, 2010) and four as ‘D’ (Chang, 2002; Moyer et al., 2002; Berglund et al., 2003; Peltzer, 2009). Table 1 and the following sections report the key findings against each focus review question, with additional characteristics of the included reviews available in Supplementary material, Appendix 2.
Table 1.
Summary of authors' conclusions and identified evidence gaps
| Study | Q1: Is alcohol BI for alcohol effective when delivered in primary health care settings? | Q2: Is alcohol BI equally effective across different countries/health care systems? | Q3: Is the alcohol BI evidence base applicable to all population groups? | Q4: What is the optimum length/frequency/content of alcohol BI and how long is it effective? |
|---|---|---|---|---|
| Babor et al. (2013) (in press) | Consistently reported that BI was clinically and cost-effective for non-treatment seeking populations. | Majority of evidence has limited or no LAMIC (low and middle income countries) applicability. Whilst there is some evidence to suggest that alcohol BI equality effective in HIC (high income countries) and LAMIC, however context-specific health issues may not be adequately addressed solely by HIC research findings. Therefore more culturally-specific research needed in LAMIC. |
Brief intervention in primary health care appears to be most impactful in non-treatment seeking populations. Inconclusive findings on alcohol BI in antenatal settings. |
Question not addressed in this review |
| Ballesteros et al. (2004a) | Results suggest BI equally effective in both men and women. | Question not addressed in this review | Results support the equality of BI outcomes for reducing hazardous alcohol consumption in both men and women. | Question not addressed in this review |
| Ballesteros et al. (2004b) | Although indicating smaller effect sizes than previous meta-analyses, results support the moderate efficacy of BIs. | Question not addressed in this review | BI appears to have greater efficacy when applied in general screening programs to non-treatment seeking populations. | Suggested more research needed to establish whether extended BI more efficacious than BI. Also, identified need for further naturalistic studies on long-term BI efficacy. |
| Beich et al. (2003) | Results suggests alcohol BI effective, though at lower levels than reported previously (pooled absolute risk reduction from BI was 10.5% (95% CI 7.1–13.9%) A random effects model yielded a similar result: 10% (6–14%). The pooled number needed to treat (NNT) was 10 (7 to 14)). | Question not addressed in this review | Question not addressed in this review | Question not addressed in this review |
| Berglund et al. (2003) | Majority (18 of 25 RCTs) showed BI had a significant positive effect in health care settings (primary care and hospital settings). Some evidence for positive impact on number of hospital days/incidence of new injuries and need for hospital care. |
Question not addressed in this review | (Limited) evidence suggests alcohol BI equally effective in men and women. However notes that most studies conducted with populations consisting of middle-aged male heavy drinkers. Lack of evidence on treatment of homeless patients and for patients with psychiatric co-morbidity. Although some studies included dependent patients, review excluded any studies focused on this group of patients only. |
However, uncertainty/limited evidence on longer-term effect sizes of alcohol BI (past 2 years). Review excluded studies that compared BI with extended BI but highlighted lack of evidence on design of optimal BI. |
| Bertholet et al. (2005) | Alcohol BI effective in reducing alcohol consumption at 6 and 12 months (adjusted intention-to-treat analysis showed a mean pooled difference of −38 g/week in favour of the BI group). Limited evidence on impact on reduction of health care utilization. |
Question not addressed in this review | BI was concluded to be beneficial in men and women in a primary care context. | Lack of evidence of alcohol BI on morbidity, mortality and quality of life measures. More research needed to identify which components of BI present evidence of efficacy in primary health care. |
| Bray et al. (2011) | Alcohol BI has a small, negative effect on emergency department utilization. However no significant effect was found for outpatient or in patient health care utilization. | Question not addressed in this review | Question not addressed in this review | Question not addressed in this review |
| Chang (2002) | Findings suggest that alcohol BI do not appear to be consistently helpful to women drinkers. | Question not addressed in this review | Mixed/inconsistent evidence for alcohol BI effectiveness in both genders. However, pregnant women were found to reduce their drinking in two of the studies reviewed; thus pregnancy may provide a powerful incentive to reduce alcohol drinking. | Question not addressed in this review |
| Cuijpers et al. (2004) | Findings suggest positive impact of alcohol BI on reducing mortality (although limited detailed/verified data available from alcohol BI trials on mortality rates between pre-test and follow-up). Pooled relative risk (RR) of dying in BI compared to control conditions was 0.47 for the four studies (95% CI: 0.25, 0.89). The pooled RR of all 32 studies was comparable (RR = 0.57; 95% CI: 0.38, 0.84). |
Meta-analysis of mortality only included USA, UK and Australian data. | Acknowledged fact that study populations differed considerably, although sensitivity analyses suggested comparable outcomes. | Acknowledges variation in content of included interventions but emphasizes that multiple sensitivity analyses excluding particular studies/sets of studies, all resulted in comparable BI outcomes. |
| Gilinsky et al. (2011) | There was some evidence from a small number of studies that singe session face to face brief interventions resulted in positive effects on the maintenance of alcohol abstinence during pregnancy. Women choosing abstinence as their drinking goals and heavier drinking women who participated with a partner were more likely to be abstinent at follow up. However more intensive interventions may be required to encourage women who continue to drink during pregnancy to reduce their consumption. |
Question not addressed in this review | Identified lack of high quality evidence for effectiveness of alcohol BI in pregnant women. Overall, there was insufficient evidence to determine whether such interventions delivered during the antenatal period are effective at helping women to reduce alcohol consumption during pregnancy. |
Question not addressed in this review |
| Gordon et al. (2007) | Although alcohol and dietary interventions appeared to be economically favourable (cost-effective), it is difficult to draw conclusions because of the variety in study outcomes. Generally, the costs of the behavioural interventions reviewed were low relative to those for other healthcare interventions such as pharmaceutical management. The behavioural interventions aimed at populations with high-risk factors for disease were more cost-effective than those aimed at healthy individuals. |
Question not addressed in this review | Noted tendency to omit cultural minorities in studies across multiple behavioural intention cost effectiveness studies. General lack of evidence (across multiple behavioural intention areas) of cost effectiveness for disadvantaged populations. |
Question not addressed in this review |
| Huibers et al. (2003) | Not possible to draw an overall conclusion concerning the effectiveness of ‘psychosocial interventions by general practitioners’ since studies were not comparable in numerous aspects (intervention, outcome, population). In relation to alcohol, review found that GP-delivered BI seem no more effective than other, more simple interventions or when delivered by a nurse practitioner. |
Question not addressed in this review | Question not addressed in this review | Question not addressed in this review |
| Jackson et al. (2010) | Evidence found for the positive impact of alcohol BI on alcohol consumption, mortality, morbidity, alcohol-related injuries, alcohol-related social consequences, and healthcare resource use. Further, alcohol BI were shown to be effective in both men and women. |
Question not addressed in this review | Study populations made up primarily of adults therefore limited evidence identified for the effectiveness of brief interventions in young people. Participants were mainly Caucasian in origin and ethnicity of study populations was poorly reported in general. Although socioeconomic status was not shown to influence the effectiveness of BI, there was limited evidence in this area. Limited evidence (only one review) of BI effectiveness in patients with dual diagnosis of psychiatric condition and alcohol misuse Relationship between the level of alcohol dependence and the effectiveness of brief interventions was unclear. |
Limited evidence suggests that even very brief interventions may be effective in reducing negative alcohol-related outcomes. The benefit arising from increased exposure or the incorporation of motivational interviewing principles was unclear. Due to the extensive heterogeneity/lack of reported detail in the characteristics of the brief interventions evaluated, it is difficult to define the effective components of brief interventions. |
| Jonas (2012) | Overall, evidence supports the effectiveness of behavioural interventions for improving several intermediate outcomes for adults, older adults, and young adults/college students (average reduction of 3.6 drinks per week for adults compared with control, 11% increase in the % of adults achieving recommended drinking limits over 12 months). | Question not addressed in this review | Limited data on effectiveness for pregnant women in terms of consumption; insufficient evidence with regards to reduction in heavy drinking episodes or with pregnant women, particular at 6 months+. Insufficient evidence on effectiveness in reducing heavy drinking episodes for older adults; on drinking within recommended limits for college age students; or on mean consumption, heavy drinking episodes or drinking within recommended limits for adolescents. Ethnicity data generally not reported for participants and low rates of non-White participants except for two included trials (one conducted in Thailand, 100% Thai) and one in urban academic practice (80–82% non-white). Not clear whether findings applicable to people with comorbid medical or psychiatric conditions. |
Brief multi-contact interventions have the best evidence of effectiveness across populations, outcomes, and have follow-up data over several years. However, differences between control and intervention groups not statistically significant past 48 months; and in general, insufficient evidence on effectiveness 6 months +. Insufficient evidence to draw firm conclusions on required intensity of intervention, including which specific components needed to be included. |
| Kaner et al. (2007) | Overall, brief interventions significantly lowered alcohol consumption at one year (mean difference: −38 grams/week, 95% CI: −54 to −23). Absence of a difference in outcomes between efficacy and effectiveness trials suggested that this literature was relevant to routine primary care. | Question not addressed in this review | Insufficient data on ethnic differences. Results suggest no significant positive effect of alcohol BI in women however there was a general lack of available evidence disaggregated by gender. |
Evidence suggests that longer duration of counseling has little additional effect. |
| Latimer et al. (2010) | Screening plus brief intervention is cost effective in the primary care setting. | Question not addressed in this review | Lack of evidence of long-term impacts of alcohol BI for young people. | Lack of evidence on long-term impacts of alcohol BI, particularly in relation to impact of re-application versus maintenance of original intervention impact. Uncertainty with regards to longer term health care resource us, crime and motor vehicle accident effects; and limited evidence on impact of alcohol BI on HRQL. Very brief interventions are likely to be more cost effective than extended brief interventions but highlighted heterogeneity of evidence base on length of BI. |
| Littlejohn (2006) | Post recruitment, patients’ SES does not appear to influence intervention outcome, with alcohol BI equally effective in patients of different socio-economic status. | Question not addressed in this review | Equivocal evidence with regards to link between SES and intervention participation. Suggested more research needed to better understand the characteristics of those who decline to participate in BI research. | Question not addressed in this review |
| Moyer et al. (2002) | 34 trials focused on prevention found small to medium aggregate effect sizes in favour of brief interventions in non-treatment seeking populations across different follow-up points. | Lack of evidence on effectiveness of alcohol BI in dependent patients. No significant difference in effect observed between men and women, but highlights lack of gender-focused studies in this field. |
Limited evidence on longer-term effects of alcohol BI (12 months +) and in general, results suggest a decay over time in impact. Overall, no significant difference in effects between brief versus extended interventions. |
|
| Parkes et al. (2008) | Some (limited) evidence to suggest alcohol BI can be effective in pregnant women and in women of child-bearing age. | Question not addressed in this review | Mixed evidence of efficacy of BI for pregnant women. In particular, lack of evidence of effect on different ethnic groups for pregnant women and on different income levels. | No evidence on long-term impact as follow up limited to 9 months at most in the included studies. |
| Peltzer (2009) | Brief alcohol interventions in sub-Saharan health settings showed positive results. | Although positive impacts identified, review highlights small number of trials and challenges experienced to embed in practice in sub-Saharan settings. | Question not addressed in this review | Question not addressed in this review |
| Saitz (2010) | Alcohol screening and BI has efficacy in primary care for patients with unhealthy but not dependent alcohol use. | Question not addressed in this review | Lack of evidence to support efficacy of alcohol BI in very heavy or dependent drinkers. Further, small sample sizes and other study design factors limit generalizability of findings. | Question not addressed in this review |
| Solberg et al. (2008) | Brief screening and counselling for alcohol misuse in primary care is both more effective/cost-effective than most other effective preventative services. Sparse data on efficacy in preventing alcohol-attributable morbidity and mortality. |
Question not addressed in this review | Highlights fact that dependent drinkers excluded or lack of disaggregated data on efficacy/adherence for dependent as opposed to non-dependent drinkers. | Limited evidence of long-term effectiveness (12 months +) and no studies at 5 years + |
| Sullivan et al. (2011) | Review offers preliminary support for the benefit of brief interventions for unhealthy alcohol use by non-physicians, either alone or in combination with physicians. There is evidence that non-physician-based interventions are as effective as physician-based interventions and when added to physician-based interventions can significantly improve drinking outcomes. However, summary effect size observed for non-physician interventions of 1.7 fewer standard drinks per week is smaller than that observed for other clinician-based interventions in primary care settings (2.7 fewer standard drinks per week but within the 95% CI [1.6–3.9 standard drinks] of that result). | Question not addressed in this review | Question not addressed in this review | Question not addressed in this review |
| Whitlock et al. (2004) | Alcohol BI in primary health care settings reduced risky and harmful alcohol use for several alcohol outcomes (at 6–12 months, brief counseling interventions (with up to 15 min contact and at least 1 follow-up) reduced the average number of drinks per week by 13–34% more than controls. The proportion of participants drinking at ‘safe’ levels was 10–19% greater than controls). | Question not addressed in this review | No consistent differences found between men and women. Some evidence to suggest alcohol BI effective in older populations in comparison with younger adults. Low or non-reported non-white participation |
Results suggested brief, multi-contact interventions more effective than very brief or brief single-contact interventions. Lack of evidence to determine relationship between intervention effects and specific BI components. Although all interventions that showed significant improvements in outcomes included at least 2 out of 3 key elements (feedback, advice and goal setting). Mixed/limited data on long-term mortality and morbidity benefits, especially for groups other than males, with less severe drinkers and with low-intensity interventions. One study reported maintenance of improved drinking at 4 years follow-up. |
Question 1: is brief alcohol intervention effective when delivered in primary healthcare settings?
Across the eligible reviews, it is consistently reported that brief alcohol interventions are effective at reducing hazardous and harmful drinking in primary healthcare (Moyer et al., 2002; Beich et al., 2003; Berglund et al., 2003; Ballesteros et al., 2004a,b; Cuijpers et al., 2004; Whitlock et al., 2004; Bertholet et al., 2005; Littlejohn, 2006; Gordon et al., 2007; Kaner et al., 2007; Solberg et al., 2008; Peltzer, 2009; Jackson et al., 2010; Latimer et al., 2010; Saitz, 2010; Bray et al., 2011; Gilinsky et al., 2011; Jonas et al., 2012). Whilst the overall evidence base suggests that brief alcohol interventions are effective in such settings, some individual trials have reported a null finding. Indeed a large UK trial (SIPS), not included in the reviews due to recency, has reported improvements in hazardous and harmful drinking in patients receiving simple feedback and a patient information leaflet (the control condition) as well as in those receiving 5 min of structured advice, and those receiving a further 20 min brief lifestyle counselling (Kaner et al. 2013). This null finding (no significant difference between the three conditions) accords with three systematic reviews focussing on control conditions only, which found consistently reduced drinking in these groups over time (Jenkins et al. 2009; Bernstein et al. 2010; McCambridge and Kypri 2011). Thus the mere fact of enrolment in a brief intervention trial may be associated with positive behaviour change due to a general ‘Hawthorn Effect’, whereby increased attention or scrutiny influences drinking, or volunteering in itself means that the individual has started a change process. Screening or assessment reactivity (a simple response to screening procedures or measurement of drinking behaviour) could also explain these reduced drinking trends. Lastly, regression to the mean is a real possibility in this field, since heavy drinking can spontaneously fall over time. Nevertheless, the cumulative (pooled) analyses reported in successive systematic reviews reveal positive brief intervention effects over and above those seen in control conditions who typically received assessment only, treatment as usual or written advice.
Weekly alcohol consumption was the most commonly reported outcome, and meta-analysis by Kaner et al. (2007) showed that compared with control conditions, brief intervention reduced the quantity of alcohol drunk by 38 g per week (95% CI (confidence interval): 23–54 g). This is slightly less than the overall effect size found by Jonas et al. (2012), which suggested that brief intervention compared with controls in primary healthcare reduced alcohol consumption by 49 g per week for adults aged 18–64 (95% CI: 33–66 g). However, the latter review also found average weekly reductions of 23 g (95% CI 8–38 g) for older adults aged 65 and over, and 23 g (95% CI 10–36 g) for young adults/college students aged 18–30 following brief alcohol intervention.
Delivery by a range of practitioners in primary healthcare settings has beneficial effects (Huibers et al., 2003), although findings of one review suggest that the effect sizes are greater if delivered by doctors (Sullivan et al., 2011). Finally, whilst available evidence remains limited, results from one meta-analysis found indications of the effectiveness of brief alcohol intervention on mortality outcomes, estimating a reduction in problem drinkers of about 23–36% (Cuijpers et al., 2004).
Question 2: is brief alcohol intervention equally effective across different countries and different health care systems?
There is a geographic bias, with the majority of previous research conducted in high-income regions, and in particular, English and Nordic speaking countries. Out of the 24 eligible reviews, fewer than half included data from studies based outside Europe and/or the developed world (ten reviews: Moyer et al., 2002; Berglund et al., 2003; Cuijpers et al., 2004; Whitlock et al., 2004; Bertholet et al., 2005; Peltzer, 2009; Latimer et al., 2010; Saitz, 2010; Jonas et al., 2012; Babor et al. 2013). As the review of reviews by Babor et al (2013) emphasizes, research findings from developed countries may not be generalizable to developing and transitional countries on a number of grounds. In addition to structural and political differences, there are known differences in drinking patterns and abstention rates between lower and higher income countries, and health consequences vary. Although the behavioural theory that underpins the design and delivery of brief intervention is likely to be ‘universally’ effective (Anderson et al., 2009), and certainly Jonas et al. (2012) found similar effectiveness for brief alcohol intervention both within and outside the USA, a need remains for further culturally-specific research in countries outside the USA and Western Europe in order to demonstrate this conclusively (Peltzer, 2009).
It is also worth mentioning that half the included reviews (12 reviews: Beich et al., 2003; Whitlock et al., 2004; Littlejohn, 2006; Gordon et al., 2007; Parkes et al., 2008; Peltzer, 2009; Latimer et al., 2010; Saitz, 2010; Bray et al., 2011; Gilinsky et al., 2011; Sullivan et al., 2011; Jonas et al., 2012) were based exclusively on studies published in the English language. Given the resulting potential for publication bias (authors are more likely to publish significant results in English-language journals (Egger et al., 1997)), this suggests a need for increased linguistic (alongside geographic) diversity in future systematic reviews in this field (Babor et al., 2013).
Question 3: is the brief alcohol intervention evidence base applicable across different population groups?
Although overall the evidence implies that brief alcohol intervention is equally effective in men and women (Ballesteros et al., 2004a; Whitlock et al., 2004; Bertholet et al., 2005), most studies to date have either focussed on male drinkers or not reported the data disaggregated by sex (Moyer et al., 2002; Berglund et al., 2003; Kaner et al., 2007). One review suggested that brief alcohol intervention may not be consistently helpful to women, or at least the results are more equivocal (Chang, 2002); and there is an identified lack of high-quality evidence on its effectiveness in pregnant women drinkers (Parkes et al., 2008; Gilinsky et al., 2011; Jonas et al., 2012; Babor et al., 2013). Whilst one review indicated that pregnancy itself may provide a powerful incentive to reduce alcohol drinking (Chang, 2002), another found insufficient evidence to determine the effectiveness of brief intervention delivered during the antenatal period, suggesting that more intensive interventions may be required to encourage women who continue to drink during pregnancy to successfully reduce their consumption (Gilinsky et al. 2011).
Further, whilst brief intervention appears to improve alcohol-related outcomes for adults aged eighteen and over, evidence on effectiveness at either end of the age spectrum is less conclusive. Previous research (predominantly conducted in US college settings) suggests that effects appear less long-lived for young adults and college-age students, and there is insufficient evidence of brief alcohol intervention effectiveness in both adolescents (Kaner et al. 2007; Jackson et al. 2010; Latimer et al. 2010) and older adults (Kaner et al. 2007; Jonas et al. 2012), with only one review showing effect in adults aged 65 and over (Whitlock et al. 2004)).
There was limited consideration of the impact of socio-economic status on the effectiveness of brief alcohol intervention in the majority of the included reviews, with a general acknowledgment of the lack of evidence for disadvantaged populations in those that did (Littlejohn, 2006; Gordon et al., 2007; Jackson et al., 2010). Further, a number of reviews noted the tendency for studies either to omit ethnic minorities (Gordon et al., 2007) or to be poorly reported where non-White participants were included (Whitlock et al., 2004; Kaner et al., 2007; Jackson et al., 2010; Jonas et al., 2012).
Finally, a number of reviews suggest that brief alcohol intervention was most impactful in non-treatment seeking, non-dependent patient populations (Moyer et al., 2002; Ballesteros et al., 2004b; Babor et al., 2013). However, other reviews highlight the equivocal nature of the existing evidence base (Jackson et al., 2010), and/or emphasize the exclusion or lack of disaggregated data in primary studies for dependent versus non-dependent patients (Berglund et al., 2003; Solberg et al., 2008). There was also a lack of conclusive evidence on the use of brief alcohol intervention in patients with co-morbid medical or psychiatric conditions (Berglund et al., 2003; Jackson et al., 2010; Jonas et al., 2012).
Question 4: what is the optimum length, frequency and content of brief alcohol intervention, and for how long is it effective?
Evidence also points towards a need for greater understanding of the temporal limits of brief alcohol intervention impact. Research shows that effect sizes are largest at the earliest follow-up points, with decay in intervention effects over time. This overview found limited information on the longer-term effectiveness of brief alcohol intervention past 48 months post-intervention (Moyer et al., 2002; Latimer et al., 2010; Jonas et al., 2012). In addition, although recent evidence suggests that greater effect sizes may be achieved with brief multi-contact interventions (each contact up to 15 min), compared with very brief (up to 5 min) and brief (>5 min, up to 15 min) single-contact interventions (Jonas et al., 2012), it is important to note that the 2007 Cochrane Review found that longer (more intensive) brief interventions offered no significant additional benefit over shorter input (Kaner et al., 2007).
Few reviews considered the impact of the actual content of interventions on their effectiveness (Berglund et al., 2003; Cuijpers et al., 2004; Whitlock et al., 2004; Jonas et al., 2012). In general, these reviews highlighted a lack of available evidence on this issue, mainly due to the heterogeneity of the included studies. Whitlock et al. (2004) reported that all interventions demonstrating statistically significant improvements in alcohol outcomes included at least two of the following three elements—feedback, advice and goal-setting—but added that, given that the most effective interventions were multi-contact, inevitably these also comprised additional assistance and follow-up. Further, as Beich et al. (2003) highlights, conversations about alcohol can take place in different ways in primary healthcare settings, thus the effectiveness of brief intervention may be as much down to the well-established ‘helping relationship’ between patient and practitioner as the frequency or content of contact per se.
DISCUSSION
This review of systematic reviews supports the effectiveness of brief intervention at reducing alcohol-related problems across 56 trials and a wide range of patients in primary healthcare. However, it highlights knowledge gaps regarding the effectiveness of brief alcohol intervention with pregnant women, with older and younger drinkers, with those from ethnic minority groups, and in transitional and low income countries. There is also a need to determine the optimum length, frequency and necessary content of brief intervention required to maintain longer-term effects.
Further, although the general consensus is that brief alcohol interventions are ill-suited to the needs of dependent drinkers, who require more specialist and intensive support (Saitz, 2010), it is inevitable that routinely screening patients for excessive alcohol use in primary healthcare—an essential precursor to intervention—will identify those at the dependence end of the spectrum. Whilst primary healthcare practitioners clearly have an important role to play in terms of ‘signposting’ alcohol-dependent patients to more specialist treatment, they are also presented with a prime opportunity to deliver an intervention themselves at that point. Along with pharmacotherapy, modelling work by Rehm and Roerecke (2013) suggests that brief intervention in hospital settings is most effective at reducing mortality in alcohol-dependent patients. However, at present, comparable modelling data for this group of drinkers in primary healthcare settings are not available due to lack of alcohol consumption or diagnosis information (Purshouse et al., 2013). With fewer than 10% of people affected by alcohol dependence currently receiving treatment (Alonso et al., 2004), there may be considerable value in furthering our understanding of the extent to which brief interventions delivered in primary healthcare work in dependent drinkers. Given the dose–response relationship of alcohol consumption and related harms, greater health gains can be achieved with a 10% reduction from a dependent drinker than from a 10% reduction from a hazardous or harmful drinker (Rehm and Roerecke, 2013).
Yet even in populations and settings where brief alcohol intervention is known to be effective, there remain unanswered questions about which ‘active ingredients’ make for successful interventions (Kaner, 2010a). Research in primary healthcare settings shows that most control groups report a decrease in alcohol consumption, suggesting the possibility of either regression to the mean (in which extreme measures of behaviour tend to shift to less extreme positions over time), or that screening or assessment reactivity affects outcomes (i.e. assessments of alcohol use themselves contain a therapeutic element) (Bertholet et al., 2005; Jonas et al., 2012). Findings from three recent reviews appear to support this latter explanation (Jenkins et al., 2009; Bernstein et al., 2010; McCambridge and Kypri, 2011) and most recently, the results of the SIPS alcohol screening and brief intervention research programme also suggest that their trial control condition, consisting of simple feedback and written information about alcohol, may have contained active factors of behaviour change (Kaner et al., 2013).
Further, as Mitchie et al. (2012) acknowledge, the issue of treatment fidelity presents an additional obstacle to our understanding of brief alcohol intervention effectiveness. For a variety of reasons, busy physicians dealing with alcohol in routine practice settings may deviate from guidelines and protocols of care (Moriarty et al., 2012), as happens in other areas of clinical practice (Dew et al., 2010). Thus, even when practitioners can be persuaded to engage in brief alcohol intervention, it is not possible to establish conclusively the causal chain between interventions as designed, and their subsequent outcomes (an issue that further complicates questions around which intervention components have most impact on alcohol-related outcomes (McCambridge, 2013)).
These evidence gaps are not merely an academic concern. Given that the demand for healthcare is always likely to outstrip supply, determining the essential intervention elements is vital in order to inform the design, commissioning and delivery of more cost-effective measures to address alcohol-related harm (McCambridge, 2013). Thus there is a need for further research in the aforementioned areas where genuine knowledge gaps exist. Moreover, available research indicates that significant public health gains could be achieved if even the basic elements of brief alcohol intervention were mainstreamed in primary healthcare. Whilst acknowledging the inadequacy of the existing implementation evidence base, previous studies highlight the positive role of alcohol-specific, multi-component, and ideally, practitioner-tailored training programmes in routinising brief alcohol intervention delivery (Anderson et al., 2004; Nilsen et al., 2006). However, workload demands remain a fundamental barrier to mainstream adoption, irrespective of individual knowledge levels and attitudes (Johnson et al., 2010). On this basis, current research would suggest that time-pressed clinicians should focus on the following three ‘easy’ wins.
Short and simple is still effective
First, busy practitioners need to be reassured that there is little evidence to suggest that longer or more intensive input provides additional benefit over shorter, simpler input (Moyer et al., 2002; Kaner et al., 2007). Although one review found greater effect sizes associated with brief multi-contact interventions compared with other intensities (Jonas et al., 2012), overall, there appears no significant advantage of extended brief intervention in reducing alcohol consumption (Kaner et al., 2007, 2013). Even a single, 5-min session of structured brief advice on alcohol using a recognized, evidence-based resource based on FRAMES principles (Feedback, Responsibility, Advice, Menu, Empathy and Self-efficacy) is still likely to be effective.
Use the most active ingredients
Second, given the weak relationship between duration of counselling and outcome, it may be the case that the structure and content of brief interventions has more influence on patients' drinking than the total length of delivery (Kaner et al., 2009). Whilst there remains an identified knowledge gap around the most ‘active ingredients’ of brief alcohol intervention, one must acknowledge some important developments in this field in recent years, not as yet reflected in published systematic reviews. Mitchie et al. (2012) sought to identify which specific behaviour change techniques (BCTs) led to improved outcomes for brief alcohol interventions (42 BCTs reviewed in total, although not all associated with brief alcohol intervention). They concluded that prompting self-recording of alcohol intake was associated with greater effect sizes from brief intervention, and called for further research to extend and develop this approach. A systematic review by McCambridge and Kypri (2011) also found that answering questions on drinking, including consumption, in brief alcohol intervention trials appeared to alter subsequent self-reported behaviour in non-intervention control groups. On this basis, asking the simple question ‘how much do you drink?’ may be enough to trigger a positive behaviour change.
Target the ‘right’ patients
Finally, whilst there is a recognized need for further evidence on the effectiveness of brief alcohol intervention in certain groups of patients (pregnant women, younger and older drinkers), given the large number of trials showing consistently positive outcomes in middle-aged men, at the very least, practitioners should target their efforts in this direction. Indeed, as two-thirds of all alcohol-attributable deaths in the 20- to 64-year-old EU population occur in those aged 45–64, Rehm et al. (2011) have argued tackling harmful use in this age group would be most effective in helping to rapidly reduce alcohol's health burden to society overall.
There are several limitations associated with this review of reviews, including some inherent weaknesses with this methodological approach in general. First, although there is a range of published reviews on brief alcohol intervention effectiveness, some questions of interest were only partially addressed by the available evidence base. For example, there were limited data available on the effectiveness of brief alcohol intervention in different models of primary healthcare systems, beyond the broad comparison on geographic grounds. Second, in basing our conclusions on the findings of previous systematic reviews, this review is necessarily limited by individual authors' decisions regarding the exclusion/inclusion of particular studies, further confounded by the fact that the standard of reporting, analysis and interpretation, whilst generally high, varied across the included papers. Third, our reliance on previous systematic reviews limits the immediacy of our findings as the most recent primary research is not included. Whilst our discussion sought to supplement the findings with the results from more recent primary studies, this approach was unsystematic. Fourth, we did not verify the information reported in the reviews by consulting individual studies, which may have introduced bias (e.g. resulting from inaccurate reporting of findings (Smith et al., 2011)). However, the overlap in results, and broad agreement in responses to the questions posed by this review of reviews, suggests that our representation of the evidence is likely to limit potential bias.
CONCLUSION
Despite the limitations identified above, this paper illuminates some commonalities across the existing evidence base. There remain unanswered questions around the effectiveness of brief alcohol intervention across different settings, different population groups, about the optimum intervention content, and the longevity of intervention effects. However, available evidence suggests that time-pressed clinicians looking for maximum impact with minimal input should direct their efforts to the delivery of short, simple interventions which focus on prompting individuals to record their alcohol intake, and that these are likely to be most effective in middle-aged, male drinkers.
Supplementary material
Supplementary material is available at Alcohol and Alcoholism online.
Funding
This work was supported by the health programme of the European Union as part of the BISTAIRS research project (Agreement number 2011_1204). The sole responsibility lies with the author and the Executive Agency is not responsible for any use that may be made of the information contained therein. For further information, visit the project website at www.bistairs.eu. Funding to pay the Open Access publication charges for this article was provided by the Institute of Health & Society, Newcastle University, England.
Conflict of interest statement
None declared.
Supplementary Material
Acknowledgements
We thank Dr Ruth McGovern, Institute of Health and Society, for proofing this publication.
REFERENCES
- Aalto M, Pekuri P, Seppa K. Obstacles to carrying out brief intervention for heavy drinkers in primary health care: a focus group study. Drug Alcohol Rev. 2003;22:169–73. doi: 10.1080/09595230100100606. doi:10.1080/09595230100100606. [DOI] [PubMed] [Google Scholar]
- Aira M, Kauhanen J, Larivaara P, et al. Factors influencing inquiry about patients’ alcohol consumption by primary health care physicians: qualitative semi-structured interview study. Fam Pract. 2003;20:270–5. doi: 10.1093/fampra/cmg307. doi:10.1093/fampra/cmg307. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer M, Bernert S, et al. ESEMeD/MHEDEA 2000 Investigators. Use of mental health services in Europe: results from the European study of the Epidemiology of Mental Disorders (ESMeD) project. Acta Psychiatr Scand. 2004;109:47–54. doi: 10.1111/j.1600-0047.2004.00330.x. doi:10.1111/j.1600-0047.2004.00325.x. [DOI] [PubMed] [Google Scholar]
- Anderson P. Managing alcohol problems in general practice. Br Med J. 1985;290:1873–5. doi: 10.1136/bmj.290.6485.1873. doi:10.1136/bmj.290.6485.1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson P, Laurant M, Kaner E, et al. Engaging general practitioners in the management of hazardous and harmful alcohol consumption: results of a meta-analysis. J Stud Alcohol. 2004;65:191–9. doi: 10.15288/jsa.2004.65.191. [DOI] [PubMed] [Google Scholar]
- Anderson P, Chisholm D, Fuhr D. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. 2009;373:2234–46. doi: 10.1016/S0140-6736(09)60744-3. doi:10.1016/S0140-6736(09)60744-3. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle J. Alcohol screening and brief intervention: dissemination strategies for medical practice and public health. Addiction. 2000;95:677–86. doi: 10.1046/j.1360-0443.2000.9556773.x. doi:10.1046/j.1360-0443.2000.9556773.x. [DOI] [PubMed] [Google Scholar]
- Babor T, Kaner E, Nilsen P, et al. Rapid Review of Current Evidence for Health Promotion Actions for Hazardous and Harmful Alcohol Use, with Specific Reference to Low- and Middle-Income Countries: WHO Mainstreaming Health Promotion Project. Geneva: World Health Organization; 2013. in press. [Google Scholar]
- Ballesteros J, Gonzalez-Pinto A, Querejeta I, et al. Brief interventions for hazardous drinkers delivered in primary care are equally effective in men and women. Addiction. 2004a;99:103–8. doi: 10.1111/j.1360-0443.2004.00499.x. doi:10.1111/j.1360-0443.2004.00499.x. [DOI] [PubMed] [Google Scholar]
- Ballesteros JA, Duffy JC, Querejeta I, et al. Efficacy of brief interventions for hazardous drinkers in primary care: systematic review and meta-analysis. Alcohol Clin Exp Res. 2004b;28:608–18. doi: 10.1097/01.alc.0000122106.84718.67. doi:10.1097/01.ALC.0000122106.84718.67. [DOI] [PubMed] [Google Scholar]
- Beich A, Thorsen T, Rollnick S. Screening in brief intervention trials targeting excessive drinkers in general practice: systematic review and meta-analysis. Br Med J (Clin Res Ed) 2003;327:536–42. doi: 10.1136/bmj.327.7414.536. doi:10.1136/bmj.327.7414.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berglund M, Thelander S, Jonsson E. Treating alcohol and drug abuse: an evidence-based review. Alcohol Clin Exp Res. 2003;27:1645–56. doi: 10.1097/01.ALC.0000090144.99832.19. doi:10.1097/01.ALC.0000090144.99832.19. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Topp D, Shaw E, et al. A preliminary report of knowledge translation: lessons from taking screening and brief intervention techniques from the research setting into regional systems of care. Acad Emerg Med. 2009;16:1225–33. doi: 10.1111/j.1553-2712.2009.00516.x. doi:10.1111/j.1553-2712.2009.00516.x. [DOI] [PubMed] [Google Scholar]
- Bernstein J, Bernstein E, Heeren T. Mechanisms of change in control group drinking in clinical trials of brief alcohol intervention: implications for bias towards the null. Drug Alcohol Rev. 2010;29:498–507. doi: 10.1111/j.1465-3362.2010.00174.x. doi:10.1111/j.1465-3362.2010.00174.x. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Daeppen J-B, Wietlisbach V, et al. Brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–95. doi: 10.1001/archinte.165.9.986. doi:10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Bray JW, Cowell AJ, Hinde JM. A systematic review and meta-analysis of health care utilization outcomes in alcohol screening and brief intervention trials. Med Care. 2011;49:287–94. doi: 10.1097/MLR.0b013e318203624f. doi:10.1097/MLR.0b013e318203624f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang G. Brief interventions for problem drinking and women. J Subst Abuse Treat. 2002;23:1–7. doi: 10.1016/s0740-5472(02)00234-9. doi:10.1016/S0740-5472(02)00234-9. [DOI] [PubMed] [Google Scholar]
- CRD. Undertaking Systematic Reviews of Research on Effectiveness: CRD's Guidance for Those Carrying Out or Com-missioning Reviews. York: Centre for Reviews and Dissemination; 2001. [Google Scholar]
- Cuijpers P, Riper H, Lemmers L. The effects on mortality of brief interventions for problem drinking: a meta-analysis. Addiction. 2004;99:839–45. doi: 10.1111/j.1360-0443.2004.00778.x. doi:10.1111/j.1360-0443.2004.00778.x. [DOI] [PubMed] [Google Scholar]
- Dew K, Stubbe M, Macdonald L, et al. The (non) use of prioritisation protocols by surgeons. Sociol Health Illn. 2010;32:545–62. doi: 10.1111/j.1467-9566.2009.01229.x. doi:10.1111/j.1467-9566.2009.01229.x. [DOI] [PubMed] [Google Scholar]
- Egger M, Zellweger-Zähner T, Schneider M, et al. Language bias in randomised controlled trials published in English and German. Lancet. 1997;350:326–9. doi: 10.1016/S0140-6736(97)02419-7. doi:10.1016/S0140-6736(97)02419-7. [DOI] [PubMed] [Google Scholar]
- Flay B. Efficacy and effectiveness trials (and other phases of research) in the development of health promotion programs. Prev Med. 1986;14:451–74. doi: 10.1016/0091-7435(86)90024-1. doi:10.1016/0091-7435(86)90024-1. [DOI] [PubMed] [Google Scholar]
- Flay B, Biglan A, Boruch R, et al. Standards of Evidence: Criteria for Efficacy, Effectiveness and Dissemination. Falls Church, VA: Society for Prevention Research; 2004. [DOI] [PubMed] [Google Scholar]
- Flay B, Biglan A, Boruch R, et al. Standards of evidence: criteria for efficacy, effectiveness and dissemination. Prev Sci. 2005;6:151–75. doi: 10.1007/s11121-005-5553-y. doi:10.1007/s11121-005-5553-y. [DOI] [PubMed] [Google Scholar]
- Gartlehner G, Hansen R, Nissman D, et al. A simple and valid tool distinguished efficacy from effectiveness studies. J Clin Epidemiol. 2006;59:1040–8. doi: 10.1016/j.jclinepi.2006.01.011. doi:10.1016/j.jclinepi.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Gilinsky A, Swanson V, Power K. Interventions delivered during antenatal care to reduce alcohol consumption during pregnancy: A systematic review. Addict Res Theory. 2011;19:235–50. doi:10.3109/16066359.2010.507894. [Google Scholar]
- Gordon L, Graves N, Hawkes A, et al. A review of the cost-effectiveness of face-to-face behavioural interventions for smoking, physical activity, diet and alcohol. Chronic Illn. 2007;3:101–29. doi: 10.1177/1742395307081732. doi:10.1177/1742395307081732. [DOI] [PubMed] [Google Scholar]
- Gual A, Sabadini MdA. Implementing alcohol disorders treatment throughout the community. Curr Opin Psychiatry. 2011;24:203–7. doi: 10.1097/YCO.0b013e3283459256. doi:10.1097/YCO.0b013e3283459256. [DOI] [PubMed] [Google Scholar]
- Heather N. The public health and brief interventions for excessive alcohol consumption: the British experience. Addict Behav. 1996;21:857–68. doi: 10.1016/0306-4603(96)00040-8. doi:10.1016/0306-4603(96)00040-8. [DOI] [PubMed] [Google Scholar]
- HoC Health Committee. Alcohol: First Report of Session 2009–10. London: The Stationery Office; 2010. [Google Scholar]
- Huibers M, Beurskens A, Bleijenberg G, et al. The Effectiveness of Psychosocial Interventions Delivered by General Practitioners. London: Cochrane database of systematic reviews; 2003. [DOI] [PubMed] [Google Scholar]
- Hutubessy R, Chisholm D, Edejer T. Generalised Cost-Effectiveness Analysis for National-Level Priority Setting in the Health Sector. Cost Effectiveness and Resource Allocation. Geneva: World Health Organisation; 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson R, Johnson M, Campbell F, et al. Screening and Brief Interventions for Prevention and Early Identification of Alcohol Use Disorders in Adults and Young People. Sheffield: University of Sheffield, School of Health and Related Research (ScHARR) Public Health Collaborating Centre; 2010. [Google Scholar]
- Jenkins RJ, McAlaney J, McCambridge J. Change over time in alcohol consumption in control groups in brief intervention studies: systematic review and meta-regression study. Drug Alcohol Depend. 2009;100:107–14. doi: 10.1016/j.drugalcdep.2008.09.016. doi:10.1016/j.drugalcdep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- Johnson M, Jackson R, Guillaume L, et al. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: a systematic review of qualitative evidence. J Public health Res. 2010;33:412–21. doi: 10.1093/pubmed/fdq095. [DOI] [PubMed] [Google Scholar]
- Jonas D, Garbutt J, Brown J, et al. Screening, Behavioral Counseling, and Referral in Primary Care to Reduce Alcohol Misuse. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [PubMed] [Google Scholar]
- Kaner E. Brief alcohol intervention: time for translational research. Addiction. 2010a;105:960–1. doi: 10.1111/j.1360-0443.2009.02848.x. doi:10.1111/j.1360-0443.2009.02848.x. [DOI] [PubMed] [Google Scholar]
- Kaner E. NICE work if you can get it: development of national guidance incorporating screening and brief intervention to prevent hazardous and harmful drinking in England. Drug Alcohol Rev. 2010b;29:589–95. doi: 10.1111/j.1465-3362.2010.00236.x. doi:10.1111/j.1465-3362.2010.00236.x. [DOI] [PubMed] [Google Scholar]
- Kaner E, Heather N, McAvoy B, et al. Intervention for excessive alcohol consumption in primary health care: attitudes and practices of English general practitioners. Alcohol Alcohol. 1999;34:559–66. doi: 10.1093/alcalc/34.4.559. doi:10.1093/alcalc/34.4.559. [DOI] [PubMed] [Google Scholar]
- Kaner E, Beyer F, Dickinson H, et al. Effectiveness of Brief Alcohol Interventions in Primary Care Populations. London: Cochrane Database of Systematic Reviews; 2007. [DOI] [PubMed] [Google Scholar]
- Kaner E, Dickinson H, Beyer F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28:301–23. doi: 10.1111/j.1465-3362.2009.00071.x. doi:10.1111/j.1465-3362.2009.00071.x. [DOI] [PubMed] [Google Scholar]
- Kaner E, Bland M, Cassidy P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. Br Med J. 2013;346:1–14. doi: 10.1136/bmj.e8501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kung J, Chiappelli F, Cajulis O, et al. From systematic reviews to clinical recommendations for evidence-based health care: validation of revised assessment of multiple systematic reviews (R-AMSTAR) for grading of clinical relevance. Open Dent J. 2010;4:84–91. doi: 10.2174/1874210601004020084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latimer N, Guillaume L, Goyder E, et al. Prevention and Early Identification of Alcohol Use Disorders in Adults and Young People: Screening and Brief Interventions, Cost Effectiveness Review. Sheffield: University of Sheffield, School of Health and Related Research (ScHARR) Public Health Collaborating Centre; 2010. [Google Scholar]
- Littlejohn C. Does socio-economic status influence the acceptability of, attendance for, and outcome of, screening and brief interventions for alcohol misuse: a review. Alcohol Alcohol. 2006;41:540–5. doi: 10.1093/alcalc/agl053. doi:10.1093/alcalc/agl053. [DOI] [PubMed] [Google Scholar]
- Lock C. Screening and brief alcohol interventions: what, why, who, where and when? A review of the literature. J Subst Abuse. 2004;9:91–101. [Google Scholar]
- Lock C, Wilson G, Kaner E, et al. A Survey of General Practitioners’ Knowledge, Attitudes and Practices Regarding the Prevention and Management of Alcohol-Related Problems: An Update of a World Health Organisation Survey Ten Years on. London: Alcohol Education and Research Council; 2009. [Google Scholar]
- McCambridge J. Brief intervention content matters. Drug Alcohol Rev. 2013;32:339–41. doi: 10.1111/dar.12044. doi:10.1111/dar.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCambridge J, Kypri K. Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLoS One. 2011;6:23748. doi: 10.1371/journal.pone.0023748. doi:10.1371/journal.pone.0023748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchie S, Whittington C, Hamoudi Z, et al. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction. 2012;107:1431–40. doi: 10.1111/j.1360-0443.2012.03845.x. doi:10.1111/j.1360-0443.2012.03845.x. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:1–4. doi: 10.7326/0003-4819-151-4-200908180-00135. doi:10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Moriarty H, Stubbe M, Chen L, et al. Challenges to alcohol and other drug discussions in the general practice consultation. Fam Pract. 2012;29:213–22. doi: 10.1093/fampra/cmr082. doi:10.1093/fampra/cmr082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, et al. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–92. doi: 10.1046/j.1360-0443.2002.00018.x. doi:10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Nilsen P, Aalto M, Bendtsen P, et al. Effectiveness of strategies to implement brief alcohol intervention in primary healthcare: a systematic review. Scand J Prim Health. 2006;24:5–15. doi: 10.1080/02813430500475282. doi:10.1080/02813430500475282. [DOI] [PubMed] [Google Scholar]
- Parkes T, Poole N, Salmon A, et al. Double Exposure: A Better Practices Review on Alcohol Interventions during Pregnancy. Vancouver: British Columbia Centre of Excellence for Women's Health; 2008. [Google Scholar]
- Peltzer K. Brief intervention of alcohol problems in Sub-Saharan Africa: a review. J Psychol Africa. 2009;19:415–22. [Google Scholar]
- Purshouse R, Brennan A, Rafia R, et al. Modelling the cost-effectiveness of alcohol screening and brief interventions in primary care in England. Alcohol Alcohol. 2013;48:180–8. doi: 10.1093/alcalc/ags103. doi:10.1093/alcalc/ags103. [DOI] [PubMed] [Google Scholar]
- Raistrick D, Heather N, Godfrey C. Review of the Effectiveness of Treatment for Alcohol Problems. London: NHS: National Treatment Agency for Substance Misuse; 2006. [Google Scholar]
- Rehm J, Roerecke M. Reduction of drinking in problem drinkers and all-cause mortality. Alcohol Alcohol. 2013;48:509–13. doi: 10.1093/alcalc/agt021. doi:10.1093/alcalc/agt021. [DOI] [PubMed] [Google Scholar]
- Rehm J, Zatonksi W, Taylor B, et al. Epidemiology and alcohol policy in Europe. Addiction. 2011;106:11–9. doi: 10.1111/j.1360-0443.2010.03326.x. doi:10.1111/j.1360-0443.2010.03326.x. [DOI] [PubMed] [Google Scholar]
- Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependance or very heavy drinking. Drug Alcohol Rev. 2010;29:631–40. doi: 10.1111/j.1465-3362.2010.00217.x. doi:10.1111/j.1465-3362.2010.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith V, Devane D, Begley C, et al. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11:1–6. doi: 10.1186/1471-2288-11-15. doi:10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: ranking its health impact and cost effectiveness. Am J Prev Med. 2008;34:143–52. doi: 10.1016/j.amepre.2007.09.035. doi:10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- Sullivan L, Tetrault J, Braithwaite S, et al. A meta-analysis of the efficacy of nonphysician brief interventions for unhealthy alcohol use: implications for the patient-centered medical home. Am J Addiction. 2011;20:343–56. doi: 10.1111/j.1521-0391.2011.00143.x. doi:10.1111/j.1521-0391.2011.00143.x. [DOI] [PubMed] [Google Scholar]
- Thorpe K, Zwarenstein M, Oxman A, et al. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol. 2009;62:464–75. doi: 10.1016/j.jclinepi.2008.12.011. doi:10.1016/j.jclinepi.2008.12.011. [DOI] [PubMed] [Google Scholar]
- Whitlock EP, Polen MR, Green CA, et al. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:557–68. doi: 10.7326/0003-4819-140-7-200404060-00017. doi:10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Wilson G, Lock C, Heather N, et al. Intervention against excessive alcohol consumption in primary health care: a survey of GPs’ attitudes and practices in England ten years on. Alcohol Alcohol. 2011;46:570–7. doi: 10.1093/alcalc/agr067. doi:10.1093/alcalc/agr067. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.