Abstract
Objectives
To determine the association of alcohol consumption and cardiovascular mortality in the U.S. population.
Background
Alcohol consumption has been associated with a lower risk of cardiovascular disease in cohort studies, but this association has not been prospectively examined in large, detailed, representative samples of the U.S. population.
Methods
We analyzed nine iterations of the National Health Interview Survey, an annual survey of a nationally representative sample of U.S. adults between 1987 and 2000. Exposures of interest included usual volume, frequency, and quantity of alcohol consumption and binge drinking. Mortality was ascertained through linkage to the National Death Index through 2002. Relative risks were derived from random-effects meta-analyses of weighted, multivariable-adjusted hazard ratios for cardiovascular mortality from nine survey administrations.
Results
Light and moderate volumes of alcohol consumption were inversely associated with cardiovascular mortality. Compared with lifetime abstainers, summary relative risks were 0.95 (95% confidence interval [CI], 0.88–1.02) among lifetime infrequent drinkers, 1.02 (95% CI, 0.94–1.11) among former drinkers, 0.69 (95% CI, 0.59–0.82) among light drinkers, 0.62 (95% CI, 0.50–0.77) among moderate drinkers, and 0.95 (95% CI, 0.82–1.10) among heavy drinkers. The magnitude of lower risk was similar in subgroups of sex, age, or baseline health status. There was no simple relation of drinking pattern with risk, but risk was consistently higher among those who consumed ≥3 compared to 2 drinks per drinking day.
Conclusions
In nine nationally representative samples of US adults, light and moderate alcohol consumption were inversely associated with CVD mortality, even when compared with lifetime abstainers, but consumption above recommended limits was not.
Introduction
Alcohol consumption has been consistently associated with a lower risk of cardiovascular disease (CVD) in epidemiological studies (1,2), an association attributed in great part to the increase in high-density lipoprotein cholesterol (HDL-C) caused by alcohol consumption (3).
However, a number of uncertainties about the association of alcohol consumption and CVD remain, punctuated by the absence of a long-term randomized controlled trial on CVD events with which to confirm the results of observational studies. These uncertainties include potentially diverse effects on coronary heart disease (CHD) and stroke (4), inclusion of former or occasional drinkers with long-term abstainers as a referent category (5), generalizability to the adult U.S. population (6), and the importance of drinking patterns in modifying the association (7). Measures of overall volume of alcohol consumption obscure the relative contributions of drinking frequency (how often alcohol is consumed), drinking quantity (how much alcohol is typically consumed on those days), and binge drinking (episodes of 5 or more drinks in a day), and their individual contributions to CVD risk have not been thoroughly investigated.
To evaluate the associations of alcohol consumption and drinking patterns with CVD, cerebrovascular, and CHD mortality in a nationally representative sample of U.S. adults, we aggregated data from nine administrations of the National Health Interview Survey (NHIS). The NHIS is an annual in-person survey conducted by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention and has included detailed questions on alcohol consumption on selected surveys since 1987.
Methods
Study Sample
Since 1957, the NCHS has conducted annual cross-sectional household interview surveys of the noninstitutionalized civilian U.S. population. NHIS data are collected during a personal household interview conducted by interviewers employed and trained by the U.S. Bureau of the Census. The sampling plan follows a multistage area probability design, with oversampling of selected minority populations, including both black and Hispanic persons. Survey participation is voluntary, and the confidentiality of responses is assured by the Public Health Service Act.
The content of the survey is updated approximately every 10–15 years and has remained relatively unchanged since 1997. The NHIS questionnaire from 1982–1996 included a core set of basic health and demographic items and one or more added sets of questions on diverse health topics, but did not consistently include questions about health-related behaviors, such as alcohol consumption. Since 1997, the NHIS questionnaire has similar core questions that include demographic information, health status and limitations, health insurance, income and assets, and diverse health behaviors.
Our study used data from NHIS years that included alcohol consumption data (1987–1988, 1990–1992, and 1997–2000). Response rates for alcohol-related modules for adults included in these NHIS years range from 70% in 1999 to 87% in 1988. All NHIS data are publicly available (http://www.cdc.gov/nchs/about/major/nhis/quest_data_related_doc.htm).
Alcohol Consumption
As noted, alcohol consumption was ascertained variably in the NHIS. Table 1 summarizes the methods used. In 1987 and 1992, a validated food frequency questionnaire (8) was administered that included separate quantity-frequency items for beer, wine, and liquor. In 1988 and 1997–2000, alcohol-related items included 1) intake of 12 or more drinks in one’s lifetime, in any previous year, and in the past year, and 2) drinking frequency, drinking quantity, and binge drinking in the past year. In 1990, similar questions were asked but with a time frame of the last two weeks for current drinking; only individuals who reported that those two weeks were typical for consumption in the past year were included in these analyses. Quantity-frequency questions were also administered in 1991 as part of a Drug and Alcohol Use module to adults aged 18–44 years, although intake in any previous year was not queried. Binge drinking was ascertained in 1988, 1991, and 1997–2000.
Table 1.
Alcohol-related variables assessed in nine administrations of the NHIS.
| Year | N | CVD Deaths | How Assessed | Time Frame | Participants | Former Drinking | Binge Drinking | Adult Response Rate |
|---|---|---|---|---|---|---|---|---|
| 1987 | 21396 | 1865 | FFQ | Past year | All | No | No | 86% |
| 1988 | 42144 | 3478 | QF | Past year | All | Yes | Yes | 87% |
| 1990 | 29527 | 2352 | QF | Past 2 weeks1 | All | Yes | No | 83% |
| 1991 | 19956 | 85 | QF | Past year | Age 18–44 years | Yes2 | Yes | 75% |
| 1992 | 11076 | 631 | FFQ | Past year | All | No | No | 86% |
| 19973 | 33477 | 888 | QF | Past year | All | Yes | Yes | 80% |
| 1998 | 29761 | 639 | QF | Past year | All | Yes | Yes | 74% |
| 1999 | 28206 | 427 | QF | Past year | All | Yes | Yes | 70% |
| 2000 | 29664 | 305 | QF | Past year | All | Yes | Yes | 72% |
Only individuals who reported that their use in the past 2 weeks was typical of their use in the past year were included in these analyses.
Former and lifetime infrequent drinking were combined in 1991.
The NHIS administered a similar questionnaire from 1997 through 2000.
From these questions, we derived six alcohol consumption categories. Current abstainers were categorized as never drinkers (<12 drinks in one’s lifetime), lifetime infrequent drinkers (>12 in one’s lifetime, <12 drinks in any previous year), and former drinkers (>12 in one’s lifetime, >12 drinks in a previous year). Current drinkers were categorized as light (current use of ≤3 drinks per week), moderate (current use of >3–7 drinks per week for women and >3–14 drinks per week for men), and heavy (current use of >7 drinks per week for women and >14 drinks per week for men). In 1987 and 1992, the three abstainer categories could not be differentiated and were combined. In 1991, former and lifetime infrequent drinkers were combined but could be distinguished from never drinkers.
Mortality Ascertainment
In 2004, the NCHS conducted an updated linkage of the NHIS to death certificate data found in the National Death Index (NDI). Linked mortality files include NHIS surveys from 1986 to 2000 with mortality follow-up from the month of interview through December 31, 2002. Mortality information is based upon the results from a probabilistic match between NHIS and NDI death certificate records (9). All NHIS participants 18 years and older were eligible for mortality follow-up. To minimize potential breaches of confidentiality, the NCHS developed a minor data perturbation plan; empirical studies suggest that the original and perturbed data files yield very similar descriptive statistics and model-based associations with mortality (10).
Deaths were coded for underlying cause using NCHS bridge codes spanning the Ninth and Tenth Revisions of the International Classification of Diseases (ICD-9, years 1979 to 1998; ICD-10, years 1999 to present) (11). We separately examined cardiovascular mortality (bridge codes 053 and 075, corresponding to ICD-10 I00–I99), CHD mortality (bridge code 058, ICD-10 I20–I25), and cerebrovascular mortality (bridge code 070, ICD-10 I60–I69).
Covariates
We included a core set of covariates available in all NHIS surveys that also assessed alcohol consumption. We categorized self-reported race/ethnicity as non-Hispanic white, non-Hispanic black, Hispanic, and other. We grouped educational attainment as less than high school, high school, and some college, and marital status as married or non-married. We categorized region of residence in four U.S. Census regions (Northeast, South, Midwest, and West). Urbanization was categorized as residence in a U.S. census-defined metropolitan statistical area (MSA) with a population of 1 million or more, a population of less than 1 million, or outside of a defined MSA. Smoking status was defined in five categories: never smokers, former smokers, and tertiles of intensity among current smokers. We calculated body-mass index (BMI) based upon self-reported height and weight and used standard World Health Organization categories of underweight, normal weight, overweight, and obese. Self-reported general health status was categorized as excellent, very good, good, and fair/poor/unknown.
NCHS queried physical activity and diet only in selected NHIS administrations. Leisure-time physical activity was assessed with a series of items on specific activities in 1990 and 1991 (12,13) and general items about moderate and heavy physical exertion in 1997–2000 (14); to combine these, activity was categorized in quartiles. Diet was assessed with a food-frequency questionnaire in 1987 and 1992. As previously described (15), we used foods grouped as fruits and vegetables, meat/poultry/fish, dairy products, added fats, and desserts, all categorized in tertiles.
Statistical Analysis
We performed separate, similar analyses of alcohol consumption and mortality for each NHIS survey year using Cox proportional hazards regression, using appropriate sample weights provided by the NCHS. We set age as the metameter (16) and adjusted for sex and race in initial models, and additionally for marital status, education, region, urbanization, smoking, BMI, and general health status in multivariable models.
From the hazards ratios estimated in individual Cox proportional hazards models, we derived summary estimates of relative risk using random effects meta-analysis to combine across survey years (17,18). Because each survey provides estimates for the same underlying population (the non-institutionalized adult population of the U.S.), we also performed pooled analyses in sensitivity analyses.
For primary analyses, we set never drinkers as a referent; because this excluded data from 1987 and 1992, we included these years in additional analyses with all non-drinkers as a referent only after comparing the risk associated with former and lifetime infrequent drinking. We tested several domains of alcohol consumption, including average volume of intake, frequency and quantity of intake, and binge drinking.
We performed sensitivity analyses with additional adjustment for diet or physical activity where such data were available, with exclusion of individuals who died within the first two years (i.e., a two-year lag), and restricted to five years of follow-up for each survey (to reduce misclassification over longer follow-up). We performed prespecified analyses stratified by sex, age (<55 versus 55 and older), race (white versus non-white), and general health (excellent versus other); to maximize precision, we used all available NHIS years in stratified analyses. Given the possibility that low folate intake attenuates the lower risk of CHD associated with alcohol intake (19), we also examined risk stratified by follow-up that occurred prior and subsequent to the initiation of folate fortification in the U.S. in 1998 (20).
Results
A total of 245,207 participants were included in the nine iterations of the NHIS included in these analyses (Table 1), generally ranging from 20,000–40,000 participants per year. There were a total of 10,670 cardiovascular deaths during 1,987,439 person-years of follow-up, including 6,135 related to CHD and 1,758 to stroke. Baseline characteristics according to alcohol consumption in the pooled sample are shown in the Supplementary Tables.
Average Volume of Alcohol Consumption
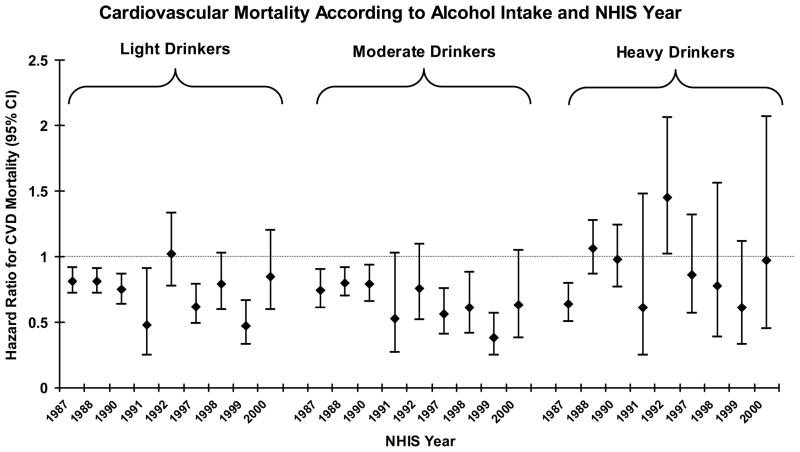
Figure 1 shows adjusted hazard ratios for CVD mortality according to light, moderate, and heavy drinking at baseline in the individual NHIS surveys. In general, light and moderate drinking were associated with lower risk than abstention, with somewhat lower risk estimates for moderate drinking, while heavy drinking was not clearly associated with higher or lower risk.
Figure 1.
Cardiovascular mortality according to alcohol intake and NHIS year. Adjusted hazard ratios are shown relative to abstainers from alcohol. T-bars indicate 95% confidence intervals.
Table 2 shows summary hazard ratios for CVD mortality according to alcohol intake across seven NHIS years with information on lifetime drinking habits. Risk tended to be similar among never drinkers and lifetime infrequent drinkers. A modestly higher risk was observed among former drinkers only in initial analyses and was eliminated by multivariable adjustment. In contrast, multivariable adjustment had relatively little effect upon risk estimates among current drinkers. There was no higher adjusted risk among former drinkers than never drinkers for CHD mortality (adjusted hazard ratio 1.00; 95% CI, 0.89–1.11) or cerebrovascular mortality (adjusted hazard ratio 1.06; 95% CI, 0.86–1.33).
Table 2.
Adjusted summary hazard ratios (and 95% confidence intervals) for cardiovascular mortality among NHIS participants in 1988, 1990, 1991, and 1997–2000, according to baseline volume of alcohol consumption.
| Volume of Alcohol Consumption
|
||||||
|---|---|---|---|---|---|---|
| Never Drinker | Lifelong Infrequent Drinker | Former Drinker | Light | Moderate | Heavy | |
| CVD Deaths1 | 2754 | 1538 | 1700 | 1131 | 697 | 354 |
| Person-Years | 305966 | 242849 | 174714 | 520562 | 238498 | 94815 |
| Age-Sex-Race Adj. | 1.00 | 0.98 (0.91–1.05) | 1.15 (1.06–1.24) | 0.66 (0.56–0.77) | 0.58 (0.47–0.72) | 1.07 (0.94–1.22) |
| Multivariable Adj.2 | 1.00 | 0.95 (0.88–1.02) | 1.02 (0.94–1.11) | 0.69 (0.59–0.82) | 0.62 (0.50–0.77) | 0.95 (0.82–1.10) |
| MV+Activity3 | 1.00 | 0.96 (0.89–1.03) | 1.02 (0.94–1.11) | 0.71 (0.61–0.83) | 0.65 (0.53–0.79) | 0.96 (0.83–1.11) |
| Pooled MV HR4 | 1.00 | 0.96 (0.89–1.03) | 1.02 (0.94–1.10) | 0.71 (0.65–0.78) | 0.70 (0.63–0.78) | 0.95 (0.82–1.10) |
| Two-Year Lag5 | 1.00 | 0.96 (0.89–1.04) | 1.03 (0.94–1.13) | 0.72 (0.62–0.84) | 0.74 (0.63–0.86) | 1.04 (0.90–1.21) |
Hazard ratios derive from random-effects meta-analyses of NHIS years 1988, 1990, 1991, and 1997–2000; 1987 and 1992 did not include information with which to identify former drinkers.
Multivariable-adjusted hazard ratios adjusted for age, sex, race, smoking, marital status, education, region, urbanization, smoking, BMI, and general health status.
Analyses adjusted for covariates in multivariable models and physical activity assessed in 1990, 1991, and 1997–2000.
Hazard ratios derive from pooled (rather than meta-analyzed) analyses of individual NHIS administrations.
Lagged analyses exclude individuals who died within the first two years after administration of the respective NHIS.
Table 3 shows the association of average alcohol intake with CVD, coronary, and stroke mortality across all NHIS years, both overall and in prespecified subgroups. In general, the association of light and especially moderate drinking with lower risk was observed to similar degrees across all subgroups, although estimates tended to be further below 1 for coronary than stroke mortality, particularly for heavy drinking. Light and moderate drinking were also inversely associated with cardiovascular deaths not coded as ischemic and cerebrovascular, with hazard ratios of 0.73 (95% CI, 0.64–0.83) and 0.71 (95% CI, 0.59–0.85), respectively.
Table 3.
Adjusted summary hazard ratios (and 95% confidence intervals) for cardiovascular, coronary heart disease, and stroke mortality among NHIS participants in 1987, 1988, 1990–1992, and 1997–2000, according to baseline volume of alcohol consumption.
| Volume of Alcohol Consumption
|
||||
|---|---|---|---|---|
| Non-Drinkers | Light | Moderate | Heavy | |
|
| ||||
| Cardiovascular Deaths | 7400 | 1804 | 936 | 530 |
| Person-Years | 856659 | 677069 | 310062 | 143649 |
| Multivariable Adjusted1 | 1.00 | 0.76 (0.68–0.85) | 0.67 (0.59–0.77) | 0.89 (0.73–1.10) |
| Multivariable +Activity/Diet2 | 1.00 | 0.77 (0.69–0.85) | 0.69 (0.61–0.80) | 0.90 (0.73–1.10) |
| 5-Year Follow-Up3 | 1.00 | 0.71 (0.60–0.84) | 0.65 (0.55–0.77) | 0.83 (0.66–1.04) |
| Men | 1.00 | 0.78 (0.69–0.90) | 0.70 (0.61–0.81) | 0.95 (0.76–1.19) |
| Women | 1.00 | 0.74 (0.66–0.83) | 0.70 (0.60–0.81) | 0.88 (0.72–1.07) |
| White | 1.00 | 0.75 (0.68–0.84) | 0.67 (0.58–0.78) | 0.90 (0.73–1.10) |
| Not White | 1.00 | 0.80 (0.65–0.99) | 0.76 (0.61–0.94) | 0.92 (0.70–1.21) |
| Age <55 Years | 1.00 | 0.76 (0.60–0.97) | 0.62 (0.45–0.86) | 0.91 (0.60–1.40) |
| Age ≥55 Years | 1.00 | 0.77 (0.69–0.86) | 0.71 (0.63–0.80) | 0.89 (0.76–1.06) |
| Excellent Health | 1.00 | 0.70 (0.56–0.88) | 0.69 (0.57–0.83) | 0.92 (0.66–1.28) |
| Not Excellent Health | 1.00 | 0.72 (0.64–0.80) | 0.61 (0.52–0.72) | 0.82 (0.65–1.03) |
|
| ||||
| Coronary Heart Disease Deaths | 4217 | 1057 | 553 | 308 |
| Coronary Mortality | 1.00 | 0.75 (0.66–0.84) | 0.67 (0.57–0.79) | 0.80 (0.61–1.05) |
| Stroke Deaths | 1241 | 288 | 135 | 94 |
| Stroke Mortality | 1.00 | 0.80 (0.61–1.05) | 0.76 (0.58–0.99) | 1.25 (0.92–1.70) |
Multivariable-adjusted hazard ratios adjusted for age, sex, race, smoking, marital status, education, region, urbanization, smoking, BMI, and general health status.
Analyses adjusted for coviarates in multivariable models, physical activity assessed in 1990, 1991, and 1997–2000, and diet assessed in 1987 and 1992.
Truncated analyses limited follow-up to five years following administration of the respective NHIS.
Hazard ratios tended to be numerically closer to 1 among minority populations, although light and moderate drinking were associated with significantly lower risk even among minority participants. This contrast was more pronounced for CHD mortality, as light and moderate drinking were associated with summary hazard ratios of 0.74 (95% CI, 0.67–0.82) and 0.66 (95% CI, 0.55–0.78), respectively, among non-Hispanic whites; the corresponding hazard ratios among members of minority populations were 0.85 (95% CI, 0.67–1.08) and 0.79 (95% CI, 0.56–1.10).
We performed several sensitivity analyses to test our findings (Table 2). Additional adjustment for physical activity and diet altered the observed summary estimates to a minimal degree. When a two-year lag was incorporated to eliminate early deaths, the observed hazard ratios were attenuated but remained statistically significant for light and moderate drinking. In contrast, restriction to five years of follow-up for each survey administration to minimize misclassification of alcohol intake over time tended to increase the lower risk associated with alcohol intake. Pooled analyses yielded roughly similar estimates, albeit with substantially tighter confidence intervals. In general, we found no material differences in CVD mortality associated with light or moderate drinking in analyses stratified by follow-up prior or subsequent to folate fortification in the U.S. (data not shown).
Frequency and Quantity of Alcohol Consumption
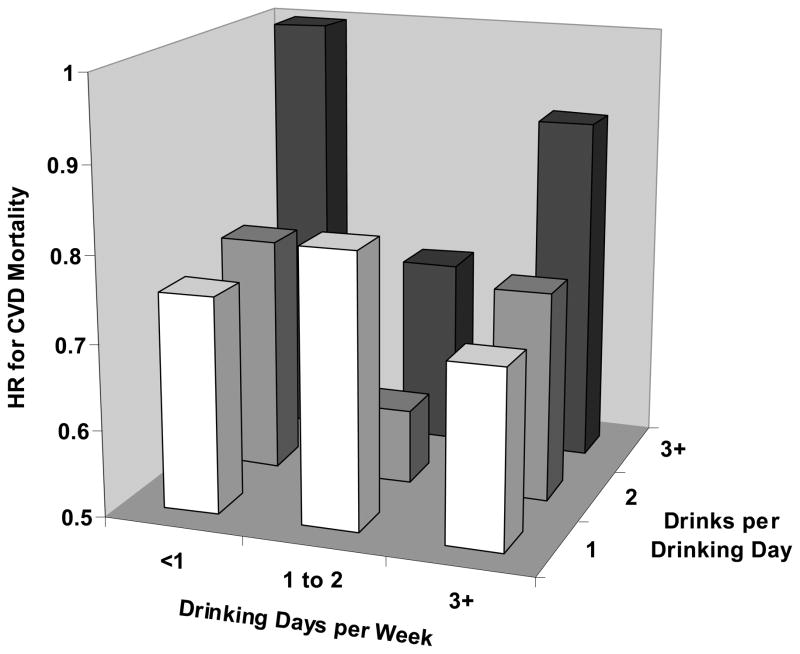
Figure 2 demonstrates the joint associations of drinking frequency and quantity with cardiovascular mortality compared with abstainers. There was not a simple clear pattern, although risk was consistently higher among those who consumed ≥3 compared to 2 drinks per drinking day. There was no consistent association of drinking frequency with risk. These general findings were similar in analyses of CHD rather than CVD mortality and among both men and women.
Figure 2.
Cardiovascular mortality according to quantity and frequency of alcohol consumption. Adjusted summary hazard ratios are shown relative to abstainers from alcohol.
Binge Drinking
There was little overall association of binge drinking with CVD mortality. In analyses of NHIS years 1988, 1991, and 1997–2000, the multivariable-adjusted hazard ratios for CVD mortality (compared with long-term abstainers) were 0.65 (95% CI, 0.51–0.81) among drinkers who reported no binge drinking, 0.66 (95% CI, 0.46–0.95) among those who endorsed binge drinking <1 day per week, and 0.68 (95% CI, 0.44–1.06) among those who reported binge drinking ≥1 day per week, consistent with the lower overall risk associated with drinking.
After taking usual drinking habits into account, we found limited evidence that binge drinking might attenuate the lower risk of CHD mortality associated with light and moderate drinking among women. For example, among women who did not report binge drinking, light and moderate drinking together were associated with a summary hazard ratio for CHD mortality of 0.56 (95% CI, 0.41–0.76), compared with long-term abstention; the corresponding hazard ratio among binge drinkers was 1.23 (95% CI, 0.42–3.61). However, relatively few women reported binge drinking, and the difference in risk between light/moderate drinkers according to binge drinking was not significant (p=0.17). Power was even more limited to assess the risk of binge drinking specifically associated with stroke mortality.
Discussion
In this analysis of nine nationally-representative samples of the U.S. population, comprising over 10,000 cardiovascular deaths, light and moderate alcohol consumption was associated with lower cardiovascular mortality, while heavy alcohol consumption was not.
Great interest remains in whether the previously observed relationships of alcohol consumption with lower rates of CVD or mortality are biased by choice of referent category (21,22). Because former drinkers may have ceased drinking for health-related reasons, they have typically been found to have higher rates of mortality in previous studies (23,24), although studies of CVD have not always demonstrated this increase in risk (25). Even less clear is the appropriate treatment of rare drinkers, as critics have variously suggested that they be fully excluded from the referent category of long-term abstainers (5) or replace abstainers as the referent (26). Our data demonstrate that, at least for CVD mortality, risk is similar among lifelong abstainers, lifelong rare drinkers, and former drinkers, and thus that the inverse associations of light and moderate drinking with risk of CVD mortality are robust with respect to the choice of referent category.
Existing data on alcohol use and CVD derive nearly exclusively from studies of limited generalizability to the full U.S. population, although some may be representative of specific U.S. communities (27,28). As a result, our results provide some of the strongest evidence to date that the observed associations can be generalized to the U.S. population, and are not limited to intensively-monitored cohorts of volunteers. However, the NHIS excludes institutionalized individuals, who are likely to include the frailest members of society for whom even limited alcohol consumption could be detrimental.
Our results also provide insight into the consistency of the association of alcohol consumption and risk of CVD across subgroups. In general, light and moderate alcohol consumption were associated similarly with lower risk of CVD in nearly all segments of the U.S. population, including those who report themselves to be in excellent health (in whom the likelihood of residual confounding seems smallest (29)). One relative exception to this finding was race/ethnicity, where the association appeared stronger among non-Hispanic whites. Limited data suggest the apparent U- or J-shaped associations of alcohol consumption with CVD and mortality observed in other groups may not extend to African-Americans, who comprise the largest minority population in these surveys (30,31). Interestingly, alcohol consumption was associated with a numerically higher risk of MI among black Africans but a lower risk among white and mixed-race Africans in the INTERHEART Africa study (32), suggesting that findings among African-Americans may reflect known ancestral variation in alcohol dehydrogenase 1B isoforms or other alcohol-metabolizing enzymes (33). Prospective studies of alcohol consumption and CVD in minority populations are needed to clarify this issue.
The association of alcohol consumption with risk of CHD mortality tended to be stronger than that for cerebrovascular mortality in our analyses. This observation mirrors that observed for incident CVD in several other cohorts, where the associations of alcohol intake with CHD (27,34,35) have been stronger and more linear than the corresponding associations even with ischemic stroke (36–38). In part, this may reflect the particularly strong contributions of hypertension and atrial fibrillation as risk factors for ischemic stroke, both of which are positively associated with at least heavy drinking (39,40). In the NHIS, the weaker association with cerebrovascular mortality likely also reflects some contribution of hemorrhagic stroke, which tends to be positively associated with alcohol consumption (41), perhaps related to the antiplatelet activity of alcohol (42).
Important limitations of our study warrant discussion. As with any observational study, our results may be confounded by factors for which we did not fully adjust, although the range of covariates available in the NHIS is relatively broad. Any unadjusted or incompletely unadjusted factor would need to be associated with both alcohol consumption and CVD and not strongly associated with the covariates already included in our models. Previous work in the Behavioral Risk Factor Surveillance System, another nationally representative survey, suggests that adjustment for race and education – which were included in these analyses – may be particularly important in reducing residual confounding (43).
The assessment of alcohol consumption in the NHIS occurred at a single point in time. This may have led us to underestimate the strength of associations for which alcohol consumption has acute effects on risk, although alcohol consumption is a relatively stable behavior among light- and moderate-drinking adults in the U.S. (44). It is most likely to have weakened associations of CVD with drinking frequency, where the presumed mechanisms of action include short-term, completely reversible effects on factors like thrombotic potential.
Although all data were collected prospectively using standardized, well-recognized instruments, the NHIS does not include measurement of biological factors that could be used to validate self-reported alcohol consumption (e.g., HDL-C (45)) or examine potential pathways that mediate the observed relationship (e.g., adiponectin (46)). Information on individual beverage types was also not uniformly collected, although most evidence suggests that wine, beer, and spirits are similar in their relationships with HDL-C(47) and with risk of CVD (48).
Despite the large overall sample size of our analyses, we were nonetheless limited in power in some cases, such as when stratifying participants by binge drinking and usual drinking habits simultaneously. In part, this reflects the relative rarity of binge drinking among otherwise light drinking women, but it nonetheless limits our ability to estimate the risk associated with binge drinking with precision. Similarly, power was insufficient to examine ischemic and hemorrhagic strokes separately; the overall association observed here likely reflects lower risk of more common ischemic strokes and higher risk of hemorrhagic strokes. (49)
The NHIS obtains mortality data from the National Death Index, which derives cause-of-death information from state vital statistics offices and ultimately from death certificates. Although this methodology matches formal nosologist evaluations reasonably well (50), death certificates are nonetheless prone to misclassify CVD as a cause of death (51). Because this type of misclassification is likely random with respect to alcohol consumption, the true strength of the associations we evaluated is apt to be greater than that observed.
In summary, in aggregate analyses of nine nationally representative surveys of the U.S. population conducted between 1987 and 2000, light and moderate alcohol consumption were inversely associated with cardiovascular mortality, with little difference in risk among lifelong abstainers, lifelong rare drinkers, and former drinkers. The magnitude of lower risk was generally strongest for CHD mortality and among non-Hispanic whites. These data bolster previous epidemiological studies that have found lower rates of incident CVD among moderate drinkers, but also provide cautionary evidence that drinking above recommended limits eliminates this risk reduction. Although randomized trials to evaluate these relationships may yet be conducted to test these issues definitively, clinicians and patients at this time must continue to make informed, individualized, and collaborative decisions about the safety of alcohol consumption.
Acknowledgments
We thank Barry I. Graubard, PhD of the National Cancer Institute’s Division of Cancer Epidemiology and Genetics for invaluable statistical advice. All of the authors participated in the conception and design of the study, analysis and/or interpretation of data, critical review and revision of the manuscript, and provision of statistical or content expertise. Chiung Chen had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: Computer programming and statistical support were provided through the Alcohol Epidemiologic Data System funded by contracts N0AA32007 and HHSN267200800023C from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). NIAAA reviewed and approved this report before submission. The findings and conclusions in this report are those of the authors and not necessarily those of the agency.
Abbreviations
- CVD
cardiovascular disease
- HDL-C
high-density lipoprotein cholesterol
- CHD
coronary heart disease
- NHIS
National Health Interview Survey
- NCHS
National Center for Health Statistics
- NDI
National Death Index
- ICD-9/10
Ninth and Tenth Revisions of the International Classification of Diseases
- CI
confidence interval
References
- 1.Cleophas TJ. Wine, beer and spirits and the risk of myocardial infarction: a systematic review. Biomed Pharmacother. 1999;53:417–23. doi: 10.1016/S0753-3322(99)80121-8. [DOI] [PubMed] [Google Scholar]
- 2.Di Castelnuovo A, Rotondo S, Iacoviello L, Donati MB, De Gaetano G. Meta-analysis of wine and beer consumption in relation to vascular risk. Circulation. 2002;105:2836–44. doi: 10.1161/01.cir.0000018653.19696.01. [DOI] [PubMed] [Google Scholar]
- 3.Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ. 1999;319:1523–8. doi: 10.1136/bmj.319.7224.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mukamal K. Alcohol intake and noncoronary cardiovascular diseases. Ann Epidemiol. 2007;17:S8–S12. doi: 10.1016/j.annepidem.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fillmore KM, Kerr WC, Stockwell T, Chikritzhs T, Bostrom A. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies. Addiction Research and Theory. 2006;14:101–132. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Rehm JT, Bondy SJ, Sempos CT, Vuong CV. Alcohol consumption and coronary heart disease morbidity and mortality. Am J Epidemiol. 1997;146:495–501. doi: 10.1093/oxfordjournals.aje.a009303. [DOI] [PubMed] [Google Scholar]
- 7.Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98:1209–28. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- 8.Block G, Subar AF. Estimates of nutrient intake from a food frequency questionnaire: the 1987 National Health Interview Survey. J Am Diet Assoc. 1992;92:969–977. [PubMed] [Google Scholar]
- 9.National Center for Health Statistics Office of Analysis and Epidemiology. The 1986–2000 National Health Interview Survey Linked Mortality Files: Matching Methodology; Hyattsville, Maryland. October 2005. [Google Scholar]
- 10.Lochner K, Hummer RA, Bartee S, Wheatcroft G, Cox C. The public-use National Health Interview Survey linked mortality files: methods of reidentification risk avoidance and comparative analysis. Am J Epidemiol. 2008;168:336–44. doi: 10.1093/aje/kwn123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson RN, Minino AM, Hoyert DL, Rosenberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. Natl Vital Stat Rep. 2001;49:1–32. [PubMed] [Google Scholar]
- 12.Ainsworth B, Haskell W, Leon A, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Prevalence of leisure-time and occupational physical activity among employed adults--United States, 1990. MMWR Morb Mortal Wkly Rep. 2000;49:420–4. [PubMed] [Google Scholar]
- 14.Blackwell DL, Collins JG, Coles R. Summary health statistics for U.S. adults: National Health Interview Survey, 1997. Vital Health Stat. 2002;10:1–109. [PubMed] [Google Scholar]
- 15.Breslow RA, Graubard BI, Sinha R, Subar AF. Diet and lung cancer mortality: a 1987 National Health Interview Survey cohort study. Cancer Causes Control. 2000;11:419–31. doi: 10.1023/a:1008996208313. [DOI] [PubMed] [Google Scholar]
- 16.Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol. 1997;145:72–80. doi: 10.1093/oxfordjournals.aje.a009034. [DOI] [PubMed] [Google Scholar]
- 17.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 18.Rao RS, Graubard BI, Schmid CH, et al. Meta-analysis of survey data: application to health services research. Health Serv Outcomes Res Methodol. 2008;8:98–114. [Google Scholar]
- 19.Rimm EB, Willett WC, Hu FB, et al. Folate and vitamin B6 from diet and supplements in relation to risk of coronary heart disease among women. JAMA. 1998;279:359–364. doi: 10.1001/jama.279.5.359. [DOI] [PubMed] [Google Scholar]
- 20.Choumenkovitch SF, Selhub J, Wilson PWF, Rader JI, Rosenberg IH, Jacques PF. Folic acid intake from fortification in United States exceeds predictions. Journal of Nutrition. 2002;132:2792–2798. doi: 10.1093/jn/132.9.2792. [DOI] [PubMed] [Google Scholar]
- 21.Rehm J, Irving H, Ye Y, Kerr WC, Bond J, Greenfield TK. Are lifetime abstainers the best control group in alcohol epidemiology? On the stability and validity of reported lifetime abstention. Am J Epidemiol. 2008;168:866–71. doi: 10.1093/aje/kwn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klatsky AL. Invited commentary: never, or hardly ever? It could make a difference. Am J Epidemiol. 2008;168:872–5. doi: 10.1093/aje/kwn192. discussion 876–7. [DOI] [PubMed] [Google Scholar]
- 23.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437–45. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 24.Gmel G, Gutjahr E, Rehm J. How stable is the risk curve between alcohol and all-cause mortality and what factors influence the shape? A precision-weighted hierarchical meta-analysis. Eur J Epidemiol. 2003;18:631–42. doi: 10.1023/a:1024805021504. [DOI] [PubMed] [Google Scholar]
- 25.Jackson R, Scragg R, Beaglehole R. Alcohol consumption and risk of coronary heart disease. BMJ. 1991;303:211–6. doi: 10.1136/bmj.303.6796.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaper AG. Alcohol and mortality: a review of prospective studies. Br J Addict. 1990;85:837–47. doi: 10.1111/j.1360-0443.1990.tb03710.x. discussion 849–61. [DOI] [PubMed] [Google Scholar]
- 27.Mukamal KJ, Chung H, Jenny NS, et al. Alcohol consumption and risk of coronary heart disease in older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 2006;54:30–7. doi: 10.1111/j.1532-5415.2005.00561.x. [DOI] [PubMed] [Google Scholar]
- 28.Friedman LA, Kimball AW. Coronary heart disease mortality and alcohol consumption in Framingham. Am J Epidemiol. 1986;124:481–489. doi: 10.1093/oxfordjournals.aje.a114418. [DOI] [PubMed] [Google Scholar]
- 29.Mukamal KJ, Chiuve SE, Rimm EB. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch Intern Med. 2006;166:2145–50. doi: 10.1001/archinte.166.19.2145. [DOI] [PubMed] [Google Scholar]
- 30.Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 2005;161:423–33. doi: 10.1093/aje/kwi062. [DOI] [PubMed] [Google Scholar]
- 31.Sempos CT, Rehm J, Wu T, Crespo CJ, Trevisan M. Average volume of alcohol consumption and all-cause mortality in African Americans: the NHEFS cohort. Alcohol Clin Exp Res. 2003;27:88–92. doi: 10.1097/01.ALC.0000046597.92232.73. [DOI] [PubMed] [Google Scholar]
- 32.Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005;112:3554–61. doi: 10.1161/CIRCULATIONAHA.105.563452. [DOI] [PubMed] [Google Scholar]
- 33.Edenberg HJ, Xuei X, Chen HJ, et al. Association of alcohol dehydrogenase genes with alcohol dependence: a comprehensive analysis. Hum Mol Genet. 2006;15:1539–49. doi: 10.1093/hmg/ddl073. [DOI] [PubMed] [Google Scholar]
- 34.Klatsky AL, Armstrong MA, Friedman GD. Relations of alcoholic beverage use to subsequent coronary artery disease hospitalization. Am J Cardiol. 1986;58:710–4. doi: 10.1016/0002-9149(86)90342-5. [DOI] [PubMed] [Google Scholar]
- 35.Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet. 1991;338:464–8. doi: 10.1016/0140-6736(91)90542-w. [DOI] [PubMed] [Google Scholar]
- 36.Klatsky AL, Armstrong MA, Friedman GD, Sidney S. Alcohol drinking and risk of hospitalization for ischemic stroke. Am J Cardiol. 2001;88:703–6. doi: 10.1016/s0002-9149(01)01824-0. [DOI] [PubMed] [Google Scholar]
- 37.Mukamal KJ, Chung H, Jenny NS, et al. Alcohol use and risk of ischemic stroke among older adults: the cardiovascular health study. Stroke. 2005;36:1830–4. doi: 10.1161/01.STR.0000177587.76846.89. [DOI] [PubMed] [Google Scholar]
- 38.Mukamal KJ, Ascherio A, Mittleman MA, et al. Alcohol and risk for ischemic stroke in men: the role of drinking patterns and usual beverage. Ann Intern Med. 2005;142:11–9. doi: 10.7326/0003-4819-142-1-200501040-00007. [DOI] [PubMed] [Google Scholar]
- 39.Klatsky AL. Alcohol and hypertension. Clin Chim Acta. 1996;246:91–105. doi: 10.1016/0009-8981(96)06230-4. [DOI] [PubMed] [Google Scholar]
- 40.Djousse L, Levy D, Benjamin EJ, et al. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am J Cardiol. 2004;93:710–3. doi: 10.1016/j.amjcard.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J. Alcohol consumption and risk of stroke: a meta-analysis. JAMA. 2003;289:579–88. doi: 10.1001/jama.289.5.579. [DOI] [PubMed] [Google Scholar]
- 42.Renaud SC, Ruf JC. Effects of alcohol on platelet functions. Clin Chim Acta. 1996;246:77–89. doi: 10.1016/0009-8981(96)06228-6. [DOI] [PubMed] [Google Scholar]
- 43.Mukamal KJ, Ding EL, Djousse L. Alcohol consumption, physical activity, and chronic disease risk factors: a population-based cross-sectional survey. BMC Public Health. 2006;6:118. doi: 10.1186/1471-2458-6-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kerr WC, Fillmore KM, Bostrom A. Stability of alcohol consumption over time: evidence from three longitudinal surveys from the United States. J Stud Alcohol. 2002;63:325–33. doi: 10.15288/jsa.2002.63.325. [DOI] [PubMed] [Google Scholar]
- 45.Giovannucci E, Colditz G, Stampfer MJ, et al. The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol. 1991;133:810–7. doi: 10.1093/oxfordjournals.aje.a115960. [DOI] [PubMed] [Google Scholar]
- 46.Beulens JW, van Loon LJ, Kok FJ, et al. The effect of moderate alcohol consumption on adiponectin oligomers and muscle oxidative capacity: a human intervention study. Diabetologia. 2007 doi: 10.1007/s00125-007-0699-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van der Gaag MS, van Tol A, Vermunt SH, Scheek LM, Schaafsma G, Hendriks HF. Alcohol consumption stimulates early steps in reverse cholesterol transport. J Lipid Res. 2001;42:2077–83. [PubMed] [Google Scholar]
- 48.Rimm EB, Klatsky A, Grobbee D, Stampfer MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits. BMJ. 1996;312:731–6. doi: 10.1136/bmj.312.7033.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Camargo CA., Jr Case-control and cohort studies of moderate alcohol consumption and stroke. Clin Chim Acta. 1996;246:107–19. doi: 10.1016/0009-8981(96)06231-6. [DOI] [PubMed] [Google Scholar]
- 50.Doody MM, Hayes HM, Bilgrad R. Comparability of national death index plus and standard procedures for determining causes of death in epidemiologic studies. Ann Epidemiol. 2001;11:46–50. doi: 10.1016/s1047-2797(00)00177-0. [DOI] [PubMed] [Google Scholar]
- 51.Lloyd-Jones DM, Martin DO, Larson MG, Levy D. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020–6. doi: 10.7326/0003-4819-129-12-199812150-00005. [DOI] [PubMed] [Google Scholar]