Abstract
Public interest in the quality and safety of health care has spurred examination of specific organizational routines believed to yield risk in health care work. Medication administration routines, in particular, have been the subject of numerous improvement projects involving information technology development, and other forms of research and regulation. This study draws from ethnographic observation to examine how the common routine of medication administration intersects with other organizational routines, and why understanding such intersections is important. We present three cases describing intersections between medication administration and other routines, including a pharmacy routine, medication administration on the next shift and management reporting. We found that each intersection had ostensive and performative dimensions; and furthermore, that IT-enabled changes to one routine led to unintended consequences in its intersection with others, resulting in misalignment of ostensive and performative aspects of the intersection. Our analysis focused on the activities of a group of nurses who provide technology use mediation (TUM) before and after the rollout of a new health IT system. This research offers new insights on the intersection of organizational routines, demonstrates the value of analyzing TUM activities to better understand the relationship between IT introduction and changes in routines, and has practical implications for the implementation of technology in complex practice settings.
Keywords: organizational routines, unintended consequences, technology use mediation, electronic health records
Introduction
Health care work is structured through the enactment of organizational routines (Greenhalgh, 2008), defined as ‘repetitive, recognizable patterns of interdependent actions, carried out by multiple actors’ (Feldman & Pentland, 2003). Widespread public interest in quality and efficiency of health care work, partly a result of a substantial amount of public financing, has resulted in certain organizational routines in health care becoming the subject of measurement, analysis, comparison and public reporting. Medication administration, handoffs of patients and information between clinical providers, and infection control practices are all examples of organizational routines that have been targeted for improvement. One result of this public focus on specific routines is the direction of information technology (IT) development and implementation resources toward those aspects of health care work. Health care organizations around the world are considering how IT can support better handoffs and safer medication administration, as it is universally acknowledged that a single error that results in patient harm is one too many.
A possible side effect of such intense focus on a limited set of organizational routines is the underspecification of the impact of new policies and technologies that are intended to alter one routine, such as medication administration, on other routines that overlap with it (Howard-Grenville, 2005). This may explain the growth of the ‘unintended consequences’ literature in health care informatics (Campbell et al, 2006; Ash et al, 2007) that points to a newly defined category of system failure and subsequent adverse patient outcomes referred to as ‘e-iatrogenesis’, or patient harm caused by health care technology (Koppel et al, 2005; Weiner et al, 2007).
This paper examines the impact of new IT on relationships among organizational routines. Using qualitative data from observation of the rollout of barcode medication administration (BCMA) in a hospital setting, we describe what happens when intersections between organizational routines are altered with the implementation of new technology. Abstract and performative dimensions of the intersections are revealed through the activities of a group of mediators who work in the space between the abstract and the concrete, between the BCMA process as designed and the situated actions of nurses giving medications to patients. In this case the mediators are the Informatics Support Team (IST), a group of nurses providing education and go-live support for clinical IT in an academic hospital environment. Our analysis of the work of these mediators reveals that their work involves reconciling collisions between intersecting organizational routines.
First we review theoretical foundations for our work. We then provide background on the technology, the setting and our research methodology. Next, we describe the organizational routine of medication administration and, using three cases, explore the effects of the introduction of BCMA on the work of nurses and on the intersection of medication administration with other routines. In the discussion, we consider the practical and theoretic insights provided by focusing the technology use mediation (TUM) (Orlikowski et al, 1995) framework on relationships among organizational routines and unintended consequences of new technology implementation. We conclude with considerations for how these findings might be used in practice and directions for future research.
Theoretical foundations
Structure and agency in organizational routines
Routines are a central characteristic of human organizations, and widely recognized as the way most organizational work is accomplished (March & Simon, 1958; Cyert & March, 1963; Nelson & Winter, 1982; Hazlehurst & McMullen, 2007). Routines have been identified as sources of both inertia (Nelson & Winter, 1982; Gersick & Hackman, 1990) and change (Feldman, 2000; Feldman & Pentland, 2003). This seeming paradox can be explained by considering the mutually constitutive relationship between abstract notions of routines (e.g. descriptions and understandings of the process) and performances of routines, in which the abstract aspect of the routine is either recreated or changed by knowledgeable agents within a particular situation (Feldman, 2003; Feldman & Pentland, 2003; D’Adderio, 2008). In other words, organizations maintain stability through recurring patterns of collective activity, such as hiring practices, and change occurs as these organizational routines are altered in their execution, for example, when a corporate recruiter begins using social networking technology in his work.
Pentland and Feldman (Feldman & Pentland, 2003; Pentland & Feldman, 2005) describe two dimensions of routines, ostensive and performative, a distinction attributed to Latour (1986). Ostensive aspects are abstract descriptions or understandings of how the routine should be enacted. This dimension includes the steps that can be depicted on a flowchart and described by the participants who carry out the work. Because it articulates organizational goals, the ostensive aspect is important for measurement and comparison of work across and within organizations, and provides for continuity of practice among participants. In a hiring routine, for example, the ostensive aspect might include descriptions of components such as performing background checks, conducting interviews and reviewing resumes. These components represent goals that can be quantified and compared across entities, for example, how many resumes were reviewed for a position, or how many days it took to complete a background check. Performative aspects of routines are specific performances of the routines by individuals or groups. Examining the performative aspect provides insight into the actors’ views of which parts of the routine are flexible, the roles of various people, artifacts and technologies in enacting the routine, and workarounds and other changes to the routine that are possible. The ostensive dimension includes references to the rules and resources that the actors make use of in enacting the routine. The relationship between ostensive and performative aspects of routines has been characterized as one of structure and practice (Feldman, 2003). In everyday practice, enacting the routine has structural influence, either reinforcing the stability of the ostensive dimension of the routine or, less frequently, leading to change in the ostensive dimension.
Organizational routines interact with each other. Howard-Grenville has described this phenomenon as ‘embeddedness’, or the ‘overlap between artifacts and expectations generated from routine performances and those generated from the enactment of other structures’ (Howard-Grenville, 2005). This approach calls for an examination of the practices and artifacts that are involved in a routine, and how those practices and artifacts are also involved in the performances of other organizational routines. With empirical qualitative data on manufacturing routines, Howard-Grenville distinguishes ‘weakly embedded’ routines, which overlap with few other institutional structures, and ‘strongly embedded’ routines that function in the core of the organization, overlapping with many other routines in significant ways (2005). The embeddedness concept is highly useful in understanding intra-organizational variation in flexibility and persistence of routines (Howard-Grenville, 2005).
We aim to extend theory about organizational routines by focusing on the work that actors do when routines come together, a site of structure and action that we conceptualize as an ‘intersection’. Below, we demonstrate empirically that these intersections have ostensive and performative dimensions of their own. Human agents participating in the routines can describe ostensive aspects of the intersection, and the performative aspects are situational, enacted in everyday work. Figure 1 provides a depiction of a generic intersection with ostensive and performative dimensions. Key terms are defined in Table 1.
Figure 1.
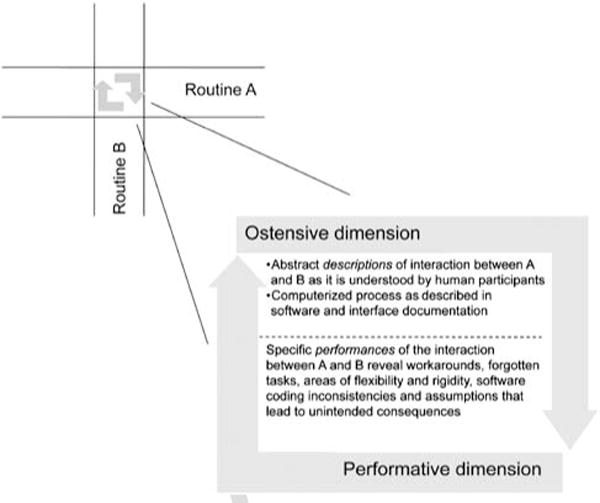
The intersections of organizational routines can have ostensive and performative dimensions, visible in the expectations and actions of participants in each routine.
Table 1.
Key terms
| Key term | Example from this study |
|---|---|
| Organizational routines. ‘Repetitive, recognizable patterns of interdependent actions, carried out by multiple actors’ (Feldman & Pentland, 2003). | Medication administration. |
| Ostensive dimension of routines. Abstract descriptions or understandings of routines (Feldman & Pentland, 2003). | Flowchart of medication administration process. |
| Performative dimension of routines. Specific performances of the routine by individuals or groups (Feldman & Pentland, 2003). | Administrations of medications to specific individuals. |
| Intersection of routines. Site of structure and action where two or more routines come together (Howard-Grenville, 2005). | Intersection of medication administration and pharmacy verification/scheduling. |
| Metastructuring. Second-order structuring where others routinely intervene to influence technological attributes, users’ understandings and interpretations, and institutional policies (Orlikowski et al, 1995). | Changing policy to increase the window of on-time medication administration to allow for longer administrations with the new system. |
| Problem solving. Activities aimed at revealing the sources or causes of negative unintended consequences, including resultant actions to modify social or material structures to improve the effectiveness of routines. | Identifying scenarios that produced the ‘rounding error’ of dose calculation between the two interfaced systems. |
When new technology is rolled out in organizations, human agents continue to bring their historical practices, including experiences with other technologies, to the performance of the routine (Leonardi, 2011). When the intersection of the routines in a particular context produces unanticipated consequences (based on expectations set by historical performances), the factors producing those consequences (e.g. a software glitch in a new interface between two systems) may not be readily obvious. The human agents in each routine rarely have time to solve complex problems that may involve work activities of others, computer program interfaces or other technical issues that fall outside their expertise. Some organizations use personnel with both content (in this case, medical) and technical training to work out the problems during a system rollout. The work of these problem solvers can be referred to as TUM (Orlikowski et al, 1995).
Technology use mediation
Orlikowski (2000) has observed that technology itself does not structure the activities of individuals in organizations, but instead is adapted to the specific context of use by knowledgeable organizational actors. Therefore, technology influences social structure through the use of the technology in routine practices (technology-in-practice), resulting in reproduction of (or change in) rules, resources, technologies and practices in organizations (Orlikowski, 2000). Further, Orlikowski and colleagues observed that mediators intervene in the use of technology and impact the trajectory of use patterns, and developed the notion of TUM (Orlikowski et al, 1995). TUM is defined as ‘deliberate, ongoing, and organizationally-sanctioned intervention within the context of use that helps to adapt a new … technology to that context, modifies the context as appropriate to accommodate use of the technology, and facilitates the ongoing effectiveness of the technology over time’ (Orlikowski et al, 1995, p. 424). TUM is explicated as a process entailing ‘metastructuring’, in which mediators intervene in the structuring process to change the organizational context and provide users with mental models and other interpretive resources to draw upon as they learn and use the technology. Orlikowski et al (1995) are careful to describe this as only one type of metastructuring, stating that due to the social nature of technology use, ‘there will always be other actors who intervene in some way or other in users’ structuring of their technologies’ (p. 437). TUM is characterized by being organizationally sanctioned and observable through activities that ‘routinely and deliberately intervene in users’ structuring activities by influencing users’ understandings, altering technological features to ease use, modifying institutional policies … and facilitating access to and operation of … technologies’ (1995, p. 437).
Davidson and Chiasson (2005) applied and expanded the TUM framework through their study of two health care organizations and their electronic medical records (EMR) systems. Responding to earlier speculation that TUM would be most applicable to generalized technologies such as groupware (Orlikowski et al, 1995), the authors were able to demonstrate the applicability of TUM with a specialized technology, the EMR.
We focus in this paper on mediation activities that involve ‘solving problems’ that arise during rollout of new technology. We define this problem-solving work as activities aimed at revealing the sources or causes of negative unintended consequences, along with resultant actions to modify social structures or material artifacts to improve the effectiveness of routines. By focusing on the problem-solving activities of mediators, we were able to examine in depth the intersections of organizational routines, an area that is somewhat opaque to all but the limited number of agents in the organization whose job descriptions focus on that space. An example of this role in IT is a software tester, using a specific protocol to test an interface between systems. Such protocols are rarely able to test all possible interactions between two applications. An example of such a role in health care is a ‘transfer nurse’, who is designated to get patients and their medical information moved from a procedural area (e.g. surgical suite) into a bed on the acute care unit, where again, omissions are likely to occur. Furthermore, given the level of coordination in the health care setting, intersections of routines are constantly in play. We contend that intersections among routines are common but not well understood, and that the work of problem-solving mediators in medical settings provides a useful window into the reproduction and change of their structure.
Setting
The study site for this research was a multi-hospital, tertiary medical center, implementing a BCMA system. For over a decade, the organization had invested in IT as part of its core strategy for improving care. Applications that had been implemented prior to the study included Computerized Provider Order Entry (CPOE) described in more detail below, nursing documentation, an EMR and all of the ancillary department systems, such as Radiology, Laboratory and Respiratory Therapy. The organization made the decision to implement ‘closed-loop’ medication management, referring to a loop beginning and ending with the physician, and facilitated by interfaced or integrated electronic systems. In the hospital setting, the majority of tests, therapies and medications are carried out or administered based on a physician’s order. As shown in Figure 2, the physician initiates an order in the CPOE system, and the order is transmitted to the pharmacy where it is processed in the integrated pharmacy system. Then the order is fulfilled and delivered to the patient unit, and the nurse administers the medication, using the barcode scanner to scan the patient’s wristband and the medication label. The work of documenting (also referred to as ‘charting’) patient care is a central part of nursing practice. For medications, nurses must document the medication, dose, time and route (e.g. via injection) for each dose they give. The BCMA system automatically documents the relevant information into the EMR, and the physician is able to monitor the administration and effects of the medication through the EMR.
Figure 2.
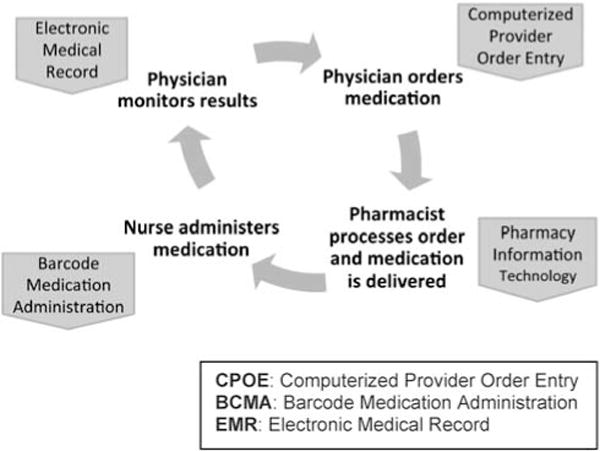
BCMA in closed loop medication management.
At the time of observation, the primary new components of the closed loop medication management system were a new pharmacy information system and BCMA. While these two systems were sourced from a single vendor, they had not been developed by the same company. The study site was an early implementer and development partner of the vendor.
The IST
The IST was a group of approximately 20 registered nurses that functioned as an interface between the informatics developers and the clinical staff. The team was a permanent group, having grown substantially over the previous 5 years as a result of its involvement in the implementation of CPOE and a nursing documentation application in the hospitals. Members of the team represented the needs of users to in-house developers for customizing vendor products and designing application solutions for specific needs. They also worked with project managers, the vendor, informatics staff, hospital management and clinical staff to design implementations, including detailed equipment considerations and rollout scheduling. The IST was also responsible for training new staff on clinical systems and training all users on new systems being rolled out. They provided implementation support, including 24/7 coverage in the early weeks for each unit, initiating and participating in problem resolution for new systems being rolled out, including interface issues with other systems. This support included one-on-one coaching of nurses relative to tasks and concepts in the BCMA system, troubleshooting hardware and software problems, and identifying issues that required policy and process changes. Finally, the IST provided ongoing support of implemented systems. In the cases presented below, aspects of the work of the IST constituting TUM are explored.
Methods
A case study methodology (Eisenhardt, 1989; Ragin & Becker, 1992; Yin, 2003) was used to gain insights into the organizational, technological and individual/group factors involved in the mutual adaptation of new technology and work practices. Data included field notes from observations, documents such as meeting minutes and reports, and email communications. This variety of sources enabled triangulation of findings between activities observed, those discussed in meetings and those reported in shift reports (Denzin & Lincoln, 1998). All names, including those of organizations and groups, have been changed for publication.
Observation
The principal investigator (PI), a Ph.D.-trained health care anthropologist, conducted approximately 50h of ethnographic observation of Informatics Support Team (IST) and nurse interactions during the weeks that the system was being brought online. The observations took place primarily during standard medication administration times in the morning and evening on 10 adult patient care units that went live on BCMA during January through August of 2007. Participants included nurses, IST staff, and other related informatics and clinical staff.
In addition, the PI observed approximately 48 meetings of the IST, including standard team meetings and special problem-solving meetings. Participants in these meetings included IST staff, informatics staff, nursing coordinators and managers, hospital administrators, pharmacy staff, and representatives from the respiratory therapy department. The PI recorded observations as written field notes and subsequently entered the field notes in expanded form into computer text files. Particular attention was placed on capturing issues the IST dealt with and strategies for problem resolution.
Email and shift reports
The IST used email extensively for informal communication as well as semi-structured reports for work shifts when supporting a particular unit ‘going live’ on BCMA. When it became clear that this was a potentially valuable source of data, approval was obtained to analyze these email communications as part of the study. Email communications contained detailed descriptions of problems and problem resolution strategies. Emails (170) were received on an email client and each message was saved as a text file for importation into the data analysis software.
Data analysis
Files containing field notes and email content were imported into QSR NVivo (QSR-International) (Versions 7 and 8 were used), a qualitative data analysis software program. In NVivo, each file becomes a ‘source’ document. Sources are then opened and text units (usually paragraphs) are coded (assigned one or more labels, or nodes). The PI performed all of the coding and was joined in the analysis by the second author. Data were coded initially to identify major themes (such as hardware issues, communication issues, situations resulting in confusion, problems stemming from orders, etc.).
We chose to focus on medication administration because it is a ubiquitous organizational routine that has garnered much attention in the media and regulatory environment. As the research progressed and the activities of the IST were identified as having a role in the adaptation of nursing work to BCMA, the TUM framework emerged as a potentially useful interpretive scheme due to its focus on the work of mediators. To operationalize the organizational routine concept, we initially used Pentland’s (1995) formulation of organizational, technological and cultural structures to examine the embeddedness of medication administration, following the example of Howard-Grenville (2005). However, given the availability of data on the intersections of specific routines, we found that we could develop more compelling insights through analysis of these intersections than through an attempt to calculate the overall embeddedness of medication administration.
Findings and analysis
In this section we first describe the nurses’ medication administration routine and provide an overview of how the introduction of BCMA impacted that routine. We then analyze three instances of the intersection of the nurses’ routine and other routines that relate to medication administration, highlighting in each case ostensive and performative dimensions of the intersection, the unintended consequences that arose with the implementation of BCMA, and the role of IST mediators in mitigating these problems. The cases are: (1) the intersection of medication administration with pharmacy verification and scheduling, (2) temporal coordination of the medication administration routine (a type of intersection) and (3) intersection of medication administration with clinical management oversight. While some aspects of the findings may appear trivial, such as the existence of a computational discrepancy between two interfaced systems, we will demonstrate that not all such discrepancies are mere ‘bugs’ that can be easily fixed, that seemingly minor technology issues can produce social consequences that impact patient care, and that mediators played a critical role in addressing subtle yet significant and complicated problems with the software.
The medication administration routine
The ostensive aspect of the medication administration routine before and after BCMA implementation is described below and depicted in Figures 3 and 4. Medication administration is a central organizational routine for all hospitals that involves many other pervasive routines such as physician ordering, pharmacy work and billing. Almost every patient is given some kind of medication, including both medications and supplements already prescribed (and sometimes brought from home) and medications ordered by physicians to be administered during the hospital stay. The ostensive aspect of the routine that we present for medication administration is conceptualized at a gross level of detail, encompassing widely varying regulatory, institutional and skill requirements of the administration of a range of drugs from narcotics to laxatives in forms that range from intravenous lines to pills.
Figure 3.
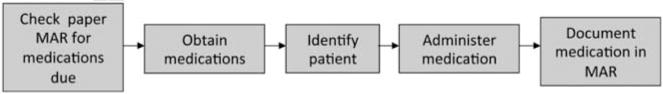
Ostensive representation of the medication administration routine before the implementation of BCMA.
Figure 4.
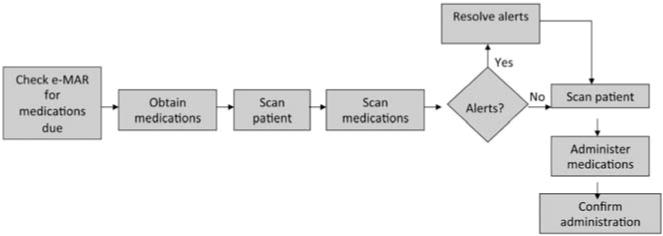
Ostensive representation of the medication administration routine after the implementation of BCMA.
As depicted in Figure 3, prior to BCMA implementation a patient-specific, paper spreadsheet-type document, called a medication administration record (MAR), was used as a central source for tracking medication schedules (i.e. the time and amount of each dose) and for documenting medication administrations. When a physician ordered a new medication (or changed an existing one) using the CPOE system, a copy of the order automatically printed on the patient unit and the unit secretary wrote the new order and schedule information on the existing MAR. Overnight, the pharmacy IT system (which was interfaced to the CPOE system) printed new paper MARs with updated schedules and these were placed in the patient charts. When a nurse was ready to administer medications, she checked the MAR for medications due, obtained the medications, identified the patient (two identifiers were required, such as checking the patient’s identification band and asking the patient for birth date) and administered the meds to the patient. She also then documented on the MAR that the medication had been administered.
In the performance of this routine, errors and other variances from the expected process were not uncommon. Examples of these variances included a medication being given early or late, the patient vomiting immediately after a medication was administered and the patient refusing the medication. Nurses had individualized methods for documenting these variances. Some nurses made a note in the paper MAR next to the affected dose if such an event occurred. They could also choose to document the event elsewhere in the patient chart, and/or discuss it with the nurse on the next shift during the shift change meeting.
With the implementation of BCMA, an electronic medication administration record (eMAR) was implemented, and was interfaced to the CPOE system. With BCMA, nurses could see a medication order on the eMAR when the physician placed the order in CPOE, but the order only became ‘active’ after the pharmacy processed it. Once the order was active, the nurse could scan the patient, scan the medication, address any alerts (such as wrong dose or early/late administration), scan the patient again, click on the ‘Confirm’ icon, and this would automatically update the eMAR that the medication had been given, including the time. If there was an alert for any variance such as a late administration, the nurse would be signaled with a dialog box. The nurse could override the alert and choose from a list of reasons or type in a reason with free text. The post-BCMA ostensive routine is shown in Figure 4.
Case 1: Intersection between medication administration and pharmacy verification and scheduling
As depicted in Figure 2, BCMA was part of a larger, ‘closed loop’ medication management implementation. Along with BCMA, a new pharmacy computer system was being implemented. Both of these systems were highly integrated into the existing informatics infrastructure, with patient data being shared at intersections between administrative and clinical systems for many purposes.
As previously indicated, the pharmacy system and the BCMA system were sourced from the same vendor, but both were the result of vendor acquisitions, therefore the two systems were developed independently, not to work together seamlessly. This project was one of the first installations of the two systems together. Therefore, although the interface code was specified in the vendor organization, it had not yet been fully operationalized in multiple customer environments.
Pharmacy verification and scheduling routine
This first case explores the intersection of the medication administration routine with the pharmacy verification and scheduling routine. When a physician entered an order into the CPOE system it was routed to the pharmacy computer system. A pharmacist processed the order by confirming the clinical validity of it (‘Is it the right medication, dose, route, frequency for the purpose and patient indicated?’), and by creating the schedule. The schedule typically followed what the physician ordered, customized as necessary based on the patient’s needs, the forms in which the drug was available (for example, perhaps a 20 mg tablet would need to be cut in half for a 10 mg dose), and getting the doses onto the standard hospital schedule. For example, sometimes a physician ordered a medication for ‘now, and then twice a day’. If the order came through at 9:00AM, and the twice-a-day schedule was 10:00AM and 6:00PM, the patient would get two doses within 1 h. In this situation the pharmacist might skip the ‘now’ order and set up the schedule for ‘twice a day’ to get the patient onto the standard schedule.
Intersection
As a result of pharmacy processing, the medication materials (pre-filled syringes, IV bags, medications and other physical artifacts) were sent to the nursing unit and a schedule was transmitted to the MAR. Prior to BCMA implementation a copy of the MAR was printed for each patient every 24h that included an updated schedule of all the doses in that time period of all the medications ordered for that patient. This printout was delivered to the nursing unit, where the unit secretary placed it in a patient-specific binder. Nurses referred to the MAR for planning purposes. For example, the nurse could see when medications would be due for a specific patient and coordinate the timing for meds with other tests or procedures to develop an overall plan for the day for that patient. Also, the nurses used the MAR to guide specific medication administration activities, sometimes bringing the MAR to the medication cabinet to ensure that the medications and doses retrieved were accurate. Finally, the nurses wrote on the MAR to document the administration of medications or any variances, such as a late dose.
After BCMA was implemented the intersection was changed by constraints imposed by the system. Nurses could view orders in BCMA that had been entered by physicians, but could not document administration of the medication until the pharmacy had verified the order. This was frustrating for the nurses occasionally, but the pharmacy was typically quick in this work. The pharmacists’ verification work was not changed significantly, but the output of the scheduling process now went to the eMAR instead of being printed on paper. This rendered the doses and schedules available for computational intervention by the BCMA system, and such interventions were the source of several unintended (performed) consequences.
Performative variations in the Case 1 intersection
The data we present on the performative aspect of the medication administration routine revolve around a common event encountered by nurses during administration: a ‘wrong dose’ alert. This frequently came up when more than one pill was required to make up the dose, such as an order of 20 mg of a medication fulfilled by the pharmacy with two 10 mg tablets. Nurses were provided little information on the fact that BCMA was designed to recalculate each dose based on information in the order. At the time of administration, when the nurse scanned the first tablet, a ‘wrong dose’ alert would appear because at that point the system only registered that the nurse was about to administer 10 mg. When the nurse scanned the second tablet, the alert disappeared. The effect of this led to new potential risks, in that nurses found that the ‘wrong dose’ alert could be safely ignored on a frequent basis.
Most notably, during the rollout, nurses were getting seemingly inexplicable ‘wrong dose’ alerts. Through the work of the IST, this issue was finally understood to be the ‘Rounding Error’, a misalignment of decimal rounding between BCMA and the new Pharmacy information system. When a medication was scanned, BCMA calculated the dose and rounded the results to three decimal places. The pharmacy system rounded doses to only two decimal places because, as one pharmacist put it, ‘you can’t draw up 3 decimal places [in a syringe]’. When BCMA came up with a different number than the pharmacy system, which produced the barcode labels, the alert was presented to the nurse. Most commonly happening with pediatric patients and injectible doses, the alert initiated an investigative process for the nurse, who had to confirm the content of the original physician order and calculate the proper dose. Below, a pharmacist colleague emails the IST members to try to clarify the complex problem (Box 1).
Box 1.
To: [Informatics Support Team]
From: Samantha [pharmacy informaticist]
Please note and share with staff:
Oral liquids drawn up by pharmacy will not scan as the patient’s dose, unless the patient’s dose happens to be the same as the concentration of the oral liquid. This applies to [pharmacy system] barcoded patient-specific oral syringes. These will scan as the concentration of the drug. It might be different based on the billing increment the pharmacy is using to charge for these meds. In this example [from forwarded email] below, ursodiol scans as 25 mg/ml. Others, for example, amoxicillin may scan as 250 mg/5 ml.
When the nurse customizes the dose to 80 mg … and presses enter, the incorrect amount warning goes away. This is working as designed. Although it would be ideal for it to scan as the patient’s dose, think of it [as] a good safety check for the nurse to look at the oral syringe in hand and double check the dose, volume, and label and then customize the dose. Please continue reading below …
If you have a medication (oral or injectable) where the incorrect amount warning does not go away after customizing the dose, this is an example of a problem with the ‘rounding’ error. The pharmacy system rounds to two decimals. Depending on the patient’s dose and the concentration of a medication, the true volume calculation could extend beyond two decimals.
For example,
Toradol 8 mg IV. Nurse is drawing up 8 mg from a 30 mg/ml vial. 8 mg = 0.26666666 ml. That is not possible to draw up so we round that volume to 0.27. However, [BCMA] does not round to only two decimals and the incorrect amount warning does not go away once the dose is customized to 8 mg.
NOTE: This is an example of a ‘rounding’ problem med that needs to be sent to pharmacy support. It is possible we will be able to add specific meds to a table so [BCMA] does not consider the volume (although the volume will still display), and it will allow the incorrect amount warning to go away.
Please let me know if you have any questions!
Thanks,
Samantha [pharmacy informaticist]
[from forwarded email]
Patient Samuelson in 12B – Med not scanning correctly. Actigall/Ursodiol scanned as 25 mg but the actual amount being scanned was 80 mg, which matches the patient specific barcode. The nurse corrected, annotated and followed the procedure. She also filled out the pharmacy form and stuck the barcode label on the back of the form
In the email, Samantha also describes yet another source of a wrong-dose error. When administering an oral liquid from a syringe prepared with a patient-specific label, a scan of the barcode did not produce the actual amount being administered. Instead the amount shown was the concentration of the drug (the amount of the drug per milliliter of solution). The nurse was required to change the dose to the actual amount being administered. Reasons were not given for this design, but Samantha tries to smooth it over by suggesting that the nurses could think of it as a ‘good safety check’. The email at the end, forwarded by Samantha, describes the nurse filling out a pharmacy form. This refers to a new process in which the pharmacy placed a box on the nursing unit to collect packaging with barcodes that did not work properly. This packaging, previously trash, was now important evidence to submit to the pharmacy when a barcode produced the wrong result, or did not scan at all. The ostensive and performative dimensions of the intersection – before and after BCMA introduction – are depicted in Figure 5.
Figure 5.
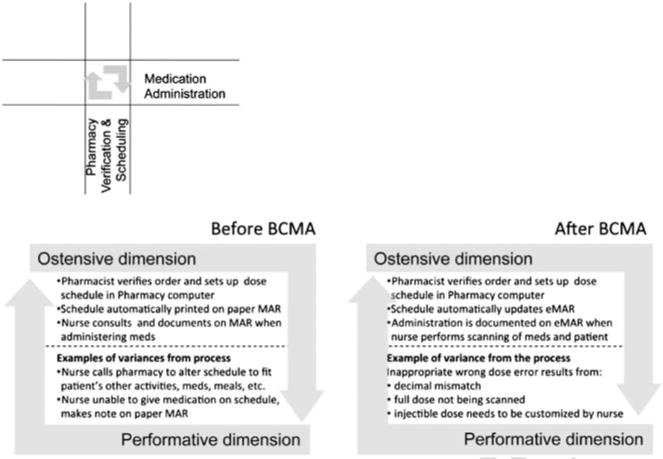
The ostensive and performative dimensions of the intersection between medication administration and pharmacy verification and scheduling were altered with the implementation of BCMA.
Mediation
The problem-solving activities of the IST related to the unintended wrong dose errors highlight the ostensive and performative dimensions of the intersection between medication administration and pharmacy dosing. To understand the ostensive dimension, the group met frequently with pharmacy informatics staff, IT staff and the vendor. These collaborators provided the IST with information on the intended interface between the two information systems (i.e. how they should interact, based on what was known about the technical interface). To understand the performative dimension, the IST mapped out the ‘behavior’ (as they referred to it) of the system in use. In one meeting, the IST and pharmacy staff collaborated to test numerous combinations of order components (drugs, drug forms, doses, etc.) to try to identify the factors producing the Rounding Error. Eventually, they were able to specify scenarios that typically generated the alert, or the performative aspect of the intersection. On the basis of the scenarios, the BCMA software was modified to suppress the error message in cases that met specific criteria. Without the skillful expertise and pattern-revealing collaboration of the IST, the discrepancy that constituted the rounding error may not have risen to the attention of the IT staff developers.
In addition, the IST mediated the use of BCMA during this transition by training nurses to recognize and manage the unintended consequence of the Rounding Error. They provided information during training about scenarios that could produce the error and coached nurses during go-live on how to identify and resolve the issue.
Case 2: Temporal coordination in medication administration
The second case deals with the intersection of the medication administration routine on a given nursing shift with the medication administration routine on the next shift. Much of the work of health care practitioners and managers has to do with preparing for the future. A nurse may spend much of her day organizing a patient’s schedule for procedures, tests and medications, documenting clinical observations and interactions with patient and family, and otherwise planning for work (to be done by someone else) in the future. Therefore it is essential that the planning and evaluation of new technology consider the impact of the technology on temporal coordination.
Medication administration routine: coordinating across shifts
The ostensive aspect of the medication administration routine before and after BCMA implementation is described in Figures 3 and 4. Prior to BCMA, medications were ordered in the Computerized Provider Order Entry (CPOE) system and were subsequently represented on a pre-printed form, the MAR. This patient-specific document organized each dose temporally across the page. Nurses documented information on the MAR in various ways, such as circling the medication and noting the time given, or just writing the time given next to the dose. If the nurse made a mistake in documenting she could write ‘error’ and a small note to explain. Documentation accomplishes several goals, including the production of a legal document of the care given to a patient, a record that the nurse can refer back to later in a shift if she needs to be reminded of a specific time or task, and a record for others to view, including people in other roles taking care of the same patient (e.g. physicians or respiratory therapists) and other nurses taking care of the same patient in the future. To coordinate with nurses on subsequent shifts, nurses sometimes wrote more detailed messages on the MAR, such as instructions for a lab test for drug levels in the blood that needed to occur on the next shift, or advice on giving specific meds to certain patients (e.g. ‘patient will only take this med mixed in applesauce’). Although it was considered an unorthodox use of the MAR and not done by all nurses, the practice of writing instructions or messages to the nurse on the next shift was a norm within a repertoire of possible actions that were considered acceptable ways of communicating. With the implementation of BCMA the paper MAR was eliminated, and with it the possibility of writing a note adjacent to a specific dose. The design of the BCMA system was intended to replace the MAR with a module called the ‘e-MAR’, which was purported to make documentation easier for the nurse. When the nurse clicked ‘confirm’ after administering medications, all of the administrations were charted on the eMAR automatically.
Performative variations in the Case 2 intersection
The reality of inpatient care is that, with delays such as patients being off the unit for tests or treatment, asleep or otherwise unavailable, nurses often must make adjustments to the schedule. Consider for example a patient with a medication ordered for twice a day. This results in doses at 10:00AM and 6:00PM. If the patient is off the unit for a procedure and misses the 10:00AM dose, the nurse must find a way to ‘stagger’ the patient back onto the standardized schedule, or perhaps decide not to give that dose and document it as ‘Not given’. The nurse on the following shift may interpret the situation differently and decide to try and give the dose to the patient. With the eMAR, if the 10:00AM dose has been charted as ‘Not given’, the nurse is unable to document against that dose. She may choose to give the 6:00PM dose early, and plan to give another one later that night, at which point she must give the next day’s 10:00AM dose. This practice occurred frequently and was referred to as ‘stealing doses’. The eMAR was therefore less flexible than the paper MAR, forcing specific doses into categories. In this case, once charted as ‘Not given’, the first 10:00AM dose could not be re-documented as a dose that was given. This phenomenon, easily dealt with using a note in the paper world, strained relations across shifts and necessitated many pharmacy interventions to balance the doses.
The nurses had been accustomed to coordinating work across shifts using the flexibility of the paper MAR. They used the MAR to write notes to the nurse on the next shift, including comments about a particular dose (missed, late, refused, etc.) and notes of advice and information about the patient. ‘Stealing doses’ represents a disruptive effect of the loss of the paper MAR as a coordination tool and the inability of the eMAR to accommodate a flexible dosing schedule. The ostensive and performative dimensions of the temporal intersection of the medication administration routine are summarized in Figure 6.
Figure 6.
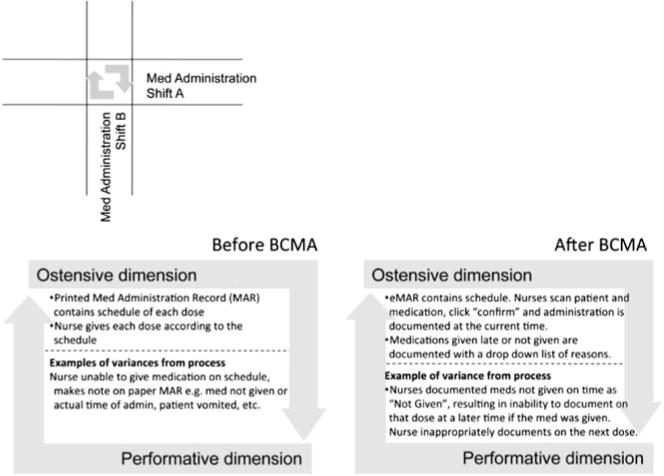
Ostensive and performative dimensions of the temporal intersection of medication administration before and after BCMA.
Mediation
IST members developed an understanding of the issues related to dose documentation and flexibility, augmenting their individual experiences as nurses with substantial time spent on patient units observing and working with nurses. This experience helped to inform the BCMA training curriculum, as the training classes were taught by IST members who were actively supporting the go-live. Through this connection between support and training, problems seen in the rollout could be communicated to new users along with potential workarounds or explanations that helped avoid the problem in the next unit going live. The problem-solving activities of the IST in this case also included working with IT to develop a workaround in the computer system that enabled nurses to create a special type of ‘order’ (similar to a physician’s order, but from nurse-to-nurse) to communicate medication instructions. The medication instructions order was visible to the nurse in the CPOE system, along with all of the other orders (e.g. medications). The workaround was not frequently used because the instructions order appeared in the CPOE system, not on the eMAR with the relevant dose. The nurse had to notice the instructions, and then go into the eMAR to find the particular dose(s) to which the instructions referred. This ‘solution’ was therefore missing the situatedness that characterized the previous practice of a note written adjacent to a dose on the paper MAR. As a result, nurses began to rely more heavily on the verbal, face-to-face shift report for communicating instructions to the nurse on the next shift. Ultimately mediation, in this case, failed to produce a technological solution to the problem, but did succeed in making nurses aware of the need for reliable forms of shift-to-shift communication.
Case 3: Medication administration and management oversight
The third case deals with the intersection of the medication administration routine and one routine for management oversight. The methods of enforcement of clinical policies vary widely among managers. The implementation of new technology offers opportunities to count, measure and report on elements of work that are captured (accurately or not) by the system. This case focuses on the clinical policy related to ‘late’ medications.
Management oversight of medication administration
There are many clinically acceptable reasons for a medication to be given late. Examples include the patient being unavailable (e.g. away from the unit having a procedure) and the patient being asleep (in the case of an optional or non-urgent medication). Just prior to BCMA implementation, a decision was made to extend the window of on-time dose administration to 1h before and 1h after the scheduled time. Previously, a dose had been classified as ‘early’ or ‘late’ if it were given 1/2h before or 1/2h after the time scheduled on the MAR.
Intersection
Before BCMA, nursing managers had minimal data to work with when assessing a nurse’s ‘performance’ regarding on-time medication administrations. Busy managers would have had to examine numerous doses documented on paper MARs to identify any pattern, therefore, oversight of medication administration timing had historically been minimal. With the implementation of BCMA came the ‘Overdue Medications Report’, flagging doses that were overdue. The report, which listed the patient, medication and ordered time, could be run for medications that were 1–8 h overdue, or 10–48 h overdue. During the early phases of the implementation, nursing managers were experimenting with multiple reports and formats to determine what was useful; the ostensive aspect of the new routine for management oversight of medication administration was therefore undetermined and shrouded in mystery.
Performative variations at the Case 3 intersection
The nurses were concerned about this new ostensive element, which they perceived as a performance indicator. In addition, given the deployment of numerous informatics staff to observe, evaluate and tweak the implementation, nurses may have felt as though they were under surveillance. Nurses adapted by overusing the ‘Not given’ documentation to take medications off the list of active orders and thus off the Overdue Medications Report. However, if the dose was removed using ‘Not given’ documentation, and then the nurse wanted to give it at a later time, she would need to document it on the next dose in the schedule, which then was registered as stealing a dose (see Case 2 above). Figure 7 summarizes the ostensive and performative dimensions of this intersection.
Figure 7.
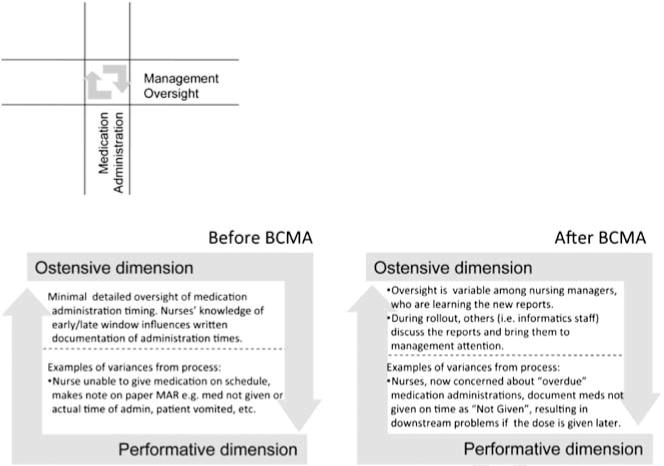
Ostensive and performative dimensions of the intersection between the medication administration routine and a routine for management oversight.
Mediation
The IST members, as nurses, understood the nurses’ desire to avoid ‘Overdue’ medications and used several strategies to bring nursing practice more in line with requirements of the tool. At the policy level, the team facilitated a name change to ‘Outstanding Medications Report’, which helped remove some of the stigma of having medications published as ‘Overdue’. The IST also engaged in an extensive educational campaign to try to convince the nurses that they were not being judged for having a late medication (whether they were or were not being judged was not confirmed in our data) and remind the nurses that there were many valid reasons for a medication being late. They trained the nurses to use other documentation categories to address off-schedule doses without using ‘Not given’. In this way, the IST members relied on their clinical and social experience as nurses to understand the goal the nurses were working toward (minimizing ‘Overdue Medications’), to transform the BCMA artifact (changing the title of the report) and to realign the nurses’ clinical priorities. These excerpts from the IST manager’s email to the team illustrate the goals of mediation in this case (Box 2):
Box 2.
To: [Informatics Support Team]
From: Sarah [IST Manager]
Sometimes an overdue dose needs to remain overdue at the end of the shift because of patient condition, IV access, patient availability, or other factors and in these cases we do NOT want staff to document against that dose…. This is a bit counterintuitive to staff who perceive the Overdue Meds list as a tool to punish forgetful nurses rather than the safety tool it’s meant to be seen as.
Sarah
Our data on the metastructuring of the intersection between medication administration and management reporting reveal ostensive and performative aspects of this intersection. The BCMA system was capable of producing 13 management reports, including data summarized by: patient, department, specific medication types (for example, controlled substances such as narcotics) and others. The organization did not go into the rollout of BCMA with a specific set of reports selected for use. Instead the system was rolled out, and managers assessed the value of various reports. This is a case of the ostensive aspect of the management reporting routine being undetermined at the time the technology was implemented, purposefully allowing for the performative dimension of the routine to shape the structure of the intersection between medication administration and management reporting. As the data became available and reports began to circulate, it became clear through the problem-solving work of the IST that nurses were reacting to the Overdue Medications Report by inappropriately documenting late doses as Not given, which then resulted in stolen doses downstream. The IST facilitated the change to the report, a metastructuring activity at the intersection, with the hopes of affecting nursing performance at that intersection (i.e., medication administration with awareness of management reporting structure).
Discussion
The results of our analysis are summarized in Table 2. These findings have both theoretical and practical implications.
Table 2.
Summary of findings relative to intersections of routines, unintended consequences and problem solving activity
| Case | Routine | Routine | Dimensions of the intersection | Unintended consequences | Problem-solving actions of IST
|
|
|---|---|---|---|---|---|---|
| 1 | 2 | Problem identification | Indications of metastructuring | |||
| 1 | Med Admin/BCMA | Pharmacy Verify and Schedule |
Ostensive: (1) Pharmacist encodes dose in pharmacy system, which transmits information to eMAR. (2) eMAR performs check of dose. Performative: (1)Specific combinations of drug forms and doses revealed that BCMA/eMAR and pharmacy systems rounded decimals differently (2) Scanning barcode on oral liquids produced concentration, not dose. (3) Nurses engaged in time-consuming research to confirm dose. |
Inaccurate wrong dose alerts necessitated nurses spending more time on search for proper dose. | • Meeting with people from pharmacy to explore erroneous alerts problem. • Testing and identifying scenarios producing problem. |
• Training and coaching nurses in recognizing rounding error. • Contributing to development of a solution to suppress the error in specific cases. |
| 2 | Med Admin/BCMA | Med Admin/BCMA | Temporal intersection of medication administration across shifts. Ostensive: Doses are given at the time and frequency prescribed. Performative: Patients were often unavailable or asleep, refused meds, vomited, dropped pills, etc. necessitating doses to be delayed or not given. Nurses could not document giving a dose that had already been documented as ‘not given’. |
If a nurse gave a dose that had been previously documented as ‘not given’, she often documented against the next dose on the schedule, creating a cascade of ‘stolen doses’. Note: Prior to BCMA this was easily addressed with a note in the paper medication record. |
• Working backward from a problematic ‘stolen dose’ to identify the reason the first dose was stolen (i.e. original late dose inappropriately documented ‘not given’) | • Contributing to the development of a special ‘order type’ for nurses to communicate with next shift. • Developing training tools to help nurses understand how to use the new order type. |
| 3 | Med Admin/BCMA | Mgmt Reporting |
Ostensive: Range of BCMA management reports available to be used. Specific ones (out of 13 available reports) were initially undetermined. Performative: Nurses, aware of the existence of the Overdue Medications Report, overused the Not given documentation to remove doses from the active medications list, and therefore from the Overdue Medications Report. |
Overuse of Not given documentation resulted in stolen doses (see Case 2) and documentation problems that arose hours and days downstream relative to future doses of that medication. | • Understanding the meaning of the Overdue Medications Report to nurses. | • Working with management to increase the on-time medication window to 2 h. • Changing the name of Overdue Meds Report. • Educating nurses on the clinical validity of ‘overdue’ meds in certain situations. |
Theoretical implications
Ostensive and performative dimensions of intersections
Research has established the existence of ostensive and performative dimensions of organizational routines (Feldman & Pentland, 2003). Our findings reveal that intersections among organizational routines also can have ostensive and performative dimensions. For example, prior to the implementation of BCMA, the ostensive aspect of the intersection between medication administration and Pharmacy Verify/Schedule (Case 1) was inscribed in the paper MAR, while the performative dimension was comprised when the nurses administered a dose through following the guidance of the MAR. Similarly, the ostensive aspect in the initial version of the temporal intersection between medication administration routines (Case 2) was detailed in the nursing documentation software, with the performative aspect comprising verbal communication supplemented by occasional notes hand-written on the MAR printout. The final case involved the management oversight routine, which entailed a manifestation of the ostensive aspect of numerous organizational routines that Feldman & Pentland (2003, p. 106) would refer to as accounting. The interaction between the management oversight routine and the medication administration routine was initially constituted ostensively by documented hospital policy on the window of early and late medication administrations. Performatively, the policy was not strictly enforced on a large scale; however, nurses did, with knowledge of the policy window, note administration times on the MAR in their administration routine.
Unintended consequences of new technology introduction
Information technology’s capacity to codify ostensive aspects of a routine is quite powerful because digital texts can be quickly, and easily replicated across time and space, with the result that changes to such representations ripple swiftly across and through intersections of routines. Our findings indicate that the introduction of new IT can therefore bring previously stable ostensive and performative aspects of an intersection out of alignment, and thereby result in unintended consequences. Although some of the ostensive aspects of the original intersections were already encoded in software, the changes wrought by introduction of the new BCMA system highlight how the increasingly fine-grained specification entailed by IT development can lead to the newly revised ostensive dimension of an intersection being out of alignment with pre-existing performative aspects. This view of the impact of new IT on previously stable ostensive and performative aspects of intersections offers a fresh perspective on the ‘intertwined’ (Becker et al, 2005) social and technical aspects of routines. It extends previous work that characterizes relations among routines as ‘embeddedness’ (Howard-Grenville, 2005) by highlighting that the intersection itself is the site of structured work practices that suffer unintended consequences when changes made to one routine propagate to others, refracting at the intersections.
For example, in Case 1, BCMA replaced some aspects of the prior performative dimension in ways that no longer jibed with remaining performative aspects, thereby leading to disrupted performances of those intersections – that is producing several types of erroneous dose error messages such as the ‘rounding error’. In the health care industry, computer applications experience long lives through acquisitions and mergers of software companies, resulting in software code that may have been developed long ago and far away from the current implementation. This distance in time and space between the developer and the user supports an agentic characterization of the tool (Leonardi & Barley, 2008), in that there may be little understanding among the humans (users and IT professionals) as to why events such as erroneous dose errors occur, and which aspects of the system(s) involved are implicated, thereby contributing to unintended consequences, and it also accentuates the need for and value of TUM mediators.
In Case 2, the temporal intersection of medication administration routines, multiple methods were initially used to communicate medication instructions to the nurse on a future shift. As the BCMA system was introduced, the ostensive dimension of the intersection was altered by the elimination of the paper MAR, and with it went the ability for nurses to leave a note adjacent to a specific dose. This case adds to previous research on technology’s role in temporal coordination in health care (Bardram, 2000; Xiao, 2005; Reddy et al, 2006) by highlighting the effect of technological change on the practices of coordination.
Data in Case 3 revealed that the BCMA technology altered the nurses’ perceptions of the consequences of a late administration through its production of the Overdue Medications Report that, for the nurses, represented potentially unwarranted reprisals, leading to further unintended consequences of inappropriate documentation on doses not given and downstream problems with future doses. The employment of a practice-based analysis (Feldman & Orlikowski, 2011) enabled exploration of the changes in the enactment of significance (Beynon-Davies, 2010): we found that the BCMA altered the meaning of ‘medication administration’ for the nurses by introducing the potential threat of task-level surveillance of their work by management. Linking such a meaning-centered analysis to the phenomenon of computer workarounds should enable improvements in implementation design, particularly related to management and policy actions (Azad & King, 2008).
TUM as corrective to misalignment of ostensive and performative aspects of intersections
Finally, our study highlights the role of mediators as problem solvers at the intersections of routines, and the methodological utility of focusing on TUM activities as a window into organizational routines. This approach can complement existing research that homes in on technology design and user behavior such as Goh et al (2011). The data from the cases presented here allow a distinction to be drawn between problem-solving activities and activities that constituted metastructuring. Whereas problem-solving activities were oriented toward identifying causes underlying negative unintended consequences, metastructuring was oriented toward reconciling the ostensive and performative aspects of the routine intersections to eliminate those problems, through ‘influencing users’ understandings, altering technological features …, modifying institutional policies, and facilitating access to … technology’ (Orlikowski et al, 1995).
Data collection initially focused primarily on problem-solving activities, and then extended to observing resultant actions to modify human or material structures to improve the effectiveness of routines. An example of the IST identifying root causes of negative unintended consequences is in Case 1, where the IST’s work homed in on the intersection between pharmacy and medication administration, starting with an understanding of the ostensive aspect of the two routines and their intersection. The IST members examined many performances of the routine and conducted simulations to understand the triggers of certain ‘behaviors’ (as they described it) of the BCMA system that produced the erroneous alerts, until the source of the ‘unintended consequence’ was found (i.e. the mismatch in dose rounding between the BCMA and pharmacy systems). In this way, the IST not only participated in identifying the problem, but in conceptualizing the solution, which was not a simple change to the rounding scheme of one of the systems, but instead an algorithm that suppressed the error in certain cases. If the IST problem-solving mediators had not pursued the ‘wrong dose’ issue in Case 1, the discrepancy would likely have been obscured by the work of nurses who are expert at ‘making do’ with systems (such as monitors, infusion pumps and computer systems) that do not work well together, and who might still be wondering why they sometimes get an erroneous wrong dose alert.
Attention to these intersections of (deeply embedded) routines harks back to Les Gasser’s work on ‘intersecting task chains … a production lattice’ (1986, p. 210), in which he noted the importance of articulation work (Strauss et al, 1985) for managing conflicts at the intersections. Our additions to this include calling attention to the value of having dedicated personnel focused specifically on doing this articulation work during new IT system implementation, and that focusing research on the work of these mediators helps clarify the aspects of articulation work, such as computer workarounds (Azad & King, 2008), that can and should be eliminated or streamlined through improvements in technological infrastructure.
With regard to metastructuring activities, we found they were undertaken to bring ostensive and performative aspects of routine intersections back into sync, either attempting to modify the ostensive aspect directly (as with written policies or computer programs), or to induce changes in performative aspects through influencing how practitioners did their work. Examples of the former were evident in Case 2, developing a new electronic ‘order type’, and in Case 3, where the IST modified institutional policy by facilitating the expansion of the on-time window to 2 h and renaming the report. Examples of the latter include training and coaching nurses to recognize the rounding error (Case 1) and educating nurses on the clinical validity of ‘overdue’ medications in certain situations (Case 3). It should be noted that efforts to influence performance were not always effective, as for example in Case 2, when the nurses did not make substantial use of the technological workaround, because the clinical value of locally situated hand-written notes on paper was not matched by the new (electronic) order type.
Practical implications
The distinction between training users on new technology and truly integrating new technology safely into everyday practice is significant in industries that deal with substantial risks to human safety, such as health care. We therefore anticipate several significant practical implications of our work.
Highlighting differences between performative and ostensive aspects of routines and their intersections helps health care managers recognize that making changes to the ostensive version of a routine or intersection of routines does not automatically carry over to corresponding performative dimensions of routine intersections. Codifying the ostensive aspects of a singular routine with IT can improve safety, for example, by explicitly constraining the dose of a drug that can be prescribed to a patient – a performance traditionally carried out by a single physician in a relatively independent (i.e. unembedded) manner. By comparison, the routine administration of medication is a type of performance intertwined with many other organizational routines involving artifacts such as pills, IV pumps and locked medication cabinets, as well as intimate physical interaction with the patient, and other factors that limit the information system’s influence over the event.
Thus a change to the ostensive aspect of a deeply embedded routine through the implementation of new IT is more likely to bring previously stable ostensive and performative aspects of an intersection out of alignment, and thereby result in negative unintended consequences. These issues became visible in our data through our focus on problem-solving work of the IST.
The organization we studied had invested substantially in the IST, which brought value to the BCMA implementation through rapid identification and resolution of problems. Such teams can employ a range of metastructuring techniques to address technology introduction problems, including altering the technology, changing clinical practice and workflow, and educating the nurses on the new concepts and tasks they need to understand in order to safely integrate the technology into everyday work. It is not incidental that all members of the IST had clinical nursing experience. Having taken care of patients and experienced the challenges of clinical coordination themselves, the IST members were able to appreciate the nurses’ competing goals and to imagine ways to integrate the new goals created by BCMA into the existing work. This is illustrated in Cases 2 and 3 by their attention to the detailed work of coordinating patient care across shifts: IST members used their subjective experiences as nurses to engage with the complex nexus of issues related to (1) coordinating dose timing (‘stealing’ doses) and (2) communication of advice and instructions to the next shift at the intersection of the medication administration and management reporting routines.
Organizational managers may therefore want to more seriously consider investing in professional TUM teams such as the IST. At the same time, it is also important for IT system developers to learn about performative aspects of routine intersections, not just follow institutionally sanctioned directions to automate individual routines as if they were not organizationally embedded. Furthermore, we also suggest that managers can benefit practically by focusing on the role of mediators and their problem-solving activities at the intersections, as this provides a particularly effective approach to identifying ‘organizational levers’ (Feldman & Orlikowski, 2011) that can be used to bring tools and practices into better alignment.
In sum, we find that scholarship and practice in the implementation of new information technologies can benefit from more closely examining the relationship between routines, new technology and organizational change. More specifically, research that relies on theories of organizational routines to examine the coordination of tasks and information across roles or groups will benefit from more closely attending to the intersections through which routines are organizationally embedded. A similar orientation to routine intersections should also prove useful for improving work analysis tools, which can aid IT system design and development by better anticipating consequences of new technology for users. And as suggested above, we contend that the role and value of mediators during the introduction of technology should be regarded as a potentially significant resource for both theory development and practical outcomes.
Conclusion
Much of the work of organizations occurs at the intersection of organizational routines, and routines have been theorized extensively in the organizational literature. However, the impact of change on routines brought about by the implementation of new IT is not nearly as well theorized. Even less attention has been paid to the activities and structural dimensions that characterize the relations among established routines. In addition to its centrality within modern health care organizations, medication administration is a routine that is rife with variability among actors, artifacts and unanticipated temporal and situational contingencies, and as such affords an extreme case for the study of IT and routines. Here we studied the impact of new technology for medication administration on this routine as it intersects with other routines, with attention to the ostensive and performative aspects of the intersections. Through following the connections and activities of technology use mediators, we were able to closely examine sites of interaction and articulation work traditionally overlooked by IT developers and theorists of organizational routines.
This research makes three key contributions. First, this study highlights the importance of intersections among established organizational routines, and the ostensive and performative dimensions of those interactions. Second, the study demonstrates that the implementation of new IT can bring previously stable ostensive and performative aspects of an intersection out of alignment, and that this misalignment can result in negative unintended consequences. Finally, the study highlights the role of mediators as problem solvers at the intersections, and reveals the utility of focusing on their metastructuring activities as a window into organizational routines.
A key limitation of this work is the characterization of ‘intersections’ among routines as a two-dimensional relationship. In reality, each routine may intersect with multiple other routines at the same time, and with different phases of itself at different times. However, the concept of intersections provides an analytical lens for examining situations in which the ostensive dimensions of more than one routine are involved in structuring the actions of human and material agents, and the consequences that may emerge when changes are made in one routine, relative to the others. Further research may elucidate more sophisticated models of intersections and embeddedness that can inform both organizational and technology design.
Future research on structuring in routine intersections may thus enable better prediction of the potential impact of new technology on existing routines and their intersections – including intersections that are upstream, downstream and adjacent to the immediate tasks being automated. Moreover, consideration of communication strategies and other performative aspects of these intersections should lead to improved technology design, especially in fields such as medical care where high reliability is crucial, as these developments can have significant impacts improving safety for both practitioners and patients.
Acknowledgments
The work reported here was supported by grants 2-T15LM007450-06 and 1K99LM-010038-01 from the U.S. National Library of Medicine. The authors acknowledge the valuable insights and enthusiastic cooperation of the study participants. Dr. Timothy Vogus is acknowledged for his insights regarding managers’ inattention to the embeddedness of organizational routines. Thanks also to the EJIS Associate Editor and anonymous reviewers for their valuable insights and critiques.
Footnotes
About the authors
Dr. Laurie Novak is Assistant Professor of Biomedical Informatics at Vanderbilt University School of Medicine. She holds a Ph.D. in Medical and Business Anthropology from Wayne State University, and a Masters in Health Services Management and Policy from the University of Michigan. Her research interests include technology-in-use in the everyday management of chronic illness, and organizational perspectives on strategies employed by clinicians and patients to create safety during transitions to new systems of care. She is a member of the Implementation Sciences Laboratory at Vanderbilt.
Dr. JoAnn Brooks is a Postdoctoral Research Associate at Syracuse University’s School of Information Studies. Her Ph.D. is from the University of Michigan in Public Policy Studies and she holds an MS in Computer and Information Science from University of Massachusetts at Amherst. Her research focuses on organizing practices in work environments, especially as they involve the use of IT.
Dr. Cynthia Gadd is Professor of Biomedical Informatics and Director of Educational Programs at Vanderbilt University. Her research interests include the evaluation of integrated clinical information systems and the development and evaluation of innovative approaches for biomedical informatics education and training to meet the needs of health care in the U.S. and globally. She is a member of the Implementation Sciences Laboratory at Vanderbilt.
Dr. Shilo Anders is Research Assistant Professor in the Center for Research and Innovation in Systems Safety at Vanderbilt University. She received her doctoral degree in Industrial and Systems Engineering from the Ohio State University. Dr. Anders’s research focuses on using Cognitive Systems Engineering principles investigate problems in information analysis, data overload, predictive analysis, information visualization and adaptive capacity in both military and health care domains. She is interested in research on system design, individual and team performance issues, and improvements in patient safety and quality.
Dr. Nancy Lorenzi is Assistant Vice Chancellor for Health Affairs, Professor of Biomedical Informatics and Clinical Professor in Nursing at Vanderbilt University. She is an internationally recognized expert on change management related to information technology, with particular focus on organizational and personnel issues related to automation in the health care industry. She is the Director of the Implementation Sciences Laboratory at Vanderbilt.
References
- Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended sociotechnical consequences of computerized provider order entry. International Journal of Medical Informatics. 2007;76(Supplement 1):S21–S27. doi: 10.1016/j.ijmedinf.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Azad B, King N. Enacting computer workaround practices within a medication dispensing system. European Journal of Information Systems. 2008;17(3):264–278. [Google Scholar]
- Bardram JE. Temporal coordination – on time and coordination of collaborative activities at a surgical department. Computer Supported Cooperative Work (CSCW) 2000;9(2):157–187. [Google Scholar]
- Becker MC, Lazaric N, Nelson RR, Winter SG. Applying organizational routines in understanding organizational change. Industrial and Corporate Change. 2005;14(5):775–791. [Google Scholar]
- Beynon-Davies P. The enactment of significance: a unified conception of information, systems and technology. European Journal of Information Systems. 2010;19(4):389–408. [Google Scholar]
- Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. Journal of the American Medical Informatics Association. 2006;13(5):547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyert RM, March JG. A Behavioral Theory of the Firm. Prentice-Hall; Englewood Cliffs, NJ: 1963. [Google Scholar]
- D’Adderio L. The performativity of routines: theorising the influence of artefacts and distributed agencies on routines dynamics. Research Policy. 2008;37(5):769–789. [Google Scholar]
- Davidson E, Chiasson M. Contextual influences on technology use mediation: a comparative analysis of electronic medical record systems. European Journal of Information Systems. 2005;14(1):6–18. [Google Scholar]
- Denzin NK, Lincoln YS, editors. Collecting and Interpreting Qualitative Materials. Sage Publications; Thousand Oaks, CA: 1998. [Google Scholar]
- Eisenhardt KM. Building theories from case study research. The Academy of Management Review. 1989;14(4):532–550. [Google Scholar]
- Feldman MS. Organizational routines as a source of continuous change. Organization Science. 2000;11(6):611–629. [Google Scholar]
- Feldman MS. A performative perspective on stability and change in organizational routines. Industrial and Corporate Change. 2003;12(4):727–752. [Google Scholar]
- Feldman MS, Orlikowski WJ. Theorizing practice and practicing theory. Organization Science. 2011;22(5):1240–1253. [Google Scholar]
- Feldman MS, Pentland BT. Reconceptualizing organizational routines as a source of flexibility and change. Administrative Science Quarterly. 2003;48(1):94–118. [Google Scholar]
- Gasser L. The integration of computing and routine work. ACM Transactions on Information Systems. 1986;4(3):205–225. [Google Scholar]
- Gersick CJG, Hackman JR. Habitual routines in task-performing groups. Organizational Behavior and Human Decision Processes. 1990;47(1):65–97. doi: 10.1016/0749-5978(90)90047-d. [DOI] [PubMed] [Google Scholar]
- Goh JM, Gao G, Agarwal R. Evolving work routines: adaptive routinization of information technology in healthcare. Information Systems Research. 2011;22(3):565–585. [Google Scholar]
- Greenhalgh T. Role of routines in collaborative work in healthcare organisations. British Medical Journal. 2008;337:1269–1271. doi: 10.1136/bmj.a2448. [DOI] [PubMed] [Google Scholar]
- Hazlehurst B, Mcmullen C. Orienting frames and private routines: the role of cultural process in critical care safety. International Journal of Medical Informatics. 2007;76(1):129–135. doi: 10.1016/j.ijmedinf.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Howard-Grenville JA. The persistence of flexible organizational routines: the role of agency and organizational context. Organization Science. 2005;16(6):618–636. [Google Scholar]
- Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203. doi: 10.1001/jama.293.10.1197. [DOI] [PubMed] [Google Scholar]
- Latour B. The powers of association. In: Law J, editor. Power Action and Belief A New Sociology of Knowledge? Routledge & Kegan Paul; London: 1986. [Google Scholar]
- Leonardi PM. When flexible routines meet flexible technologies: affordance, constraint, and the imbrication of human and material agencies. MIS Quarterly. 2011;35(1):147–167. [Google Scholar]
- Leonardi PM, Barley SR. Materiality and change: challenges to building better theory about technology and organizing. Information and Organization. 2008;18(3):159–176. [Google Scholar]
- March JG, Simon HA. Organizations. Wiley; New York: 1958. [Google Scholar]
- Nelson RR, Winter SG. An Evolutionary Theory of Economic Change. Belknap Press; Cambridge, MA: 1982. [Google Scholar]
- Orlikowski WJ. Using technology and constituting structures: a practice lens for studying technology in organizations. Organization Science. 2000;11(4):404–428. [Google Scholar]
- Orlikowski WJ, Yates J, Okamura K, Fujimoto M. Shaping electronic communication – the metastructuring of technology in the context of use. Organization Science. 1995;6(4):423–444. [Google Scholar]
- Pentland BT. Grammatical models of organizational processes. Organization Science. 1995;6(5):541–556. [Google Scholar]
- Pentland BT, Feldman MS. Organizational routines as a unit of analysis. Industrial and Corporate Change. 2005;14(5):793–815. [Google Scholar]
- QSR-International. NVivo by QSR International [Online]. [WWW document] www.qsrinternational.com(accessed 12 October 2010)
- Ragin CC, Becker HS, editors. What is a Case? Exploring the Foundations of Social Inquiry. Cambridge University Press; Cambridge: 1992. [Google Scholar]
- Reddy M, Dourish P, Pratt W. Temporality in medical work: time also matters. Computer Supported Cooperative Work. 2006;15(1):29–53. [Google Scholar]
- Strauss AL, Fagerhaugh S, Suczek B, Wieder C. Organization of Medical Work. University of Chicago Press; Chicago, IL: 1985. Social. [Google Scholar]
- Weiner JP, Kfuri T, Chan K, Fowles JB. ‘e-Iatrogenesis’: the most critical unintended consequence of CPOE and other HIT. Journal of the American Medical Informatics Association. 2007;14(3):387–388. doi: 10.1197/jamia.M2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y. Artifacts and collaborative work in healthcare: methodological, theoretical, and technological implications of the tangible. Journal of Biomedical Informatics. 2005;38(1):26–33. doi: 10.1016/j.jbi.2004.11.004. [DOI] [PubMed] [Google Scholar]
- Yin RK. Case Study Research: Design and Methods. Sage Publications; Thousand Oaks, CA: 2003. [Google Scholar]


