Case presentation: A 68 year-old man presents to his primary care physician describing an irregular and rapid heartbeat that has awakened him from sleep. The patient has a blood pressure of 148/92 mm Hg, body mass index (BMI) of 35.5 kg/m2, and history of diabetes that has been managed with oral glycemics On auscultation, the physician appreciates occasional irregular beats without a cardiac murmur. An electrocardiogram shows normal sinus rhythm with a PR interval of 180 ms and infrequent premature atrial contractions (PACs). A 24-hour Holter monitor identifies intermittent PACs and demonstrates paroxysmal atrial fibrillation (AF) that is primarily nocturnal. The patient’s inquires about (1) how obesity has contributed towards his developing AF, and (2) whether weight loss would ameliorate risk of AF or burden of the arrhythmia.
Background: Obesity is a well-described risk factor for atrial fibrillation
Obesity is a profound public health concern with increasing prevalence. AF is the most commonly encountered clinical arrhythmia and results in multiple adverse sequelae that include stroke, heart failure, cognitive decline, dementia, diminished quality of life, and death.1 In community- and population-based cohort studies, obesity has consistently emerged as a risk factor for AF. Compared to normal-weight referents, obese individuals have up to a 2.4-fold increased AF risk.2 In cardiothoracic surgery cohorts, the post-operative risk of AF ranges from a 1.4- to 2.4-fold increased risk compared to non-obese referents.3, 4 The risk of AF increases progressively with rising BMI. In a large cardiothoracic surgery series, individuals at the extreme of BMI (≥40.0 kg/m2) had a 2.3-fold increased post-operative AF risk, compared to a 1.2-fold increased risk in the overweight (BMI 25–30 kg/m2).4 An observational cohort from the Mayo Clinic similarly showed increased likelihood of transitioning from paroxysmal to permanent AF with progressive increase in BMI.5
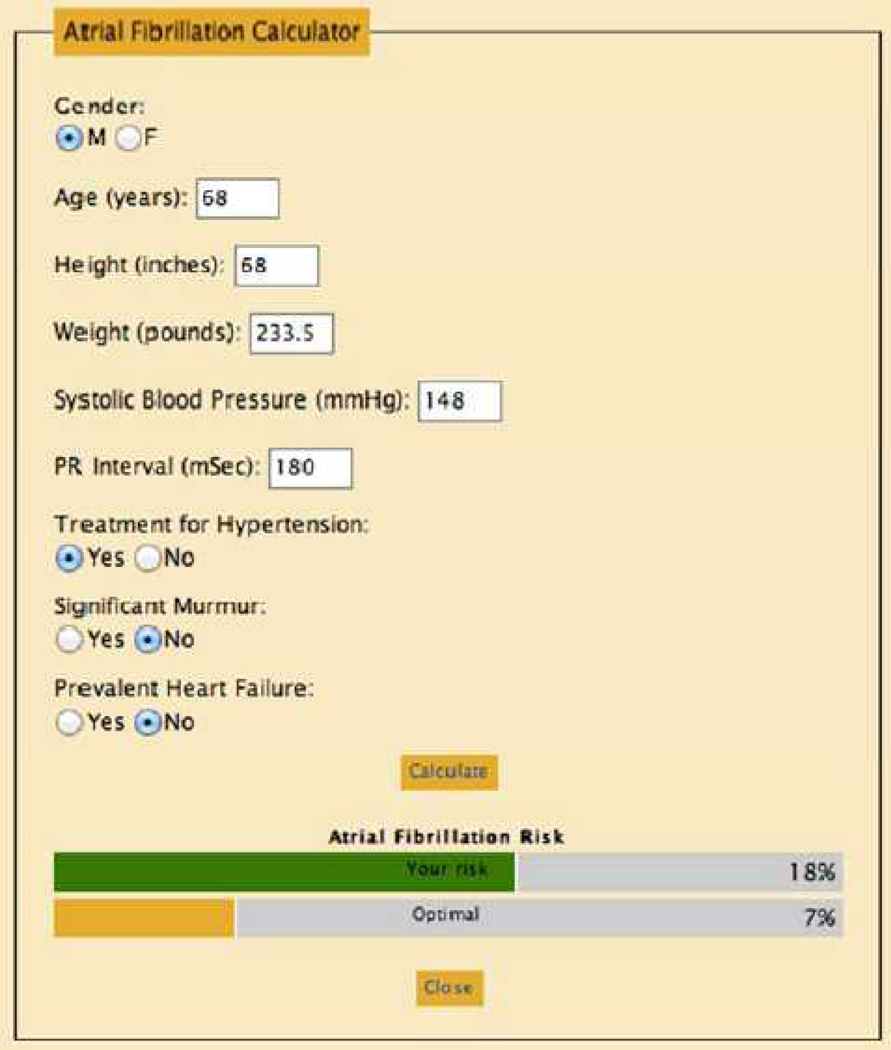
BMI has emerged as relevant to longitudinal AF risk in multiple AF risk scores developed in community-based cohorts.6–8 Two of the risk scores were conducted in biracial cohorts, thereby enhancing their generalizability.7, 8 Figure 1 presents the Framingham Heart Study 10-year AF risk calculator for the patient described in the case presentation (available on-line at http://www.framinghamheartstudy.org/risk/atrial.html). The patient’s 10-year AF risk is calculated as 18%. In addition to systemic adiposity, regional adipose tissue deposition, specifically epicardial adipose tissue volume measured by CT or MRI, has emerged as a potent risk factor for AF. The effect of epicardial fat is independent of BMI and other known risk factors for AF.9 The epidemiologic data summarized here consistently indicate that obesity is associated with substantial risk for development of AF. A meta-analysis reported that obese individuals have a 49% increased risk of AF compared to non-obese.10 Of paramount importance is that obesity is one of the very few modifiable risk factors for AF that have been identified.
Figure 1.
Application of the Framingham Heart Study 10-year Atrial Fibrillation Risk calculator. The patient has a 10-year risk of developing AF of 18%. Of note, body mass index is only one of two modifiable risk factors identified by the risk score. The calculator may be accessed at: http://www.framinghamheartstudy.org/risk/atrial.html.
Future research is essential to understand better the epidemiologic associations of obesity and AF. Table 1 provides a summary of future directions in obesity and AF research.
Table.
Future directions and potential research in the investigation of obesity and AF.
| Domain | Directions and potential research questions |
|---|---|
| Epidemiology and phenotype modeling | Diversity of adiposity phenotypes (DEXA, skin caliper measurement, obesity subphenotypes, CT imaging) |
| Trajectories of obesity exposure and “obesity-years” | |
| Childhood obesity and early-age weight with longitudinal (i.e. multi-decade) AF risk | |
| Effect modification and augmented risk from comorbidities | |
| Cohort studies and secondary data analysis | Weight loss, i.e. bariatric cohorts, and AF risk assessment |
| Effect of weight loss on epicardial adiposity and AF risk | |
| Atrial and cardiovascular remodeling | Community- and population-based studies of atrial remodeling and simultaneous biomarker assessment (i.e. adipokines, inflammatory markers) |
| Regression (reverse remodeling) following bariatric intervention or weight loss | |
| Regression (reverse remodeling) with risk factor amelioration (e.g. OSA treatment) | |
| Genetics and genomics | Gene-environment interaction relating obesity-years, genetic expression, and AF risk |
| Relation of microRNA expression in AF to obesity-years |
AF indicates atrial fibrillation; DEXA, dual-energy X-ray absorptiometry; CT, computerized tomography; OSA, obstructive sleep apnea.
Obesity and AF: shared risk factors, shared intermediates
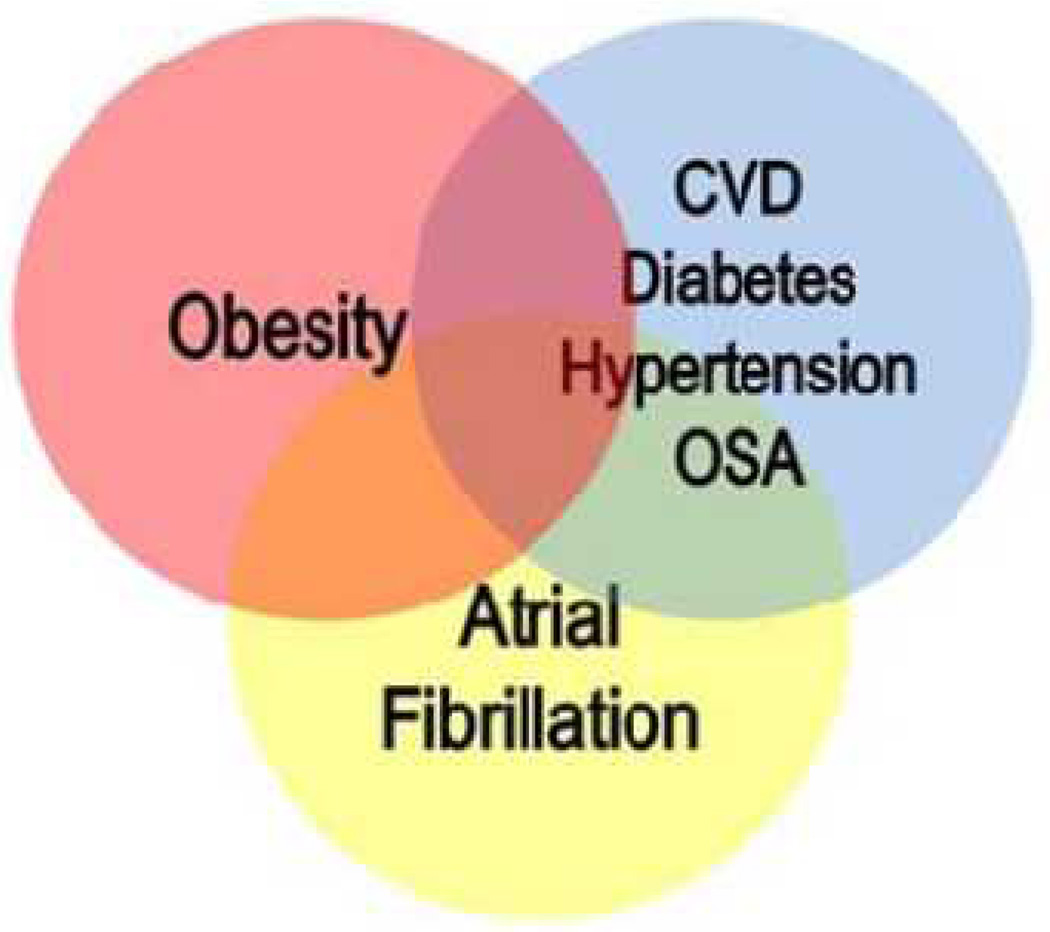
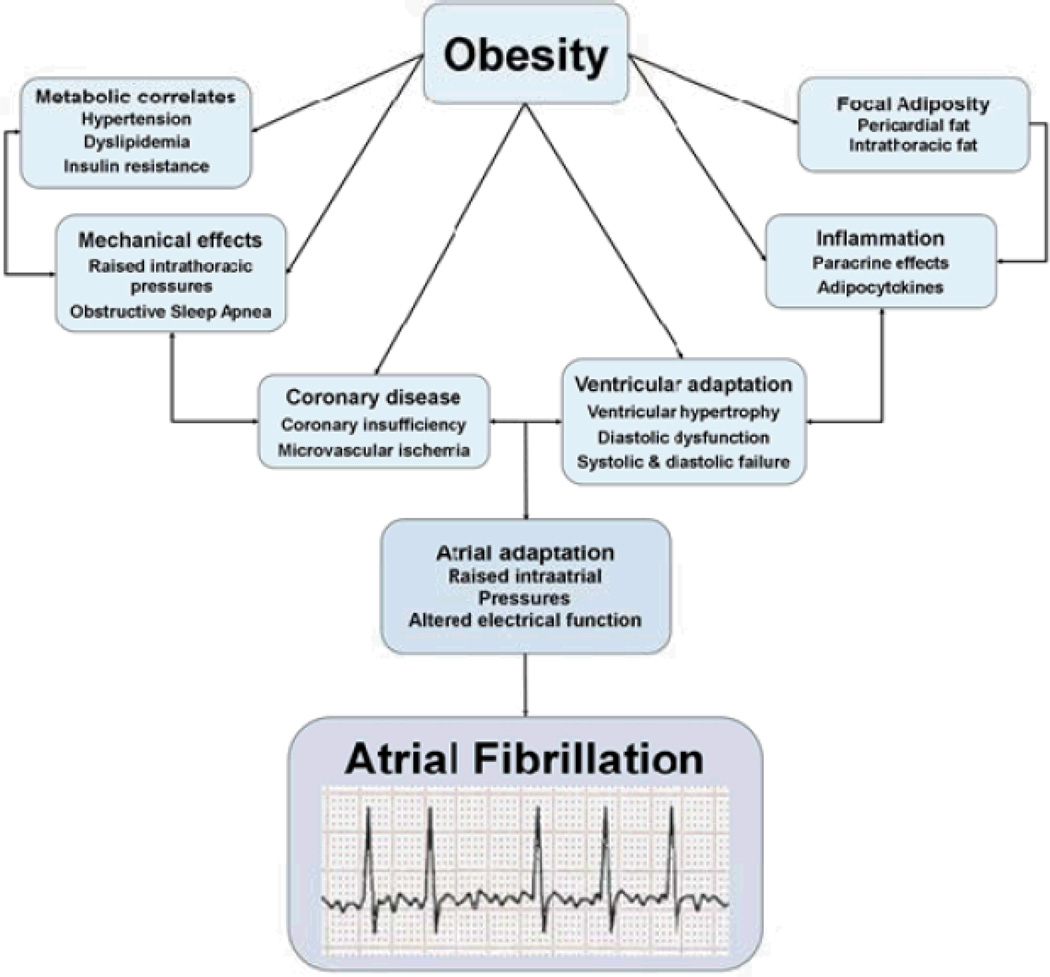
Obesity and metabolic disease have multifactorial contributions toward AF risk. Figure 2 describes the overlapping relation between obesity, AF, and their common, foremost clinical correlates. Hypertension, strongly associated with obesity, is a well-described risk factor for AF; the incidence of hypertension increases alongside body weight and progressive rise in obesity class. Cardiovascular disease, comprising both macro- and microvascular ischemia, is a second, highly prevalent intermediate linking obesity and AF.. Central obesity comprises part of the metabolic syndrome, and in a community-based cohort, additional metabolic syndrome components increased the 10-year risk of incident AF to 4-fold when all 5 were present.11 Obstructive sleep apnea (OSA) merits increased emphasis for its association with nocturnal arrhythmias and being a highly prevalent comorbidity of obesity. In obese cohorts the prevalence of OSA extends up to 90%.12 OSA promotes sympathetic overactivity, vascular inflammation, and heart rate variability and has associations with hypertension and metabolic risk factors. Figure 3 includes intermediate steps in order to suggest the multiple clinical pathways through which obesity may result in AF pathogenesis.
Figure 2.
Venn diagram demonstrating overlap between obesity, atrial fibrillation and selected clinical correlates. The clinical correlates are the chief clinical associations shared by obesity and atrial fibrillation. CVD indicates cardiovascular disease; OSA, obstructive sleep apnea.
Figure 3.
The figure describes the predominant intermediate mechanisms, including clinical pathways and atrial remodeling, that bridge obesity and AF.
Back to Our Case
The patient instituted the DASH diet and received medical clearance for exercise. Over the next 2 years, he was able to reduce his BMI to 32.5 kg/m2. He employed antiobesity agents (e.g., tetrahydrolipstatin, or Orlistat) that work to reduce fat absorption in the gut. His history of AF precluded use of phentermine, an appetite suppressant. He developed pronounced dyspnea on exertion, and repeated ECGs and another Holter now showed persistent AF. The patient’s CHA2DS2-VASc score was calculated as 3 (1 point each for history of hypertension, diabetes, and age 65–74), and he was started on long-term oral anticoagulation in addition to continuing a daily aspiring. He underwent an elective cardioversion and was started on sotalol with appropriate monitoring for QT interval prolongation and bradyarrhythmia.
Obesity and cardiovascular remodeling
Cardiovascular remodeling secondary to obesity is a critical focus of investigation, identifying intermediate steps in the pathway between exposure and outcome. Atrial remodeling may be summarized as a heterogeneous process characterized by disruption of atrial electrical integrity secondary to long-term clinical exposures. Alterations in atrial electrophysiologic function and concomitant remodeling are maladaptive responses to the resulting metabolic, hemodynamic, and ischemic stresses. The cumulative results are electrical disturbances, structural modification, and inflammation that promote interstitial atrial fibrosis and yield a proarrhythmic substrate. Obesity is associated with a 2.4-fold 10-year risk of echocardiographic left atrial (LA) volumetric enlargement.13 Ventricular diastolic function further impacts atrial integrity. Obesity and hypertension may yield ventricular hypertrophy, which in turn alters diastolic function, raising atrial pressures and promoting atrial remodeling. The up-stream mediators of atrial remodeling in from obesity are shown in Figure 3.
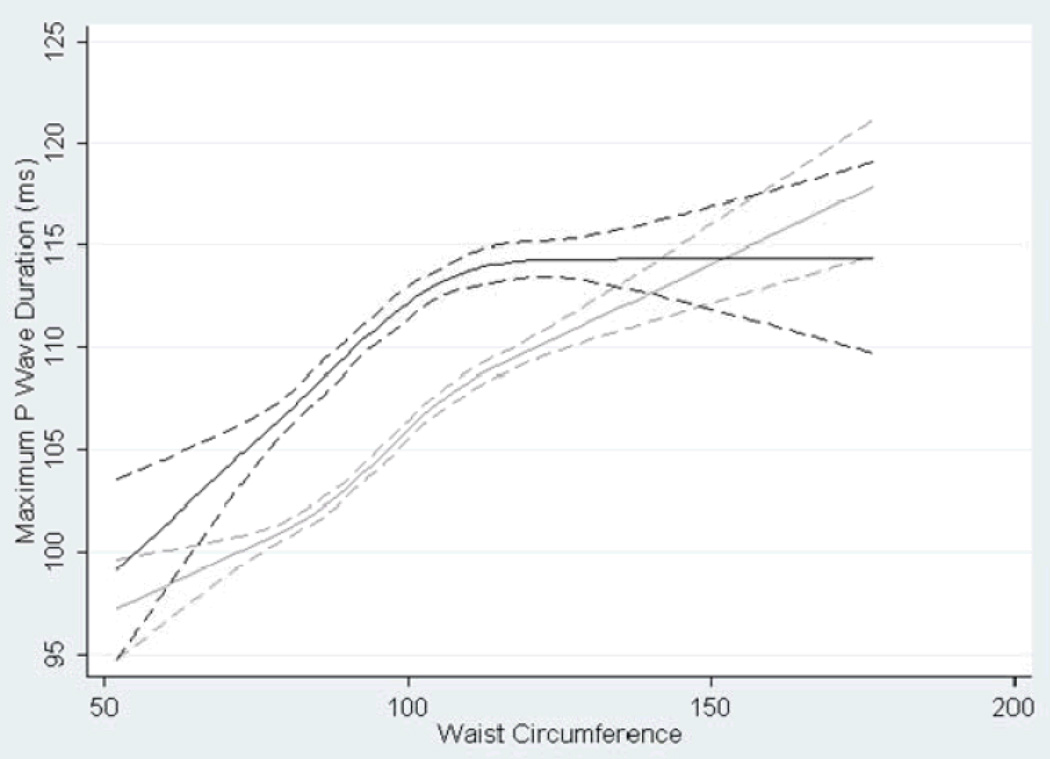
P wave indices (PWI) are derived from the surface ECG and are vectorcardiographic measurements of P wave morphology, duration, and amplitude. They provide a low-cost, reproducible measurement of atrial electrical function. PWI are progressively altered by obesity and waist circumference. Figure 4 shows the cubic restricted splines that graphically display the relation between BMI and maximum P wave duration as continuous variables in a large, biracial cohort (n=14,433).14 A single-center, small-sized (n=63) study reported significant differences in atrial and pulmonary vein electrophysiology between obese and non-obese individuals.15 Obese individuals had shorter atrial and pulmonary vein refractory periods than non-obese individuals, suggesting a proarrhythmic substrate.
Figure 4.
Cubic splines relating waist circumference and P wave duration in the Atherosclerosis Risk in Communities Study by racial strata. The solid line represents Black participants and the dotted line White participants. Reproduced with permission from Magnani et al. P wave indices, Obesity and the Metabolic Syndrome: the Atherosclerosis Risk in Communities Study. Obesity. 2012;20666-672.14
Biomarkers and intermediate pathways relating obesity and AF
Inflammatory biomarkers, increased in obesity, are an alternative avenue for relating obesity and AF pathogenesis.. C-reactive protein has likely been best studied and characterized for its relation to AF. Pericardial fat, overlying atrial tissue, has received attention for its relation to obesity, adipocytokine expression, and correlation with inflammatory markers.
Genomics of Obesity and AF
We are at the frontier of integrating genomics in examining the relation of obesity and AF.
Case Conclusion
The patient, now aged 70, regained his prior weight. He complained of continued dyspnea and daytime drowsiness. He underwent polysomnography that diagnosed OSA and during which he was in continuous AF. Anticoagulation for stroke prevention was continued. He was taken off sotalol, given his persistent AF while on the medication, and referred for electrophysiologic ablation to treat symptomatic AF.
Acknowledgments
None
Funding sources:
Dr. Magnani is supported by AHA award 09FTF2190028.
Dr. Hylek is supported by NIH R01NS070307.
Dr. Apovian is supported by NIH P30DK046200.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures:
Jared W Magnani – None
Elaine M Hylek – None
Caroline Apovian – Dr. Apovian has participated on advisory boards for Amylin Pharmaceuticals, Orexigen Therapeutics, Merck & Co., Inc., Johnson and Johnson, Arena Pharmaceuticals, Nutrisystem, Inc., Zafgen Inc. and sanofi-aventis US LLC, and has received research funding from Eli Lilly & Co., Amylin Pharmaceuticals, Pfizer, Inc., sanofi-aventis US LLC, Orexigen Therapeutics, MetaProteomics LLC, and the Dr. Robert C. and Veronica Atkins Foundation.
References
- 1.Magnani JW, Rienstra M, Lin H, Sinner MF, Lubitz SA, McManus DD, Dupuis J, Ellinor PT, Benjamin EJ. Atrial fibrillation: Current knowledge and future directions in epidemiology and genomics. Circulation. 2011;124:1982–1993. doi: 10.1161/CIRCULATIONAHA.111.039677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frost L, Hune LJ, Vestergaard P. Overweight and obesity as risk factors for atrial fibrillation or flutter: The danish diet, cancer, and health study. The American Journal of Medicine. 2005;118:489–495. doi: 10.1016/j.amjmed.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 3.Echahidi N, Mohty D, Pibarot P, Despres JP, O'Hara G, Champagne J, Philippon F, Daleau P, Voisine P, Mathieu P. Obesity and metabolic syndrome are independent risk factors for atrial fibrillation after coronary artery bypass graft surgery. Circulation. 2007;116:I213–I219. doi: 10.1161/CIRCULATIONAHA.106.681304. [DOI] [PubMed] [Google Scholar]
- 4.Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Obesity and risk of new-onset atrial fibrillation after cardiac surgery. Circulation. 2005;112:3247–3255. doi: 10.1161/CIRCULATIONAHA.105.553743. [DOI] [PubMed] [Google Scholar]
- 5.Tsang TS, Barnes ME, Miyasaka Y, Cha SS, Bailey KR, Verzosa GC, Seward JB, Gersh BJ. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: A longitudinal cohort study of 21 years. European Heart Journal. 2008;29:2227–2233. doi: 10.1093/eurheartj/ehn324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D'Agostino RB, Sr, Newton-Cheh C, Yamamoto JF, Magnani JW, Tadros TM, Kannel WB, Wang TJ, Ellinor PT, Wolf PA, Vasan RS, Benjamin EJ. Development of a risk score for atrial fibrillation (framingham heart study): A community-based cohort study. Lancet. 2009;373:739–745. doi: 10.1016/S0140-6736(09)60443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chamberlain AM, Agarwal SK, Folsom AR, Soliman EZ, Chambless LE, Crow R, Ambrose M, Alonso A. A clinical risk score for atrial fibrillation in a biracial prospective cohort (from the atherosclerosis risk in communities [aric] study) The American Journal of Cardiology. 2011;107:85–91. doi: 10.1016/j.amjcard.2010.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schnabel RB, Aspelund T, Li G, Sullivan LM, Suchy-Dicey A, Harris TB, Pencina MJ, D'Agostino RB, Sr, Levy D, Kannel WB, Wang TJ, Kronmal RA, Wolf PA, Burke GL, Launer LJ, Vasan RS, Psaty BM, Benjamin EJ, Gudnason V, Heckbert SR. Validation of an atrial fibrillation risk algorithm in whites and african americans. Arch Intern Med. 2010;170:1909–1917. doi: 10.1001/archinternmed.2010.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Chekakie MO, Welles CC, Metoyer R, Ibrahim A, Shapira AR, Cytron J, Santucci P, Wilber DJ, Akar JG. Pericardial fat is independently associated with human atrial fibrillation. Journal of the American College of Cardiology. 2010;56:784–788. doi: 10.1016/j.jacc.2010.03.071. [DOI] [PubMed] [Google Scholar]
- 10.Wanahita N, Messerli FH, Bangalore S, Gami AS, Somers VK, Steinberg JS. Atrial fibrillation and obesity--results of a meta-analysis. American Heart Journal. 2008;155:310–315. doi: 10.1016/j.ahj.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Chamberlain AM, Agarwal SK, Ambrose M, Folsom AR, Soliman EZ, Alonso A. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the atherosclerosis risk in communities (aric) study. American Heart Journal. 2010;159:850–856. doi: 10.1016/j.ahj.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frey WC, Pilcher J. Obstructive sleep-related breathing disorders in patients evaluated for bariatric surgery. Obes Surg. 2003;13:676–683. doi: 10.1381/096089203322509228. [DOI] [PubMed] [Google Scholar]
- 13.Stritzke J, Markus MR, Duderstadt S, Lieb W, Luchner A, Doring A, Keil U, Hense HW, Schunkert H. The aging process of the heart: Obesity is the main risk factor for left atrial enlargement during aging the monica/kora (monitoring of trends and determinations in cardiovascular disease/cooperative research in the region of augsburg) study. Journal of the American College of Cardiology. 2009;54:1982–1989. doi: 10.1016/j.jacc.2009.07.034. [DOI] [PubMed] [Google Scholar]
- 14.Magnani JW, Lopez FL, Soliman EZ, Maclehose RF, Crow RS, Alonso A. P wave indices, obesity, and the metabolic syndrome: The atherosclerosis risk in communities study. Obesity (Silver Spring) 2012;20:666–672. doi: 10.1038/oby.2011.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munger TM, Dong YX, Masaki M, Oh JK, Mankad SV, Borlaug BA, Asirvatham SJ, Shen WK, Lee HC, Bielinski SJ, Hodge DO, Herges RM, Buescher TL, Wu JH, Ma C, Zhang Y, Chen PS, Packer DL, Cha YM. Electrophysiological and hemodynamic characteristics associated with obesity in patients with atrial fibrillation. Journal of the American College of Cardiology. 2012;60:851–860. doi: 10.1016/j.jacc.2012.03.042. [DOI] [PubMed] [Google Scholar]