Abstract
Antimicrobial proteins influence intestinal microbial ecology and limit proliferation of pathogens, yet the regulation of their expression has only been partially elucidated. Here, we have identified a putative pathway involving epithelial cells and intestinal intraepithelial lymphocytes (iIELs) that leads to antimicrobial protein (AMP) production by Paneth cells. Mice lacking γδ iIELs (TCRδ-/-) express significantly reduced levels of the AMP angiogenin 4 (Ang4). These mice were also unable to up-regulate Ang4 production following oral challenge by Salmonella, leading to higher levels of mucosal invasion compared to their wild type counterparts during the first 2 hours post-challenge. The transfer of γδ iIELs from wild type (WT) mice to TCRδ-/- mice restored Ang4 production and Salmonella invasion levels were reduced to those obtained in WT mice. The ability to restore Ang4 production in TCRδ-/- mice was shown to be restricted to γδ iIELs expressing Vγ7-encoded TCRs. Using a novel intestinal crypt co-culture system we identified a putative pathway of Ang4 production initiated by exposure to Salmonella, intestinal commensals or microbial antigens that induced intestinal epithelial cells to produce cytokines including IL‑23 in a TLR-mediated manner. Exposure of TCR-Vγ7+ γδ iIELs to IL-23 promoted IL‑22 production, which triggered Paneth cells to secrete Ang4. These findings identify a novel role for γδ iIELs in mucosal defence through sensing immediate epithelial cell cytokine responses and influencing AMP production. This in turn can contribute to the maintenance of intestinal microbial homeostasis and epithelial barrier function, and limit pathogen invasion.
Introduction
The gastrointestinal (GI) tract is a focal point of microbial/host interactions, accommodating the vast resident microbiota, yet protecting against invasion by microbial pathogens. Protection of the intestinal mucosa is multilayered comprising physical, chemical and immunological mediators that collectively contribute to the development of innate immune responses and maintenance of intestinal homeostasis [1]. Prominent among chemical defences in the small intestine are antimicrobial proteins (AMPs) such as defensins (cryptdins in mice), lysozyme and Angiogenin 4 (Ang4) that are produced by Paneth cells residing at the base of the crypts. AMPs have a broad activity against Gram‑positive and ‑negative bacteria, protozoa and fungi [2,3]. AMP-deficient mice are more susceptible to bacterial infection [4], and over-expression of human defensins in transgenic mice increases resistance to pathogen invasion [3]. AMPs are therefore assumed to play a central role in preventing pathogen invasion and constraining proliferation of commensal microorganisms in close vicinity to the epithelium [5]. Since only few direct molecular pathways of microbe-induced AMP production have been defined, the possibility exists that other locally produced factors influence Paneth cell AMP production. Potential sources of these factors and cytokines are the populations of mucosa-associated immune cells including intestinal intraepithelial lymphocytes (iIELs) [6], B‑1 B cells [7], mucosa-associated invariant T (MAIT) cells [8], and various innate lymphoid cells (e.g. NK cells, lymphoid tissue inducer cells and nuocytes) distinguished on the basis of their functional characteristics and cytokine profile [9,10]. Of these immune cell populations, iIELs are the closest populations of immune cells to the host-lumen interface, residing between the basolateral faces of adjacent epithelial cells, making them ideally suited to interact with epithelial cells and influence their response to microbial challenge [11,12].
iIELs are found in the majority of mammals and birds [12-16] and are enriched in lymphocytes expressing the γδ T cell receptor (TCR). In most inbred strains of mice T cells expressing Vγ7 or Vγ1 encoded TCRs make up to 90% of γδ iIELs, among which Vγ7+ cells comprises the largest population [17,18]. The biological function of iIELs is still unclear although studies carried out primarily in mice demonstrating their inherent cytotoxicity [19], their capacity to produce pro-inflammatory cytokines, epithelial cell growth factors and AMPs [20], their involvement in epithelial restitution [21] and maintenance of epithelial tight junction complexes [22] suggest they play a central role in intestinal defence [21,23-25].
Here we have investigated the role that γδ iIELs play in the immediate response to oral infectious challenge and in particular, in influencing Paneth cell production of AMPs.
Study rationale
γδ iIELs dominate iIEL populations in mammals [12,13,15] and their absence or depletion in mice is associated with increased susceptibility to infection by enteric pathogens [26,27]. Here we tested the hypothesis that γδ iIELs contribute to gut barrier functions by rapidly influencing local AMP production in response to microbial challenge using Salmonella enterica serovar Typhimurium as a model bacterium to trigger host innate intestinal antimicrobial responses. The approach was to capture events occurring in vivo immediately and within 2 hours of oral microbial challenge as iIELs are fast‑acting cells [28,29], and Paneth cells release pre-formed antimicrobial proteins from their granules within minutes of exposure to appropriate inflammatory stimuli [2].
Materials and Methods
Mice and infections
Six to ten week old C57BL/6J (Harlan Labs), C57BL/6J-TCRδ-/- (JAX Laboratories) and C57BL/6J-TCRVγ1-/- [30] were housed in a conventional animal facility at the Universities of Leeds and East Anglia. Mice were challenged using isolated intestinal loops [31] or by oral gavage with 4x108 of viable or killed invasive WT SL1344 [32] and non-invasive (ΔSPI-1) Salmonella enterica serovar Typhimurium (S. Typhimurium) SL1344 [33] or 4x108 invasive Salmonella expressing a luciferase (lux) reporter gene (SL1344-Tn5lux) [34]. Bacterial CFU in the intestinal mucosa was determined after PBS rinse of intestinal tissue by plating serial dilutions of tissue homogenates on BHI, and LB (Oxoid) agar plates. In the case of SL1344‑Tn5lux, luminescent bacterial colonies were also counted (IVIS 100, Xenogen Corp.).
Ethics Statement
Protocols for all the animal experiments included in this manuscript were conducted in full accordance with the Animal Scientific Procedures Act 1986 under Home Office approval. Mice were euthanized by Schedule One approved methods, and all efforts were made to minimize animal suffering.
iIELs culture
iIELs were isolated from Peyer’s patch-excised small intestines [35]. Highly purified preparations of Vγ7+ and Vγ7- iIELs were obtained by staining iIELs from WT mice with F(ab’)2 fragments of anti-TCRδ (clone GL3), CD3 (H57-597) and ‑TCR-Vγ7 (F2.67) antibodies and sorting on an inFlux High Speed Cell Sorter (Becton Dickinson); isolated cells were routinely >98% TCRγδ+ and >95% viable. iIEL-conditioned medium was obtained by incubating 3x104 iIELs with phorbol myristate acetate (PMA) and ionomycin (Io) or anti-CD3 (UCHT-1, Becton Dickinson) and anti-CD28 (CD28.2, Becton Dickinson) antibodies at 37°C in 5% CO2 for 16h. For adoptive transfer, 5-8 x105 FACS‑isolated iIELs were injected i.v. into C57BL/6-TCRδ-/- mice. Five to six weeks later these mice were orally challenged with S. Typhimurium (SL1344) as described above. Two hours later intestines were removed for immunohistochemical analysis and/or bacterial counts. γδ iIEL reconstitution was verified by staining sections of intestine with anti-CD3, -TCRγδ and ‑TCRVγ7 antibodies and counting the number of stained cells per villus in at least 30 villi per section on a minimum of 5 sections per tissue sample from ≥4 mice.
Intestinal crypt and epithelial cell culture
Crypts were isolated from fragments of small intestine by sequential incubation with 30mM EDTA, 10% FCS (Biosera) and 1mM DTT (adapted from [2,36]) and identified by their morphology, phloxine-tartrazine staining, expression of Ki-67 and lack of alkaline phosphatase activity. 500 to 2x104 crypts were cultured in iPIPES (10mM PIPES pH7.4 containing 137mM NaCl) with or without secretory stimuli. Stimuli (10μM CCh, 103 Salmonella, 100ng/ml IL-22) were added for 30 min at 37°C. Crypt exudates were obtained by incubating crypts in iPIPES at 37°C, 5% CO2 for 3h followed by centrifugation for 5 min at 150g, and used in killing assays. The average volume of a small intestinal crypt of 120μm in height was calculated to be 13pl using the method of Ayabe [2]. Monolayer cultures of intestinal epithelial cells were obtained as described previously [37]. For co-culture with iIELs in iIEL-conditioned medium and recombinant cytokines, crypts were cultured at 37°C for 4h in complete tissue culture media. In some experiments, anti-IL‑22 neutralising antibodies (1.5μg/ml) or isotype control antibodies (1.5μg/ml) were added. Supernatants were collected and stored at -20°C and cells were harvested for mRNA extraction. Culture supernatants were analysed for lysozyme activity using the EnzChek lysozyme assay kit (Invitrogen).
Polarised monolayers of intestinal epithelial cells were challenged with 1-5x106 CFU wild type or specific mutants of the S. Typhimurium strain SL1344 [31] for up to 16h. For challenge with microbial antigens, cells were incubated with 10μg/ml peptidoglycan (S. aureus), 1μg/ml lipopolysaccharide (S. Typhimurium), 1μg/ml muramyl dipeptide or 500ng/ml CpG for up to 16h in 5% CO2 at 37°C. Supernatants were analysed for protein production by ELISA and cell pellets for cytokine/Ang4 mRNA expression by qPCR. Lamina propria cells were isolated on ice from Peyer’s patch‑excised and longitudinally cut small intestines of WT mice. The epithelial layer was removed by incubation at 37°C for 20 min in RPMI containing 10% FBS, 5mM EDTA and 1mM DTT. Remaining tissue was washed in RPMI and then digested at 37°C for 1h under agitation (200rpm/min) in RPMI containing 10% FBS, 2mg/ml Collagenase D and 1mg/ml Dispase. Lamina propria cells were further enriched by Percoll gradient (40-70%) centrifugation with cell purity confirmed by staining with anti‑CD45 antibodies (FITC/PE‑conjugated (Ly-5), e‑Biosciences Ltd). In vitro Salmonella infection was performed using a multiplicity of infection of 10:1 (10 bacterial cell per lamina propria cell). At the end of the experiment, cells were harvested and RNA was purified with Tri‑reagent, reverse transcribed and analysed for IL‑23 mRNA expression by qPCR.
Cell line culture
In vitro control experiments were carried out on the mouse trans‑immortalised cell line of intestine epithelial cells, m‑ICc12 [38] and on the mouse tumour‑derived macrophages, RAW264.7 (ATCC® TIB71™), cultivated to a density of 1 and 6-8x106 cells, respectively , in T25 flasks and infected with S. Typhimurium SL1344 at a multiplicity of infection of 10:1 and 100:1, respectively [21,39,40] or with gut commensal isolates grown overnight and used at a multiplicity of infection of 10:1. The murine commensals tested were Escherichia coli, Enterococcus gallinarum, both isolated from the caecum of C57BL/6J mice (IFR GH collection strains GH260 and GH76 GenBank JN412816, respectively), and human gut isolates Bifidobacterium longum (DSM20219) and Bacteroides thetaiotaomicron VPI‑5482 (DMSZ collection). Epithelial cells were harvested and RNA purified and processed as mentioned above. For in vitro TLR‑mediated challenge with Salmonella, 1x106 epithelial cells were incubated with 1‑5x106 CFU wild type or specific mutants of the Salmonella strain SL1344 [31] for up to 16 h. For challenge with microbial antigens intestinal epithelial cells were incubated with 10μg/ml peptidoglycan (S. aureus), 1μg/ml lipopolysaccharide (S. Typhimurium), 1μg/ml muramyl dipeptide or 500ng/ml CpG for up to 16 h in 5% CO2 at 37°C. Supernatants were analysed for protein production by ELISA, and cell pellets for cytokine/Ang4 mRNA expression by qPCR.
Transmission electron microscopy
Salmonella cells were harvested, after treatment in 3% glutaraldehyde (Agar Scientific, UK), in 0.1M cacodylate buffer (pH 7.2) for 3h, washed three times in 0.1M cacodylate buffer (pH 7.2) and centrifuged. The cell pellets were embedded in molten 2% low-melting-point agarose (TypeVII, Sigma) that were sectioned, fixed in 2% aqueous osmium tetroxide for 2h then dehydrated three times through an ethanol series (10-100%). Samples were immersed in 1:2 mix of LR White medium grade resin (London Resin Company Ltd) and 100% ethanol for 18h followed by sequential 6h impregnation in 1:1 and a 2:1 mix of LR White resin and 100% ethanol. Samples were then bathed three times for 6h in 100% resin. Resin blocks from each sample were put into individual gelatine capsules with fresh resin and polymerised for 18h at 60°C. Ninety nm thick sections were cut using an ultramicrotome (Ultracut E, Reichert-Jung) with a glass knife, collected on film/carbon coated copper grids, and stained sequentially with uranyl acetate (saturated in 50% ethanol) and Reynold’s lead citrate. Sections were examined and imaged in a FEI Tecnai G2 20 Twin transmission electron microscope at 200kV.
Microarray
For microarray analysis RNA was isolated from small intestinal epithelium of wild type, TCRδ-/- and TCRVγ1-/- mice (n=4) at 2h post infection with Salmonella and processed using the GeneChip Mouse Genome 430A 2.0 array by the Univ. Manchester Microarray Core Facility according to standard protocols [41]. Gene expression values were normalised with gcRNA and anti-logged (average from 3 samples). Technical quality control was performed with dChip (V2005) (www.dchip.org; [42]) using the default settings. Background correction, quantile normalization, and gene expression analysis were performed using GCRMA in Bioconductor [43].
Ang4
Recombinant Ang4 was produced as described previously [44] with purity assessed by SDS-PAGE, N-terminal sequencing and biological activity determined by RNase activity [45]. Ang4 immunoblotting of total cellular lysates of small intestinal mucosa was carried out as described previously [44]. Membranes were stripped and re-probed with an anti-GAPDH antibody. Ang4 microbicidal activity was tested against 1x105‑1x106 cells of S. Typhimurium (SL1334wt) grown to mid-exponential phase, washed in PBS and incubated with increasing concentrations of recombinant Ang4 (10, 28, 64 and 280μM), or in exudates of isolated crypt in iPIPES buffer [2] prepared as above for 60 min at 37°C. Viable and culturable counts were determined by plating serial dilutions of test suspensions on LB agar plates and counting CFU 16h later.
Flow Cytometry
iIELs were stained with different combinations of CD3 (clone 1452C11), TCRγ (GL3) and TCRαβ (H57-597) (Caltag Laboratories), IL-23R antibodies (Imgenex) and, anti-TCR-Vγ7 (F2.67) and TCR-Vγ1 (2.11) antibodies provided by L. Lefrançois (Univ. Connecticut, CT) and P. Pereira (Institut Pasteur, Paris, France), respectively. For intracellular cytokine staining surface stained cells were fixed, permeabilised, stained with PE-conjugated anti-IL-22, IL-17A or isotype matched control antibodies (R&D Systems) and analysed on a FACSCalibur flow cytometer (Becton Dickinson). For the assessment of the in vitro impact of Ang4 on Salmonella cell membrane integrity, bacterial cells were treated with Ang4 or control PBS as described above, stained with PI (1μg/ml) and analysed on a Cytomics FC500 MPL flow cytometer (Beckman Coulter). Data analysis was performed using Flow Jo v7.6.2 software (Tree Star, Inc.).
ELISA
ELISAs were used to quantify IL-22 (R&D Systems) and IL-23 (Insight Biotechnology Ltd) in iIEL and epithelial cell conditioned medium. An Ang4 ELISA was developed using an antiserum (M20; Santa Cruz) for the capture antibody and a rabbit anti-Ang4 antiserum [44] for detection of bound Ang4. Recombinant Ang4 was used to establish a standard curve for determining concentrations in conditioned medium. Limit of detection was 100pg.
Immunohistochemistry
Paneth cells were visualised in paraffin-embedded sections of intestine by staining with phloxine-tartrazine. For localisation of Ang4 protein in Paneth cells, frozen sections of small intestine were stained with rabbit anti-mouse angiogenin antiserum [44] in combination with anti-lysozyme antibodies (Dako Cytomation) conjugated in house to Alexa‑Fluor 488 (Molecular Probes). Biotinylated goat anti-rabbit antibody (Caltag-Medsystems) and Texas Red streptavidin conjugate (Calbiochem) were used as secondary reagents. Sections were counterstained with DAPI. All sections were mounted and viewed using an inverted Zeiss Axiovert 200M microscope using Axiovision image analysis software (Imaging Associates Ltd).
ang4::luc reporter system
An 829bp fragment, containing sequences immediately upstream of the Ang4 transcription initiation start site was cloned into the luciferase reporter vector pGL3-basic (Promega, Southampton, UK) and used to transfect (Metafectene Pro; Biontex, Germany) confluent monolayers of m‑ICc12 cells. To control for differences in transfection efficiency, epithelial cells were co-transfected with a Renilla luciferase reporter gene containing plasmid (pRL-TK; Promega) in which expression is under the control of the Herpes simplex virus thymidine kinase (HSV-TK) promoter, which provides constitutive expression of the reporter gene in mammalian cells. Transfected cells were grown in 96-well plates with serum-free media in the absence or presence Salmonella or a range of concentrations of LPS or recombinant IL-22 for 4h after which luciferase activity was determined using the Dual-Glo Luciferase assay system (Promega) and Berthold Technologies Lumat LB 9507 luminometer. Results are expressed as the ratio of Ang4-reporter:Renilla luminescence, which was background-subtracted (non-transfected cells with Dual-Glo substrate) and where multiple plates were used, normalised to the ratio of control wells treated consistently on all plates.
qPCR
RNA was extracted from highly purified preparations (>97% cytokeratin+, <2% CD45+) of intestinal epithelial cells [46] or (~40% CD45+) LP cells using Tri-reagent and reverse transcribed using ImpromII reverse transcriptase (Promega). cDNA was used for Taqman real time quantitative PCR using optimised primer sets (Applied Biosystems) for Ang4 (Mm01315577_s1), IL-23/p19 (Mm00518984_m1), IL-22 (Mm00444241_m1) and the reference gene, β-actin (Mm00607939_sl). Data was analysed using the ∆∆Ct comparative method. Results were expressed as relative expression to the β-actin reference gene or compared with control samples as stated.
Statistical analysis
All data were assessed for normal distribution using a Shapiro-Wilk test. Kruskal Wallis with post Nemeyi-Damico-Wolfe-Dunns test and ANOVA with post-test of Bonferroni were also used when appropriate. For parametric data on experiments comparing two groups only, analysis was performed using a Student t‑test and for non-parametric data analysis was performed using Mann Whitney U tests using the Statistical Package for the Social Sciences software, SPSS (Surrey, UK). Statistical significance was taken as P<0.05.
Results
Mice lacking a subset of iIELs exhibit reduced levels of Ang4
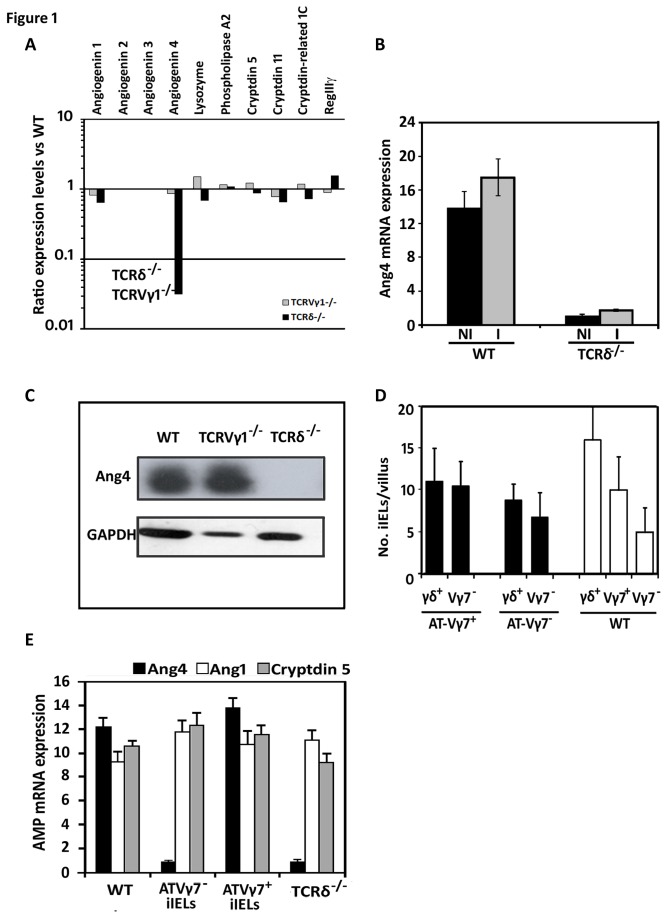
Global transcriptional changes in AMP expression associated with the absence of γδ iIELs were assessed by microarray-based mRNA profiling of the intestinal epithelium of naïve wild type (WT) mice, mice lacking all γδ T cells (TCRδ-/-) and mice lacking the TCR-Vγ1+‑subset of γδ T cells (TCRVγ1-/-) [30]. The profile of all but one AMP mRNA examined was comparable in all three strains of mice except for Ang4 that was expressed at significantly (p≤0.01) lower levels (up to ~30-fold) in naïve TCRδ-/- mice (Figure 1A and B). Of note, the levels of RegIIIγ mRNA were similar in all three strains of mice despite γδ iIELs being a source of this lectin [20]; indicative perhaps of biological redundancy and the ability of other RegIIIγ-producing cells compensating for the absence of γδ T cells under the experimental conditions used here. Reduced baseline levels of Ang4 protein in intestinal tissue of naive TCRδ-/- mice were confirmed by confocal microscopy (Figure S1) but were not associated with defective Paneth cell development or numbers of Paneth cells (Figure S1B). Murine Ang4 is a member of the pancreatic ribonuclease superfamily that possesses poor angiogenic but strong microbicidal activity [44,47]. Using immunoblotting no Ang4 protein was detected in extracts of TCRδ-/- intestinal mucosa (Figure 1C). Ang4 expression was further up‑regulated, although not significantly (p<0.06), in the small intestine of WT mice in response to oral infection by Salmonella. This increase did not occur in mice lacking γδ iIELs (Figure 1B). We have no evidence of altered Ang4 production in TCRδ-/- mice other than in the small intestine and in Paneth cells (unpublished observations).
Figure 1. γδ T cells modulate the production of Ang4.
(A) Expression levels of Paneth cell AMPs in the intestinal mucosa of naïve wild type (WT), TCRδ-/- and TCRVγ1‑/- mice as determined by RNA microarrays [82]. Levels are displayed as a ratio of the value obtained in TCRδ-/- or TCRVγ1-/- versus WT samples. (B) The level of Ang4 mRNA in the intestinal epithelium of TCRδ-/- and WT mice was determined both prior to (NI) and 2h post-oral challenge and infection (I) with Salmonella Typhimurium by qPCR. Data (mean±SEM) are expressed relative to levels of β‑actin mRNA and were collated from 6 RNA samples in each group. (C) Ang4 protein levels in the intestine of naïve WT, TCRδ‑/- and Vγ1‑/- mice determined by immunoblotting. Membranes were stripped and re-probed with an anti-GAPDH antibody. The results shown are representative of those obtained using 4-6 mice of each strain. (D) Number of γδ+ and TCR-Vγ7+ iIELs in intestinal tissue sections by immunohistochemistry 6 weeks after transfusion of γδ iIEL-deficient mice with TCR-Vγ7+ or TCR-Vγ7- iIELs. The data were collated (mean±SEM) by counting stained cells in at least 30 villi per section on a minimum of 5 sections per tissue from 4-6 mice. (E) Ang4 production is restored in iIEL-reconstituted TCRδ‑/- mice to WT levels after transfusion of Vγ7+ (ATVγ7+) iIELs. Levels of Ang4, Ang1 and cryptidin 5 mRNA were determined by qPCR in samples of small intestine obtained from WT, TCRδ-/- and TCRδ-/- mice 6 weeks post‑reconstitution with Vγ7+ or Vγ7- (ATVγ7-) iIELs and 2h after oral challenge with Salmonella. Data (mean±STD) are expressed relatively to levels of β‑actin mRNA and were collated from RNA samples of 4-6 mice of each group.
iIEL reconstitution experiments showed that Vγ7+ but not Vγ7- iIELs from WT donors were sufficient to restore mRNA levels of Ang4 to WT levels in TCRδ-/- recipients (Figure 1D and E). Of note, iIEL reconstitution did not affect the mRNA levels of other reference AMPs (Figure 1E) consistent with the RNA profiling data showing that the levels of other AMPs are unaffected by the absence of γδ T cells in TCRδ-/- mice (Figures 1A and S1C).
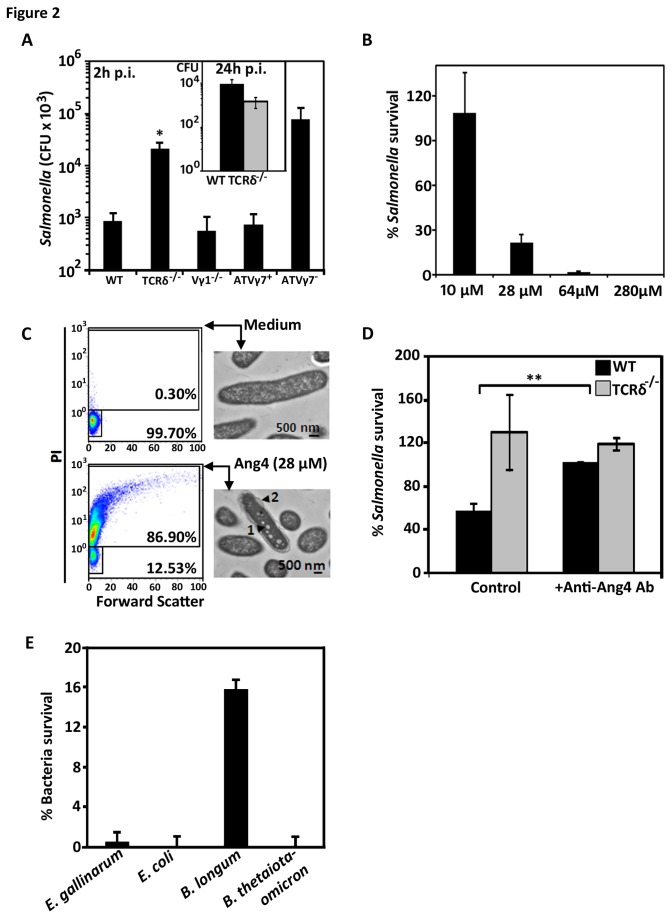
γδ iIELs are involved in the initial host response against Salmonella
As γδ (Vγ7+) iIELs are necessary for the production of Ang4 (Figure 1A, B and E), we determined whether these cells could impact upon pathogen invasion of the intestinal mucosa through the control of Ang4 production, as shown for the intestinal parasite Trichuris muris [48]. During the first 2h of infection, the intestinal tissue (ileum) of mice lacking γδ iIELs was colonised by approximately 30 times more Salmonella than WT mice (Figure 2A). However, in TCRδ-/- mice reconstituted with Vγ7+ iIELs the intracellular population levels of Salmonella were brought back to levels similar to those observed in WT mice (Figure 2A). By contrast, in TCRδ-/- mice reconstituted with Vγ7- iIELs the levels of Salmonella were comparable to those seen in non-manipulated TCRδ-/- mice (Figure 2A). Of note, at later time points post infection, differences in the levels of Salmonella associated with small intestinal tissue (Figure 2A Inset) between WT and TCRδ-/- mice were no longer apparent, consistent with recent findings [20] and suggesting that γδ iIELs act in the initiating of the host response.
Figure 2. Vγ7+ iIELs are involved in resisting Salmonella invasion.
(A) SL1344-Tnlux Salmonella population levels in the intestinal (ileal) mucosa of WT, TCRδ-/- and TCRVγ1-/- mice (n=10-12) and in TCRδ-/- mice reconstituted with either Vγ7+ iIELs (ATVγ7+) or Vγ7- iIELs (ATVγ7-) (n=5-6) 2h after oral challenge, (*p<0.01 comparing TCRδ-/- with WT group). Salmonella CFU were quantified as described in the Materials and Methods. Inset: CFU of Salmonella SL1344wt strain in ileal mucosa 24h post-oral challenge. (B) Survival of 1x105 S. Typhimurium SL1344 after 1h exposure to increasing amounts of recombinant Ang4, expressed as a percentage of population treated with PBS only. Data shown (mean±SEM) are representative of three independent experiments, each performed in triplicates. (C) Viability and cell membrane alteration of Ang4-treated Salmonella as assessed by PI staining and flow cytometry, and by transmission electron microscopy. The proportion of viable and dead bacteria after incubation with Ang4 or PBS is indicated by the % values shown in the quadrants. The TEM images are representative of 200‑300 Salmonella cells observed. The black arrowheads indicate regions of vesicle‑like structures (1) and blebbing of the outer membrane (2). (D) Survival of 1x105 CFU S. Typhimurium SL1344 exposed to freshly collected TCRδ-/- and WT crypt exudates in 10mM iPIPES (PIPES containing 137mM NaCl) in presence or absence of anti-Ang4 neutralising antibody (M20; Santa Cruz) (mean±SEM; **p≤0.005). Survival to Ang4 exposure was measured relative to that in non-treated exudates. (E) Survival of 1x105 Enterococcus gallinarum, Escherichia coli, Bifidobacterium longum and Bacteroides thetaiotaomicron commensal bacteria after 1h exposure to 28μM of recombinant Ang4, expressed as a percentage of population treated with PBS only. Data shown are the mean±SEM of three independent experiments.
Ang4 possesses bactericidal activity against the entero-pathogens L. monocytogenes and E. faecalis [44]. Using the same protocol as Hooper and colleagues [44] we determined whether Ang4 could kill Salmonella using recombinant Ang4. Recombinant Ang4 was active against Salmonella in a concentration‑dependent manner (Figure 2B); using amounts (280μM) comparable to those estimated to be present in the crypt lumen (Table 1) (~300μM), 100% of the Salmonella inoculum was killed (Figure 2B). Ang4 strongly affected bacterial membrane integrity with nearly 90% of the bacterial population that had been exposed to only 28μM Ang4 staining positive for propidium iodide (Figure 2C). Transmission electron micrographs confirmed abnormal cell structure of Ang4‑treated bacteria with affected cells exhibiting pore‑like structures in the cell membrane (Figure 2C). Native Ang4 in intestinal crypts was also active. Freshly obtained WT crypt exudates killed up to 70% of Salmonella, a significant proportion of which (~45%) could be attributed to Ang4 killing activity as seen by the reduction of killing in the presence of a neutralising anti-Ang4 monoclonal antibody (Figure 2D). This indicates that Ang4 produced in vivo remains active under conditions that reflect luminal electrolyte composition. As expected, no bactericidal activity was observed in TCRδ-/- crypt exudates. As we speculated that Ang4 also contributes to the homeostasis of the intestinal microbial ecology, we tested whether Ang4 was also active against commensal bacteria using a selection of Gram‑positive and Gram‑negative strains from the sub‑ and predominant intestinal microbiota. Gram‑negative Escherichia coli and Bacteroides thetaiotaomiron were highly susceptible to Ang4 with less than 0.005% of the population surviving one-hour exposure to 28μM Ang4 (Figure 2E). Gram‑positive strains were also susceptible to Ang4 killing activity but to a lesser extent than the Gram‑negative strains tested, with approximately 0.5 and 16% of the population of Enterococcus gallinarum and Bifidobacterium longum surviving, respectively (Figure 2E). Overall, the high susceptibility to Ang4 killing activity of the commensals strains tested is consistent with Ang4 contributing to intestinal microbial homeostasis. Our findings also extend the known spectrum of Ang4 bactericidal activity to include Salmonella and intestinal commensal strains. Next we investigated how γδ iIELs modulate Ang4 expression.
Table 1. Estimated Ang4 content of mouse small intestinal crypts.
| Secretory stimulus a | Ang4 content | Crypt Ang4 |
|---|---|---|
| ng/crypt ± SD | Concentration mM | |
| Non-stimulated | 0.025 ± 0.014 | 0.30 |
| IL-22 (100ng/ml) | 0.175 ± 0.073 | 3.32 |
| Salmonella (103 CFU) | 0.075 ± 0.016 | 1.51 |
| Carbamyl Choline (10mM) | 0.307 ± 0.064 | 4.38 |
a Secretions collected after stimulation at 37°C for 30min
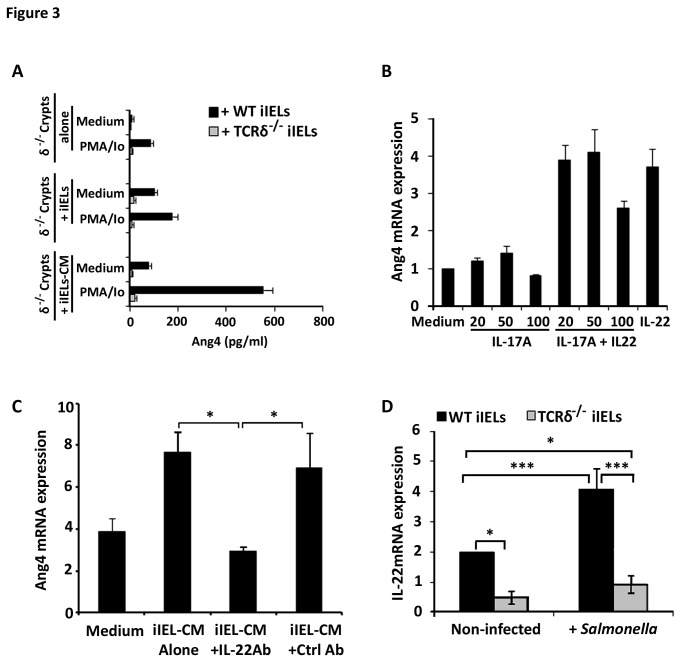
γδ T cells are the major source of secreted factors necessary for increasing Ang4 production
An iIEL-intestinal crypt/Paneth cell co-culture system was developed to determine the role γδ iIELs play in inducing Ang4 production by Paneth cells and whether it requires cognate or non-cognate interactions. Intestinal crypts from TCRδ‑/- mice were used as they produce no or undetectable amounts of Ang4 (Figure 1B and C). The addition of WT iIELs to TCRδ‑/- intestinal crypts resulted in small increases in Ang4 protein (Figure 3A) and mRNA (Figure S3A) expression with iIELs expressing no Ang4 expression themselves (data not shown and [44]). By contrast, supernatants of in vitro activated WT iIELs (IEL-CM) induced up to 10 and 50 times more Ang4 mRNA and protein production compared to crypts cultured in medium alone, respectively (Figure 3A, S3A). No significant stimulatory activity of Ang4 production was observed in control cultures containing the chemical stimuli used to activate iIELs in vitro or using supernatants from activated TCRδ-/- iIELs. Thus, γδ iIELs are a source of factors that up‑regulate Ang4 expression, requiring no direct interaction with crypt/Paneth cells for Ang4 production.
Figure 3. Paneth cells produce Ang4 in response to IL‑22 of which γδ iIELs are a source.
(A) ELISA-determined Ang4 protein levels produced by small intestinal crypts (2x103) from TCRδ-/- mice after culture at 37°C for 4h in media alone (Medium) or in media containing PMA/Io. Additional crypt samples were cultured with 103 WT iIELs (+iIELs) with and without prior in vitro stimulation by PMA/Io or, with conditioned medium (iIEL-CM) obtained from 104 in vitro stimulated WT (black bars) and TCRδ-/- (grey bars) iIELs. Data (mean±SEM) were collated from three experiments. (B) Ang4 mRNA levels (qPCR) detected in isolated intestinal TCRδ-/- crypts/Paneth cells incubated at 37°C for 4h with recombinant murine IL‑17A alone or in combination with recombinant IL‑22 (100ng/ml). Control cultures contained medium or 100ng/ml IL-22 alone. Data (mean±SEM) are expressed relatively to mRNA levels obtained when crypts were exposed to medium alone and were collated from two experiments (see also Figure S2). (C) Anti-IL‑22 antibodies abrogate Ang4 expression by iIEL-CM. Small intestinal crypts from TCRδ-/- mice were cultured at 37°C for 4h with iIEL-CM in the presence or absence of neutralising anti-IL‑22 or control antibodies (Ctrl Ab). Crypt Ang4 mRNA levels were measured by qPCR and expressed relative to β‑actin mRNA, with values (mean±SEM) representative of three experiments. (D) IL‑22 expression is reduced in TCRδ‑/- iIELs. IL‑22 mRNA was isolated from iIELs of WT and TCRδ-/- mice prior to (Non-infected) and 2h post‑challenge with Salmonella by qPCR. The data (mean±SEM) are expressed relative to β‑actin mRNA and were collated from four experiments (*p≤0.05; ***p≤0.001).
IL‑22 is necessary and sufficient for up‑regulating Ang4 expression
IL‑22 and IL‑17 are required for the production of AMPs in the skin and the inflamed intestine [49-54] with activated T lymphocytes being a source of both [55,56]. We therefore tested the possibility that IL-17 and IL-22 might regulate Ang4 production by Paneth cells. Recombinant IL‑22 up‑regulated Ang4 expression in isolated intestinal crypts from TCRδ‑/- mice whereas IL‑17 alone or in combination with IL‑22 had no significant effect (Figure 3B and S3B). By contrast, IL‑22 did not affect the production of any of the other Paneth cell AMPs tested here, including lysozyme, (Figure S1C and data not shown). The addition of neutralising anti‑IL‑22 antibodies to supernatants from activated WT iIELs inhibited their ability to up‑regulate Ang4 mRNA expression in Paneth cell‑containing crypts (Figure 3C), suggesting that IL‑22 is both necessary and sufficient to increase Ang4 expression in Paneth cells. Furthermore, using an ang4 promoter::luc reporter system, IL‑22 was shown to act at the transcriptional level on Ang4 expression in m-ICc12 epithelial cells (Figure S4). iIELs isolated from TCRδ-/- animals expressed significantly lower levels of IL‑22 mRNA compared to those of both naïve and infected WT mice (Figure 3D). IL‑22 mRNA was more abundant in γδ+ than in αβ+ iIELs (Figure S5A) and the majority (75%) of IL-22 secreting iIELs from Salmonella infected WT mice were TCRγδ+ (Figure S5B) of which 75% were Vγ7+ (Figure S5C).
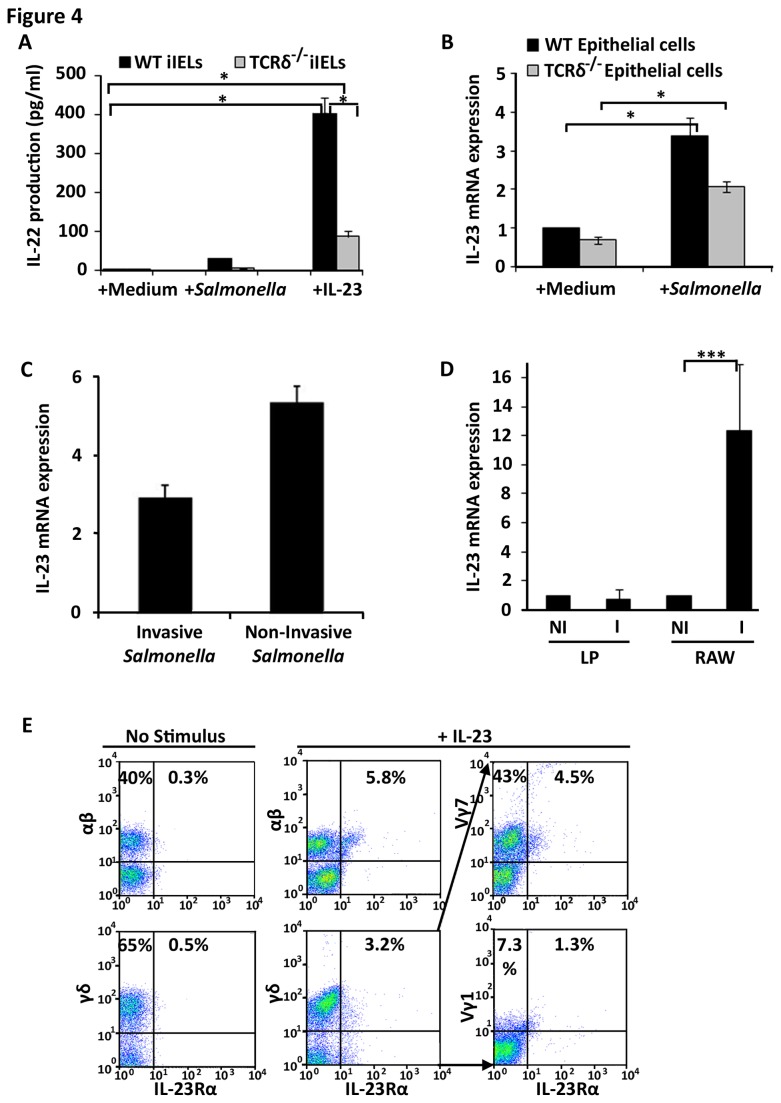
iIELs produce IL‑22 in response to IL‑23 produced by stressed intestinal epithelial cells
The finding that IL‑22 production by γδ iIELs is increased upon Salmonella infection suggests that γδ iIELs either directly interact with Salmonella and secrete IL‑22, as shown for lung γδ IELs exposed to Bacillus subtilis [57], or that local pathogen-exposed epithelial cells produce signalling molecules able to trigger IL‑22 production by iIELs. Several studies have previously demonstrated that IL‑23 regulates mucosal inflammation induced by pathogen infection such as Salmonella [58,59]. IL‑23 has also been shown to induce IL-22 production by Th17 cells and peripheral γδ T cells [60]. The possibility that IL-22 production by iIELs is regulated by IL‑23 was determined by exposing highly purified WT and TCRδ-/- iIELs to Salmonella or recombinant IL‑23. Exposure to Salmonella increased the levels of IL‑22 produced by WT iIELs with IL‑23 having an even greater effect (Figure 4A), leading to a ~400‑fold increase in the amount of IL‑22 protein detected compared to that produced by iIELs exposed to medium alone. By contrast, IL‑23 induced much lower levels of IL‑22 among TCRδ-/- iIELs, consistent with γδ+ iIELs being the major source of IL‑22 among iIELs.
Figure 4. iIELs produce IL-22 in response to IL-23, a cytokine produced by intestinal epithelial cells.
(A) iIELs from WT and TCRδ‑/‑ mice were cultured at 37°C for 6h with medium alone or medium containing 1x105 CFU S. Typhimurium or recombinant IL‑23 (100ng/ml) after which supernatants were analysed by IL‑22 ELISA (*p≤0.05). Data (mean±SEM) were collated from three experiments. (B) Intestinal epithelial cells (106) from WT and TCRδ‑/- mice were exposed for 2h to medium alone or medium containing Salmonella at a ratio of 10 bacteria per epithelial cell. IL‑23 mRNA expression was then assessed by qPCR. The data (mean±SEM) were expressed relative to mRNA levels found in WT epithelial cells exposed to medium alone and were collated from three experiments (*p≤0.05). (C) m-ICcl2 intestinal epithelial cells were cultivated on 0.4µm pore size filters and incubated at 37°C for 4h with medium alone, or medium containing invasive or non‑invasive Salmonella after which cells were harvested, RNA extracted and IL‑23 expression analysed by qPCR. Data are expressed relative to mRNA levels obtained on m‑ICc12 cells exposed to medium alone. (D) RNA was purified from lamina propria (LP) cells isolated from orally infected (2h p.i.) and non‑infected WT mice. As a positive control for IL-23 production, cultivated RAW264.7 macrophages (RAW) were analysed pre- (NI) and post-infection (I) (6h p.i.) with Salmonella. Data are shown as mean±STD relative to mRNA levels in non‑infected samples, and are representative of 5 and 4 experiments, respectively. (E) iIELs from WT mice were cultured at 37°C for 2h with medium alone (No Stimulus) or with medium containing IL‑23. The distribution of IL-23Rα expression among Vγ1 and Vγ7 iIELs was determined by flow cytometry from 4-colour/antibody staining protocols: combining CD3, TCR-γδ, IL-23R and either TCR-Vγ7 or TCR-Vγ1 antibodies with a gating strategy of selecting CD3+, TCR-γδ+, IL-23R+ events (middle panels) and then analysing them for Vγ7+, IL-23Rα+ and Vγ7-, IL-23Rα+ events (far right hand panels). The profiles shown are representative of three experiments with the percentage values representing the frequency of positive cells in the designated quadrants.
IL‑23 is expressed by macrophages and other professional phagocytes upon pathogenic or commensal challenges [61-64] although non-phagocytic cells are now being identified as additional sources of IL‑23 [65]. We therefore tested the possibility that intestinal epithelial cells are an immediate source of IL-23 following challenge with Salmonella. Upon a 4h exposure of primary small intestinal epithelial cells (>99% CD45-; Figure S6) or m‑ICc12 cells to Salmonella the levels of IL‑23 mRNA significantly increased in both cell types (Figure 4B and C). Salmonella induced slightly lower levels of IL-23 mRNA in epithelial cells from TCRδ-/- mice compared to WT cells which we cannot explain but may reflect the absence of γδ iIELs in vivo and perhaps their requirement for optimal epithelial cell responses. Of note, up‑regulation of IL‑23 expression in m‑ICc12 epithelial cells was also observed in response to non‑invasive Salmonella (Figure 4C), suggesting that invasion was not required to trigger the IL‑23‑mediated epithelial response.
The contribution of other, non-epithelial, intestinal mucosal cells to IL-23 production during the initial response to oral Salmonella infection was investigated by examining IL-23 mRNA expression by mucosal immune cells directly ex‑vivo during the first 2h of infection. Under these experimental conditions it was not possible to detect IL-23 expression by these cells (Figure 4D). However, these lamina propria cells are capable of expressing IL‑23 when directly challenged in isolation after exposure to Salmonella in vitro for 4h, as done for primary and m‑ICc12 epithelial cells (Figure S7). In response to IL-23 iIELs rapidly expressed IL-23Rα; approximately 10% of iIELs (~6% TCR-αβ+ and ~3% TCR-γδ+) expressed IL‑23Rα within 2h of in vitro stimulation which represents a 6- to almost 20-fold increase in IL‑23Rα+ iIELs when compared with IELs exposed to medium alone (Figure 4E). The majority of IL‑23Rα+ cells were γδ iIELs of which >43% were Vγ7+, consistent with this subset being instrumental in the IL‑23‑dependent signalling cascade leading to Ang4 expression (Figure 4E). Naive iIELs were virtually devoid (<1% positive) of IL‑23Rα expression (Figure 4E).
Invasion of intestinal epithelial cells by Salmonella is not essential for up‑regulation of IL‑23 by intestinal epithelial cells and Ang4 production by Paneth cells
The relationship between IL‑23 expression by intestinal epithelial cells after oral challenge by Salmonella and Ang4 expression by Paneth cells was investigated in vivo. Salmonella was injected into ligated loops of small intestine in WT mice, resulting in increased levels of Ang4 mRNA irrespective of whether Salmonella was invasive or not (Figure 5A). Similarly, IL‑23 secretion was increased in cultured intestinal epithelial cells after challenge with both invasive and non-invasive Salmonella strains (Figure 5B), with up‑regulation of Ang4 in vivo and of IL‑23 in vitro surprisingly being 1.5 to 2‑fold higher when non‑invasive Salmonella was used. Although difficult to explain, these results in combination with the bactericidal activity spectrum observed (Figure 2) raised the possibility that the IL‑23/IL‑22/Ang4 pathway is also active in response to non‑invasive bacteria such as components of the intestinal microbiota. Gram-negative E. coli and to a lower extent B. thetaiotaomicron triggered IL‑23 mRNA expression in intestinal epithelial cells (Figure 5C) whereas two Gram-positive bacteria tested, E. gallinarum and B. longum, failed to invoke an IL‑23 response from epithelial cells, although they are susceptible to Ang4 activity (Figure 2E). Overall these results suggest that the pathway described here may contribute to the host-microbe homeostasis of the GI tract.
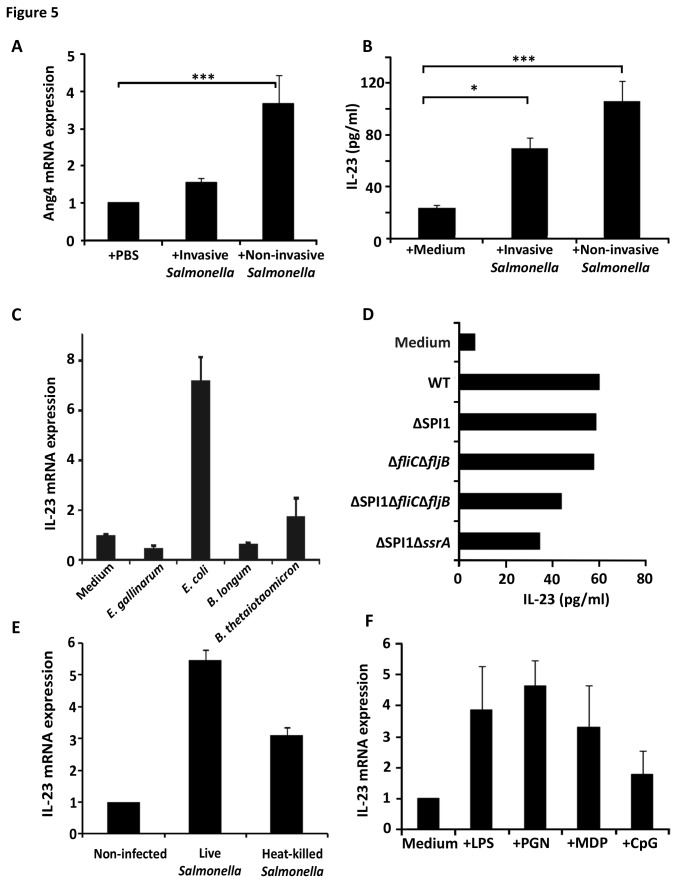
Figure 5. Requirements for microbe-induced Ang4 and IL‑23 production by intestinal epithelial cells.
(A) Invasive or non-invasive Salmonella strains (4x107 CFU in PBS) were injected into exteriorised intestinal ligated loops of WT mice. Four hours later mucosal RNA was isolated and Ang4 mRNA expression analysed by qPCR. The data (mean±SEM) are expressed relative to mRNA levels obtained from loops exposed to PBS alone (n=3; ***p<0.001). (B) IL‑23 protein levels assessed by ELISA (mean±SEM) from intestinal epithelial cells of WT mice exposed for 12h to medium alone, (+Medium) or media containing invasive or non‑invasive Salmonella strains at a ratio of 10 bacteria per epithelial cell (n=3; ***p<0.001, *p<0.05). (C) m-ICc12 intestinal epithelial cells were cultured for 4h with medium alone (control) or containing live cells of various intestinal commensal bacteria at a ratio of 10 bacteria per epithelial cell. IL‑23 mRNA expression was assessed by qPCR. Data (mean±SEM) were expressed relatively to mRNA levels in control samples (n=4). (D) IL‑23 protein production measured by ELISA in intestinal epithelial cells from WT mice cultured at 37°C for 12h with medium alone or containing either, live WT (SL1344) or various Salmonella mutant strains that are non-invasive (SL1344ΔSPI1), invasive but non-flagellated (JH3220=SL1344ΔfliCΔfljB), non-invasive and non-flagellated (JH3515=SL1344∆SPI1ΔfliCΔfljB) or non-invasive, flagellated but unable to transcytose flagellin (JH3574=SL1344∆SPI1ΔssrA) (n=3; mean±SEM). (E) IL‑23 mRNA expression assessed by qPCR in m-ICc12 epithelial cells cultured at 37°C for 4h with medium alone or containing live or heat‑killed WT Salmonella SL1344 cells at a ratio of 10 bacteria per epithelial cell. Data (n=4; mean±SEM) are expressed relative to mRNA levels obtained in non‑infected cells. (F) IL‑23 mRNA levels analysed by qPCR in intestinal epithelial cells from WT mice cultured at 37°C for 2h with medium alone or containing lipopolysaccharide (LPS), peptidoglycan (PGN), muramyl dipeptide (MDP) or methylated DNA (CpG). Data (n=3; mean±SEM) are expressed relative to mRNA levels obtained in cells exposed to medium alone.
To understand in more details the pathway leading from bacterial challenge to IL‑23 production, intestinal epithelial cells from WT mice were exposed to a virulent strain of Salmonella or Salmonella strains lacking various virulence factors including flagellin, invasion‑associated pathogenicity island (Salmonella Pathogenicity Island 1, SPI1), or SsrA, which is a key regulator of the SPI2 (essential for intracellular survival, replication and flagellin translocation across the epithelial layer). Irrespective of whether or not bacteria could invade, synthesise or transcytose flagellin, all mutant strains induced IL‑23 secretion by primary epithelial cells (Figure 5D), suggesting that the three key virulence gene clusters were not required for IL‑23 up‑regulation. In general agreement with this, we observed a trend of increased numbers of bacteria (~5-fold) in the small intestinal tissue of TCRδ‑/- mice compared to WT mice after 2h infection with two mutant, non-flagellated and non‑invasive, strains of Salmonella (SL1344ΔfliCΔfljB = 7.47x103±1.53x103 CFU/g in WT mice compared with 3.14x104±9.18x103 CFU/g in TCRδ‑/- mice; SL1344ΔSPI1 = 5.09x103±3.93x103 CFU/g in WT mice compared with 2.32x104± 1.80x104 CFU/g in TCRδ‑/- mice). Heat-killed Salmonella cells also induced IL‑23 mRNA expression by m‑ICc12 cells (Figure 5E), suggesting that bacterial cell components, likely to be surface‑exposed were sufficient to elicit IL‑23 expression. To test this hypothesis purified microbe‑associated molecular patterns (MAMPs) including LPS, Peptidoglycan and muramyl dipeptide (MDP) were applied for up to 16h to cultured intestinal epithelial cells. All bacterial components (MDP to a lesser extent than others) triggered up‑regulation of IL-23 mRNA expression in intestinal epithelial cells (Figure 5F). By contrast, the TLR9 ligand CpG did not affect IL‑23 production and the ability of non-flagellated Salmonella to invoke IL-23 production by epithelial cells excluded TLR5 involvement in this response. These findings suggest that recognition of Salmonella by epithelial cells is mediated by multiple MAMPs recognised by epithelial cell surface or cytoplasmic pattern recognition receptors (PRRs).
Discussion
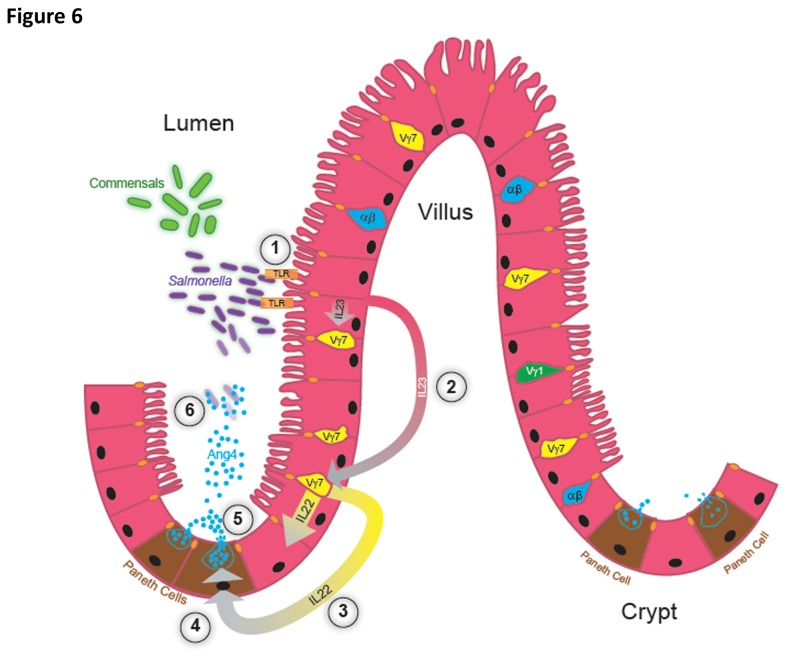
The intimate association of TCRγδ+ iIELs with the epithelium of the small intestine is indicative of their involvement in maintaining intestinal barrier function. Exactly how γδ iIELs fulfil this role, the nature of their interactions with the epithelium, and the pathways leading to their activation and deployment of effector function is unclear. Here, we describe a new putative host response pathway involving the interaction of γδ (Vγ7+) iIELs with epithelial cells leading to Ang4 production by Paneth cells, using Salmonella as a model pathogen to trigger this response in vivo (Figure 6). Of note, commensal members of the intestinal microbiota also appear to have the capacity to trigger this pathway. While we can provide no evidence that this pathway is directly involved in determining the outcome of oral Salmonella infection and the development of salmonellosis, it has the potential to act in synergy with or in addition to other mechanisms leading to AMP production, to reduce the level of host cell infection by pathogens as well as proliferation of commensals in close vicinity to the epithelium and maintaining the integrity of the intestinal epithelial barrier.
Figure 6. Hypothetical model of the production of Ang4 in response to microbial challenge.
(1) Upon exposure to Salmonella or recognition of commensal bacteria or MAMPs, intestinal epithelial cells secrete IL‑23, in a TLR‑dependent manner in the case of Salmonella. (2) Via extracellular or transcellular routes, epithelial cells secrete IL‑23 (pink to grey gradient arrows) that binds to its cognate receptor IL‑23R expressed by γδ iIELs. (3) IL-23R+ iIELs enriched in Vγ7+ cells respond to IL-23 by secreting IL‑22 (yellow to grey gradient arrows). Via extracellular or transcellular routes IL‑22 acts on IL-22R-bearing Paneth cells up-regulating Ang4 transcription (4) and/or secretion (5) of pre-formed protein stored in intracellular granules. Ang4 is secreted into the lumen at levels sufficient (5) to effectively kill Salmonella located in the vicinity of the intestinal tissue (6), helping to protect it from proliferation of and invasion by the pathogen.
Commensal intestinal bacteria influence both Ang4 production and iIELs. Ang4 expression increases dramatically in ex‑germfree mice in response to colonisation by gut bacteria [44] and iIEL populations require exposure to environmental antigens and commensal bacteria to become functionally mature [66,67]. Our finding that Ang4 production is initiated by epithelial non‑clonotypic PRRs and that both commensals and pathogens can elicit the pathway leading to Ang4 production [44] demonstrate a lack of distinction in the origin of bacteria that triggers Ang4 expression. Our data does however suggest that Gram-negative bacteria are more effective at triggering IL‑23 expression, and are noticeably more susceptible to Ang4 than Gram‑positive bacteria. Depending on the diffusion gradient of secreted Ang4 in the crypt/villous lumen it may impact on microbes within the mucus layer covering the epithelium or on microbes able to penetrate the mucus layer, which has a thinner viscosity at the bottom of crypts [68] thereby preventing microbial access to the underlying epithelium and resulting in limited activation of inflammatory responses. Our data suggest that the ability of bacteria or bacterial cell components to make contact with surface epithelial cells and elicit PRR-mediated IL‑23 production could be the driving force behind epithelial cell interactions with IL‑22‑producing Vγ7+ iIELs that subsequently leads to Ang4 production. This bacteria-driven response may serve the host by containing and restricting the growth of populations of commensal bacteria at the luminal surface and by containing the growth of invasive pathogens that encroach into intestinal crypts. It was technically not possible to reconstitute Ang4 activity in TCRδ-/- mice by enteric delivery of native, highly labile, Ang4 (data not shown) to determine whether the lack of Ang4 in TCRδ‑/- mice directly accounted for the higher Salmonella burden in intestinal tissue immediately after oral challenge. However, we have shown that Ang4 produced in vivo is bactericidal in intestinal crypt exudates. Salmonella is unlikely to be the only target of Ang4 bactericidal activity and it may target other enteric bacterial pathogens including Listeria [44] to which TCRδ-/- mice display increased susceptibility [26]. Ang4 can therefore be considered part of the AMP armament that protects the host against invasion by a range of enteric microbial challenges.
How γδ T cell responses are triggered and the nature of the antigens they recognise are uncertain. This study shows that their activation involves signals delivered through cytokine-cytokine receptor axes, in particular IL‑23/IL‑23R signalling, extending previous reports of γδ T cell involvement in IL‑23‑orchestrated mucosal responses to bacteria [62] or to Salmonella [69]. Our findings clearly show that IL-23 alone is sufficient to elicit IL-22 production by cultured γδ iIELs, consistent with the lack of evidence of a requirement for cognate iIEL-Paneth cell interactions in Ang4 production. How accurately this reflects the requirements for γδ iIEL activation and IL-22 production in vivo requires further study. It is possible is that other mucosa-associated immune cells support γδ T cells in their IL-23-driven IL-22 production, as for example shown for populations of macrophages and Lymphoid inducer cells responding to Citrobacter rodentium infection [70,71]. The apparent lack of TCR involvement in γδ iIEL activation and IL‑22 production is similar to that described for splenic and lymph node γδ T cells that produce IL‑22 and IL‑17 in response to IL‑23 plus IL1 and TLR ligands [72,73], the cellular source of which includes activated dendritic cells [72]. During the immediate response to oral Salmonella challenge our results identify epithelial cells as the source of IL-23, although we do not exclude that at later times post-microbial challenge IL‑23 is expressed by innate immune cells present or recruited to the lamina propria, as has been described for other pathogens in different mucosal systems [74-76]. We cannot formally exclude the involvement of specific antigen receptors (TCR and PRRs) in iIEL responses to Salmonella infection in vivo. However, our findings exclude the TCR acting in isolation to trigger their response and suggest that TLR involvement in γδ iIELs activation and IL‑22 production is indirect and is consequent to upstream response of intestinal epithelial cells that rapidly produce IL‑23 in response to bacterial cells and/or their products. We cannot exclude that lamina propria immune cells are an additional and major source of IL‑23 later during infection. However, these cells did not up-regulate IL‑23 mRNA expression in vivo within the first 2h of infection whereas primary epithelial cells did in our in vivo and in vitro model systems. Interestingly, certain Gram-negative commensals such as E. coli elicited an IL-23 response from intestinal epithelial cells, similar in magnitude to that triggered by Salmonella. The IL‑23 signalling pathway may therefore not be microbe‑specific and unable to discriminate between pathogens and commensals. Instead, it may be part of a more generic homeostatic response aimed at controlling microbial proliferation in close vicinity of the intestinal mucosa. The apparent lack of TLR responsiveness and the absence of IL‑23R expression among γδ iIELs in naïve animals provide a means by which their activation can be regulated. Furthermore this can be coordinated through the response of epithelial cells, preventing them from responding directly to enteric microbes. The transient and low levels of IL‑23 produced by stressed/infected epithelial cells could act in a similar way to restrict and contain iIEL activation and the production of pro-inflammatory cytokines, which if sustained and uncoordinated could promote tissue damaging responses. Of note, patients with IL-12/IL-23 component deficiency are susceptible to recurrent Salmonella infection [77]. It would be of interest to determine if this is associated with abnormalities in iIEL and/or AMP function.
In the context of the initial response of γδ IELs to oral Salmonella exposure and intestinal epithelial stress, the findings presented here add on to previous studies showing that IL‑22 is of primary importance in host antimicrobial defence in ensuring the production of potent AMPs [54,78]. IL‑22 deficiency in patients with acne inversa associated with defective AMP production and bacterial overgrowth is consistent with this interpretation and the importance of IL‑22 in microbial defence at mucosal sites [79]. The level at which IL‑22 acts to regulate Ang4 secretion has not been fully established although the data presented here suggests that Ang4 production is controlled at the transcriptional level by iIELs and IL‑22. Although iIELs are a source of IL-17 that plays a central role in (inflammatory) mucosal immune responses it is not required for iIEL-driven Ang4 production. It may however contribute in other ways to reinforce barrier functions via, for example, its effects on mucin and other AMP production (Lipocalin 2) and epithelial tight junctions [52,80,81].
In summary, our findings identify a novel host response pathway triggered by the model enteric pathogen Salmonella and components of the microbiota that involves the coordinated interaction of γδ iIELs with microbe/pathogen exposed epithelial cells. This cross‑talk occurs through specific cytokine-cytokine receptor signalling, resulting in up‑regulation of Ang4 production by Paneth cells (Figure 6) that can contribute to maintaining intestinal microbial homeostasis and mucosal defence of the GI tract.
Supporting Information
Paneth cell development and lysozyme production occurs normally in the absence of γδ T cells.
(TIFF)
Intestinal crypt isolation.
(TIF)
qPCR quantitation of Ang4 mRNA expression in small intestinal crypts.
(TIFF)
IL‑22 acts at the transcriptional level to regulate Ang4 expression.
(TIFF)
IL‑22 induces Ang4 mRNA and protein expression and is produced by TCRVγγ+ iIELs.
(TIFF)
Purity of intestinal epithelial cell preparations.
(TIFF)
In vitro stimulated lamina propria cells express IL‑23 mRNA.
(TIFF)
Acknowledgments
We are grateful to Drs. Louise Wakenshaw, Regis Stentz, Elizabeth Bassity, Kamal Ivory, Nikki Horn, Sacha Lucchini and Ida Porcelli (IFR) for technical advice, assistance with experiments and/or commenting on the manuscript. We thank Kathryn Cross for transmission electron microscopy and Paul Pople and Angie Walker for assistance with Figure 6. We thank Andy Hayes and Leo Zeef of the Genomic Technologies and Bioinformatics Core Facilities in the Faculty of Life Sciences at the University of Manchester for providing technical support and analysis with regard to Affymetrix arrays. Finally, the authors thank Drs. L. Hooper (Univ. Texas Southwestern Medical Center, Dallas, TX), L. Lefrançois (Univ. Connecticut, CT) and P. Pereira (Institut Pasteur, Paris, France) for providing reagents, antibodies and advice on experimental protocols.
Funding Statement
This work was supported in part by grants awarded by the Biotechnology of Biological Sciences Research Council (BBSRC) and the Wellcome Trust (SRC). Catherine Walker was supported by a BBSRC-DTA studentship awarded to the University of Leeds. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Sansonetti PJ (2004) War and peace at mucosal surfaces. Nat Rev Immunol 4: 953-964. doi: 10.1038/nri1499. PubMed: 15573130. [DOI] [PubMed] [Google Scholar]
- 2. Ayabe T, Satchell DP, Wilson CL, Parks WC, Selsted ME et al. (2000) Secretion of microbicidal α-defensins by intestinal Paneth cells in response to bacteria. Nat Immunol 1: 113-118. doi: 10.1038/77783. PubMed: 11248802. [DOI] [PubMed] [Google Scholar]
- 3. Salzman NH, Ghosh D, Huttner KM, Paterson Y, Bevins CL (2003) Protection against enteric salmonellosis in transgenic mice expressing a human intestinal defensin. Nature 422: 522-526. doi: 10.1038/nature01520. PubMed: 12660734. [DOI] [PubMed] [Google Scholar]
- 4. Wilson CL, Ouellete AJ, Satchell DP, Ayabe T, Lopez-Boado YS et al. (1999) Regulation of intestinal α-defensin activation by the metalloproteinase matrilysin in innate host defence. Science 286. [DOI] [PubMed] [Google Scholar]
- 5. Salzman NH, Hung K, Haribhai D, Chu H, Karlsson-Sjöberg J et al. (2010) Enteric defensins are essential regulators of intestinal microbial ecology. Nat Immunol 11: 76-82. doi: 10.1038/ni.1825. PubMed: 19855381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vantourout P, Hayday A (2013) Six-of-the-best: unique contributions of γδ T cells to immunology. Nat Rev Immunol 13: 88-100. doi: 10.1038/nri3384. PubMed: 23348415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cerutti A, Cols M, Puga I (2013) Marginal zone B cells: virtues of innate-like antibody-producing lymphocytes. Nat Rev Immunol 13: 118-132. doi: 10.1038/nri3383. PubMed: 23348416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gold MC, Lewinsohn DM (2013) Co-dependents: MR1-restricted MAIT cells and their antimicrobial function. Nat Rev Microbiol 11: 14-19. PubMed: 23178389. [DOI] [PubMed] [Google Scholar]
- 9. Spits H, Artis D, Colonna M, Diefenbach A, Di Santo JP et al. (2013) Innate lymphoid cells - a proposal for uniform nomenclature. Nat Rev Immunol 13: 145-149. doi: 10.1038/nrc3470. PubMed: 23348417. [DOI] [PubMed] [Google Scholar]
- 10. Spits H, Cupedo T (2012) Innate Lymphoid Cells: Emerging Insights in Development, Lineage Relationships, and Function. Annu Rev Immunol 30: 647-675. doi: 10.1146/annurev-immunol-020711-075053. PubMed: 22224763. [DOI] [PubMed] [Google Scholar]
- 11. Ismail AS, Behrendt CL, Hooper LV (2009) Reciprocal Interactions between Commensal Bacteria and γδ Intraepithelial Lymphocytes during Mucosal. Injury - J Immunol 182: 3047-3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bonneville M, Janeway CA Jr, Ito K, Haser W, Ishida I et al. (1988) Intestinal intraepithelial lymphocytes are a distinct set of γδ T cells. Nature 336: 479-481. doi: 10.1038/336479a0. PubMed: 2461518. [DOI] [PubMed] [Google Scholar]
- 13. Bucy RP, Chen CL, Cihak J, Lösch U, Cooper MD (1988) Avian T cells expressing γ/δ receptors localize in the splenic sinusoids and the intestinal epithelium. J Immunol 141: 2200-2205. PubMed: 3262650. [PubMed] [Google Scholar]
- 14. Goodman T, Lefrançois L (1988) Expression of the γδ T cell receptor on intestinal CD8+ intraepithelial lymphocytes. Nature 333: 855-858. doi: 10.1038/333855a0. PubMed: 2968521. [DOI] [PubMed] [Google Scholar]
- 15. Trejdosiewicz LK, Smart CJ, Oakes DJ, Howdle PD, Malizia G et al. (1989) Expression of T-cell receptors TCR1 (γ/δ) and TCR2 (α/β) in the human intestinal mucosa. Immunol 68: 7-12. [PMC free article] [PubMed] [Google Scholar]
- 16. Jabri B, Ebert E (2007) Human CD8+ intraepithelial lymphocytes: a unique model to study the regulation of effector cytotoxic T lymphocytes in tissue. Immunol Rev 215: 202-214. doi: 10.1111/j.1600-065X.2006.00481.x. PubMed: 17291290. [DOI] [PubMed] [Google Scholar]
- 17. Kyes S, Carew E, Carding SR, Janeway CA Jr, Hayday A (1989) Diversity in T-cell receptor γ gene usage in intestinal epithelium. Proc Natl Acad Sci U S A 86: 5527-5531. doi: 10.1073/pnas.86.14.5527. PubMed: 2546157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pereira P, Gerber D, Huang SY, Tonegawa S (1995) Ontogenetic development and tissue distribution of Vγ1-expressing γ/δ T lymphocytes in normal mice. J Exp Med 182: 1921-1929. doi: 10.1084/jem.182.6.1921. PubMed: 7500038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guy-Grand D, Cuénod-Jabri B, Malassis-Seris M, Selz F, Vassalli P (1996) Complexity of the mouse gut T cell immune system: Identification of two distinct natural killer T cell intraepithelial lineages. Eur J Immunol 26: 2248-2256. doi: 10.1002/eji.1830260942. PubMed: 8814274. [DOI] [PubMed] [Google Scholar]
- 20. Ismail AS, Severson KM, Vaishnava S, Behrendt CL, Yu X et al. (2011) γδ intraepithelial lymphocytes are essential mediators of host-microbial homeostasis at the intestinal mucosal surface. Proc Natl Acad Sci U S A 108: 8743-8748. doi: 10.1073/pnas.1019574108. PubMed: 21555560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen Y, Chou K, Fuchs E, Havran WL, Boismenu R (2002) Protection of the intestinal mucosa by intraepithelial γδ T cells. Proc Natl Acad Sci U S A 99: 14338-14343. doi: 10.1073/pnas.212290499. PubMed: 12376619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dalton JE, Cruickshank SM, Egan CE, Mears R, Newton DJ et al. (2006) Intraepithelial γδ+ Lymphocytes Maintain the Integrity of Intestinal Epithelial Tight Junctions in Response to Infection. Gastroenterol 131: 818-829. doi: 10.1053/j.gastro.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 23. Cheroutre H (2005) IELs: enforcing law and order in the court of the intestinal epithelium. Immunol Rev 206: 114-131. doi: 10.1111/j.0105-2896.2005.00284.x. PubMed: 16048545. [DOI] [PubMed] [Google Scholar]
- 24. Havran WL, Jameson JM, Witherden DA (2005) Epithelial cells and their neighbors: III. Interactions between intraepithelial lymphocytes and neighboring epithelial cells. Am J Physiol 289: 627-630. [DOI] [PubMed] [Google Scholar]
- 25. Hayday AC, Tigelaar R (2003) Immunoregulation in the tissues by γδ T cells. Nat Rev Immunol 3: 233-242. doi: 10.1038/nrc1069. PubMed: 12658271. [DOI] [PubMed] [Google Scholar]
- 26. Andrew EM, Carding SR (2005) Murine γδ T cells in infection: beneficial or deleterious? Microbes and Infect 7: 529-536. doi: 10.1016/j.micinf.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 27. Mixter PF, Camerini V, Stone BJ, Miller VL, Kronenberg M (1994) Mouse T lymphocytes that express a γδ T-cell antigen receptor contribute to resistance to Salmonella infection in vivo . Infect Immun 62: 4618-4621. PubMed: 7927728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fahrer AM, Konigshofer Y, Kerr EM, Ghandour G, Mack DH et al. (2001) Attributes of γδ intraepithelial lymphocytes as suggested by their transcriptional profile. Proc Natl Acad Sci U S A 98: 10261-10266. doi: 10.1073/pnas.171320798. PubMed: 11526237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shires J, Theodoridis E, Hayday AC (2001) Biological Insights into TCRγδ+ and TCRαβ+ Intraepithelial Lymphocytes Provided by Serial Analysis of Gene Expression (SAGE). Immunity 15: 419-434. doi: 10.1016/S1074-7613(01)00192-3. PubMed: 11567632. [DOI] [PubMed] [Google Scholar]
- 30. Andrew EM, Newton DJ, Dalton JE, Egan CE, Goodwin SJ et al. (2005) Delineation of the function of a major γδ T cell subset during infection. J Immunol 175: 1741-1750. PubMed: 16034115. [DOI] [PubMed] [Google Scholar]
- 31. Arques JL, Hautefort I, Ivory K, Bertelli E, Regoli M et al. (2009) Salmonella Induces Flagellin- and MyD88-Dependent Migration of Bacteria-Capturing Dendritic Cells Into the Gut Lumen. Gastroenterol 137: 579-587. doi: 10.1053/j.gastro.2009.04.010. PubMed: 19375423. [DOI] [PubMed] [Google Scholar]
- 32. Hoiseth SK, Stocker BA (1981) Aromatic-dependent Salmonella Typhimurium are non-virulent and effective as live vaccines. Nature 291: 238-239. doi: 10.1038/291238a0. PubMed: 7015147. [DOI] [PubMed] [Google Scholar]
- 33. Schechter LM, Damrauer SM, Lee CA (1999) Two AraC/XylS family members can independently counteract the effect of repressing sequences upstream of the hilA promoter. Mol Microbiol 32: 629-642. doi: 10.1046/j.1365-2958.1999.01381.x. PubMed: 10320584. [DOI] [PubMed] [Google Scholar]
- 34. Burns-Guydish SM, Olomu IN, Zhao H, Wong RJ, Stevenson DK et al. (2005) Monitoring age-related susceptibility of young mice to oral Salmonella enterica serovar Typhimurium infection using an in vivo murine model. Pediatr Res 58: 153-158. doi: 10.1203/01.PDR.0000157725.44213.C4. PubMed: 15774831. [DOI] [PubMed] [Google Scholar]
- 35. Guy-Grand D, Griscelli C, Vassalli P (1978) The mouse gut T lymphocyte, a novel type of T cell. Nature, origin, and traffic in mice in normal and graft-versus-host conditions. J Exp Med 148: 1661-1677. doi: 10.1084/jem.148.6.1661. PubMed: 31410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Inan MS, Tolmacheva V, Wang QS, Rosenberg DW, Giardina C (2000) Transcription factor NF-κB participates in regulation of epithelial cell turnover in the colon. Am J Physiol Gastrointest Liver Physiol 279: 1282-1291. [DOI] [PubMed] [Google Scholar]
- 37. Baumgart DC, Olivier W-A, Reya T, Peritt D, Rombeau JL et al. (1998) Mechanisms of intestinal epithelial cell injury and colitis in interleukin 2 (IL-2)-deficient mice. Cell Immunol 187: 52-66. doi: 10.1006/cimm.1998.1307. PubMed: 9682004. [DOI] [PubMed] [Google Scholar]
- 38. Bens M, Bogdanova A, Cluzeaud F, Miquerol L, Kerneis S et al. (1996) Transimmortalized mouse intestinal epithelial cells (m-ICcl2) that maintain a crypt phenotype. Am J Physiol 270: C1666-C1674. PubMed: 8764149. [DOI] [PubMed] [Google Scholar]
- 39. Eriksson S, Lucchini S, Thompson A, Rhen M, Hinton JC (2003) Unravelling the biology of macrophage infection by gene expression profiling of intracellular Salmonella enterica . Mol Microbiol 47: 103-118. PubMed: 12492857. [DOI] [PubMed] [Google Scholar]
- 40. Rowley G, Stevenson A, Kormanec J, Roberts M (2005) Effect of Inactivation of degS on Salmonella enterica Serovar Typhimurium In Vitro and In Vivo . Infect Immun 73: 459-463. doi: 10.1128/IAI.73.1.459-463.2005. PubMed: 15618185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fodor SP, Rava RP, Huang XC, Pease AC, Holmes CP et al. (1993) Multiplexed biochemical assays with biological chips. Nature 364: 555-556. doi: 10.1038/364555a0. PubMed: 7687751. [DOI] [PubMed] [Google Scholar]
- 42. Li C, Wong WH (2001) Model-based analysis of oligonucleotide arrays: expression index computation and outlier detection. Proc Natl Acad Sci U S A 98: 31 - 36. doi: 10.1073/pnas.98.1.31. PubMed: 11134512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wu Z, Irizarry RA, Gentleman R, Martinez-Murillo F, Spencer F (2004) A Model-Based Background Adjustment for Oligonucleotide Expression Arrays. Journal of the American Statistical Association 99: 909-917. doi: 10.1198/016214504000000683. [DOI] [Google Scholar]
- 44. Hooper LV, Stappenbeck TS, Hong CV, Gordon JI (2003) Angiogenins: a new class of microbial proteins involved in innate immunity. Nat Immunol 4: 269-273. doi: 10.1038/ni888. PubMed: 12548285. [DOI] [PubMed] [Google Scholar]
- 45. Shapiro R, Weremowicz S, Riordan JF, Vallee BL (1987) Ribonucleolytic activity of angiogenin: essential histidine, lysine, and arginine residues. Proc Natl Acad Sci U S A 84: 8783-8787. doi: 10.1073/pnas.84.24.8783. PubMed: 3122207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Singh JC, Cruickshank SM, Newton DJ, Wakenshaw L, Graham A et al. (2005) Toll-like receptor-mediated responses of primary intestinal epithelial cells during the development of colitis. Am J Physiol Gastrointest Liver Physiol 288: 514-524. PubMed: 15499080. [DOI] [PubMed] [Google Scholar]
- 47. Crabtree B, Holloway DE, Baker MD, Acharya KR, Subramanian V (2007) Biological and Structural Features of Murine Angiogenin-4, an Angiogenic Protein. Biochemistry 46: 2431-2443. doi: 10.1021/bi062158n. PubMed: 17279775. [DOI] [PubMed] [Google Scholar]
- 48. Datta R, deSchoolmeester ML, Hedeler C, Paton NW, Brass AM et al. (2005) Identification of novel genes in intestinal tissue that are regulated after infection with an intestinal nematode parasite. Infect Immun 73: 4025 - 4033. doi: 10.1128/IAI.73.7.4025-4033.2005. PubMed: 15972490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Liang SC, Tan X-Y, Luxenberg DP, Karim R, Dunussi-Joannopoulos K et al. (2006) Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J Exp Med 203: 2271-2279. doi: 10.1084/jem.20061308. PubMed: 16982811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ma HL, Liang S, Li J, Napierata L, Brown T et al. (2008) IL-22 is required for Th17 cell-mediated pathology in a mouse model of psoriasis-like skin inflammation. J Clin Invest 118: 597-607. PubMed: 18202747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Matsuzaki G, Umemura M (2007) Interleukin-17 as an effector molecule of innate and acquired immunity against infections. Microbiol Immunol 51: 1139-1147. doi: 10.1111/j.1348-0421.2007.tb04008.x. PubMed: 18094532. [DOI] [PubMed] [Google Scholar]
- 52. Raffatellu M, George MD, Akiyama Y, Hornsby MJ, Nuccio SP et al. (2009) Lipocalin-2 resistance confers an advantage to Salmonella enterica serotype Typhimurium for growth and survival in the inflamed intestine. Cell Host Microbe 5: 476-486. doi: 10.1016/j.chom.2009.03.011. PubMed: 19454351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Wolk K, Witte E, Wallace E, Döcke W-D, kunz S et al. (2006) IL-22 regulates the expression of genes responsible for antimicrobial defense, cellular differentiation, and mobility in keratinocytes: a potential role in psoriasis. Eur J Immunol 36: 1309-1323. doi: 10.1002/eji.200535503. PubMed: 16619290. [DOI] [PubMed] [Google Scholar]
- 54. Zheng Y, Valdez PA, Danilenko DM, Hu Y, Sa SM et al. (2008) Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nat Med 14: 282-289. doi: 10.1038/nm1720. PubMed: 18264109. [DOI] [PubMed] [Google Scholar]
- 55. Stark MA, Huo Y, Burcin TL, Morris MA, Olson TS et al. (2005) Phagocytosis of apoptotic neutrophils regulates granulopoiesis via IL-23 and IL-17. Immunity 22: 285-294. doi: 10.1016/j.immuni.2005.01.011. PubMed: 15780986. [DOI] [PubMed] [Google Scholar]
- 56. Umemura M, Kawabe T, Shudo K, Kidoya H, Fukui M et al. (2004) Involvement of IL-17 in Fas ligand-induced inflammation. Int Immunol 16: 1099-1108. doi: 10.1093/intimm/dxh111. PubMed: 15237105. [DOI] [PubMed] [Google Scholar]
- 57. Simonian PL, Wehrmann F, Roark CL, Born WK, O'Brien RL et al. (2010) γδ T cells protect against lung fibrosis via IL-22. J Exp Med 207: 2239-2253. doi: 10.1084/jem.20100061. PubMed: 20855496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Awoniyi M, Miller SI, Wilson CB, Hajjar AM, Smith KD (2012) Homeostatic Regulation of Salmonella-Induced Mucosal Inflammation and Injury by IL-23. PLOS ONE 7: e37311. doi: 10.1371/journal.pone.0037311. PubMed: 22624013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Godinez I, Raffatellu M, Chu H, Paixão TA, Haneda T et al. (2009) Interleukin-23 Orchestrates Mucosal Responses to Salmonella enterica Serotype Typhimurium in the Intestine. Infect Immun 77: 387-398. doi: 10.1128/IAI.00933-08. PubMed: 18955477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zheng Y, Danilenko DM, Valdez P, Kasman I, Eastham-Anderson J et al. (2007) Interleukin-22, a T(H)17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis. Nature 445: 648-651. doi: 10.1038/nature05505. PubMed: 17187052. [DOI] [PubMed] [Google Scholar]
- 61. Becker C, Wirtz S, Blessing M, Pirhonen J, Strand D et al. (2003) Constitutive p40 promoter activation and IL-23 production in the terminal ileum mediated by dendritic cells. J Clin Invest 112: 693-706. doi: 10.1172/JCI200317464. PubMed: 12952918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. McGovern D, Powrie F (2007) The IL-23 axis plays a key role in the pathogenesis of IBD. Gut 56: 1333-1336. doi: 10.1136/gut.2006.115402. PubMed: 17872562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Oppmann B, Lesley R, Blom B, Timans JC, Xu Y et al. (2000) Novel p19 Protein Engages IL-12p40 to Form a Cytokine, IL-23, with Biological Activities Similar as Well as Distinct from IL-12. Immunity 13: 715-725. doi: 10.1016/S1074-7613(00)00070-4. PubMed: 11114383. [DOI] [PubMed] [Google Scholar]
- 64. Yen D, Cheung J, Scheerens H, Poulet F, McClanahan T et al. (2006) IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J Clin Invest 116: 1310-1316. doi: 10.1172/JCI21404. PubMed: 16670770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Piskin G, Sylva-Steenland RMR, Bos JD, Teunissen MBM (2006) In Vitro and In Situ Expression of IL-23 by Keratinocytes in Healthy Skin and Psoriasis Lesions: Enhanced Expression in Psoriatic Skin. Journal of Immunology 176: 1908-1915. PubMed: 16424222. [DOI] [PubMed] [Google Scholar]
- 66. Kawaguchi-Miyashita M, Shimizu K, Nanno M, Shimada S, Watanabe T et al. (1996) Development and cytolytic function of intestinal intraepithelial T lymphocytes in antigen-minimized mice. Immunol 89: 268-273. doi: 10.1046/j.1365-2567.1996.d01-740.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lefrancois L, Goodman T (1989) In vivo modulation of cytolytic activity and Thy-1 expression in TCR-γδ+ intraepithelial lymphocytes. Science 243: 1716-1718. doi: 10.1126/science.2564701. PubMed: 2564701. [DOI] [PubMed] [Google Scholar]
- 68. Swidsinski A, Loening-Baucke V, Herber A (2009) Mucosal flora in Crohn's disease and ulcerative colitis- An overview. JPhysio l Pharmacol 60: 61-71 [PubMed] [Google Scholar]
- 69. Godinez I, Raffatellu M, Chu H, Paixão TA, Haneda T et al. (2009) Interleukin-23 orchestrates mucosal responses to Salmonella enterica serotype Typhimurium in the intestine. Infect Immun 77: 387-398. doi: 10.1128/IAI.00933-08. PubMed: 18955477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Manta C, Heupel E, Radulovic K, Rossini V, Garbi N et al. (2013) CX3CR1+ macrophages support IL-22 production by innate lymphoid cells during infection with Citrobacter rodentium . Mucosal Immunol 6: 177-188. doi: 10.1038/mi.2012.61. PubMed: 22854708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Sonnenberg GF, Monticelli LA, Elloso MM, Fouser LA, Artis D (2011) CD4+ Lymphoid Tissue-Inducer Cells Promote Innate Immunity in the Gut. Immunity 34: 122-134. doi: 10.1016/j.immuni.2010.12.009. PubMed: 21194981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Martin B, Hirota K, Cua DJ, Stockinger B, Veldhoen M (2009) Interleukin-17-producing γδ T cells selectively expand in response to pathogen products and environmental signals. Immunity 31: 321-330. doi: 10.1016/j.immuni.2009.06.020. PubMed: 19682928. [DOI] [PubMed] [Google Scholar]
- 73. Sutton CE, Lalor SJ, Sweeney CM, Brereton CF, Lavelle EC et al. (2009) Interleukin-1 and IL-23 induce innate IL-17 production from γδ T cells, amplifying Th17 responses and autoimmunity. Immunity 31: 331-341. doi: 10.1016/j.immuni.2009.08.001. PubMed: 19682929. [DOI] [PubMed] [Google Scholar]
- 74. Dubin PJ, Kolls JK (2007) IL-23 mediates inflammatory responses to mucoid Pseudomonas aeruginosa lung infection in mice. Am J Physiol Lung Cell Mol Physiol 292: L519-L528. PubMed: 17071720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Lockhart E, Green AM, Flynn JL (2006) IL-17 Production Is Dominated by γδ T Cells rather than CD4 T Cells during Mycobacterium tuberculosis Infection. The Journal of Immunology 177: 4662-4669. [DOI] [PubMed] [Google Scholar]
- 76. Wu Q, Martin RJ, Rino JG, Breed R, Torres RM et al. (2007) IL-23-dependent IL-17 production is essential in neutrophil recruitment and activity in mouse lung defense against respiratory Mycoplasma pneumoniae infection. Microbes Infect 9: 78-86. doi: 10.1016/j.micinf.2006.10.012. PubMed: 17198762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. MacLennan C, Fieschi C, Lammas DA, Picard C, Dorman SE et al. (2004) Interleukin (IL)-12 and IL-23 Are Key Cytokines for Immunity against Salmonella in Humans. J Infect Dis 190: 1755-1757. doi: 10.1086/425021. PubMed: 15499529. [DOI] [PubMed] [Google Scholar]
- 78. Hooper LV, Littman DR, Macpherson AJ (2012) Interactions Between the Microbiota and the Immune System. Science 336: 1268-1273. doi: 10.1126/science.1223490. PubMed: 22674334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Wolk K, Warszawska K, Hoeflich C, Witte E, Schneider-Burrus S et al. (2011) Deficiency of IL-22 Contributes to a Chronic Inflammatory Disease: Pathogenetic Mechanisms in Acne Inversa . J Immunol 186: 1228-1239. doi: 10.4049/jimmunol.0903907. PubMed: 21148041. [DOI] [PubMed] [Google Scholar]
- 80. Chen Y, Thai P, Zhao YH, Ho YS, DeSouza MM et al. (2003) Stimulation of airway mucin gene expression by interleukin (IL)-17 through IL-6 paracrine/autocrine loop. J Biol Chem 278: 17036-17043. doi: 10.1074/jbc.M210429200. PubMed: 12624114. [DOI] [PubMed] [Google Scholar]
- 81. Kinugasa T, Sakaguchi T, Gu XB, Reinecker H-C (2000) Claudins regulate the intestinal barrier in response to immune mediators. Gastrenterol 118: 1001-1011. doi: 10.1016/S0016-5085(00)70351-9. PubMed: 10833473. [DOI] [PubMed] [Google Scholar]
- 82. D'Elia R, deSchoolmeester ML, Zeef LA, Wright SH, Pemberton AD et al. (2009) Expulsion of Trichuris muris is associated with increased expression of angiogenin 4 in the gut and increased acidity of mucins within the goblet cell. BMC Genomics 10: 492. doi: 10.1186/1471-2164-10-492. PubMed: 19852835. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Paneth cell development and lysozyme production occurs normally in the absence of γδ T cells.
(TIFF)
Intestinal crypt isolation.
(TIF)
qPCR quantitation of Ang4 mRNA expression in small intestinal crypts.
(TIFF)
IL‑22 acts at the transcriptional level to regulate Ang4 expression.
(TIFF)
IL‑22 induces Ang4 mRNA and protein expression and is produced by TCRVγγ+ iIELs.
(TIFF)
Purity of intestinal epithelial cell preparations.
(TIFF)
In vitro stimulated lamina propria cells express IL‑23 mRNA.
(TIFF)