Abstract
An 86-year-old woman presented with sudden back pain. Computed tomography (CT) revealed thrombosed type A acute aortic dissection (AD) with a large ascending aorta. Due to the patient’s advanced age, medical therapy was performed. While an ulcer-like projection was recognized at the ascending aorta on follow-up CT, the patient was eventually discharged without surgery. Four-months follow-up CT showed complete resorption of the thrombus in the false lumen. While the patient was asymptomatic after discharge, 1 year later, CT revealed overt AD involving the ascending aorta. In order to prevent aortic events, we performed graft replacement of the ascending aorta.
Keywords: thrombosed type A acute aortic dissection, redissection, painless dissection
Introduction
Conservative treatment for early thrombosed type A acute aortic dissection has a better prognosis than classic type A acute aortic dissection.1) Spontaneous resolution of the thrombosed false lumen can occur during the healing process. We report our experience of painless redissection of the healed ascending aorta 7 months after disappearance of the thrombosed false lumen.
Case Report
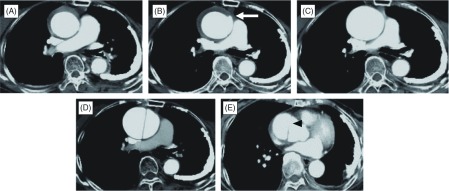
An 86-year-old woman presented with the sudden onset of back penetrating pain. The patient had no medical history of hypertension. Contrast-enhanced computed tomographic (CT) scan revealed early thrombosed type A acute aortic dissection with an ascending aortic diameter of 52 mm and a false lumen thrombosis thickness of 5 mm (Fig. 1A). There were no sign of pericardial effusion or aortic regurgitation (AR). Although the diameter of the ascending aorta exceeded 50 mm, we considered that the patient was a poor candidate for emergent surgery because of her advanced age. We selected the medical treatment including blood pressure- and pulse-controlled medication and complete bed rest during the initial 48 hours. The clinical course under medical management was stable with both the blood pressure and pain well-controlled. However, the patient experienced a recurrent episode of sudden chest pain 3 weeks after the initial onset. CT scan demonstrated that the thrombosed false lumen was thickened even further and an ulcer-like projection (ULP) emerged at the ascending aorta (Fig. 1B). We continued with more intensive blood pressure-controlled treatment. Despite the worsening of the scenario, the patient made satisfactory progress thereafter, and she was discharged 39 days after the initial onset without any surgical interventions.
Fig. 1.
Serial contrast-enhanced computed tomography (CT) images. (A) At onset, CT showed thrombosed type A acute aortic dissection with a large ascending aorta. (B) At 3 weeks after the onset, an ulcer-like projection (ULP) developed at the ascending aorta (white arrow). (C) At 4 months after the onset, outpatient CT revealed complete resolution of the thrombus in the false lumen and complete disappearance of the aortic dissection. (D) At 12 months after the onset, follow-up CT demonstrated overt aortic dissection at the ascending aorta. (E) A new entry (black arrowhead) was evident at the ascending aorta, which was recognized at a different location from the ULP.
On a follow-up CT scan taken 2 months after discharge, the thrombus in the false lumen was resorbed completely and the aortic dissection disappeared with the ascending aortic diameter of 51 mm, which implied the potential for a good prognosis except for being a large ascending aorta (Fig. 1C). However, 1 year later, a repeat CT scan revealed overt aortic dissection involving the ascending aorta with no pericardial effusion (Fig. 1D). The dissected ascending aortic diameter was 55 mm. A new entry was recognized at the right side of the aortic root, which was different from the site of the ULP (Fig. 1E). The patient was asymptomatic during the regular observation at the outpatient clinic. In order to prevent any aortic events, we finally performed graft replacement of the ascending aorta under the selective cerebral perfusion using a 26-mm artificial graft. The patient recovered well without any residual aortic dissection.
Discussion
We experienced an early thrombosed type A aortic dissection which had two clinically important findings: (1) complete resolution of the thrombosed false lumen was achieved following intense medical treatment despite the large ascending aorta greater than 50 mm in diameter at onset and the development of ULP in the early period; (2) redissection occurred in a painless condition several months after disappearance of the false lumen.
The optimal treatment for early thrombosed type A aortic dissection has been an issue of much debate. In the Japanese guideline, the surgical treatment was indicated for patients with cardiac tamponade, aortic regurgitation (AR), large ascending aorta (>50 mm) and thick thrombosed false lumen (>11 mm).2) In our case, while the patient had a large ascending aorta with a diameter of 52 mm, the advanced age of the patient, greater than 85 years, caused us to hesitate in selecting the emergent graft replacement. We chose medical therapy because of the stable hemodynamics with neither cardiac tamponade nor AR. Fortunately, neither recanalization nor redissection occurred during the hospitalization, and the false lumen disappeared completely 4 months after the onset.
Complete resolution of the thrombus in the false lumen is a well-recognized phenomenon after appropriate medical treatment. The rate of disappearance of the false lumen has been reported to be 25% to 71%.3–5) In our case, despite the development of ULP at the large ascending aorta, complete resolution of the false lumen was achieved four months after the onset through intense medical management. This clinical course implied a good prognosis with no need for surgical intervention. However, redissection of the ascending aorta occurred with a new entry at the opposite side of the ULP within 1 year from the first onset. This event suggested that redissection at the remaining large aorta could develop at any time even with complete resolution of the thrombosed false lumen. For this reason, we should care for such high-risk patients with more frequent radiographic follow-up to improve early detection or with a timed surgery to replace the large aorta.
There have been some reports of painless aortic dissection at onset.6) The incidence of painless aortic dissection ranges from 6.4% to 17%.6,7) Imamura and colleagues reported that painless aortic dissection is associated with older age, Stanford type A dissection, and high morbidities such as cerebral ischemia, and cardiac tamponade.6) Our patient was asymptomatic with neither chest pain nor neurological deficit when redissection of the ascending aorta occurred. There was no report describing the association between the redissection and painless condition at the onset of aortic dissection. We need to address the potential for the painless redissection of the previously affected large aorta late after complete absorption of the thrombosed false lumen.
Conclusion
We should be aware of the potential for redissection of the large ascending aorta even after the aortic dissection has disappeared as a result of complete resolution of the thrombosed false lumen. Close radiographic follow-up is necessary for the patients with an ascending aortic diameter greater than 50 mm and a timed surgery is mandatory to avoid catastrophic aortic events.
Disclosure Statement
The author declares no conflict of interest.
References
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000; 283: 897-903. [DOI] [PubMed] [Google Scholar]
- JCS Joint Working Group Guidelines for diagnosis and treatment of aortic aneurysm and aortic dissection (JCS 2011): digest version. Circ J 2013; 77: 789-828. [DOI] [PubMed] [Google Scholar]
- Nishigami K, Tsuchiya T, Shono H, et al. Disappearance of aortic intramural hematoma and its significance to the prognosis. Circulation 2000; 102: III243-7. [DOI] [PubMed] [Google Scholar]
- Song JK, Kim HS, Kang DH, et al. Different clinical features of aortic intramural hematoma versus dissection involving the ascending aorta. J Am Coll Cardiol 2001; 37: 1604-10. [DOI] [PubMed] [Google Scholar]
- Kaji S, Akasaka T, Horibata Y, et al. Long-term prognosis of patients with type a aortic intramural hematoma. Circulation 2002; 106: I248-52. [PubMed] [Google Scholar]
- Imamura H, Sekiguchi Y, Iwashita T, et al. Painless acute aortic dissection. —Diagnostic, prognostic and clinical implications—. Circ J 2011; 75: 59-66. [DOI] [PubMed] [Google Scholar]
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000; 283: 897-903. [DOI] [PubMed] [Google Scholar]