Abstract
Disparities in incarceration rates and in prison-based TB/HIV testing may contribute to health disparities in the communities most affected by incarceration. We analyzed Bureau of Justice Statistics surveys of federal and state prison inmates to assess TB and HIV screening rates for US-born Hispanics, foreign-born Hispanics, non-Hispanic blacks, and non-Hispanic whites. Screening rates were high overall but foreign-born Hispanic inmates had significantly lower odds of being tested for TB in both state (AOR 0.55) and federal prisons (AOR 0.31) compared to white inmates. Foreign-born Hispanics also had lower odds of being tested for HIV in state prisons and Hispanics had lower odds of being tested for HIV in federal prisons compared to white inmates. Screening for infectious diseases in state and federal prisons is high but Hispanics have higher odds of going untested; this has important consequences for prevention of further transmission in the communities to which they return.
Keywords: Incarceration, Prisons, Hispanics, Disparities, HIV, TB
Introduction
The US has the highest incarceration rate in the world, and prisons are mandated to provide certain screenings and healthcare. Correctional facilities thus have the potential to serve as public health sentinels by diagnosing and treating a medically underserved, high-needs population [1, 2]. State and federal prisons screen the vast majority of inmates for selected infectious diseases and other medical conditions, but some remain untested. Although non-Hispanic black, non-Hispanic white, and Hispanic inmates appear to undergo health screening at similar rates for most types of tests, there are disparities in Hispanic screening that may reflect unequal diagnosis and subsequent provision of care. 95 % of state prison inmates eventually return to their communities [3] and those communities are predominantly low-income and non-white. Thus, disparities in screening for infectious disease in prison may contribute to disparities in communities most affected by incarceration.
Background
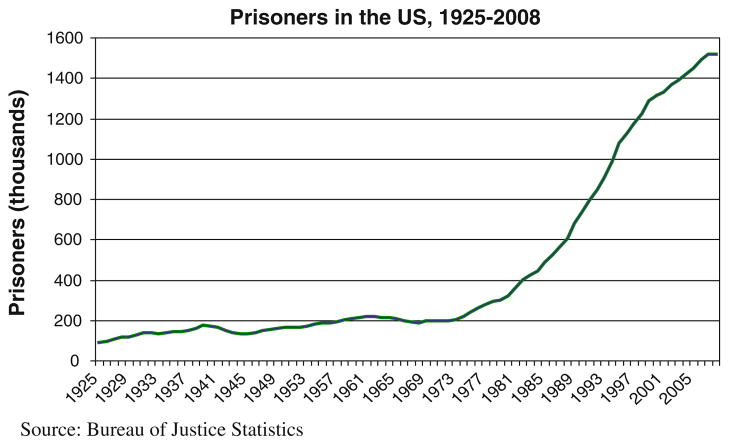
The 30-year-old HIV epidemic largely overlaps with a 40-year-old epidemic of incarceration in the US. Starting in the 1970s, incarceration rates in the US accelerated rapidly (see Fig. 1). Much of the increase stemmed from insufficient community-based mental health services; even more was caused by the war on drugs, which has been especially responsible for the widening racial and ethnic disparities of incarceration [4]. While Hispanics, blacks, and whites use drugs at roughly equal rates, whites are far less likely to be arrested and imprisoned for drug-related offenses [5–8].
Fig. 1.
US incarceration trends, 1925–2005
Prison and jail inmates have a higher disease burden and are more medically underserved than the general population. For some inmates, correctional facilities provide the first sustained health care they have had access to since childhood. Well over 50 % suffer from mental disorders and/or substance dependence [9–11], which can further complicate diagnosis and treatment. Inmates constitute a declining share of the nation’s HIV burden, but 17 % of Americans with HIV—including 22–33 % of Hispanic Americans with HIV—still pass through prisons and jails annually [12]. Prisons constitute a healthcare provider of last resort for the marginalized and an opportunity to link the previously untreated to care, and correctional facilities in some places have become a venue for medical and public health interventions to provide diagnosis, treatment, and prevention [13–17].
However, release back to the community is typically a highly stressful time when former inmates struggle to restore housing, work, and social networks, often resorting to high-risk behaviors as a result. Moreover, HIV treatment is interrupted upon release in about 90 % of all cases, potentially increasing infectiousness and the likelihood of developing a resistant virus [18]. HIV and TB are largely controlled in the US population at large, but incidence remains high in specific demographic pockets. Because releasees are concentrated in low-resource communities and limited social networks, the failure to test and treat them compounds risk in those networks [19–23]. To ensure continuity of care and thereby decrease the risk of transmission following release, prisons and public health officials must work together to develop and implement successful discharge planning. In order to do so, prisons also need to ensure that screening programs are equitably identifying all inmates in need of treatment.
Despite socioeconomic (SES) measures and frequent discrimination comparable to those of blacks, Hispanics have many health measures close to or better than whites, including infant mortality and smoking [24–29]. This so-called Hispanic paradox thus appears to break the close association between SES and health in the US. But the Hispanic health advantage does not extend to HIV and TB: Hispanics overall have higher rates, later diagnosis, later enrollment in care, and worse outcomes of HIV than whites [30, 31]. Because the same risk factors (e.g. drug dependence) contribute to both incarceration and poor health, screening in correctional facilities may provide access to those Hispanics most at risk of delayed diagnosis and care for HIV and other infectious diseases. Other analyses have identified where screening and treatment differ between black and white inmates [32]. We analyzed data from two national surveys of prison inmates to assess screening rates for Hispanic, black, and white inmates, and additionally compared rates for US-born Hispanics and foreign-born Hispanics.
Methods
The Bureau of Justice Statistics and US Census Bureau conduct the Survey of Inmates in Federal Correctional Facilities (SIFCF), Survey of Inmates in State Correctional Facilities (SISCF), and Survey of Inmates in Local Jails (SILJ) every few years. Because jails experience much higher turnover and are therefore more complicated sites for health screenings, only the SIFCF and SISCF were used in this analysis. The surveys employ a two-stage sample design selecting prisons in the first stage and inmates in the second. Of 1,585 state prisons in the US, 301 were selected and 287 participated. Of the 148 eligible federal prisons, 40 were selected of which one refused to participate. Inmates were then randomly selected for interviews regarding criminal, incarceration, personal, and health histories. In the 2004 survey used for this study, the overall response rate was 89.1 % for state inmates and 84.6 % for federal inmates [33].
The independent variable of interest was race/ethnicity as self-reported by inmates. Responses were first categorized as non-Hispanic white, non-Hispanic black, Hispanic, and other. Hispanics were then classified as born in the US or born elsewhere. Analyses were run separately for several dependent variables. The primary outcomes were self-reported testing for TB and HIV during the current incarceration. In addition, inmates were asked about three types of screening upon admission (whether prison staff checked to see if the inmate was sick, injured, or intoxicated; whether staff asked about health or medical history; and whether staff asked about suicidal thoughts or prior suicide attempts) and two questions regarding post-admission processes (whether they had received a medical test and a blood test). All dependent variables were recoded to become binary, with responses of “Don’t know” and refusals removed from the analysis. “Don’t know” responses were then tested separately for racial/ethnic patterns. We ran logistic regressions separately for each outcome variable, controlling for age (categorized as 16–34; 35–49; and 50 or more years), sex, and education level (no high school; some high school; high school degree or GED; and any post-secondary). Income was tested but not included in the final model due to the high number of missing responses (reflecting 16.5 % of state prisoners and 19.5 % of federal prisoners). Because state and federal prisons were in different datasets, and are additionally subject to different testing policies, we ran all models separately for state and federal prisoners. All analyses were conducted in STATA version 11, using survey commands to account for the complex sampling of the SISCF and SIFCF.
Results
The study sample includes 14,250 state prisoners and 3,686 federal prisoners, representing a total state prison population of over 1.2 million and federal prison population of 129,300. In both types of facilities, less than 10 % of prisoners were female and about 50 % were under 35 years old. Just under 50 % of federal inmates and about 61 % of state inmates had less than a high school degree. Compared to state prisons, federal prisons hold a higher percentage of Hispanics (18.9 vs. 12.6 %) and a higher ratio of foreign born-to-US born Hispanics (2:1, compared to 1:2 in state prisons). The unequal distribution of foreign-born versus US-born Hispanics between state and federal facilities reflects the different jurisdiction of offenses of which Hispanics are accused, especially whether they were sentenced under federal immigration or drug laws [34] (Table 1).
Table 1.
Demographic profile of state and federal prison inmates, 2004
| STATE prisons
|
FEDERAL prisons
|
|||
|---|---|---|---|---|
| n | Weighted % | n | Weighted % | |
| Sex | ||||
| Male | 11,407 | 93.3 | 2,728 | 93.0 |
| Female | 2,843 | 6.7 | 958 | 7.0 |
| Race/ethnicity | ||||
| Latino/Hispanic | 1,726 | 12.6 | 688 | 18.9 |
| US-born | 1,185 | 8.4 | 243 | 6.5 |
| Not US-born | 541 | 4.2 | 445 | 12.4 |
| Non-Hispanic black | 5,817 | 41.3 | 1,455 | 43.7 |
| Non-Hispanic white | 5,211 | 35.3 | 1,075 | 26.0 |
| Other | 1,496 | 10.9 | 468 | 11.4 |
| Age group | ||||
| 16–34 | 7,100 | 50.4 | 1,632 | 47.4 |
| 35–49 | 5,808 | 39.7 | 1,506 | 39.8 |
| 50+ | 1,342 | 9.9 | 548 | 12.8 |
| Education | ||||
| < 8th grade | 1,675 | 11.8 | 421 | 12.2 |
| Some high school | 6,837 | 49.0 | 1,277 | 37.3 |
| HS graduate/GED | 3,540 | 25.3 | 912 | 27.6 |
| Some college/degree | 2,029 | 13.9 | 996 | 22.9 |
Data source US Department of Justice, Bureau of Justice Statistics
Table 2 indicates the percentage of inmates receiving different types of screening. The overwhelming majority of both state and federal inmates received medical screening both during and following admission, and rates for most tests were similar for Hispanics, blacks, and whites. The question on HIV testing was the only one for which a significant number of respondents (398 federal prisoners and 1,092 state prisoners) indicated that they did not know if they had been screened: among those who had received a blood test, 14.3 % of whites and 13.2 % of Hispanics in federal prisons did not know if the prison had tested them for HIV, compared to 7.9 % of blacks (data not shown).
Table 2.
Numbers and weighted percentages of state and federal prisoners receiving medical tests, 2004
| State screening | Hispanics born in the US | Hispanics born outside the US | All Hispanics | Blacks | Whites |
|---|---|---|---|---|---|
| n = 1,185 | n = 541 | n = 1,726 | n = 5,817 | n = 5,211 | |
| Medical history taken | 1,028 (88.1) | 465 (87.0) | 1,493 (87.7) | 5,103 (89.1) | 4,535 (88.3) |
| Checked for suicidal thoughts/attempts | 1,028 (88.3) | 446 (83.6) | 1,474 (86.7) | 4,958 (87.2) | 4,539 (88.7) |
| Checked for injury, illness, or intoxication | 844 (73.3) | 403 (75.2) | 1,247 (73.9) | 4,271 (75.4) | 3,727 (73.3) |
| Received a medical exam | 970 (81.4) | 429 (78.5) | 1,399 (80.4) | 4,919 (85.1) | 4,522 (86.5) |
| Received a blood test | 1,024 (87.2) | 466 (87.5) | 1,490 (87.3) | 4,975 (87.5) | 4,538 (88.2) |
| Tested for TB | 1,111 (94.5) | 500 (92.5) | 1,611 (93.8) | 5,460 (95.2) | 4,924 (95.5) |
| Tested for HIV | 815 (85.4) | 338 (79.0) | 1,153 (83.3) | 4,011 (86.1) | 3,408 (84.3) |
| If not tested for HIV in prison: | |||||
| Ever tested for HIV | 208 (56.7) | 60 (27.7) | 268 (45.8) | 1,021 (57.2) | 982 (53.2) |
| Unsure if ever tested for HIV | 26 (8.3) | 39 (19.6) | 65 (12.6) | 140 (8.6) | 190 (11.4) |
|
| |||||
| Federal screening | n = 243 | n = 445 | n = 688 | n = 1,455 | n = 1,075 |
| Medical history taken | 218 (93.9) | 388 (90.1) | 606 (91.4) | 1,301 (91.3) | 967 (90.7) |
| Checked for suicidal thoughts/attempts | 225 (93.5) | 367 (84.6) | 592 (87.7) | 1,283 (90.8) | 965 (92.9) |
| Checked for injury, illness, or intoxication | 194 (84.7) | 351 (83.4) | 545 (83.9) | 1,100 (77.8) | 801 (78.3) |
| Received a medical exam | 220 (91.1) | 385 (87.5) | 605 (88.8) | 1,327 (93.3) | 982 (92.6) |
| Received a blood test | 225 (94.1) | 406 (92.5) | 631 (93.1) | 1,304 (92.) | 1,025 (96.6) |
| Tested for TB | 232 (96.1) | 403 (92.1) | 635 (93.5) | 1,366 (96.4) | 1,021 (97.3) |
| Tested for HIV | 162 (83.6) | 311 (88.3) | 473 (86.8) | 1,099 (91.5) | 802 (93.4) |
| If not tested for HIV in prison: | |||||
| Ever tested for HIV | 40 (41.6) | 52 (41.4) | 92 (41.5) | 215 (64.5) | 119 (44.6) |
| Unsure if ever tested for HIV | 13 (20.0) | 27 (21.6) | 40 (21.0) | 28 (9.3) | 60 (26.5) |
Data source US Department of Justice, Bureau of Justice Statistics
Despite the high rates of screening for all major races/ethnicities, adjusted odds ratios indicate that after controlling for age, sex, and education, there were several points where Hispanics, blacks, and whites were not tested equally. In both state and federal facilities, Hispanics had lower odds of being checked for suicidal thoughts or attempts during admission compared to whites (state AOR 0.81 [95 % CI 0.68–0.97], federal 0.51 [95 % CI 0.33–0.78]) and in state prisons were less likely to receive medical exams post-admission. The differences were especially marked for infectious disease (ID) testing. In both state and federal prisons, Hispanics overall were less likely than whites to be tested for TB (AOR 0.68 [95 % CI 0.53–0.89] for state prisons and 0.40 [95 % CI 0.22–0.72] for federal). Hispanics in federal prisons were half as likely (AOR 0.48; 95 % CI 0.31–0.74) as whites to indicate they had been tested for HIV specifically. In state facilities, differences between Hispanics and whites were not statistically significant for either general blood or HIV testing since admission. However, among state inmates not tested in prison, Hispanics had 0.75 the odds (95 % CI 0.60–0.94) of ever having been tested compared to whites (Table 3).
Table 3.
Odds ratios for state and federal prisoners receiving medical tests, by race/ethnicity with whites as reference (adjusted for age, sex, and education), 2004
| Hispanics born in the US
|
Hispanics born outside the US
|
All Hispanics
|
Blacks | |||||
|---|---|---|---|---|---|---|---|---|
| AOR | 95 % CI | AOR | 95 % CI | AOR | 95 % CI | AOR | 95 % CI | |
| State screening | ||||||||
| Medical history taken | 0.97 | .78–1.2 | 0.96 | .71–1.28 | 0.96 | .80–1.16 | 1.07 | .94–1.22 |
| Checked for suicidal thoughts/attempts | 0.90 | .73–1.11 | 0.67* | .51–.87 | 0.81 * | .68–.97 | 0.82* | .72–.93 |
| Checked for injury/illness/intoxication | 1.02 | .87–1.19 | 1.12 | .89–1.40 | 1.05 | .91–1.20 | 1.13* | 1.03–1.24 |
| Received a medical exam | 0.75* | .62–.90 | 0.60* | .47–.77 | 0.70* | .60–.82 | 0.96 | .85–1.08 |
| Received a blood test | 1.01 | .82–1.24 | 0.93 | .69–1.25 | 0.98 | .82–1.18 | 1 | .88–1.13 |
| Tested for TB | 0.76 | .56–1.04 | 0.55* | .38–.81 | 0.68* | .53–.89 | 0.9 | .74–1.09 |
| Tested for HIV | 1.07 | .85–1.32 | 0.66* | .50–.87 | 0.9 | .75–1.08 | 1.15* | 1.01–1.31 |
| Ever tested for HIV, if not in prison | 1.06 | .81–1.39 | 0.37* | .25–.53 | 0.75* | .60–.94 | 1.1 | .94–1.28 |
| Federal screening | ||||||||
| Medical history taken | 1.51 | .74–3.09 | 0.93 | .56–1.53 | 1.07 | .68–1.68 | 1.1 | .76–1.57 |
| Checked for suicidal thoughts/attempts | 0.90 | .43–1.92 | 0.41* | .26–.66 | 0.51* | .33–.78 | 0.65* | .45–.94 |
| Checked for injury/illness/intoxication | 1.53 | .95–2.46 | 1.39 | .95–2.02 | 1.43* | 1.04–1.98 | 0.96 | .74–1.23 |
| Received a medical exam | 1.04 | .55–1.97 | 0.56* | .34–.90 | 0.69 | .44–1.07 | 1.35 | .90–2.03 |
| Received a blood test | 0.67 | .31–1.44 | 0.48* | .25–.93 | 0.54* | .30–.97 | 0.46* | .30–.75 |
| Tested for TB | 0.72 | .26–1.95 | 0.31* | .17–.58 | 0.40* | .22–.72 | 0.75 | .43–1.3 |
| Tested for HIV | 0.41* | .23–.73 | 0.53* | .32–.88 | 0.48* | .31–.74 | 0.86 | .58–1.27 |
| Ever tested for HIV, if not in prison | 0.66 | .32–1.36 | 0.68 | .36–1.31 | 0.68 | .39–1.18 | 1.62 | .99–2.64 |
Data source US Department of Justice, Bureau of Justice Statistics
p<.05
There were some differences among Hispanics. For multiple outcomes, foreign-born Hispanics’ odds of having been screened were lower than whites’ odds even when US-born Hispanics were not different from whites. The same pattern held for medical exams, blood tests, and TB testing in state as well as federal prisons. In state facilities, US-born Hispanics were 1.6 times more likely to be tested for HIV in prison, and had 2.85 the odds of having ever been tested if they were not, compared to foreign-born Hispanics (data not shown).
Discussion
Researchers are trying to map the complex relationships between incarceration and health disparities. Incarceration may ultimately exacerbate health disparities, affecting a greater percentage of Hispanics and blacks than whites in increasing risks of unemployment, homelessness, and disruption of stable sexual partnerships [35–38]. At the same time, prison-based screening has the potential to identify the health needs of the medically underserved and link them to care. State and federal prisons succeed in screening very high rates of all inmates, but disparities continue among Hispanics, blacks, and whites. Hispanic inmates had lower odds of being screened than white inmates in several, but not all, important measures. These disparities exist in both state and federal prisons with more disparities present in federal prisons than state prison; they were also greater for foreign-born Hispanic inmates than for US-born Hispanic inmates.
There are specific risks which may be overlooked among Hispanics in both state and federal prison-based screening, primarily suicide, medical exams and TB screening. While Hispanic inmates overall had similar odds as whites of being tested for HIV in state prisons, they had less than half the odds of being tested for HIV in federal prisons. This means an important opportunity to both halt transmission and reduce disparities of infectious diseases among Hispanics is lost, particularly given the trends for those inmates who had never been tested for HIV. Prior incarceration did not affect the relative odds of being tested for Hispanics or blacks compared to whites, suggesting that it was not an explanation for testing patterns in the current incarceration (data not shown).
The results for US-born versus foreign-born Hispanics reinforce concerns that the Hispanic paradox is not equally experienced across the diverse US Hispanic population. The few studies examining racial identity among US Hispanics suggest that racial disparities do exist among Hispanics, albeit not to the same extent as among non-Hispanics: for example, Hispanic Blacks have been found to have worse outcomes on self-rated health and hypertension than Hispanic whites [39–41]. Previous research also indicates that as Hispanics acculturate in the US, they improve on some health measures (primarily access to health care) but worsen on others [42–46]. In our study, foreign-born Hispanics had significantly lower odds of all screening except having a medical history taken, being checked for injury/illness/intoxication upon admission, and (in state prisons) receiving a blood test. The differences that we found between US-born and foreign-born Hispanics vis-à-vis incarceration patterns and TB/HIV testing rates in prison indicate that more attention must be paid to potential trends in Hispanic communities. Since TB is more prevalent in Latin American countries, it is particularly important to understand why foreign-born Hispanics are not being tested for it and whether there is any corresponding transmission in predominantly Hispanic communities.
There are a number of limitations to our analysis. Screenings were self-reported and, if inmates had been incarcerated for a significant amount of time, subject to recall bias. It is also possible that Hispanic rates reflect a lower level of comprehension of either the nature of the medical screening or the interview. However, an analysis of patterns of “Don’t know” responses does not suggest this is a primary explanation for disparities in screening rates (data not shown). Among state inmates, adjusted odds ratios for responding “don’t know” were the same for whites and Hispanics. Among federal inmates, Hispanics did have higher odds than whites of responding “don’t know” for several screening questions, but the confidence intervals were unusually wide and the percentage of Hispanics selecting this answer was under 1.5 % for all types of screening except past suicidal tendencies (3 %). Especially notably, Hispanics did not have higher odds than whites of saying “don’t know” on the question of HIV testing. We were also not able to speculate on the causes of disparities in testing, and especially whether they resulted from protocols, staff decisions, or inmate requests.
Conclusion
While the overall percentage of prison inmates screened for infectious diseases is much higher than in the general population, screening in state and federal prisons may not be capturing Hispanics in need of linkage to health care at the same rates as whites, though similar rates for most other screenings indicate that disparities may not be systemic. Because the US Hispanic population is both younger and growing more rapidly than other major races/ethnicities and because Hispanics are disproportionately affected by the epidemic of incarceration in the US, both the effects and opportunities of their incarceration will assume an increasing importance in overall public health. Public health and correctional officials should work together to understand why Hispanics are not being tested for IDs at the same rate as whites.
Acknowledgments
Dr. Rich’s work for this project was supported by NIDA Midcareer Investigator Award 5K24DA22112-4 and NIH-funded Center for AIDS Research (P30-AI-42853). Dr. Chen was supported by a diversity supplement provided through NIDA R01DA028692-02S1. All authors report that they have no conflicts of interest or financial disclosures to report.
Contributor Information
Dora M. Dumont, Email: ddumont1@lifespan.org, The Center for Prisoner Health, The Miriam Hospital, 1125 North Main Street, Providence, RI 02909, USA
Annie Gjelsvik, Email: annie_gjelsvik@brown.edu, Department of Epidemiology, Brown University, Providence, RI, USA.
Nadine Chen, Email: nadinechen@ucsd.edu, Division of Global Public Health, University of California, San Diego, San Diego, CA, USA.
Josiah D. Rich, Email: jrich@lifespan.org, Division of Infectious Diseases, The Miriam Hospital, Providence, RI, USA. Brown University Medical School, Providence, RI, USA
References
- 1.Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78(2):214–35. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rich JD, Wakeman SE, Dickman SL. Medicine and the epidemic of incarceration in the United States. N Engl J Med. 2011;364(22):2081–3. doi: 10.1056/NEJMp1102385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hughes T, Wilson D. Reentry trends in the United States. Washington, DC: Bureau of Justice Statistics, Department of Justice; 2004. [Google Scholar]
- 4.Dumont D, Brockmann B, Dickman S, Alexander N, Rich J. Public health and the epidemic of incarceration. Ann Rev Public Health. 2012;33:325–39. doi: 10.1146/annurev-publhealth-031811-124614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blacks Targeting. drug law enforcement and race in the United States. New York: Human Rights Watch; 2008. [Google Scholar]
- 6.Fellner J. Decades of disparity: drug arrests and race in the United States. New York: Human Rights Watch; 2009. [Google Scholar]
- 7.Alexander M. The new Jim Crow: mass incarceration in the age of colorblindness. New York: The New Press; 2010. [Google Scholar]
- 8.Provine D. Unequal under law: race in the war on drugs. Chicago: University of Chicago Press; 2007. [Google Scholar]
- 9.Binswanger IA, Krueger PM, Steiner JF. Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health. 2009;63(11):912–9. doi: 10.1136/jech.2009.090662. [DOI] [PubMed] [Google Scholar]
- 10.James DJ, Glaze LE. Mental health problems of prison and jail inmates. Washington, DC: Bureau of Justice Statistics; 2006. [Google Scholar]
- 11.Lamb HR, Weinberger LE. The shift of psychiatric inpatient care from hospitals to jails and prisons. J Am Acad Psychiatry Law. 2005;33(4):529–34. [PubMed] [Google Scholar]
- 12.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. J Acquir Immune Defic Syndr. 2010;55(Suppl 1):S49–55. doi: 10.1097/QAI.0b013e3181f9c0f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA. 2009;301(2):183–90. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark BC, Grossman E, White MC, Goldenson J, Tulsky JP. Diabetes care in the San Francisco County jail. Am J Public Health. 2006;96(9):1571–4. doi: 10.2105/AJPH.2004.056119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conklin T, Lincoln T, Wilson R. A public health manual for correctional health care. Ludlow, MA: Hampden County Sheriff’s Department and Massachusetts Public Health Association; 2002. [Google Scholar]
- 17.Wakeman SE, Rich JD. HIV treatment in US prisons. HIV Ther. 2010;4(4):505–10. doi: 10.2217/hiv.10.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301(8):848–57. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson R, Raphael S. The effects of male incarceration dynamics on acquired immune deficiency syndrome Infection rates among African American women and men. J Law Econ. 2009;52:251–93. [Google Scholar]
- 20.Khan MR, Epperson MW, Mateu-Gelabert P, Bolyard M, Sandoval M, Friedman SR. Incarceration, sex with an STI- or HIV-infected partner, and infection with an STI or HIV in Bushwick, Brooklyn, NY: a social network perspective. Am J Public Health. 2011;101(6):1110–7. doi: 10.2105/AJPH.2009.184721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas JC, Levandowski BA, Isler MR, Torrone E, Wilson G. Incarceration and sexually transmitted infections: a neighborhood perspective. J Urban Health. 2008;85(1):90–9. doi: 10.1007/s11524-007-9231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rogers SM, Khan MR, Tan S, Turner CF, Miller WC, Erbelding E. Incarceration, high-risk sexual partnerships and sexually transmitted infections in an urban population. Sex Transm Infect. 2012;88(1):63–8. doi: 10.1136/sextrans-2011-050280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Sadr WM, Mayer KH, Hodder SL. AIDS in America–forgotten but not gone. N Engl J Med. 2010;362(11):967–70. doi: 10.1056/NEJMp1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franzini L, Ribble JC, Keddie AM. Understanding the hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- 25.Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44(3):441–57. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maher J, Boysun M, Rohde K, Stark M, Pizacani B, Dilley J, et al. Are Latinos really less likely to be smokers? Lessons from Oregon. Nicotine Tob Res. 2005;7(2):283–7. doi: 10.1080/14622200500056259. [DOI] [PubMed] [Google Scholar]
- 27.Pallodi A, Arias E. Paradox lost: explaining the hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 28.Pallodi A, Morenoff J. Interpreting the paradoxical in the hispanic paradox: demographic and epidemiologic approaches. Ann NY Acad Sci. 2001;954:140–74. doi: 10.1111/j.1749-6632.2001.tb02751.x. [DOI] [PubMed] [Google Scholar]
- 29.Perez-Stable EJ, Ramirez A, Villareal R, Talavera GA, Trapido E, Suarez L, et al. Cigarette smoking behavior among US Latino men and women from different countries of origin. Am J Public Health. 2001;91(9):1424–30. doi: 10.2105/ajph.91.9.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen NE, Gallant JE, Page KR. A systematic review of HIV/ AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2011;14(1):65–81. doi: 10.1007/s10903-011-9497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gonzalez JS, Hendriksen ES, Collins EM, Duran RE, Safren SA. Latinos and HIV/AIDS: examining factors related to disparity and identifying opportunities for psychosocial intervention research. AIDS Behav. 2009;13(3):582–602. doi: 10.1007/s10461-008-9402-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosen DL, Hammond WP, Wohl DA, Golin CE. Disease prevalence and use of health care among a national sample of black and white male state prisoners. J Health Care Poor Underserved. 2012;23(1):254–72. doi: 10.1353/hpu.2012.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bureau of Justice Statistics DoJ. Survey of inmates in state and federal correctional facilities, 2004. Washington, D.C: Inter-University Consortium for Political and Social Research; 2007. [Google Scholar]
- 34.Lopez M, Light M. A rising share: hispanics and federal crime. Washington, DC: Pew Research Center; 2009. [Google Scholar]
- 35.Iguchi MY, Bell J, Ramchand RN, Fain T. How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved. 2005;16(4 Suppl B):48–56. doi: 10.1353/hpu.2005.0114. [DOI] [PubMed] [Google Scholar]
- 36.Massoglia M. Incarceration as exposure: the prison, infectious disease, and other stress-related illnesses. J Health Soc Behav. 2008;49(1):56–71. doi: 10.1177/002214650804900105. [DOI] [PubMed] [Google Scholar]
- 37.Massoglia M. Incarceration, health, and racial disparities in health. Law Soc Rev. 2008;42(2):275–305. [Google Scholar]
- 38.Wildeman C. Invited commentary: (Mass) imprisonment and (inequities in) health. Am J Epidemiol. 2011;173(5):488–91. doi: 10.1093/aje/kwq420. [DOI] [PubMed] [Google Scholar]
- 39.Borrell LN. Race, ethnicity, and self-reported hypertension: analysis of data from the National Health Interview Survey, 1997–2005. Am J Public Health. 2009;99(2):313–9. doi: 10.2105/AJPH.2007.123364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Borrell LN, Crawford ND. Disparities in self-reported hypertension in hispanic subgroups, non-hispanic black and non-hispanic white adults: the national health interview survey. Ann Epidemiol. 2008;18(10):803–12. doi: 10.1016/j.annepidem.2008.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Borrell LN, Dallo FJ. Self-rated health and race among Hispanic and non-Hispanic adults. J Immigr Minor Health. 2008;10(3):229–38. doi: 10.1007/s10903-007-9074-6. [DOI] [PubMed] [Google Scholar]
- 42.Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61(6):1243–55. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bethel JW, Schenker MB. Acculturation and smoking patterns among hispanics: a review. Am J Prev Med. 2005;29(2):143–8. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 44.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77(6):1707–46. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 45.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaplan MS, Huguet N, Newsom JT, McFarland BH. The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med. 2004;27(4):323–6. doi: 10.1016/j.amepre.2004.07.005. [DOI] [PubMed] [Google Scholar]