Abstract
The present study examined temporal dependencies of change of panic symptoms and two promising mechanisms of change (self-efficacy and anxiety sensitivity) during an 11-session course of cognitive-behavior therapy (CBT) for Panic Disorder (PD). 361 individuals with a principal diagnosis of PD completed measures of self-efficacy, anxiety sensitivity, and PD symptoms at each session during treatment. Effect size analyses indicated that the greatest changes in anxiety sensitivity occurred early in treatment, whereas the greatest changes in self-efficacy occurred later in treatment. Results of parallel process latent growth curve models indicated that changes in self-efficacy and anxiety sensitivity across treatment uniquely predicted changes in PD symptoms. Bivariate and multivariate latent difference score models indicated, as expected, that changes in anxiety sensitivity and self-efficacy temporally preceded changes in panic symptoms, and that intraindividual changes in anxiety sensitivity and self-efficacy independently predicted subsequent intraindividual changes in panic symptoms. These results provide strong evidence that changes in self-efficacy and anxiety sensitivity during CBT influence subsequent changes in panic symptoms, and that self-efficacy and anxiety sensitivity may therefore be two distinct mechanisms of change of CBT for PD that have their greatest impact at different stages of treatment.
Keywords: Panic disorder, Mechanisms of change, CBT, Self-efficacy, Anxiety sensitivity, Latent difference score
The unique effects of self-efficacy and anxiety sensitivity
Decades of research have demonstrated that cognitive behavior therapy (CBT) is an effective treatment for panic disorder with and without agoraphobia (PD) (Craske & Barlow, 2013). Large randomized controlled trials have demonstrated that CBT results in superior outcomes to placebo and similar outcomes to medication at post-treatment, as well as greater durability at follow-up points (Barlow, Gorman, Shear, & Woods, 2000). Multiple meta-analyses have demonstrated that CBT has large effects on PD (e.g., Mitte, 2005; Westen & Morrison, 2001). Although there is now extensive evidence for the efficacy of CBT for PD, less is known about the mechanisms of change of CBT for PD. The present study examines two potential mechanisms of change of CBT for PD: self-efficacy beliefs and anxiety sensitivity.
Self-efficacy beliefs represent individuals’ perceptions that they will be able to execute the actions necessary to achieve desired outcomes. Self-efficacy beliefs have been proposed to be a transdiagnostic mechanism of change for psychological treatments and to play an important role in the development and treatment of anxiety (Bandura, 1977, 1988, 1997). CBT for PD is thought to promote self-efficacy primarily through mastery experiences in which patients develop the belief that they are able to effectively cope with panic related sensations, as well as through social persuasion by the therapist through discussion of the true dangers of panic symptoms and encouragement regarding that patient’s ability to cope with panic symptoms (Casey, Oei, & Newcombe, 2004). Self-efficacy beliefs have been shown to predict PD symptom severity (Richards, Richardson, & Pier, 2002; Telch, Brouillard, Telch, Agras, & Taylor, 1989), and there is promising evidence that self-efficacy may be a mechanism of change of CBT for PD (Bouchard et al., 2007; Casey, Newcombe, & Oei, 2005; Reilly, Peterson, Gursky, & McNally, 2005).
Anxiety sensitivity is another promising mechanism of change of CBT for PD. Anxiety sensitivity reflects a fear of anxiety-related bodily sensations that is thought to be particularly relevant to the development of PD (Bentley et al., 2013; McNally, 2002; Reiss, Peterson, Gursky, & McNally, 1986; Taylor et al., 2007), although recent meta-analytic reviews suggest that anxiety sensitivity may be an important factor across all the anxiety disorders (Naragon-Gainey, 2010). CBT for PD is thought to produce decreases in anxiety sensitivity by providing psychoeducation about the true dangers of anxiety related bodily sensations, cognitive restructuring of catastrophic appraisals of anxiety related bodily sensations, and by helping individuals develop a tolerance of these sensations through interoceptive and in vivo exposure exercises (Barlow, 1988; 2002; Craske & Barlow, 2013). Previous research has demonstrated that anxiety sensitivity changes following CBT (Shear, Houck, Greeno, & Masters, 2001; Smits, Berry, Tart, & Powers, 2008) and there is promising evidence that anxiety sensitivity may be a mechanism of change of CBT for PD (Reilly, Gill, Dattilio, & Mc Cormick, 2005; Smits, Powers, Cho, & Telch, 2004).
Limitations of current mechanisms research
Although the existing research examining self-efficacy and anxiety sensitivity as mechanisms of CBT for PD is promising, there are some crucial limitations. The primary limitation of the majority of previous research examining potential mechanisms of CBT for PD is the failure to demonstrate the temporal precedence of change in the proposed mechanisms. Without evidence demonstrating that change in hypothesized mechanisms precedes symptom change, it is impossible to determine whether a hypothesized mechanism is truly a mechanism of change rather than simply a correlate or consequence of symptom change (Kazdin, 2007). With a few recent notable exceptions that have provided promising evidence that cognitive changes may precede symptom change (e.g., Bouchard et al., 2007; Teachman, Marker, & Clerkin, 2010), the majority of previous examinations of mechanisms of change have relied on designs (i.e., pre-post assessments) that do not permit conclusions regarding temporality.
A second common limitation in mechanisms research is the failure to use methods of data analysis that allow for the appropriate modeling of idiographic change. Many approaches to longitudinal data analysis (i.e., panel models; Cole & Maxwell, 2003) focus on interindividual standing across time rather than intraindividual differences across time (Selig & Preacher, 2009). Given that current theories regarding hypothesized mechanisms of change of CBT almost universally focus on intraindividual changes thought to occur during treatment, it is crucial that appropriate methods of data analysis (e.g., latent difference score models; McArdle, 2001) are used that permit conclusions regarding idiographic processes of change (Molenaar & Campbell, 2009). As with the issue of temporal precedence of change, a focus on idiographic methods of data analysis has increased in recent years (e.g., Teachman, Marker, & Smith-Janik, 2008; Teachman et al., 2010), but the majority of previous research examining mechanisms of CBT for PD used methods of data analysis that do not focus on intraindividual change. Additionally, previous research has typically examined potential mechanisms of change in isolation, thereby preventing conclusions regarding whether hypothesized mechanisms of change have unique effects on treatment outcome. Our current understanding of when and how anxiety sensitivity and self-efficacy may change during treatment and therefore potentially function as unique mechanisms of CBT for PD remains limited.
The present study
The goal of the present study was to determine whether self-efficacy beliefs and anxiety sensitivity function as two distinct mechanisms of change of CBT for PD. Anxiety sensitivity and self-efficacy beliefs were chosen a-priori as two mechanisms of change that may each play in important role in promoting recovery during CBT for PD. Anxiety sensitivity was initially conceptualized as a vulnerability factor that would be particularly relevant to PD (Reiss et al., 1986), and subsequent research has demonstrated that PD is associated with higher levels of anxiety sensitivity than each of the other anxiety disorders with the exception of post-traumatic stress disorder (Olatunji & Wolitzki-Taylor, 2009). The reduction of anxiety sensitivity may therefore be a mediator of treatment response that is particularly relevant during CBT for PD. In contrast, self-efficacy beliefs have been shown to be a transdiagnostic factor relevant across the anxiety disorders (Bandura, 1997), and were originally conceptualized as a transdiagnostic mechanism of change that would play an important role across different disorders (Bandura, 1977). The simultaneous examination of both anxiety sensitivity and self-efficacy as potential mechanisms of change would therefore allow us to examine the relative role that diagnosis specific (i.e., anxiety sensitivity) and transdiagnostic (i.e., self-efficacy) factors may play as unique mechanisms of CBT for PD.
We examined the effects of CBT on self-efficacy and anxiety sensitivity using data from a large clinical trial of CBT for PD (Aaronson et al., 2008). In addition to demonstrating the effects of CBT on self-efficacy and anxiety sensitivity during treatment for PD, we were particularly interested in examining 1) whether temporal change in self-efficacy and anxiety sensitivity preceded change in PD symptoms, and 2) whether changes in self-efficacy and anxiety sensitivity uniquely predicted changes in PD symptoms. We hypothesized that CBT would produce large changes in self-efficacy and anxiety sensitivity, that intraindividual changes in self-efficacy and anxiety sensitivity would both uniquely predict intraindividual changes in PD symptoms, and that changes in self-efficacy and anxiety sensitivity would temporally precede changes in PD symptoms, thus providing strong evidence that self-efficacy and anxiety sensitivity function as two distinct mechanisms of change of CBT for PD.
Method
Participants and procedure
The sample was 361 individuals who participated in a large multi-site randomized controlled trial examining long term treatment strategies for PD (Aaronson et al., 2008). In the original study, 379 adult individuals with PD completed a baseline diagnostic interview and attended at least one treatment session. The present study focuses on data from the acute treatment phase for the 361 participants who completed the measures of self-efficacy, anxiety sensitivity, and PD at one or more sessions. The majority (64.7%) of these participants were female, with a mean age of 37.1 years (SD = 11.7 years). The racial background of the sample was 86.8% Caucasian, 5.8% Asian/Pacific Islander, 5.2% African American, and 2.2% other. All participants received CBT based on a modification of the protocol developed by Barlow and Craske (2007). The acute phase of treatment consisted of eleven sessions that could take place over a maximum of eighteen weeks. See Aaronson et al. (2008) for a detailed description of the original study and White et al. (2010) for additional information about attrition during the acute treatment phase.
Measures
Panic disorder symptoms
The self-report version of the Panic Disorder Severity Scale (PDSS-SR; Houck, Spiegel, Shear, & Rucci, 2002; Shear et al., 1997) was used to measure the course of PD symptoms during treatment. The PDSS-SR is a seven-item patient self-report measure that assesses the severity of seven dimensions of PD: frequency of panic attacks, distress during panic attacks, anticipatory anxiety, agoraphobic fear and avoidance, interoceptive fear and avoidance, impairment in work functioning, and impairment in social functioning. A total score is generated (range = 0–28), with higher scores indicating greater severity. The PDSS-SR has demonstrated good psychometric properties (α = .92; Houck et al., 2002). Participants completed the PDSS-SR at each of the 11 treatment sessions. The internal consistency of the PDSS-SR in the present study across assessments was good (α = .91).
Anxiety sensitivity
Anxiety sensitivity was measured using the Anxiety Sensitivity Index (ASI; Reiss et al., 1986). The ASI is a widely used sixteen item scale that measures fear of bodily sensations. Factor analytic studies of the ASI have indicated that the ASI measures three lower-order facets (i.e., physical, cognitive, and social concerns) of anxiety sensitivity that each load on a higher order factor of anxiety sensitivity (Zinbarg, Barlow, & Brown, 1997). The mean response to the 16 items was used in the present study as a continuous indicator of the higher order factor of anxiety sensitivity. Although anxiety sensitivity was initially conceptualized as a continuous dimension of vulnerability, some researchers (e.g., Bernstein et al., 2007) have proposed that anxiety sensitivity is best conceptualized in terms of dimensions of vulnerability within distinct latent taxonic classes. However, evidence for a categorical dimensional model is mixed, as although some recent studies have supported this conceptualization of anxiety sensitivity (e.g., Bernstein, Zvolensky, Marshall, & Schmidt, 2009; Bernstein, Stickle, & Schmidt, 2013), a recent taxometric investigation of anxiety sensitivity provided consistent support for a dimensional conceptualization of anxiety sensitivity (Broman-Fulks et al., 2010). We chose to model anxiety sensitivity as a continuous latent dimension for all analyses in the present study. We chose to focus on the higher order anxiety sensitivity construct as previous research has demonstrated that the higher order factor accounts for the majority of the variance in ASI scores (Zinbarg et al., 1997), and unlike more recent measures of anxiety sensitivity such as the Anxiety Sensitivity Index-3 (Taylor et al., 2007), the original ASI was not constructed to assess the three lower order facets of anxiety sensitivity. Participants completed the ASI at each of the 11 treatment sessions. The internal consistency of the ASI in the present study across assessments was good (α = .93).
Self-efficacy
Self-efficacy beliefs for PD related sensations and experiences were measured with a ten-item scale that was developed for this study in a manner consistent with Bandura’s (2006) guide for constructing self-efficacy scales. The measure lists five situations that individuals with PD commonly avoid due to interoceptive sensitivity and avoidance (e.g., exercising vigorously alone) and five situations that individuals with PD commonly avoid due to agoraphobia (e.g., going long distances from home alone).1 For each situation, participants were asked to rate “How confident you are that you could do it” using a 0 to 100 scale, where 0 = “absolutely sure you couldn’t do it” and 100 = “absolutely sure you could do it.” The mean response to the ten items was used in the present study. Participants completed the self-efficacy questionnaire at each of the 11 treatment sessions. The internal consistency of the self-efficacy questionnaire in the present study across assessments was good (α = .89).
Data analysis strategy
We began by examining session-by-session and cumulative changes in self-efficacy, anxiety sensitivity, and PD symptoms. As would be expected in a clinical trial, there was a moderate amount of missing data due to participant attrition (White et al., 2010). Full-information maximum likelihood (FIML) estimation procedures were used to account for the missing data in all analyses. FIML methods use all of the available data to provide appropriate estimates of parameters and standard errors while accounting for missing data, and are currently considered a best-practice method of handling missing data (Enders, 2010). We first obtained FIML estimates of the means and standard deviations of the three outcomes across the eleven assessments. These FIML estimates were then used to calculate effect sizes for the session-by-session and cumulative change in the three outcomes during treatment. The standardized mean gain (ESsg) was used as the effect size for these analyses (Lipsey & Wilson, 2001). ESsg can be interpreted in a similar fashion to Cohen’s d, but is a more appropriate effect size for intraindividual change as it includes a correction for the association between two assessments due to repeated measurement. The results of the ESsg effect size analyses were used to quantify the temporal course of change in the hypothesized mechanisms and panic symptoms.
Latent growth curve modeling (Duncan, Duncan, & Strycker, 2006; Preacher, Wichman, MacCallum, & Briggs, 2008) was then used to model the relationships between intraindividual trajectories of change in PD symptoms, anxiety sensitivity, and self-efficacy during the course of CBT treatment. Parallel process latent growth curve models were used to examine 1) the associations between change in the three constructs of interest (PD symptoms, anxiety sensitivity, and self-efficacy), and 2) the unique effects of change in self-efficacy and change in anxiety sensitivity on change in PD symptoms.
Latent difference score models (LDS; McArdle, 2001, 2009) were then used to examine the temporal dynamics between intraindividual changes in self-efficacy, anxiety sensitivity, and panic symptoms. LDS models are a relatively recent development in latent variable modeling and are ideally suited for the examination of the temporal dynamics between change in one or more variables (Ferrer & McArdle, 2010; Hawley, Ho, Zuroff, & Blatt, 2006; King et al., 2006; Sbarra & Allen, 2009). The primary advantage of the LDS approach is that it permits the modeling of the true, latent change between two assessments of a variable. LDS models are therefore similar to traditional difference scores in that they quantify intraindividual change between two assessments, but retain all of the advantages of latent variable modeling (i.e., accounting for measurement error). Within the LDS framework, the longitudinal course of any variable can be modeled in terms of the initial status on the variable and the accumulation of differences between each assessment. Intraindividual change in the LDS models is most commonly quantified using the following equation:
| (1) |
where Δy[t] represents the latent change in variable y at time t, αy represents the constant change coefficient (typically constrained to equality across time) associated with the underlying slope ys, βy represents the proportional change coefficient (can be constrained or freely estimated across time) of the same variable at the previous time component (y[t − 1]). This model is referred to as the dual change score model, and represents latent change as the combination of a constant underlying growth process represented by the αy parameter, and a self-feedback process represented by the βy parameter, that together model intraindividual trajectories of change as the accumulation of differences between assessments up to that point. The dual change score model can be directly compared to competing models to determine the most appropriate method of modeling growth (i.e., a constant change model in which a constant growth parameter is included but no proportional effects are modeled). For the present study, a series of univariate LDS models was first specified to determine the most appropriate method of modeling change in self-efficacy, anxiety sensitivity, and panic symptoms.
After determining the most appropriate univariate LDS model for each construct, bivariate LDS models were specified next to determine the temporal dynamics of change between self-efficacy and panic symptoms, and anxiety sensitivity and panic symptoms. Intraindividual change in the bivariate LDS model is quantified using the following equation:
| (2) |
which extends the univariate model by including a coupling parameter γ to represent the effect of one variable on subsequent change in the other variable. These coupling parameters are included for both outcomes, which allows for an examination of the reciprocal temporal dependencies in change of two variables. The coupling parameters can be freely estimated or constrained to equality across time. For the present study a series of bivariate models were specified to determine the most appropriate method of modeling the coupling between self-efficacy and panic symptoms, and anxiety sensitivity and panic symptoms.
Our final analysis extended the bivariate LDS model to a multivariate model that included all three outcomes based on the following equation:
| (3) |
This multivariate LDS model allowed for an examination of the unique effects that change in self-efficacy beliefs and anxiety sensitivity had on subsequent change in panic symptoms, while also modeling the reciprocal effects of change in panic symptoms on change in self-efficacy and anxiety sensitivity. As the temporal dependencies between self-efficacy and anxiety sensitivity were not the focus of the present study, in the interest of parsimony the latent difference scores of self-efficacy and anxiety sensitivity were allowed to freely covary with one another rather than specifying temporal dependencies between change in these variables.
All analyses were conducted using FIML estimation procedures in MPlus 5.1 (Muthén & Muthén, 2007). Model fit for the latent growth curve and latent difference score models was evaluated using the root mean square error of approximation (RMSEA; Steiger & Lind, 1980), the standardized root mean residual (SRMR; Jöreskog & Sörbom, 1996), the comparative fit index (CFI; Bentler, 1990), and the nonnormed fit index (NNFI; Bentler & Bonett, 1980).
Results
Temporal course of change during treatment
We began by examining the FIML estimates of the means and standard deviations of self-efficacy, anxiety sensitivity, and PD symptoms in order to determine the overall change in these constructs during treatment and to determine when this change occurred. Table 1 presents the session by session FIML estimates of the means and standard deviations of self-efficacy, anxiety sensitivity, and PD symptoms as well as the session-by-session and cumulative effect sizes (ESsg). As can be seen in Table 1, there were large cumulative effects for self-efficacy (ESsg = .87), anxiety sensitivity (ESsg = −1.45), and PD symptoms (ESsg = −1.16). These results indicate that treatment produced large changes in each construct, with the largest change occurring for anxiety sensitivity. However, the estimate of change in self-efficacy beliefs may be downwardly biased by a ceiling effect as seventy individuals (19.4%) had reported the maximum level of self-efficacy on every question by the end of treatment.
Table 1.
Full information maximum likelihood (FIML) estimates (n = 361) of weekly means, standard deviations (SD), and weekly/cumulative effect sizes (ESsg) with 95% confidence intervals for self-efficacy, anxiety sensitivity, and panic disorder symptoms.
| Outcome | Session | FIML estimates
|
Weekly change
|
Cumulative change
|
|||
|---|---|---|---|---|---|---|---|
| Mean | SD | ESsg | 95% CI | ESsg | 95% CI | ||
| Self-efficacy | 1 | 68.60 | 22.93 | – | – | – | – |
| 2 | 69.33 | 22.94 | .03 | −.03:.09 | .03 | −.03:.09 | |
| 3 | 71.18 | 23.19 | .08 | .03:.13 | .11 | .05:.18 | |
| 4 | 73.46 | 22.63 | .10 | .05:.15 | .21 | .14:.28 | |
| 5 | 75.62 | 22.04 | .09 | .04:.15 | .30 | .23:.38 | |
| 6 | 77.63 | 20.47 | .09 | .05:.13 | .40 | .32:.48 | |
| 7 | 77.70 | 21.04 | .00 | −.03:.04 | .40 | .32:.49 | |
| 8 | 80.64 | 18.87 | .14 | .09:.18 | .54 | .45:.63 | |
| 9 | 82.72 | 18.98 | .11 | .06:.16 | .63 | .53:.73 | |
| 10 | 85.66 | 17.19 | .15 | .11:.18 | .78 | .67:.89 | |
| 11 | 87.29 | 17.20 | .09 | .06:.12 | .87 | .75:.98 | |
| Anxiety sensitivity | 1 | 2.18 | .73 | – | – | – | – |
| 2 | 2.00 | .72 | −.25 | −.19: −.30 | −.25 | −.19: −.30 | |
| 3 | 1.85 | .73 | −.21 | −.16: −.27 | −.46 | −.38: −.53 | |
| 4 | 1.74 | .79 | −.13 | −.08: −.19 | −.57 | −.48: −.66 | |
| 5 | 1.62 | .81 | −.15 | −.10: −.19 | −.72 | −.61: −.82 | |
| 6 | 1.52 | .78 | −.13 | −.08: −.18 | −.87 | −.75: −.98 | |
| 7 | 1.46 | .80 | −.07 | −.03: −.11 | −.93 | −.81: −1.05 | |
| 8 | 1.35 | .78 | −.13 | −.10: −.17 | −1.09 | −.96: −1.22 | |
| 9 | 1.29 | .78 | −.08 | −.04: −.12 | −1.17 | −1.03: −1.31 | |
| 10 | 1.20 | .76 | −.12 | −.07: −.16 | −1.32 | −1.17: −1.47 | |
| 11 | 1.10 | .77 | −.13 | −.09: −.17 | −1.45 | −1.30: −1.61 | |
| Panic disorder symptoms | 1 | 11.29 | 5.58 | – | – | – | – |
| 2 | 10.36 | 5.20 | −.16 | −.09: −.23 | −.16 | −.09: −.23 | |
| 3 | 9.44 | 5.41 | −.17 | −.10: −.24 | −.33 | −.24: −.41 | |
| 4 | 9.20 | 5.45 | −.04 | .03: −.11 | −.36 | −.27: −.46 | |
| 5 | 8.10 | 5.49 | −.20 | −.13: −.28 | −.57 | −.46: −.67 | |
| 6 | 7.80 | 5.24 | −.05 | .03: −.13 | −.63 | −.52: −.73 | |
| 7 | 7.55 | 5.26 | −.04 | .03: −.11 | −.67 | −.56: −.78 | |
| 8 | 7.28 | 5.04 | −.05 | .02: −.12 | −.73 | −61: −.84 | |
| 9 | 6.57 | 4.89 | −.14 | −.06: −.21 | −.86 | −.74: −.99 | |
| 10 | 5.95 | 4.55 | −.12 | −.05: −.20 | −1.01 | −.87: −1.15 | |
| 11 | 5.16 | 4.60 | −.18 | −.10: −.25 | −1.16 | −1.02: −1.30 | |
Note: Positive effect sizes indicate an increase during treatment, negative effect sizes indicate a decrease during treatment.
We next examined the session-by-session effect sizes to determine whether changes in self-efficacy, anxiety sensitivity, and PD symptoms occurred at different times during the course of treatment. Results indicated that the largest changes in anxiety sensitivity occurred during the first few sessions that emphasize psychoeducation, breathing retraining and cognitive restructuring, prior to the start of interoceptive exposure exercises. In contrast, the largest session to session changes in self-efficacy occurred during the later sessions of CBT that emphasize interoceptive and situational exposure exercises. The effect size results for PD symptoms indicated that there may have been two discrete periods of change in panic symptoms. There was a medium effect from sessions one to five (ESsg = −.57) and a medium effect from sessions eight to eleven (ESsg = −.43), with less change occurring during the middle of treatment from sessions five to eight. Together these results suggest that change in self-efficacy, anxiety sensitivity, and PD symptom severity during the course of CBT treatment may not occur in a linear fashion, and that the majority of change in these constructs may occur at different periods during the course of treatment.
Trajectories of change
We used latent growth curve modeling to examine the relationship between initial status (i.e., scores at session 1) and changes in self-efficacy, anxiety sensitivity, and PD symptoms across treatment. Preliminary analyses supported the specification of a parallel process latent growth curve model in which freely estimated slope factors were specified for self-efficacy, anxiety sensitivity, and PD symptoms. These slope factors were identified by fixing the loading of the first session scores on the slope factors to 0, the loading of the last session scores on the slope factors to 1.0, and freely estimating the loadings of scores at sessions 2–10 on the slope factor. The mean and variance of the slope factors in these models reflect the total change in and individual differences in change in each construct, respectively. The associations between the intercept and slope factors for each latent construct were freely estimated. Residual covariances between the three measures at each assessment (e.g., self-efficacy scores at session 2 with anxiety sensitivity at session 2) were specified to capture time-specific covariations between the measures. The model fit of this latent growth curve model was acceptable: χ2 (501) = 1657.20, p < .001; RMSEA = .08, 90% CI: .076, .084, CFI = .92, NNFI = .92, SRMR = .07, and the intercept and slope growth parameters for each of the three constructs can be seen in Table 2.
Table 2.
Estimates of temporal variation in self-efficacy, anxiety sensitivity, and panic disorder symptom severity from parallel process latent growth curve models.
| Parameter estimate | Self-efficacy | Anxiety sensitivity | Panic disorder symptoms |
|---|---|---|---|
| Growth intercept | |||
| Mean (SE) | 69.65 (1.27) | 2.14 (.042) | 11.19 (.30) |
| Variance (SE) | 493.27 (39.69) | .530 (.043) | 25.80 (2.20) |
| Growth slope | |||
| Mean (SE) | 16.75 (1.07) | −.972 (.050) | −5.54 (.33) |
| Variance (SE) | 258.34(27.86) | .606 (.059) | 20.773(2.47) |
| Intercept–slope covariance (SE) | −214.52 (27.74) | −.227 (.039) | −13.37 (1.95) |
| Intercept–slope correlation | −.601 | −.281 | −.577 |
Note: all parameters significant at p < .001; SE = Standard error.
As expected, the results of the intercept and slope parameters for each construct demonstrated that there was significant change in panic symptoms and in the two mechanisms in the hypothesized directions. The relationships between changes in self-efficacy, anxiety sensitivity, and PD symptom severity were examined next using the correlations between the slope factors for each construct from the associative parallel process model (Table 3). As expected, results indicated a large and statistically significant latent correlation between changes in self-efficacy during treatment and changes in PD symptoms (r = −.518, p < .001) such that larger increases in self-efficacy beliefs during treatment were associated with larger decreases in PD symptoms during treatment. Results also indicated a large and statistically significant latent correlation between changes in anxiety sensitivity during treatment and changes in PD symptoms (r = .679, p < .001) such that larger decreases in anxiety sensitivity during treatment were associated with larger decreases in PD symptoms during treatment.
Table 3.
Latent correlations from parallel process unconditional latent growth curve models of self-efficacy, anxiety sensitivity, and panic symptoms.
| Self-efficacy intercept | Self-efficacy slope | Anxiety sensitivity intercept | Anxiety sensitivity slope | Panic intercept | Panic slope | |
|---|---|---|---|---|---|---|
| Self-efficacy intercept | – | |||||
| Self-efficacy slope | −.601* | – | ||||
| Anxiety sensitivity intercept | −.301* | .283* | – | |||
| Anxiety sensitivity slope | .044 | −.406* | −.400* | – | ||
| Panic intercept | −.450* | .339* | .605* | −.281* | – | |
| Panic slope | −.198* | −.518* | −.401* | .679* | −.577* | – |
Note:
p < .001.
Effects of mechanisms of changes on panic disorder symptoms in LGC models
Our final LGC analyses focused on determining the unique effects that changes in self-efficacy and anxiety sensitivity had on changes in PD symptoms. An additional parallel process latent growth curve model was specified in which the slope factor for PD symptoms was regressed onto the slope factors of self-efficacy and anxiety sensitivity. The associations between the three intercept factors were freely estimated in this model, as was the association between the slope factors of self-efficacy and anxiety sensitivity.
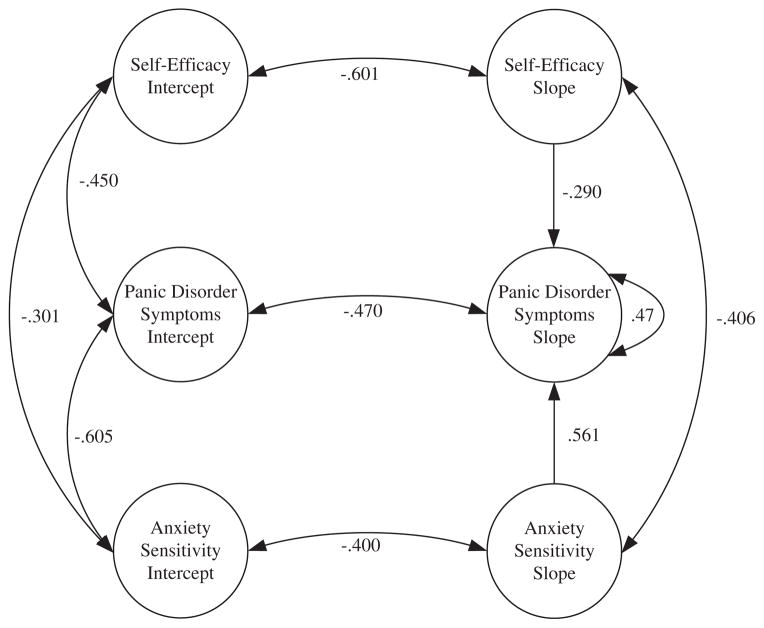
The completely standardized results of this model can be seen in Fig. 1. The fit for this model was identical to the associative parallel process with freely estimated slope factors. The results of this model indicated that there were unique effects for changes in both self-efficacy beliefs (B = −.082, SE = .017, Z = 4.81, p < .001) and changes in anxiety sensitivity (B = 3.285, SE = .357, Z = 9.20, p < .001) on changes in PD symptoms. A comparison of the completely standardized effects reveals that the magnitude of the unique effect of anxiety sensitivity (β = .561, 95% CI .458 : .665) was larger than the effect of self-efficacy beliefs (β =−.290, 95% CI −.175 : −.404). Together, changes in self-efficacy and anxiety sensitivity accounted for a very large proportion (R2 = .53) of variance in change in PD symptoms. These results support our hypothesis that change in self-efficacy beliefs and anxiety sensitivity over the course of CBT treatment are important predictors of change in panic symptoms, but provide limited information about the temporal precedence of change in the two mechanisms.
Fig. 1.
Completely standardized results of parallel process latent growth curve model of self-efficacy, anxiety sensitivity, and panic symptoms in which panic symptoms slope is regressed on self-efficacy and anxiety sensitivity slopes. Note: covariances between intercepts and slopes across constructs (e.g., anxiety sensitivity intercept slope with self-efficacy slope) were estimated but are not presented in order to simply the presentation of the results. Model fit: χ2 (501) = 1657.20, p < .001; RMSEA = .08, 90% CI: .076, .084, CFI = .92, NNFI = .92, SRMR = .07.
Modeling temporal dependencies of change
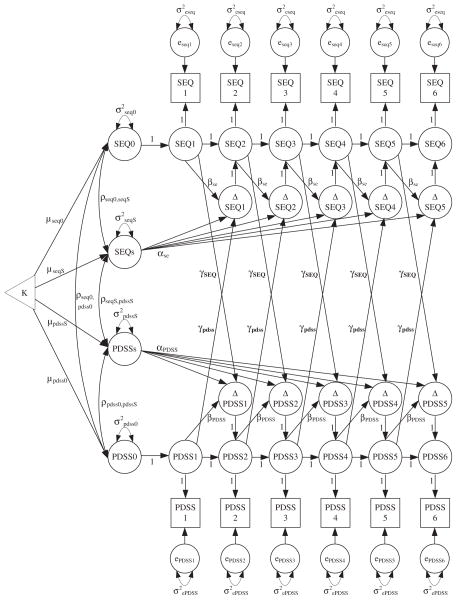
Latent difference score models were used next to better understand the temporal dependencies between changes in self-efficacy, anxiety sensitivity, and panic symptoms. Univariate LDS models indicated that a full dual change score model with varying proportional change parameters provided the best fit for modeling the longitudinal course of self-efficacy, anxiety sensitivity, and PD symptoms.2 After identifying the most appropriate univariate LDS model for each outcome, bivariate LDS models were specified to examine the reciprocal effects of 1) changes in self-efficacy and changes in panic symptoms, and 2) changes in anxiety sensitivity and changes in panic symptoms. Fig. 2 presents an example of how the bivariate LDS models were specified and the results of the bivariate LDS models can be seen in Table 4. The coupling parameters (γ) are the most important parameters in the bivariate LDS models as they represent the influence of one variable on subsequent change in another variable after controlling for autoregressive effects and nonstationarity.
Fig. 2.
Example of bivariate latent difference score model to examine the effects of change in self-efficacy beliefs (SEQ) on subsequent change in panic symptoms (PDSS).
Table 4.
Results of bivariate latent difference score models examining the reciprocal effects of self-efficacy and panic symptoms, and anxiety sensitivity and panic symptoms.
| Parameter estimate | Self-efficacy and panic
|
Anxiety sensitivity and panic
|
||
|---|---|---|---|---|
| SEQ | PDSS | ASI | PDSS | |
| Initial status | ||||
| Mean (SE) | 68.48 (1.24)*** | 11.21 (.302)*** | 2.171 (.039)*** | 11.27 (.287)*** |
| Variance (SE) | 430.46 (38.18)*** | 25.05 (2.48)*** | .487 (.04)*** | 22.26 (2.02)*** |
| Constant change (α) | ||||
| Mean (SE) | −38.59 (15.27)* | 7.49 (3.13)* | −.006 (.048) | .951 (.235)*** |
| Variance (SE) | 63.90 (43.87) | 2.55 (1.57) | .154 (.036)*** | 1.772 (.476)*** |
| Proportional change (β) | ||||
| β1 (SE) | .366 (.119)** | −.375 (.111)** | −.589 (.071)*** | .297 (.092)** |
| β2 (SE) | .325 (.115)** | −.396 (.119)** | −.597 (.068)*** | .319 (.093)** |
| β3 (SE) | .323 (.119)** | −.367 (.125)** | −.534 (.063)*** | .297 (.091)** |
| β4 (SE) | .313 (.122)* | −.441 (.122)*** | −.566 (.063)*** | .266 (.090)** |
| β5 (SE) | .321 (.124)* | −.401 (.128)** | −.507 (.059)*** | .173 (.089) |
| β6 (SE) | .331 (.124)* | −.389 (.126)** | −.558 (.063)*** | .337 (.098)** |
| β7 (SE) | .315 (.124)* | −.412 (.131)** | −.524 (.055)*** | .221 (.090)* |
| β8 (SE) | .356 (.127)* | −.468 (.128)*** | −.563 (.058)*** | .090 (.086) |
| β9 (SE) | .314 (.124)* | −.498 (.137)*** | −.585 (.066)*** | .149 (.105) |
| β10 (SE) | .322 (.125)* | −.499 (.137)*** | −.637 (.073)*** | .246 (.119)* |
| Residual error | ||||
| 125.57 (11.98)*** | 7.864 (.281)*** | .072 (.011)*** | 7.883 (.227)*** | |
| 61.33 (6.57)*** | 7.864 (.281)*** | .068 (.007)*** | 7.883 (.227)*** | |
| 82.06 (7.33)*** | 7.864 (.281)*** | .071 (.006)*** | 7.883 (.227)*** | |
| 65.51 (5.92)*** | 7.864 (.281)*** | .066 (.006)*** | 7.883 (.227)*** | |
| 55.64 (5.66)*** | 7.864 (.281)*** | .067 (.006)*** | 7.883 (.227)*** | |
| 28.37 (3.59)*** | 7.864 (.281)*** | .060 (.006)*** | 7.883 (.227)*** | |
| 39.89 (4.16)*** | 7.864 (.281)*** | .043 (.004)*** | 7.883 (.227)*** | |
| 31.79 (3.29)*** | 7.864 (.281)*** | .038 (.004)*** | 7.883 (.227)*** | |
| 22.91 (2.38)*** | 7.864 (.281)*** | .048 (.004)*** | 7.883 (.227)*** | |
| 13.64 (1.85)*** | 7.864 (.281)*** | .048 (.005)*** | 7.883 (.227)*** | |
| 14.33 (3.08)*** | 7.864 (.281)*** | .055 (.006)*** | 7.883 (.227)*** | |
| Bivariate coupling (γ) | SEQt − 1 → ΔPDSSt | PDSSt − 1 → ΔSEQt | ASIt − 1 → ΔPDSSt | PDSSt − 1 → ΔASIt |
| γ1 (SE) | −.060 (.028)* | 1.282 (.668) | −2.434 (.460)*** | .099 (.015)*** |
| γ2 (SE) | −.060 (.028)* | 1.725 (.729)* | −2.516 (.451)*** | .101 (.015)*** |
| γ3 (SE) | −.060 (.028)* | 1.874 (.741)* | −2.186 (.447)*** | .095 (.014)*** |
| γ4 (SE) | −.060 (.028)* | 1.919 (.711)** | −2.534 (.448)*** | .095 (.014)*** |
| γ5 (SE) | −.060 (.028)* | 2.001 (.747)** | −1.641 (.419)*** | .088 (.014)*** |
| γ6 (SE) | −.060 (.028)* | 1.650 (.735)* | −2.619 (.472)*** | .102 (.015)*** |
| γ7 (SE) | −.060 (.028)* | 2.236 (.764)** | −1.982 (.420)*** | .088 (.013)*** |
| γ8 (SE) | −.060 (.028)* | 1.644 (.715)* | −1.647 (.413)*** | .098 (.014)*** |
| γ9 (SE) | −.060 (.028)* | 2.401 (.808)** | −1.949 (.476)*** | .101 (.016)*** |
| γ10 (SE) | −.060 (.028)* | 2.195 (.826)** | −2.576 (.521)*** | .113 (.018)*** |
| Correlations | ||||
| ρ0s | −.511*** | .515*** | .150* | −.366*** |
| ρx0 y0 | −.438*** | .653*** | ||
| ρxs ys | −.976*** | .947*** | ||
| Model fit | ||||
| χ2 (df) | 618.48 (217)*** | 534.73 (208)*** | ||
| RMSEA | .078 | .066 | ||
| CFI | .945 | .963 | ||
| TLI | .942 | .959 | ||
Note:
p < .05
p < .01
p < .001;
SEQ = self-efficacy, ASI = anxiety sensitivity; PDSS = panic disorder symptoms. SE = standard error, CFI = comparative fit index; TLI = Tucker–Lewis index.
In the self-efficacy and panic symptoms bivariate LDS model, the results indicated that higher self-efficacy beliefs predict greater subsequent decreases in panic symptoms, while higher panic symptoms predict greater subsequent increases in self-efficacy beliefs. The effect of self-efficacy beliefs on subsequent change in panic symptoms was consistent across treatment, while the effect of panic on subsequent change in self-efficacy varied. In the anxiety sensitivity and panic symptoms bivariate LDS model, all coupling parameters were statistically significant and the results indicated that higher levels of anxiety sensitivity predict greater subsequent decreases or smaller increases in panic symptoms, while higher panic symptoms predict greater subsequent increases or smaller decreases in anxiety sensitivity.
Our final analyses combined the two bivariate LDS models into a multivariate LDS model in which change in panic symptoms was modeled as a function of constant change, proportional self-feedback, previous self-efficacy and previous anxiety sensitivity, as specified in equation (3). The results of this model are presented in Table 5 and indicated that self-efficacy and anxiety sensitivity were both significant predictors of subsequent change in panic symptoms. As with the previous LDS models, the parameters from this model can be used to create estimated change equations such as:
which indicates that change in panic symptoms from session 1 to session 2 is a function of 1) a constant change process that results in the maintenance of panic symptoms, 2) panic symptoms at time 1, such that higher baseline panic symptoms are associated with an increase in or maintenance of panic symptoms, 3) anxiety sensitivity at time 1, such that higher baseline anxiety sensitivity are associated with a decrease in panic symptoms, and 4) self-efficacy beliefs such that higher baseline self-efficacy beliefs are associated with a decrease in panic symptoms. Combined with the proportional change parameters and estimated descriptive statistics indicating that self-efficacy gradually increases during treatment while anxiety sensitivity gradually decreases, these results suggest a dynamic process in which the effects of anxiety sensitivity on subsequent intraindividual changes in panic may be greatest earlier in treatment when individuals tend to have the highest level of anxiety sensitivity. Conversely, the effects of self-efficacy on subsequent intraindividual changes in panic may be greatest later in treatment when individuals tend to have the highest level of self-efficacy. Anxiety sensitivity and self-efficacy may therefore be two important mechanisms of change in CBT for PD that are most influential at different stages of treatment.
Table 5.
Results of multivariate latent difference score models examining the unique effects of change in self-efficacy and anxiety sensitivity on subsequent change in panic symptoms.
| Parameter estimate | Reciprocal causality SEQ + ASI on PDSS
|
||
|---|---|---|---|
| SEQ | PDSS | ASI | |
| Initial Status | |||
| Mean (SE) | 68.398 (1.23)*** | 11.261 (.288)*** | 2.174 (.039)*** |
| Variance (SE) | 416.52 (37.24)*** | 22.38 (2.05)*** | .463 (.039)*** |
| Constant Change (α) | |||
| Mean (SE) | −25.685 (4.11)*** | 4.625 (.823)*** | −.045 (.052) |
| Variance (SE) | 30.93 (7.94)*** | 1.765 (.355)*** | .176 (.042)*** |
| Proportional Change (β) | |||
| β1 (SE) | .282 (.044)*** | .194 (.097)* | −.628 (.076)*** |
| β2 (SE) | .245 (.045)*** | .174 (.096) | −.614 (.071)*** |
| β3 (SE) | .251 (.040)*** | .146 (.096) | −.552 (.067)*** |
| β4 (SE) | .232 (.039)*** | .134 (.096) | −.584 (.067)*** |
| β5 (SE) | .244 (.039)*** | .044 (.093) | −.529 (.063)*** |
| β6 (SE) | .240 (.038)*** | .192 (.100) | −.579 (.067)*** |
| β7 (SE) | .226 (.038)*** | .095 (.096) | −.552 (.061)*** |
| β8 (SE) | .257 (.039)*** | −.048 (.088) | −.586 (.063)*** |
| β9 (SE) | .209 (.037)*** | .049 (.110) | −.633 (.073)*** |
| β10 (SE) | .216 (.037)*** | .142 (.126) | −.675 (.079)*** |
| Residual error | |||
| 131.64 (11.26)*** | 7.999 (.224)*** | .083 (.010)*** | |
| 66.19 (6.314)*** | 7.999 (.224)*** | .065 (.006)*** | |
| 83.58 (7.360)*** | 7.999 (.224)*** | .068 (.006)*** | |
| 60.97 (5.476)*** | 7.999 (.224)*** | .061 (.005)*** | |
| 58.91 (5.535)*** | 7.999 (.224)*** | .069 (.006)*** | |
| 29.28 (2.900)*** | 7.999 (.224)*** | .059 (.005)*** | |
| 38.94 (3.443)*** | 7.999 (.224)*** | .040 (.004)*** | |
| 36.81 (3.330)*** | 7.999 (.224)*** | .042 (.004)*** | |
| 23.46 (2.265)*** | 7.999 (.224)*** | .052 (.005)*** | |
| 14.34 (1.755)*** | 7.999 (.224)*** | .053 (.005)*** | |
| 18.35 (2.556)*** | 7.999 (.224)*** | 059 (.006)*** | |
| Bivariate coupling | SEQt − 1 → ΔPDSSt | PDSSt − 1 → ΔSEQt | ASIt − 1 → ΔPDSSt | PDSSt − 1 → ΔASIt |
|---|---|---|---|---|
| γ1 (SE) | −.037 (.007)*** | .655 (.206)*** | −2.425 (.446)*** | .110 (.016)*** |
| γ2 (SE) | −.037 (.007)*** | 1.020 (.208)*** | −2.324 (.422)*** | .109 (.016)*** |
| γ3 (SE) | −.037 (.007)*** | 1.058 (.222)*** | −1.967 (.417)*** | .102 (.015)*** |
| γ4 (SE) | −.037 (.007)*** | 1.174 (.211)*** | −2.383 (.418)*** | .103 (.0150*** |
| γ5 (SE) | −.037 (.007)*** | 1.151 (.216)*** | −1.527 (.390)*** | .097 (.015)*** |
| γ6 (SE) | −.037 (.007)*** | .914 (.211)*** | −2.362 (.436)*** | .111 (.016)*** |
| γ7 (SE) | −.037 (.007)*** | 1.456 (.221)*** | −1.871 (.403)*** | .098 (.015)*** |
| γ8 (SE) | −.037 (.007)*** | .956 (.213)*** | −1.436 (.374)*** | .107 (.015)*** |
| γ9 (SE) | −.037 (.007)*** | 1.707 (.230)*** | −1.939 (.453)*** | .117 (.018)*** |
| γ10 (SE) | −.037 (.007)*** | 1.476 (.238)*** | −2.455 (.513)*** | .128 (.020)*** |
| Correlations | ||||
| ρx0 y0 | −.410*** | .666*** | ||
| ρxs ys | −.365* | .779*** | ||
Note: Model Fit: χ2 (n = 367; df = 479) = 1217.91 ***, RMSEA = .065, CFI = .950; TLI = .945;
p < .05
p < .01
p < .001;
SEQ = self-efficacy, ASI = anxiety sensitivity; PDSS-SR = panic disorder symptoms; SE = standard error, CFI = comparative fit index; TLI = Tucker–Lewis index; RMSEA = root-mean-square error of approximation.
Discussion
It is clear that CBT for PD is an effective treatment, but also that there is room for improvement, so the focus of treatment outcome research for PD has increasingly shifted towards an examination of the mechanisms of change of CBT in order to improve our understanding of why CBT is effective, with the possible outcome of further increases in efficacy. Previous research has provided promising evidence regarding mechanisms of change of CBT in comparison to medication (e.g., Hofmann et al., 2007), pill placebo (e.g., Shear et al., 2001), and waitlist comparison conditions (e.g., Casey et al., 2005), but the majority of previous research has relied on pre and post-treatment assessments of the hypothesized mechanisms. The goal of the present study was to improve our understanding of how CBT promotes recovery from PD by examining the temporal dependencies of change in PD symptoms, anxiety sensitivity, and self-efficacy beliefs.
The results of the present study demonstrate that self-efficacy and anxiety sensitivity both change throughout the course of CBT treatment, and that changes in these constructs occur at different times during treatment. The greatest changes in anxiety sensitivity occurred early in treatment while the greatest changes in self-efficacy occurred later. Consistent with our hypotheses, results of the parallel process latent growth curve models indicated that change in each construct uniquely predicted change in panic symptoms across the course of treatment and results of the bivariate and multivariate LDS models indicated that each construct predicted subsequent changes in panic symptoms.
Together, these findings suggest that CBT has the greatest impact on anxiety sensitivity, and anxiety sensitivity has a greater impact on subsequent panic symptom changes early in treatment when the focus of treatment is on psychoeducation, breathing retraining, and cognitive restructuring. These results are noteworthy in that the largest changes in anxiety sensitivity occurred prior to the start of interoceptive exposure exercises. Although anxiety sensitivity continued to decrease on average during the later stages of treatment that focused on interoceptive and situational exposure exercises, it appears that CBT for PD results in rapid improvements in patients’ fear of bodily sensations. This finding suggests that somatic sensations that provoke anxiety are largely based on misconceptions that are corrected early in treatment, although later interoceptive exposure may also be necessary in order to confirm new, less catastrophic attitudes and to facilitate reductions in interoceptive avoidance.
In contrast, our findings suggest that CBT has the greatest impact on self-efficacy, and self-efficacy has a greater impact on subsequent panic symptom changes, later in treatment when the focus of treatment is on interoceptive and in vivo exposure exercises. These findings are consistent with self-efficacy theory in that, although verbal persuasion is considered one important method for increasing self-efficacy, mastery experiences are thought to always provide the most effective method of increasing self-efficacy (Bandura, 1997). Clinicians providing CBT should therefore be aware that correcting patients’ maladaptive perceptions of bodily sensations may be one of the most important factors for promoting recovery early in treatment, while the promotion of patients’ mastery and personal agency regarding their ability to cope with panic related physical sensations and agoraphobic situations may be one of the most important factors for promoting recovery later in treatment, and that both would seem important for improvement.
Our results are consistent with previous research that suggesting that self-efficacy and anxiety sensitivity may be mechanisms of change of CBT for PD (Bouchard et al., 2007; Casey et al., 2005; Reilly et al., 2005; Shear et al., 2001; Smits et al., 2004). By simultaneously examining the effects of self-efficacy and anxiety sensitivity, the present study builds upon this previous research in demonstrating that both self-efficacy and anxiety sensitivity uniquely predict PD severity (Casey, Oei, & Newcombe, 2004) and that intraindividual changes in self-efficacy and anxiety sensitivity uniquely predict improvement in PD during CBT. The results of the present study also provide additional evidence of the benefits of a dual focus on both positive (i.e., self-efficacy) and negative (i.e., anxiety sensitivity) cognitions in relation to PD (Casey, Oei, & Newcombe, 2004; Casey, Oei, Newcombe, & Kenardy, 2004), as these constructs appear to uniquely predict the longitudinal course of PD symptoms during treatment. The strengths of the present study include the use of assessments at each treatment session and the use of a large sample. These methodological characteristics permit a more fine-grained analysis of exactly when changes in the mechanisms and symptoms occurred, which strengthens conclusions about whether changes in the hypothesized mechanisms determine subsequent changes in symptoms.
Limitations and future directions
The primary limitation of the present study was the absence of a comparison condition. Our findings are consistent with previous research in demonstrating that individuals completing CBT for PD report large changes in anxiety sensitivity and self-efficacy during treatment (Casey et al., 2005; Smits et al., 2004), but the absence of a comparison treatment group prevents definitive conclusions regarding whether these changes are truly specific mechanisms of CBT. Nevertheless, the temporal sequence of changes in the examined mechanisms is theoretically consistent with both cognitive-behavioral models of PD and current theories for how CBT may influence anxiety sensitivity and self-efficacy. Another important limitation is that the sample used was relatively ethnically homogenous, so it will be important for future research to replicate the current findings in more diverse samples as well as to examine whether any other patient characteristics potentially moderate the degree to which self-efficacy and anxiety sensitivity function as mechanisms of change in the treatment of panic.
The measures used to assess the examined mechanisms of change are also limitations of the present study. Although the original ASI continues to be widely used to measure anxiety sensitivity, more recent measures of anxiety sensitivity have been developed such as the Anxiety Sensitivity Index-3 (Taylor et al., 2007) that have superior psychometric properties than the original ASI and are better suited to modeling the subfactors of anxiety sensitivity. Replicating our findings using the ASI-3 would allow for a more fine grained analysis of how the different facets of anxiety sensitivity may uniquely promote recovery during CBT for PD. Our analyses also exclusively focused on modeling anxiety sensitivity as a continuous latent construct. The use of latent transition analysis may therefore be an important future direction for examining the role of anxiety sensitivity as a mechanism of change as, although findings have been inconsistent, there is some evidence that anxiety sensitivity is most appropriately modeled using a categorical-dimensional latent structure (Bernstein et al., 2007, 2013).
The method of assessing of self-efficacy beliefs in the present study is also a limitation. The measure used to assess self-efficacy was developed specifically for the present study, and although the self-efficacy measure was constructed in a manner consistent with Bandura’s (2006) guide for constructing self-efficacy scales, our findings are still based on the use of a self-efficacy measure that has not previously been validated. This is a relatively common limitation in self-efficacy research as the crucial importance of evaluating self-efficacy beliefs in relation to a specific domain often necessitates the creation of novel measures of self-efficacy. This is nevertheless an important issue as, although self-efficacy beliefs continue to be widely studied in clinical psychology, much of the research examining self-efficacy in relation to panic disorder area is dated and there have been frequent criticisms of self-efficacy theory over the past decades (e.g., Cahill, Gallo, Lisman, & Weinstein, 2006; Kirsch, 1985). Researchers continue to raise questions about the causal influences and effects of self-efficacy beliefs (Williams, 2010), which may help to explain why there has been relatively less research examining the role of self-efficacy in predicting the development of and recovery from panic disorder in recent years. Replicating our findings using measures using a measure of panic related self-efficacy with more extensive evidence of reliability and validity (i.e., Telch et al., 1989) will therefore be an important direction for future research in order to confirm the unique role that self-efficacy beliefs may play as a mechanism of change of CBT for PD.
The present study is also limited by the nomothetic focus on patterns of change. LGC and LDS modeling techniques permit the modeling of intraindividual trajectories and successive intraindividual differences, respectively, but our results focus on the nomothetic patterns of these idiographic processes. Our results therefore speak to how self-efficacy and anxiety sensitivity related to the average degree of intraindividual change rather than focusing on an examination of how these factors relate to or predict exactly when individuals recover from PD. It will be important for future research to examine the role that these distinct mechanisms of change may play in identifying or predicting different patterns of treatment response (i.e., early responders vs. late responders vs. non-responders). It may be the case that rapid early changes in anxiety sensitivity could predict early response during CBT for PD in a subset of individuals for whom maladaptive cognitions regarding somatic sensations are the principal cause of their PD symptoms, similar to how sudden gains during CBT for depression are predicted by cognitive changes in some individuals (Tang, DeRubeis, Beberman, & Pham, 2005). Future research using techniques such as latent class growth analysis or latent growth mixture modeling (Jung & Wickrama, 2008) to examine the role of changes in self-efficacy and anxiety sensitivity in predicting distinct classes of response during treatment could improve our understanding of how and why some individuals exhibit rapid vs. delayed response during treatment.
Conclusions
The identification of mechanisms of change is a crucial step for improving our understanding of how and why empirically supported treatments work. A limitation of the majority of previous research on mechanisms is the use of assessment schedules that preclude conclusions regarding the temporal precedence of change in hypothesized mechanisms. By examining session-by-session changes in self-efficacy, anxiety sensitivity, and panic symptoms, the present study addresses the issue of temporality and improves our understanding of the temporal sequences of change during the treatment of PD. The finding of the differential timing of the effects of CBT on self-efficacy and anxiety sensitivity is particularly noteworthy, as these results suggest that the principal mechanism of change of CBT may vary across different stages of treatment such that correcting maladaptive beliefs about bodily sensations plays a greater role earlier in treatment while instilling personal agency regarding the ability to cope with PD related sensations/situations plays a greater role later in treatment. Our results therefore provide strong evidence that self-efficacy and anxiety sensitivity both play important, but seemingly independent, roles as mechanisms of change of CBT for PD.
Acknowledgments
This research was supported by the National Institute of Mental Health with grants: R01 MH45963, MH45964, MH45965, and MH45966.
Footnotes
A copy of the self-efficacy scale used in the present study is available from the first author.
Complete results for the univariate latent difference score models are available from the first author.
References
- Aaronson CJ, Shear M, Goetz RR, Allen LB, Barlow DH, White KS, et al. Predictors and time course of response among panic disorder patients treated with cognitive-behavioral therapy. Journal of Clinical Psychiatry. 2008;69:418–424. doi: 10.4088/jcp.v69n0312. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy conception of anxiety. Anxiety Research. 1988;1:77–98. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan T, editors. Self-efficacy beliefs of adolescents. Vol. 5. Greenwich, CT: Information Age Publishing; 2006. pp. 307–337. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford; 1988. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: The Guilford Press; 2002. [Google Scholar]
- Barlow DH, Craske MG. Mastery of your anxiety and panic: Client workbook. 4. New York: Oxford University Press; 2007. [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. Journal of the American Medical Association. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Bentler PM. Comparative fit indices in structural equation models. Psychological Bulletin. 1990;28:97–104. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentley KH, Gallagher MW, Boswell JF, Gorman JM, Shear MK, Woods SW, et al. The interactive effects of perceived control and anxiety sensitivity: exploring panic disorder within a triple vulnerabilities framework. Journal of Psychopathology and Behavioral Assessment. 2013;35:57–64. [Google Scholar]
- Bernstein A, Stickle TR, Schmidt NB. Factor mixture model of anxiety sensitivity and anxiety psychopathology vulnerability. Journal of Affective Disorders. 2013;149:406–417. doi: 10.1016/j.jad.2012.11.024. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Marshall EC, Schmidt NB. Laboratory test of a novel structural model of anxiety sensitivity and panic vulnerability. Behavior Therapy. 2009;40:171–180. doi: 10.1016/j.beth.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Norton P, Schmidt NB, Taylor S, Forsyth J, et al. Taxometric and factor analytic models of anxiety sensitivity: integrating approaches to latent structural research. Psychological Assessment. 2007;19:74–87. doi: 10.1037/1040-3590.19.1.74. [DOI] [PubMed] [Google Scholar]
- Bouchard S, Gauthier J, Nouwen A, Ivers H, Valieres A, Simard S, et al. Temporal relationship between dysfunctional beliefs, self-efficacy and panic apprehension in the treatment of panic disorder with agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38:275–292. doi: 10.1016/j.jbtep.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Deacon BJ, Olatunji BO, Bondy CL, Abramowitz JS, Tolin DF. Categorical or dimensional: a re-analysis of the anxiety sensitivity construct. Behavior Therapy. 2010;41:154–171. doi: 10.1016/j.beth.2009.02.005. [DOI] [PubMed] [Google Scholar]
- Cahill SP, Gallo LA, Lisman SA, Weinstein A. Willing or able? The meanings of self-efficacy. Journal of Social and Clinical Psychology. 2006;25:196–209. [Google Scholar]
- Casey LM, Newcombe PA, Oei TPS. Cognitive mediation of panic severity: the role of catastrophic misinterpretation of bodily sensations and panic self-efficacy. Cognitive Therapy and Research. 2005;29:187–200. doi: 10.1016/S0887-6185(02)00257-8. [DOI] [PubMed] [Google Scholar]
- Casey LM, Oei TPS, Newcombe PA. An integrated cognitive model of panic disorder: the role of positive and negative cognitions. Clinical Psychology Review. 2004;24:529–555. doi: 10.1016/j.cpr.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Casey LM, Oei TPS, Newcombe PA, Kenardy J. The role of catastrophic misinterpretation of bodily sensations and panic self-efficacy independently predicted panic severity. Journal of Anxiety Disorders. 2004;18:325–340. doi: 10.1016/S0887-6185(02)00257-8. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediation models with longitudinal data: questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Craske MG, Barlow DH. Panic disorder and agoraphobia. In: Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 5. New York: Guilford Press; 2013. in press. [Google Scholar]
- Duncan TE, Duncan SC, Strycker LS. An introduction to latent variable growth curve modeling. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- Enders CK. Applied missing data analysis. New York, NY: Guilford Press; 2010. [Google Scholar]
- Ferrer E, McArdle JJ. Longitudinal modeling of developmental changes in psychological research. Current Directions in Psychological Science. 2010;19:149–154. [Google Scholar]
- Hawley LL, Ho MHR, Zuroff DC, Blatt SJ. The relationship of perfectionism, depression, and therapeutic alliance during treatment for depression: latent difference score analysis. Journal of Consulting and Clinical Psychology. 2006;74:930–942. doi: 10.1037/0022-006X.74.5.930. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Meuret AE, Rosenfield D, Suvak MK, Barlow DH, Woods SW. Preliminary evidence for cognitive mediation during cognitive-behavioral therapy of panic disorder. Journal of Consulting and Clinical Psychology. 2007;3:374–379. doi: 10.1037/0022-006X.75.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P. Reliability of the self-report version of the Panic Disorder Severity Scale. Depression and Anxiety. 2002;15(4):183–185. doi: 10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: User’s reference guide. Chicago: Scientific Software International; 1996. [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2:302–317. [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, McArdle JJ, Saxe GN, Doron-LaMarca S, Orazem RJ. Latent difference score approach to longitudinal trauma research. Journal of Traumatic Stress. 2006;19:771–785. doi: 10.1002/jts.20188. [DOI] [PubMed] [Google Scholar]
- Kirsch I. Self-efficacy and expectancy: old wine with new labels. Journal of Personality and Social Psychology. 1985;49:824–830. [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- McArdle JJ. A latent difference score approach to longitudinal dynamic structural analyses. In: Cudeck R, duToit S, Sorbom D, editors. Structural equation modeling: Present and future. Lincolnwood, IL: Scientific Software International; 2001. pp. 342–380. [Google Scholar]
- McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Mitte K. A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. Journal of Affective Disorders. 2005;88:27–45. doi: 10.1016/j.jad.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Molenaar PCM, Campbell CG. The new person-specific paradigm in psychology. Current Directions in Psychology. 2009;18(2):112–117. [Google Scholar]
- Muthén LK, Muthén BO. Mplus: The comprehensive modeling program for applied researchers: User’s guide. 5. Los Angeles, CA: Muthén & Muthén; 2008. [Google Scholar]
- Naragon-Gainey K. Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin. 2010;136:128–150. doi: 10.1037/a0018055. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzki-Taylor KB. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychological Bulletin. 2009;135:974–999. doi: 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Wichman AL, MacCallum RC, Briggs NE. Latent growth curve modeling. Thousand Oaks, CA: Sage Publications; 2008. [Google Scholar]
- Reilly KP, Gill MJ, Dattilio FM, Mc Cormick A. Panic and agoraphobia: do treatments targeted for one problem also improve the other? A pilot study. Archives in Psychiatry and Psychotherapy. 2005;7:11–28. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Richards JC, Richardson V, Pier C. The relative contributions of negative cognitions and self-efficacy to severity of panic attacks in panic disorder. Behaviour Change. 2002;19:102–111. [Google Scholar]
- Sbarra DA, Allen JJB. Decomposing depression: do sleep disturbances lead changes in cognitive-affective symptom recovery? Journal of Abnormal Psychology. 2009;118:171–182. doi: 10.1037/a0014375. [DOI] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Research in Human Development. 2009;6:144–164. [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, et al. Multicenter collaborative panic disorder severity scale. American Journal of Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Shear MK, Houck P, Greeno C, Masters S. Emotion-focused psychotherapy for patients with panic disorder. American Journal of Psychiatry. 2001;158:1993–1998. doi: 10.1176/appi.ajp.158.12.1993. [DOI] [PubMed] [Google Scholar]
- Smits JA, Berry AC, Tart CD, Powers MB. The efficacy of cognitive-behavioral interventions for reducing anxiety sensitivity: a meta-analytic review. Behaviour Research and Therapy. 2008;46:1047–1054. doi: 10.1016/j.brat.2008.06.010. [DOI] [PubMed] [Google Scholar]
- Smits JA, Powers MB, Cho Y, Telch MJ. Mechanism of change in cognitive–behavioral treatment of panic disorder: evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology. 2004;72:646–652. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Steiger JH, Lind JC. Statistically-based tests for the number of common factors. Paper presented at the annual Spring meeting of the psychometric society; Iowa City. May 30 1980.1980. [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, Pham T. Cognitive changes, critical sessions, and sudden gains in cognitive–behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 2005;73(1):168–172. doi: 10.1037/0022-006X.73.1.168. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176– 188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Marker CD, Clerkin EM. Catastrophic misinterpretations as a predictor of symptom change during treatment for panic disorder. Journal of Consulting and Clinical Psychology. 2010;78:964–973. doi: 10.1037/a0021067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teachman BA, Marker CD, Smith-Janik SB. Automatic associations and panic disorder: trajectories of change over the course of treatment. Journal of Consulting and Clinical Psychology. 2008;76:988–1002. doi: 10.1037/a0013113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch MJ, Brouillard M, Telch CF, Agras WS, Taylor CB. Role of cognitive appraisal in panic-related avoidance. Behaviour Research and Therapy. 1989;27:373–383. doi: 10.1016/0005-7967(89)90007-7. [DOI] [PubMed] [Google Scholar]
- Westen D, Morrison K. A multidimensional meta-analysis of treatments for depression, panic, and generalized anxiety disorder: an empirical examination of the status of empirically supported therapies. Journal of Consulting and Clinical Psychology. 2001;69:875–899. [PubMed] [Google Scholar]
- White KS, Allen LB, Barlow DH, Gorman JM, Shear M, Woods SW. Attrition in a multicenter clinical trial for panic disorder. Journal of Nervous and Mental Disease. 2010;198:665–671. doi: 10.1097/NMD.0b013e3181ef3627. [DOI] [PubMed] [Google Scholar]
- Williams DM. Outcome expectancy and self-efficacy: theoretical implications of an unresolved contradiction. Personality and Social Psychology Review. 2010;14:417–425. doi: 10.1177/1088868310368802. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH, Brown TA. Hierarchical structure and general factor saturation of the Anxiety Sensitivity Index: evidence and implications. Psychological Assessment. 1997;9:277–284. [Google Scholar]