Abstract
OBJECTIVES
Lung metastases are non-anatomically resected while sparing as much parenchyma as possible. For this purpose, a few surgeons use the Nd:YAG Laser LIMAX® 120, whereas the majority of surgeons use a monopolar cutter like the MAXIUM®. The aim of this experimental study was to investigate which instrument causes less lung-tissue damage at the same power output.
METHODS
These experiments were conducted on left lungs (n = 6) taken from freshly slaughtered pigs. The laser and the monopolar cutter were fixed in a hydraulic mover. The laser was focused at a distance of 3 cm to the lung tissue and the monopolar cutter was fixed in pressure-free contact with the lung surface. Both instruments were manoeuvred at a speed of 5, 10 and 20 mm/s in a straight line at an output of 100 watts over the lung surface. The lung lesions that ensued were then examined macro- and microscopically. The same procedures were repeated at a distance of 1 cm creating parallel lesions in order to analyse the lung tissue in between the lesions for thermal damage. In addition, two implanted capsules in the lung tissue simulating a lung nodule were resected with either the laser or the monopolar cutter. The resection surfaces were then examined by magnetic resonance imaging and histology for tissue damage. Finally, we created a 2-cm wide mark on the lung surface to test the resection capacity of both instruments within 1 min.
RESULTS
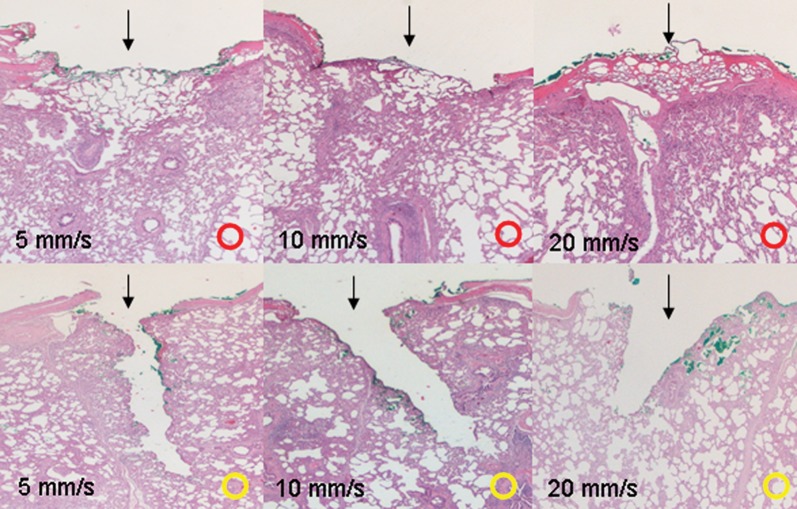
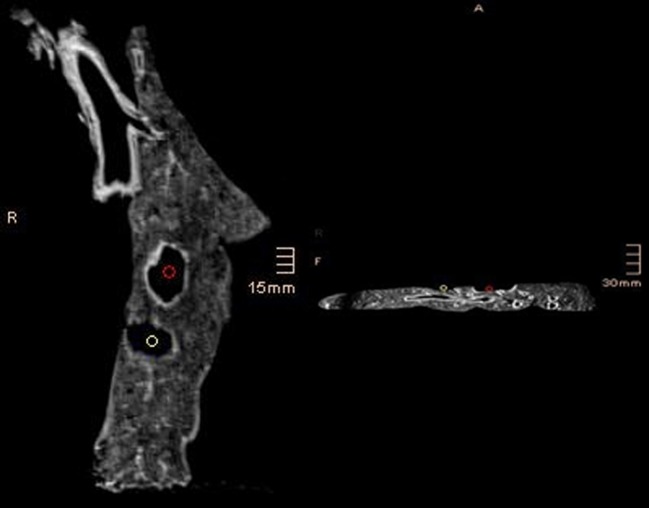
The laser created sharply delineated lesions with a vaporization and coagulation zone without thermal damage of the surrounding lung tissue. With lowering the working speed, each zone was extended. At a working speed of 10 mm/s, the mean vaporization depth using the laser was 1.74 ± 0.1 mm and the mean coagulation depth was 1.55 ± 0.09 mm. At the same working speed, the monopolar cutter demonstrated a greater cutting effect (mean vaporization depth 2.7 ± 0.11 mm; P < 0.001) without leaving much coagulation on the resection surface (mean coagulation depth 1.25 ± 0.1 mm; P = 0.002). In contrast to the laser, the monopolar cutter caused thermal damage of the adjacent lung tissue. The adjacent tissue injury was detected in histological examination as well as in the MRI findings. Adjacent lung tissue after lung metastasectomy using the monopolar cutter was hyper-intensive in T2-weighted MR imaging, indicating a severe tissue damage. No significant changes in signal intensity were observed in T2-weighted imaging of the adjacent lung tissue after using the laser for lung resection. One minute of laser applied at a 100-watt output penetrated a lung surface area of 3.8 ± 0.4 cm2 compared with 4.8 ± 0.6 cm2 of surface after application of the monopolar cutter (P = 0.001).
CONCLUSIONS
The monopolar cutter possesses indeed a greater cutting capacity than the laser, but it also causes more adjacent tissue injury. Thus, laser resection might be preferred for lung metastasectomy.
Keywords: Electrosurgical scalpel, Laser, Lung metastases, Lung resection, Tissue damage
BACKGROUND
Lung metastases are resected non-anatomically whenever possible [1, 2]. If located in the lung's periphery, they can be clamped off and resected. The opened parenchyma is then closed with a running suture for airtightness. Alternatively, a stapler can be used [3]. The drawback of the stapler technique is that much more healthy lung tissue is sacrificed, especially when the metastases lie farther towards the lung's centre. Both the laser and the monopolar cutter enable removal of lung metastases by sparing as much healthy lung parenchyma as possible [4–8]. At a safety distance of 5 mm from the metastases' borders, tumours can be successfully curatively (R0-) resected, even when they lie farther towards the centre of the lung parenchyma. With the laser, the collimated monochromatic laser ray strikes the lung tissue directly. Its cutting effect is created by intense local light energy. At temperatures >900°C, the lung tissue is effectively vaporized. Homogeneously coagulated resection surfaces, which tend not to bleed, are thus created on the borders of such zones. These coagulated surfaces are about 3 mm thick. The monopolar cutter also brings energy into contact with the lung tissue via an electroscalpel. Its high energy also suffices to penetrate and dissolve the lung parenchyma via a cutting effect. Nevertheless, the resection surface is likewise coagulated in a somewhat haphazard manner. The monopolar cutter is easy to handle, no preparatory measures are necessary and it is standard equipment in most operating theatres. The laser is also easy to handle, but its acquisition is costly and its use demands to follow distinct safety measures as well a special smoke suction devise during laser application. In addition, technicians must be specially trained to operate it. The aim of our study was to evaluate which of the two devices causes the lowest damage to healthy lung tissue after a non-anatomical resection, in order to prefer this device for the resection of lung metastases.
MATERIALS AND METHODS
Intact healthy left lungs from freshly slaughtered pigs weighing 90 kg were removed in the slaughterhouse. A total of 6 lungs were visually inspected for any pathological anomalies. Once in the laboratory, we investigated the following issues:
The local effects of the laser and the monopolar cutter on the lung tissue at various working speeds (5, 10, 20 mm/s);
Any thermal damage to the adjacent lung tissue after lung metastasectomy, based on histopathology;
Lung tissue changes in the vicinity of non-anatomical resection determined by magnetic resonance images (MRI) and
The extent of tissue cutting within a minute of laser or monopolar cutter application.
All experiments were done with the Nd:YAG Laser LIMAX® 120 (KLS Martin GmbH & Co KG, Tuttlingen, Germany) with a wavelength of 1318 nm and a power output of 100 watts.
We routinely use this laser in our clinic for the resection of lung metastases.
Local effects of the laser and the monpolar cutter on lung tissue
The laser's and the monopolar cutter's hand heald were fixed in the mount of an automatic hydraulic mover. Consequently, the instruments were moved at a constant speed and in a straight line over the lung tissue. We set a distance of 3 cm between the laser's hand heald and the lung tissue so that the laser ray was in exact focus at all times (Fig. 1A). The handle on the monopolar cutter was affixed so that its end came into contact with the lung tissue surface without exerting any pressure on it. Both devices were operated at an output power of 100 watts. The experiments were conducted at three working speeds: 5, 10 and 20 mm/s. After creating each lesion on the lung surface, we examined the tissue macroscopically and histologically after haematoxylin and eosin (HE) staining. We measured the depth of the vaporization and coagulation zone using the program Image J 1.46r.
Figure 1:
(A) Superficial lung lesion caused by the laser moving focussed over the lung surface. (B) Two lesions caused by the laser in a distance of 1 cm.
We compared both groups (laser vs monopolar cutter) by the unpaired t-test for independent samples (using Graph Prism 5, La Jolla, CA, USA). A P -value of <0.05 was considered statistically significant.
Thermal tissue damage caused by laser or monopolar cutter in adjacent tissue
To examine thermal tissue damage caused by laser and monopolar cutter in adjacent lung tissue, we created two lesions 1 cm apart from each other (Fig. 1B). The lesions were resected by one of the devices. The adjacent lung tissue was also histologically assessed for thermal damage, macroscopically and microscopically, by doing a HE staining. Thermal damage of the lung parenchyma was considered whenever the cells were obviously oedematous, swollen and when lung tissue appeared coagulated. To better evaluate the degree of the thermal damage, we created our own score based on the histological examinations:
0 = no thermal damage, 1 = light thermal damage (5–25% of the cells showed signs of damage), 2 = middle thermal damage (40–60% of the cells showed signs of thermal damage) and 3 = severe thermal damage (>70% of the cells showed signs of thermal damage).
MRI examination of lung tissue after laser or monopolar cutter resection
To facilitate the MRI assessment, two open Adalate capsules were implanted in the lung parenchyma ∼1 cm beneath the lung surface via a small incision in order to simulate a lung nodule. The lung opening was then closed with a suture. The capsules were readily visible in the T1- and T2-weighted MR images, revealing a sharply delineated 10 × 8 mm hyper-intense lesion. A non-anatomical resection of the lesions was performed with either the laser or the monopolar cutter at 100 watts. After this resection, the close resection areas were compared regarding morphological characteristics by MRI. To address the fourth point, a 2-cm wide mark was done on the lung surface. The lung tissue was then penetrated vertically at 100 watts with either the laser or the monopolar cutter.
Evaluation of the resection capacity
Afterward, we measured how much tissue had been cut within a minute, and compared the mean values of each surface measured in both groups by the unpaired t-test for independent samples. A P-value of <0.05 was considered statistically significant. The size of the resection surface per minute was calculated as the degree for the instrument's resection capacity.
Results
Macroscopic and microscopic assessment of tissue lesions
Macroscopic inspection of all laser lesions showed vaporized cut surfaces whose bases were coagulated. The lesions damage inversely correlated with the working speed. The cut surfaces were sharply delineated and revealed no signs of damage to the surrounding lung parenchyma.
The lesions caused by the monopolar cutter were considerably broader and deeper, while the coagulated base of those lesions was smaller than those made by the laser. The colour of the lung tissue surrounding the lesions appeared changed by the monopolar cutter's effect. The extent of the tissue vaporized by the laser appeared microscopically to inversely correlate with the working speed and with the coagulated zone. It was the largest at the lowest (5 mm/s) speed (mean: 2.45 ± 0.18 mm) and the smallest at the highest (20 mm/s) speed (mean of the vaporized tissue: 1.63 ± 0.08 mm and mean of the coagulated zone: 1.88 ± 0.17 mm). We observed a wider, deeper tissue defect in the lesions made by the monopolar cutter that was larger the lower (mean 5 mm/s) the hydraulic feeder's working speed had been (mean: 3.45 ± 0.18 mm). The actual coagulated zones beneath all the lesions were relatively small (mean: 1.39 ± 0.08 mm). The extension of the vaporization zone caused by the monopolar cutter was in all different speeds significantly greater than the defect caused by the laser. The extension of the coagulation zone caused by the monopolar cutter was in all speeds significantly smaller in comparison with the laser (Fig. 2, Table 1).
Figure 2:
Lung lesions (→) caused by the laser (red button) and the monopolar cutter (yellow button) [power output 100 watts] at working speeds of 5, 10 and 20 mm/s. ×12.5, HE staining.
Table 1:
Measurement of the depth vaporization and coagulation zone
| Mover speed | Laser 5 mm/s | Monopolar cutter 5 mm/s | P | Laser 10 mm/s | Monopolar cutter 10 mm/s | P | Laser 20 mm/s | Monopolar cutter 20 mm/s | P |
|---|---|---|---|---|---|---|---|---|---|
| Mean vaporization depth (mm) SD ± | 2.45 ± 0.18 | 3.45 ± 0.18 | <0.001 | 1.74 ± 0.1 | 2.7 ± 0.11 | <0.001 | 1.63 ± 0.08 | 2.26 ± 0.1 | <0.001 |
| Mean coagulation depth (mm) SD ± | 1.88 ± 0.17 | 1.39 ± 0.08 | <0.001 | 1.55 ± 0.09 | 1.25 ± 0.1 | 0.002 | 1.53 ± 0.06 | 1.34 ± 0.07 | 0.003 |
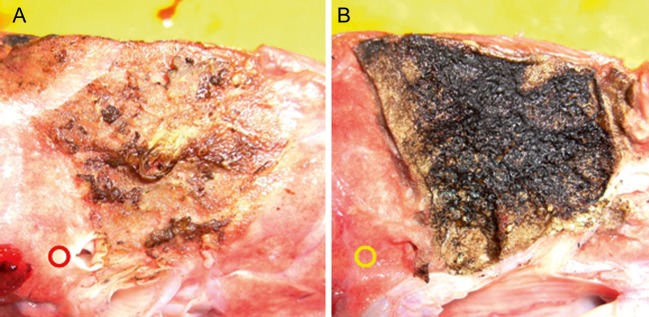
Assessment of the lung tissue between two lesions (1 cm distance)
As the two lesions caused by laser were so sharply delineated, the macroscopic appearance of the adjacent lung tissue remained unchanged. This was confirmed histopathologically (Fig. 3). In contrast, after monopolar cutter resection, the lung parenchyma between the lesions was oedematously swollen and whitish in colour. It appeared shrunken and much denser under the microscope, the cells were swollen and thus, demonstrating signs of severe thermal damage, equivalent to tissue damage score 3 (Fig. 3).
Figure 3:
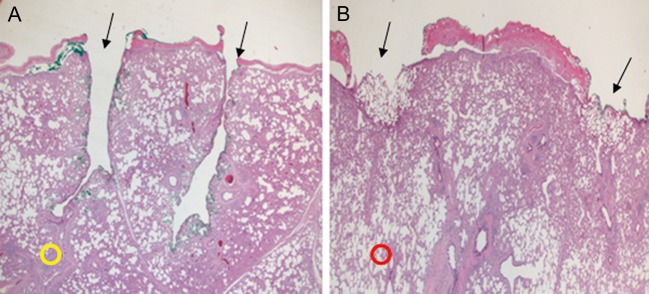
Histological examination of the lung tissue between two lesions (→); laser (red button) vs monopolar cutter (yellow button) [power output 100 watts working speed 10 mm/s] 12, ×5, HE staining.
MRI examination of non-anatomical lung resections
The capsules implanted in the lung tissue were readily identifiable on MR images (at both T1 and T2-weighting) as hyper-intense round masses. After their complete laser resection, the resection area revealed a 2–3-mm-wide, hyper-intense, sharply delineated border. The surrounding lung tissue displayed no signal changes compared with the rest of the lung tissue.
On the other hand, the monopolar cutter created an irregular border of various depths. The local tissue revealed areas that were sometimes more, other times less, hyper-intense at T2-weighting (see Fig. 4) indicating a severe tissue damage.
Figure 4:
Magnetic resonance tomography [T2 weighted, TE: 1.21, TR: 5.33, SL: 1, FA: 8] examination of the lung tissue after laser (red button) and monopolar cutter (white button) resection. After laser resection, the resection area revealed a 2–3 mm wide, hyper-intense, sharply delineated border (red button). No signal change was noticed in the adjacent lung tissue. The monopolar cutter created an irregular border of various depths (white button). The local tissue revealed areas that were sometimes more, other times less, hyper-intense at T2-weighting indicating a severe tissue damage.
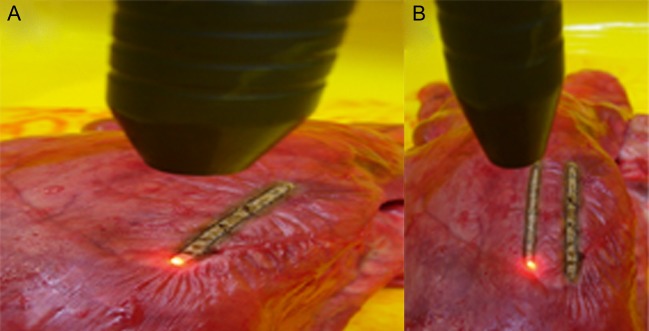
Resection capacity
Lung tissue is cut effectively by both laser and the monopolar cutter. A minute of laser applied at a 100-watt output penetrated a surface area measuring 3.8 ± 0.4 cm2. The resection surface was firm and evenly coagulated (Fig. 5). A minute of the monopolar cutter applied at the same output cuts a 4.8 ± 0.6 cm2 surface, which is highly significant (P = 0.001) compared with the surface resected by the laser. The resection surface performed by the monopolar cutter appeared considerably more irregular revealing a discontinuous and more superficially coagulated ‘turf’ (Fig. 5).
Figure 5:
Evaluation of the resection capacity (A): view of the 1-mm resected area (→); diffuse irregular coagulated areas caused by monopolar cutter (red button) and (B) homogneous coagulated area by laser application (yellow button) [power output: 100 watts].
DISCUSSION
For the resection of lung metastases, two devices were used in clinical practice: the diode-pumped Nd:YAG Laser LIMAX® 120 (KLS Martin GmbH & Co KG, Tuttlingen, Germany) and the monopolar cutter MAXIUM® (KLS Martin GmbH & Co KG, Tuttlingen, Germany). Each device has its advantages and disadvantages. In our study, we wanted to know which device makes less damage to the lung tissue, in order to use this device in our daily practice. For this purpose, we created a new experimental model, carrying out this experiment on left lungs removed from freshly slaughtered pigs. Precisely reproducible lesions on the lung surface were done with each device, set at a power output of 100 watts. The experiments were carried out at three different working speeds: 5, 10 and 20 mm/s. In both the macroscopic and microscopic lesion assessments, the lesions created by the monopolar cutter revealed obviously more thermal damage. The monopolar cutter causes substantial tissue destruction, yet the amount of surrounding coagulation is relatively minor. In contrast, the laser creates a clearly delineated lesion in the lung parenchyma. If the lesions are located 1 cm apart, the laser still performs safely, leaving no microscopic or macroscopic changes in the adjacent lung. In addition to that, the lesions do not overlap. The monopolar cutter fails in this regard: the lung tissue between deep lesions located a centimetre apart reveals post-resection thermal damage.
After performing the resection of similar lung nodules with either the laser or the monopolar cutter, we examined the lung parenchyma histologically. The nodules were completely removed in all specimens. We paid particular attention to the condition of the tissue bordering the resection surface. Those areas revealed an irregular increase in signal intensity on the MRI after performing a resection with the monopolar cutter, which we interpreted as thermal tissue damage. The lung tissue surrounding the surface following laser resection displayed no changes at all on MRI. This finding is reinforced by results from an investigation by Scanagatta et al. [9], who demonstrated in their electron-microscope examination substantial tissue damage following resection with the monopolar cutter. Therefore, they recommended that lung metastases should be laser-resected.
Lung parenchyma can be efficiently penetrated by both the laser and monopolar cutter. The latter's resection capacity at the same output is, therefore, much greater than the laser's. The monopolar cutter can also cut through a larger surface of the lung much faster than the laser. However, when closely examining the resection surface after laser application, it is evenly, that is, homogeneously coagulated, whereas the resection surface after monopolar-cutter application displays quite uneven and irregular coagulation damage which is not very deep. In this regard, the risk of bleeding and later haemorrhage after monopolar-cutter resection is much higher than after laser application. Sugimoto et al. [10] performed 12 lung wedge resections in each group of pigs. In group A, they used the LigaSure system and in group B a monopolar cutter. As a result, there was a significant greater blood loss in the monopolar cutter group.
The monopolar cutter causes greater damage to the lung tissue than the laser, especially when resecting tumours at close proximity. The laser creates sharply delineated lesions while leaving the adjacent tissue intact. Granted, lung metastases can be resected faster with the monopolar cutter, but the serious drawbacks associated with its use are: the greater tissue damage it causes and the fact that it leaks on leaving a well-coagulated resection surface, which increases the risk of haemorrhagia. Marulli et al. [11] concluded in a study about 44 patients that the aero–haemostatic laser properties (by sealing of small blood vessels and checking air leaks) allow a safe application during pulmonary lobectomy in interlobar fissure completion avoiding stapler use.
We, therefore, maintain that whenever possible, lung metastases should be resected via laser application.
CONCLUSION
Both the monopolar cutter and the laser penetrate lung tissue effectively; nevertheless, the monopolar cutter's resection capacity is greater. As the laser causes less tissue damage, it might be the preferable device for the resection of multiple lung metastases.
Conflict of interest: none declared.
REFERENCES
- 1.Lo Faso F, Solaini L, Lembo R, Bagioni P, Zago S, Pascotto RD, et al. Thoracoscopic lung metastasectomies: a 10-year, single-center experience. Surg Endosc. 2013;27:1938–1944. doi: 10.1007/s00464-012-2691-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pfannschmidt J, Egerer G, Bischof M, Thomas M, Dienemann H. Surgical intervention for pulmonary metastases. Dtsch Ärztebl Int. 2012;109:645–651. doi: 10.3238/arztebl.2012.0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maniwa Y, Okada M, Yamamoto H, Kanki M, Kiyooka K. An availability of video-assisted thoracic surgery for the resection of pulmonary metastases. Ann Thorac Cardiovasc Surg. 1999;5:69–73. [PubMed] [Google Scholar]
- 4.Vodicka J, Spidlen V, Klecka J, Simanek V, Safranek J. Use of the KLS Martin Nd:YAG laser MY 40 in lung parenchyma surgery. Rozhl Chir. 2009;88:248–252. [PubMed] [Google Scholar]
- 5.Rolle A, Pereszeleny A, Koch R, Richard M, Baier B. Is surgery for multiple lung metastases reasonable? J Thorac Cardiovasc Surg. 2006;131:1236–1242. doi: 10.1016/j.jtcvs.2005.11.053. [DOI] [PubMed] [Google Scholar]
- 6.Rolle A, Pereszlenyi A, Koch R, Bis B, Baier B. Laser resection technique and results of multiple lung metastasectomies using a new 1318 nm Nd:YAG Laser system. Lasers Surg Med. 2006;38:26–32. doi: 10.1002/lsm.20259. [DOI] [PubMed] [Google Scholar]
- 7.Rolle A, Kozlowski M. Laser resection of lung parenchyma—a new technical and clinical approach. Rocz Akad Med Bialymst. 2005;50:193–196. [PubMed] [Google Scholar]
- 8.Rolle A, Pereszlenyi A. Laser resection of lung metastases. MMCTS(2005):mmcts.2004.000570. doi: 10.1510/mmcts.2004.000570. doi:10.1510/mmcts.2004.000570. [DOI] [PubMed] [Google Scholar]
- 9.Scanagatta P, Pelosi G, Leo F, Furia S, Duranti L, Fabbri A, et al. Pulmonary resections: cytostructural effects of different—wavelength lasers versus electrocautery. Tumori. 2012;98:90–93. doi: 10.1177/030089161209800112. [DOI] [PubMed] [Google Scholar]
- 10.Sugimoto S, Toyooka S, Iga N, Furukawa M, Sugimoto R, Shien K, et al. Use of a vessel sealing system versus conventional electrocautery for lung parenchymal resection. Surg Today. 2013 doi: 10.1007/s00595-013-0545-1. doi:10.1007/s00595-013-0545-1. [DOI] [PubMed] [Google Scholar]
- 11.Marulli G, Droghetti A, DiChiara F, Calabrese F, Rebusso A, Perissinotto E, et al. A prospective randomized trial comparing stapler and laser techniques for interlobar fissure completion during pulmonary lobectomy. Lasers Med Sci. 2013;28:505–511. doi: 10.1007/s10103-012-1097-0. [DOI] [PubMed] [Google Scholar]