Abstract
Bone is the most common metastatic site of breast cancer (BC) and sternal metastasis usually occurs in an isolated setting. We performed sternal reconstruction using a new total titanium custom-made neosternum after subtotal sternectomy for an isolated BC metastasis. Postoperative care was uneventful during a 7-day in-hospital stay. After a 6-month follow-up, the patient denied any shortness of breath, chest pain or limitation on her daily activities. The chest was stable without any paradoxical motion. Chest X-ray did not show any material fracture, pleural effusion or lung abnormalities. As it entails lower postoperative risk than previously existing reconstructive materials, the new material used in our sternal reconstruction may extend the existing range of indications of sternectomy for cancer with curative intent.
Keywords: Sternal replacement, Breast cancer, Sternectomy
INTRODUCTION
Breast cancer (BC) is the leading cause of death by cancer in women in industrialized countries. Bone is the most common metastatic site of BC and sternal metastasis usually occurs in an isolated setting [1]. Although no curative treatment for metastatic BC is currently available, complete surgical resection may be of interest for BC patients with isolated sternal metastasis, and long-term survival has already been reported. In addition, surgical resection could relieve symptoms such as pain, thereby improving quality of life [2].
Several techniques have been proposed to correct chest wall defects following subtotal or total sternectomy, but none can ensure satisfactory results as regards the following goals in sternal reconstruction: (i) to achieve chest wall rigidity so as to avoid any paradoxical chest wall motion leading to respiratory discomfort or failure and prolonged hospital stay [3], (ii) to protect the mediastinal organs from external trauma and (iii) to reduce the likelihood of infection [4].
With these criteria in mind, we performed a sternal reconstruction using a new total titanium custom-made neosternum after subtotal sternectomy for an isolated BC metastasis.
CASE REPORT
A 28-year old woman presented with left BC with dull pain in the upper-mid chest. Diagnosis of invasive ductal carcinoma was made by echo-guided core biopsy. 18-Fluoro-Desoxy-Glucose (FDG) positron-emission tomography (FDG-PET) showed hypermetabolic left breast mass, axillary lymph nodes and sternal body (Fig. 1A). The patient initially underwent four cycles of chemotherapy (doxorubicin and docetaxel). Based on post-chemotherapy FDG-PET results, all hypermetabolic foci disappeared and cancer response was consequently judged complete. While initially osteolytic (Fig. 1B), the sternal lesion became bone-condensing. Sternal and breast resection was decided after discussion with oncologists and radiotherapists.
Figure 1:

(A) 18-FDG-PET showed hypermetabolic left breast mass and sternal body. (B) Chest tomography scan of the osteolytic sternal metastasis before neoadjuvant chemotherapy. (C) The custom-made titanium neosternum with a design based on three dimensional simulation from preoperative chest CT.
A custom-made titanium neosternum was designed based on three dimensional simulation from preoperative chest computed tomography (Thorib™, NeuroFrance Implants, La Ville aux Clercs, France). It was composed of a multiperforated plate connected to three staples on each side drawn to be tightened on the second, third and fourth ribs (Fig. 1C). We then performed a left radical mastectomy with Level III axillary lymph node dissection and subtotal sternectomy with chest wall reconstruction. Sternal resection started just below the first rib insertion down to the xiphoid process. Chest wall reconstruction was carried out using the custom-made titanium neosternum without any mesh interposition (Fig. 2A). A chest tube on each pleural space was inserted before covering the neosternum with the two pectoralis majors. The patient was immediately extubated and no paradoxical motion of the chest was noted. She denied any chest pain and could breathe deeply, cough and even undergo physiotherapy without any limitations. Postoperative care was uneventful during a 7-day in-hospital stay. Pathological examination of the resected tumour showed no residual tumour consistent with the clinical complete response after chemotherapy. After a 6-month follow-up, the patient denied any shortness of breath, chest pain or limitation on her daily activities. The chest was stable without paradoxical motion. Chest X-ray did not show any material fracture, pleural effusion or lung abnormalities (Fig. 2B).
Figure 2:
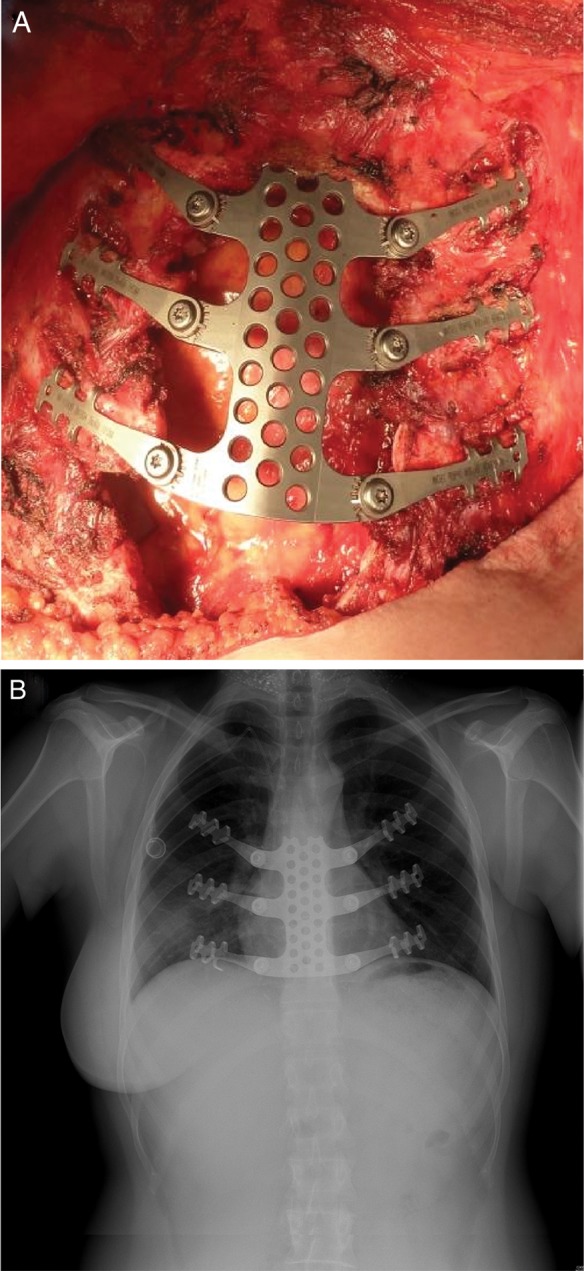
(A) Intraoperative view after chest wall reconstruction showing the anatomical restitution of the chest wall. (B) Postoperative chest radiography showing the neo-titanium sternum.
DISCUSSION
Over the past decades, the benefits of sternal or large chest wall resections were usually counterbalanced by high postoperative morbidity and mortality rates. Mansour et al. [5] reported 7% overall mortality, with a 24% rate of pneumonia and an overall length of stay of 18 ± 16 days after chest wall reconstruction using mesh. Indeed, a lack of postoperative chest wall rigidity could lead to paradoxical chest motion with acute respiratory failure, difficulty in weaning the patient from the ventilator and a high risk of pneumonia. The rigidity of the chest wall cavity must be restored in order to diminish the number and severity of complications. In this context, large chest wall resections with low postoperative risk have become possible, since titanium bars attached between ribs can sufficiently rigidify the chest wall [3, 4]. However, bars did not protect the heart from external trauma as custom-made titanium plate could do. However, when a custom-made titanium plate is used instead of bars, it better protects the heart from external trauma. Titanium is a biocompatible, inert material, malleable enough to allow a custom-made design reproducing the shape of the sternum and the chest wall. Moreover, without compromising rigidity, holes were added to the plate surface so as to avoid seroma, which is a source of infection. At least, titanium does not interfere with computed tomography or magnetic resonance imaging during the postoperative follow-up.
CONCLUSION
In conclusion, this new material for sternal reconstruction may extend the existing range of indications of sternectomy for cancer with curative intent with lower postoperative risk compared with the reconstructive materials that have already been used. The long-term follow-up result will be useful to define this technique as the conventional surgical reconstruction after sternal resection.
Conflict of interest: none declared.
REFERENCES
- 1.Noguchi S, Miyauchi K, Nishizawa Y, Imaoka S, Koyama H, Iwanaga T. Results of surgical treatment for sternal metastasis of breast cancer. Cancer. 1988;62:1397–401. doi: 10.1002/1097-0142(19881001)62:7<1397::aid-cncr2820620726>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 2.Levy Faber D, Fadel E, Kolb F, Delaloge S, Mercier O, Mussot S, et al. Outcome of full-thickness chest wall resection for isolated breast cancer recurrence. Eur J Cardiothorac Surg. 2013;44:637–642. doi: 10.1093/ejcts/ezt105. [DOI] [PubMed] [Google Scholar]
- 3.Billè A, Okiror L, Karenovics W, Routledge T. Experience with titanium devices for rib fixation and coverage of chest wall defects. Interact CardioVasc Thorac Surg. 2012;15:588–95. doi: 10.1093/icvts/ivs327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fabre D, El Batti S, Singhal S, Mercier O, Mussot S, Fadel E, et al. A paradigm shift for sternal reconstruction using a novel titanium rib bridge system following oncological resections. Eur J Cardiothorac Surg. 2012;42:965–70. doi: 10.1093/ejcts/ezs211. [DOI] [PubMed] [Google Scholar]
- 5.Mansour KA, Thourani VH, Losken A, Reeves JG, Miller JI, Jr, Carlson GW, et al. Chest wall resection and reconstruction: a 25-year experience. Ann Thorac Surg. 2002;73:1720–5. doi: 10.1016/s0003-4975(02)03527-0. [DOI] [PubMed] [Google Scholar]


