Abstract
Background:
Kinesiological taping (KT) is commonly used to improve symptoms associated with musculoskeletal disorders. However, review of the literature revealed minimal evidence to support the use of KT in treatment of shoulder disorders and controversy exists regarding the effect of KT in patients with shoulder impingement syndrome (SIS).
Objective:
The purpose of this study was to investigate the effect of KT on pain intensity during movement, pain experienced during the night (nocturnal pain), and pain‐free shoulder range of motion (ROM) immediately after taping, after three days and after one week, in patients with SIS.
Design:
Randomized, Double blinded, Placebo‐controlled design.
Participants:
A total of 30 patients with SIS participated in this study. Patients were assigned randomly to a control (N = 15) and an experimental group (N = 15).
Methods:
The patients in the experimental group received a standardized therapeutic KT. The standardized, placebo neutral KT was applied for control group. KT was applied two times with a three day interval, remaining on during the 3 day interval. Both groups followed the same procedures. Pain‐free active ROM during shoulder abduction, flexion, and elevation in the scapular plane was measured. Visual analogue scale (VAS) for pain intensity during movement or nocturnal pain and was assessed at baseline, immediately after KT, after three days, and one week after KT.
Results:
The result of repeated measures ANOVA showed a significant change in pain level during movement, nocturnal pain, and pain‐free ROM (p = 0.000) after KT in the experimental group. In the ANCOVA, controlling for pre‐test scores, change in pain level at movement (p = 0.009) and nocturnal pain (p = 0.04) immediately after KT was significantly greater in the experimental group than in control group. There was no significant difference in ROM measures (p > 0.05) between groups immediately after KT. No significant differences were found between the two groups in the after one week measurements of pain intensity and shoulder ROM.
Conclusion:
The KT produces an immediate improvement in the pain intensity at movement and nocturnal pain in patients with SIS.
Level of Evidence:
1
Keywords: Kinesiological taping, pain, range of motion, shoulder impingement
INTRODUCTION
Shoulder pain is a common musculoskeletal complaint in today's societies. Previous authors have indicated that lifetime prevalence of shoulder pain ranged from 7% to 36% of the population.1,2 Shoulder impingement syndrome (SIS) is the most common shoulder complaint in individuals attending orthopedic and physical therapy clinics (44–65%).3 Several factors, based on clinical findings and scientific experiments, have been associated with the development of SIS. Investigators have attributed subacromial impingement to various factors, such as anatomic morphology, overuse, and instability of the glenohumeral joint. Moreover, investigators have focused on the role of scapular control in SIS. The scapula, along with the humerus, clavicle, and thorax, makes up the shoulder complex. The scapula is considered a key link between the upper extremity and the axial skeleton, and the musculature around it provides the proximal stability for upper extremity activities.5‐7 Coordinated movements of the scapula and the humerus known as “scapulohumeral rhythm” contribute to the range of motion (ROM) at the glenohumeral joint. Abnormal scapulothoracic kinematics may play a role in the development of SIS and are often considered in the clinical management and rehabilitation of this condition.6‐8
Abnormal patterns of scapular motion including dec‐reased scapular posterior tipping, increased internal rotation, and decreased upward rotation have been identified in patients with SIS.6‐8 These changes may reduce the subacromial space, resulting in impingement of the subacromial structures.9 Thus, the restoration of scapular control has been emphasized in the rehabilitation programs for SIS.10,11
Taping has been recently considered as an option to control scapular movement in patients with shoulder problems.11 Taping is commonly used in the field of rehabilitation as both a means of treatment and prevention of musculoskeletal disorders.12‐16 The function of tape is to provide support during movement.17 The underlying mechanisms of taping effects are still unclear. It has been speculated that taping works by inducing proprioceptive feedback or providing alignment correction during dynamic movements.18,19
Although some investigators applied rigid tape across the muscle bellies of the shoulder girdle and found pain relief and increased shoulder ROM,16,19 Ackerman et al found negative effects of using rigid tape on movement and performance of the upper extremity due to movement restriction and skin irritation.18 More recently, there has been increased interest in the use of kinesiological taping (KT) by physical therapists in order to facilitate control of scapula.20 KT has been designed to mimic the qualities of human skin and can be applied to virtually any muscle or joint in the body.
Review of the literature revealed minimal evidence to support the use of KT in the treatment of shoulder disorders. Controversy exists regarding the effects of KT on patients with shoulder pain and related disorders. Some investigators have demonstrated that taping effectively improved the postural alignment, increased the shoulder ROM, and reduced pain and discomfort of the glenohueral joint.15,16,21,28,29 However, the results of the other studies did not support the utilization of KT for decreasing pain intensity or disability in patients with suspected shoulder tendonitis/impingement.18,19 This controversy may be due to the use of different designs, taping methods, subject samples, and testing procedures. The participants in most similar previous studies were those in specified population (i.e.: athletes, musicians) with SIS or rotator cuff tendinitis. Few studies have been conducted in patients with shoulder impingement within the general population. Some authors have assessed pain intensity (nocturnal or daily pain)16,21,29 while others assessed shoulder ROM after the application of KT.15,30 Most of the previous studies applied KT only to one muscle (upper trapezius, lower trapezius, supraspinatus, or deltoid). Other studies used two or three taping techniques applied to different muscles. Moreover, most of the previous studies applied KT solely for muscle effects and did not use glenohumeral mechanical correction technique, which is purported to provide more space under subacromial space, by inducing external rotation at glenohumeral joint.21
To the authors' knowledge, no study has directly investigated the effect of KT on pain intensity during shoulder movement, nocturnal pain of the shoulder, and pain free ROM in patients with SIS. The purpose of this study was to investigate the effect of KT on pain intensity during movement, pain experienced during the night (nocturnal pain), and pain‐free shoulder range of motion (ROM) immediately after taping, after three days and after one week in patients with SIS. The authors' hypothesis for this study was that the application of KT would have a significant effect (decrease) on pain intensity and pain free shoulder ROM (increase) in patients with SIS.
Methods and Subjects
A randomized, double blinded, placebo controlled study was conducted in order to assess the effectiveness of KT in patients with SIS. Thirty patients with SIS, who had been referred by orthopedic physicians for outpatient physical therapy evaluation and intervention, participated in this study. The patient population was a sample of convenience made up of subjects who agreed to participate and fulfilled the inclusion criteria. Patients were included if they were positive on two or more shoulder impingement screening items, and tested positive on at least one of the specific subacromial impingement tests. The shoulder impingement screening items included: a history of proximal anterior or lateral shoulder pain that had continued for more than one week during the last six months prior to study; a painful arc sign during active shoulder elevation; tenderness to rotator cuff tendon palpation; pain with resisted isometric shoulder abduction; positive Jobe's test (empty can test). Specific subacromial impingement tests used in the present study included the Neer sign, the Hawkins sign,24‐26 and theYocum test.27
Patients were excluded if they had a history of dislocation, fracture, or traumatic injuries within the shoulder complex; a history of shoulder surgery within the last six months; reproduction of symptoms during the cervical screening examination; failure to complete testing sessions; or complete rupture of rotator cuff muscles with acute inflammation.26 After the initial screening, 30 patients fulfilled all inclusion criteria. Before participating in the study, all subjects signed an informed consent form approved by the human subjects committee.
Patients who were prescribed a non‐steroidal anti‐inflammatory drug (NSAID) prior to the study were instructed to not take the medication. Subjects who were not prescribed or taking NSAID or analgesics were instructed to avoid doing so during the study. To control for activity level, subjects were asked to not perform upper extremity exercises for one week during the study. This issue was monitored with the subjects when they returned for re‐assessments.
Group Assignment
Patients were randomly assigned to a control group (N = 15, mean age = 46.6 ±?14.24 years) and an experimental group (N = 15, mean age = 46.53 ±?13.31). Block randomization was used to keep the numbers in each group very close. Power analysis was used to determine the sample size for the study. Type I error (α) was set at 0.05 and power of the test was 0.80. Considering this, the calculated sample size showed that 15 subjects in each group was appropriate to test the hypothesis and have confidence in the results. Physical characteristics of the subjects in each group are shown in Table 1.
Table 1.
Demographic data of the subjects (Mean ±SD)
| Variables | Control group (n=15) | Experimental group (n=15) | |
|---|---|---|---|
| Age (years) | 46.6 ±14.24 | 46.53 ± 13.31 | |
| Weight (kg) | 75.4 ± 7.45 | 78.43 ±11.01 | |
| Height (cm) | 166 ± 9.07 | 165 ± 8.45 | |
| BMI | 28.84 ±3.65 | 27.52 ±3.92 | |
| Pain duration (month) | 9.33 ± 10.48 | 7.63 ± 7.43 | |
| Sex | Male | (n=8) 53.3% | (n=7) 46.7% |
| Female | (n=7) 46.7% | (n=8) 53.3% | |
| Affected side | Right | (n=11) 73.33% | (n=9) 60% |
| Left | (n=4) 26.66% | (n=6) 40% | |
| Dominant side | Right | (n=13) 86.7% | (n=13) 86.7% |
| Left | (n=2) 13.3% | (n=2) 13.3% | |
SD = Standard Deviation
BMI= Body mass index
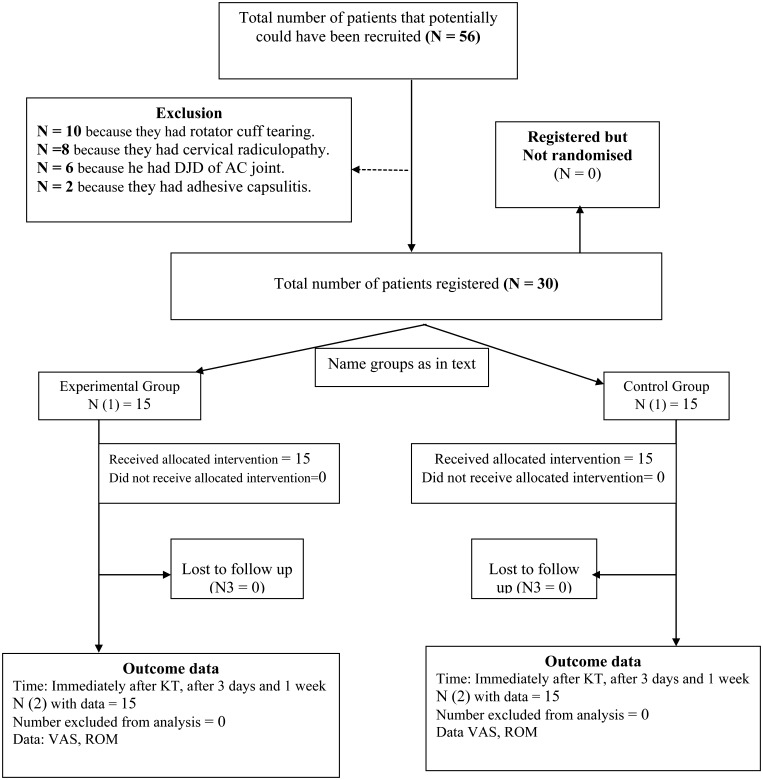
The participant flow diagram provided in Figure 1 reports the numbers and timing of randomization assignment, interventions, and measurements for each group (Figure 1).
Figure 1.
Flow diagram for the study.
Taping technique
KT has several benefits, depending on the amount of stretch applied to the tape during application. It has been hypothesized to provide positional stimulus through the skin, allow for “more space” by lifting fascia and soft tissue, provide sensory stimulation to assist or limit motion, and aid in removal of edema.28 Standard 2‐in (5‐cm) beige Kinesio TexTM tape was used for application in both groups. The patients in the experimental group received a standardized therapeutic KT. The general application guidelines were consistent with the procedure described by Kase et al.28 The first strip was a Y‐strip which was applied from insertion to origin of supraspinatus with paper off tension. A Y‐strip refers to a section of tape that has a portion cut down the middle to produce 2 tails. Paper‐off tension means applying the tape directly to the skin as it comes off the paper backing. The first strip was applied with the subject in a position combining contra‐lateral cervical side bending and the arm reaching behind the back as if reaching into the contralateral backside pocket. The second strip was a Y‐strip applied to the deltoid, from insertion to origin with paper‐off tension. The second strip was applied with the first tail to the anterior deltoid while the arm was externally rotated and horizontally abducted. The other tail for the posterior deltoid was applied with the arm horizontally adducted and internally rotated. The third strip, an I‐strip (no cut down the middle of the tape), was applied from the coracoid process to the posterior deltoid with approximately 50% to 75% stretch (tension) and downward pressure applied to the tape at the region of perceived tenderness for glenohumeral mechanical correction. To apply the third strip, the upper extremity was externally rotated while at the side and then moved into shoulder flexion and slight horizontal adduction as the end of the tape was applied with no stretch. The fourth strip was a Y‐strip KT to lower trapezius from the thoracic spine to the medial border of the scapula with approximately 50% stretch (tension).
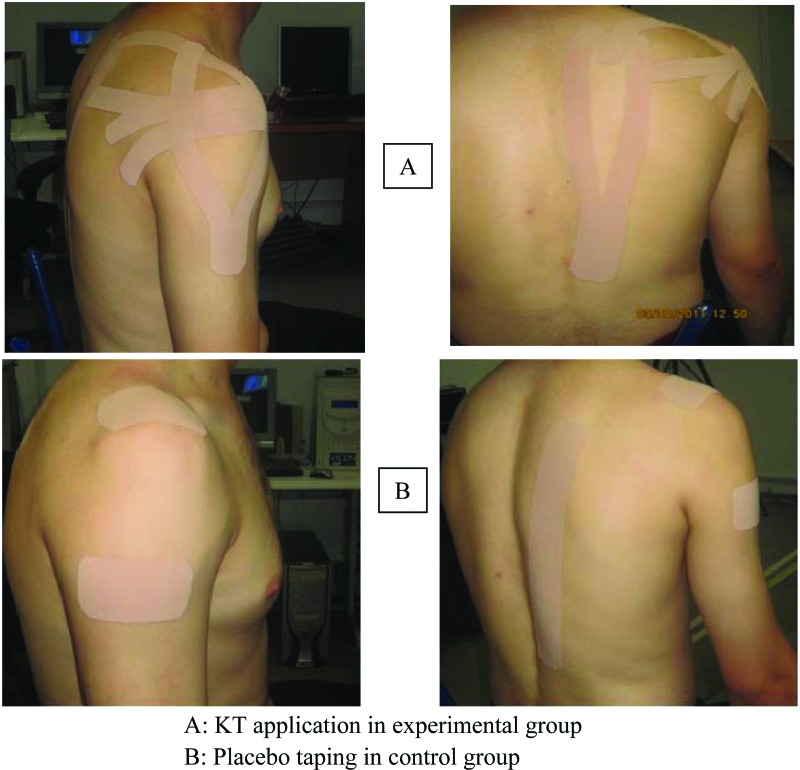
The patients in control group received a standardized, placebo KT. The placebo taping consisted of three I‐strips KT with no tension. One piece of tape was placed over the acromioclavicular joint in the sagittal plane and one on the distal deltoid in the transverse plane, both with no tension. Finally, an I‐strip KT was applied on the lower trapezius muscle without any tension. The placebo group sites were selected because they are the most common locations of perceived pain by patients with rotator cuff tendonitis or impingement28‐30 Figure 2 depicts the taping technique for both groups.
Figure 2.
Techniques for KT application in the two groups.
Outcome measures
The primary outcome measures were: pain intensity during movement and nocturnal pain measured using visual analogue scale (VAS) and pain‐free active ROM of abduction, flexion, and scapular plane elevation. All the measures were obtained at baseline, immediately after taping, after 3 days of wearing the tape (on the fourth day), and finally at one week after wearing the KT. The VAS is a simple, sensitive, and reproducible instrument frequently used for the assessment of pain intensity. In clinical practice the amount of pain relief, assessed by VAS, is often considered as a measure of the efficacy of treatment. In this study, a 100‐mm (10‐cm) VAS for pain was used to record the pain intensity during ADL as well as nocturnal pain. For pain during movement, the pain intensity experienced at the end point of the pain‐free active ROM test was recorded. The reliability of VAS for assessment of pain intensity has been previously established.31 For nocturnal pain, the worst pain during the night was reported by the patient.32
Using a standard goniometer, shoulder ROM measurements of forward flexion, abduction, and scapular plane elevation (scaption) were taken. Investigators have commonly used the universal goniometer to measure active shoulder elevation. The reliability and validity of shoulder elevation measurements has been previously established using a digital inclinometer and goniometer.33 In this study, one investigator assessed shoulder AROM in the three different planes. Pain‐free active ROM was operationally defined as the ROM achieved at the “point of first onset of pain.”
Procedures
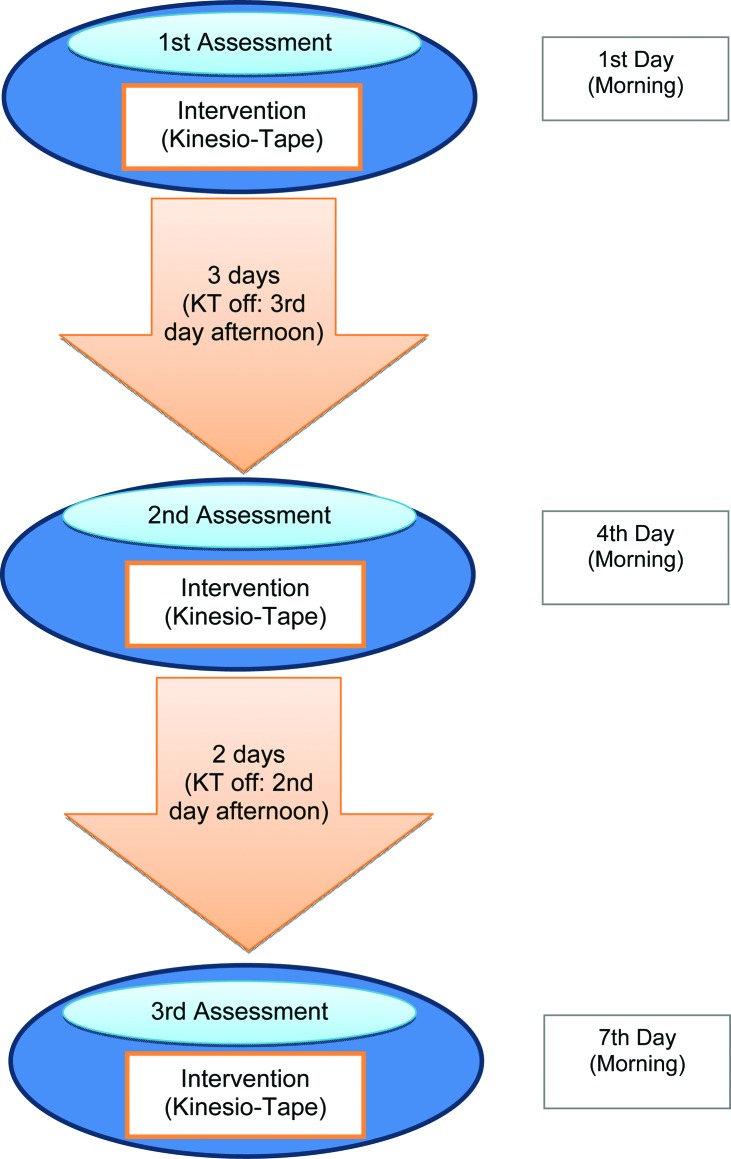
Participants were instructed to maintain the tape as applied for three days and to come back to the clinic for re‐evaluation on the fourth day. Subjects were asked to remove the tape on the afternoon of the third day, and come to clinic on the morning of the fourth day for the second assessment. At the day four follow‐up, the investigator inspected the subjects' skin and re‐assessed the outcome measures. Subjects were then taped with the same method used before, based on their group assignment, and instructed to wear the tape for an additional two days. Again with the tape removed on the afternoon of the sixth day, and all subjects were instructed to return to the clinic on seventh day at the morning for the final evaluation. The details of the flow of the procedures are provided in Figure 3.
Figure 3.
Diagram for timing of intervention and measurement of outcome.
Two investigators were involved in this study. One performed the taping in both groups, and the second, who was unaware of the group assignment, performed the measurements before and after KT. The participants were unaware whether they were in the experimental or control group of the study.
Statistical Methods
Kolmogrov‐Smirnov test was utilized to assess the normality of distribution for tested variables (shoulder nocturnal pain and ADL's, shoulder abduction, flexion and scaption ROM) before and after treatment. Normal distribution was observed for variables in both groups. Independent t–tests were used to determine whether any differences existed in the VAS and goniometeric measurements between two groups before treatment. Repeated measures ANOVA was used to determine any significant change occurred in the tested variables (VAS during movement or nocturnal pain, and pain‐free ROM) after KT (immediately after taping, after three days, and after one week) when compared with pre‐treatment scores in both the control and experimental groups. Analysis of Covariance (ANCOVA) was used to determine whether significant differences existed between the control and experimental groups in post‐test measurement scores, with pre‐treatment scores used as covariates in the analysis. The test for homogeneity of regression coefficient was conducted because it is a necessary condition for valid application of the ANCOVA. Analysis was conducted using SPSS version 16.0.
RESULTS
Pre‐ and post‐measurement scores for the variables tested in control and experimental groups are provided in Table 2.
Table 2.
The pre‐ and post‐measurement scores for tested variables in the control and experimental group
| Variable | Group | Before KT | Immediately after taping | After 3 days | After 1 week | P‐value |
|---|---|---|---|---|---|---|
| Pain intensity during movement | Exp. | 5.86 ±1.80 | 3.73 ± 1.90 | 3.75 ± 1.76 | 2.9 ±2.25 | 0.000 |
| Cont. | 5.53 ± 1.55 | 5.13 ± 2.26 | 4.6 ± 2.02 | 4.2 ±2.70 | 0.06 | |
| Nocturnal Pain intensity | Exp. | 6.73 ± 1.86 | 3.66 ± 2.41 | 3.8 ± 2.21 | 2.7 ± 2.34 | 0.000 |
| Cont. | 5.86 ± 2.44 | 4.8 ± 2.95 | 3.93 ± 2.63 | 3.73 ± 3.23 | 0.02 | |
| Abduction ROM | Exp. | 152.8 ± 5.32 | 165.53 ± 4.08 | 167.4 ± 4.71 | 172.33 ± 3.93 | 0.000 |
| Cont. | 164.93 ± 4 | 166.93 ± 3.45 | 170.86 ± 2.62 | 174.2 ± 2.09 | 0.005 | |
| Flexion ROM | Exp. | 159.06 ± 4.16 | 169.46 ± 3.32 | 170.13 ± 3.16 | 172.33 ± 3.51 | 0.000 |
| Cont. | 172.06 ± 3.05 | 173.46 ± 2.09 | 175.66 ± 1.94 | 176.53 ± 1.76 | 0.40 | |
| Scaption ROM | Exp. | 155.86 ± 5.55 | 165.4 ± 4.23 | 167.73 ± 3.93 | 171.53 ± 4 | 0.000 |
| Cont. | 166.86 ± 3.95 | 169.2 ± 3.26 | 171.06 ± 2.99 | 174.93 ± 2.01 | 0.01 |
Exp. = Experimental
Cont. = Control
ROM = Range of motion
Experimental Group Results
The result of repeated measures ANOVA showed a significant difference of 2‐3 points in VAS for pain intensity during movement (p = 0.000) when compared with subjects' pre‐treatement scores. A significant difference of 3‐4 points in VAS for nocturnal pain measures was also demonstrated after KT (p = 0.000) when compared with subjects' pre‐treatment scores.
Significant differences in pain‐free shoulder active ROM in each of the three ROM measurements were found after KT, (ranging between 10 and 19 degrees) (p=0.000) and when compared with subjects' pre‐treatment scores (Table 2). Post hoc analysis revealed significant decrease in pain intensity and significant increase in active shoulder ROM in experimental group immediately or one week after KT.
Control Group Results
In the control group, repeated measures ANOVA showed no significant difference in pain intensity during movement, nocturnal pain, and shoulder flexion ROM after placebo taping as compared to pre‐treatment scores. However, a significant difference of 1 and 2 points in VAS for nocturnal pain measures was found immediately and one week after placebo respectively as compared to pre‐treatment scores. A significant difference in pain‐free shoulder abduction ROM (9 degrees) and scaption ROM (8 degrees) and was found after one week of placebo taping as compared to pre‐treatment values (Tables 2 & 3). However, the data revealed no significant increase in pain‐free shoulder abduction ROM (2 degrees) and scaption ROM (2 degrees) immediately after placebo taping (Tables 2 & 3).
Table 3.
The results of ANCOVA in control and experimental groups with pre‐test scores as the covariates immediately after taping, after 3 days and 1 week
| Variable | Measurement session | Control | Experimental | Between group differnces | P‐value of ANCOVA |
|---|---|---|---|---|---|
| Mean ± SD | Mean +SD | ||||
| Pain inetnsity during movement | Change immediately after taping | 0.4 ± 0.71 | 2.13±0.1 | 1.73 | 0.009* |
| Change after 3 days | 0.93± 0.47 | 2.11±0.04 | 1.18 | 0.05 | |
| Change after 1 week | 1.33 ± 1.15 | 2.96 ± 0.45 | 1.63 | 0.10 | |
| Nocturnal Pain intensity | Change immediately after taping | 1.06 ±0.51 | 3.07 ±0.55 | 2.01 | 0.04* |
| Change after 3 days | 1.93±0.19 | 2.93±0.35 | 1.00 | 0.51 | |
| Change after 1 week | 2.13 ± 0.79 | 4.3 ± 0.48 | 2.17 | 0.23 | |
| Abduction ROM | Change immediately after taping | 2 ± 0.55 | 12.73 ± 1.24 | 10.73 | 0.10 |
| Change after 3 days | 5.93 ± 1.38 | 14.6 ±0.61 | 8.67 | 0.28 | |
| Change after 1 week | 9.27± 1.91 | 19.53 ±1.39 | 10.26 | 0.34 | |
| Flexion ROM | Change immediately after taping | 1.4 ±0.96 | 10.4 ±0.84 | 9.00 | 0.09 |
| Change after 3 days | 3.6± 1.11 | 11.07 ±1 | 7.47 | 0.88 | |
| Change after 1 week | 4.47± 1.29 | 13.27 ± 0.65 | 8.8 | 0.70 | |
| Scaption ROM | Change immediately after taping | 2.34 ± 0.69 | 9.54 ±1.32 | 7.2 | 0.23 |
| Change after 3 days | 4.2 ± 0.96 | 11.87 ±1.62 | 7.67 | 0.28 | |
| Change after 1 week | 8.07 ±1.94 | 15.67 ±1.55 | 7.6 | 0.73 |
‐ Bolded cell indicates significant difference in change of variables tested between groups after kinesio taping.
The findings of the ANCOVA using pre‐treatment score as the covariate revealed that change in pain intensity during movement (p = 0.009) and nocturnal pain (p = 0.04) immediately after KT was significantly greater in the experimental group (2 and 3 points in VAS for pain intensity during movement and nocturnal pain respectively) than in the control group (0.4 and 1.3 points in VAS for pain intensity during movement and nocturnal pain respectively) (Table 3). However, the ANCOVA demonstrated that change in pain intensity during movement (p = 0.10) or nocturnal pain (p = 0.23) and change in shoulder abduction ROM (p =0.34), flexion ROM (p = 0.70) and scaption ROM (p = 0.73) after one week was not statistically significantly different between the control and experimental groups (Table 3).
DISCUSSION
The results of this study showed a significant improvement in pain intensity during movement, nocturnal pain, and pain‐free shoulder abduction, flexion and scaption ROM immediately after taping as compared to the pre‐test values. The results also revealed no significant difference in pain intensity during movement and shoulder flexion ROM immediately, after three days, and at the one week after placebo taping assessment. However, a significant decrease in nocturnal pain measures was found immediately and one week after taping in control group. Although no significant differences were noted in shoulder abduction or scaption ROM immediately after placebo taping, a significant increase in shoulder abduction or scaption ROM was found one week after taping in control group.
These data showed a significant difference in change of pain intensity during movement or nocturnal pain between the groups immediately after taping. The authors found a significantly greater decrease in pain intensity during movement or nocturnal pain immediately after KT application (experimental group) than placebo taping (control group). There was no significant difference in change of pain intensity (during movement or nocturnal) and change of pain‐free shoulder ROM between two groups after one week.
The fact that the experimental group showed a significantly greater improvement in pain intensity immediately after KT, but did not maintain this pattern after one week, may suggest that the immediate effect of KT is the important part of the intervention in the experimental group. Similar findings have been reported elsewhere. Kaya et al29 studied 55 patients with SIS treated by KT or local modalities and found that although immediate effect of KT is greater than the local modalities, KT was similarly effective at the second week of the treatment. They suggested KT as an alternative treatment option in the management of SIS especially when an immediate effect is desired.29The results of the study conducted by Miller and Osmotherly34 provided evidence for a short‐term role for taping as an adjunct to routine physiotherapy program in the treatment of SIS. They found that KT has main effect on the early stage of treatment and that there was not a significant KT effect after several weeks. The immediate results and improvements following the KT are also reflected in the work of researchers who found significant improvements immediately following KT compared with placebo taping in patients with other musculoskeletal disorders such as patellofemoral pain syndrome35,36 or whiplash‐associated disorders.37,38
Review of the literature demonstrates few reports of KT being used in the treatment of SIS. In the current study, four taping techniques were applied while the other previous studies applied one to three taping techniques.30,32 More skillfully applied KT may promote a greater proprioceptive effect, joint mechanical correction, and enhancement of muscle function. Moreover, the four taping techniques that were applied in this study sought to provide facilitation of the lower trapezius muscle, inhibition of the deltoid and upper trapezius muscles, and mechanical correction affecting the subacromial space.29,30,32
Although the underlying mechanisms of taping effects are still unclear and proposed physiological mechanisms regarding this topic remain hypothetical, some investigators believe that taping works by offering constant proprioceptive feedback or providing alignment correction during movements. In this study, however, pain intensity improvement was significantly different between two groups immediately after KT without a concurrent significant difference in change in shoulder active ROM. Pain modulation via the gate control theory is one probable explanation for such a change. It has been speculated that tape stimulates neuromuscular pathways by increased afferent feedback.12 Increase in afferent stimulus to large‐diameter nerve fibers can lessen the input received from the small‐diameter nerve fibers conducting nociception. Another possibility is that the improved motion might have been due to an increase in the number of supraspinatus motor units recruited to perform the activity due to an increase in the proprioceptive stimulus. However, this proposition has not been supported by recent publications, which showed that there was no significant increase in muscular activity after taping as measured by electromyography.19
The immediate effect of KT may also be due to space correction or lymphatic effects. Space correction in this case is aimed at increasing the subacromial space as well as enhancing the control of the muscles stabilizing the scapula throughout an arc of glenohumeral elevation motion.32 Such increase in space may allow for a decrease in pain intensity during movement.
No significant differences in the change in shoulder ROM existed between the two groups immediately and one week after KT application. This is in accordance with the findings of the study conducted by McConnell et al39 who showed no significant effect of shoulder taping on maximum shoulder abduction ROM. Likewise, Lin et al40 attributed the effects of shoulder taping to proprioceptive feedback factors.
The reason the authors of the current study found no statistical differences between groups may be explained by the relatively small between‐group differences observed (Table 3). As shown, the maximum between group change scores for pain related to nocturnal pain scores on a 10 cm scale were 2.01 cm immediately after taping and 2.17 cm after one week, respectively. Although, at this time point the between groups differences were not statistically different, both could be considered clinically important changes.11 However, it should be noted that the minimally clinically important change of the VAS score has been described to be between 3.00‐3.50 cm in descriptions of musculoskeletal pain intensity.41,42 Likewise, the change in shoulder abduction ROM in the treatment group of approximately 11 degrees may be clinically, although not statistically significant.
Limitations and suggestions for future studies
In this study, the effect of KT on kinematics of the scapula was not assessed. Further studies are needed to investigate the effect of KT on the scapular kinematics in patients with SIS. Another area of concern is that in this study the pain intensity and shoulder ROM were assessed before and after treatment as outcome measures. Future study is suggested to assess the effect of KT on functional ablilty/disability of the arm and shoulder in patients with SIS.
CONCLUSION
KT produced an immediate improvement in pain intensity during movement and in the measure of nocturnal pain. However, no longer term effects of KT existed after one week. No significant effect of KT on shoulder active ROM was discovered. KT can be prescribed for patients with SIS especially when pain relief is the short‐term goal of the treatment. More clinical research is needed to investigate the effect of KT on scapular and shoulder kinematics and on disability of the arm and shoulder.
REFERENCES
- 1. Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003. CD004258. DOI: 10.1002/14651858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guerra de Hoyos JA, Andres Martin Mdel C, Bassas y Baena de Leon E, et al. Randomised trial of long term effect of acupuncture for shoulder pain. Pain. 2004;112:289‐298 [DOI] [PubMed] [Google Scholar]
- 3. Michener L, Walsworth M, Burnet E. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther. 2004; 17(2):152‐164 [DOI] [PubMed] [Google Scholar]
- 4. Braman J, Engel S, LaPrade R, Ludewig P. In vivo assessment of scapulohumeral rhythm during unconstrained overhead reaching in asymptomatic subjects. J Shoulder Elbow Surg. 2009;18:960‐967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lombardi Jr I, Magri, Fleury A, Da Silva A, Natour J. Progressive resistance training in patients with shoulder impingement syndrome: a randomized controlled trial. Arthritis Rheum. 2008;59(5):615‐622 [DOI] [PubMed] [Google Scholar]
- 6. Michener L, McClure P, Karduna A. Anatomical and biomechanical mechanisms of subacromial impinge‐ment syndrome. Clin Biomech. 2003;18(5):369‐79 [DOI] [PubMed] [Google Scholar]
- 7. McClure P, Michener L, Karduna A. Shoulder function and 3‐dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86(8):1075. [PubMed] [Google Scholar]
- 8. Ebaugh D, McClure P, Karduna A. Three‐dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech. 2005;20(7):700‐9 [DOI] [PubMed] [Google Scholar]
- 9. Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment? Br J Sports Med. 2009;43(4):259‐64 [DOI] [PubMed] [Google Scholar]
- 10. Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003; 11:142‐151 [DOI] [PubMed] [Google Scholar]
- 11. Mottram SL. Dynamic stability of the scapula. Man Ther. 1997; 2:123‐131 [DOI] [PubMed] [Google Scholar]
- 12. Kneeshaw D. Shoulder taping in the clinical setting. J Bodyw Mov Ther. 2002; 6:2‐8 [Google Scholar]
- 13. Lewis JS, Wright C, Green A. Subacromial impingement syndrome: the effect of changing posture on shoulder range of movement. J Orthop Sports Phys Ther. 2005; 35:72‐87 [DOI] [PubMed] [Google Scholar]
- 14. Morrissey D. Proprioceptive shoulder taping. J Bodyw Mov Ther. 2000; 4(3):189‐94 [Google Scholar]
- 15. Jaraczewska E, Long C. Kinesio® taping in stroke: Improving functional use of the upper extremity in hemiplegia. Top Stroke Rehabil. 2006;13(3):31‐42 [DOI] [PubMed] [Google Scholar]
- 16. Wang S. The effect of Mcconnell shoulder taping on people with anterior shoulder pain. Dissertation. Houston, TX: Texas Women's University; 1999 [Google Scholar]
- 17. Halseth T, McChesney JW, DeBeliso M, et al. The effects of kinesio taping on proprioception at the ankle. J Sports Science Med. 2004; 3:1‐7 [PMC free article] [PubMed] [Google Scholar]
- 18. Ackermann B, Adams R, Marshall E. The effect of scapula taping on electromyographic activity and musical performance in professional violinists. Aust J Physiother. 2002; 48:197‐203 [DOI] [PubMed] [Google Scholar]
- 19. Alexander CM, Stynes S, Thomas A, et al. Does tape facilitate or inhibit the lower fibres of trapezius? Man Ther. 2003; 8:37‐41 [DOI] [PubMed] [Google Scholar]
- 20. Smith M, Sparkes V, Busse M, Enright S. Upper and lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009;10(2):45‐50 [DOI] [PubMed] [Google Scholar]
- 21. Lewis J, Green A, Wright C. Subacromial impingement syndrome: the role of posture and muscle imbalance. Journal of Shoulder and Elbow Surgery. 2005;14(4):385‐92 [DOI] [PubMed] [Google Scholar]
- 22. Thelen M, Dauber J, Stoneman P. The clinical efficacy of kinesio tape for shoulder pain: A randomized, double‐blinded, clinical trial. J Orthop Sports Phys Ther. 2008;38(7):389‐95 [DOI] [PubMed] [Google Scholar]
- 23. Frazier S., Whitman J., Smith M. Utilization of kinesio tex tape in patients with shoulder pain or dysfunction: a case series. Advanced Healing. 2006; 18‐20 [Google Scholar]
- 24. Pappas GP, Blemker SS, Beaulieu CF, et al. In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. J Shoulder Elbow Surg. 2006; 15:40‐49 [DOI] [PubMed] [Google Scholar]
- 25. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg. 2000; 9:299‐301 [DOI] [PubMed] [Google Scholar]
- 26. Ludewig P, Cook T. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000; 80(3):276‐291 [PubMed] [Google Scholar]
- 27. Silva L, Andreu J, Munoz P, et al. Accuracy of physical examination in subacromial impingement syndrome. Rheumatology. 2008; 47: 679‐683 [DOI] [PubMed] [Google Scholar]
- 28. Kase K, Wallis J, Kase T. Clinical Therapeutic Applications of the Kinesio Taping Method. Tokyo, Japan: Ken Ikai Co Ltd; 2003 [Google Scholar]
- 29. Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clin Rheumatol. 2011; 30: 201‐207 [DOI] [PubMed] [Google Scholar]
- 30. Hsu Y, Chen W, Lin H, et al. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. J Electromyogr Kinesiol. 2009;19(6): 1092‐1099 [DOI] [PubMed] [Google Scholar]
- 31. Hawker GA, Mian S, Kendzerska T, French M. Measures of Adult Pain. Arthritis Care & Research. 2011; 63: S240–S252 [DOI] [PubMed] [Google Scholar]
- 32. Thelen M, Dauber J, Stoneman P. The clinical efficacy of kinesio tape for shoulder pain: A randomized, double‐blinded, clinical trial. J Orthop Sports Phys Ther. 2008; 38(7): 389‐395 [DOI] [PubMed] [Google Scholar]
- 33. Kolber MJ, Fuller C, Marshall J, Wright A, Hanney WJ. The reliability and concurrent validity of scapular plane shoulder elevation measurements using a digital inclinometer and goniometer. Physiother Theory Pract. 2012:28: 161‐168 [DOI] [PubMed] [Google Scholar]
- 34. Miller P, Osmotherly P. Does scapula taping facilitate recovery for shoulder impingement symptoms? A pilot Randomized Controlled Trial. J Man Manipulative Ther. 2009; 17(1):E6‐E13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Crossley KM, Marino GP, Macilquham MD, et al. Can patellar tape reduce the patellar malalignment and pain associated with patellofemoral osteoarthritis? Arthritis Rheum. 2009; 61:1719‐25 [DOI] [PubMed] [Google Scholar]
- 36. Lan TY, Lin WP, Jiang CC, et al. Immediate effect and predictors of effectiveness of taping for patellofemoral pain syndrome: a prospective cohort study. Am J Sports Med. 2010; 38: 1626‐1630 [DOI] [PubMed] [Google Scholar]
- 37. Gonzalez‐Iglesias J, Fernendez‐de‐Lad‐Penas C, Cleland J, et al. Short‐term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: A randomized clinical trial. J Orthop Sports Phys Ther. 2009; 39:515‐521 [DOI] [PubMed] [Google Scholar]
- 38. Nederhand, Marc J., et al. Cervical muscle dysfunction in chronic whiplash‐associated disorder grade 2: the relevance of the trauma. Spine. 2002; 27:1056‐1061 [DOI] [PubMed] [Google Scholar]
- 39. McConnell J, Donnelly C, Hamner S, et al. Effect of shoulder taping on maximum shoulder external and internal rotation range in uninjured and previously injured overhead athletes during a seated throw. J Orthop Res. 2011; 29(9): 1406‐11 [DOI] [PubMed] [Google Scholar]
- 40. Lin J, Lim H, Soto‐quijano D, et al. Altered patterns of muscle activation during performance of four functional tasks in patients with shoulder disorders: interpretation from voluntary response index. J Electromyogr Kinesiol. 2006; 16(5):458‐468 [DOI] [PubMed] [Google Scholar]
- 41. Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004; 8(4):283‐91 [DOI] [PubMed] [Google Scholar]
- 42. Ostelo RWJG, de Vet HCW. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005; 19(4), 593‐607 [DOI] [PubMed] [Google Scholar]