Abstract
Background and Purpose:
Bony avulsion of the pectoralis major muscle is a rare but potentially devastating injury for athletes. Pectoralis major rupture typically occurs in 20 to 39 year‐old males. The shoulder region is one of the most frequently injured areas in Judo athletes. The purpose of this case report is to describe diagnosis and treatment following a pectoralis major bony avulsion due to an atypical mechanism of injury in a young Judo athlete.
Case Description:
A 19‐year‐old military cadet and competitive judo athlete reported to a direct‐access sports physical therapy clinic 7 weeks after incurring a shoulder injury during a judo match. He complained of shoulder pain and weakness with the inability to perform pushups. He presented with horizontal adduction weakness and visible discontinuity of the pectoralis muscle with resisted adduction.
Outcomes:
Radiographs demonstrated a bony avulsion of the pectoralis major from its humeral attachment. The patient underwent surgical repair of the lesion the next week and was able to resume most military cadet activities within 5 months post‐operation.
Discussion:
Bony avulsions are exceptionally rare injuries, and are even more uncommon in athletes under the age of 20. It is important for clinicians to perform a thorough history and physical examination in order to avoid missing this diagnosis. Surgery is likely the best option for a young athletic population; while conservative management may be optimal for the older, inactive population.
Level of Evidence:
4
Keywords: Athlete, avulsion, martial arts, pectoralis major, rupture
BACKGROUND AND PURPOSE
Pectoralis major (PM) avulsions are rare but potentially devastating injuries for athletes with the potential to cause significant weakness as well as cosmetic defects. Mild strains and partial tears of the PM are relatively common and often result in favorable outcomes following conservative treatment.1,2 Bony avulsion of the PM, however, is uncommon with very few published cases between 1822‐2010.1,2
The PM is a unique, triangular‐shaped muscle with many attachment sites allowing function throughout a wide variety of motions. The PM is described as having two “heads”, a clavicular head and a sternal head.3 The clavicular portion of the muscle originates from the medial aspect of the clavicle and the sternal portion from the sternum and cartilage of the first six ribs.3 The two heads insert via a single tendon on the lateral lip of the bicipital groove; the muscle fibers twist on each other so that the lowest part of the muscle fibers insert highest on the humerus.4 The PM functions as an adductor, flexor, and internal rotator of the humerus, contributing to nearly every upper extremity activity.3,4
PM rupture typically occurs in 20 to 39 year‐old males.2,5‐8 It is most commonly ruptured during weightlifting activities, specifically the bench press.1,2 Wrestling is the second most common mechanism of injury followed by a small number of cases reported in various other sports, such as rappelling, parachuting, ice hockey, skating, and soccer.2,5,7‐9 The use of anabolic steroids can be a contributing factor to an increased incidence of PM rupture.8 De Castro Ponchini and colleagues reported that 16 out of 20 individuals with PM ruptures in their study were taking steroids.7
Rupture can occur at various sites in the muscle but is typically grouped into 3 categories: muscle origin or belly injuries, musculotendinous junction and tendon insertion injuries, and bony avulsion at the humerus.2 PM rupture at the musculotendinous junction or tendon insertion at the humerus is by far the most common site reported.2,5 A systematic review of PM injuries reported that 245 out of the 365 published cases occurred at the musculotendinous junction, with only 5 bony avulsions at the humerus.2 It is important to distinguish between bony avulsion and tendon avulsion as there have been many reports of avulsions in the literature referring specifically to tendon avulsions.9‐12
Judo is one of the most practiced sports in the world.13,14 It is a grappling style martial art with emphasis on dynamic throws and submissions (forcing the opponent to surrender using “joint lock” or “choke” hold positions). The nature of the sport can lead to significant injuries due to the high velocity of the maneuvers used. Sprain injuries are the most common type of judo injury, followed by contusions.15 The upper extremity is the most frequently injured region during judo competition, with the shoulder being one of the most commonly affected parts of the body.13,15‐17
Bony avulsions are very rare among PM ruptures, and it is even more uncommon for a complete PM rupture to occur in an individual under the age of 20 with few cases reported in the literature.18,19 To the authors' knowledge, there are no previously reported cases of PM bony avulsion injuries in martial arts athletes. The purpose of this case report is to describe diagnosis and treatment following a PM bony avulsion due to an atypical mechanism of injury in a young Judo athlete.
CASE DESCRIPTION
Patient History
The patient was a 19‐year‐old male Judo athlete and cadet at the United States Military Academy, who presented to the direct‐access physical therapy clinic during “walk‐in” hours with left shoulder pain and weakness. The athlete described having injured his shoulder 7 weeks prior during a judo competition. He reported the mechanism of injury (MOI) occurred while he was prone, with his opponent pulling his left arm up and back into shoulder horizontal abduction. He was able to maneuver out of the position and finish the match, which lasted approximately three additional minutes. Immediately following the match, he was evaluated by the physician covering the competition and was told his injury was likely a muscle strain, and given instructions to use ice and rest his shoulder.
His primary complaint upon presentation to the physical therapist (PT) at the initial evaluation (nearly two months following the injury), was pain with reaching forward for objects (shoulder flexion) and weakness with pressing activities, including the inability to perform a pushup over the past 7 weeks. During the subjective evaluation, he also indicated that ecchymosis had developed in the biceps region within a day following the initial injury. He denied previous injury to the shoulder or use of supplements or anabolic steroids. His past medical history included a left elbow open reduction internal fixation (ORIF) in 2007 following a dislocation injury, which he had fully recovered from. The patient was otherwise healthy without significant past medical history.
CLINICAL IMPRESSION #1
Due to the reported MOI, history of ecchymosis in the biceps region, and difficulty with pressing activities; the initial concern was for a strain injury of the pectoralis or biceps muscles. The differential diagnoses included: biceps strain, pectoralis strain, rotator cuff tear, acromioclavicular sprain, and intercostal muscle strain. The plan for evaluation included active range of motion (AROM), manual muscle testing (MMT), a thorough palpation exam, as well as special testing of the shoulder complex.
EXAMINATION
During the initial examination, the patient reported his resting pain as 0/10 and pain during reaching activities as 6/10 on a numerical pain rating scale (NPRS), with “0” being pain free and “10” being the worst pain imaginable. He completed several self‐reported outcome measures, including the Shoulder Pain and Disability Index (SPADI), the Single Assessment Numeric Evaluation (SANE) and a Patient Specific Functional Scale (PSFS). The SPADI is a reliable tool for assessing outcomes in the shoulder,20,21 and the SANE has been validated for multiple conditions.22 The PSFS provides meaningful information regarding activities specific to individual patients, which may not be captured by other measures. The PSFS is used for all injuries in the author's facility and has been validated for various injuries.23‐25 The global rating of change (GROC) was also used to track the patient's opinion of his symptoms over time. GROC has been found useful when utilized in conjunctin with another outcome measure that assesses baseline status.26,27 This patient's initial, 4 month, and 9 month outcomes scores are presented in Table 1. The PSFS activities were self‐selected by the patient and are reflective of activities (boxing, for example) which may not be typical for judo athletes, but are required of male cadets at the academy.
Table 1.
Outcome Measures from Initial Evaluation. (A) Patient specific functional scale with activity breakdown. (B) Other outcome measures collected at initial evaluation included shoulder specific functional scale (SPADI), numerical pain rating scale (NPRS) and single assessment numerical evaluation (SANE).
| Patient Specific Functional Scale | ||||
|---|---|---|---|---|
| (A) | Activity | Score (initial/pre‐op) | Score (4 months post‐op) | Score (9 months post‐op) |
| Pushups | 0 | 0* | 10 | |
| Boxing | 3 | 0* | 10 | |
| Lifting | 3 | 10 | 10 | |
| Judo | ‐ | 0* | 10 | |
| Average Score (mdc = 2) | 2 | 2.5 | 10 | |
| (B) | Outcome Measure | Score (initial/pre‐op) | Score (4 months post‐op) | Score (9 months post‐op) |
| SPADI (MDC=18) | 44% (57/130) | 0% (0/130) | 0% (0/130) | |
| NPRS(MDO3) | 6 | 0 | 0 | |
| SANE | 70% | 100% | 100% | |
| GR0C(MCID = 2) | NA | +7 | +7 | |
Patient had not attempted activity yet due to protocol
MDC: Minimal Detectable Change
MOD: Minimum Cli lically Important Difference
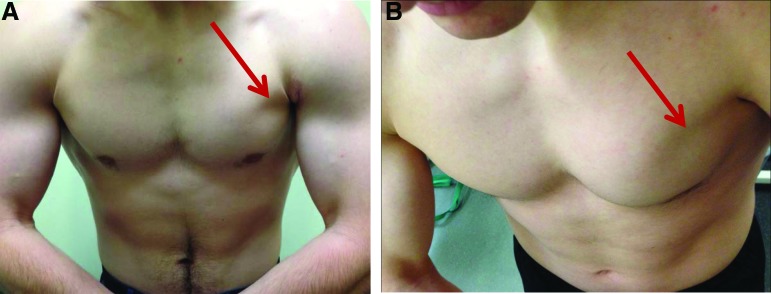
The initial physical examination included AROM and MMT in flexion, abduction, external rotation, and internal rotation; all results were within functional limits and equal bilaterally.28 Horizontal adduction strength was graded as a 4/5 with pain produced at the anterior aspect of the shoulder.28 The patient was tender to palpation over the axillary fold and exquisitely tender over the bicipital groove. When asked to press his palms together in front of his body (resisted horizontal adduction) to elicit a pectoralis major contraction, an obvious visible discontinuity of the pectoralis muscle in the left axillary fold was revealed (Figure 1).
Figure 1.
The patient was asked to press his palms together to contract the pectoralis major muscles bilaterally. There is an indentation at the left axillary fold (arrow) when compared to the right side (A), indicating a pectoralis major rupture. The indentation is more apparent from a superior angle (B).
CLINICAL IMPRESSION #2
Due to the reported mechanism, the patient's symptoms, and the axillary fold deformity during muscle contraction, the PT concluded that the injury was consistent with a pectoralis major rupture. Consistent with the American College of Radiology Appropriateness Criteria regarding shoulder injuries,29 the therapist ordered shoulder radiographs (AP, Axillary‐Y view, and Internal/External rotation). The Axillary‐Y image revealed a pectoralis major bony avulsion from the humeral insertion (Figure 2).
Figure 2.
In the axillary, or Y‐view, radiographic image of the left shoulder there is a large bony avulsion fragment anterior to the glenohumeral joint, measuring 15.6 3 7.2 mm.
INTERVENTION
The patient was referred to an orthopedic surgeon for further evaluation and surgical consideration due to the nature of the injury. Advanced imaging was determined unnecessary by the orthopedic surgeon, as physical exam and radiographs demonstrated conclusive evidence of the injury, and the patient was scheduled for surgical repair of the avulsion.
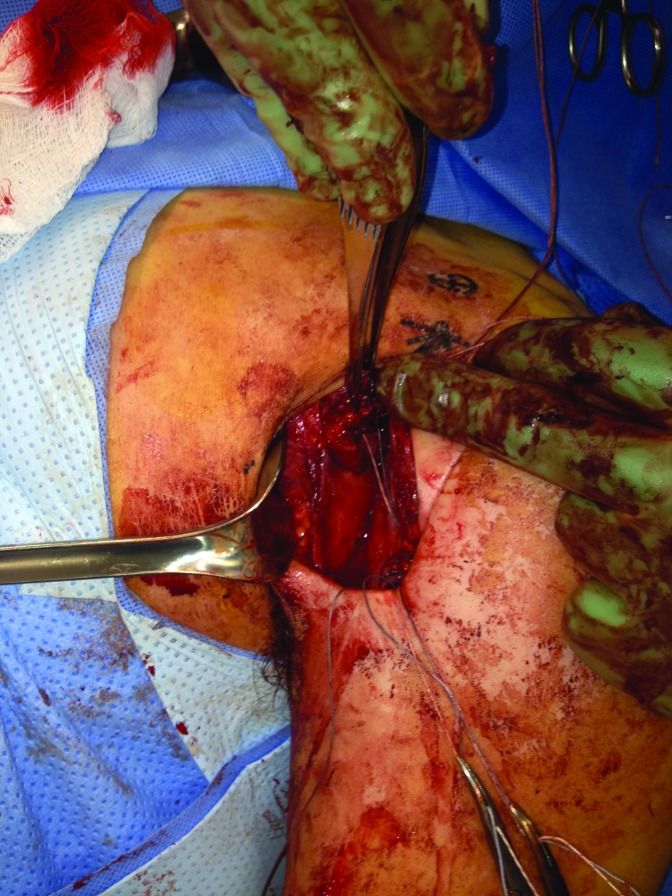
Surgical repair was performed 6 days following the initial PT evaluation (8 weeks after initial injury). The procedure was performed similar to the “preferred technique” described by Petilon and colleagues.1 A 5 cm longitudinal incision was made along the delto‐pectoral interval, allowing for easy identification of the tendon stump and bony fragments. The tendon and muscle belly were mobilized and running, locking stitches were placed along the tendon stump. The surgeon used a burr to create a trough at the anatomic site of the pectoralis major insertion,30 then two drill holes were placed into the trough and metal suture buttons with sutures were inserted and flipped in the medullary canal. Using the free suture ends the surgeon was able to reduce the tendon into the trough. Once the sutures were tied and the repair was tested through a range of motion, the skin was closed in layers and the arm placed into a sling (Figure 3).
Figure 3.
Open pectoralis major tendon repair with sutures placed in the tendon stump and finger pointing to the small bony fragment.
REHABILITATION
Post‐operative rehabilitation following PM tendon repair can vary somewhat, depending on patient‐specific surgical considerations.31 Patients are typically immobilized in a sling for 4 to 6 weeks.1,32 It is important for the treating therapist to communicate with the surgeon, as the duration of immobilization often depends on the amount of mobilization and tension required to achieve fixation during the surgical repair.1 Patients can be expected to regain full AROM within 3 months and progress strengthening exercises to be able to perform push‐ups by 6 months.1 Graduated post‐operative rehabilitation, as described by Manske and Prohaska, facilitates safe and effective return to activity.31 An example of the post‐operative progression used in this case is presented in Appendix 1.
The patient was immobilized in a sling and rehabilitation was initiated immediately after surgery. Before discharge from the hospital the patient was instructed in pendulums and active‐assisted range of motion. The surgeon and therapist communicated regarding the stability of the repair and it was determined that early mobilization should be encouraged. At 2 weeks post‐operation the patient was allowed to take off the sling in safe environments (in his room) and begin gentle isometric exercises for the rotator cuff muscles. Within 4 weeks post‐operation, sling use was completely discontinued. By 6 weeks post‐operation he had regained full AROM in all directions and began low resistance isotonic strength training. He was able to progress neuromuscular and strength exercises and return to running within 3 months. Pushups and bench press were avoided until after four months post‐operation and heavy resistance bench press was discouraged indefinitely.
OUTCOMES
At four months post‐operation the patient reported doing very well with full, pain free AROM and 5/5 strength throughout all shoulder movements. For additional protection of the surgical repair, he was allowed to return to judo practice at 6 months but not compete until 9 months post‐operation. Table 1 shows the increase in all of his outcome measure scores, which were rated as completely normal at 9 months post‐operation and all were above the clinically significant ranges by 9 months. At 4 months post‐operation the protocol didn't allow him to return to pushups, boxing, or judo. At 9 months post‐operation he had fully returned to all activities, including judo.
DISCUSSION
PM injuries typically occur from forced shoulder horizontal abduction and external rotation. They are most commonly seen in 20‐39 year‐old, male weightlifters. However, there are exceptional cases in which physical therapists and other medical providers must be aware of the signs and symptoms of a PM rupture. Diagnosis begins with a thorough history, including inquiry regarding the mechanism of injury. Swelling and ecchymosis will usually be present in the injured athlete's anterior humerus with initial signs between 3‐48 hours.8 The defect seen with a complete PM rupture will be present in the axillary fold with abduction or resisted adduction, however, significant swelling may mask the defect for up to 3 weeks.8 Pain and especially weakness with adduction and internal rotation motions are normally present.8
Upper extremity and shoulder related injuries are fairly common in judo athletes, yet the authors were unable to locate a single reported case of pectoralis muscle rupture or avulsion in this population. Since the most common mechanism of injury is related to bench press exercises, the patient was cautioned against heavy bench press resistance training indefinitely. To the authors knowledge there are no published studies describing the amount of tensile load a surgically repaired PM can tolerate.31 Some of the “joint lock” positions and high‐velocity dynamic throwing and takedown maneuvers in judo may indeed place significant strain on the repaired tissue, therefore the patient was advised to return to those activities no sooner than 9 months following surgery. The ultimate goal is to assist the patient in returning to their previous level of activity through a supervised, graduated rehabilitation program.31
This case is rare because not only is the athlete under the age of 20, his injury resulted in an atypical bony avulsion from a somewhat uncommon mechanism. Research has demonstrated that shoulder internal rotation of judo athletes in this age range is significantly higher compared to matched, healthy controls.17 Although skeletal maturity was not assessed in this particular patient, previous authors have suggested that the skeletally immature population may be more susceptible to bony avulsion since tendons and ligaments are stronger than bone in the skeletally immature.19 However, there are several reported cases of adults with bony avulsions.33
PM ruptures and avulsion have good reported outcomes with early surgical repair, but with delayed repair and conservative treatment the outcomes decrease respectively.5,6,18,34 Return of strength with immediate repair (within 2 weeks) has been reported between 99‐102%, reduced to 94% for chronic repairs, and between 56‐71% when treated conservatively relative to the contralateral side.34,35 The majority of published studies report improved strength gains after surgical repair compared to conservative treatment. Disregarding strength outcomes, some patients elect to have surgery merely for cosmetic reasons.
CONCLUSION
PM ruptures are uncommon and bony avulsions are extremely rare. It is important for clinicians to perform a thorough history and physical examination to avoid missing this diagnosis. Surgical outcomes appear to be time dependent and most studies report remarkably better results over conservative management. Surgery is likely the best option for young athletes, while conservative management may be optimal for the older, less active population.
Appendix 1
Rehabilitation Protocol Utilized Following Pectoralis Major Repair
| Phase | Goals | Therapeutic Exercises | Precautions |
|---|---|---|---|
| Phase 1 Protection (generally first 2‐6 weeks) |
|
|
|
| Phase 2a Motion (generally weeks 4‐8) |
|
|
|
| Phase 2b Motion Progression (generally weeks 6‐10) |
|
|
|
| Phase 3a Strength (week 9 up to 3 months) |
|
|
|
| Phase 3b Strength Progression (4 months to 8 months) |
|
|
|
| Phase 3c Strength Progression (6 months to 12 months) |
|
|
|
Abbreviations: Abduction (ABD), Flexion (FLEX), External Rotation (ER), Internal Rotation (IR), Passive Range of Motion (PROM), Active Range of Motion (AROM), Active Assisted Range of Motion (AAROM)
REFERENCES
- 1. Petilon J, Carr DR, Sekiya JK, et al. Pectoralis major muscle injuries: evaluation and management. J Am Acad Orthop Surg. 2005;13:59‐68 [DOI] [PubMed] [Google Scholar]
- 2. ElMaraghy AW, Devereaux MW. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg. 2012;21:412‐422 [DOI] [PubMed] [Google Scholar]
- 3. Fung L, Wong B, Ravichandiran K, et al. Three‐dimensional study of pectoralis major muscle and tendon architecture. Clin Anat. 2009;22:500‐508 [DOI] [PubMed] [Google Scholar]
- 4. Netter FH. Atlas of Human Anatomy. Fifth; Saunders Elsevier; 2010 [Google Scholar]
- 5. Bak K, Cameron EA, Henderson IJ. Rupture of the pectoralis major: a meta‐analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc. 2000;8:113‐119 [DOI] [PubMed] [Google Scholar]
- 6. Antosh IJ, Grassbaugh JA, Parada SA, et al. Pectoralis major tendon repairs in the active‐duty population. Am J Orthop (Belle Mead NJ). 2009;38:26‐30 [PubMed] [Google Scholar]
- 7. de Castro Pochini A, Ejnisman B, Andreoli CV, et al. Pectoralis major muscle rupture in athletes: a prospective study. Am J Sports Med. 2010;38:92‐98 [DOI] [PubMed] [Google Scholar]
- 8. Provencher MT, Handfield K, Boniquit NT, et al. Injuries to the pectoralis major muscle: diagnosis and management. Am J Sports Med. 2010;38:1693‐1705 [DOI] [PubMed] [Google Scholar]
- 9. Warme WJ, Whitaker DC. Pectoralis major tendon avulsion from rappelling. Mil Med. 2004. Feb;169(2):151‐4 2004; [DOI] [PubMed] [Google Scholar]
- 10. Mackenzie DB. Avulsion of the insertion of the pectoralis major muscle. A case report. S Afr Med J. 1981. Jul 25;60(4):147‐8 1981; [PubMed] [Google Scholar]
- 11. Liu J, Wu JJ, Chang CY, et al. Avulsion of the pectoralis major tendon. Am J Sports Med. 1992. May‐Jun;20(3):366‐8 1992; [DOI] [PubMed] [Google Scholar]
- 12. Egan TM, Hall H. Avulsion of the pectoralis major tendon in a weight lifter: repair using a barbed staple. Can J Surg. 1987. Nov;30(6):434‐5 1987; [PubMed] [Google Scholar]
- 13. Nishime RS. Martial arts sports medicine: current issues and competition event coverage. Curr Sports Med Rep. 2007;6:162‐169 [DOI] [PubMed] [Google Scholar]
- 14. Terry CM. The martial arts. Phys Med Rehabil Clin N Am. 2006;17:645‐676 [DOI] [PubMed] [Google Scholar]
- 15. Souza M, Monteiro H, Del Vecchio F, et al. Referring to judo's sports injuries in Sao Paulo State Championship. Science & Sports. 2006;21:280‐284 [Google Scholar]
- 16. Green CM, Petrou MJ, Fogarty‐Hover ML, et al. Injuries among judokas during competition. Scand J Med Sci Sports. 2007;17:205‐210 [DOI] [PubMed] [Google Scholar]
- 17. Ruivo R, Pezarat‐Correia P, Carita A. Elbow and shoulder muscles strength profile in judo athletes. Isokinetics and Exercise Science. 2012;20:41‐45 [Google Scholar]
- 18. Aarimaa V, Rantanen J, Heikkila J, et al. Rupture of the pectoralis major muscle. Am J Sports Med. 2004;32:1256‐1262 [DOI] [PubMed] [Google Scholar]
- 19. Simonian PT, Morris ME. Pectoralis tendon avulsion in the skeletally immature. Am J Orthop (Belle Mead NJ). 1996. Aug;25(8):563‐4 1996; [PubMed] [Google Scholar]
- 20. Bot SDM, Terwee CB, van der Windt DAWM, et al. Clinimetric evaluation of shoulder disability questionnaires: a systematic review of the literature. Annals of the Rheumatic Diseases. 2004;63:335‐341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009. May 15;61(5):623‐32. 10.1002/art.24396. 2009; [DOI] [PubMed] [Google Scholar]
- 22. Williams GN, Gangel TJ, Arciero RA, et al. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214‐221 [DOI] [PubMed] [Google Scholar]
- 23. Westaway MD, Stratford PW, Binkley JM. The patient‐specific functional scale: validation of its use in persons with neck dysfunction. J Orthop Sports Phys Ther. 1998;27:331‐338 [DOI] [PubMed] [Google Scholar]
- 24. Cleland JA, Fritz JM, Whitman JM, et al. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976). 2006;31:598‐602 [DOI] [PubMed] [Google Scholar]
- 25. Pengel LH, Refshauge KM, Maher CG. Responsiveness of pain, disability, and physical impairment outcomes in patients with low back pain. Spine (Phila Pa 1976). 2004;29:879‐883 [DOI] [PubMed] [Google Scholar]
- 26. Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989. Dec;10(4):407‐15 1989; [DOI] [PubMed] [Google Scholar]
- 27. Schmitt J, Di Fabio RP. The validity of prospective and retrospective global change criterion measures. Arch Phys Med Rehabil. 2005. Dec;86(12):2270‐6 2005; [DOI] [PubMed] [Google Scholar]
- 28. Kendall FP, McCreary EK, Provance PG, et al. Muscles: Testing and Function with Posture and Pain. 5th. Baltimore MD: Lippincott, Williams & Wilkins; 2005 [Google Scholar]
- 29. American College of Radiology ACR Appropriateness Criteria: acute shoulder pain. Available at: http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/AcuteShoulderPain.pdf Accessed 15 August 2013,
- 30. Carey P, Owens BD. Insertional footprint anatomy of the pectoralis major tendon. Orthopedics. 2010;33:23. [DOI] [PubMed] [Google Scholar]
- 31. Manske RC, Prohaska D. Pectoralis major tendon repair post surgical rehabilitation. N Am J Sports Phys Ther. 2007;2:22‐33 [PMC free article] [PubMed] [Google Scholar]
- 32. Merolla G, Paladini P, Campi F, et al. Pectoralis major tendon rupture. Surgical procedures review. Muscles Ligaments Tendons J. 2012;2:96‐103 [PMC free article] [PubMed] [Google Scholar]
- 33. Verfaillie SM, Claes T. Bony avulsion of the pectoralis major muscle. J Shoulder Elbow Surg. 1996. Jul‐Aug;5(4):327‐9 1996; [DOI] [PubMed] [Google Scholar]
- 34. Schepsis AA, Grafe MW, Jones HP, et al. Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med. 2000;28:9‐15 [DOI] [PubMed] [Google Scholar]
- 35. Hanna CM, Glenny AB, Stanley SN, et al. Pectoralis major tears: comparison of surgical and conservative treatment. Br J Sports Med. 2001;35:202‐206 [DOI] [PMC free article] [PubMed] [Google Scholar]