Abstract
Context:
Hydration has been shown to be an important factor in performance; however, the effects of mild dehydration during intense cycling are not clear.
Objective:
To determine the influence of mild dehydration on cycling performance during an outdoor climbing trial in the heat (ambient temperature = 29.0°C ± 2.2°C).
Design:
Crossover study.
Setting:
Outdoor.
Patients or Other Participants:
Ten well-trained, male endurance cyclists (age = 28 ± 5 years, height = 182 ± 0.4 cm, mass = 73 ± 4 kg, maximal oxygen uptake = 56 ± 9 mL·min−1·kg−1, body fat = 23% ± 2%, maximal power = 354 ± 48 W).
Intervention(s):
Participants completed 1 hour of steady-state cycling with or without drinking to achieve the desired pre-exercise hydration level before 5-km hill-climbing cycling. Participants started the 5-km ride either euhydrated (EUH) or dehydrated by −1% of body mass (DEH).
Main Outcome Measure(s):
Performance time, core temperature, sweat rate, sweat sensitivity, and rating of perceived exertion (RPE).
Results:
Participants completed the 5-km ride 5.8% faster in the EUH (16.6 ± 2.3 minutes) than DEH (17.6 ± 2.9 minutes) trial (t1 = 10.221, P = .001). Postexercise body mass was −1.4% ± 0.3% for the EUH trial and −2.2% ± 0.2% for the DEH trial (t1 = 191.384, P < .001). Core temperature after the climb was greater during the DEH (39.2°C ± 0.3°C) than EUH (38.8°C ± 0.2°C) trial (t1 = 8.04, P = .005). Sweat rate was lower during the DEH (0.44 ± 0.16 mg·m−2·s−1) than EUH (0.51 ± 0.16 mg·m−2·s−1) trial (t8 = 2.703, P = .03). Sweat sensitivity was lower during the DEH (72.6 ± 32 g·°C−1·min−1) than EUH (102.6 ± 54.2 g·°C−1·min−1) trial (t8 = 3.072, P = .02). Lastly, RPE after the exercise performance test was higher for the DEH (19.0 ± 1.0) than EUH (17.0 ± 1.0) participants (t9 = −3.36, P = .008).
Conclusions:
We found mild dehydration decreased cycling performance during a 5-km outdoor hill course, probably due to greater heat strain and greater perceived intensity.
Key Words: hypohydration, heat stress, hyperthermia, hydration status, exercise
Key Points
Euhydrated athletes were faster during a 5-km, outdoor, hill-climbing course.
Mild dehydration decreased physiologic function.
Dehydration hindered cyclists' ability to maintain cycling cadence.
Mild dehydration decreased cycling performance during a 5-km, outdoor, hill-climbing course, possibly due to thermoregulatory strain and perceived exertion.
Researchers have documented well that dehydration exceeding 2% of body mass reduces exercise performance1,2 and increases thermoregulatory strain, especially in the heat.3 Dehydration-induced hypovolemia leads to increased heart rate to maintain cardiac output.1 Dehydration also decreases blood flow in the skin and sweat rate and increases the risk of hyperthermia when exercise is performed in a hot environment. All these physiologic responses to dehydration lead to lower aerobic capacity and exercise performance.1,4
Greater levels of dehydration result in greater reductions in aerobic exercise performance. Investigators5 have demonstrated that levels of dehydration of −1%, −2%, −3%, and −4% of body mass are increasingly detrimental to cardiovascular and thermoregulatory function. Similarly, researchers6 have shown that dehydration at −2.5% of body mass reduces exercise time to exhaustion even in a temperate environment. In addition, Cheuvront et al7 reported that, when cyclists performed a fixed 30-minute cycling test in a temperate environment dehydrated (DEH) at −3% of body mass, their total work production was 8% lower than their performance in a euhydrated (EUH) state. In addition, Ebert et al8 studied the effect of dehydration on cycling performance during hill climbing in the heat. Dehydration was induced by a 2-hour submaximal exercise bout, with low (0.4 L) or high (2.4 L) fluid intake causing a −1.3% or −3.6% reduction, respectively, in body mass. After the 2-hour exercise bout, participants mounted their own bicycles and cycled on a treadmill set at an 8% grade and a speed of 88% of each maximal aerobic power output. Time to exhaustion was 5.6 minutes shorter when participants were dehydrated.
In a separate study,9 cyclists completed a performance test involving a fixed amount of work in a hot environment either EUH or with less than 2% dehydration. Time to completion was 6.5% (43 seconds) shorter in EUH participants (P < .05). The researchers suggested cyclists could self-select higher workloads while EUH, probably due to lower esophageal temperatures and ratings of perceived exertion (RPE).9 Nevertheless, some investigators have not shown a negative effect of modest dehydration (<−2% body mass) on 1-hour cycling performance in temperate environments.10,11 Interestingly, these researchers have tested cycling performance only in a laboratory setting through an exercise-to-exhaustion or constant time protocol, but no data are available for real outdoor conditions.
Investigators12,13 have documented well that a substantial percentage of athletes start training or competing when inadequately hydrated based on high urine specific gravity (USG) values. Although this technique cannot provide a precise level of dehydration, we believe that their degree of dehydration might be just below the threshold of thirst. Thirst usually is activated when body water deficit exceeds 1% of body mass.14 Therefore, we suspect that these hypohydrated athletes might be dehydrated by approximately −1% of their body mass.
Currently, few investigators have examined the effects of mild dehydration (1% of body mass loss) on cycling performance, so the physiologic responses during intense cycling remain unclear. Furthermore, no one has examined the effect of dehydration on cycling performance in outdoor conditions, especially when air flow over the skin is much higher in cycling than in a laboratory setting with a fan. Therefore, the purpose of our study was to determine the influence of mild dehydration (−1% of body mass) on cycling performance during outdoor hill climbing in the heat.
METHODS
Participants
Ten well-trained, heat-acclimated male cyclists (age = 28 ± 5 years, height = 182 ± 0.4 cm, mass = 73 ± 4 kg, maximal oxygen uptake = 56 ± 9 mL·min−1·kg−1, body fat = 23% ± 2%, maximal power [Powermax] = 354 ± 48 W) were recruited to participate in the study. Participants had competed in national cycling races for 8.4 ± 3.3 years. Eligibility criteria for participation in the study were a normal physical examination; no metabolic, cardiovascular, or renal disease; and no history of heat stroke. All participants provided written informed consent, and the protocol was approved by the Harokopio University Bioethics Committee.
Preliminary Testing
Body Composition
Anthropometric measurements were collected during the first visit to the laboratory. We measured body mass with a balance beam (model 770; Seca, Hamburg, Germany) and standing height with a wall-mounted stadiometer (model 700; Seca). Participants wore light clothing and no shoes, and measurements were recorded to the nearest 0.5 kg and 0.5 cm, respectively. Body composition was determined by dual-energy x-ray absorptiometry (model DPX; Lunar, Madison, WI).
Peak Oxygen Uptake Test
We determined peak oxygen uptake in a thermocomfortable environment (22°C) using an incremental-resistance exercise test on an automated, mechanically braked cycle ergometer (839 E; Monark Exercise AB, Vansbro, Sweden). After a 5-minute warm-up, participants cycled at 100 W for 1 minute, at which point cycling power increased by 20 W every minute until volitional exhaustion. During the test, expiratory gases were analyzed breath by breath via an online gas analyzer (VMax 229D; Sensormedics, Yorba Linda, CA). Three of the 4 following criteria were used to verify the attainment of peak oxygen uptake: (1) oxygen uptake plateau with increased workload, (2) respiratory exchange ratio greater than 1.1, (3) heart rate greater than 90% of predicted maximal value (220 − age), and (4) RPE15 greater than 17.
Experimental Protocol
All participants performed in counterbalanced mode a 5-km hill-climbing cycling trial at maximal effort EUH or DEH at −1% of body mass on 2 separate occasions in the summer. Trials were separated by at least 1 week but not more than 2 weeks. The participants were instructed to abstain from alcohol, caffeine, and training for 24 hours before each trial; maintain the same training regime; and abstain from racing between the 2 experimental trials. To avoid diurnal variations, the exercise trials were performed individually in the morning at the same time of day on both visits.16 To achieve the desired pre-exercise hydration state, participants exercised on a cycle ergometer (CompuTrainer Lab; RacerMate Inc, Seattle, WA) with or without water intake. During the previous day of each trial, all participants were given oral and written instructions to consume the same diet and drink plenty of fluids to ensure their optimal hydration state before the trial. To minimize differences in starting muscle glycogen concentrations, participants were instructed to record their diets 24 hours before their first visit. Their diet records were copied and returned to them with instructions to follow the same diet before each subsequent visit. For each testing day, first morning urine samples were collected and analyzed for proper hydration (USG < 1.026).17 Each participant's second trial was scheduled only when the predicted environmental conditions were ±2°C of the first trial.
Familiarization Session
On a separate visit, participants were familiarized with the experimental protocol and the cycling route. For this purpose, participants rode the ascending route as fast as possible while researchers recorded their average time performance and heart rate data. All participants had cycled this route many times because it is one of the most popular ascents for both training and competition. The starting point of the route was at an altitude of 271 m, and the finish was at an altitude of 591 m; the total altitude difference was 320 m, and the average grade was 6.4%.
Baseline Hydration State
The intensity of exercise was adjusted to elicit a heart rate of 70% to 75% of maximal heart rate (131 to 140 beats per minute) during cycling. Participants cycled indoors on their own bicycles mounted on the cycle ergometer in a warm environment (28.0°C ± 1.8°C). A fan was placed directly in front of the participants to provide airflow of 3.2 m/s. All participants performed 1 hour of exercise, which comprised 2 sets of 25 minutes of cycling followed by 5 minutes of rest after each set, with or without drinking to achieve the desired pre-exercise hydration status. During rest, the participants were towel dried, and their body mass was recorded while they were wearing only their cycling shorts. To achieve pre-exercise EUH, body mass loss was replenished by an equal amount of bottled water every 25 minutes. Similarly, at the end of the 1-hour exercise protocol in the DEH trial, total body mass loss was calculated. If dehydration exceeded 1%, we provided additional water to achieve the desired loss. For the experiment, Volvic (Danone, France) bottled water was used during both trials.
Performance Test
When the desired initial hydration state was achieved, blood and urine were collected immediately. Participants rested and then prepared for the performance test within 20 minutes. All cyclists wore cycling shoes with cleats and cycling clothes and used the same bicycle for both trials. Tires were pumped at 110 pounds per square inch, and bicycles were checked to ensure proper functioning for both trials. No use of a cycling computer was allowed. Ambient (Ta) and wet bulb globe temperature (WBGT) were measured by a handheld WBGT thermometer (WBGT-103; Kyoto Electronics Manufacturing Co, Ltd, Kyoto, Japan). During the EUH trial, Ta and WBGT at the starting point were 29.4°C ± 2.1°C and 24.6°C ± 2.1°C, respectively, whereas the temperatures at the finishing point were 28.0°C ± 2.5°C and 23.3°C ± 3.1°C, respectively (P > .05). During the DEH trial, the Ta and WBGT at the starting point were 30.1°C ± 1.0°C and 25.2°C ± 1.1°C, respectively, whereas the temperatures at the finishing point were 28.6°C ± 2.4°C and 24.1°C ± 2.3°C, respectively (P > .05). Wind speed data based on a local meteorological station were 0.9 ± 0.4 m/s for the EUH trial and 1.0 ± 0.6 m/s for the DEH trial (P > .05).
Thermoregulatory Measurements
Gastrointestinal temperature was recorded as a measure of core temperature (Tc). Participants were instructed to ingest a thermosensitive pill that was 20-mm long and had a diameter of 12 mm (HQ, Inc, Palmetto, FL) 8 to 10 hours before the test. We measured Tc before starting the baseline hydration state, immediately before each trial (pretrial), and immediately after each trial (posttrial). Next, the Tc was graphed against time,18 allowing computation of the area under the heating curve (ie, the integral °C/min). Total body sweat rate also was calculated from body mass changes adjusted for urine output.19 In addition, sweat sensitivity was calculated by dividing the sweat loss in grams by the area under the heating curve in degrees Celsius per minute.20
Cardiovascular Variables
Heart rate was recorded during both the dehydration protocol and the race trial via a wireless heart rate monitor (model T6c; Suunto, Vantaa, Finland).
Performance Variables
Wireless speed and cadence sensors were mounted on each bicycle to record distance, time, and cadence data. Data were recorded via the heart rate monitor mounted under the bicycle saddle so participants could not receive feedback. Upon completion of the trial, participants were instructed to rate their efforts using the RPE scale.15
Blood and Urine Samples
Samples were collected upon arrival, pretrial, and posttrial. All blood samples were drawn without stasis after participants sat for at least 20 minutes.21 From the whole blood, 1 mL was analyzed immediately for hematocrit and hemoglobin, whereas the remaining blood was transferred to a serum tube and a lithium heparin tube and both tubes were spun at 2000g for 10 minutes. Plasma and serum were refrigerated at −80°C for further analyses at a later time. Given that plasma osmolality (Osmp) was measured in previously frozen samples, only the changes from baseline are reported in the Results section.22 Urine volume, USG, and urine color were measured, and a urine sample was stored at −80°C for further analyses at a later time.
Blood and Urine Analyses
We measured USG and total plasma proteins using a refractometer (SUR-NE; Atago Co Ltd, Tokyo, Japan). The urine color was estimated immediately using the 8-level color scale described by Armstrong et al.23,24 We determined hematocrit in triplicate from whole blood using the microcapillary technique after centrifugation for 5 minutes at 9500g. We measured hemoglobin in duplicate from whole blood with the cyanmethemoglobin technique using a commercially available kit (Drabkin reagent; Sigma, St Louis, MO). Percentage change in plasma volume was calculated using the equation of Dill and Costill.25 Urine osmolality and Osmp were measured in duplicate via freezing-point depression (3D3 osmometer; Advanced Instruments Inc, Norwood, MA). Serum potassium and sodium concentrations were determined in duplicate (ILyte Na/K/Li Analyzer; Instrumentation Laboratory, Milan, Italy).
Statistical Analysis
Normality of the data was tested and explored graphically using percentile plots. All variables are presented as means ± standard deviations because they were normally distributed. Differences in the mean values or the distributions of variables among EUH and DEH, sweat rate, sweat sensitivity, and RPE were assessed using paired t tests. Generalized estimating equations were fitted to evaluate differences between the 2 experimental trials (EUH and DEH) and across time points. For the dependent variables (ie, performance test time, cycling cadence, Tc, heart rate, body mass, change in body mass, urine osmolality, USG, urine color, Osmp, serum potassium concentration, serum sodium concentration, total plasma proteins, and percentage change in plasma volume), the normal distribution was used for fitting generalized estimating equations with the identity as the link function. The unstructured formation of the correlation matrix was used after comparing various scenarios using the corresponding quasilikelihood under the independence criterion for the model's goodness of fit. Independent variables were time (baseline, pretrial, posttrial) and trial (EUH, DEH) or kilometers (1, 2, 3, 4, 5) and trial (EUH, DEH). First-order interactions between time and trial or between kilometers and trial also were applied. Post hoc analysis for comparing mean values between trials across time points, as well as at different time points, was applied by using the sequential Bonferroni correction rule to adjust for the inflation of type I error due to multiple comparisons. All statistical analyses were carried out with SPSS (version 19; IBM Corporation, Armonk, NY). The α level was set at equal to or less than .05.
RESULTS
Performance Test Time
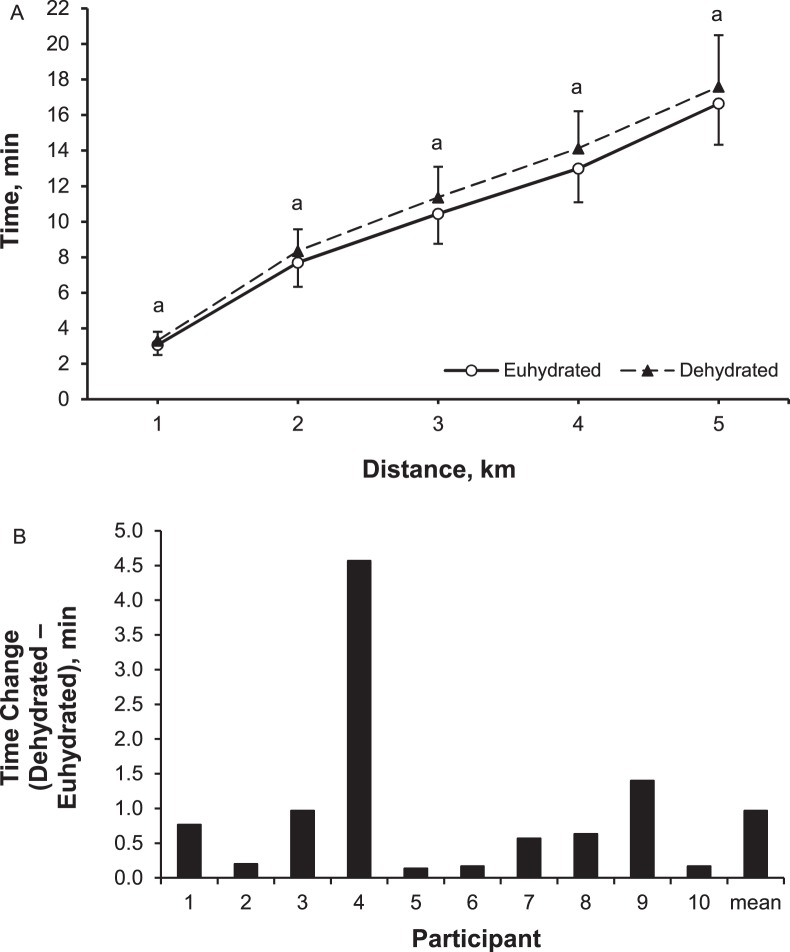
Participants completed the 5-km hill-climbing race 57 ± 80 seconds (5.8%, t1 = 10.221, P = .001) faster when EUH (16.6 ± 2.3 minutes) than when DEH (17.6 ± 2.9 minutes; Figure 1). This performance benefit was evident at 1, 2, 3, 4, and 5 km of the race (P < .05). All 10 participants performed better when EUH than DEH (Figure 1).
Figure 1. .
A, Elapsed time of each kilometer of the test (mean ± SD). B, Time change for each participant. a Indicates differences between trials at same time point (P ≤ .05).
Cycling Cadence
Cycling cadence was greater during the EUH (76 ± 8 revolutions per minute [rpm]) than DEH (70 ± 8 rpm) trial (t1 = 33.75, P < .001). Cadence was also greater during the EUH than DEH trial at 1 km (79 ± 12 rpm and 73 ± 11 rpm, respectively; P = .001), 2 km (66 ± 16 rpm and 63 ± 19 rpm, respectively; P = .003), 3 km (85 ± 8 rpm and 78 ± 8 rpm, respectively; P < .001), 4 km (76 ± 8 rpm and 71 ± 10 rpm, respectively; P = .006), and 5 km (73 ± 10 rpm and 66 ± 12 rpm, respectively; P = .02).
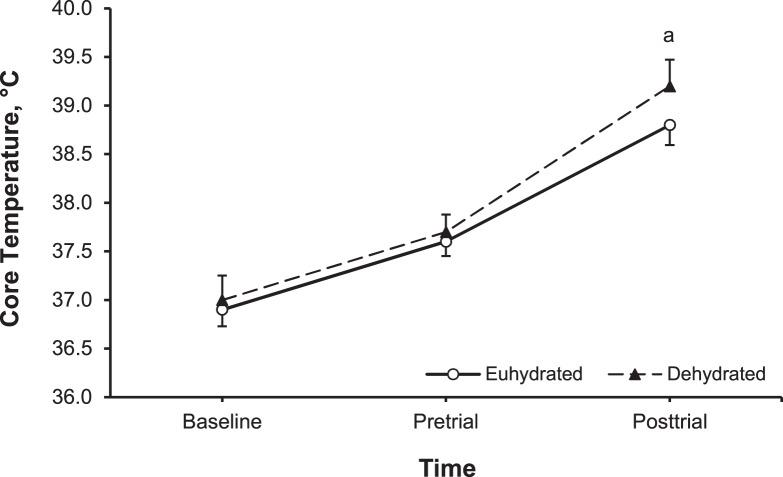
Core Temperature, Heart Rate, and RPE
Core temperature data at baseline, pretrial, and posttrial cycling test are depicted in Figure 2. Posttrial Tc was greater during the DEH (39.2°C ± 0.3°C) than EUH (38.8°C ± 0.2°C) trial, indicating a greater thermal load (t1 = 8.04, P = .005). Heart rate during the performance test trials was near maximal (93% ± 5%) and did not differ by hydration state (DEH = 179 ± 10 beats per minute, EUH = 176 ± 11 beats per minute; t1 = 3.033, P = .08). The RPE immediately after the hill climb was higher during DEH (19.0 ± 1.0) than EUH (17.0 ± 1.0) trial (t9 = −3.36, P = .008).
Figure 2. .
Core temperature at baseline and immediately before (pretrial) and immediately after (posttrial) the 5-km performance test (Mean ± SD). a Indicates differences between trials at same time point (P ≤ .05).
Body Mass, Sweat Rate, and Sweat Sensitivity Changes
For the DEH trial, participants started the hill-climbing cycling test with a water deficit of −0.7 ± 0.1 kg (−1.0% ± 01% body mass), whereas for the EUH trial, they started without a water deficit. As a response to exercise, participants in the EUH and DEH trials lost −1.0 ± 0.3 kg (−1.4% ± 0.3% body mass) and −1.6 ± 0.3 kg (−2.2% ± 0.2% body mass), respectively (t1 = 191.384, P < .001; Table). Whole-body sweat rate during the 5-km hill climb was lower in DEH (0.44 ± 0.16 mg·m−2·s−1, 3.08 ± 1.10 L/h) than EUH (0.51 ± 0.16 mg·m−2·s−1, 3.53 ± 1.09 L/h) trial (t8 = 2.703, P = .03), although the exercise lasted longer. Sweat sensitivity was lower in the DEH (72.6 ± 32 g·°C−1·min−1) than EUH (102.6 ± 54.2 g·°C−1·min−1) trial (t8 = 3.072, P = .02; Figure 3).
Table.
Blood and Urine Variables During the Experiment (Mean ± SD)
| Group |
||||||
| Euhydrated |
Dehydrated |
|||||
| Baseline |
Immediately Pretrial |
Immediately Posttrial |
Baseline |
Immediately Pretrial |
Immediately Posttrial |
|
| Body mass, kg | 73.0 ± 4.0 | 73.0 ± 4.0 | 72.0 ± 4.0 | 73.1 ± 3.8 | 72.4 ± 3.8 | 71.5 ± 3.8 |
| Change in body mass, kg | NA | 0 | −1.0 ± 0.3 | NA | −0.7 ± 0.1a | −1.6 ± 0.3a |
| Change in body mass, % | NA | 0 | −1.4 ± 0.3 | NA | −1.0 ± 0.1a | −2.2 ± 0.2a |
| Urine osmolality, mOsm/kg | 597 ± 129 | 634 ± 102 | 757 ± 91 | 507 ± 132 | 676 ± 52 | 792 ± 56 |
| Urine specific gravity, g/mL | 1.018 ± 0.005 | 1.016 ± 0.005 | 1.021 ± 0.004 | 1.013 ± 0.006 | 1.016 ± 0.004 | 1.023 ± 0.004 |
| Urine color | 4 ± 1 | 4 ± 1 | 6 ± 1 | 4 ± 1 | 4 ± 1 | 6 ± 1 |
| Change in plasma osmolality from baseline, mOsm/kg | NA | 1.2 ± 2.4 | 6.8 ± 2.7 | NA | 6.6 ± 2.7a | 13.2 ± 3.7a |
| Serum sodium, mmol/L | 142.7 ± 1.2 | 146.3 ± 3.9 | 146.9 ± 3.3 | 143.5 ± 2.9 | 145.5 ± 1.9 | 147.0 ± 1.8 |
| Serum potassium, mmol/L | 4.0 ± 0.2 | 4.4 ± 0.2 | 4.1 ± 0.3 | 4.2 ± 0.2 | 4.3 ± 0.2 | 4.2 ± 0.2 |
| Total plasma proteins, g/L | 66 ± 4 | 67 ± 4 | 69 ± 6 | 64 ± 4 | 64 ± 10 | 65 ± 9 |
| Change in plasma volume, % | NA | −0.1 ± 0.3 | −4.1 ± 1.2 | NA | −2.3 ± 0.7a | −5.7 ± 2.1a |
Abbreviation: NA, not available.
Indicates difference between hydrated and dehydrated trials at the corresponding time points (P < .05).
Figure 3. .
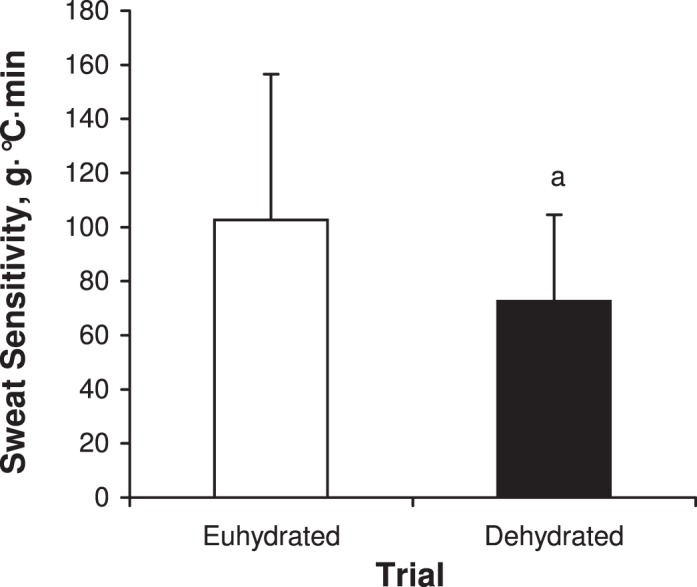
Sweat sensitivity for the 2 experimental trials (mean ± SD). a Indicates differences between trials at same time point (P ≤ .05).
DISCUSSION
We examined the effect of mild dehydration (−1% of body mass) on an outdoor 5-km hill-climbing cycling ride in the heat. The data indicated that even a mild degree of dehydration could detrimentally affect cycling performance during hill cycling, probably due to greater thermal stress. We found that, by the end of the race, Tc was greater in the DEH than EUH trial. We expected EUH athletes to have higher Tc due to greater exercise intensity, as supported by the literature.26,27 To the contrary, Tc was lower in the EUH than DEH trial, probably due to a greater sweating response.
In this regard, Walsh et al,28 who examined the performance of cyclists at 32°C, found that the time to exhaustion at 90% of maximal oxygen uptake was decreased by 31% when participants started cycling dehydrated by −1.8%. Below et al9 also showed that, when cyclists were dehydrated by less than −2%, their exercise performance was 6.5% lower. Similarly, Casa et al29 found that Tc was 0.22°C greater for every 1% of body mass lost during the DEH trial than the hydrated trial. Exercise intensity causes a rise in body Tc,26 especially in a hot environment. However, dehydration can play a modulating role in the extent of exercise-induced hyperthermia.5 Sweat sensitivity has been used as an index of thermoregulatory efficiency because it represents sweating as a response to a rise in Tc. Our data indicated that even −1% dehydration induces lower sweat sensitivity.
Armstrong et al20 examined the thermoregulatory responses during fixed 90-minute treadmill walking in the heat when participants were EUH or DEH with or without ad libitum water intake during exercise. Both sweating and sweat sensitivity were reduced in the hypohydrated trial (−3.9% body mass) when participants did not drink fluids during exercise, showing that dehydration modulates thermoregulatory responses. Armstrong et al20 also found that lower sweat sensitivity was associated with lower body mass and greater Osmp.
In our study, heart rate response during the 5-km cycling test did not differ between the EUH and DEH trials. Maybe the high intensity of the exercise induced near-maximal heart rate in both trials. Although we did not measure cardiac output during exercise, we speculate that both stroke volume and cardiac output might have been compromised as a response to dehydration. This response has been well documented with a greater degree of dehydration by others.1
The cycling cadence of our participants in each single kilometer of the performance trial was higher in the EUH than DEH condition, suggesting that dehydration hinders a cyclist's ability to maintain cycling cadence. We also found RPE was lower at the end of the EUH than DEH trial. We speculate that the combined effect of dehydration and hyperthermia influenced participants' perceptions of effort, possibly due to cardiovascular drift.1,30 All cyclists in our study had better performance during the EUH than DEH trial even though the lower body mass could have provided a potential performance benefit (ie, greater power-to-mass ratio) in the hill-climbing cycling course. In summary, our main finding was that mild dehydration decreased hill-climbing cycling performance via increased thermoregulatory strain and RPE.
ACKNOWLEDGMENTS
The study was supported by the Department of Nutrition and Dietetics Graduate Program, Harokopio University, Athens, Greece. We thank Ms Katerina Spagi for her technical support during data collection.
REFERENCES
- 1.Gonzalez-Alonso J, Mora-Rodriguez R, Below PR, Coyle EF. Dehydration markedly impairs cardiovascular function in hyperthermic endurance athletes during exercise. J Appl Physiol. 1997;82(4):1229–1236. doi: 10.1152/jappl.1997.82.4.1229. [DOI] [PubMed] [Google Scholar]
- 2.American College of Sports Medicine. Sawka MN, Burke LM, et al. American College of Sports Medicine position stand: exercise and fluid replacement. Med Sci Sports Exerc. 2007;39(2):377–390. doi: 10.1249/mss.0b013e31802ca597. [DOI] [PubMed] [Google Scholar]
- 3.Gonzalez-Alonso J, Mora-Rodriguez R, Below PR, Coyle EF. Dehydration reduces cardiac output and increases systemic and cutaneous vascular resistance during exercise. J Appl Physiol. 1995;79(5):1487–1496. doi: 10.1152/jappl.1995.79.5.1487. [DOI] [PubMed] [Google Scholar]
- 4.Nybo L, Jensen T, Nielsen B, Gonzalez-Alonso J. Effects of marked hyperthermia with and without dehydration on VO(2) kinetics during intense exercise. J Appl Physiol. 2001;90(3):1057–1064. doi: 10.1152/jappl.2001.90.3.1057. [DOI] [PubMed] [Google Scholar]
- 5.Montain SJ, Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol. 1992;73(4):1340–1350. doi: 10.1152/jappl.1992.73.4.1340. [DOI] [PubMed] [Google Scholar]
- 6.Nielsen B, Kubica R, Bonnesen A, Rasmussen IB, Stoklosa J, Wilk B. Physical work capacity after dehydration and hyperthermia: a comparison of the effect of exercise versus passive heating and sauna and diuretic dehydration. Scand J Sports Sci. 1981;3(1):2–10. [Google Scholar]
- 7.Cheuvront SN, Carter R, III, Castellani JW, Sawka MN. Hypohydration impairs endurance exercise performance in temperate but not cold air. J Appl Physiol. 2005;99(5):1972–1976. doi: 10.1152/japplphysiol.00329.2005. [DOI] [PubMed] [Google Scholar]
- 8.Ebert TR, Martin DT, Bullock N. Influence of hydration status on thermoregulation and cycling hill climbing. Med Sci Sports Exerc. 2007;39(2):323–329. doi: 10.1249/01.mss.0000247000.86847.de. [DOI] [PubMed] [Google Scholar]
- 9.Below PR, Mora-Rodriguez R, Gonzalez-Alonso J, Coyle EF. Fluid and carbohydrate ingestion independently improve performance during 1 h of intense exercise. Med Sci Sports Exerc. 1995;27(2):200–210. [PubMed] [Google Scholar]
- 10.McConell GK, Stephens TJ, Canny BJ. Fluid ingestion does not influence intense 1-h exercise performance in a mild environment. Med Sci Sports Exerc. 1999;31(3):386–392. doi: 10.1097/00005768-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Robinson TA, Hawley JA, Palmer GS. Water ingestion does not improve 1-h cycling performance in moderate ambient temperatures. Eur J Appl Physiol Occup Physiol. 1995;71(2–3):153–160. doi: 10.1007/BF00854973. [DOI] [PubMed] [Google Scholar]
- 12.Osterberg KL, Horswill CA, Baker LB. Pregame urine specific gravity and fluid intake by National Basketball Association players during competition. J Athl Train. 2009;44(1):53–57. doi: 10.4085/1062-6050-44.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stover EA, Petrie HJ, Passe D, Horwill CA, Murray B, Wildman R. Urine specific gravity in exercisers prior to physical training. Appl Physiol Nutr Metab. 2006;31(3):320–327. doi: 10.1139/h06-004. [DOI] [PubMed] [Google Scholar]
- 14.Anastasiou CA, Kavouras SA, Amaoutis G, et al. Sodium replacement and plasma sodium drop during exercise in the heat when fluid intake matches fluid loss. J Athl Train. 2009;44(2):117–123. doi: 10.4085/1062-6050-44.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 16.Atkinson G, Todd C, Reilly T, Waterhouse J. Diurnal variation in cycling performance: influence of warm-up. J Sports Sci. 2005;23(3):321–329. doi: 10.1080/02640410410001729919. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong LE, Pumerantz AC, Fiala KA, et al. Human hydration indices: acute and longitudinal reference values. Int J Sport Nutr Exerc Metab. 2010;20(2):145–153. doi: 10.1123/ijsnem.20.2.145. [DOI] [PubMed] [Google Scholar]
- 18.Takamata A, Mack GW, Gillen CM, Jozsi AC, Nadel ER. Osmoregulatory modulation of thermal sweating in humans: reflex effects of drinking. Am J Physiol. 1995;268(2 pt 2):R414–R422. doi: 10.1152/ajpregu.1995.268.2.R414. [DOI] [PubMed] [Google Scholar]
- 19.Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known, 1916. Nutrition. 1989;5(5):303–313. [PubMed] [Google Scholar]
- 20.Armstrong LE, Maresh CM, Gabaree CV, et al. Thermal and circulatory responses during exercise: effects of hypohydration, dehydration, and water intake. J Appl Physiol. 1997;82(6):2028–2035. doi: 10.1152/jappl.1997.82.6.2028. [DOI] [PubMed] [Google Scholar]
- 21.Hagan RD, Diaz FJ, Horvath SM. Plasma volume changes with movement to supine and standing positions. J Appl Physiol. 1978;45(3):414–417. doi: 10.1152/jappl.1978.45.3.414. [DOI] [PubMed] [Google Scholar]
- 22.Seifarth CC, Miertschischk J, Hahn EG, Hensen J. Measurement of serum and plasma osmolality in healthy young humans: influence of time and storage conditions. Clin Chem Lab Med. 2004;42(8):927–932. doi: 10.1515/CCLM.2004.150. [DOI] [PubMed] [Google Scholar]
- 23.Armstrong LE, Soto JA, Hacker FT, Jr, Casa DJ, Kavouras SA, Maresh CM. Urinary indices during dehydration, exercise, and rehydration. Int J Sport Nutr. 1998;8(4):345–345. doi: 10.1123/ijsn.8.4.345. [DOI] [PubMed] [Google Scholar]
- 24.Kavouras SA. Assessing hydration status. Curr Opin Clin Nutr Metab Care. 2002;5(5):519–524. doi: 10.1097/00075197-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Dill DB, Costill DL. Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol. 1974;37(2):247–248. doi: 10.1152/jappl.1974.37.2.247. [DOI] [PubMed] [Google Scholar]
- 26.Maughan RJ, Leiper BJ, Thompson J. Rectal temperature after marathon running. Br J Sports Med. 1985;19(4):192–195. doi: 10.1136/bjsm.19.4.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saltin B, Hermansen L. Esophageal, rectal, and muscle temperature during exercise. J Appl Physiol. 1966;21(6):1757–1762. doi: 10.1152/jappl.1966.21.6.1757. [DOI] [PubMed] [Google Scholar]
- 28.Walsh RM, Noakes TD, Hawley JA, Dennis SC. Impaired high-intensity cycling performance time at low levels of dehydration. Int J Sports Med. 1994;15(7):392–398. doi: 10.1055/s-2007-1021076. [DOI] [PubMed] [Google Scholar]
- 29.Casa DJ, Stearns RL, Lopez RM, et al. Influence of hydration on physiological function and performance during trail running in the heat. J Athl Train. 2010;45(2):147–156. doi: 10.4085/1062-6050-45.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wingo JE, Ganio MS, Cureton KJ. Cardiovascular drift during heat stress: implications for exercise prescription. Exerc Sport Sci Rev. 2012;40(2):88–94. doi: 10.1097/JES.0b013e31824c43af. [DOI] [PubMed] [Google Scholar]