Abstract
Context:
A number of comprehensive injury-prevention programs have demonstrated injury risk-reduction effects but have had limited adoption across athletic settings. This may be due to program noncompliance, minimal exercise supervision, lack of exercise progression, and sport specificity. A soccer-specific program described as the F-MARC 11+ was developed by an expert group in association with the Federation Internationale de Football Association (FIFA) Medical Assessment and Research Centre (F-MARC) to require minimal equipment and implementation as part of regular soccer training. The F-MARC 11+ has been shown to reduce injury risk in youth female soccer players but has not been evaluated in an American male collegiate population.
Objective:
To investigate the effects of a soccer-specific warm-up program (F-MARC 11+) on lower extremity injury incidence in male collegiate soccer players.
Design:
Cohort study.
Setting:
One American collegiate soccer team followed for 2 seasons.
Patients or Other Participants:
Forty-one male collegiate athletes aged 18–25 years.
Intervention(s):
The F-MARC 11+ program is a comprehensive warm-up program targeting muscular strength, body kinesthetic awareness, and neuromuscular control during static and dynamic movements. Training sessions and program progression were monitored by a certified athletic trainer.
Main Outcome Measure(s):
Lower extremity injury risk and time lost to lower extremity injury.
Results:
The injury rate in the referent season was 8.1 injuries per 1000 exposures with 291 days lost and 2.2 injuries per 1000 exposures and 52 days lost in the intervention season. The intervention season had reductions in the relative risk (RR) of lower extremity injury of 72% (RR = 0.28, 95% confidence interval = 0.09, 0.85) and time lost to lower extremity injury (P < .01).
Conclusions:
This F-MARC 11+ program reduced overall risk and severity of lower extremity injury compared with controls in collegiate-aged male soccer athletes.
Key Words: injury prevention, sport injuries, athletic trainers
Key Points
The F-MARC 11+ reduced the risk of lower extremity injuries in youth female soccer players, but limited evidence for its effectiveness exists in males and at the collegiate level.
A traditional warm-up did not prevent injury as effectively as the F-MARC 11+ program, despite taking the same amount of time.
When supervised by an athletic trainer, the F-MARC 11+ prevented injuries in collegiate male soccer players.
An athletic trainer administered intervention, reduced injury risk, and improved program compliance, progression, and execution.
Soccer is among the most popular sports in the world, boasting more than 265 million1 youth and amateur players and more than 37 000 American collegiate players.2 Soccer participation has continued to increase over the past decade worldwide and especially in the United States National Collegiate Athletic Association (NCAA).2 Lower extremity injury rates for male NCAA soccer athletes have remained relativity stable over the past decade (practice versus game: 8 versus 12.18 per 1000 exposures).2 Junge and Dvorak,3 in a systematic review of soccer injuries in international male players, reported 10 to 35 injuries per 1000 hours of match play and 2 to 7 per 1000 hours of training in international male soccer players. In cohorts of international, elite-level soccer athletes, the injury rate was high (1.3 injuries per player per season); most injuries affected the lower extremity (87%) and resulted from noncontact mechanisms (58%).4 The most common injury in male collegiate soccer players was ankle sprains (3.19 per 1000 exposures), followed by thigh muscle strains and knee sprains at 2.28 and 2.07 per 1000 exposures, respectively.2 These findings are consistent with reports of international-level soccer athletes.4 These lower extremity injuries have substantial short-term consequences, such as loss of participation, and the potential for long-term consequences, such as decreased physical activity5 and increased risk of osteoarthritis.5–10 Nearly 20% of all soccer injuries were severe, requiring greater than 10 days of time lost from activity.2 Knee ligament ruptures and leg fractures accounted for 35% of these injuries, many of which required surgical intervention and prolonged rehabilitative care; these patients also had a greatly increased risk of a secondary injury when they returned to soccer competition.2,11
The high injury rate in soccer players has persisted despite scientific advances in injury etiology,12–17 screening techniques, and the identification of athletes who may be at greater risk.18–25 Although injury-prevention programs have successfully decreased lower extremity injuries such as ankle sprains,24,26–29 anterior cruciate ligament (ACL) injuries,18,30,31 and hamstrings strains,20,24,29,32–34 they have not yet been widely adopted,35 limiting their potential effects in soccer athletes.36
Although numerous training programs have been designed to prevent injury,3,24,26,29,31,32,37–55 few incorporate sport-specific components.37,38,41,42,56,57 Many of these programs have shown promising results in decreasing the risk of injury.18,37,38,41,58 However, extensive time, expert personnel, and special equipment are needed for these programs to be effective. To make injury-prevention programs as widely accessible as possible, the F-MARC 11+ program was developed by the Federation International de Football Association (FIFA) Medical Assessment and Research Center (F-MARC).59 This program can be completed in a short time frame, takes minimal training to implement, and requires only a soccer ball, making it an attractive alternative for sport coaches, strength and conditioning professionals, and rehabilitation specialists already working with limited time and budgets. Thus far, 4 studies37,38,41,60 have reported on the use of a version of the F-MARC 11+ program in adolescent males and females, with injury reductions ranging from 21% to 71%. In Norwegian handball players, similar training programs have produced a 49% reduction in injury risk40 and 94% reduction in ACL injury risk.39
To our knowledge, the F-MARC 11+ has yet to be investigated for effectiveness in injury risk reduction in an American male collegiate soccer population. Therefore, our aim was to examine the effect of a sport-specific program implemented with athletic trainer supervision to track compliance, injury occurrence, and program performance quality. We hypothesized that the comprehensive, exercise-based soccer warm-up program (the F-MARC 11+) would be more effective than the traditional dynamic warm-up in preventing lower extremity injuries in male NCAA Division III collegiate soccer athletes.
METHODS
We used a prospective single-cohort study design to determine the potential effect of the program on injury risk. We obtained approval from the College of Mount Saint Joseph institutional review board before the study began. The independent variable was season (preseason, competition season [2009 referent versus 2010 experimental]) and the dependent variable was injury rate per athlete-exposures (AEs in-season practice or game). Athlete-exposure was defined as any team practice or game during the in-season or preseason period. An injury was defined as a limitation in function that required medical attention and the loss of at least 1 day of activity (practice or game).61 A thigh muscle strain was clinically diagnosed with a decrease in strength (manual muscle testing) and pain in the affected musculature of the hamstrings, quadriceps, hip flexors, or adductors and was severe enough to require time loss from activity. Injuries were tracked, and days lost were recorded daily for each exposure. All injuries, practices, and games were monitored by the same athletic trainer to ensure accuracy and consistency in daily data reporting. If an injury was severe (grade 2 or higher muscle strain or joint sprain), the patient was referred to the team physician for further examination and imaging if necessary to confirm the diagnosis. Strain and sprain grading was completed at the time of injury based on previously reported guidelines of grade 1 (minor), grade 2 (moderate), and grade 3 (severe).62,63
A total of 41 NCAA Division III male collegiate soccer players from the same team volunteered to participate in a training intervention and injury-surveillance study for 2 seasons (see Table 1 for demographic information). The 2009 season players served as the monitored referent (control) group, whereas the 2010 players who received the training intervention throughout the entire season served as the experimental group. Thirty players participated in the 2009 season and 34 in the 2010 season. Seven of the 30 players from 2009 did not participate in 2010 (5 seniors graduated and 2 athletes transferred). Eleven freshmen or transfer players were added in 2010. Of the departing players in 2010, 2 had time-loss injuries: a foot stress injury with 16 days lost and hamstrings strain with 14 days lost (Figure).
Table 1. .
Group Demographicsa
| 2009 (n = 30) |
2010 (n = 34) |
Total (n = 41) |
P Value |
|
| Age, y | 20.3 ± 1.6 | 20.0 ± 2.4 | 20.1 ± 2.0 | .56 |
| Height, cm | 176.8 ± 6.2 | 177.8 ± 6.1 | 177.3 ± 6.1 | .55 |
| Mass, kg | 74.6 ± 10.9 | 72.8 ± 9.4 | 73.6 ± 10.1 | .47 |
Values are mean ± SD.
Figure. .
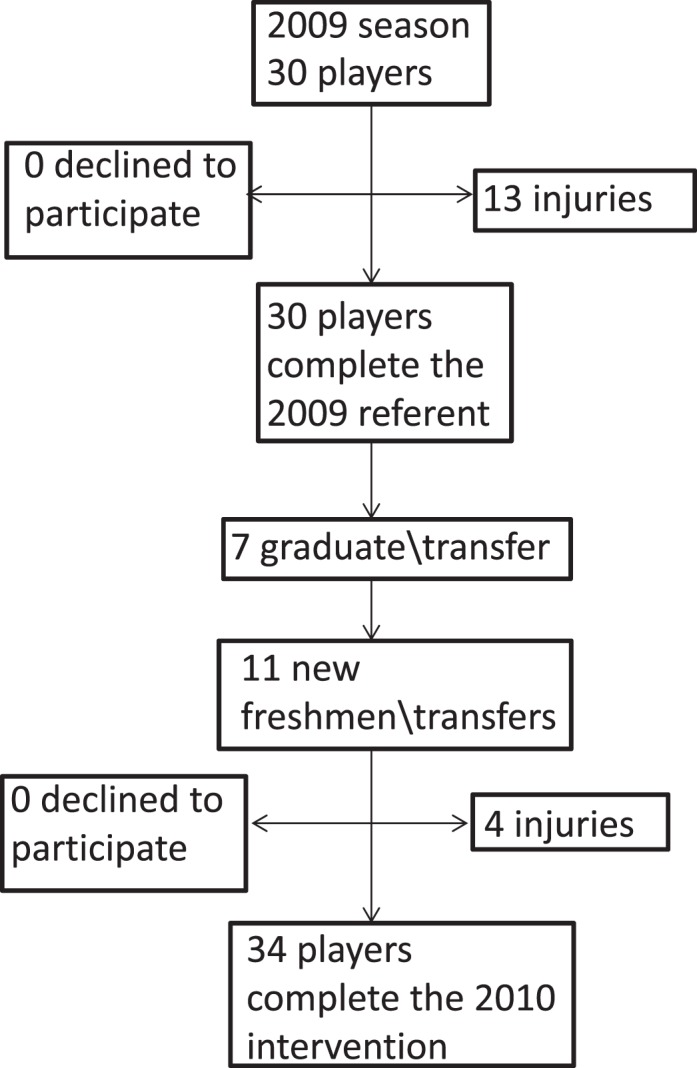
Flow chart depicting participant selection.
The referent team completed a standard dynamic warm-up following National Strength and Conditioning Association guidelines64 before every practice and game (Table 2). During the intervention season, the entire team completed the F-MARC 11+59 injury prevention program before every practice and an abbreviated form of the program involving only the running exercises before games. The same clinician (a certified athletic trainer and strength and conditioning specialist with 3 years' experience) supervised and instructed participants in both the referent standard warm-up and F-MARC 11+ intervention for each season. The referent and intervention program was completed during the preseason and in-season, lasting approximately 12 weeks.
Table 2. .
2009 and 2010 Warm Up
| Warm-Up Programs |
| 2009 Referent |
| Jog |
| Hip-in |
| Hip-out |
| Toe walk |
| Heel walk |
| Lunge walk |
| Knee to chest |
| Heel to glute |
| Leg swing |
| 2010 Intervention |
| Initial running drills |
| Jog |
| Hip-in |
| Hip-out |
| Circle partner |
| Shoulder contact |
| Cut up and back |
| Exercises |
| Plank |
| Side plank |
| Eccentric hamstring |
| Single-legged balance |
| Squats |
| Jumps |
| Final running drills |
| Sprint |
| Bounding |
| Cut side to side |
Referent Program
The 2009 referent warm up (Table 2) was a standardized warm-up performed at the beginning of every practice and game. It consisted of 5 minutes of light jogging followed by dynamic lower extremity movements to prepare for activity. The hip-in and hip-out was done standing with maximum hip flexion and knee flexion and then internal rotation and external rotation, 5 times for each leg and each rotation. The toe-and-heel walk consisted of 10-yard walks while maintaining maximum dorsiflexion or plantar flexion. The lunge walk consisted of 20 yards of an alternating walking lunge. For the knee-to-chest movement, after maximal active hip flexion, the athletes used their arms to pull themselves into maximal passive hip flexion or soft tissue approximation with the torso, holding for 1–2 seconds, 5 times for each leg. The heel-to-gluteus movement involved maximal knee flexion with the hip in slight extension, using the ipsilateral hand to grasp the foot and hold it for 1–2 seconds, 5 times for each leg. The single-legged deadlift involved reaching down to touch the ground while maintaining 1 leg in contact with the ground and the other leg behind, moving the body and nonstance limb parallel with the ground, 5 times for each leg. Leg swings consisted of maximal active hip flexion with the knee extended, followed by maximal active hip extension with the knee extended, 5 times for each leg.
Intervention Program
The F-MARC 11+ program (www.f-marc.com/11plus) takes approximately 20 minutes and consists of 3 components. The first component is 6 running exercises performed at moderate speed with dynamic stretching and controlled perturbations with a partner. The second component is 6 exercises targeting strength, balance, and jump-landing control with progression (Table 3). The last component is 3 higher-speed running drills with cutting maneuvers. The soccer field was set up as presented in the F-MARC manual.59 Each intervention session was supervised by the athletic trainer to ensure compliance and consistency of verbal feedback regarding exercise technique. The 6 exercises have 3 levels of progressive difficulty. All athletes were advanced to the next level individually by the team's athletic trainer as they became proficient in the desired movement skills. Each athlete's progression for each exercise was documented. Compliance with the training program was tracked at every in-season practice and game by the attending athletic trainer. This equated to the program being completed 5 to 6 times per week. No players chose to abstain, and every player completed the program before participating in each game or practice. When athletes lost time to injury and did not participate in a game or practice, they also did not participate in the intervention.
Table 3. .
Progressive Exercises
| F-MARC 11+ Exercise-Specific Progressions | ||||||
| Progressive Exercise |
Plank |
Side Plank |
Eccentric Hamstrings |
Single-Limb Balance |
Squats |
Jumps |
| Level 1 | 3 × 30 s | 3 × 30 static | 5 | 2 × 30 s | 2 × 10 squat | 2 × 30 s in place |
| Level 2 | 4 × 40 s alternate leg | 3 × 30 active | 10 | Ball throw 2 × 30 | 2 × 10 lunge | 2 × 30 s side |
| Level 3 | 3 × 30 s 1-legged hold | 3 × 30 active with leg | 15 | Partner perturbation 2 × 30 | 2 × 10 SL squat | 2 × 30 s box |
Statistical Analysis
Mean time loss associated with lower extremity injury between groups was examined with an independent t test and an a priori α level set at P ≤ .05. Relative risk calculations were used to compare lower extremity injury incidence (per 1000 AEs) between the referent and experimental seasons. A secondary analysis was performed between the seasons, analyzing only those players who participated in both seasons. A paired t test with a P ≤ .05 was used to assess between-groups differences in mean time loss to lower extremity injury, and relative risk was calculated for injury incidence.
RESULTS
The 2010 intervention team demonstrated a lower extremity injury rate of 2.2 per 1000 AEs versus 8.1 per 1000 AEs in the 2009 referent team (Table 4). The referent team lost 291 days to injury, and the intervention season lost 52 days to injury. The effect size of the intervention program to reduce days lost to lower extremity injury was 0.733, indicating a medium to large effect. The relative risk for injury occurrence of 0.28 was significant, with a 95% confidence interval (CI) that did not cross 1 (0.09, 0.85), indicating that the intervention group had a 72% reduction in lower extremity injury risk. The intervention-season participants lost less time to lower extremity injury than did the referent-season group (P < .01).
Table 4. .
Exposure and Injury Data
| Variable |
Season |
Time Lost Breakdown |
||
| 2009 Referent |
2010 Intervention |
2009 Referent |
2010 Intervention |
|
| Total exposures | 1612 | 1802 | ||
| Injury incidence per 1000 exposures | 8.1 | 2.2 | ||
| Training hours | 2104.5 | 2389.5 | ||
| Match hours | 313.5 | 313.5 | ||
| Training injuries | 10 | 2 | ||
| Match injuries | 3 | 2 | ||
| Injuries per 1000 training hours | 4.8 | 0.8 | ||
| Injuries per 1000 match hours | 9.6 | 6.4 | ||
| Days lost (lower extremity injury) | 291 | 52 | ||
| Total injuries | 13 | 4 | ||
| Specific injury incidence | ||||
| Hip flexor strain | 1 | 0 | 5 | 0 |
| Hamstrings strain | 5 | 1 | 13, 14, 14, 17, 35 | 10 |
| Quadriceps strain | 3 | 0 | 15, 18, 65 | 0 |
| Groin strain | 1 | 0 | 21 | 0 |
| Knee medial collateral ligament sprain | 0 | 1 | 0 | 5 |
| Knee meniscus injury | 1 | 0 | 32 | 0 |
| Lower leg (tibial stress injury) | 1 | 1 | 26 | 20 |
| Ankle sprain | 0 | 0 | 0 | 0 |
| Midfoot sprain | 1 | 0 | 16 | 0 |
| First metatarsophalangeal joint sprain (turf toe) | 0 | 1 | 0 | 17 |
Except for 1 grade 3 quadriceps strain in 2009 (65 days lost) and 1 grade 1 hip-flexor strain in 2009 (5 days lost), all other muscle strains were diagnosed as grade 2 upon initial examination. Diagnostic imaging confirmed the knee injuries, tibial stress injuries, hamstrings strain associated with 35 days lost, and quadriceps strain associated with 65 days lost (Table 4). The team physician was involved in confirming the diagnosis for all time-loss muscle injuries. In the paired analysis, players who did not compete in both seasons were removed, resulting in lower extremity injury rates of 8.8 per 1000 AEs for the 2009 referent team and 1.7 per 1000 AEs for the 2010 intervention team. A total of 213 days were lost to injury during the referent season, compared with 25 days during the intervention season. The relative risk for injury occurrence was significant at 0.19, with a 95% confidence interval that did not cross (0.04, 0.88) indicating that the intervention group had an 81% decrease in lower extremity injury risk. The paired analysis confirmed the overall analyses, with the intervention group demonstrating less time lost to lower extremity injury than the referent group (P < .01).
For comparison with international injury reporting, the injury and exposure breakdown per hour of exposure model as described by Fuller at al65 is shown in Table 4.
Specific Injuries
No ACL injuries or other severe internal knee derangements occurred during either season. Thigh muscle strains were the most common injury in both seasons. Muscle strains accounted for 217 days lost in the referent season and only 10 days in the intervention season (187 and 0, respectively, in the paired analysis). Thigh muscle strains occurred 10 times in the referent season and 1 time in the intervention season (8 and 0, respectively, in the paired analysis). Muscle strain injury rate in the referent season was 6.20 per 1000 AEs versus 0.55 per 1000 AEs in the intervention season. Time lost to thigh muscle strain was less in the intervention season in both the paired and independent analyses (P <.001). Relative risk for a thigh muscle strain was 0.05 (95% CI = 0.03, 0.09), indicating a 95% decrease in thigh muscle strain injury risk in the intervention group. The paired analysis (same athletes from both seasons) confirmed the reduction in relative risk (mean = 0.003, 95% CI = 0.0002, 0.04) from the intervention.
DISCUSSION
Our main findings were that lower extremity injuries and time lost decreased with implementation of a supervised injury-prevention program. Not only did the overall lower extremity injury risk decrease, but the severity of those injuries decreased as shown by the decrease in time lost. Previous injury-prevention studies using an older version of the F-MARC 11+ or other multifaceted injury-prevention/warm-up programs have been limited by noncompliance66; lack of progression in volume or intensity,42 causing physiologic improvements to level off or decrease67; and a lack of direct qualified supervision.41 Compliance is highly related to the effectiveness of reducing lower extremity injury using preventive interventions.36 This investigation benefited from having athletic training staff present to administer the program at every exposure.
Exercise Program
We used the latest version of the F-MARC 11+59 program in this study. The “+” portion reflects the addition of running drills and progressive exercise to the original 11 programs to increase compliance, improve the soccer specificity of the program, and teach proper knee and trunk control during cutting and landing. McCann et al67 reported that, without program progression and continued compliance with a program, the initial effects of the intervention on neuromechanical risk factors dissipated. In our study, not only was the intervention continued from the preseason throughout the season, but the exercises were progressive. As a result, the physiologic improvements initially brought about by the intervention were probably less likely to deteriorate.68 Limitations of many injury-prevention studies are the lack of compliance, continued follow-up, and progression.36,37,42,55 We demonstrated a model for program compliance, injury and exposure monitoring, and exercise progression that can be implemented to decrease the risk of lower extremity injury. An athletic trainer implemented and monitored the intervention program with minimal time and resource requirements beyond those of the control season. In addition, in-season–only training programs that are intended to reduce injury or injury risk factors may have less efficacy46 or no effect until the second part of the season, by which time the intervention dosage has become adequate.31 As supported by our findings, a more intense preseason training program combined with an in-season maintenance program may be ideal for injury risk reduction.58,68
A limitation of past programs was that the coach or other nonmedical personnel was required to implement the program, monitor compliance, and document exposures and injury incidence.41,42,55,66 Not having a clinician present may restrict the quality of feedback, corrective technique, and progression. Failure to progress the exercises may reduce compliance42 and increase the chance that the benefits of the program (improved neuromuscular control, increased muscular strength and endurance, improved stability and balance) will plateau.67,69 Improving injury-prevention program compliance42,66 and increasing the involvement of highly trained medical personnel to ensure quality of the feedback and intervention technique have been proposed to significantly affect the success of the program.18,42,66
Implications
The F-MARC 11+ program may be more effective than a traditional soccer warm-up in preventing lower extremity injury and limiting time lost from sport. Because medical or training personnel are present at both practices and games in many collegiate and professional programs, having a supervised and monitored intervention such as the one we used can be implemented within their scope of practice and integrated into their workflow. However, our results cannot be generalized to teams or institutions with fewer resources that may lack appropriate personnel. The F-MARC 11+ training program required a similar time commitment (20 minutes) as the traditional warm-up program but resulted in a decreased injury risk.
Methodologic Limitations
Several factors should be considered when interpreting the results of this study. The investigation took place at a single NCAA Division III institution with 1 male collegiate soccer program. However, the clinical benefits derived in this study demonstrate the effects of a certified athletic trainer and an intervention program that requires minimal resources.
Seven athletes in the 2009 season did not play on the 2010 team. The 2010 team added 11 players; hence, exposures were greater than in 2009. Additionally, we did not account for previous injuries or other potential predisposing factors for injury in either year; players were included regardless of injury history. Although previous injury has repeatedly been shown to be the best predictor of future injury,70–75 the injury-prevention program still demonstrated efficacy. Thus, the higher number of time-loss injuries in the 2009 season relative to the 2010 intervention season only strengthens our results. No other substantial changes occurred between the seasons in practice or game field, coaches or medical staff, or other training variables. The 9-month period between seasons limits the possibility of any carryover in strength or conditioning from the 2009 program to affect injury incidence in the 2010 season.
The F-MARC 11+ is a multifaceted program, which limits the ability to identify any particular section of the intervention program that may be more effective for injury prevention. This is a common concern with injury-prevention programs. Because most of the injuries in the referent season were hamstrings muscle strains and only 1 such strain occurred in the intervention season, the eccentric hamstring exercises may have been key to decreasing hamstrings injury rates.33,34,76–80
Future Research
Work is underway to continue this intervention, broaden it to other soccer programs, and modify it for other sports. The 2009 referent season had an injury rate of 8.1 per 1000 AEs, compared with the NCAA average of 8.0 per 1000 exposures. During the intervention season, the injury rate dropped to only 2.2 per 1000 exposures. Comparing our data with international soccer injury reporting is difficult because of different injury definitions. Hawkins et al,4 for instance, used 48 hours removed from training or competition and included all injuries, not just those to the lower extremity. The rules of international soccer regarding substitutions (eg, NCAA allows multiple player substitutions in a match up to 11 at a time, whereas FIFA allows only 3 per game) may influence exposure match hours for each player as well as return-to-play decision making.65
The lack of quantifiable gains in performance, neuromuscular, proprioceptive, or strength function is a limiting factor in many injury-prevention research studies.18 Because we did not quantify physiologic variables, we cannot adequately determine the mechanism of decreased injury risk or identify the most effective part of the intervention program. Future researchers should assess the biomechanical and physiologic changes the F-MARC 11+ program targets to decrease injury risk, such as cutting kinematics and kinetics, core stability, and lower extremity neuromuscular control.
This program was effective in a male collegiate population and in similar programs involving youth and adolescent handball and both male and female soccer players,37,39–41 but our results cannot be generalized to populations beyond male NCAA Division III soccer players. Given the high volume of literature supporting a sex difference in injury rates2,81 and risk factors,82–85 our findings add to the current information about interventions in the male population, especially at the collegiate level, and provide an effective option for intervention. Future authors should expand on different implementation strategies involving strength coaches, sport coaches, team captains, physical therapists, and physiotherapists.41,42,60,86 We used a cohort design, so randomized controlled trials for higher-level evidence in this population are still needed.
CONCLUSIONS
The risk of lower extremity injury in soccer may be decreased with a structured, exercise-based warm-up program targeting balance, neuromuscular control, and muscular strength. This program was simple to implement, required no extra equipment, and was conducted during the typical warm-up timeframe of a collegiate soccer practice or game. Our results offer ways for the practicing athletic trainer to be more involved in injury prevention in a relatively simple and evidence-supported manner that requires limited resources.
ACKNOWLEDGMENTS
We thank the College of Mount Saint Joseph soccer players, coaches, and medical staff for their hard work and participation, specifically athletic trainers Krisi Stauffer, MEd, ATC, and Katelyn Freece, MS, ATC; head coach Rudy Argueta; assistant coach Leah Todd; and team captains Lee Rogers and Tommy Sunderhaus.
REFERENCES
- 1.FIFA. 270 Million people active in football. 2006 http://www.fifa.com/mm/document/fifafacts/bcoffsurv/bigcount.statspackage_7024.pdf. [Google Scholar]
- 2.Agel J, Evans TA, Dick R, Putukian M, Marshall SW. Descriptive epidemiology of collegiate men's soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2002–2003. J Athl Train. 2007;42(2):270–277. [PMC free article] [PubMed] [Google Scholar]
- 3.Junge A, Dvorak J. Soccer injuries: a review on incidence and prevention. Sports Med. 2004;34(13):929–938. doi: 10.2165/00007256-200434130-00004. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. 2001;35(1):43–47. doi: 10.1136/bjsm.35.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 6.Turner AP, Barlow JH, Heathcote-Elliott C. Long term health impact of playing professional football in the United Kingdom. Br J Sports Med. 2000;34(5):332–336. doi: 10.1136/bjsm.34.5.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63(3):269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roos EM. Joint injury causes knee osteoarthritis in young adults. Curr Opin Rheumatol. 2005;17(2):195–200. doi: 10.1097/01.bor.0000151406.64393.00. [DOI] [PubMed] [Google Scholar]
- 9.Thelin N, Holmberg S, Thelin A. Knee injuries account for the sports-related increased risk of knee osteoarthritis. Scand J Med Sci Sports. 2006;16(5):329–333. doi: 10.1111/j.1600-0838.2005.00497.x. [DOI] [PubMed] [Google Scholar]
- 10.Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–620. doi: 10.1177/0363546505281813. [DOI] [PubMed] [Google Scholar]
- 11.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):705–729. doi: 10.1007/s00167-009-0813-1. [DOI] [PubMed] [Google Scholar]
- 13.Dvorak J, Junge A, Chomiak J, et al. Risk factor analysis for injuries in football players: possibilities for a prevention program. Am J Sports Med. 2000;28(5 suppl):S69–S74. doi: 10.1177/28.suppl_5.s-69. [DOI] [PubMed] [Google Scholar]
- 14.Gabbe BJ, Finch CF, Bennell KL, Wajswelner H. Risk factors for hamstring injuries in community level Australian football. Br J Sports Med. 2005;39(2):106–110. doi: 10.1136/bjsm.2003.011197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gazivoda P, Rzonca EC, Schiraldi F. Soccer injuries. Types, locations, etiologies, and preventive measures. J Am Podiatr Med Assoc. 1986;76(2):109–111. doi: 10.7547/87507315-76-2-109. [DOI] [PubMed] [Google Scholar]
- 16.Inklaar H. Soccer injuries, II: aetiology and prevention. Sports Med. 1994;18(2):81–93. doi: 10.2165/00007256-199418020-00002. [DOI] [PubMed] [Google Scholar]
- 17.Inklaar H, Bol E, Schmikli SL, Mosterd WL. Injuries in male soccer players: team risk analysis. Int J Sports Med. 1996;17(3):229–234. doi: 10.1055/s-2007-972837. [DOI] [PubMed] [Google Scholar]
- 18.Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17(8):859–879. doi: 10.1007/s00167-009-0823-z. [DOI] [PubMed] [Google Scholar]
- 19.Barber-Westin SD, Noyes FR, Smith ST, Campbell TM. Reducing the risk of noncontact anterior cruciate ligament injuries in the female athlete. Phys Sportsmed. 2009;37(3):49–61. doi: 10.3810/psm.2009.10.1729. [DOI] [PubMed] [Google Scholar]
- 20.Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36(8):1469–1475. doi: 10.1177/0363546508316764. [DOI] [PubMed] [Google Scholar]
- 21.Gabbe BJ, Finch CF, Wajswelner H, Bennell KL. Predictors of lower extremity injuries at the community level of Australian football. Clin J Sport Med. 2004;14(2):56–63. doi: 10.1097/00042752-200403000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Hrysomallis C. Relationship between balance ability, training and sports injury risk. Sports Med. 2007;37(6):547–556. doi: 10.2165/00007256-200737060-00007. [DOI] [PubMed] [Google Scholar]
- 23.Soderman K, Alfredson H, Pietila T, Werner S. Risk factors for leg injuries in female soccer players: a prospective investigation during one outdoor season. Knee Surg Sports Traumatol Arthrosc. 2001;9(5):313–321. doi: 10.1007/s001670100228. [DOI] [PubMed] [Google Scholar]
- 24.Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008;36(6):1052–1060. doi: 10.1177/0363546508314432. [DOI] [PubMed] [Google Scholar]
- 25.Zebis MK, Andersen LL, Bencke J, Kjaer M, Aagaard P. Identification of athletes at future risk of anterior cruciate ligament ruptures by neuromuscular screening. Am J Sports Med. 2009;37(10):1967–1973. doi: 10.1177/0363546509335000. [DOI] [PubMed] [Google Scholar]
- 26.Handoll HH, Rowe BH, Quinn KM, de Bie R. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2001 doi: 10.1002/14651858.CD000018. 3):CD000018. [DOI] [PubMed] [Google Scholar]
- 27.Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35(6):922–926. doi: 10.1177/0363546507299259. [DOI] [PubMed] [Google Scholar]
- 28.Ergen E, Ulkar B. Proprioception and ankle injuries in soccer. Clin Sports Med. 2008;27(1):195–217. doi: 10.1016/j.csm.2007.10.002. x. [DOI] [PubMed] [Google Scholar]
- 29.Kraemer R, Knobloch K. A soccer-specific balance training program for hamstring muscle and patellar and achilles tendon injuries: an intervention study in premier league female soccer. Am J Sports Med. 2009;37(7):1384–1393. doi: 10.1177/0363546509333012. [DOI] [PubMed] [Google Scholar]
- 30.Caraffa A, Cerulli G, Projetti M, Aisa G, Rizzo A. Prevention of anterior cruciate ligament injuries in soccer: a prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 31.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 32.Arnason A, Andersen TE, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1):40–48. doi: 10.1111/j.1600-0838.2006.00634.x. [DOI] [PubMed] [Google Scholar]
- 33.Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13(4):244–250. doi: 10.1034/j.1600-0838.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- 34.Gabbe BJ, Branson R, Bennell KL. A pilot randomised controlled trial of eccentric exercise to prevent hamstring injuries in community-level Australian football. J Sci Med Sport. 2006;9(1–2):103–109. doi: 10.1016/j.jsams.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 35.Parkkari J, Kujala UM, Kannus P. Is it possible to prevent sports injuries? Review of controlled clinical trials and recommendations for future work. Sports Med. 2001;31(14):985–995. doi: 10.2165/00007256-200131140-00003. [DOI] [PubMed] [Google Scholar]
- 36.Sugimoto D, Myer GD, Bush HM, Klugman MF, McKeon JM, Hewett TE. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714–723. doi: 10.4085/1062-6050-47.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Junge A, Rosch D, Peterson L, Graf-Baumann T, Dvorak J. Prevention of soccer injuries: a prospective intervention study in youth amateur players. Am J Sports Med. 2002;30(5):652–659. doi: 10.1177/03635465020300050401. [DOI] [PubMed] [Google Scholar]
- 38.Longo UG, Loppini M, Berton A, Marinozzi A, Maffulli N, Denaro V. The FIFA 11+ program is effective in preventing injuries in elite male basketball players: a cluster randomized controlled trial. Am J Sports Med. 2012;40(5):996–1005. doi: 10.1177/0363546512438761. [DOI] [PubMed] [Google Scholar]
- 39.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469. doi: 10.1136/bmj.a2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Steffen K, Myklebust G, Olsen OE, Holme I, Bahr R. Preventing injuries in female youth football: a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18(5):605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 43.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 44.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 45.Faigenbaum AD, Farrel A, Fabiano M, et al. Effects of integrative neuromuscular training on fitness performance in children. Pediatr Exerc Sci. 2011;23(4):573–584. doi: 10.1123/pes.23.4.573. [DOI] [PubMed] [Google Scholar]
- 46.Klugman MF, Brent JL, Myer GD, Ford KR, Hewett TE. Does an in-season only neuromuscular training protocol reduce deficits quantified by the tuck jump assessment? Clin Sports Med. 2011;30(4):825–840. doi: 10.1016/j.csm.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 48.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic Balance training on power, balance and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 49.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 50.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8(39) doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42(7):614–619. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of noncontact anterior cruciate ligament injuries in elite and adolescent female team handball athletes. Instr Course Lect. 2007;56:407–418. [PubMed] [Google Scholar]
- 53.Emery CA, Meeuwisse WH. The effectiveness of a neuromuscular prevention strategy to reduce injuries in youth soccer: a cluster-randomised controlled trial. Br J Sports Med. 2010;44(8):555–562. doi: 10.1136/bjsm.2010.074377. [DOI] [PubMed] [Google Scholar]
- 54.Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33(7):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 55.Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. doi: 10.1136/bmj.e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Steffen K, Bakka HM, Myklebust G, Bahr R. Performance aspects of an injury prevention program: a ten-week intervention in adolescent female football players. Scand J Med Sci Sports. 2008;18(5):596–604. doi: 10.1111/j.1600-0838.2007.00708.x. [DOI] [PubMed] [Google Scholar]
- 57.Heidt RS, Jr, Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 58.Grindstaff TL, Hammill RR, Tuzson AE, Hertel J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: a numbers-needed-to-treat analysis. J Athl Train. 2006;41(4):450–456. [PMC free article] [PubMed] [Google Scholar]
- 59.Dvorak J JA. Football Medicine Manual. Zurich, Switzerland: Fédération Internationale de Football Association;; 2005. [Google Scholar]
- 60.Junge A, Lamprecht M, Stamm H, et al. Countrywide campaign to prevent soccer injuries in Swiss amateur players. Am J Sports Med. 2011;39(1):57–63. doi: 10.1177/0363546510377424. [DOI] [PubMed] [Google Scholar]
- 61.Dick R, Agel J, Marshall SW. National Collegiate Athletic Association Injury Surveillance System commentaries: introduction and methods. J Athl Train. 2009;42(2):173–182. [PMC free article] [PubMed] [Google Scholar]
- 62.Zarins B, Ciullo JV. Acute muscle and tendon injuries in athletes. Clin Sports Med. 1983;2(1):167–182. [PubMed] [Google Scholar]
- 63.Magee DJ. Orthopedic Physical Assessment. 4th ed. St. Louis, MO: WB Saunders Ltd; 2002. p. 29. [Google Scholar]
- 64.Baechle TR, Earle RW. Essentials of Strength and Conditioning. 2nd ed. Champaign, IL: Human Kinetics;; 2000. [Google Scholar]
- 65.Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports. 2006;16(2):83–92. doi: 10.1111/j.1600-0838.2006.00528.x. [DOI] [PubMed] [Google Scholar]
- 66.Soligard T, Nilstad A, Steffen K, et al. Compliance with a comprehensive warm-up programme to prevent injuries in youth football. Br J Sports Med. 2010;44(11):787–793. doi: 10.1136/bjsm.2009.070672. [DOI] [PubMed] [Google Scholar]
- 67.McCann R, Cortes N, Van Lunen BL, Greska E, Ringleb S, Onat JA. Neuromuscular changes following an injury prevention program for ACL injuries. Int J Athl Ther Train. 2011;16(4):16–20. [Google Scholar]
- 68.Padua DA, DiStefano LJ, Marshall SW, Beutler AI, de la Motte SJ, DiStefano MJ. Retention of movement pattern changes after a lower extremity injury prevention program is affected by program duration. Am J Sports Med. 2012;40(2):300–306. doi: 10.1177/0363546511425474. [DOI] [PubMed] [Google Scholar]
- 69.Mujika I, Padilla S. Detraining: loss of training-induced physiological and performance adaptations. Part I: short term insufficient training stimulus. Sports Med. 2000;30(2):79–87. doi: 10.2165/00007256-200030020-00002. [DOI] [PubMed] [Google Scholar]
- 70.Risk factors: meta-analysis shows that previous knee injury significantly increases the risk of OA development. Nature reviews. Rheumatology. 2011;7(11):621. [Google Scholar]
- 71.Swaine BR, Tremblay C, Platt RW, Grimard G, Zhang X, Pless IB. Previous head injury is a risk factor for subsequent head injury in children: a longitudinal cohort study. Pediatrics. 2007;119(4):749–758. doi: 10.1542/peds.2006-1186. [DOI] [PubMed] [Google Scholar]
- 72.Hagglund M, Walden M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767–772. doi: 10.1136/bjsm.2006.026609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Walden M, Hagglund M, Ekstrand J. High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med. 2006;40(2):158–162. doi: 10.1136/bjsm.2005.021055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nadler SF, Malanga GA, Feinberg JH, Rubanni M, Moley P, Foye P. Functional performance deficits in athletes with previous lower extremity injury. Clin J Sport Med. 2002;12(2):73–78. doi: 10.1097/00042752-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 75.Watson AW. Sports injuries related to flexibility, posture, acceleration, clinical defects, and previous injury, in high-level players of body contact sports. Int J Sports Med. 2001;22(3):222–225. doi: 10.1055/s-2001-16383. [DOI] [PubMed] [Google Scholar]
- 76.Petersen J, Thorborg K, Nielsen MB, Budtz-Jorgensen E, Holmich P. Preventive effect of eccentric training on acute hamstring injuries in men's soccer: a cluster-randomized controlled trial. Am J Sports Med. 2011;39(11):2296–2303. doi: 10.1177/0363546511419277. [DOI] [PubMed] [Google Scholar]
- 77.Greenstein JS, Bishop BN, Edward JS, Topp RV. The effects of a closed-chain, eccentric training program on hamstring injuries of a professional football cheerleading team. J Manipulative Physiol Ther. 2011;34(3):195–200. doi: 10.1016/j.jmpt.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 78.Brughelli M, Nosaka K, Cronin J. Application of eccentric exercise on an Australian Rules football player with recurrent hamstring injuries. Phys Ther Sport. 2009;10(2):75–80. doi: 10.1016/j.ptsp.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 79.Hibbert O, Cheong K, Grant A, Beers A, Moizumi T. A systematic review of the effectiveness of eccentric strength training in the prevention of hamstring muscle strains in otherwise healthy individuals. N Am J Sports Phys Ther. 2008;3(2):67–81. [PMC free article] [PubMed] [Google Scholar]
- 80.Mjolsnes R, Arnason A, Osthagen T, Raastad T, Bahr R. A. 10-week randomized trial comparing eccentric vs. concentric hamstring strength training in well-trained soccer players. Scand J Med Sci Sports. 2004;14(5):311–317. doi: 10.1046/j.1600-0838.2003.367.x. [DOI] [PubMed] [Google Scholar]
- 81.Dick R, Putukian M, Agel J, Evans TA, Marshall SW. Descriptive epidemiology of collegiate women's soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2002–2003. J Athl Train. 2007;42(2):278–285. [PMC free article] [PubMed] [Google Scholar]
- 82.Fagenbaum R, Darling WG. Jump landing strategies in male and female college athletes and the implications of such strategies for anterior cruciate ligament injury. Am J Sports Med. 2003;31(2):233–240. doi: 10.1177/03635465030310021301. [DOI] [PubMed] [Google Scholar]
- 83.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Neuromuscular and lower limb biomechanical differences exist between male and female elite adolescent soccer players during an unanticipated side-cut maneuver. Am J Sports Med. 2007;35(11):1888–1900. doi: 10.1177/0363546507300823. [DOI] [PubMed] [Google Scholar]
- 84.Noyes FR, Barber-Westin SD, Fleckenstein C, Walsh C, West J. The drop-jump screening test: difference in lower limb control by gender and effect of neuromuscular training in female athletes. Am J Sports Med. 2005;33(2):197–207. doi: 10.1177/0363546504266484. [DOI] [PubMed] [Google Scholar]
- 85.Pappas E, Hagins M, Sheikhzadeh A, Nordin M, Rose D. Biomechanical differences between unilateral and bilateral landings from a jump: gender differences. Clin J Sport Med. 2007;17(4):263–268. doi: 10.1097/JSM.0b013e31811f415b. [DOI] [PubMed] [Google Scholar]
- 86.LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165(11):1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]


