Abstract
Context:
Understanding concussion-assessmment and -management practices that athletic trainers (ATs) currently use will allow clinicians to identify potential strategies for enhancing the quality of care provided to patients.
Objective:
To assess current clinical concussion diagnostic and return-to-participation practices among ATs.
Design:
Cross-sectional study.
Setting:
Web-based survey.
Patients or Other Participants:
A link to the survey was sent randomly to a convenience sample of 3222 members of the National Athletic Trainers' Association. A total of 1053 (32.7%) certified ATs (experience as an AT = 11.2 ± 9.1 years) responded to the survey.
Intervention(s):
Prospective participants received electronic correspondence informing them of the purpose of the study and providing a link to the Web-based survey instrument. A reminder e-mail was sent approximately 6 weeks later, and the survey remained online for a total of 8 weeks.
Main Outcome Measure(s):
We collected information on the annual number of concussions assessed and tools employed to diagnose, manage, and safely return an athlete to participation. Descriptive statistics were computed for each variable.
Results:
Participants reported observing 10.7 ± 11.0 concussions per year. Clinical examination (n = 743, 70.6%) was the most commonly reported means for evaluating and diagnosing concussion. Less than half of our respondents employed the Standardized Assessment of Concussion (n = 467, 44.3%), any variation of the Romberg test (n = 461, 43.8%), and computerized neuropsychological testing (n = 459, 43.6%). Clinical examination (n = 773, 73.4%), return-to-participation guidelines (n = 713, 67.7%), physician recommendation (n = 660, 62.7%), or player self-report (n = 447, 42.5%) contributed to the return-to-participation decisions of ATs. Only 20.8% (n = 219) of ATs reported using all 3 recommended domains of the concussion battery.
Conclusions:
Our study demonstrated a growth in the number of ATs incorporating objective clinical measures of concussion as a part of their concussion management. Conversely, fewer ATs reported using a standard clinical examination in their concussion assessment. These findings suggest ATs must continue to increase their use of both objective concussion assessment tools and the standard clinical examination.
Key Words: traumatic brain injuries, return-to-play guidelines, evaluation
Key Points
Athletic trainers are making progress in assessing concussions and formulating safe return-to-participation decisions after these injuries.
Athletic trainers are using more objective tools available to them but have greatly decreased their use of clinical examinations and symptom evaluations when assessing and managing concussions.
More athletic trainers appear to be using all 3 components of the concussion-assessment battery than in the past, but the overall percentage who use all 3 components remains low.
Athletic trainers need to remember that the most effective concussion management involves using both objective clinical assessment tools and a standard clinical examination.
Research and knowledge about sport-related concussions have increased dramatically over the past decade.1–5 A PubMed search revealed that more concussion-related research papers have been published in the last 7 years than in the entire preceding 45-year period (Table 1). In addition, many states have enacted laws pertaining to concussions and safe return to participation among high school athletes. Currently, 49 states and Washington, DC, have laws in various forms to address concussion in youth sports.6
Table 1. .
Concussion Studies Found in PubMed Search
| Dates Searcheda |
No. of Published Studies |
| 1960–1969 | 8 |
| 1970–1979 | 27 |
| 1980–1989 | 25 |
| 1990–1999 | 108 |
| 2000–2004 | 207 |
| 2005–Present | 473 |
Search terms were concussion, mild traumatic brain injury, and sport.
Clinicians and researchers continue to search for more effective and safe ways to diagnose and return athletes to participation after concussion. Whereas management of this injury has evolved over the last decade, much debate still remains about the best methods to use in determining safe return to activity. Many researchers4,7–11 have advocated for a multifaceted approach to return to participation that includes at least a graded symptom checklist, neuropsychological test, and balance assessment. Investigators4,7 widely agree on the use of these tests, known as the concussion-assessment battery. However, we do not know how athletic trainers (ATs) are clinically applying the current research and recommendations. Given that ATs and physicians are allowed to make return-to-participation decisions in many states, they must not only understand the latest research but also apply it.
Two previous surveys1,12 have been used to assess the management of concussions by ATs. Although the survey results have provided insight into how ATs are applying the recommended methods, they also have pointed out where concussion management is lacking. Most concerning, Notebaert and Guskiewicz1 reported that 97% of respondents to their survey did not use all 3 recommended components of the concussion-assessment battery and noted that 24% used 2 methods and 80% used only 1. Since the publication of these results, several consensus statements and a large amount of research about concussions and concussion management have been published.3,4,11,13
Therefore, the purpose of our study was to assess current clinical concussion diagnostic and return-to-participation practices among ATs working in various settings and with various sports. By comparing our findings with data collected in previous studies, we will aid in clarifying where concussion education is lacking. These results may help clinicians, educators, and researchers promote and provide optimal management practices for concussion assessment and safe return of athletes to participation, leading to more standardized and effective procedures.
METHODS
Participants
A convenience sample of 3222 e-mail addresses of ATs who were members of the National Athletic Trainers' Association (NATA) was generated randomly from the NATA database. No specific work settings were targeted or excluded. Respondents who did not report currently being an AT were excluded. According to a Board of Certification representative, approximately 70% of certified ATs are NATA members (S. Leftwich, written communication, November 2011).
All participants provided written informed consent before reading the first survey questions, and the study was approved by the Illinois State University Institutional Review Board. Survey questions were not presented to an individual if consent was not given.
Instrumentation
The Web-based survey was hosted by Qualtrics (Qualtrics Inc, Provo, UT) and took approximately 10 minutes to complete. All responses were anonymous, and only the researchers had access to the resultant data. Questions were grouped in small blocks for the ease of the participants. The survey employed logic by which questions pertaining to concussion-assessment tools (eg, neuropsychological testing, graded symptom checklist) were asked only if the participant had indicated them as part of his or her concussion management.
The survey was a modification of surveys that were obtained with permission from the authors and had been used for similar research.1,12 We conducted a small pilot study to ensure the participants easily understood the survey. The pilot study included approximately 20 ATs from various settings, including National Collegiate Athletic Association Divisions I and III and high school athletics. We used feedback from the pilot-study participants along with the earlier surveys to construct our survey. Given the logic built into the survey, the number of questions ranged from 33 to 47. First, demographic information; current employment, including setting (ie, high school, college, clinic, or professional) and sport or sports covered; degrees earned; years certified; and numbers of concussions observed per year were obtained. Second, questions were asked to assess tools or methods used to diagnose, manage, and safely return athletes to participation after concussions. Third, several questions addressed various widely used concussion-assessment tools, such as a graded symptom checklist, the Standardized Assessment of Concussion,14 the Balance Error Scoring System (BESS),15 computerized and noncomputerized neuropsychological tests, and the Sport Concussion Assessment Tool 2 (SCAT2),4 and the value of these tools to the AT. Fourth, several questions were asked about the respondent's understanding of current concussion-related research and the effect this information has had on his or her clinical practices.
Procedures
From the random list generated by the NATA, we distributed an e-mail that directed the participants to the Web-based survey. Approximately 6 weeks after the initial e-mail, we sent a follow-up e-mail to all recipients of the first e-mail, regardless of whether they had already completed the survey. The survey remained online for a total of 8 weeks.
Data Analysis
All data were analyzed using Excel 2007 (Microsoft Corporation, Redmond, WA) to determine descriptive statistics. We also performed χ2 tests of association using SAS (version 9.3, SAS Institute Inc, Cary, NC). The α level was set a priori at .05 for all tests.
RESULTS
Participants
A total of 1057 surveys were submitted. Four respondents reported they were not ATs and were removed from the dataset, leaving a total of 1053 responses, for a response rate of 32.7% (1053/3222). In reporting the findings, we included all information that was received, which sometimes resulted in a varying number of responses to each question. For some of the questions in which the respondent was instructed to select all that apply, the respondent may have skipped the question; thus, our reported percentage was likely lower than the actual percentage.
The average experience among the respondents was 11.2 ± 9.1 years (11 802/1053). The most selected primary employment position or setting was high school, followed by collegiate athletics and sports medicine clinic (Table 2). When applicants were instructed to select all sports for which they provide clinical coverage, the most commonly selected response was men's basketball (615/1053 [58.4%]) followed by women's basketball (601/1053 [57.1%]), men's football (583/1053 [55.4%]), and women's soccer (564/1053 [53.6%].
Table 2. .
Work Setting of Respondents
| Work Setting |
Total Athletic Trainers, n (%) |
| High school athletics | 522 (49.6) |
| College athletics | 364 (34.6) |
| Sports medicine clinic | 189 (18.0) |
| Other | 107 (10.2) |
| Academic department | 45 (4.3) |
| Corporate health/fitness center/personal trainer | 40 (3.8) |
| Professional athletics | 39 (3.7) |
| General hospital | 33 (3.1) |
Concussion Frequency
The respondents reported observing 11 246 total concussions per year for an average of 10.7 ± 11.0 concussions (11 246/1047) per respondent. Athletic trainers working primarily with football reported the highest number of concussions per year (3716/11 246 [33.0%]), followed by ATs working with women's soccer (1266/11 246 [11.3%]) and men's soccer (1025/11 246 [9.1%]).
Approximately 30% of reported concussions involved amnesia of any kind (3143/11 246) or required more than 10 days for complete resolution of symptoms (3383/11 246). About 7% (783/11 246) of the total reported concussions involved loss of consciousness of any duration, whereas almost 40% (4391/11 246) required more than 10 days for complete return of the athlete to participation in sport.
Concussion Assessment and Management
When asked about the use of several of the most common grading scales, most respondents reported not using a grading scale (396/840 [47.1%]). The American Academy of Neurology16 grading scale was the next most selected response (168/840 [20.0%]), followed closely by the Cantu17 evidence-based grading scale (159/840 [18.9%]). Among total responses, no other grading scale was selected by more than 5.8% (49/840) of the participants. Regarding return-to-participation guidelines used, the Consensus Statement on Concussion in Sport4 was the most selected response (248/846 [29.3%]).
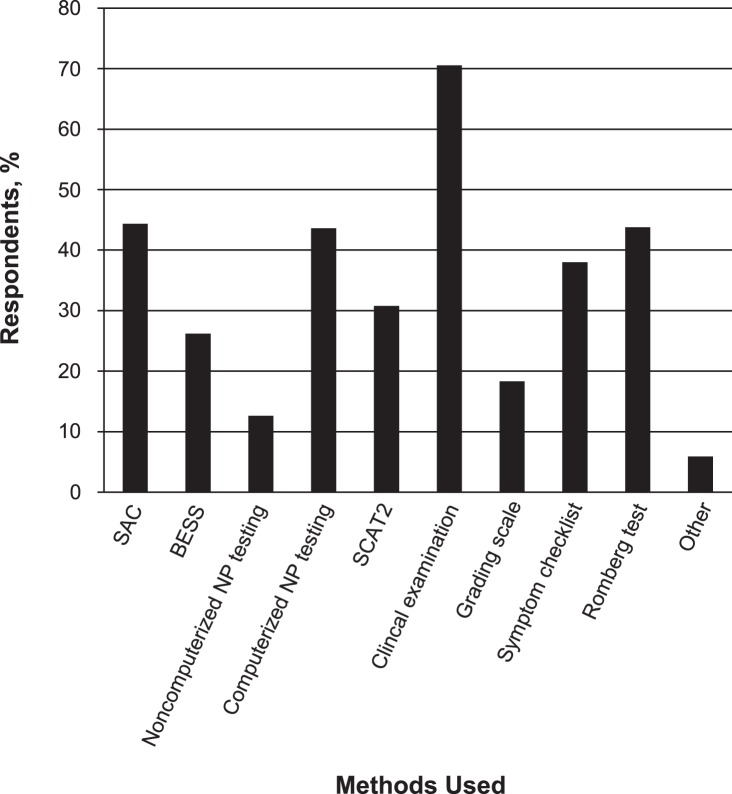
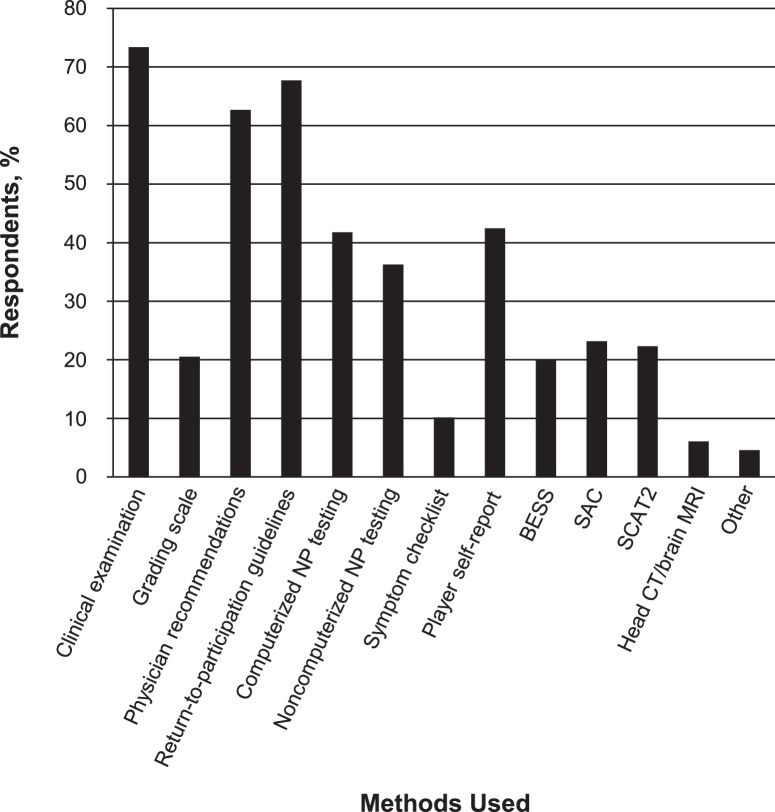
Clinical examination was the most commonly reported method used to assess and diagnose a concussion, followed by the Standardized Assessment of Concussion,14 any variation of a Romberg test, and computerized neuropsychological testing (Figure 1). Of ATs who selected computerized neuropsychological testing, more than 90% (415/459) reported using the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT; ImPACT Applications, Inc, Pittsburgh) computer-based test, and no other option received more than 4% of the responses. The most commonly selected response used to determine when to return an athlete to participation was clinical examination, followed by return-to-participation guidelines, physician's recommendations, and player self-report (Figure 2). About 77% (602/783) of respondents indicated they believed the standardized methods of concussion assessment are more clinically informative than a routine clinical examination alone. According to about 10% (74/702) of ATs, an athlete would be allowed to return to participation if he or she had a normal clinical examination but abnormal findings with standardized methods of concussion assessment.
Figure 1. .
Frequency of methods used to assess and diagnose concussion. Participants selected all methods that applied. Abbreviations: BESS, Balance Error Scoring System; NP, neuropsychological; SAC, Standardized Assessment of Concussion; and SCAT2, Sport Concussion Assessment Tool 2.
Figure 2. .
Frequency of methods used to determine when an athlete could return to participation. Participants selected all methods that applied. Abbreviations: BESS, Balance Error Scoring System; CT, computerized tomography; MRI, magnetic resonance imaging; NP, neuropsychological; SAC, Standardized Assessment of Concussion; and SCAT2, Sport Concussion Assessment Tool 2.
Athletic trainer was the most selected response for the primary person responsible for making return-to-participation decisions, followed by the team physician and primary care physician (Table 3). Coach and player were not selected, and only 2 respondents selected parents. About 38% (300/781) and 54% (422/778) of respondents reported having access to a neuropsychologist and neurologist, respectively, for consultation after concussion.
Table 3. .
Caregiver Primarily Responsible for Return-to-Participation Decision
| Caregiver Responsible for Return-to-Participation Decision |
Responses, n (%) |
| Athletic trainer | 369 (43.8) |
| Team physician | 301 (35.7) |
| Primary care physician | 113 (13.4) |
| Neurologist | 14 (1.7) |
| Neuropsychologist | 9 (1.1) |
| Neurosurgeon | 5 (0.6) |
| Coach | 0 (0) |
| Player | 0 (0) |
| Parents | 2 (0.2) |
| Other | 30 (3.6) |
When asked about familiarity with publications or directives about concussion, the most commonly selected item was the NATA position statement on concussion (2004)7 (730/1053 [69.3%]), followed by the Consensus Statement on Concussion in Sport (Zurich 2008)4 (512/1053 [48.6%]) and the National Collegiate Athletic Association Concussion Management Plan Legislation (2010)18 (475/1053 [45.1%]) (Table 4). Most respondents (680/753 [90.3%]) reported 1 or more of the publications or directives with which they were familiar had affected the way they manage concussions.
Table 4. .
Publications or Directives With Which Athletic Trainers are Familiar
| Publication or Directive |
Responses, n (%) |
| National Collegiate Athletic Association Concussion Management Plan Legislation (2010)18 | 475 (45.1) |
| Consensus Statement on Concussion in Sport (Zurich 2008)4 | 512 (48.6) |
| National Athletic Trainers' Association position statement on concussion (2004)7 | 730 (69.3) |
| Summary and agreement statement of conference on concussion (Prague 2004)3 | 296 (28.1) |
| Summary and agreement statement of conference on concussion (Vienna 2001)2 | 230 (21.8) |
| Other | 29 (2.8) |
Comparison of Practice Settings
We observed an association between the tools used as part of the diagnostic decision-making process and clinical setting ( = 48.93, P = .007). College ATs were 1.72 times more likely to use the BESS than high school ATs. We found high school ATs were 1.62 times more likely to use noncomputerized neuropsychological testing than their college counterparts. Conversely, college ATs were 1.18 and 1.39 times more likely to use computerized neuropsychological testing than high school ATs and ATs working in clinical settings, respectively.
= 48.93, P = .007). College ATs were 1.72 times more likely to use the BESS than high school ATs. We found high school ATs were 1.62 times more likely to use noncomputerized neuropsychological testing than their college counterparts. Conversely, college ATs were 1.18 and 1.39 times more likely to use computerized neuropsychological testing than high school ATs and ATs working in clinical settings, respectively.
We observed an association between the tools used as part of the return-to-participation decision-making process and clinical setting ( = 72.66, P < .001). Based on our data, ATs in clinical settings relied more on grading scales and physician recommendations and less on computerized neuropsychological testing to make return-to-participation decisions than we expected. Similarly, high school ATs were more likely to rely on physician recommendations and return-to-participation guidelines and less likely to rely on computerized neuropsychological testing and the BESS or SCAT2 to render these same decisions. Lastly, we observed that college ATs were more likely to use computerized neuropsychological testing, symptom checklists, BESS, and SCAT2 and less likely to use a grading scale, physician recommendations, return-to-participation guidelines, and player self-report to determine return-to-participation readiness than we expected due to chance.
= 72.66, P < .001). Based on our data, ATs in clinical settings relied more on grading scales and physician recommendations and less on computerized neuropsychological testing to make return-to-participation decisions than we expected. Similarly, high school ATs were more likely to rely on physician recommendations and return-to-participation guidelines and less likely to rely on computerized neuropsychological testing and the BESS or SCAT2 to render these same decisions. Lastly, we observed that college ATs were more likely to use computerized neuropsychological testing, symptom checklists, BESS, and SCAT2 and less likely to use a grading scale, physician recommendations, return-to-participation guidelines, and player self-report to determine return-to-participation readiness than we expected due to chance.
DISCUSSION
According to our data, ATs are using more objective tools available to them, such as balance testing and neuropsychological testing, but have greatly decreased their use of clinical examinations and symptom evaluations when assessing and managing concussions. Whereas we sought to assess current clinical concussion diagnoses and return-to-participation practices among ATs working in various settings and with various sports, we believe our findings reinforce the need for standardization in the management and safe return to participation of the athlete after concussion.
We noted several differences when comparing our survey results with those of surveys conducted in 199912 and 2005.1 The number of concussions assessed yearly on average were 7.0 in 199912 and 8.2 in 20051 but rose to 10.7 at the time of our survey. The reason for the possible rise in the number of concussions evaluated is unclear, but increased media scrutiny along with a growing number of state practice acts about concussion management are 2 likely contributors. More than 90% of our respondents stated their management of concussions has been affected by 1 or more of the publications or directives about which they were asked in the survey. Therefore, the growing number of concussion consensus statements and management guidelines also may play a role in the overall number of concussions assessed per year by each AT.
Another potential difference from the previous 2 surveys is the tools used to assess and diagnose concussions. About 15% of respondents used neuropsychological testing in 199912 and 18% in 2005,1 but our survey revealed approximately 57% of ATs now use these tests. The number of ATs using computerized neuropsychological tests markedly increased from about 15% in 2005 to about 44% at the time of our survey. The number of respondents using BESS15 also appears to have increased from 5% in 199912 to 16% in 200515 and to 26% at the time of our survey. This finding is encouraging because it demonstrates the possibility that more ATs are educated about and are applying the recommendations on which experts in the field of concussion management agree.
Conversely, several items likely were selected less often in our survey. Use of clinical examination and symptom checklist decreased from 95% and 85%, respectively, in 20051 to 71% and 38%, respectively, among our respondents. These findings are very disturbing because a thorough clinical examination, which should include a history and list of symptoms, observation, palpation, and special testing (eg, a cranial nerve assessment), is one of the most important components of proper concussion management.7 The “NATA Position Statement: Management of Sport-Related Concussion”7 made this point very clear, noting that other tools, such as postural-stability and neuropsychological testing, should be viewed as adjuncts to the clinical examination. One of the main reasons for conducting a clinical examination is to rule out a more serious focal injury, such as a subdural hematoma, epidural hematoma, or cerebral contusion. The downward trend in the number of ATs reporting the use of a clinical examination in their concussion management calls into question the practices that athletic training programs accredited by the Commission on Accreditation of Athletic Training Education are teaching and the standards the Board of Certification is using to certify entry-level ATs. It is possible the apparent increase in other areas of concussion management, such as neuropsychological and balance testing, has led to declines in more traditional areas, such as the clinical examination and symptom checklist. In addition, it is possible that more of our respondents actually use symptom checklists than reported doing so because many neuropsychological tests include a section in which the injured athlete can report current symptoms. Regardless of the reason or reasons why it appears clinical examination and symptom checklist were used less often, ATs in all clinical settings must recognize the need for and importance of the examination.
When asked whether standardized methods of concussion assessment are more clinically informative than a routine clinical examination alone, about 77% (602/783) of respondents indicated they believed the tests are helpful. Interestingly, the rate is between the 2 reported percentages from the previous studies (86% in 199912 and 68% in 20051). About 10% (74/702) of our respondents, compared with 1.2% in 199912 and 12.6% in 2005,1 stated an athlete would be allowed to return to participation if he or she had a normal clinical examination but abnormal findings using standardized methods of concussion assessment. Even with the increase in the use of neuropsychological and balance testing, this response suggests some clinicians continue to rely on the routine clinical examination alone. This finding is alarming because many researchers8,10,19–22 have shown the effectiveness of several tests in determining when athletes can safely return to participation after concussion.
In 1999, Ferrara et al12 found that about 18% of ATs used no concussion grading scale, whereas our survey revealed the percentage is now around 47%. Many researchers and clinicians2–4 have suggested concussion grading scales should be abandoned in favor of a more individualized approach, which takes into account all signs and symptoms of concussion. Existing grading scales, such as the scale put forth by the American Academy of Neurology,16 tend to focus on loss of consciousness and amnesia to grade the severity of the concussion. Many investigators22,23 have found loss of consciousness and amnesia occur in relatively few patients with concussions, making these symptoms unreliable as predictors of injury severity or outcome. Our results show amnesia and loss of consciousness are uncommon in athletes with concussions, further strengthening the argument against some of the formal concussion grading scales that stress these variables as predictors of severity of concussion.
Many researchers4,7,10 now advocate a 3-part concussion-assessment battery consisting of a symptom checklist, postural-stability assessment, and neuropsychological test to properly identify athletes who have sustained concussions. In 2005, Notebaert and Guskiewicz1 discovered an alarmingly low 3% of respondents were using all 3 areas of the assessment battery; however, about 24% used at least 2 methods, and about 80% used at least 1 method. Our data showed the percentage of ATs using all 3 recommended areas of the concussion-assessment battery has increased to about 21%, with about 53% using 2 methods and about 75% using at least 1 method. Our findings may be slightly low because we only inquired about the BESS test and any variation of the Romberg test when asking about postural-stability testing. Whereas 21% of ATs using all 3 methods is still a relatively small percentage, it potentially shows more ATs are educated about current recommendations than in the past, which is a positive step toward standardizing concussion management.
When comparing ATs by their work settings, we noted several interesting trends. First, for concussion diagnosis, high school ATs were more likely to use noncomputerized neuropsychological testing, whereas college ATs were more likely to use computerized neuropsychological testing. This finding is not unexpected because college ATs typically have larger budgets with which to work than high school ATs, potentially allowing them greater access to more expensive computer-based tests. Second, for return-to-participation decisions after concussion, we noted high school ATs were more likely to rely on physician recommendations and return-to-participation guidelines and less on computerized neuropsychological testing and the BESS or SCAT2. Conversely, college ATs were more likely to use computerized neuropsychological testing, symptom checklists, BESS, and SCAT2 and less likely to employ a grading scale, physician recommendations, return-to-participation guidelines, and player self-report in making return-to-participation decisions. The apparent de-emphasis on physician recommendations and return-to-participation guidelines by college ATs is an interesting finding and shows college ATs may rely more on various tools available to them when making return-to-participation decisions. The ATs at the college level often appeared to make their own return-to-participation decisions rather than referring athletes to physicians after concussion.
Our study was limited by inherent restrictions associated with survey research. We expected that the respondents answered all questions honestly and accurately and interpreted each the same way. Given that explaining each question to each individual respondent was impossible, some of the variability in responses likely was due to this lack of complete understanding of the question. However, we provided our contact information to all participants so they could ask us any questions. In addition, we instructed participants to answer questions based on their recollection of experiences with concussions. It is likely many respondents did not remember all the details of every concussion they evaluated within the past year, possibly leading to skewed responses. Although similar to the response rate of 34% reported in 2005,1 our response rate of 33% was relatively low. This finding partly is due to e-mail addresses changing often and not always being updated in the NATA database, which likely accounted for a sizable percentage of surveys that were not completed. However, we believe our data accurately represent ATs because our corrected response rate was near the norm for similar Web-based survey research.24 In addition, given that we did not have access to the previous survey datasets,1,12 we could not perform statistical analysis to compare our data with previous data. Whereas we provided numerical comparisons, we cannot determine if these findings were different at this time. In addition, some of our respondents possibly were retired or not currently practicing, but they may have remained certified. If the respondent reported being certified, his or her responses were counted regardless of retiree status.
CONCLUSIONS
Our results suggest ATs continue to make progress when assessing concussions and formulating safe return-to-participation decisions after these injuries. These data also suggest clinicians need to continue to review current recommendations and guidelines about concussion management because in many areas they are still lacking. Educators also should be aware of the most current recommendations to ensure the information conveyed in a classroom setting is up to date and accurate, allowing students to eventually use the knowledge gained in a clinical setting. As computerized tests become more readily available to clinicians, the AT needs to remember that the most effective concussion management appears to come from the use of multiple tools. Researchers should continue to focus on concussion-assessment tools and methods that allow the clinician to make the best decision regarding the safety of the athlete.
REFERENCES
- 1.Notebaert AJ, Guskiewicz KM. Current trends in athletic training practice for concussion assessment and management. J Athl Train. 2005;40(4):320–325. [PMC free article] [PubMed] [Google Scholar]
- 2.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Clin J Sport Med. 2005;15(2):48–55. doi: 10.1097/01.jsm.0000159931.77191.29. [DOI] [PubMed] [Google Scholar]
- 4.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med. 2009;19(3):185–200. doi: 10.1097/JSM.0b013e3181a501db. [DOI] [PubMed] [Google Scholar]
- 5.McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frollo J. See where your state stands on concussion law. USA Football Web site. http://usafootball.com/concussion/see-where-your-state-stands-concussion-law. Published April 21, 2013. Updated June 2013. Accessed July 9, 2013. [Google Scholar]
- 7.Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 8.Guskiewicz KM. Postural stability assessment following concussion: one piece of the puzzle. Clin J Sport Med. 2001;11(3):182–189. doi: 10.1097/00042752-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Peterson CL, Ferrara MS, Mrazik M, Piland S, Elliott R. Evaluation of neuropsychological domain scores and postural stability following cerebral concussion in sports. Clin J Sport Med. 2003;13(4):230–237. doi: 10.1097/00042752-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Broglio SP, Macciocchi SN, Ferrara MS. Sensitivity of the concussion assessment battery. Neurosurgery. 2007;60(6):1050–1057. doi: 10.1227/01.NEU.0000255479.90999.C0. [DOI] [PubMed] [Google Scholar]
- 11.Broglio SP, Sosnoff JJ, Ferrara MS. The relationship of athlete-reported concussion symptoms and objective measures of neurocognitive function and postural control. Clin J Sport Med. 2009;19(5):377–382. doi: 10.1097/JSM.0b013e3181b625fe. [DOI] [PubMed] [Google Scholar]
- 12.Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36(2):145–149. [PMC free article] [PubMed] [Google Scholar]
- 13.Valovich McLeod TC. The value of various assessment techniques in detecting the effects of concussion on cognition, symptoms, and postural control. J Athl Train. 2009;44(6):663–665. doi: 10.4085/1062-6050-44.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCrea M, Kelly JP, Randolph C, et al. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13(2):27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36(3):263–273. [PMC free article] [PubMed] [Google Scholar]
- 16.Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48(3):581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 17.Cantu RC. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36(3):244–248. [PMC free article] [PubMed] [Google Scholar]
- 18.Brasfield K. Legislative requirement—concussion management plan—Effective August 16, 2010 [memorandum] Indianapolis, IN: National Collegiate Athletic Association; August 13, 2010. [Google Scholar]
- 19.Iverson GL, Brooks BL, Collins MW, Lovell MR. Tracking neuropsychological recovery following concussion in sport. Brain Inj. 2006;20(3):245–252. doi: 10.1080/02699050500487910. [DOI] [PubMed] [Google Scholar]
- 20.Iverson GL, Lovell MR, Collins MW. Validity of ImPACT for measuring processing speed following sports-related concussion. J Clin Exp Neuropsychol. 2005;27(6):683–689. doi: 10.1081/13803390490918435. [DOI] [PubMed] [Google Scholar]
- 21.McCrea M. Standardized mental status testing on the sideline after sport-related concussion. J Athl Train. 2001;36(3):274–279. [PMC free article] [PubMed] [Google Scholar]
- 22.Maroon JC, Lovell MR, Norwig J, Podell K, Powell JW, Hartl R. Cerebral concussion in athletes: evaluation and neuropsychological testing. Neurosurgery. 2000;47(3):659–669. doi: 10.1097/00006123-200009000-00027. [DOI] [PubMed] [Google Scholar]
- 23.Lovell MR, Iverson GL, Collins MW, McKeag D, Maroon JC. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9(4):193–198. doi: 10.1097/00042752-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Braithwaite D, Emery J, De Lusignan S, Sutton S. Using the internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20(5):545–551. doi: 10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]