Abstract
Little is known about how care providers’ perceptions of religion and genetics affect interactions with patients/parishioners. This study investigates clinicians’ and clergy’s perceptions of and experiences with religion and genetics in their clinical and pastoral interactions. An exploratory qualitative study designed to elicit care providers’ descriptions of experiences with religion and genetics in clinical or pastoral interactions. Thirteen focus groups were conducted with members of the caring professions: physicians, nurses, and genetics counselors (clinicians), ministers and chaplains (clergy). Preliminary analysis of qualitative data is presented here. Preliminary analysis highlights four positions in professional perceptions of the relationship between science and faith. Further, differences among professional perceptions appear to influence perceptions of needed or available resources for interactions with religion and genetics. Clinicians’ and clergy’s perceptions of how religion and genetics relate are not defined solely by professional affiliation. These non-role-defined perceptions may affect clinical and pastoral interactions, especially regarding resources for patients and parishioners.
Keywords: Clinician perceptions, clergy perceptions, religious beliefs, genetic services, resources, science/faith relation
INTRODUCTION
The vast majority of Americans espouse religious and spiritual beliefs, and these concepts permeate our cultural discourse. In addition, a great deal of attention has been paid to the roles that religious beliefs play for health care providers and patients, as both a source of solace and healing, or even as a reason to refuse to provide or to accept certain kinds of health care. At the same time, advances in science, and in particular genetics have achieved an iconic, if contested, status.
But while the intersections of religion and genetics, both compatible and in tension, have reached the public eye, relatively little attention has been paid to the ways these issues arise when clinicians, clergy, parishioners and patients are confronting specific genetic information. To shed more light on these interactions, we conducted 13 focus groups with “caring professionals” - physicians, nurses, genetic counselors, clergy, and hospital chaplains – exploring how they perceived issues surrounding religion and genetics and how those issues arose for them and for their patients. A large number of topics emerged in these conversations. In this paper, we present preliminary analysis of two important and related topics that emerged: 1) the relationship between science and faith and 2) participants’ perceptions of resources to help patients and parishioners navigate that relationship. Clinicians and clergy described the many ways issues of religion and genetics emerged from their professional experiences. In particular, participants offered four main descriptions of the relationship between science and faith, and they gave examples of the resources they would like to have and the resources they have discovered in their professional interactions. In describing and analyzing how professionals perceive these relationships and the resources needed and available we hope to deepen understandings of how clinicians, clergy, patients, clients and parishioners are working together.
BACKGROUND
People confronting genetic information are not simply patients, inhabiting roles defined by the structures and customs of the medical system and the perspectives of health care providers. Rather, they inhabit additional roles, as members of family, of social groups, and of religious groups. The layers of these roles can influence how people understand genetic testing, information, and medicine. For example, religious affiliation or faith can affect whether one sees the use of genetic testing as a scientific tool, as an illustration of God’s creation, or as an unwarranted human intervention, ‘Playing God’.
Patients understand and respond to the prospects and results of genetic testing using a complex set of psychosocial resources. Several studies suggest that religion is a factor that affects patients’ responses to genetic services. Most of these studies have reported how patients relate genetic information to religious beliefs in processes of interpretation, decision-making, and coping. Care providers, who bring their own beliefs and perceptions to clinical encounters, may also be a factor in patients’ responses to genetic services. Thus, it may matter if those to whom they turn for advice have differing perceptions of religion and genetics or differing perceptions of useful resources. Very few studies, however, have investigated the experiences of care providers and their perceptions of religion and medical genetics [Stuck et al., 2001]. Understanding these experiences and perceptions may improve communication in clinical encounters by identifying common concerns, clarifying unstated assumptions, and suggesting additional research and resources needed in the complex field of religion and genetics.
Significant work has been done on factors in patients’ responses to religion and genetics. Researchers have tracked variations in whether and how patients ascribe meaning or divine purpose to genetic conditions [Harris et al., 2004; Kinney et al., 2002; Pew Research Center, 2002; Turnbull et al., 2005]. Researchers have investigated the impact of religious beliefs on genetic testing for cystic fibrosis, breast cancer, and pulmonary arterial hypertension (PAH) and have explored how religious beliefs and practices influence knowledge of and decisions about genetic testing, particularly prenatal testing and abortion [Clayton et al., 1996; Furr and Seger, 1998; Lientz and Clayton, 2000; Pew Research Center, 2002; Press and Browner, 1998; Robert Wood Johnson Foundation, 2006; Schwartz et al., 2000; Singer et al., 2004]. Other studies have focused on racial or ethnic differences in how religious beliefs affect discussing and choosing genetic services [Harris et al., 2004; Kinney et al., 2002; Singer et al., 2004]. Others have focused on religious coping: the ways religion may function as a resource for patients coping with genetic conditions or risks [Harris et al., 2004; Kinney et al., 2002; Lientz and Clayton, 2000].While these studies provide important insights into patients’ experiences and attitudes, they represent only one part of the beliefs that influence these understandings and responses to genetic services and information. The experiences of clinicians and clergy, along with their patients, clients, and parishioners, are key locations for learning how religion and genetics intersect [Collins and Guttmacher, 2001; Collins and McKusick, 2001; Curlin et al., 2007; D’Onofrio et al., 1999; Reis et al., 2007]. Because care providers are often the first or primary patient source for genetic services and information, the care providers’ beliefs and perceptions of religion and genetics may have a profound impact on patient experiences.
METHODS
Over the course of three years, the Vanderbilt Working Group, a multidisciplinary team of ethicists, physicians, genetics counselors, nurses, and clergy members’ has explored the intersections of religion and genomics through theoretical and empirical investigations (received approval from the Vanderbilt University Institutional Review Board in November 2006). The Working Group began conducting focus groups with members of five ‘caring professions’ in the early months of 2007 [Glaser and Strauss, 1967; Hansen, 2006; Krueger and Casey, 2000; O’Dea, 1970; Press and Browner, 1998]. Our primary research problem was to learn how care providers described their perceptions of and experiences with religion and genetics. In this study, we approached care providers from five professions to learn 1) how they perceived issues of religion and genetics in their professional experiences and 2) how these perceptions affected the ways people seek, offer, and provider genetic services.
We conducted 13 focus groups with various members of the caring professions: physicians, nurses, and genetics counselors (referred to as ‘clinicians’ – Groups 3, 4, 5, 6, 8, 9, 10, 11, & 13) along with ministers and hospital chaplains (referred to as ‘clergy’ – Groups 1, 2, 7, & 12). Focus group participants were recruited in two ways. Religious advisors and clinicians were identified and solicited through investigator contacts and ‘snowball sampling’ [Hansen, 2006]. Because the genetic counseling profession is relatively small and the number of counselors locally was limited, we recruited additional participants through the American Society of Genetic Counselors. Genetic counselors from across the country participated in a series of telephone focus groups of 3 to 4 participants each. Informed consent was obtained before each focus group began, and each group lasted between 1.5 and 2 hours. Each focus group was moderated by a member of the Vanderbilt Working Group and observed by another member [Glaser and Strauss, 1967; Hansen, 2006].
All the moderator guides included a brief description of the study, a broad definition of spirituality and religion, a set of case studies, and a series of open ended questions [Glaser and Strauss, 1967; Hansen, 2006; Press, 2005]. The case studies described four situations where religion and genetics might interact: prenatal diagnosis, genetic testing of children, genetics and cancer, and predictive testing of Huntington disease (HD). In each semi-structured focus group, we asked a series of open-ended questions about how issues relating to religion and genetics shaped participants’ interactions with patients, clients, and/or parishioners. We invited participants to consider the case studies or their own experiences in reflecting on their answers.
We asked clinicians about their perceptions of and experiences with religion and health concerns in general and with issues raised by genetics in particular (See Table I).
Table I.
Focus Group Questions
Questions for Clinicians:
|
Questions for Clergy:
|
We asked the clergy similar questions but with the aim of learning how they perceived the impact of genetic and broader medical concerns on their parishioners and their relationships with parishioners. Some participants focused on the case studies in their responses, and others told stories from their own experiences. Each focus group was recorded, transcribed, and all research participant identifiers were removed [Glaser and Strauss, 1967; Hansen, 2006; Press, 2005]. Prior to analysis, the focus group transcripts were reviewed for accuracy. Investigators used content analysis and constant comparison to code the data and develop themes, [Ayres et al., 2003; Coffey and Atkinson, 1996; Glaser and Strauss, 1967; Hansen, 2006; Press, 2005]. We used over 30 distinct topics, which emerged from the language of our focus group participants, as codes to organize and analyze our data. Three readers performed initial coding to ensure reliability [Glaser and Strauss, 1967; Hansen, 2006; Press, 2005].
RESULTS
Relationships and Resources in the Caring Professions
Focus group participants framed their discussions about religion and genetics in a variety of ways, often using broader domains like science and religion or medicine and spirituality. When moderators introduced questions about genetics and religion or spirituality, participants used genetics, medicine, and science interchangeably for the former, and used religion, spirituality, and faith for the latter. For clarity and ease of presentation, the discussions below are framed in terms of the science/faith relation.
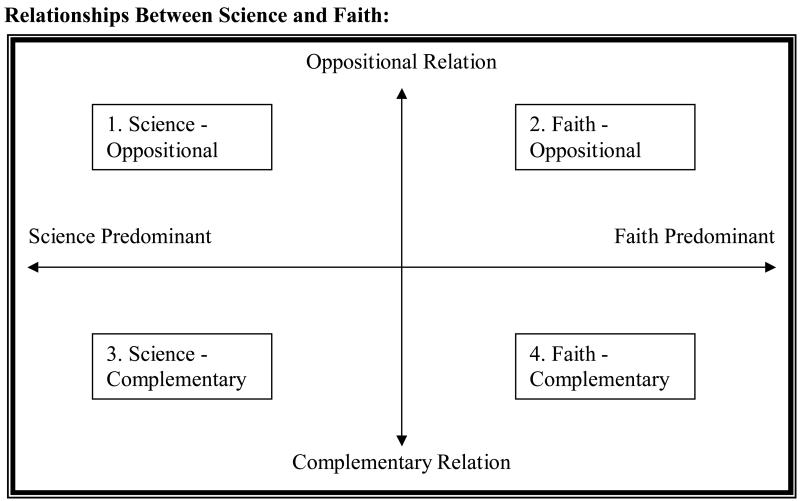
Preliminary analysis identified multiple ways in which clinicians and clergy encounter religion and genetics in their professional roles. One of our preliminary findings was that participants’ perceptions of the relationship between science and faith affected what they saw in terms of availability of or need for resources regarding religion and genetics. In particular, participants in each focus group reflected on how the two domains of science and faith related to or influenced one another and what resources they needed or used to navigate these relationships. Some participants described areas of tension in the science/faith relationship that often led to discussions of needed resources for religion and genetics. Other participants described points of connection and complementarity between science and faith that led to discussions of the resources clinicians and clergy have used to help their patients and parishioners. In the sections below, we will map out the four main relationships between science and faith, based on descriptions from focus group participants. We will also present the descriptions of what resources were needed by whom and what resources were available and to whom.
Perceptions of the science/faith relation fell along two axes, with four main positions emerging from the data. The first axis illustrates a spectrum of whether faith or science carries more substantive weight in respondents’ descriptions of their experiences. Substantive descriptions illustrated how faith or science affected people’s lives and often came with concrete normative claims for action and belief. For example, some clergy and self-disclosed “believing” clinicians explained that faith provided meaning, guidance, and the structure of their experiences. Science, on the other hand, was viewed in a functional way – it was a tool or technique that could further or hinder the goals or practices of faith. Other participants described the substantive influence of science while assigning faith a functional value – science explained, ordered, and shaped their experiences, while faith was a tool or technique that could further or hinder the goals or practices of science in general and medicine in particular. Participants generally gave either science or faith priority in negotiating the intersections of religion and genetics. The second axis illustrates the spectrum of relationships between science and faith – from an oppositional, either/or relationship to a complementary relationship. For some participants, either science or faith provided an accurate worldview and guide for action: as substantive domains, they were incompatible. Others saw a ‘different but complementary’ relation between science and faith: each domain contributed to and benefited the other in interactions with patients, clients, and parishioners.
At the intersections of these axes, participants described four key positions regarding the relationship between science and faith. The four positions help illustrate the ways clinicians and clergy talk about their experiences with religion/faith and genetics/science in their professional roles. Further, preliminary analysis shows a connection between how professionals perceive the relationship between science and faith and how they perceive the need for or availability of resources for patients and parishioners. In the following sections, we will describe the four key positions (Science-oppositional, Religion-oppositional, Science-complementary, and Religion-Complementary) and will end by indicating the connection between these positions and perceptions of resources for religion and genetics.
Position 1: Science – Oppositional
The position designated “Science-Oppositional” emerged in several focus group discussions, and most of its proponents were clinicians. This perceived relationship between science and faith was not explicitly identified by participants, but rather took shape as people described contentious or negative interactions between science and faith. Participants described religion or faith negatively: science, by contrast, appeared positively.
While science is only implicitly described as a positive in this position, faith or religion is explicitly described in negative terms and by negative stories. In the stories clinicians told about their experiences, the goals and practices of medicine and science constantly battled interference and opposition from the religion and faith of patients and from other clinicians. Clinicians with a “Science-Oppositional” stance told stories of how patients’ faith interfered with the clinicians’ ability to provide appropriate care. One family, for example, did not tell their surgical or nursing team about the patient’s genetic condition because the family believed their prayer had cured the condition. The family’s reasoning, and the genetic condition itself, came to light only after the patient died in surgery. The nurse telling this story expressed frustration with this and similar conflicts between belief and medical recommendations (R8-1).
Other clinicians told stories of religious leaders who negatively influenced their parishioners regarding medical or genetic issues. Clinicians told stories of clergy who walked out on patients for not having enough faith, and patients who refused medical testing or treatment as contrary to God’s will. One genetic counselor told us about an experience that haunted her years after it occurred. She said,
I can remember a case that was horrible because the minister and the whole group of faith actually walked out on the woman because the baby was… born with the problems that they’d all been praying for the miracle… and they actually walked out on her and told her… She didn’t pray hard enough and believe hard enough and that’s why the baby still had the problem and then they, literally, walked out on her. She just about had a nervous breakdown because she lost her whole support system… That is the worst one I was ever involved in. -- Genetic Counselor (R3-1)
This story illustrates some of the sharpest tensions clinicians encounter with religion. Another set of negative interactions emerged from stories nurses told about religious leaders’ operating as obstacles for diagnosis or treatment. For example, one nurse expressed frustration with some pastors “of some of these churches, they sort of reinforce some of the beliefs that people don’t really have any control over their destiny, so to speak. You know, if it’s God’s will it’s going to happen” (R8-2). This nurse, and others, viewed some pastors as “holding onto power” and influence over their parishioners to the detriment of patient understanding and to the care the nurses offered.
Further, in the “Science – Oppositional” position, clinicians described the limitations personal faith placed on providing clinical care. Clinicians in religiously affiliated hospitals reported limitations on the topics they could raise or referrals they could make. One counselor described a situation where a colleague’s beliefs made interactions difficult. She explained,
“I worked with only one clinician that it was sort of abundantly clear to everyone exactly what his beliefs were. It was a geneticist, and he was very pro-life, and the only time that it was ever really any kind of an issue was if we had a prenatal diagnosis of, you know, Down syndrome or Trisomy 18. If the family was considering termination, he wouldn’t speak with them about it. He would kind of outline all the medical things, and then say, ”And if you need to talk about termination, I’d see our genetic counselor here.“ And then I just would kind of feel like—it was kind of like ”And if you want to talk about termination, here’s Satan to talk to.“ You know? (R5-1)
As one genetics counselor explained, she has difficulty at times in explaining the goals of genetic testing to clients: they equate genetic testing with abortion because ”a physician has said, ‘Well, if you don’t want to terminate, then you don’t need an amnio(centesis)’“ (R5-1). The beliefs of one clinician can hamper the ability of another to fulfill his or her professional role.
Another genetics counselor pointed out the difficulties of working for a religiously affiliated hospital. She explained,
Our office has actually been threatened, in the past, to be shut down by some of the higher-ups and higher authorities because of discussions about termination and so technically, we’re not allowed to bring up the issue of termination with patients, and it is a big challenge in my job here, because I’m always kind of—have a fear in the back of my mind that I might lose my job (R3-2).
Several clinicians brought up similar concerns about the way religion/faith may limit or interfere with science/medicine, particularly in religiously affiliated hospitals and in typically conservative areas of the country, such as the ”Bible Belt“ in the Southeast. All but one clinician focus group had participants whose stories and descriptions of their experiences fell into the position of ‘Science-Oppositional’, describing negative interactions between faith and science or between religion and genetics.
Finally, not every clinician told negative stories about religion. For some, in the weakest version of the ”Science-Oppositional“ position, religion was described as irrelevant and inappropriate to a clinical setting. For example, one clinician talked about the difficulty she faced being non-Christian in the South, with a mostly Christian population, and her discomfort when her patients asked her about her faith. She said ”I don’t know what to say and I consider myself an atheist now and nobody’s going to accept that. They’re going to try to convert me and I don’t want to hear it.“ (R4-3). Rather than seeing the faith and science relationship as potentially harmful, this clinician and others found faith in the clinic to be more of a nuisance. These clinicians talked about religion as being personal or private, not something they wanted to discuss or bring up with patients or clients.
While most of the proponents of the ”Science-Oppositional“ model were clinicians, not all clinicians held this model, as we shall see below. In this model, science was described as rational, ”absolute“, and was characterized by an implicit assumption that science is ”real“ or describes ”reality,“ especially regarding medical care or even genetic diagnosis. In contrast, these participants did not see faith activities and beliefs as changing the realities of disease or diagnosis, though they may change the experience for an individual or family. Science and medicine were unquestioned as to their efficacy and practices – the questions that emerged about science focused around how scientists and clinicians could best navigate or manage conflicts with faith or religion.
Position 2: Faith-Oppositional
The second position – entitled ”Faith-Oppositional“ – emerged as both clergy and self-disclosed ‘believing’ clinicians described the relationship between science and faith. For these clergy and clinicians, religion/faith had personal significance as one’s denomination or faith tradition, a community of support, activities like prayer, or trying to discern what it means to live ”this side of the Promised Land“ (R1-1). Participants described experiences where faith or religion positively influenced interactions with patients, clients, or parishioners. Even so, participants in this group described an overall picture where science and faith were in contention or in opposition.
Both clergy and ‘believing’ clinicians described the ways personal faith determined their choice of profession and their interactions with parishioners or patients in medical or genetics situations. For some clinicians, personal faith directed career choice and employment locations. For example, one participant described his Christian medical practice saying, ”It’s really an opportunity to minister. It’s really an opportunity to live out our mission statement. Reflect on the loving compassion of Jesus Christ.“ (R13-4). Or, as another member of the same practice explained, ”with new patients, I basically say, you know, we’re here at this clinic because we love Jesus Christ and I just want you to know that I’m happy to pray with you or if you ever need to pray in the future“ (R13-2). Personal faith directed these clinicians towards their medical profession and towards their unique practice.
In another example, one genetic counselor explained that she chose to work in a Catholic hospital because its policies against discussing or providing abortions allowed her to do her job without challenging her beliefs. She explained,
When I first came out of grad school, I probably would not have worked in prenatal unless I was at a Catholic hospital, and it’s interesting that in my two years of working at a Catholic hospital, my attitudes have changed a little bit. More understanding of circumstances in which termination is considered by families. But I knew, going in to my job that that was kind of the restrictions that were placed on people who worked there. (R3-2)
Knowing the restrictions a religious institution had on discussing abortion in the context of prenatal genetic testing allowed this genetic counselor to work in prenatal care. This example highlights the ways personal religious beliefs can influence professional roles and even choice of employment. According to focus group participants, it can also influence how they see the relation between faith and science.
Most participants who articulated this ”Faith-Oppositional“ position highlighted one of three areas of contention between faith and science. In the first area, participants criticized science for not asking the ‘big questions’ about creation or the meaning of existence. For example, one genetics counselor with an “active religious life” explained that her colleagues wouldn’t even address certain questions about science and faith. She said,
they will not concede the point that you could be a good scientist without believing in evolution. And so they would say, well, you’re just good in one field only but you’re not a real scientist or you’re not really following the science. But if you want to address the actual evolution question, I don’t see that those particular people are open to debate it openly because they have certain words that they use for their debate which are full of closing off words rather than opening the debate words. (R3-3).
From this clinician’s experience, she felt that her fellow scientists and clinicians disregarded her opinions and that she “got classified as ‘she’s close-minded, right wing negative, and anti-thinking, anti-science, anti-rational…’” Her sense of alienation also illustrates the second major area of contention between science and faith: the sense that science imposes itself on or disregards the faith of patients and even other clinicians.
Many clergy members reported that clinicians often overemphasized the negative aspects of genetic conditions and were hostile to religion: clinicians “overlooked the importance of religion and faith in the patient’s interpretation of the information” (R2-2). This negative emphasis caused tensions because for many clergy and their parishioners religion was significant as a way of “creating or making meaning” (R7-3) in health-related situations. One minister explained, “I think too many times the medical community ah, obviously their challenge is to preserve life, save life and now that genetics is involved, design life and these options you know, really don’t take into consideration some life experiences” (R2-1). He went on to describe the blessings a child with Down syndrome had brought to a parishioner’s life, noting “maybe the medical community too, overlooks those kind of examples for people in these situations.” Or, as another participant in that focus group explained his concerns,
Here we are and I don’t know where that line is but I want the right to not to have imposed on me everything the medical community discovers…I want to have the right to say no and still be thought of as a sensible human being and I fear so much of that you know, with the medical thing (R2-2).
He was anxious and angry that the goals of science and medicine might override his faith and goal of “seeking God’s way in your life.” In a similar vein, one genetic counselor noted that “we, genetic counselors and the profession, are very accepting of different opinions and, and, ah, the religious beliefs in our patients but for our colleagues and other genetic counselors within our profession, we are not accepting” (R3-3). Much of the contention about faith and science centered on this perceived imposition of science on persons of faith and the ways the scientific perspective disregarded faith.
The final area of opposition between science and faith concerns the practices of science and medicine in general and genetics in particular. Several participants described particular scientific and medical practices as immoral and in conflict with faith perspectives. For example, several participants talked about the dangers of prenatal testing because it would lead to abortion. One participant asked about the motivations for testing and whether people test to decide about abortion. He argued, “I don’t think genetic testers are testing with love or moral and ethical principles from what I’m hearing. Seemingly. It’s that when you start testing, you’re gonna find all kinds of no reasons for anybody to be here” (R12-1). Other participants made a direct leap from discussions of genetic testing to genetic manipulation as immoral uses of science and as points of conflict between science and faith. One participant observed, “And I see, without parameters, this genetic trend becoming you know, designer babies and the super athlete and we just tweak these genes so I think saying to the person, we can make your baby perfect is a dangerous option for people” (R2-2). Participants acknowledge the potential benefits from science and genetic technology, as we shall see in position 4 below, but they were also uncomfortable with the motives and methods for implementing them.
Position 3: Science – Complementary
The third position “Science – Complementary” is characterized by descriptions that viewed science and faith as complementary domains, even when participants prioritized or focused on science. These descriptions focused on the usefulness of religion or faith in clinical care – faith as supplementing science or helping science to achieve its goals. Both clinicians and clergy gave several kinds of examples of how religion or faith could help medicine or science in the interactions with patients, clients, and parishioners.
In the first kind of example, participants talked about religion or faith as providing a lens for interpreting genetic information. In particular, they described patients who used ideas like God’s will or divine providence to explain the presence of their genetic or medical conditions, as well as the consequences or outcomes of those conditions. As one clinician explained,
Religion, or religious faith, helped them sort of make peace with the situation, or helped them to develop some sense of meaning; Regardless of origin, whether it’s a congenital defect or an acquired issue…make sense of that, making sense of the tragedy is hard to do, and sometimes, at least in my population, I would guess…that assigning things divine attribution is really the only way to make peace with the situation. (R6-1)
Another participant gave a more specific comment about God’s will regarding the prenatal diagnosis of Down syndrome. This minister noted,
Well God is sovereign in this and that you know, if it’s His Will then He will work it out. The verse says, you know, all things work together for good so even if there is a Down syndrome baby (sic) here, which if you’re like one of our church members, it can be a blessing, I mean. (R2-2).
The theological understanding of God’s will allowed this participant to explain and respond to the possibilities raised by prenatal diagnosis and genetic testing.
A second set of examples revolved around coping – faith was useful because it provided a mechanism for coping with genetic and medical issues. Clergy in this group described the positive impact of prayer, church attendance, and communal discernment in responding to genetic or medical situations. Faith is useful in clinical interactions because it helped patients cope with potentially devastating diagnoses or medical situations. Describing a similar position, clinicians in this group explained that they often brought in or welcomed clergy to discussions with patients and families. In particular, some clinicians raised the importance of religious hope in their patients’ experiences: several nurses described faith as having a positive impact on clinical encounters. They described their patients’ faith as providing ways of “coping” and “hoping.” As one respondent explained, for patients, “if there’s hope, then it gives a different perspective on how you view a crisis then if there were no hope” (R6-3). Other participants described hope as evolving with additional information or with the experience of the condition. One nurse explained hope as “dynamic, and it evolves and is fluid. It goes in many different directions” (R6-3). From the perspective of these clinicians and clergy, faith and religious hoping helped patients cope with genetic diagnosis and with other health crisis in positive ways.
Finally, focus group participants gave examples of complementary interactions between science and faith that centered around the pragmatic benefits or effects of faith on clinical care. Clinicians and clergy described science and faith as complementary because faith was useful to science or to clinical interactions. Participants described how their personal faith, as well as the faith of patients and parishioners could encourage people to accept genetic or other medical testing, and often helped promote compliance with medical advice. A group of Christian clinicians talked about the benefits of their faith-based view of the patient and their clinical practice. One of these clinicians explained that their practice had
a very unique environment where we’re able to, … to deliver health care with a different view, with a different view of the patient. With what I would consider to be more eternal view of the patient as opposed to simply a temporal view or even an encounter view. (R13-1)
Faith directly influenced how professionals viewed their interactions with patients and parishioners. A similar perspective emerged when another clinician told us that she took a moment to herself to pray before meeting with each client. She said, “I would pray for my patients, and I just saw a dramatic change in my ability to help them figure out what they wanted and go forward” (R5-2). Personal faith also affected what religious activities and communications participants saw as acceptable in the clinical setting. For example, one genetic counselor at a Catholic hospital talked about a nun who was on call to talk to families. She explained,
If we have an anomaly or a miscarriage or whatever, just call her [the Sister] and she’ll come over without asking the patient first, because her reason is that that’s the way they do it in the hospital for in-patients, is that they have the chaplain come, and then if they get to the patient and the patient says, “No thank you,” then they’re done and that’s fine, but she said, “If you ask people ‘Do you want us to bring a chaplain over?’ they’ll just say no, even if they might, later on, wish they’d said yes, or might derive some benefit from it.” (R3-1)
For this clinician, the religious perspectives and services provided by the nun helped her counsel her clients. In each of the examples above, these clinicians emphasized the ways their personal faith assisted them in their clinical or professional roles.
Other clinicians discussed how patients’ faith could be useful in achieving clinical goals. Science and faith are not necessarily opposed because faith is ‘useful’ to both patients and clinicians. One group of participants talked about using religious or faith language with religious patients. She explained,
Speaking the cultural language that they choose to use … If I’m a faith-based person, and I say, “Well, yes, you have your strong faith; the Lord has given us these tests to use to help you,” and that helps someone get tested, no: I don’t see that as being unethical. And to me, to be stoic and only say, “Well, this is just how science is, and you need to do this scientifically” … You know you’re alienating them, because they don’t believe in that way, so why alienate folks? Why not bring more people in, using whatever cues you have to use?(R8-1)
Some participants were concerned, however, about manipulating patients by ‘using’ faith as a “tool or a ploy” (R6-3), and even gave examples of how some language was manipulative and inappropriate. One participant observed “When it gets unethical is when you say, ‘If you don’t take advantage of this, God’s going to send you to hell’” (R8-4). She noted the distinction between the utility of faith in clinical care as a good practice and as a potentially harmful manipulation. For other participants, using religious language was a way of “meeting patients on their path” (R6-2) and as the nurse quoted above asks, “why not bring more people in using whatever cues you have to use?” (R8-1). This theme exemplifies the complex negotiations clergy and clinicians face regarding the relation between science and faith in their experiences, for health care in general and genetic medicine in particular.
Position 4: Faith-Complementary
The fourth and final major position, “Faith-Complementary” emerged as participants articulated the many ways science or medicine or even genetics in particular served or benefited the faith of professionals and their patients, clients, and parishioners. The focus and priority remained with faith or religion, and participants described how they used science or medicine to support or share their personal faith. For example, in one focus group, a genetic counselor talked about bringing her genetic knowledge to illuminate her Bible study class, particularly on issues of consanguinity and marriage laws from Leviticus. She explained,
It’s kind of interesting to see where the genetics come in and I enjoy doing that and I think, you know, people in a study group like that enjoy hearing that angle because they all have this idea that through religion all is science, you know. People always say versus or “Or” like it’s one or the other so it’s very nice whenever I can, to try and integrate them (R3-3).
Her training and background in genetic counseling brought new insights to her faith community.
Similarly, one group of pediatricians talked about using their medical practice as a way of ministering to the community – their presence and the services they provided allowed them to witness to peoples’ spiritual lives as such as they care for peoples’ physical needs. One participant from this group explained,
But you have the opportunity … to speak into their life. And so whether the issue is, is simply a standard health care issue or social issue, or a genetic issue, that relationship that you cultivate over time is, I would say, paramount, probably the most important thing that actually allows you to speak into their lives (R13-1).
Their medical practice allows these practitioners to live out and share their Christian principles with the local community.
Several clergy groups talked about the ways science complemented and illuminated aspects of creation – science provided a window into God’s works.
God has given us glimpses into Creation. God has given us the curiosity to discover things, and I’m just convinced that is not an accident; that’s a part of who we are as human beings, and far from destroying an understanding of God, when we become more and more aware of, in my words, how God created us, I think it enhances our wonder at God’s creativeness. I mean, it enhances—the more we understand about the genome, for instance, the more we marvel at God’s Creation, so that would be my approach, that I think God smiles when we discover a new genetic marker. I think God is not threatened by our knowledge. (R1-3).
As one chaplain explained, science itself was a gift from God that allowed human minds to understand the wonders of creation or the natural world.
Finally, some clergy talked about the importance of science for bringing families and communities closer together. In these examples, participants talked about genetic testing as providing helpful information and strengthening peoples’ faith. For example, when prenatal testing reveals a genetic abnormality like Down syndrome, the clergy talked about it as an opportunity to connect that couple with other families of faith who have similar experiences. One minister explained, “We need to introduce folks in these situations, I think, to other people’s life experiences who have gone through this and it didn’t…yes it’s troubling and it’s difficult but it’s not devastating. It becomes a blessing in God’s family…” (R2-2). The information gathered from genetic testing and medical interventions can help connect believers with others in the faith community.
Opposition – Resources Needed:
In the first two positions, ‘Science-Oppositional’ and ‘Faith-Oppositional’, participants described a tension-filled relationship between science and faith, and participants in both categories commented on the lack of resources for engaging these tensions. Participants described difficult encounters and expressed concern about the lack of available resources. This preliminary analysis raises several questions for further research. How do these factors contribute to one another? Does an oppositional view of the science/faith relation mean professionals are less likely to see available resources? Or does a lack of resources lead to an oppositional view of the relation between science and faith? Finally, what resources do these professionals describe as needed and absent? Although the former questions require more research, the last question was asked in each focus group.
The ‘Science-Oppositional’ group generally wanted information on the beliefs of different faiths or religious denominations. Many participants told stories of conflict that stemmed from misunderstanding differences in denomination or faith tradition. They cited examples of Muslim birth practices and the Jehovah’s Witness’s avoidance of blood products to illustrate their need for more information about other faiths. Participants expressed a hope that such information would help navigate the difficult situations they encounter. They asked for more information and more training in helping people cope with genetic diagnosis. As one nurse explained,
I think for healthcare professionals in general, and social service professionals, there needs to be baseline understanding of how to do “psychological first aid,” how to attend to spirituality… We’re never going to have enough clergy available to deal with the everyday kinds of spiritual issues…(R8-3).
Participants in the “Science-Oppositional” category wanted resources that would help them understand, learn about, and respond to patients with unfamiliar faith traditions. While many clinicians cited a need for more educational resources on specific religious beliefs, particularly those beyond mainline Christianity, they also noted the limitations of relying on those materials. They explained that in their experiences with families, personal beliefs often carried more weight than denominational or doctrinal positions (R8-2).
Participants in the “Faith-Oppositional” group, on the other hand, focused on the need for information and training in genetic issues. They wanted to learn how to ‘translate’ information about genetic testing, options, and diagnosis for laypersons. In this group, the clergy participants also wanted to connect people with genetic diagnosis to other people with the same diagnosis – preferably people of faith who could help them cope with their experiences. Finally, participants from both ‘oppositional’ positions wanted to know when and where to send their patients, clients, and parishioners for additional help when religious questions or science questions were beyond the capabilities of the particular professional to address.
When asked what kind of resources they would like or could imagine being helpful, participants from both ‘oppositional’ stances identified support groups, publications, or reference materials on the Internet as well as professional development programs such as cultural competency training, continuing medical education, and clinical pastoral education. Participants from each focus group indicated a desire for more educational resources on genetics for non-specialists and reported the desire among their patients, clients, and parishioners for resources to help make sense of new and changing genetic options and information.
Complementary – Resources Available
Participants who described the relationship between science and faith as complementary described a number of available resources regarding religion and genetics. They saw mutually beneficial relationship between science and faith, between religion and genetics, and they easily identified available resources for patients and parishioners. There were several areas of overlap between clergy and clinicians. For example, ministers reported using physicians in their congregations as resources for learning about genetic conditions and as an authority for counseling their parishioners. As one minister explained,
[It] was a comfort to me because I could tell just the families, look, I‘ve got a friend who’s a physician, and here’s what he would do. And it’s that kind of thing, that kind of knowledge, you know, you’re coming from a position… so it’s not just my opinion…it’s a guy who really understands medicine but he also believes that God is at work. (R 2-1)
Some clinicians embraced religion and religious issues as they provided patient care. They publicly disclosed their own faith and invited patients to do the same. These clinicians reported that “acknowledging religion as a resource opens conversational doors” (R10-1) with families. Similarly, health care professionals reported using chaplains as resources in patient care. One genetic counselor, described above, worked with a nun at a Catholic hospital to help counsel patients. Several physicians and genetics counselors reported working closely with hospital chaplains.
Clinicians and clergy also reported that their patients and parishioners found resources within their religious communities, including clinicians in those communities. Several care providers cited the Internet as another resource accessed by patients and parishioners although they raised concerns about the reliability of this information source. Clinicians worried about patients encountering misinformation about the scientific aspects of genomics, particularly from websites. Clergy, on the other hand, worried parishioners would find “misinformation and scare tactics” about genetic disorders that might lead to abortions (R2-2). Focus group members reported that their patients and parishioners wanted more accurate and understandable information, and wanted the opportunity to discuss concerns about religion and genetics with knowledgeable people and people of faith.
CONCLUSION
A key finding from our preliminary analysis is that the ways participants described the relationship between science and faith or between religion and genetics was related to how they perceived the need for or availability of resources. Participants with a view that science and faith were in tension described a lack of resources and a sense of uncertainty about navigating the intersections of religion and genetics in their professional experiences. On the other hand, participants with a view that science and faith were complementary saw fewer conflicts between religion and genetics, and easily perceived available resources for their patients, clients, and/or parishioners. Perceptions of the science and faith relation are closely related to perceptions of resources for navigating that relation.
Though this data and these findings are preliminary, they also indicate that clinician and clergy perceptions of religion and genetics are not easily characterized. There were no clear lines drawn among groups or even between the broad categories of ‘clinician’ and ‘clergy’. The most important practical finding in this preliminary data is the perceived lack of resources described by some clinicians and some clergy. In spite of the professional, academic, and media coverage of genetic issues and even issues of religion and genetics [Anderson, 2002; Chapman, 1999; Cole-Turner, 1993; Collins and Guttmacher, 2001; Pew Research Center, 2002; Reiset al., 2007; Smith and Cohen, 2003; Stucket al., 2001; van Biema, 2006], some clinicians and clergy feel unprepared for responding to issues of religion and genetics when working with those they tried to serve. They are looking for more education and more resources in their professional interactions, and participants mentioned specific forums (e.g., CPE or CME) that could fulfill those needs.
The preliminary analysis mapped above illustrates two starting points for future analysis and research. First, perceptions of how science and faith or religion and genetics relate and interact are very complex and do not always follow professional divisions or lines. These non-role-defined perceptions may affect clinical and pastoral interactions, especially regarding resources for patients and parishioners. Second, the domains of science and faith, or religion and genetics that coexist and interact in the experiences of many professionals are often sources of tension or conflict for professionals. Further research will investigate how professionals use various resources to navigate those tensions and to improve the care they provide to patients, clients, and parishioners. A major challenge for our study and for future research will be in finding ways to pay attention to how professionals’ perceptions of religion and genetics affect their experiences, in finding ways to develop resources for professionals, and in finding ways to get those resources to the professionals who help patients, clients, and parishioners confront religion and genetics.
Figure 1.
Science and Faith
ACKNOWLEDGMENTS
The authors would like to thank Joe Fanning, PhD and Ellen Wright Clayton, MD, JD, for their invitation to join the project, as well as for their support and diligence throughout the process. We would also like to thank Jill Fisher, PhD for her helpful comments. We gratefully acknowledge the support and funding from the Vanderbilt University Center for the Study of Religion and Culture, and the Center for Biomedical Ethics and Society at Vanderbilt University. The opportunity to present this paper was supported by conference grant 1 R13 HG004689-01 from the National Human Genome Research Institute.
Biography
Virginia L Bartlett, MTS is a Clinical Ethics Fellow at the Center for Biomedical Ethics and Society at the Vanderbilt University Medical Center and a graduate student in Vanderbilt University’s Graduate Department of Religion. Her research interests include religion and the moral experience of women in relation to reproductive technologies, maternal-fetal medicine, and genetics.
Rolanda L. Johnson, PhD, RN is an Assistant Professor in Vanderbilt University School of Nursing. With the goal of understanding health behaviors of African Americans, Dr. Johnson’s research interests are African American perceptions and beliefs about genetics and health.
Contributor Information
Virginia L Bartlett, Center for Biomedical Ethics and Society, Vanderbilt University Medical Center Vanderbilt University Graduate Department of Religion.
Rolanda L Johnson, Vanderbilt University School of Nursing.
REFERENCES
- Anderson RR. Religious Traditions and Prenatal Genetics Counseling. 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres L, Kavanaugh K, Knafl KA. Within-case and across-case approaches to qualitative data analysis. Qual Health Res. 2003;13:871–883. doi: 10.1177/1049732303013006008. [DOI] [PubMed] [Google Scholar]
- Chapman AR. Unprecedented choices: religious ethics at the frontiers of genetic science. ix. Fortress Press; Minneapolis: 1999. p. 261. [Google Scholar]
- Clayton EW, Hannig VL, Pfotenhauer JP, Parker RA, Campbell PW, 3rd, Phillips JA., 3rd. Lack of interest by nonpregnant couples in population-based cystic fibrosis carrier screening. Am J Hum Genet. 1996;58:617–627. [PMC free article] [PubMed] [Google Scholar]
- Coffey A, Atkinson P. Making sense of qualitative data: complementary research strategies. x. Sage Publications; Thousand Oaks: 1996. p. 206. [Google Scholar]
- Cole-Turner R. The New Genetics: Theology and the Genetics Revolution. Westminster/John Knox; Louisville, KY: 1993. [Google Scholar]
- Collins FS, Guttmacher AE. Genetics Moves in the Medical Mainstream. Journal of the American Medical Association. 2001;286:2322–2324. doi: 10.1001/jama.286.18.2322. [DOI] [PubMed] [Google Scholar]
- Collins FS, McKusick VA. Implications of the Human Genome Project for Medical Science. Journal of the American Medical Association. 2001;285:540–544. doi: 10.1001/jama.285.5.540. [DOI] [PubMed] [Google Scholar]
- Curlin FA, Lawrence RE, Chin MH, Lantos JD. Religion, conscience, and controversial clinical practices. N Engl J Med. 2007;356:593–600. doi: 10.1056/NEJMsa065316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio BM, Eaves LJ, Murrelle L, Maes HH, Spilka B. Understanding biological and social influences on religious affiliation, attitudes, and behaviors: a behavior genetic perspective. J Pers. 1999;67:953–984. doi: 10.1111/1467-6494.00079. [DOI] [PubMed] [Google Scholar]
- Furr LA, Seger RE. Psychosocial predictors of interest in prenatal genetic screening. Psychol Rep. 1998;82:235–244. doi: 10.2466/pr0.1998.82.1.235. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. x. Aldine; New York: 1967. p. 271. [Google Scholar]
- Hansen EC. Successful Qualitative Health Research. Allen and Unwin; Sydney: 2006. [Google Scholar]
- Harris TM, Parrott R, Dorgan KA. Talking about human genetics within religious frameworks. Health Commun. 2004;16:105–116. doi: 10.1207/S15327027HC1601_7. [DOI] [PubMed] [Google Scholar]
- Kinney AY, Emery G, Dudley WN, Croyle RT. Screening behaviors among African American women at high risk for breast cancer: do beliefs about god matter? Oncol Nurs Forum. 2002;29:835–843. doi: 10.1188/02.ONF.835-843. [DOI] [PubMed] [Google Scholar]
- Krueger RA, Casey MA. Focus groups: a practical guide for applied research. xvi. Sage Publications; Thousand Oaks, Calif.: 2000. p. 215. [Google Scholar]
- Lientz EA, Clayton EW. Psychosocial Implications of Primary Pulmonary Hypertension. American Journal of Human Genetics. 2000:59. [Google Scholar]
- O’Dea TF. Sociology and the study of religion; theory, research, interpretation. x. Basic Books; New York: 1970. p. 307. [Google Scholar]
- Pew Research Center . Public Makes Distinctions on Genetic Research. 2002. [Google Scholar]
- Press N. Qualitative research: thoughts on how to do it; how to judge it; when to use it. Genet Med. 2005;7:155–158. doi: 10.1097/00125817-200503000-00001. [DOI] [PubMed] [Google Scholar]
- Press N, Browner CH. Characteristics of women who refuse an offer of prenatal diagnosis: data from the California maternal serum alpha fetoprotein blood test experience. Am J Med Genet. 1998;78:433–445. [PubMed] [Google Scholar]
- Reis LM, Baumiller R, Scrivener W, Yager G, Warren NS. Spiritual assessment in genetic counseling. J Genet Couns. 2007;16:41–52. doi: 10.1007/s10897-006-9041-8. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation . Public Opinion Survey Finds Racial and Ethnic Differences Regarding Genetic Testing. 2006. [Google Scholar]
- Schwartz MD, Hughes C, Roth J, Main D, Peshkin BN, Isaacs C, Kavanagh C, Lerman C. Spiritual faith and genetic testing decisions among high-risk breast cancer probands. Cancer Epidemiol Biomarkers Prev. 2000;9:381–385. [PubMed] [Google Scholar]
- Singer E, Antonucci T, Van Hoewyk J. Racial and ethnic variations in knowledge and attitudes about genetic testing. Genet Test. 2004;8:31–43. doi: 10.1089/109065704323016012. [DOI] [PubMed] [Google Scholar]
- Smith DH, Cohen CB. A Christian response to the new genetics: religious, ethical, and social issues. xiv. Lanham, Md.: Rowman: 2003. p. 190. [Google Scholar]
- Stuck J, Faine J, Boldt A. The perceptions of Lutheran pastors toward prenatal genetic counseling and pastoral care. J Genet Couns. 2001;10:251–263. doi: 10.1023/a:1016680425337. [DOI] [PubMed] [Google Scholar]
- Turnbull J, Lohi H, Kearney JA, Rouleau GA, Delgado-Escueta AV, Meisler MH, Cossette P, Minassian BA. Sacred disease secrets revealed: the genetics of human epilepsy. Hum Mol Genet. 2005;14(Spec No. 2):2491–2500. doi: 10.1093/hmg/ddi250. [DOI] [PubMed] [Google Scholar]
- van Biema D. God Vs. Science. Time Magazine. 2006:168. [PubMed] [Google Scholar]