Abstract
The Tampa Bay Community Cancer Network (TBCCN) is one of the Community Network Program sites funded (2005–10) by the National Cancer Institute’s Center to Reduce Cancer Health Disparities. TBCCN was tasked to form a sustainable, community-based partnership network focused on the goal of reducing cancer health disparities among racial–ethnic minority and medically underserved populations. This article reports evaluation outcome results from a social network analysis and discusses the varying TBCCN partner roles—in education, training, and research—over a span of three years (2007–09). The network analysis included 20 local community partner organizations covering a tricounty area in Southwest Florida. In addition, multiple externally funded, community-based participatory research pilot projects with community–academic partners have either been completed or are currently in progress, covering research topics including culturally targeted colorectal and prostate cancer screening education, patient navigation focused on preventing cervical cancer in rural Latinas, and community perceptions of biobanking. The social network analysis identified a trend toward increased network decentralization based on betweenness centrality and overall increase in number of linkages, suggesting network sustainability. Degree centrality, trust, and multiplexity exhibited stability over the three-year time period. These results suggest increased interaction and interdependence among partner organizations and less dependence on the cancer center. Social network analysis enabled us to quantitatively evaluate partnership network functioning of TBCCN in terms of network structure and information and resources flows, which are integral to understanding effective coalition practice based on Community Coalition Action Theory ( Butterfoss and Kegler 2009). Sharing the results of the social network analysis with the partnership network is an important component of our coalition building efforts. A comprehensive baseline needs assessment for the next five-year funding phase (2010–15) of TBCCN Community Networks Program Centers (CNP Center) is under way to further evaluate the growth and sustainability of the partnership network, with an emphasis on community-based intervention research that takes into account culture and literacy. [social network, health care disparities, cancer screening]
The practice of coalition building in the field of health promotion has been established as a viable strategy for achieving desired community-level health, behavior, and social outcomes (Zakocs and Edwards 2006). The ability of collaborative interorganizational networks to build and sustain community capacity to improve health outcomes has been extensively studied and measured by health researchers in the social and behavioral sciences (Edberg et al. 2010; Goodman et al. 1998; Granner and Sharpe 2004; Provan et al. 2003, 2005a; Singer and Kegler 2004). As such, the fruits of coalition research and practice contribute to the development of coalition theory to provide frameworks for understanding the benefits of interorganizational collaboration (Butterfoss and Kegler 2009). This article illustrates how SNA can be used as a tool to examine coalition building and partnerships that are crucial to anthropological praxis (Schensul 1999; Singer 1995).
Support for community health coalition-directed action as a strategy to reduce health disparities has been bolstered in recent years through federal funding program announcements by the National Institutes of Health (NIH; e.g., “Community Participation in Health Disparities Intervention Research” and “Community Networks Program”), the Centers for Disease Control and Prevention, (e.g., “Racial and Ethnic Approaches to Community Health” and “HIV Prevention Projects for Community-Based Organizations”), and the Office of Minority Health, (e.g., “Partnerships Active in Communities to Achieve Health Equity”). Collaborations and partnerships, categorized by Shaw-Ridley and Ridley (2010) as community–academic, majority population serving-minority population serving institutions, and interorganizational, are the primary mechanisms integral to the functioning of the health disparities sponsored research field.
The National Cancer Institute’s (NCI) Center to Reduce Cancer Health Disparities’ Special Populations Networks Program, Community Networks Program, and most recently the Community Networks Program Centers constitute a series of programs of research, training, and outreach aimed to reduce and eliminate health disparities. These initiatives have been designed to create sustainable community–academic partnerships, build community-based infrastructure in medically underserved communities for outreach and the conduct of health disparities research, mentor junior researchers, and increase racial–ethnic minority participation in clinical trials (Freeman and Vydelingum 2006). To evaluate interorganizational relationships of community-based research activities, some program sites conducted social network analysis (SNA).I These analyses intended to gauge whether their respective community-academic networks led to increased communication and resource exchange networks over time and whether their community-based initiatives were tied to improved community access to cancer research and information, or strengthened community-academic cancer coalition networks (Albrecht et al. 2006; Luque et al. 2010c; Valente et al. 2010). The results from these evaluations indicated that community-based participatory research activities increased linkages between academic researchers and representatives of community-based organizations over time. Moreover, different stakeholder groups reached a greater understanding of other partners’ needs, concerns, and constraints, thus fostering community capacity. SNA is well suited for this purpose, because its theories, tools, and models have been adapted to studying coalition formation, dynamics, and stages of development (Valente 2010). Thus, network indices can show how interorganizational relationships might evolve and change over time, providing an evaluation metric for partnership development and sustainability.
The Tampa Bay Community Cancer Network (TBCCN) has been a formal community network program since 2005 and is now a community network program center. TBCNN was formed to reduce cancer health disparities and is characterized by community-based partnerships that serve medically underserved communities. The partnership network cuts across all racial and ethnic groups, including a growing number of foreign-born populations in selected portions of the greater Tampa Bay area in southwest Florida (Gwede et al. 2010a; Meade et al. 2011). Moffitt Cancer Center, which serves as a hub of TBCCN’s activities in collaboration with community organizations, is the only NCI-designated Comprehensive Cancer Center in Florida.
We analyze the SNA results of TBCCN (2007–09) as a case study to understand partnership network development and coalition building activities for increasing linkages between and among organizations. Evaluation activities will continue during the next five-year funding period to measure outputs and target outcomes according to the program’s logic model. This network evaluation is largely descriptive and is based on quantitative survey data collected from network partners. The evaluation was initiated after the first two authors received formalized SNA training workshops from fellow anthropologists (Bernard 2008). The results of this type of analysis provide graphical network diagrams of interorganizational linkages that may be shared with partners at meetings to foster engagement and discussion of network roles (Provan et al. 2005b). These diagrams show changes in network configurations over time and can engage partners to think about their place and role in the partnership as it evolves.
TBCCN was tasked to create a collaborative infrastructure for a community-academic partnership to develop effective and sustainable interventions to impact cancer health disparities, and to address critical cancer access, prevention and control issues that impact the priority populations it serves. To do this, TBCCN sustains formal partnerships (e.g., signed memoranda of understanding) with multiple community-based organizations, and it has a Steering Committee composed of cancer center leadership, community partners and stakeholders, university–academic-based researchers, TBCCN investigators and staff, and the NCI program director. A description of the partnership formation and creation of TBCCN can be found elsewhere (Gwede et al. 2010a; Meade et al. 2011).
This article describes a retrospective synthesis of the SNA evaluation data primarily from three consecutive annual quantitative surveys, and secondarily from an evaluation of meeting minutes and rosters of partner meetings from 2007 to 2009. We approached the SNA with three underlying, post hoc evaluation questions. First, was there a change in the organizations that are the most central to the TBCCN partnership network (centrality) over time? Second, do the SNA data help to explain the greater network integration and active roles of some partner organizations over others, because resources for nonprofits and healthcare organizations are dynamic? Third, do the SNA data shed light on understanding the most productive collaborative ties based on linkage type and relationship quality among partners over time? Additional outcomes discussed are benefits and drawbacks of participation, and partner engagement with three institutional review board (IRB) approved, community-based participatory research pilot projects to provide examples of synergy with TBCCN’s research goals. Finally, to link with the theme of this special issue, the article discusses how TBCCN functioned according to the community coalition model, as described by Community Coalition Action Theory (Butterfoss and Kegler 2009) and how the case study might provide lessons that would be instructive to anthropologists working within other community–academic networks.
METHODS
Study Population
TBCCN is a community-based partnership network composed of multiple community-based organizations, academic institutions, and healthcare organizations. The specific types of organizations and institutions include grassroots organizations, faith-based organizations, cancer survivorship nonprofit organizations, Hispanic farmworker advocacy organizations, adult literacy groups, federally qualified community health centers, county health departments, and local affiliates of national nonprofit cancer organizations. Many of the organizations had previous relationships with the cancer center without the formalized structure of TBCCN, and some of the partnership network members had achieved prior joint successes in outreach and health insurance coverage for uninsured county residents (Meade et al. 2002; Penzell et al. 1995). One representative from each of the 20 partner organizations who attended the TBCCN quarterly meetings completed the social network survey instrument on three consecutive occasions as part of ongoing evaluation activities: December 2007, September 2008, and September 2009.
Measures
The social network survey instrument was designed as a paper–pencil survey, based on an instrument developed by Provan and colleagues (2004). Prior to administration, the partner organizations received information about the purpose of the SNA in a quarterly partner meeting and received a presentation of the initial SNA results during a subsequent meeting. The instrument employed a matrix so each representative of the 20 partner organizations could indicate the presence or absence of specific links with every other partner organization based on the following five linkage (interaction) types or ties: (1) shared information, (2) shared resources, (3) collaboration on community events, (4) referrals, and (5) collaboration on grant proposals. In addition, each partner organization representative rated the strength of their relationship (trust)—from their organizational perspective—with other partners (from 1 = poor relationship/little trust to 4 = excellent relationship/high trust). TBCCN staff administered the survey to partner organizations over three consecutive years during the quarterly partner meetings (2007–09), and followed up to complete any missing surveys to decrease missing survey data through fax and email communication. The 2009 survey was expanded to include additional questions on the benefits and drawbacks of cooperating and collaborating with the network by answering with the following range of response categories (from 1 = strongly disagree to 4 = strongly agree), as well as an open-ended question on general attitudes toward network participation. To measure partner engagement, we used attendance roster sheets and meeting minutes to calculate the frequency of partner member attendance across three years (four quarterly meetings per year), based on mean number of attendees from all organizations per year, and read through all TBCCN-related activities as reported in the minutes. The SNA data were collected as part of an ongoing evaluation plan, which included the network analysis, and was approved by the University of South Florida Institutional Review Board.
Analysis
Quantitative survey data were manually entered into Excel and exported to UCINET 6.0 for social network analysis (Borgatti et al. 2002). The five different linkage types were combined to calculate a multiplexity value (frequency of the linkage types between partner organizations, or nodes) to assess the strength of relationship between partners. In addition, we calculated centrality measures to assess how central different organizations were to the network. One of these centrality measures is termed betweenness centrality, and refers to the frequency that a node connects pairs of other nodes who would otherwise not be connected. We were also interested in the core–periphery structure of the partnership network and used the continuous model to estimate coreness (the degree of coreness or closeness to the core for each node) to assess organizational relationships among the partners, assuming those closest to the core are more influential (Borgatti and Everett 1999). We also examined other network constructs including density (proportion of actual ties to possible ties) to examine how partner organizations were connected, and calculated degree centrality (number of direct ties to any given node) to assess the most active or engaged network partners. Centralization is an indicator of the extent to which influence is shared throughout a network. To increase reliability estimates, we completed the analysis of density for different linkage types using confirmed links—meaning that there was consensus between dyads on the presence of a tie—yet we also report unconfirmed links—where only one node confirmed a tie (Scott 2000). In addition, we used the egonet change function in UCINET to calculate the number of new ties present in 2009 that were not present in 2007. We used the bootstrap paired sample t test in UCINET to compare the mean densities of information sharing networks and of “any linkage” type (presence of at least one tie of any of the five linkage types) from 2007 and 2009 to detect if there was a significant change in network density, based on the 95 percent bootstrap confidence interval (CI). Moreover, the Quadratic Assignment Procedure (QAP) correlation in UCINET (Borgatti et al. 2002) was used to test the statistical significance of correlations between pairs of matrices (information sharing and resources sharing) for each consecutive year to examine whether the correlation of these networks of linkage types changed over time (i.e., information exchange and interorganizational cooperation; see Wells et al. 2007). Differences in mean trust values between the three years were calculated using the Kruskal-Wallis test (nonparametric equivalent of the one-way ANOVA test) and differences in mean benefits versus drawbacks in the 2009 survey were calculated using the Wilcoxon Signed Rank test (nonparametric equivalent of the paired t-test) using SPSS (ver. 18.0).
RESULTS
This section summarizes the SNA results related to density, centrality, and multiplexity. In addition, specific examples from partner engagement in education, training, and research provide contextual information to complement the SNA results. The response rates for the three years of surveys for the 20 partners used in the analysis were the following: 2007 (80 percent), 2008 (100 percent), and 2009 (95 percent). For the four missing partner surveys from 2007, imputation by last value carried backward was used, and for the one missing survey in 2009, imputation by reconstruction was used, because there was consensus among the evaluation team that the data from 2008 would not accurately represent this partner’s relationships in 2009, which had greatly diminished because of organization dissolution (Stork and Richards 1992). The areas of specialization of all partner organizations are summarized in Table 1, and included primary health care (35 percent), advocacy (20 percent), health education (15 percent), cancer-related services (e.g., support groups; 15 percent), and other areas (e.g., adult literacy services; 15 percent).
TABLE 1.
Summary of Services Provided by TBCCN Partner Organizations (N = 20)
| Service Type | Main Focus, n (%) |
|---|---|
| Primary health care | 7 (35) |
| Advocacy | 4 (20) |
| Health education | 3 (15) |
| Cancer-related services | 3 (15) |
| Other services | 3 (15) |
Changes in Centrality
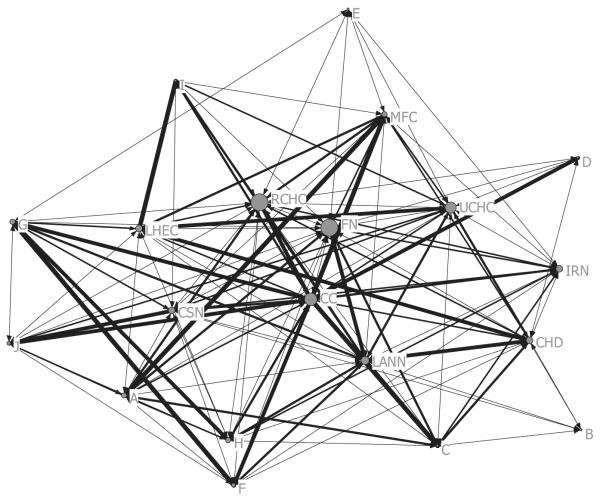
The first evaluation question examined changes in centrality over time. In both 2007 and 2008, the cancer center had the highest betweenness centrality. (See Table 2.) The network-level centralization index had the following values: 7.0 percent (2007); 11.9 percent (2008); and 4.3 percent (2009), indicating a less concentrated pattern of intermediary nodes in 2009. Although the cancer center was the main intermediary for indirect connections between partners in 2007 and 2008, in 2009, a rural community health center in one county and a farmworker nonprofit organization in another county increased their betweenness centrality to values exceeding the cancer center, thus contributing to the overall decentralization of the network. (See Figure 1.) Comparing 2007 to 2009, the farmworker nonprofit organization added five new ties, and the cancer center lost six previous ties. This dynamic of adding or losing ties affected the centrality values for these and other partner organizations. The core–periphery analysis found that the recommended size of the core membership was limited to one organization, namely, the cancer center, in both 2007 and 2008. This type of analysis is similar to eigenvector centrality, an indicator of who holds power in the network; however, while all nodes in the core are also highly central by any centrality measure, the converse does not always hold (Borgatti and Everett 1999). In 2009, the core–periphery analysis changed the recommended size of the core, expanding it to four organizations, which in addition to the cancer center included the farmworker nonprofit, the urban community health center, and the local health education center—ranked second, fourth, and sixth, respectively, in terms of betweenness centrality in 2009. Finally, change in mean trust levels over the three years for the overall network was not statistically significant. However, the cancer center received the highest mean trust value (3.6) compared to any other partner organization across the three years, and overall mean trust values showed an increasing trend from 2007 to 2009.
TABLE 2.
Centrality, Multiplexity, and Relationship Quality Values for Most Central TBCCN Partner Organizations
| Betweenness Centrality |
Degree Centrality |
Multiplexity |
Relationship Quality |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Organization | 2007 | 2008 | 2009 | 2007 | 2008 | 2009 | 2007 | 2008 | 2009 | 2007 | 2008 | 2009 |
| Rural Community Health Center | 1.8 (11) | 1.7 (12) | 9.9 (1) | 10 | 8 | 18 | 1.05 | 1.16 | 1.45 | 1.7 | 2.0 | 2.1 |
| Farmworker Nonprofit | 0.4 (17) | 1.0 (15) | 9.9 (2) | 7 | 9 | 18 | 1.00 | 1.21 | 0.90 | 1.6 | 2.0 | 1.8 |
| Cancer Center | 15.3 (1) | 23.9 (1) | 7.2 (3) | 19 | 19 | 17 | 3.21 | 3.74 | 3.30 | 3.4 | 3.9 | 3.5 |
| Urban Community Health Center | 4.5 (5) | 9.7 (4) | 6.4 (4) | 13 | 15 | 15 | 0.95 | 1.05 | 1.00 | 1.8 | 1.8 | 1.9 |
| Local Affiliate of National Nonprofit |
3.2 (7) | 9.9 (3) | 3.5 (5) | 13 | 14 | 15 | 1.47 | 1.58 | 1.00 | 2.2 | 2.5 | 1.9 |
| Local Health Education Center | 15.3 (2) | 4.1 (7) | 2.6 (6) | 19 | 11 | 13 | 1.32 | 1.63 | 1.20 | 2.2 | 2.8 | 2.5 |
| County Health Department | 2.1 (9) | 7.3 (5) | 2.5 (7) | 12 | 12 | 12 | 1.53 | 1.26 | 1.25 | 1.8 | 2.2 | 2.2 |
| Cancer Survivorship Nonprofit | 4.2 (6) | 2.6 (9) | 2.5 (8) | 13 | 9 | 13 | 0.79 | 0.95 | 1.10 | 1.7 | 2.5 | 2.2 |
| Immigration Resources Nonprofit | 1.5 (12) | 1.2 (14) | 2.5 (9) | 10 | 8 | 12 | 0.47 | 0.42 | 0.50 | 1.5 | 1.6 | 1.7 |
| Migrant Farmworker Clinic | 1.9 (10) | 10.3 (2) | 2.3(10) | 10 | 15 | 12 | 1.53 | 1.95 | 1.60 | 2.0 | 2.8 | 2.6 |
| Mean for all organizations | 3.9 | 4.6 | 2.9 | 11.2 | 9.9 | 11.4 | 1.07 | 1.10 | 1.11 | 1.8 | 2.1 | 2.0* |
Notes: 10 of 20 partner organizations are ranked in order of their betweenness centrality values in 2009. Individual ranking appears in parentheses next to the value.Multiplexity values range from 0 to 5 for any possible link. Relationship quality/trust values range from 1 = low to 4 = high.
χ2 = 2.46, df = 2; p = .29.
FIGURE 1.
The Tampa Bay Community Cancer Network in 2009 (node size based on betweenness centrality, line width based on tie strength, ranging from 1 to 5 linkage types). 10 of 20 partner organizations are labeled in order of their betweenness centrality values (refer to Table 2 for actual values): RCHC, Rural Community Health Center; FN, Farmworker Nonprofit; CC, Cancer Center; UCHC, Urban Community Health Center; LANN, Local Affiliate of National Nonprofit; LHEC, Local Health Education Center; CHD, County Health Department; CSN, Cancer Survivorship Nonprofit; IRN, Immigration Resources Nonprofit; MFC, Migrant Farmworker Clinic; letters A–J, other partner organizations.
The second evaluation question explored the dynamics of partner organizations becoming more or less central to TBCCN. In the beginning of the partnership network the local health education center—an organization that provides health career recruitment programs—had high betweenness centrality, but its centrality diminished over time as other nonprofits, which could more directly benefit from education and service opportunities related to cancer prevention, moved into more central roles in terms of network structure. The urban community health center and the local affiliate of the national nonprofit cancer organization remained central partner organizations over the three-year period. The national nonprofit organization provided local grants for screening and education to partners, and the urban community health center was in close geographic proximity to the cancer center. These factors might partly explain their continued centrality in the partnership network.
Changes in Linkage Types
The third evaluation question examined whether the most common linkage type, information sharing, was related to resources sharing, and how these collaborative ties defined the partnership network. Of the five linkage types, only information sharing showed a trend for increased density. Change in network density—based on increased density of information sharing from 2007 to 2009—approached statistical significance (average bootstrap difference = 0.01, 95 percent bootstrap CI [−0.15, 0.01], p = .04). (See Table 3.) For any linkage type, the increase in network density from 2007 to 2009 was significant (average bootstrap difference = −0.50, 95 percent bootstrap CI [−0.81, −0.46], p < .001). The “average” partner accounted for 5.4 confirmed links out of a possible 19 ties in 2009, increasing from 4.2 confirmed links in 2007. Based on the QAP correlations between information sharing and resources sharing, there was a significant but declining Pearson correlation coefficient for each year (p < .001): r = 0.73 (2007); r = 0.65 (2008); and r = 0.45 (2009).
TABLE 3.
Confirmed and Unconfirmed Network Values for TBCCN Partner Organizations
| Unconfirmed density |
Confirmed density |
Mean confirmed links |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Linkage type | 2007 | 2008 | 2009 | 2007 | 2008 | 2009 | 2007 | 2008 | 2009 |
| Shared information | .484 | .490 | .621 | .174 | .205 | .242* | 3.3 | 3.9 | 4.6 |
| Referrals | .195 | .242 | .279 | .053 | .063 | .048 | 1.0 | 1.2 | 0.9 |
| Shared resources | .347 | .326 | .416 | .100 | .142 | .116 | 1.9 | 2.7 | 2.2 |
| Collaborated on community events | .321 | .311 | .316 | .121 | .147 | .116 | 2.3 | 2.8 | 2.2 |
| Collaborated on grant proposals | .216 | .226 | .153 | .090 | .090 | .032 | 1.7 | 1.7 | 0.6 |
| Any links | .221 | .274 | .284** | 4.2 | 5.3 | 5.4 | |||
Note: “Any links” represents a confirmed tie of any of the 5 linkage types with another partner. “Mean confirmed links” equals the total number of confirmed links maintained by the “average partner.”
2007 vs. 2009 avg. bootstrap diff. = .01, 95% bootstrap CI (−.15, .01).
2007 vs. 2009 avg. bootstrap diff. = −.50, 95% bootstrap CI (−.81, −.46).
Benefits and Drawbacks of Participation
According to the quantitative scale, TBCCN partners responded that the benefits of participation outweighed the drawbacks. (See Table 4.) The highest rated responses were for building new relationships helpful to the agency, greater capacity to serve the community, and ability to serve their clients better. The reported largest drawbacks of participation were the amount of time and resources required (e.g., staff time to attend meetings). There was a significant difference in reported partner benefits and drawbacks of partner participation, with benefits outweighing the drawbacks (z = −8.49, p < .001). In the open-ended written responses, one of the partners listed an additional benefit of receiving more resources and learning multicultural skills, echoing the sentiments of another partner who reported, “participation has enhanced our community services.” Another partner responded, “The only drawback was not having the staff to send to the meetings. It was a very positive and rewarding experience.”
TABLE 4.
Results from Benefits and Drawbacks Survey Questions
| Question | Mean (SD) |
|---|---|
| Benefits | |
| Ability to serve my clients better | 3.6 (0.5) |
| Greater capacity to serve the community as a whole | 3.6 (0.5) |
| Acquisition of additional funding and other resources | 3.1 (0.9) |
| Acquisition of new knowledge or skills | 3.5 (0.6) |
| Better use of my organization’s services | 3.1 (0.8) |
| Building new relationships helpful to my agency | 3.8 (0.4) |
| Heightened public profile of my organization | 3.3 (0.7) |
| Enhanced influence in the community | 3.2 (0.8) |
| Increased ability to reallocate resources | 3.1 (0.9) |
| Drawbacks | |
| Takes too much time and resources | 1.9 (0.8) |
| Loss of control/autonomy over decisions | 1.5 (0.6) |
| Strained relations within my organization | 1.5 (0.5) |
| Difficulty in dealing with partners | 1.4 (0.6) |
| Not enough credit given to my organization | 1.5 (0.6) |
Notes: Response options were 1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree.
Another benefit to network participation was the engagement of community partners in community-based participatory research. Multiple externally funded, community-based participatory research pilot projects with academic and community partners are either currently in progress or have been completed, covering varied research topics including culturally tailored colorectal and prostate cancer screening education, patient navigation for the prevention of cervical cancer in rural Latinas, and community perceptions of biobanking. The following section offers a brief synopsis of community–academic research partnership network examples.
Partner Engagement
Based on the Memorandum of Understanding with TBCCN, partner representatives were required to attend at least three out of four quarterly partner meetings per year. Based on a review of meeting attendance rosters, out of an average of 20 possible partner representatives attending over the three-year period (N.B. sometimes more than one partner representative per organization attended), the average number of partners attending meetings was the following: 21 in 2007; 16 in 2008, and 18 in 2009. During the same period, the average number of cancer center employee meeting attendees was recorded as: 13 in 2007; 12 in 2008; and 14 in 2009. These employee attendees included TBCCN staff (three–four individuals), TBCCN coinvestigators, and other faculty and staff from the cancer center. In sum, over the three-year period, there was an average of 18 partner attendees and 13 cancer center employee attendees per meeting.
Some of the partner organizations benefited from TBCCN membership by receiving seed funding grants ranging from $1,000 to $2,000 based on yearly internal competitions. Applications were reviewed by a committee, consisting of the TBCCN Principal Investigator, TBCCN program manager, collaborating cancer center researchers, and the coordinator of the cancer center’s Education and Outreach Department. From 2008 to 2010, 36 seed funding grants were awarded. As an example of these grant-supported activities, healthcare organization representatives from multiple agencies reported using funds for various purposes including health education materials (e.g., cervix models, posters, and brochures for placement in exam rooms and waiting areas) and cervical cancer screening supplies (e.g., gowns, gloves, medical instruments, and lubricants). One health department was able to use the seed funding to offset the salary of a part-time health educator tasked to promote cervical cancer screening and counsel young women to receive HPV vaccinations and routine Pap tests. An advocacy nonprofit working with migrant farmworkers was able to hire a bilingual community health outreach worker to provide community education on cervical cancer prevention. The same nonprofit worked with TBCCN staff to implement a “Girl Talk” series to provide cancer education workshops as a strategy to improve health literacy among Latina adolescents. At one of the partner meetings, the nonprofit’s representatives reported that the workshops, which focused on cancer prevention, awareness and healthy lifestyles, was well received by the participants. In addition to these grant-supported activities, partners benefited through continuing education opportunities offered as part of the quarterly partner meetings on the following topics: Cancer 101—focused specifically on cervical and colorectal cancer screening and access; grant writing—directed toward writing local American Cancer Society (ACS) and Susan G. Komen Foundation project grants; clinical trials education; developing low literacy materials; and biobanking—including a tour of a tissue repository facility, or biobank. In addition to these service projects, there were a number of investigator-initiated, pilot research projects. The following section provides examples of these pilot projects, which led to new relationships between academic researchers and TBCCN partner representatives.
Examples of Pilot Projects
As examples of tangible outcomes from the partnership network, the following sections include brief descriptions of partnership activities that led to three NCI-funded, TBCCN pilot research projects. Previously funded pilot research projects have been discussed comprehensively elsewhere (Gwede et al. 2010c, in press; Luque et al. 2010b, 2011a; Meade et al. 2011). All three pilot projects were fueled by findings from the initial TBCCN partner assessment (Gwede et al. 2010a), and by the partnership network’s readiness to leverage new funding opportunities.
Community Perceptions of Biobanking
The first pilot project was on the subject of community engagement with biobanking. Biobanking is the storage of human tissue, often combined with medical and personal information, for the purposes of diagnostic procedures, surgical treatment, and educational or research purposes (Hewitt 2011). Accountability, transparency, and proper monitoring are necessary to engender and maintain the public’s trust in biobanking (Deschênes and Sallée 2005). A study involving a series of community engagement activities was undertaken to assess community attitudes, perceptions, beliefs, and informational needs about biobanking. Interactive activities to engage community members on the topic included educational presentations, a biobanking tour, and the formation of a Community Advisory Group (CAG). The group is composed of key community stakeholders selected from existing TBCCN partners, provided ongoing feedback on study methods, recruitment strategies, focus group content, educational materials, and offered important community insights about biobanking. As one CAG member commented, “I didn’t really understand what the topic was all about, but if we educate our community members about its importance and how they can benefit … then we can make it work.” Twelve focus groups were conducted to examine community members’ knowledge and attitudes about biospecimen collection, motivations toward research participation, ethical concerns, and learning preferences. Data gathered from this research are aiding in identification of strategies to effectively frame educational messages with respect to health literacy, cultural competency, and informed decision making. Community-based research outputs include (1) formation of a CAG that could be used to advise future studies and inform policies on biobanking research; (2) development of educational communication tools that present new biomedical technologies in an easy-to-understand manner; (3) establishment of linkages to the NCI’s Minority Biospecimen/Biobanking— Geographic Management Program Regional initiatives, known as BMaP-GMaP; and (4) creation of community-based infrastructure for a subsequent biobanking pilot project to evaluate educational communication priming tools. Use of community engagement methods to improve communications about biobanking is one way to bring constituents’ voices into discussions and may ultimately influence the way biobanks are implemented (O’Doherty and Hawkins 2010).
Cervical Cancer Patient Navigation
The second pilot project focuses on addressing cervical cancer disparities with Latina farmworker populations. Latina farmworkers are at an elevated risk for cervical cancer and for various other cancers (Coughlin and Wilson 2002). The TBCCN Cervical Cancer Patient Navigator Research Project was developed following previous studies, which included an NCI funded Patient Navigation Research Program (Wells et al. 2008) and a community-based research project on cervical cancer screening with a faith-based farmworker clinic (Luque et al. 2010a, 2011b). The farmworker clinic provides free medical, health promotion, and disease prevention services to uninsured and low-income populations residing in Hillsborough County. Developed using qualitative formative research, the patient navigation services focus on providing education and psychosocial support, reducing personal barriers, and increasing facilitating factors to assist women in overcoming health system and logistical barriers to appropriate cervical cancer screening and follow-up. The project is evaluating the feasibility and impact of the pilot patient navigation intervention, which is designed to increase the number of women who obtain cervical cancer screening. Other secondary outcomes include reducing the time clients wait for their screening exam results and increasing adherence to follow-up tests in the event of abnormal results. The community-based patient navigator program assists the farmworker clinic in creating a safety net for uninsured farmworker women. This program contributes to a sustainable research partnership for future research opportunities with this vulnerable priority population.
Colorectal Cancer Education
The third pilot project addressed the need for colorectal cancer (CRC) education and screening resources identified by community partners. This pilot examined awareness, perceptions and behaviors related to CRC among three subgroups of blacks including U.S.-born African Americans, foreign-born blacks from English-speaking Caribbean countries (e.g., Jamaica, Trinidad and Tobago) and from Haiti (Gwede et al. 2010c, in press). U.S. blacks have the highest CRC incidence and mortality rate of all racial and ethnic groups, and these disparities have remained unchanged for decades (American Cancer Society 2011). Because health statistics for blacks are often presented in the aggregate, differences in colorectal cancer screening (CRCS) perceptions and behavior across subgroups within the U.S. black population are largely unknown. To further explore this research topic, cancer center researchers partnered with nonprofit organizations serving these three population subgroups. In addition, the project formed a cultural advisory group composed of four community leaders from the three population subgroups to assist with study design (research questions, research design, and measures), hiring and training of study staff with regard to cultural sensitivity, implementing the study (e.g., designing recruitment strategies) and interpreting findings. Overall, findings showed lack of awareness of CRC and CRCS across all three subgroups, similar cultural perceptions of the disease, and common barriers to access and utilization of screening (Gwede et al. 2010c, in press). However, there were subtle differences in perceived strategies to prevent colon cancer, rates of self-reported screening, health insurance as a perceived barrier to screening, and expressed need for educational materials in Haitian Creole. In response to the need for language and culturally appropriate CRC education materials, we developed a CRCS photo novella booklet culturally targeted for blacks and adapted this concept into Haitian Creole using transcreation—culturally appropriate translation—to capture cultural meanings that go beyond mere translation (Simmons et al. 2011). As such, our CRC pilot project has resulted in development of materials that are now undergoing extensive testing for efficacy in larger scale randomized controlled trials in community settings, as well as in safety net clinics (federally qualified health centers).
COALITION FUNCTIONING OF TBCCN ACCORDING TO COMMUNITY COALITION ACTION THEORY
In this article we have described the TBCCN partnership development based on quantitative social network data and examples of specific activities from three pilot projects conducted with partner organizations. The network processes described herein provide a backdrop for understanding how the overall network functions in terms of coalition theory. To characterize TBCCN as a case study of an action-oriented partnership network and understand network functioning in terms of Community Coalition Action Theory (CCAT), we will discuss the extent to which the evaluation of the partnership, based on the data presented here, resonates with this theory of effective coalition development (Butterfoss and Kegler 2009). Public health researchers have only recently begun to test relationships between coalition factors and outcomes predicted by CCAT using survey research data (Kegler et al. 2010; Kegler and Swan 2011). Survey research based on CCAT constructs with cancer coalitions in Arkansas found that high levels of member engagement, leadership, development, and ownership were correlated with coalition capacity effectiveness (Torrence et al. in press). This case study adds to this literature by understanding partnership network functioning in terms of CCAT, and areas of strengths and weaknesses for future development can be assessed and evaluated to provide theory-based recommendations for other similar community–academic networks. The results of the social network analysis enable us to quantitatively evaluate partnership network functioning in terms of network structure and information and resources flows, which are integral to understanding effective coalition practice. However, we believe that additional research into the partnership network through the conduct of ethnographic research is needed to thoroughly understand relationships between coalition factors and positive outcomes. Thus, qualitative interviews with network partners are currently being conducted, and the analysis of these findings will be the subject of a future report. Further, for SNA to be an effective tool, community organizations need to be partners in evaluation efforts by providing feedback on their evolving positions in the partnership to strengthen these networks (Provan et al. 2005b).
Stages of Development
TBCCN has moved through partnership development stages including formation, implementation, maintenance, and outcomes and is now moving through the stages again with the expansion of the partnership network for another five years of TBCCN activities. Currently, TBCCN is implementing a second needs assessment to identify activities and goals as a baseline for further coalition development. The network continues to engage new members and has grown from an initial 19 partner organizations to 23 current partners. As evident in the core–periphery analysis, TBCCN is evolving from a one-institution core membership structure to a multiple-organization core membership structure. The Tampa Bay region continues to experience cancer health disparities, and TBCCN is recognized in the community for its partnership activities to address this issue.
Lead Institution–Convener Group
The cancer center continues to serve as the lead academic institution for TBCCN, having received NCI funding for education, training, and research activities. Through community-based participatory research partnerships, the cancer center has leveraged additional supplemental and research grants from NCI, and helped improve capacity among partners to leverage support from organizations such as ACS, NCI, and the Susan G. Komen Foundation to support education, navigation and outreach services. The TBCCN staff effectively recruits partners to attend meetings and outreach activities such as cultural events and health fairs to foster a sense of community and shared mission. Importantly, the cancer center has maintained a high level of trust in the eyes of its fellow partners based on the survey results.
By only examining data from 2007 and 2008, based on betweenness centrality and multiplexity values, as well as the core–periphery analysis, TBCCN was a highly centralized network, with the cancer center at the nexus (Luque et al. 2010a). One benefit of centralized networks is the ability to facilitate the adoption of evidence-based programs (Valente et al. 2007). However, based on a lower centralization index in 2009 and expansion of the core, there was a new trend toward decentralization. This result shows the value of longitudinal data for evaluating network change. Some evidence has shown that decentralization might be necessary for sustained action for coalitions who provide services collectively and need to mobilize resources (Wells et al. 2007). Based on the belief that network sustainability will eventually be tied to network decentralization, ongoing efforts to continually gauge partner expectations, identify shifts in community priorities, and pinpoint ways to enhance individual and collective capacity are required. As such, our ongoing dialogue at quarterly partners meetings, community sites, and the annual retreat is needed to ensure that the dynamics of the partnership are productive, engaging, and meaningful. TBCCN has fostered the capacity to make collective decisions to act as a network with a shared purpose, rather than functioning as an autonomous entity with structural holes benefiting the core (Borgatti et al. 2009). Further SNA evaluation data and ethnographic research are needed to better understand the movement of the cancer center toward decreased betweenness centrality and decreased coreness.
Coalition Membership
The membership of TBCCN is diverse in terms of organization type and clients served. Furthermore, the partner representatives are diverse in terms of age, education, occupation, race, and ethnicity. There are factors of geography and community context that have affected the network membership composition. Because TBCCN is dispersed throughout three counties—with most members located in northern Hillsborough County, where both the city of Tampa and the cancer center are located—some newer partners in the other counties have expressed that they have minimal contact with some of the other network partners. This is also evident in the social network results, which shows that some members have low degree centrality. Nevertheless, a shared vision and mission focused on reducing cancer health disparities resonated with partner organizations and helped to propel collaborative action. Moreover, these results are helpful to direct our engagement with newer partners where there are current gaps in interorganizational linkages. A common mission committed to building community networks to reduce cancer health disparities unites partner organizations.
Coalition Operations and Processes
A comprehensive review of meeting minutes found that coalition activities consisted of sharing information, updates from community-based participatory research projects, updates on TBCCN community activities, training opportunities to build capacity, and breakout sessions focused on specific goals such as assessing needs, developing and evaluating educational materials, and mission and goal setting. TBCCN leaders and staff met frequently to strategize on varying meeting locations, increasing partner attendance, reaching out to new members, and holding yearly annual retreats with longer scheduled meetings for training workshops.
Leadership and Staffing
From the inception of TBCCN, the network has had a Principal Investigator, a full-time project coordinator, a part-time outreach worker, and an administrative assistant who devoted part of her time to network activities. In the current grant period, TBCCN now has two principal investigators, a center coordinator, and a community health educator. TBCCN staff ensured partner representatives received meeting agendas, meeting minutes, newsletters, and other related announcements. The cancer center, serving as the lead academic agency for TBCCN, with a well-defined personnel infrastructure (principal investigator, coinvestigators, project coordinator, outreach workers, junior investigators, and administrative personnel) and sufficient space to hold partner meetings, worked collectively with partner representatives to set objectives and goals. For example, the types of capacity building workshops (e.g., grant writing workshops) offered were identified by the partners. In addition, during community meetings, partners had the opportunity to network with partners and were formally recognized for their successes in partnership network activities. Moreover, TBCCN staff attended numerous community events, such as health fairs, cultural events, and other community activities (e.g., Men’s Health Forum). In addition, the TBCCN Steering Committee met annually to provide direction, oversight, and expert feedback of community-based participatory research projects and related community outreach activities to foster effective and sustainable community cancer intervention programs
Coalition Structures
The Memorandum of Understanding defines criteria for network membership and the roles and responsibilities of the members. TBCCN functions formally with agendas, meeting minutes, and leader-facilitated meetings. Partner organizations formed work groups that focused on specific activities such as developing low literacy materials, increasing capacity for grant writing, and disseminating network outcomes to their stakeholders.
Member Engagement
TBCCN staff supported involvement of partner representatives by welcoming people to meetings, taking minutes, communicating through email, newsletters, inviting interested members to conferences (both locally and nationally), and playing other supportive roles to maintain open communication lines. Average attendance over 12 TBCCN partner meetings was 90 percent, providing evidence of a high level of partner engagement. Based on the diverse membership in terms of organization types, the network engaged a wide variety of community-based organizations, advocacy organizations, and healthcare institutions. The results of the survey questions on benefits and drawbacks of participation indicate that organizations might have decided to join TBCCN and remain engaged over the years because the perceived benefits of participation outweighed the costs. This line of reasoning has support in the field of interorganizational relations (Prestby et al. 1990).
The continued attendance at TBCCN meetings and activities and network sustainability, based on continued federal funding, provides further evidence that the benefits of membership, which include building community capacity, leveraging resources, and strengthening personal ties between partner organization representatives were perceived as valuable enough to offset the possible drawbacks, such as time involvement and potential conflict with other network partners. Open-ended survey responses revealed that some communication challenges existed between partner organizations; and a process needs to be implemented to improve opportunities for collaboration. In one example of engagement, seven partner organizations implemented and promoted “cancer information stations” at their facilities using resources obtained from the cancer center to educate their clients with multimedia presentations. Moreover, the ability to secure small seed grants for special projects offered an incentive for continued participation. To increase future engagement, partners suggested that TBCCN reach out to churches and other faith-based organizations, and conduct community outreach activities in unconventional settings such as bus stops, food pantries, and grocery stores. Community partners also identified cancer survivorship as a critical gap in education and outreach, and consequently, they recommended that TBCCN enhance its efforts by focusing on educational programs for cancer survivors.
Pooled Member and External Resources
TBCCN was able to define priority areas (e.g., access to colorectal cancer screening) and leverage outside resources to conduct an asset mapping activity involving a Geographic Information Systems (GIS) expert to identify community resources (Gwede et al. 2010b). Another example of leveraging resources was a federal grant awarded to area health departments that provided CRCS to under- and uninsured populations. Partner organizations were also able to leverage their own resources to provide health screenings and education activities at community events. Additionally, more efforts will be needed in the future to identify and pursue funding opportunities for outreach and education for partner organizations for continued sustainability. To foster sustainability, continued discussions about methods to maintain partnership network synergistic activities will be vital over the upcoming years. Kegler and Swan (2011) found that broad representation in the maintenance stage of a coalition was correlated with dollars leveraged, and our findings are consistent with this observation. As evidenced by the results of the three pilot studies described here, these new projects provided opportunities for partners to join new efforts, learn new skills, and contribute to partnership synergy.
Assessment and Planning
In the initial needs assessment, the partners identified the need to increase their capacity to provide health education services, preventive screenings and follow-up services, and to improve their success in grant applications. Partners also stressed the importance of sharing knowledge and formally solidifying the partnership network. Based on these network assessments, the partnership network has forged ahead with development of a service directory to identify resources for cancer education and screening for medically underserved populations. The network has also leveraged and received new funding from NCI and ACS to address cancer disparities through education, training, outreach, and research projects. Specifically, two recently funded colorectal cancer screening intervention projects directly address the needs identified in our needs assessment. Hence, the network has demonstrated a strategic focus on sustainability and community benefit, and is poised to address cancer health disparities for another five years.
Implementation of Strategies
Community engagement with an emphasis on service represents the foundation for strengthening partner relationships, in addition to the regular TBCCN partner meetings. TBCCN tracks the number of health promotion activities it undertakes each year (e.g., health fairs, workshops, and small group education sessions) and the number of participants reached through these activities as part of its ongoing process evaluation. Importantly, TBCCN is not a service provider itself, so its presence at community outreach events does not compete with other partners’ services.
Community Change and Health Outcomes
Provan and colleagues (2003) argue that benchmarks for the success of community coalitions focused on reducing chronic disease should be tied to short-term outcomes of community capacity building linked to maximizing the use of community-identified resources. Examples of such capacity building activities include service collaborations from participating in health fairs, and leveraging resources from the cancer center (mobile mammography screening), the migrant farmworker mobile clinic (Pap tests), the health departments (HIV testing and health education), and the federally qualified health centers (other preventive screenings and wellness education services). However, the goal of reducing cancer health disparities is tied to long-term health outcomes, and benchmarks for success will be measured by the increase in breast, cervical and colorectal screening rates among TBCCN’s priority populations. In terms of positive health outcomes, the evidence for coalitions to produce documented changes in health status is scant (Butterfoss and Kegler 2009). However, the case of TBCCN provides some evidence for increased sharing of information and resources, as well as indicating a trend for decreased centralization for a federally funded community partnership network, indicating potential sustainability. However, these intermediate outcomes cannot yet be shown to lead to direct health improvement gains as measured by reduction in health disparities or decreases in cancer mortality. To address health disparities, the recently funded colorectal cancer screening intervention research project will implement a longitudinal, randomized, community-based intervention study to increase screening uptake and reduce colorectal cancer morbidity in medically underserved populations.
Community Capacity
Some necessary elements of community capacity include a feeling of community, commitment to action, and mobilization of resources aimed at addressing specific community-identified problems (Chaskin et al. 2001). Community capacity development is defined here as a positive outcome of community health promotion activities (Goodman et al. 1998). Based on the QAP correlation results, there was a significant correlation between sharing of resources and information, but this association diminished over time. This finding might indicate that while information sharing trended toward increased density, sharing of resources declined. This result points to an area where TBCCN might concentrate its efforts, toward more interorganizational cooperation to pool resources toward achieving research and service objectives. TBCCN has attempted to balance the needs of service providers by offering capacity-building activities (e.g., developing grant writing skills for service grants). Although pilot research projects improve community partner’s understanding of research, the short-term nature of pilot project research and undetermined fate of follow-up, larger-scale studies might place strain on community–academic partnerships (Strong et al. 2009). Despite the potential shortcomings of these types of preliminary studies, partner involvement in TBCCN pilot research projects enhanced their sense of participation in the research process, from problem formulation through dissemination of results, and leveraging continuation funding for sustainability. As such, TBCCN has produced exceptional results in engagement of community partners and sustainability beyond the initial funding period. A summary finding, which is found in the coalition literature and applies to the TBCCN example, is that organizational capacity is greatest in coalitions that have received sustained funding and recognized the importance of participatory decision making, or alternatively, partners who believe that the coalition acts on behalf of their interests are more likely to continue their investment in the coalition’s activities (Zakocs and Guckenburg 2007).
Findings from the SNA of TBCCN are similar to findings from previous studies that illustrate how information from organizational networks can be used to assess community capacity (Singer and Kegler 2004; Wells et al. 2007) and strengthen community partnerships (Provan et al. 2005a). TBCCN strives for an equitable distribution of voice and power between academic and community partners. The trend toward decentralization of the network, evidenced by the cancer center’s decreased centrality in 2009, is illustrative of this phenomenon. Furthermore, as previous research suggests, decentralization has the potential to lead to the network’s sustainability and effectiveness (Feinberg et al. 2005; Wells et al. 2007).
CONCLUSION
The experience of TBCCN supports the proposition that community partnerships are critical to raising awareness of cancer health disparities. Moreover, capacity building and interventions that benefit community members are positive outcomes of partnership synergy. As with any coalition, there are constraints and limitations because of the criteria for partner involvement, limited resources, and history of collaboration. For example, other at-risk populations, such as the elderly, represent possible areas for expansion and growth of the network in the future thereby increasing the network’s potential to address cancer disparities broadly. In reference to Morris’s (this issue) expansion of CCAT’s propositions, TBCCN has reached out to marginalized groups (e.g., Hispanic farmworkers) and secured active participation from representative organizations. As Butterfoss and Kegler (2009) observe, much research on coalitions is cross-sectional. By analyzing the constructs of CCAT within the context of a longitudinal SNA case study, we have begun a discussion of some of the causal pathways that could be tested in evaluations with a larger number of coalitions to test the applicability of the community coalition model in a broader context. In addition, we have found that yearly assessments of community partners combined with the presentation of these assessment results at regular partner meetings keeps partners engaged and leads to network sustainability.
One of the advantages of using a SNA approach to measure community partnership network development is the ability to accurately describe changing network dynamics and share the results in an interactive manner with fellow stakeholders through discussing the network diagrams. Assessing organizations that have strong working relationships, as well as those that need to be strengthened, will enhance a network’s capacity to better address community needs (Provan et al. 2005b). This case study shows the value of collecting longitudinal social network data to understand changing network dynamics and development. Applied anthropologists trained in the methodology of social network analysis can contribute to the praxis of coalition development, evaluation, and action.
Acknowledgments
This publication was supported by Grant Number U01 CA114627 from the Center to Reduce Cancer Health Disparities. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Center to Reduce Cancer Health Disparities awarding office of NIH. We thank our community partners for their dedication to the TBCCN partnership goals and commitment to reduce cancer disparities.
Footnotes
For an introduction to social network analysis, see Scott (2000) and Hanneman and Riddle (2005); and for a primer on social network analysis as applied to public health research, see Valente (2010).
Contributor Information
John S. Luque, Georgia Southern University
Dinorah Martinez Tyson, University of South Florida.
Shalanda A. Bynum, Moffitt Cancer Center
Shalewa Noel-Thomas, Moffitt Cancer Center.
Kristen J. Wells, University of South Florida
Susan T. Vadaparampil, Moffitt Cancer Center
Clement K. Gwede, Moffitt Cancer Center
Cathy D. Meade, Moffitt Cancer Center
REFERENCES CITED
- Albrecht Terrance, Berry-Bobovski Lisa, Lichtenberg Peter, Underwood Willie, Penner Louis, Stengle William. Applying Social Network Analytic Techniques to Developing Community Partnerships: Crucial Lessons from the NCI/Detroit Community Network Program. Paper presented at the APHA 134th Annual Meeting and Exposition; Boston, Massachusetts. November 5–8.2006. [Google Scholar]
- American Cancer Society . Cancer Facts and Figures. American Cancer Society; Atlanta: [accessed August 25, 2011]. 2011. http://www.cancer.org/ [Google Scholar]
- Bernard H. Russell. Commentary: The History and Purpose of Methods Camp. Practicing Anthropology. 2008;30(1):4–5. [Google Scholar]
- Borgatti Stephen P., Everett Martin G. Models of Core/Periphery Structures. Social Networks. 1999;21:375–395. [Google Scholar]
- Borgatti Stephen P., Everett Martin G., Freeman Linton C. Ucinet for Windows: Software for Social Network Analysis. Analytic Technologies; Harvard, MA: 2002. [Google Scholar]
- Borgatti Stephen P., Mehra Ajay, Brass Daniel J., Labianca Giuseppe. Network Analysis in the Social Sciences. Science. 2009;323(5916):892–895. doi: 10.1126/science.1165821. [DOI] [PubMed] [Google Scholar]
- Butterfoss Frances D., Kegler Michele C. The Community Coalition Action Theory. In: DiClemente Ralph, Crosby Richard, Kegler Michelle., editors. Emerging Theories in Health Promotion Practice and Research. 2nd edition Jossey-Bass; San Francisco: 2009. pp. 237–276. [Google Scholar]
- Chaskin Robert J., Brown Prudence, Venkatesh Sudhir, Vidal Avis. Building Community Capacity. Aldine de Gruyter; New York: 2001. [Google Scholar]
- Coughlin Steven S., Wilson Katherine M. Breast and Cervical Cancer Screening among Migrant and Seasonal Farmworkers: A Review. Cancer Detection and Prevention. 2002;26(3):203–209. doi: 10.1016/s0361-090x(02)00058-2. [DOI] [PubMed] [Google Scholar]
- Deschênes Mylene, Sallée Clementine. Accountability in Population Biobanking: Comparative Approaches. Journal of Law, Medicine and Ethics. 2005;33(1):40–53. doi: 10.1111/j.1748-720x.2005.tb00209.x. [DOI] [PubMed] [Google Scholar]
- Edberg Mark, Cleary Sean D., Andrade Elizabeth, Leiva Rodrigo, Bazurto Martha, Rivera Maria I., Montero Luisa, Calderon Melba. SAFER Latinos: A Community Partnership to Address Contributing Factors for Latino Youth Violence. Progress in Community Health Partnerships. 2010;4(3):221–233. doi: 10.1353/cpr.2010.0009. [DOI] [PubMed] [Google Scholar]
- Feinberg Mark E., Riggs Nathaniel R., Greenberg Mark T. Social Networks and Community Prevention Coalitions. Journal of Primary Prevention. 2005;26(4):279–298. doi: 10.1007/s10935-005-5390-4. [DOI] [PubMed] [Google Scholar]
- Freeman Harold P., Vydelingum Nadarajen A. The Role of the Special Populations Networks Program in Eliminating Cancer Health Disparities. Cancer. 2006;107(8, supp.):1933–1935. doi: 10.1002/cncr.22162. [DOI] [PubMed] [Google Scholar]
- Goodman Robert M., Speers Marjorie A., McLeroy Kenneth, Fawcett Stephen, Kegler Michelle, Parker Edith, Smith Steven R., Sterling Terrie D., Wallerstein Nina. Identifying and Defining the Dimensions of Community Capacity to Provide a Basis for Measurement. Health Education and Behavior. 1998;25(3):258–278. doi: 10.1177/109019819802500303. [DOI] [PubMed] [Google Scholar]
- Granner Michelle L., Sharpe Patricia A. Evaluating Community Coalition Characteristics and Functioning: A Summary of Measurement Tools. Health Education Research. 2004;19(5):514–532. doi: 10.1093/her/cyg056. [DOI] [PubMed] [Google Scholar]
- Gwede Clement K., Menard Janelle M., Martinez-Tyson Dinorah, Lee Ji-Hyn, Vadaparampil Susan T., Padhya Tapan A., Meade Cathy D. Strategies for Assessing Community Challenges and Strengths for Cancer Disparities Participatory Research and Outreach. Health Promotion Practice. 2010a;11(6):876–887. doi: 10.1177/1524839909335803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwede Clement K., Quinn Gwen P., Vadaparampil Susan T., Jean-Francois Emmanuel, Wilson Shani, Tarver Will, Thomas Kamilah B., Meade Cathy D. Perceptions of Colorectal Cancer in Three Ethnic Subgroups of US Blacks: A Qualitative Study. Journal of the National Medical Association. doi: 10.1016/s0027-9684(15)30406-5. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwede Clement K., Ward Beverly G., Luque John S., Vadaparampil Susan T., Rivers Desiree, Martinez-Tyson Dinorah, Noel-Thomas Shalewa, Meade Cathy D. [accessed May 21, 2011];Application of Geographic Information Systems and Asset Mapping to Facilitate Identification of Colorectal Cancer Screening Resources. Online Journal of Public Health Informatics. 2010b 2(1):2893. doi: 10.5210/ojphi.v2i1.2893. http://ojphi.org/htbin/cgiwrap/bin/ojs/index.php/ojphi/article/view/2893/2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwede Clement K., William Claire M., Thomas Kamilah B., Tarver Will L., Quinn Gwendolyn P., Vadaparampil Susan T., Kim Jongphil, Lee Ji-Hyun, Meade Cathy D. Exploring Disparities and Variability in Perceptions and Self-Reported Colorectal Cancer Screening among Three Ethnic Subgroups of U.S. Blacks. Oncology Nursing Forum. 2010c;37(5):581–591. doi: 10.1188/10.ONF.581-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanneman Robert A., Riddle Mark. [accessed April 5, 2011];Introduction to Social Network Methods. 2005 http://faculty.ucr.edu/~hanneman/
- Hewitt Robert E. Biobanking: The Foundation of Personalized Medicine. Current Opinion in Oncology. 2011;23(1):112–119. doi: 10.1097/CCO.0b013e32834161b8. [DOI] [PubMed] [Google Scholar]
- Kegler Michelle C., Rigler Jessica, Honeycutt Sally. How Does Community Context Influence Coalitions in the Formation Stage? A Multiple Case Study Based on the Community Coalition Action Theory. BMC Public Health. 2010;10:90. doi: 10.1186/1471-2458-10-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kegler Michelle C., Swan Deanne W. An Initial Attempt at Operationalizing and Testing the Community Coalition Action Theory. Health Education and Behavior. 2011;38(3):261–270. doi: 10.1177/1090198110372875. [DOI] [PubMed] [Google Scholar]
- Luque John S., Castañeda Heide, Tyson Dinorah Martinez, Vargas Natalia, Proctor Sara, Meade Cathy D. HPV Awareness among Latina Immigrants and Anglo-American Women in the Southern United States: Cultural Models of Cervical Cancer Risk Factors and Beliefs. NAPA Bulletin. 2010a;34(1):84–104. doi: 10.1111/j.1556-4797.2010.01053.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luque John S., Rivers Brian, Gwede Clement, Kambon Maisha, Green B. Lee, Meade Cathy D. Barbershop Communications on Prostate Cancer Screening Using Barber Health Advisers. American Journal of Men’s Health. 2011a;5(2):129–139. doi: 10.1177/1557988310365167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luque John S., Rivers Brian M., Kambon Maisha, Brookins Ronald, Green B. Lee, Meade Cathy D. Barbers Against Prostate Cancer: A Feasibility Study for Training Barbers to Deliver Prostate Cancer Education in an Urban African American Community. Journal of Cancer Education. 2010b;25(1):96–100. doi: 10.1007/s13187-009-0021-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luque John S., Tyson Dinorah Martinez, Lee Ji-Hyun, Gwede Clement K., Vadaparampil Susan T., Noel-Thomas Shalewa, Meade Cathy D. Using Social Network Analysis to Evaluate Community Capacity Building of a Regional Community Cancer Network. Journal of Community Psychology. 2010c;38(5):656–668. doi: 10.1002/jcop.20386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luque John S., Tyson Dinorah Martinez, Markossian Talar, Lee Ji-Hyun, Turner Rachel, Proctor Sarah, Menard Janelle, Meade Cathy D. Increasing Cervical Cancer Screening in a Hispanic Migrant Farmworker Community through Faith-Based Clinical Outreach. Journal of Lower Genital Tract Disease. 2011b;15(3):200–204. doi: 10.1097/LGT.0b013e318206004a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade Cathy D., Calvo Arlene, Rivera Marlene. Screening and Community Outreach Programs for Priority Populations: Considerations for Oncology Managers. Journal of Oncology Management. 2002;11(5):20–28. [PubMed] [Google Scholar]
- Meade Cathy D., Menard Janelle M., Luque John S., Martinez-Tyson Dinorah, Gwede Clement K. Creating Community-Academic Partnerships for Cancer Disparities Research and Health Promotion. Health Promotion Practice. 2011;12(3):456–462. doi: 10.1177/1524839909341035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Doherty Kieran, Hawkins Alice. Structuring Public Engagement for Effective Input in Policy Development on Human Tissue Biobanking. Public Health Genomics. 2010;13(4):197–206. doi: 10.1159/000279621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penzell Dennis H., Rivera Marlene, Parmer Bert. Forging a Community Health Partnership: Hillsborough County, Florida. Journal of the American Medical Association. 1995;273(15):1173. [PubMed] [Google Scholar]
- Prestby John E., Wandersman Abraham, Florin Paul, Rich Richard, Chavis Chad. Benefits, Costs, Incentive Management and Participation in Voluntary Organizations—A Means to Understanding and Promoting Empowerment. American Journal of Community Psychology. 1990;18(1):117–149. [Google Scholar]
- Provan Keith G., Harvey Jennel, de Zapien Jill G. Network Structure and Attitudes toward Collaboration in a Community Partnership for Diabetes Control on the US-Mexican border. Journal of Health Organization and Management. 2005a;19(6):504–518. doi: 10.1108/14777260510629706. [DOI] [PubMed] [Google Scholar]
- Provan Keith G., Nakama Leigh, Veazie Mark A., Teufel-Shone Nicolette I., Huddleston Carol. Building Community Capacity around Chronic Disease Services through a Collaborative Interorganizational Network. Health Education and Behavior. 2003;30(6):646–662. doi: 10.1177/1090198103255366. [DOI] [PubMed] [Google Scholar]
- Provan Keith G., Veazie Mark A., Staten Lisa K., Teufel-Shone Nicolette I. The Use of Network Analysis to Strengthen Community Partnerships. Public Administration Review. 2005b;65(5):603–613. [Google Scholar]
- Provan Keith G., Veazie Mark A., Teufel-Shone Nicolette I., Huddleston Carol. Network Analysis as a Tool for Assessing and Building Community Capacity for Provision of Chronic Disease Services. Health Promotion Practice. 2004;5(2):174–181. doi: 10.1177/1524839903259303. [DOI] [PubMed] [Google Scholar]
- Schensul Jean J. Organizing Community Research Partnerships in the Struggle against AIDS. Health Education and Behavior. 1999;26(2):266–283. doi: 10.1177/109019819902600209. [DOI] [PubMed] [Google Scholar]
- Scott John P. Social Network Analysis: A Handbook. Sage Publications; Thousand Oaks, CA: 2000. [Google Scholar]
- Shaw-Ridley Mary, Ridley Charles R. The Health Disparities Industry: Is it an Ethical Conundrum? Health Promotion Practice. 2010;11(4):454–464. doi: 10.1177/1524839910375612. [DOI] [PubMed] [Google Scholar]
- Simmons Vani N., Cruz Ligia M., Brandon Thomas H., Quinn Gwen P. Translation and Adaptation of Smoking Relapse-Prevention Materials for Pregnant and Postpartum Hispanic women. Journal of Health Communication. 2011;16(1):90–107. doi: 10.1080/10810730.2010.529492. [DOI] [PubMed] [Google Scholar]
- Singer Helen H., Kegler Michelle C. Assessing Interorganizational Networks as a Dimension of Community Capacity: Illustrations from a Community Intervention to Prevent Lead Poisoning. Health Education and Behavior. 2004;31(6):808–821. doi: 10.1177/1090198104264220. [DOI] [PubMed] [Google Scholar]
- Singer Merrill. Beyond the Ivory Tower: Critical Praxis in Medical Anthropology. Medical Anthropology Quarterly. 1995;9(1):80–106. doi: 10.1525/maq.1995.9.1.02a00060. [DOI] [PubMed] [Google Scholar]
- Stork Diana, Richards William D. Nonrespondents in Communication Network Studies. Group and Organization Management. 1992;17(2):193–209. [Google Scholar]
- Strong Larkin L., Israel Barbara A., Schulz Amy J., Reyes Angela, Rowe Zachary, Weir Sheryl S., Poe Cecil. Piloting Interventions within a Community-Based Participatory Research Framework: Lessons Learned from the Healthy Environments Partnership. Progress in Community Health Partnerships. 2009;3(4):327–334. doi: 10.1353/cpr.0.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torrence William A., Yeary Karen H.-c. K., Stewart Chara, Mehta Paulette, Duke Kelly, Greer-Williams Nancy, Guidry Jeffrey J., Erwin Deborah, Greene Paul, Henry-Tillman Ronda S. Evaluating Coalition Capacity to Strengthen Community-Academic Partnerships Addressing Cancer Disparities. Journal of Cancer Education. doi: 10.1007/s13187-011-0240-0. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente Thomas W. Social Networks and Health: Models, Methods, and Applications. Oxford University Press; New York: 2010. [Google Scholar]
- Valente Thomas W., Chou Chich P., Pentz Mary A. Community Coalitions as a System: Effects of Network Change on Adoption of Evidence-Based Substance Abuse Prevention. American Journal of Public Health. 2007;97(5):880–886. doi: 10.2105/AJPH.2005.063644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente Thomas W., Fujimoto Kayo, Palmer Paula, Tanjasiri Sora Park. A Network Assessment of Community-Based Participatory Research: Linking Communities and Universities to Reduce Cancer Disparities. American Journal of Public Health. 2010;100(7):1319–1325. doi: 10.2105/AJPH.2009.171116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells Kristen J., Battaglia Tracy A., Dudley Donald J., Garcia Roland, Mandelblatt Jeanne S., Paskett Electra D., Raich Peter C. Patient Navigation: State of the Art or is it Science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells Rebecca, Ford Erica W., McClure Jennifer A., Holt Michelle L., Ward Ann. Community-Based Coalitions’ Capacity for Sustainable Action: The Role of Relationships. Health Education and Behavior. 2007;34(1):124–139. doi: 10.1177/1090198105277851. [DOI] [PubMed] [Google Scholar]
- Zakocs Ronda C., Edwards Erica. What Explains Community Coalition Effectiveness?: A Review of the Literature. American Journal of Preventive Medicine. 2006;30(4):351–361. doi: 10.1016/j.amepre.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Zakocs Ronda C., Guckenburg Sarah. What Coalition Factors Foster Community Capacity? Lessons Learned from the Fighting Back Initiative. Health Education and Behavior. 2007;34(2):354–375. doi: 10.1177/1090198106288492. [DOI] [PubMed] [Google Scholar]