Abstract
Many risk factors have been identified as contributing to the development or persistence of low back pain (LBP). However, the juxtaposition of both high and low levels of physical activity being associated with LBP reflects the complexity of the relationship between a risk factor and LBP. Moreover, not everyone with an identified risk factor, such as a movement pattern of increased lumbopelvic rotation, has LBP.
Objective
The purpose of this study was to examine differences in activity level and movement patterns between people with and people without chronic or recurrent LBP who participate in rotation-related sports.
Design Case
Case-control study.
Setting
University laboratory environment.
Participants
52 people with chronic or recurrent LBP and 25 people without LBP who all play a rotation-related sport.
Main Outcome Measures
Participants completed self-report measures including the Baecke Habitual Activity Questionnaire and a questionnaire on rotation-related sports. A 3-dimensional motion-capture system was used to collect movement-pattern variables during 2 lower-limb-movement tests.
Results
Compared with people without LBP, people with LBP reported a greater difference between the sport subscore and an average work and leisure composite subscore on the Baecke Habitual Activity Questionnaire (F = 6.55, P = .01). There were no differences between groups in either rotation-related-sport participation or movement-pattern variables demonstrated during 2 lower-limb movement tests (P > .05 for all comparisons).
Conclusions
People with and people without LBP who regularly play a rotation-related sport differed in the amount and nature of activity participation but not in movement pattern variables. An imbalance between level of activity during sport and daily functions may contribute to the development or persistence of LBP in people who play a rotation-related sport.
A number of different factors, including high and low levels of activity, low muscular fitness, altered movement patterns, changes in muscle activation patterns, increased body mass index, low education and smoking, are frequently associated with an increased risk of having low back pain (LBP).1–9 However, not everyone with LBP demonstrates every identified risk factor, nor does everyone with an identified risk factor develop LBP.1,5,6,8,10 Understanding the complex relationship between LBP and risk factors may be improved through examining the combined effect of identified risk factors. A common principle of tissue mechanics is that individual risk factors sum to create a greater cumulative risk.11–14 This principle may be particularly useful in understanding how multiple risk factors contribute to chronic or recurrent non-specific LBP. The current study examines the relationship between LBP (chronic or recurrent) and the combination of two risk factors: (1) relative contributions of different types of activities to overall activity level, and (2) altered lumbopelvic movement patterns during active limb movement tests.
Physical activity levels can be assessed in many different ways. The use of multiple methods may contribute to contradictory findings in the literature on the association between physical activity and LBP.15–18 A meta-analysis by Lin and colleagues supports the common assumption that lower overall activity levels are associated with chronic LBP.18 In contrast, there is also evidence to suggest that participation in certain types of athletic activity increases the risk of LBP.19,20 This seemingly conflicting evidence on LBP risk can be understood when activity level is defined to include both daily functions and sporting activities. However, there has been no report of how the relative contribution of different types of activities performed throughout the day relate to a LBP problem.17,21 The current study examines habitual activity levels, including sport activities and daily functions, among people who all participate in a sport associated with an increased risk of LBP.
One factor that contributes to LBP symptoms associated with activity may be the lumbopelvic movement patterns used while performing sport activities and daily functions.22–24 A movement pattern is evident when the same lumbopelvic motion, such as rotation, is demonstrated during a variety of tasks, for example kicking or reaching, that provoke LBP symptoms.25 A limb movement test is a standardized method of examining the lumbopelvic movement pattern and LBP symptoms with a simple upper or lower extremity movement. 25,26 During the limb movement test, a person is asked to isolate a component of an extremity motion, which is used during activities that are associated with an increase in LBP symptoms.25,26 For example, the test of active knee flexion performed in prone replicates one component of the motion used during a serve or walking down stairs. People with LBP often demonstrate lumbopelvic motion and report reproduction of LBP during limb movement tests during a clinical examination.22–25 When these tests are modified to decrease the lumbopelvic motion, people report a decrease in LBP symptoms during the limb movement test.24,27 Considering the limb movement test findings, a repeated pattern of lumbopelvic motion with limb movements during daily tasks has the potential to contribute to an accumulation of mechanical stress in tissues of the lumbopelvic region. For example, the mechanical stress in the lumbopelvic region absorbed during a given task is likely to increase during movements of greater speed or greater magnitude of rotation. This increase in mechanical stress may potentially exceed the threshold of tissue maintenance and result in LBP symptoms.12
Rotational forces occurring in the transverse plane are applied to the lumbopelvic region during participation in rotation-related sports. Rotation-related sports (RRS) are defined as sports requiring repeated lumbopelvic rotation, e.g., tennis or golf. Repeated lumbopelvic rotation during RRS participation may contribute to a pattern of increased or earlier lumbopelvic rotation during daily functions. A prior study reported that people with LBP who played a RRS demonstrated greater and earlier lumbopelvic rotation during limb movement tests than people without LBP who did not participate in a RRS.9 Thus, it is unclear if people with LBP who play a RRS demonstrate a movement pattern that is specific to people with LBP or is an adaptation to the rotation-related activity. Prior literature examining differences between athletes and non-athletes suggests the activities people participate in may alter joint ranges of motion, postural sway, and postural stability.28–33 For example, throwers demonstrate differences in shoulder range of motion between the dominant and non-dominant shoulder,30,31 and dancers demonstrate differences in hip range of motion compared to non-dancers.32,33 The greater and earlier lumbopelvic rotation demonstrated during limb movement tests by people with LBP, who play a RRS, may be an adaption to the increased amount and frequency of rotational movement required to play the sport. This movement pattern adaptation, when combined with other factors, such as a low activity level during daily functions, may contribute to a LBP problem.
The purpose of the current study was to examine activity levels related to sport participation and daily function as well as movement patterns in people with and without LBP who regularly play a RRS. We hypothesized that the groups would differ in the relative amount and nature of activities contributing to a person’s overall physical activity level. However due to their similar sports participation, we hypothesized they would demonstrate similar lumbopelvic movement patterns during lower limb movement tests.
Methods
Design
A case-control study design was used to examine differences in activity level and movement patterns between people with and people without LBP at one point in time. The independent variable used to define groups was the presence or absence of LBP. The dependent variables collected to describe these groups were: subscores of the Baecke Habitual Activity Questionnaire, responses to items of a sport-related questionnaire, and the amount and timing of lumbopelvic motion during two lower limb movement tests. Motion analysis was used to measures characteristics of the lower limb movement tests of knee flexion performed in prone and hip lateral rotation performed in prone.
Subjects
Seventy-seven people who participated in a RRS recreationally at least 1–2 hours per week were enrolled in the study. A RRS was defined as a sport that put repeated rotational demands on the trunk and hips during most of the activity (e.g. tennis, racquetball, golf). Twenty-five subjects reported no history of LBP. Fifty-two subjects reported a history of at least 12 months of either (1) chronic LBP, defined as symptoms present on at least half the days in a 12-month period in single or multiple episodes, or (2) recurrent LBP, defined as symptoms present on less than half the days in a 12-month period, occurring in multiple episodes over the year.34 In addition, all subjects with LBP reported an increase in LBP symptoms during or after participation in their sport. People were excluded from the study if they reported a history of a spinal fracture or surgery. They were also excluded if they reported any of the following conditions: spinal stenosis, osteoporosis, disc pathology, significant lower extremity impairment, a systemic inflammatory condition, current pregnancy, or other serious medical condition. An informed consent statement approved by the Washington University School of Medicine Human Studies Committee was read and signed by all subjects before enrolling in the study.
Procedures
Self-Report Measures
All subjects completed self-report measures including (1) a demographic, sport-related, and LBP history questionnaire,35 (2) a verbal numeric pain rating scale,36 and (3) the Baecke Habitual Activity Questionnaire (BHAQ).37 The demographic, sport-related, and LBP history questionnaire included categorical and continuous measures of sport-specific activity that may contribute to the development or persistence of LBP. The questions were modeled after an assessment of lifetime sporting activities described by Videman and colleagues.35 The BHAQ provides a score for overall activity level as well as subscores for activity level during (1) sport, (2) work, and (3) non-sport, leisure activities. Each subscore is reported on a 5-point scale, with 1 representing the lowest level of activity and 5 the highest level of activity.37 The total BHAQ score is the sum of the three subscores (range: 3–15).37 Because our primary interest was in comparing the relative contribution of sporting activities and daily functions to overall activity levels, we calculated a composite subscore to quantify activity level with daily functions. The composite subscore was the average of the work and non-sport leisure subscores (AveWorkLeisure).
Laboratory Measures
Subjects performed two active lower limb movement tests in prone: knee flexion and hip lateral rotation. Knee flexion and hip lateral rotation were examined because: (1) both tests provoke symptoms in people with LBP,22,38 and (2) we have previously reported differences between people with and people without LBP in movement patterns demonstrated during knee flexion and hip lateral rotation.9 Methods for kinematic analyses for both clinical tests have been described previously.9 Briefly, for both tests, subjects were positioned in prone with the hip in neutral abduction/adduction and neutral femoral rotation. At the start of the knee flexion trials, both lower limbs were fully extended; at the start of the hip lateral rotation trials, the knee of the tested limb was flexed to 90°. The subjects performed one trial of each test on the right and left leg separately at a self-selected speed.
Data were collected using a six-camera, three-dimensional, motion capture system (EVaRT, Motion Analysis Corporation, Santa Rosa, CA, USA). Angular displacement (degrees) and velocity (degrees/second) of movement across time were calculated for the limbs and the lumbopelvic region relative to the initial starting position. Limb and lumbopelvic motion were examined from start to maximal angle of limb movement. Lumbopelvic anterior tilt represents rotation of the pelvis in the sagittal plane. Lumbopelvic rotation represents rotation of the pelvis in the transverse plane. In addition to examining maximal angles for lumbopelvic anterior tilt and rotation, a timing variable was calculated for both lumbopelvic motions. Timing of lumbopelvic motion was calculated as the difference in time between the start of the limb movement and the start of the lumbopelvic motion. The time difference was normalized to each subject’s self-selected movement speed by dividing by the total limb movement time.38
Statistical Analyses
All data analyses were performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA). Statistical significance was defined as a two-tailed P-value ≤ 0.05 for all analyses.
Self-Report Measures
Descriptive statistics were calculated for relevant subject characteristics. Self-report variables were analyzed using independent samples t-tests and Chi-square test for independence as appropriate. Independent samples t-tests were used to test for differences between groups on three activity-related variables of the BHAQ (total score, sport subscore, and the composite AveWorkLeisure subscore). A mixed model analysis of variance test was used to assess the difference between activity level during sport activities and daily functions. The between groups factor was group, with two levels, people with LBP and people without LBP. The within groups factor was activity subscores, with two levels, sport and AveWorkLeisure.
Laboratory Measures
Because previous data suggest no differences in limb or lumbopelvic motion between the left and right limb,9 left and right trials of the movement variables were averaged. Independent samples t-tests were used to examine differences between the two groups with regard to (1) maximum angle of knee or hip movement (2) maximum angle of lumbopelvic rotation and anterior tilt, and (3) timing of lumbopelvic rotation and anterior tilt during the limb movement tests of knee flexion and hip lateral rotation.
Results
Self-Report Measures
There were no differences between groups in age, body mass index, sex, hand dominance, family history of LBP, or occupation (Table 1). There were also no differences in number of years of participation in individual or team RRS, amount of strength or endurance training, frequency of play, session duration, primary RRS, or most frequent stroke/swing used (Table 2).
TABLE 1.
Demographics of people with and people without chronic or recurrent low back pain who participate in rotation-related sports.
| Characteristic | People without LBP (N = 25) | People with LBP (N = 52) | Statistical Value, Degrees of Freedom, P-value |
|---|---|---|---|
| Age (y) | 25.5 ± 6.7 | 28.5 ± 8.2 | t = 1.73, df = 57.67a, P = 0.09 |
| Body mass index (kg/m2) | 25.2 ± 3.5 | 24.9 ± 3.5 | t = 0.41, df = 75, P = 0.68 |
| Sex (%) | Male: 76 Female: 24 |
Male: 64 Female: 36 |
χ2 = 1.21, df = 1, P = 0.27 |
| Hand dominance (%) | Right: 92 Left: 8 |
Right: 94 Left: 6 |
χ2 = 0.14, df = 1, P = 0.71 |
| Family history of LBP (%) | Yes: 24 No: 76 |
Yes: 37 No: 63 |
χ2 = 1.21, df = 1, P = 0.27 |
| Level of activity associated with occupationb (%) | Low: 88 Medium: 12 High: 0 |
Low: 92 Medium: 6 High: 2 |
χ2 = 1.36, df = 2, P = 0.51 |
| Type of LBP (%) | NA | Chronic: 40 Recurrent: 60 |
NA |
| duration of LBP (y) | NA | 6.6 ± 5.4 | NA |
| Number of acute flare-ups in previous 12 Monthsc | NA | 7.1 ± 3.8 | NA |
Abbreviation: LBP, low back pain
Values expressed as means ± standard deviation or as otherwise indicated.
Equal variances not assumed
The Baecke Habitual Physical Activity Questionnaire 37 includes a subscale in which the person rates the activity level associated with his occupation on a 3-point scale. Examples of low level activities include office work, teaching, or studying. Examples of medium level activities include factory work, plumbing, or carpentry. Examples of high level activities include dock work or construction work.
All LBP subjects reported a history of at least 12 months of either (1) chronic LBP, defined as symptoms present on at least half the days in a 12-month period in a single or multiple episodes, or (2) recurrent LBP, defined as symptoms present on less than half the days in a 12-month period, occurring in multiple episodes over the year.34
TABLE 2.
Sport participation of people with and people without chronic or recurrent low back pain who participate in rotation-related sports.
| Variable | People without LBP | People with LBP | Statistical Value, Degrees of Freedom, P-value |
|---|---|---|---|
| Participation in | |||
| Individual RRS (y) | 8.4 ± 4.5 | 10.7 ± 7.8 | t = 1.34, df = 73, P = 0.18 |
| Team RRS (y) | 3.7 ± 4.5 | 4.3 ± 5.5 | t = 0.47, df = 72, P = 0.64 |
| Strength training (y) | 5.5 ± 5.1 | 6.2 ± 6.0 | t = 0.49, df = 73, P = 0.63 |
| Endurance training (y) | 5.6 ± 5.7 | 8.0 ± 6.6 | t = 1.56, df = 73, P = 0.12 |
| RRS frequency (times per week) | 2.8 ± 1.6 | 3.1 ± 1.7 | t = 0.73, df = 74, P = 0.47 |
| Duration of each RRS session (min per session) | 78.3 ± 31.2 | 91.0 ± 39.4 | t = 1.38, df = 74, P = 0.17 |
| Primary RRS (%) | Tennis: 63 Racquetball: 29 Squash: 4 Golf: 0 Badminton: 4 |
Tennis: 46 Racquetball: 38 Squash: 12 Golf: 4 Badminton: 0 |
χ = 6.91, df = 6, P = 0.33 |
| Most frequent stroke or swing with RRS (%) | Forehand: 88 Backhand: 8 Serve: 4 Forehand and Backhand: 0 Iron shots: 0 Driving: 0 |
Forehand: 77 Backhand: 6 Serve: 2 Forehand and Backhand: 11 Iron shots: 2 Driving: 2 |
χ = 4.46, df = 5, P = 0.49 |
Abbreviations: LBP, chronic or recurrent low back pain; RRS, rotation-related sport
Values expressed as means ± SD unless otherwise indicated.
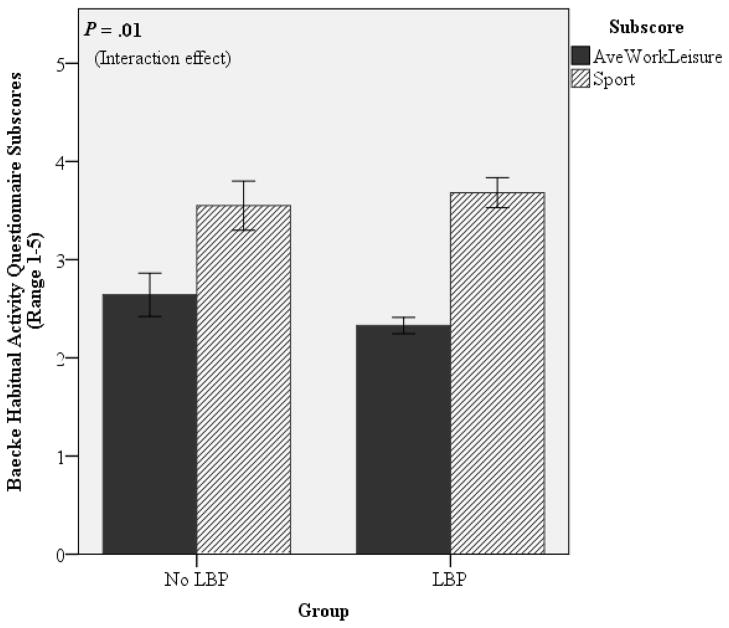
There were no differences in total activity level or sport between people with LBP and people without LBP as reported on the BHAQ (Table 3). When work and non-sport leisure activity levels were combined to examine the average level of activity with daily functions, people with LBP reported being less active than people without LBP (P=0.01, Table 3). When activity level during sports (sport subscore) was compared to activity level during daily functions (AveWorkLeisure composite subscore) the analysis of variance revealed an interaction effect between group and activity (F=6.55, P=0.01; Figure 1). Compared to people without LBP (sport subscore: 3.55 ± 0.61; AveWorkLeisure composite subscore: 2.64 ± 0.54), people with LBP reported a greater difference in activity levels between sports and daily functions (sport subscore: 3.68 ± 0.55, AveWorkLeisure composite subscore: 2.33 ± 0.30, Table 3).
TABLE 3.
Results from the Baecke Habitual Activity Questionnaire for people with and people without chronic or recurrent low back pain.
| Characteristic | People without LBP | People with LBP | Statistical Value, Degrees of Freedom, P-value |
|---|---|---|---|
| Total score (range 3–15)a | 8.84 ± 1.24 | 8.34 ± 0.73 | t = 1.84, df = 32.3b, P = 0.08 |
| Sport subscore (range 1–5)a | 3.55 ± 0.61 | 3.68 ± 0.55 | t = 0.96, df = 75, P = 0.34 |
| AveWorkLeisure composite subscore (range 1–5)c | 2.64 ± 0.54 | 2.33 ± 0.30 | t = 2.73, df = 31.4b, P = 0.01 |
Statistically significant differences are in bold (P ≤0.05)
Abbreviation: LBP, chronic or recurrent low back pain
Values expressed as mean ± standard deviation
Activity level as reported on the Baecke Habitual Activity Questionnaire.37 A higher value indicates greater activity. The total score is the sum of the sport, work and leisure subscores.
Equal variances not assumed
Average of the work and non-sport leisure subscores
Figure 1.
Laboratory Measures
There were no differences between groups in movement pattern variables measured during the limb movement tests of knee flexion or of hip lateral rotation (P>0.05 for all comparisons; Table 4).
TABLE 4.
Means and standard deviations for movement pattern variables calculated during active limb movements in people with and people without chronic or recurrent low back pain.
| People without LBP | People with LBP | |
|---|---|---|
|
Knee Flexion
| ||
| Maximal knee flexion angle | 94.32° ± 28.38° | 107.87° ± 69.67° |
| Maximal lumbopelvic rotation angle | 3.30° ± 1.69° | 3.28° ± 1.76° |
| Maximal anterior pelvic tilt angle | 3.90° ± 2.00° | 3.42° ± 2.02° |
| Timing of lumbopelvic rotation | 0.30 ± 0.18 | 0.25 ± 0.21 |
| Timing of anterior pelvic tilt | 0.30 ± 0.18 | 0.25 ± 0.21 |
|
| ||
|
Hip Lateral Rotation
| ||
| Maximal hip lateral rotation angle | 46.79° ± 5.40° | 44.52° ± 6.47° |
| Maximal lumbopelvic rotation angle | 6.22° ± 2.75° | 5.76° ± 3.00° |
| Timing of lumbopelvic rotation | 0.20 ± 0.13 | 0.21 ± 0.18 |
P>0.1 for all comparisons
Abbreviation: LBP, chronic or current low back pain
Values expressed as mean ± standard deviation
Discussion
The purpose of the current study was to examine activity levels related to sport participation and daily function as well as movement patterns in people with and without LBP who regularly play a RRS. We hypothesized that people with and without LBP would differ in the relative amount and nature of activities contributing to an overall physical activity level, but would demonstrate similar lumbopelvic movement patterns during lower limb movement tests. Consistent with our hypothesis, people with LBP reported lower activity levels with their daily functions (AveWorkLeisure composite subscore of work and non-sport leisure) compared to people without LBP. Interestingly, despite participants reporting a worsening of LBP symptoms with their RRS activity, people with LBP were as active in their sport as people without LBP. Also consistent with our hypothesis, people with and people without LBP who played a RRS demonstrated similar movement patterns during the tests of knee flexion and hip lateral rotation. Thus, the primary difference between groups was that people with LBP had a greater difference in activity levelbetween sports and daily functions than people without LBP. The findings of the current study suggest that a discrepancy in the nature of activities, i.e. a greater difference in activity level between sport activities and daily functions, that contribute to overall activity level concurrent with an altered lumbopelvic movement pattern, may increase a person’s risk for LBP.
The potential effect of this combination of factors to increased risk for LBP is consistent with the principles outlined in the Physical Stress Theory (PST).14 The PST describes how the physical stress level on a tissue is a sum of the direction, time and magnitude of the stress applied to the tissue. In the context of our study, the primary direction (rotation) of the stress on the lumbar tissues and the time-related characteristics (duration, repetition, rate) of the stress associated with sport participation were similar for the two groups (Table 2). However, because there was a larger discrepancy in activity levels between sport activities and daily functions in people with LBP, the relative magnitude of stress with RRS participation may be greater for people with LBP than people without LBP. The result would be that the high velocity, high magnitude trunk movements performed during a RRS may be more likely to exceed the maintenance range of the trunk tissue in people with LBP than in people without LBP, contributing to a cascade of events that result in LBP symptoms.14
There are potential alternative explanations for the greater discrepancy between activity level during sport activities and daily functions in people with LBP compared to people without LBP found in the current study. It is possible that people with LBP simply choose occupations that require less activity throughout the day. In the current study, however, there was no difference in the nature of the occupations between the two groups (Table 1). Both groups reported occupations associated with low to moderate activity levels. It is also possible that people with LBP limit their activity throughout the day to avoid LBP symptoms yet continue to engage in an activity they enjoy (i.e., RRS) even though they experience mild to moderate LBP symptoms during the activity. Although this is a plausible option, it does not negate the importance of the findings of the current study. Whether people are less active during daily functions because of habit or pain avoidance, our data suggests it may be important to maintain a balance between activity level during sport participation and daily functions. This recommendation may be particularly relevant for workers with sedentary jobs, which composed 91% of our sample (Table 1). A study of municipal employees reported that people with more sedentary jobs chose to participate in more physically challenging activities outside of work than people with physically demanding jobs.39 Thus, having a sedentary job may put a person at more risk for LBP because of the discrepancy in the relative contributions of different types of activity to the person’s overall activity level.
Symptoms of LBP also have been related to movement patterns demonstrated during limb movement tests. One group of researchers9 reported that people with LBP who participated in a RRS demonstrated greater and earlier lumbopelvic motion during lower limb movement tests than people without LBP who did not participate in a RRS. In contrast, in the current study all people participated in a RRS and there were no significant differences in movement patterns demonstrated during limb movement tests between people with and people without LBP (Table 4). Interestingly, a comparison to findings from the previous study9 demonstrates that regardless of LBP people in the current study who participated in a RRS demonstrated greater maximal lumbopelvic rotation with knee flexion (LBP/RRS: 3.28° ± 1.76°, No LBP/RRS: 3.30° ± 1.69°) and hip rotation (LBP/RRS: 5.75° ± 3.00°, No LBP/RRS: 6.22° ± 2.75°) than the people without LBP who did not play a RRS in the previous study (lumbopelvic rotation angles: knee flexion: 2.32° ± 1.48°, hip rotation: 4.47° ± 2.55°).9 Also, people who played RRS demonstrated a shorter time difference between the start of the limb motion and the start of the lumbopelvic rotation than people without LBP who did not play a RRS. In the current study people who played RRS demonstrated earlier lumbopevlic rotation during knee flexion (LBP/RRS: 0.25 ± 0.21, No LBP/RRS: 0.30 ± 0.18) and hip rotation (LBP/RRS: 0.21 ± 0.81, No LBP/RRS: 0.20 ± 0.13) in comparison to people without LBP who did not play a RRS in the previous study (timing of lumbopelvic rotation: knee flexion: 0.39 ± 0.33; hip rotation: 0.31 ± 0.26). These data suggest that the increased and earlier lumbopelvic rotation demonstrated by people who participate in a RRS for a similar amount of time per week may be more related to the sporting activity than the presence or absence of LBP symptoms.
The relationship between sport activity and movement patterns proposed in our study is consistent with previously described models and research reports.28,29,40,41 It has been proposed that activities performed repeatedly throughout the day, whether activities of daily living, occupational tasks, or higher-level tasks such as fitness and sport, may produce changes in movement patterns.40,41 Schmit et al28 proposed that ballet dancers demonstrate better postural control than track athletes as a result of their balance-focused classical ballet training. Gymnasts have been reported to demonstrate greater postural stability compared to non-gymnasts.29 Similarly, people who consistently participate in a RRS may develop movement patterns as an adaptation to the sports activity. The cross-sectional nature of these studies limits the ability to determine whether a causal relationship exists between RRS activity and movement patterns. These studies do, however, provide additional evidence to support the importance of these theoretical concepts and the need for further investigation using a prospective, longitudinal study design.
One limitation of the current study is the use of the BHAQ, a self-report measure, as the measurement tool for habitual activity level. Although the BHAQ has been reported to be a reliable tool for different populations including LBP,42–44 its validity in measuring habitual activity level has not been consistently reported. A number of different methods have been used to validate the BHAQ,43–45 however, there is no single measure that is comparable to the intention of the BHAQ, which is to examine habitual activity levels over a period of time rather than activity level or energy expenditure during a particular task.37 A second limitation is the generalizability of the findings to people who perform repetitive activities other than a RRS. In the current study we recruited people who play a RRS at least 1–2 days per week in order to model the relationship between participation in an activity that requires repeated movement in the same direction and a lumbopelvic movement pattern. Further investigation would be necessary to determine whether LBP is associated with a discrepancy in activity levels in individuals who perform other types of repetitive activities, such as work.
Conclusions
People with chronic or recurrent LBP report a greater difference in activity levels between sport activities and the majority of daily functions (work and non-sport leisure) than people without LBP. People with and people without LBP who play RRSs recreationally demonstrate similar movement patterns during lower limb movement tests. The discrepancy between the relative amount and nature of the physical activities contributing to an overall activity level, along with a repetitively used pattern of movement may together contribute to the development or persistence of a LBP problem in people who play a RRS.
Acknowledgments
This work was funded in part by the National Institutes of Health, National Institute of Child Health and Human Development, National Center for Medical Rehabilitation Research, Grant #K01HD-01226, Grant #R01HD047709, and Grant #T32 RR023255, the National Center for Research Resources, Grant # 1 TL1 RR024995-01, and Promotion of Doctoral Studies II and Florence P. Kendal doctoral scholarships from the Foundation for Physical Therapy. The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding sources.
Footnotes
Competing interests
The authors acknowledge that they do not have any financial or personal relationships with other people or organizations that could inappropriately influence the work described in the current manuscript.
Contributor Information
Ruth L. Chimenti, Email: ruth_chimenti@urmc.rochester.edu.
Sara A. Scholtes, Email: sara.scholtes@umontana.edu.
Linda R. Van Dillen, Email: vandillenl@wustl.edu.
References
- 1.Harris-Hayes M, Sahrmann SA, Van Dillen LR. Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil. 2009;18(1):60–75. doi: 10.1123/jsr.18.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodges PW. Changes in motor planning of feedforward postural responses of the trunk muscles in low back pain. Exp Brain Res. 2001;141(2):261–266. doi: 10.1007/s002210100873. [DOI] [PubMed] [Google Scholar]
- 3.Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic region: Effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13(4):361–370. doi: 10.1016/s1050-6411(03)00042-7. [DOI] [PubMed] [Google Scholar]
- 4.Hodges PW, Richardson CA. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80(9):1005–1012. doi: 10.1016/s0003-9993(99)90052-7. [DOI] [PubMed] [Google Scholar]
- 5.Rivinoja AE, Paananen MV, Taimela SP, et al. Sports, smoking, and overweight during adolescence as predictors of sciatica in adulthood: a 28-year follow-up study of a birth cohort. Am J Epidemiol. 2011;173(8):890–897. doi: 10.1093/aje/kwq459. [DOI] [PubMed] [Google Scholar]
- 6.van Oostrom SH, Monique Verschuren WM, de Vet HC, Picavet HS. Ten year course of low back pain in an adult population-based cohort - The Doetinchem Cohort Study. Eur J Pain. 2011;15(9):993–998. doi: 10.1016/j.ejpain.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 7.Khruakhorn S, Sritipsukho P, Siripakarn Y, Vachalathiti R. Prevalence and risk factors of low back pain among the university staff. J Med Assoc Thai. 2010;93 (Suppl 7):S142–S148. [PubMed] [Google Scholar]
- 8.Taanila HP, Suni JH, Pihlajamaki HK, et al. Predictors of low back pain in physically active conscripts with special emphasis on muscular fitness. Spine J. 2012 doi: 10.1016/j.spinee.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Scholtes SA, Gombatto SP, Van Dillen LR. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech. 2009;24(1):7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radebold A, Cholewicki J, Panjabi MM, Patel TC. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine. 2000;25(8):947–954. doi: 10.1097/00007632-200004150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Adams MA, Dolan P. Spine biomechanics. J Biomech. 2005;38(10):1972–1983. doi: 10.1016/j.jbiomech.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 12.McGill SM. The biomechanics of low back injury: Implications on current practice in industry and the clinic. J Biomech. 1997;30(5):465–475. doi: 10.1016/s0021-9290(96)00172-8. [DOI] [PubMed] [Google Scholar]
- 13.Marras WS, Lavender SA, Ferguson SA, Splittstoesser RE, Yang G. Quantitative dynamic measures of physical exposure predict low back functional impairment. Spine. 2010;35(8):914–923. doi: 10.1097/BRS.0b013e3181ce1201. [DOI] [PubMed] [Google Scholar]
- 14.Mueller MJ, Maluf KS. Tissue adaptation to physical stress: A proposed “Physical Stress Theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82(4):383–403. [PubMed] [Google Scholar]
- 15.Sitthipornvorakul E, Janwantanakul P, Purepong N, Pensri P, van der Beek AJ. The association between physical activity and neck and low back pain: A systematic review. Eur Spine J. 2011;20(5):677–689. doi: 10.1007/s00586-010-1630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Weering M, Vollenbroek-Hutten MM, Kotte EM, Hermens HJ. Daily physical activities of patients with chronic pain or fatigue versus asymptomatic controls. A systematic review. Clin Rehabil. 2007;21(11):1007–1023. doi: 10.1177/0269215507078331. [DOI] [PubMed] [Google Scholar]
- 17.Heneweer H, Staes F, Aufdemkampe G, van RM, Vanhees L. Physical activity and low back pain: A systematic review of recent literature. Eur Spine J. 2011;20(6):826–845. doi: 10.1007/s00586-010-1680-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin CW, McAuley JH, Macedo L, Barnett DC, Smeets RJ, Verbunt JA. Relationship between physical activity and disability in low back pain: A systematic review and meta-analysis. Pain. 2011;152(3):607–613. doi: 10.1016/j.pain.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 19.Baranto A, Hellstrom M, Cederlund CG, Nyman R, Sward L. Back pain and MRI changes in the thoraco-lumbar spine of top athletes in four different sports: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1125–1134. doi: 10.1007/s00167-009-0767-3. [DOI] [PubMed] [Google Scholar]
- 20.Sward L. The thoracolumbar spine in young elite athletes. Current concepts on the effects of physical training. Sports Med. 1992;13(5):357–364. doi: 10.2165/00007256-199213050-00005. [DOI] [PubMed] [Google Scholar]
- 21.Hildebrandt VH, Bongers PM, Dul J, van Dijk FJ, Kemper HC. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. 2000;73(8):507–518. doi: 10.1007/s004200000167. [DOI] [PubMed] [Google Scholar]
- 22.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31(8):402–418. doi: 10.2519/jospt.2001.31.8.402. [DOI] [PubMed] [Google Scholar]
- 23.Scholtes SA, Van Dillen LR. Gender-related differences in prevalence of lumbopelvic region movement impairments in people with low back pain. J Orthop Sports Phys Ther. 2007;37(12):744–753. doi: 10.2519/jospt.2007.2610. [DOI] [PubMed] [Google Scholar]
- 24.Van Dillen LR, Sahrmann SA, Norton BJ, Caldwell CA, McDonnell MK, Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84(3):313–322. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 25.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis, MO, USA: Mosby; 2002. [Google Scholar]
- 26.Van Dillen LR, Sahrmann SA, Norton BJ, et al. Reliability of physical examination items used for classification of patients with low back pain. Phys Ther. 1998;78(9):979–988. doi: 10.1093/ptj/78.9.979. [DOI] [PubMed] [Google Scholar]
- 27.Van Dillen LR, Maluf KS, Sahrmann SA. Further examination of modifying patient-preferred movement and alignment strategies in patients with low back pain during symptomatic tests. Man Ther. 2007;88:351–361. doi: 10.1016/j.math.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmit JM, Regis DI, Riley MA. Dynamic patterns of postural sway in ballet dancers and track athletes. Exp Brain Res. 2005;163(3):370–378. doi: 10.1007/s00221-004-2185-6. [DOI] [PubMed] [Google Scholar]
- 29.Carrick FR, Oggero E, Pagnacco G, Brock JB, Arikan T. Posturographic testing and motor learning predictability in gymnasts. Disabil Rehabil. 2007;29(24):1881–1889. doi: 10.1080/09638280601141335. [DOI] [PubMed] [Google Scholar]
- 30.Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- 31.Borsa PA, Dover GC, Wilk KE, Reinold MM. Glenohumeral range of motion and stiffness in professional baseball pitchers. Med Sci Sports Exerc. 2006;38(1):21–26. doi: 10.1249/01.mss.0000180890.69932.15. [DOI] [PubMed] [Google Scholar]
- 32.Hamilton WG, Hamilton LH, Marshall P, Molnar M. A profile of the musculoskeletal characteristics of elite professional ballet dancers. Am J Sports Med. 1992;20(3):267–273. doi: 10.1177/036354659202000306. [DOI] [PubMed] [Google Scholar]
- 33.Gupta A, Fernihough B, Bailey G, Bombeck P, Clarke A, Hopper D. An evaluation of differences in hip external rotation strength and range of motion between female dancers and non-dancers. Br J Sports Med. 2004;38(6):778–783. doi: 10.1136/bjsm.2003.010827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Von Korff M. Studying the natural history of back pain. Spine. 1994;19(18 Suppl):2041S–2046S. doi: 10.1097/00007632-199409151-00005. [DOI] [PubMed] [Google Scholar]
- 35.Videman T, Sarna S, Battie MC, et al. The long-term effects of physical loading and exercise lifestyles on back-related symptoms, disability, and spinal pathology among men. Spine. 1995;20(6):699–709. doi: 10.1097/00007632-199503150-00011. [DOI] [PubMed] [Google Scholar]
- 36.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58(3):387–392. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 37.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 38.Gombatto SP, Collins DR, Sahrmann SA, Engsberg JR, Van Dillen LR. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech. 2006;21(3):263–271. doi: 10.1016/j.clinbiomech.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 39.Ilmarinen J, Louhevaara V, Korhonen O, Nygard CH, Hakola T, Suvanto S. Changes in maximal cardiorespiratory capacity among aging municipal employees. Scand J Work Environ Health. 1991;17 (Suppl 1):99–109. [PubMed] [Google Scholar]
- 40.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. Vol. 1. St. Louis, MO: Mosby, Inc; 2002. Movement impairment syndromes of the lumbar spine; pp. 5–118. [Google Scholar]
- 41.Borsa PA, Laudner KG, Sauers EL. Mobility and stability adaptations in the shoulder of the overhead athlete: A theoretical and evidence-based perspective. Sports Med. 2008;38(1):17–36. doi: 10.2165/00007256-200838010-00003. [DOI] [PubMed] [Google Scholar]
- 42.Jacob T, Baras M, Zeev A, Epstein L. Low back pain: reliability of a set of pain measurement tools. Arch Phys Med Rehabil. 2001;82(6):735–742. doi: 10.1053/apmr.2001.22623. [DOI] [PubMed] [Google Scholar]
- 43.Ono R, Hirata S, Yamada M, Nishiyama T, Kurosaka M, Tamura Y. Reliability and validity of the Baecke physical activity questionnaire in adult women with hip disorders. BMC Musculoskelet Disord. 2007;8:61. doi: 10.1186/1471-2474-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Philippaerts RM, Lefevre J. Reliability and validity of three physical activity questionnaires in Flemish males. Am J Epidemiol. 1998;147(10):982–990. doi: 10.1093/oxfordjournals.aje.a009389. [DOI] [PubMed] [Google Scholar]
- 45.Jacobs DR, Jr, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25(1):81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]