Abstract
PURPOSE
Patients with cognitive impairment (CI) are at high risk of fracture but often denied osteoporosis therapy. We tested whether the effects of zoledronic acid (Zol) on re-fracture and mortality differed in patients presenting with a hip fracture by cognitive status.
METHODS
We used data from the HORIZON Recurrent Fracture Trial, of yearly intravenous 5mg Zol vs. placebo in patients presenting with a hip fracture. Primary outcome was new fracture and secondary outcome mortality.
Short Portable Mental Status Questionnaire (SPMSQ) with a cut-point of >2 was used to identify CI. Fine-Gray models for competing events were fitted to study the effect of Zol on re-fracture and Cox regression for death. A multiplicative term was introduced to study a potential interaction between treatment and cognitive status on outcomes.
RESULTS
1,966/2,127 (92.4%) patients had baseline SPMSQ measured. 350 (17.8%) had CI, balanced between treatment arms. In the placebo arm, there was similar fracture incidence between those with and without CI (15.4% vs. 12.3%, p=0.26). There was no significant interaction for the effect of CI on Zol and re-fracture (p=0.66)). CI was associated with higher 1-year mortality (12.6% vs. 4.3%, p<0.001) and the interaction was bordering significance (interaction p=0.066). Zol prolonged survival only in patients with normal cognitive status (HR 0.56 [95%CI 0.40-0.80]) and not in those with CI (HR 0.90 [95%CI 0.59-1.38]).
CONCLUSIONS
While these results require confirmation, the findings support the use of bisphosphonates in patients with both osteoporotic fracture and CI expected to live for more than 6 months.
Keywords: Fractures, Bone; Mortality; Zoledronic Acid; Dementia; Epidemiology
INTRODUCTION
Hip fractures represent a significant burden to patients, their relatives, the healthcare system and society(1). Secondary fracture prevention has been highlighted internationally as an effective and important healthcare intervention(2). Many patients admitted with an osteoporotic hip fracture have cognitive impairment and this is associated with a higher risk of falls, recurrent multiple fractures, and death(3, 4). Using simulation models, the effect of higher mortality rates appears to be offset by a higher re-fracture rate, favouring the use of osteoporosis therapies in this patient group(5). However, there is little randomised controlled trial data describing the effectiveness of anti-resorptive therapy in patients with cognitive impairment, as most osteoporosis trials excluded those patients unable to give informed consent(6). This has lead to a treatment gap for patients with cognitive impairment not routinely receiving pharmacological secondary fracture prevention(7). This is a concern given the high prevalence of cognitive impairment in patients admitted with osteoporotic hip fracture(8).
The primary aim of the HORIZON Recurrent Fracture Trial was to examine the effect of treatment (zoledronic acid 5mg versus placebo) on time to a new clinical fracture(9). A unique feature of this trial was the inclusion of patients with cognitive impairment using caregiver assent. We a priori hypothesised that heterogeneity may exist whereby the effect of zoledronic acid may differ according to whether or not patients had cognitive impairment. The aim of this study was to conduct a subgroup analysis to examine whether the beneficial effect of zoledronic acid on outcomes of time to clinical fracture and death was attenuated if patients had cognitive impairment compared to those without cognitive impairment.
METHODS
The methods for the Health Outcomes and Reduced Incidence with Zoledronic Acid Once Yearly (HORIZON) Recurrent Fracture Trial have been reported in detail elsewhere(9), and are outlined below.
Study design, interventions and follow-up
The HORIZON Recurrent Fracture Trial was an international, multicentre, randomised, double blind, placebo-controlled trial involving patients with recent hip fracture comparing annual 5mg zoledronic acid vs. placebo intravenous infusion. All patients received daily supplementation with oral calcium (1000 to 1500 mg) and vitamin D (800 to 1200 IU), and those with baseline serum 25-hydroxyvitamin D unknown levels or ≤15 ng/mL received a loading dose of either vitamin D3 or D2 (at a dose of 50,000 to 125,000 IU given orally or intramuscularly) 14 days before first infusion. Participants were followed for up to 5 years using quarterly telephone interviews and attended a yearly clinic visit.
Cognitive status
Cognitive impairment was assessed at baseline using the 10 point Short Portable Mental Status Questionnaire (SPMSQ)(10). In the design of the questionnaire a score greater than 2 errors detects cognitive impairment, and among medical inpatients a cut-off point of >2 errors has a sensitivity of 86% and specificity of 99% for moderate to severe dementia(11).
Outcomes
In this secondary analysis, time from intervention to first clinical fracture is the primary outcome, with time to death being the secondary outcome.
Incident non-vertebral clinical fractures (excluding facial, digital, or skull fractures) were confirmed reviewing radiographic reports, and/or medical records..Incident vertebral fractures were identified by blinded review of both baseline and recent radiographs.
Statistical analyses
For the primary outcome of time to new clinical fracture, we used survival analysis methods to describe the association of treatment on time to new clinical fracture. Given that a high mortality rate would significantly overestimate effect sizes(12), the competing risk of death was accounted for using the method of Fine and Gray(13). For the secondary outcome of time to death, we used Cox proportional hazard regression models. For the primary and secondary outcomes, we performed a pre-specified single test for interaction between the treatment and subgroup (whether or not the patient had cognitive impairment)(14, 15): we introduced a multiplicative term in multivariable models (ie treatment arm × cognitive impairment y/n), after adjustment for confounders (age, gender, ethnic group, Charlson co-morbidity index, and region) and used likelihood ratio test to estimate the p-value for the interaction. A modified Kaplan–Meier method was implemented for the outcome of time to new clinical fracture. In the modified Kaplan–Meier method, individuals who died before the fracture endpoint were not censored at the time of death. Instead they are assigned 4-years follow up time (the end of the observation period) and assumed to be fracture free up to that date(16). All analyses were carried out using Stata version 12.1.
RESULTS
Among a total of 2,127 participants within the HORIZON Recurrent Fracture Trial, data on cognitive status was available for 1,966 (92.4%) patients. Patients with missing SPMSQ data were significantly older, and had more co-morbid conditions (Table 1).
TABLE 1.
Baseline characteristics of eligible participants with and without available data on cognitive status.
| Available SPMSQ |
Missing SPMSQ |
P-value | ||
|---|---|---|---|---|
| N | 1,966 (92.4%) | 161 (7.6%) | ||
| AGE (years) | 74.2 (9.6) | 77.7 (9.4) | <0.001 | |
| MALE GENDER (%) | 1,498 (76.2) | 121 (75.2) | 0.78 | |
| TREATMENT ARM (ZOLEDRONATE) (%) |
977 (49.7) | 88 (54.7) | 0.23 | |
| CAUCASIAN (%) | 1,793 (91.2) | 145 (90.1) | 0.63 | |
| BMI (kg/m2) (SD) | 24.8 (4.4) | 24.1 (4.2) | 0.06 | |
| REGION (%) |
NORTH AMERICA |
537 (27.3) | 86 (53.4) | <0.001 |
| SOUTH AMERICA |
237 (12.1) | 26 (16.2) | ||
| EASTERN EUROPE |
545 (27.7) | 0 (0) | ||
| WESTERN EUROPE |
647 (32.9) | 49 (30.4) | ||
| TOTAL HIP (n=1,687) BMD (g/cm2) (SD) |
0.72 (0.15) | 0.71 (0.15) | 0.73 | |
| FEMORAL NECK (n=1,765) BMD (g/cm2) (SD) |
0.65 (0.14) | 0.61 (0.11) | 0.005 | |
| OP CONCOMITANT MEDICATIONS (%) |
218 (11.1) | 29 (18.0) | 0.008 | |
| CHARLSON INDEX (%) |
1-2 | 376 (19.1) | 20 (13.5) | 0.001 |
| 3-4 | 1,111 (56.6) | 77 (52.0) | ||
| 5-6 | 394 (20.1) | 35 (23.7) | ||
| ≥ 7 | 82 (4.2) | 16 (10.8) | ||
Of those with a recorded SPMSQ, 350 (17.8%) had cognitive impairment and were balanced between zoledronic acid (n=168 [48%]) and placebo (n=182 [52%]) arms. Baseline characteristics for participants with normal and impaired cognitive function are shown in Table 2. Patients with cognitive impairment were significantly older, less likely to be Caucasian, had a lower BMI and a higher Charlson co-morbidity index, but were more likely to have been users of concomitant anti-osteoporosis medications. Those with cognitive impairment who had baseline bone density measurements also had lower bone density at both the total hip and femoral neck.
TABLE 2.
Baseline characteristics of participants stratified by cognitive status.
| Normal cognitive status (SPMSQ ≤2) |
Impaired cognitive status (SPMSQ>2) |
P-value | ||
|---|---|---|---|---|
| N | 1,616 (82.2%) | 350 (17.8%) | ||
| AGE (years) | 73.2 (9.6) | 78.9 (8.3) | <0.001 | |
| FEMALE GENDER (%) | 392 (24.3) | 76 (21.7) | 0.31 | |
| TREATMENT ARM (ZOLEDRONATE) (%) |
809 (50.1) | 168 (48.0) | 0.49 | |
| CAUCASIAN (%) | 1,488 (92.1) | 305 (87.1) | 0.003 | |
| BMI (kg/m2) (SD) | 24.9 (4.4) | 24.3 (4.5) | 0.016 | |
| REGION (%) |
NORTH AMERICA |
378 (23.4) | 159 (45.4) | <0.001 |
| SOUTH AMERICA |
183 (11.3) | 54 (15.4) | ||
| EASTERN EUROPE |
518 (32.1) | 27 (7.7) | ||
| WESTERN EUROPE |
537 (33.2) | 110 (31.4) | ||
| TOTAL HIP (n=1,687) BMD (g/cm2) (SD) |
0.73 (0.15) | 0.67 (0.19) | <0.001 | |
| FEMORAL NECK (n=1,765) BMD (g/cm2) (SD) |
0.66 (0.13) | 0.62 (0.16) | <0.001 | |
| FN T score <= −2.5 (%) | 653 (40.4) | 185 (52.9) | <0.001 | |
| OP CONCOMITANT MEDICATIONS (%) |
167 (10.3) | 51 (14.6) | 0.022 | |
| CHARLSON INDEX (%) |
1-2 | 344 (21.3) | 32 (9.2) | <0.001 |
| 3-4 | 944 (58.5) | 167 (48.0) | ||
| 5-6 | 281 (17.4) | 113 (32.5) | ||
| ≥ 7 | 46 (2.9) | 36 (10.3) | ||
Legend: Charlson Index of co-morbidity
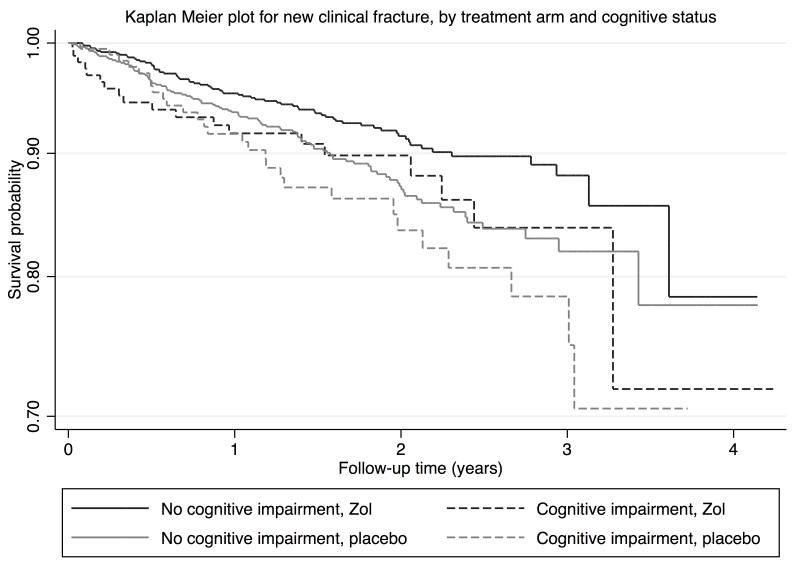
The rates of re-fracture and death in treatment and placebo arms of the trial are shown in Table 3. In the placebo arm, there was no significant difference in the incidence of new clinical fracture between patients with and without cognitive impairment (p=0.26). Further, there was no evidence of interaction between treatment allocation and cognitive impairment (p = 0.66) on clinical fracture risk in the competing risks regression model: SHR for the effect of Zoledronate on clinical fracture risk in participants with and without cognitive impairment was of 0.84 [95%CI 0.42 to 1.66] and 0.74 [95%CI 0.53 to 1.02] respectively (Figure 1). The proportional sub-hazards assumption was satisfied when introducing treatment and cognitive impairment as time-varying covariates in the model.
TABLE 3.
FRACTURE INCIDENCE, MORTALITY RATES BY COGNITIVE STATUS AND TREATMENT ARM
| Normal cognitive function (SPMSQ ≤2) |
Impaired cognitive function (SPMSQ >2) |
||
|---|---|---|---|
| N = 1,616 | N = 350 | ||
| Outcome | N (%) participants with the event of interest |
N (%) participants with the event of interest |
Chi- square p-value |
|
Clinical
fracture |
|||
| All | 168 (10.4%) | 47 (13.4%) | 0.099 |
| Zoledronic acid arm |
69 (8.5%) | 19 (11.3%) | 0.25 |
| Placebo arm | 99 (12.3%) | 28 (15.4%) | 0.26 |
| Death | |||
| All | 135 (8.4%) |
88 (25.1%) |
<0.001 |
| Zoledronic acid arm |
50 (6.2%) |
39 (23.2%) |
<0.001 |
| Placebo arm | 85 (10.5%) |
49 (26.9%) |
<0.001 |
N = Number of patients
FIG 1.
MODIFIED KAPLAN-MEIER ESTIMATORS FOR INCIDENT FRACTURE: TREATMENT EFFECT STRATIFIED ON COGNITIVE STATUS
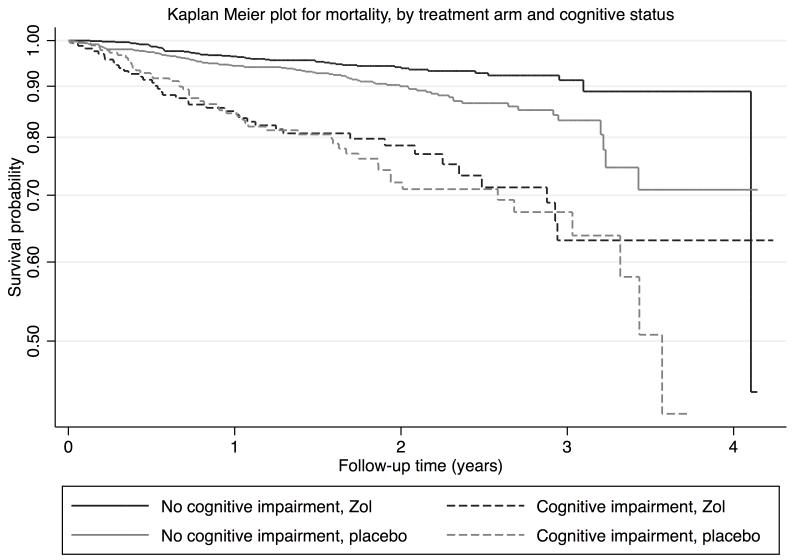
For mortality, rates were higher in those with cognitive impairment compared with normal cognition (six month and one year mortality: 6.6% vs. 1.2%, and 12.6% vs. 4.3% respectively; Table 2). For time to death, there was weak evidence of an interaction between treatment and cognitive impairment (p=0.066). Schoenfelds residuals suggested the proportional hazards assumption was satisfied. The survival effect of zoledronic acid treatment was significant in those without cognitive impairment (HR 0.56 [95%CI 0.40 to 0.80]) compared to the cognitively impaired (HR 0.90 [95%CI 0.59 to 1.38]) (Figure 2). Only about 5% of patients had the infusion within 14 days of the hip fracture and excluding these did not change the findings (data not shown).
FIG 2.
MODIFIED KAPLAN-MEIER ESTIMATORS FOR DEATH: TREATMENT EFFECT STRATIFIED ON COGNITIVE STATUS
DISCUSSION
There is an evidence gap demonstrating efficacy of secondary fracture prevention in patients with cognitive impairment. While we were unable to demonstrate a statistically significant difference in outcomes by cognitive status, the beneficial effect of zoledronic acid appeared to be maintained for fracture reduction in those with cognitive impairment. This was despite patients with cognitive impairment having many more risk factors for fractures and falls when compared with those with normal cognitive function. In contrast, there was a suggestion that the effect of zoledronic acid to improve survival did differ, with a significant survival advantage in patients with no cognitive impairment and no benefit in those with cognitive impairment.
The two cornerstones of secondary fracture prevention are falls prevention and bone health. The benefits of fall-prevention programmes remain controversial in individuals with moderate/severe dementia(17). Hence, improving bone health remains the major focus for secondary fracture prevention in the cognitively impaired population. One concern is the ability of cognitively impaired patients to consistently follow the complicated administration regimes for oral bisphosphonates, as this may not only severely limit drug bioavailability,(18) but also has the potential for adverse events if not adequately followed. Other reasons for non-treatment in this group include polypharmacy concerns and under-recognition of fracture risk8. The advent of parenteral therapies therefore represented a major therapeutic advance in the field(6). However, the systematic use of zoledronic acid in those with cognitive impairment has been tempered due to concerns that patients do not live long enough to benefit from the fracture reduction benefit of treatment. These data suggest that the effect of fracture reduction with zoledronic acid therapy does not differ by cognitive status.
A number of studies have demonstrated that those who have cognitive impairment and are admitted with a hip fracture have a range of poorer outcomes including prolonged length of stay(19), in hospital complications, lower rehabilitation success(20, 21), poorer post discharge ambulation(22) and higher mortality of up to 55% at 6 months (23-25). This has led to validated scores to predict mortality after hip fractures in the elderly such as the Nottingham Hip Fracture Score(26). However, on an individual level, the discrimination of these scores is sub-optimal, with up to 55% of those in the highest risk group still alive at one year(27). Further, the mortality after hip fracture appears to be improving over the recent years as demonstrated by the National Hip Fracture Database(28).
Whilst one study has demonstrated a potential reduction in fracture in those with cognitive impairment who were prescribed daily risedronate and ergocalciferol(29), the study’s validity has been questioned(30). This analysis for the first time demonstrates in a placebo-controlled trial that patients with cognitive impairment may still benefit from an extended fracture free time with zoledronic acid compared with those receiving placebo.
In common with the parent study, we were able to demonstrate a significant survival advantage with zoledronic acid, but this was limited to only those with normal cognitive function on entry to the study and of a higher magnitude (42%). Previous work has identified that pneumonia and arrhythmias were significantly reduced in those who received zoledronic acid even after adjusting for a wide range of potential confounders(31).
Strengths and Limitations
HORIZON is one of few robust, randomised, double blind placebo controlled trials with patients with cognitive impairment in this area of medicine. This study is based on a subgroup analysis of the parent trial. It is recognised that credible subgroup effects may enhance benefits and reduce harm and unnecessary use of health resources, and recently a set of criteria for judging the results from subgroup analyses has been published(32). The major strength of this study is that we defined the research question based on biological rationale before the data was analysed, so reducing the risk of type I error(33) Rather than looking for significance in each subgroup separately, we tested the hypothesis that the effect of zoledronate differed by subgroup using an interaction term(14). In terms of criteria for the subgroup analysis(15), cognitive impairment was recorded at baseline and, while not specified a priori to trial initiation, was specified prior to data analysis.
A major limitation is that we then lacked power to demonstrate statistically significant differences in the interaction term and the effect of zoledronic acid on the subgroup of patients with cognitive impairment. However, we believe the effects we found remain of clinical importance given difficulty in recruiting this high-risk population and the limited current level of evidence. Unfortunately, the measure of cognitive impairment was made only at baseline. Hence, we were unable to examine the chronicity of cognitive impairment and potentially misclassified those who then went on to develop incident cognitive impairment after their baseline assessment, or those only temporarily confused at the time of surgery. This would bias our findings to the null. Also, about 7.5% of the study participants had missing data on cognitive status, and these are potentially the patients with a more severe cognitive impairment.
No reliable data on vitamin D supplementation was available, and we therefore cannot explore how this would modify our findings.
Further, the rates of mortality found were lower than those reported in the literature. This probably reflects the fact that the investigators excluded those patients with a survival of less than 6 months, and the overall better health status of patients recruited to clinical trials. Finally, data on cause of death was lacking, and therefore we were unable to explore whether the observed heterogeneity in mortality reduction were due to different causes of death in the cognitively impared.
Conclusions
In patients admitted with a hip fracture, the reduction in future fracture rates by zoledronic acid was similar in those with and without cognitive impairment even with large differences in mortality rate. Given the rising prevalence of cognitive impairment in patients presenting with osteoporotic hip fracture, these exploratory findings urgently require confirmation in future trials but, in the interim, support the use of bisphosphonate therapy in those with cognitive impairment expected to live for more than 6 months.
Acknowledgements
We wish to thank the patients, carers and research staff involved in the original trial and Professor A Munoz for his advice on competing risk models.
Funding
While the parent study was sponsored by Novartis Pharmaceuticals Corporation and Novartis Pharma AG, the origination of the research question, statistical methodology, analysis and interpretation of the data, and authoring of the manuscript were performed independently by the Oxford NIHR Musculoskeletal Biomedical Research Unit, University of Oxford, UK. The pre-submission manuscript was sent to Novartis Pharmaceuticals Corporation for comment.
Footnotes
Disclosures and Competing interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that: 1.DPA and AJ have no conflicts of interest to declare; 2.MKJ, NKA and CC have received honorarium, advisory boards and consortium research grants respectively from: Novartis, Alliance for Better Health and Lilly; Merck, MSD, Roche, Novartis, Smith and Nephew, Q-MED, Nicox, Servier, GSK, Schering-Plough, Pfizer and Rottapharm; Alliance for Better Bone Health, Amgen, Novartis, MSD, Servier, Eli Lilly and GSK; 3. Dr. Lyles reports receiving grant support from Novartis, the Alliance for Better Bone Health (Sanofi-Aventis and Procter & Gamble), and Amgen, consulting fees from Novartis, Procter & Gamble, Merck, Amgen, GTx, GlaxoSmithKline, Eli Lilly and Bone Medical, and being listed as an inventor on a U.S. patent application (20050272707) covering methods for preventing or reducing secondary fractures after hip fracture and on another provisional patent application for medication kits and formulations for preventing, treating, or reducing secondary fractures after a previous fracture; and 4. their spouses, partners, or children have no financial relationships that may be relevant to the submitted work.
Ethics approval
Informed consent was obtained from subjects, and investigations were approved by an institutional human research committee. The study was conducted according to the ethical principles of the 1989 Declaration of Helsinki and local applicable laws and regulations.
Trial registration
CLINICALTRIALS.GOV NUMBER, NCT00046254
REFERENCES
- 1.Ström O, Borgström F, Kanis J, Compston J, Cooper C, McCloskey E, Jönsson B. Osteoporosis: burden, health care provision and opportunities in the EU. Archives of Osteoporosis. :1–97. doi: 10.1007/s11657-011-0060-1. [DOI] [PubMed] [Google Scholar]
- 2.Marsh D, Akesson K, Beaton DE, Bogoch ER, Boonen S, Brandi ML, McLellan AR, Mitchell PJ, Sale JE, Wahl DA. Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int. 2011;22:2051–2065. doi: 10.1007/s00198-011-1642-x. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd BD, Williamson DA, Singh NA, Hansen RD, Diamond TH, Finnegan TP, Allen BJ, Grady JN, Stavrinos TM, Smith EU, Diwan AD, Fiatarone Singh MA. Recurrent and injurious falls in the year following hip fracture: a prospective study of incidence and risk factors from the Sarcopenia and Hip Fracture study. J Gerontol A Biol Sci Med Sci. 2009;64:599–609. doi: 10.1093/gerona/glp003. [DOI] [PubMed] [Google Scholar]
- 4.Beringer TR, Clarke J, Elliott JR, Marsh DR, Heyburn G, Steele IC. Outcome following proximal femoral fracture in Northern Ireland. Ulster Med J. 2006;75:200–206. [PMC free article] [PubMed] [Google Scholar]
- 5.Curtis JR, Arora T, Matthews RS, Taylor A, Becker DJ, Colon-Emeric C, Kilgore ML, Morrisey MA, Saag KG, Safford MM, Warriner A, Delzell E. Is withholding osteoporosis medication after fracture sometimes rational? A comparison of the risk for second fracture versus death. J Am Med Dir Assoc. 2010;11:584–591. doi: 10.1016/j.jamda.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 7.Vik SA, Jantzi M, Poss J, Hirdes J, Hanley DA, Hogan DB, Maxwell CJ. Factors associated with pharmacologic treatment of osteoporosis in an older home care population. J Gerontol A Biol Sci Med Sci. 2007;62:872–878. doi: 10.1093/gerona/62.8.872. [DOI] [PubMed] [Google Scholar]
- 8.Haasum Y, Fastbom J, Fratiglioni L, Johnell K. Undertreatment of osteoporosis in persons with dementia? A population-based study. Osteoporos Int. 2012;23:1061–1068. doi: 10.1007/s00198-011-1636-8. [DOI] [PubMed] [Google Scholar]
- 9.Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–1809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 11.Erkinjuntti T, Sulkava R, Wikstrom J, Autio L. Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly. J Am Geriatr Soc. 1987;35:412–416. doi: 10.1111/j.1532-5415.1987.tb04662.x. [DOI] [PubMed] [Google Scholar]
- 12.Berry SD, Ngo L, Samelson EJ, Kiel DP. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc. 2010;58:783–787. doi: 10.1111/j.1532-5415.2010.02767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fine JP, Gray RJ. A proportional hazards model for the subdistributions of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 14.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326:219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun X, Briel M, Walter SD, Guyatt GH. Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ. 2010;340:c117. doi: 10.1136/bmj.c117. [DOI] [PubMed] [Google Scholar]
- 16.Leslie WD, Lix LM, Wu X. Competing mortality and fracture risk assessment. Osteoporos Int. 2012;24:681–688. doi: 10.1007/s00198-012-2051-5. [DOI] [PubMed] [Google Scholar]
- 17.Tinetti ME, Kumar C. The patient who falls: “It’s always a trade-off”. JAMA. 2010;303:258–266. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gertz BJ, Holland SD, Kline WF, Matuszewski BK, Freeman A, Quan H, Lasseter KC, Mucklow JC, Porras AG. Studies of the oral bioavailability of alendronate. Clin Pharmacol Ther. 1995;58:288–298. doi: 10.1016/0009-9236(95)90245-7. [DOI] [PubMed] [Google Scholar]
- 19.Ensberg MD, Paletta MJ, Galecki AT, Dacko CL, Fries BE. Identifying elderly patients for early discharge after hospitalization for hip fracture. J Gerontol. 1993;48:M187–195. doi: 10.1093/geronj/48.5.m187. [DOI] [PubMed] [Google Scholar]
- 20.Heruti RJ, Lusky A, Barell V, Ohry A, Adunsky A. Cognitive status at admission: does it affect the rehabilitation outcome of elderly patients with hip fracture? Arch Phys Med Rehabil. 1999;80:432–436. doi: 10.1016/s0003-9993(99)90281-2. [DOI] [PubMed] [Google Scholar]
- 21.Cree M, Carriere KC, Soskolne CL, Suarez-Almazor M. Functional dependence after hip fracture. Am J Phys Med Rehabil. 2001;80:736–743. doi: 10.1097/00002060-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Hirose J, Ide J, Yakushiji T, Abe Y, Nishida K, Maeda S, Anraku Y, Usuku K, Mizuta H. Prediction of postoperative ambulatory status 1 year after hip fracture surgery. Arch Phys Med Rehabil. 2010;91:67–72. doi: 10.1016/j.apmr.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Ceder L, Elmqvist D, Svensson SE. Cardiovascular and neurological function in elderly patients sustaining a fracture of the neck of the femur. J Bone Joint Surg Br. 1981;63B:560–566. doi: 10.1302/0301-620X.63B4.7298685. [DOI] [PubMed] [Google Scholar]
- 24.Wood DJ, Ions GK, Quinby JM, Gale DW, Stevens J. Factors which influence mortality after subcapital hip fracture. J Bone Joint Surg Br. 1992;74:199–202. doi: 10.1302/0301-620X.74B2.1544951. [DOI] [PubMed] [Google Scholar]
- 25.Evans JG, Prudham D, Wandless I. A prospective study of fractured proximal femur: factors predisposing to survival. Age Ageing. 1979;8:246–250. doi: 10.1093/ageing/8.4.246. [DOI] [PubMed] [Google Scholar]
- 26.Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–517. doi: 10.1093/bja/aen236. [DOI] [PubMed] [Google Scholar]
- 27.Wiles MD, Moran CG, Sahota O, Moppett IK. Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br J Anaesth. 2011 doi: 10.1093/bja/aeq405. [DOI] [PubMed] [Google Scholar]
- 28.Currie C, Partridge M, Plant F, Roberts J, Wakeman R, Williams A. In: The National Hip Fracture Database Natioanl Report 2011. Partnership HQI, editor. 2011. [Google Scholar]
- 29.Sato Y, Kanoko T, Satoh K, Iwamoto J. The prevention of hip fracture with risedronate and ergocalciferol plus calcium supplementation in elderly women with Alzheimer disease: a randomized controlled trial. Arch Intern Med. 2005;165:1737–1742. doi: 10.1001/archinte.165.15.1737. [DOI] [PubMed] [Google Scholar]
- 30.Halbekath JM, Schenk S, von Maxen A, Meyer G, Muhlhauser I. Risedronate for the prevention of hip fractures: concern about validity of trials. Arch Intern Med. 2007;167:513–514. doi: 10.1001/archinte.167.5.513-b. author reply 514-515. [DOI] [PubMed] [Google Scholar]
- 31.Colon-Emeric CS, Mesenbrink P, Lyles KW, Pieper CF, Boonen S, Delmas P, Eriksen EF, Magaziner J. Potential mediators of the mortality reduction with zoledronic acid after hip fracture. J Bone Miner Res. 2010;25:91–97. doi: 10.1359/jbmr.090704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sun X, Briel M, Busse JW, You JJ, Akl EA, Mejza F, Bala MM, Bassler D, Mertz D, Diaz-Granados N, Vandvik PO, Malaga G, Srinathan SK, Dahm P, Johnston BC, Alonso-Coello P, Hassouneh B, Walter SD, Heels-Ansdell D, Bhatnagar N, Altman DG, Guyatt GH. Credibility of claims of subgroup effects in randomised controlled trials: systematic review. BMJ. 2012;344:e1553. doi: 10.1136/bmj.e1553. [DOI] [PubMed] [Google Scholar]
- 33.Oxman AD. Subgroup analyses. BMJ. 2012;344:e2022. doi: 10.1136/bmj.e2022. [DOI] [PubMed] [Google Scholar]