Abstract
Purpose
To effectively evaluate activity-based interventions for weight management and disease risk reduction, objective and accurate measures of exercise dose are needed. This study examined cumulative exercise exposure defined by heart rate-based intensity, duration, and frequency as a measure of compliance with a prescribed exercise program and a predictor of health outcomes.
Methods
1,150 adults (21.3 ± 2.7 yrs) completed a 15-week exercise protocol consisting of 30 min/day, three days/wk at 65–85% maximum heart rate reserve (HRR). Computerized HR monitor data were recorded at every exercise session (33,473 valid sessions). To quantify total exercise dose, duration for each session was adjusted for average exercise intensity (%HRR) to create a measure of intensity-minutes for each workout, which were summed over all exercise sessions to formulate a heart rate physical activity score (HRPAS). Regression analysis was used to examine the relationship between HRPAS and physiological responses to exercise training. Compliance with the exercise protocol based on achievement of the minimum prescribed HRPAS was compared to adherence defined by attendance.
Results
Using HRPAS, 868 participants were empirically defined as compliant, and 282 were non-compliant. HRPAS-based and attendance-based classifications of compliance and adherence differed for approximately 9% of participants. Higher HRPAS was associated with significant positive changes in body mass (p<0.001), BMI (p<0.001), waist and hip circumferences (p<0.001), percent body fat (%Fat, p<0.001), systolic blood pressure (p<0.011), resting heart rate (RHR, p<0.003), fasting glucose (p<0.001), and total cholesterol (p<.02). Attendance-based adherence was associated with body mass, hip circumference, %Fat, RHR, and cholesterol (p<0.05).
Conclusions
The HRPAS is a quantifiable measure of exercise dose associated with improvement in health indicators beyond that observed when adherence is defined as session attendance.
Keywords: heart rate, physical activity, monitoring, dropout, attrition, compliance
Introduction
The health benefits associated with physical activity are well-established (17), and the magnitude of health improvements generally increases as the volume of activity is increased (18). However, a central issue for understanding the impact of physical activity exposure, or dose, on fitness and health outcomes is the ability to empirically evaluate and compare the actual dose to the recommended or prescribed dose of physical activity (22). Factors that influence biological adaptability to exercise may also influence exercise tolerance (4) and may help to define which exposures will be effective for sustaining participation. For example, higher intensity has been associated with greater improvements in health and fitness and increased longevity (8, 14, 20), but also with potentially poorer adherence (7, 19). As stated in the 2008 Physical Activity Guidelines, studies that evaluate the effects of intensity, frequency, duration, and multiple exercise bouts are needed to fill the gaps in our knowledge about dose response (17). Recent research has provided evidence that up to 7% of individuals exposed to physical activity may actually experience deleterious health outcomes (3). Thus, the ability to quantify total exercise exposure is a critical factor for identifying individuals most likely to respond, positively or negatively, to exercise training.
The intensity, frequency, and duration of physical activity and exercise sum to a total volume of exposure (10, 17). Although about 60% of US adults report meeting the recommended volume of physical activity (~500 MET minutes/week) (25), less than 5% meet the physical activity criterion when physical activity volume is estimated objectively by an accelerometer (24). Moreover, similarly objective estimates show less than 2.5% of Americans meet recommendations for vigorous physical activity necessary to improve fitness (25).
Population studies have largely relied on participant recall and crude estimates of intensity derived from physical activity types (1) or from motion detectors that do not indicate the intensity of exercise relative to a person’s level of fitness. Early clinical trials of exercise commonly reported that nearly half the participants dropped out before healthful adaptations could occur, or be identified (16). Many efficacy trials report high adherence rates (e.g., 75–85% of the prescribed number of sessions in trials lasting six to 24 months), but trials rarely report the extent to which participants who attend also comply with the prescribed intensities and durations of exercise, despite early recommendations that this be done (15). The use of objective measures of intensity, duration, frequency, and total volume of physical activity exposure in population studies has been identified as a key research need (17).
Heart rate monitoring is an objective, relatively inexpensive measure that has been used to successfully evaluate exercise intensity and duration among both healthy and medically-ill adults (5, 12, 21); it thus provides information about the volume of exercise that can be used to judge compliance beyond that provided by measures of session attendance or frequency of exposure (12). Here we report the development and application of an empirical measure of exercise compliance using heart rate monitor-based measures of intensity, duration, and frequency in a large prospective study of young adults undergoing 15 weeks of aerobic exercise training. Heart rate monitor data were utilized to compute total exercise dose in the form of a heart rate physical activity score (HRPAS, described below), which was used to objectively assess compliance with the exercise prescription. Health-related outcomes were examined for association to the HRPAS and compared between compliant and non-compliant individuals and with adherence defined by attendance alone.
Methods
Study Design and Sample
The Training Interventions and Genetics of Exercise Response (TIGER) Study is a prospective cohort study with the goals of introducing sedentary college-aged adults to regular exercise and identifying genetic factors that influence physiological responses to exercise training and exercise adherence. The target participant for the TIGER study is a sedentary (i.e., < 30 minutes activity/week for the previous 30 days prior to enrollment) individual who was not restricting energy intake for weight loss. Exclusion criteria included having a physical contraindication to aerobic exercise (e.g., cardiomyopathy), a metabolic condition that may alter body composition, and/or pregnancy. All participants provided written informed consent, and the study protocol was approved by the Institutional Review Boards at University of Houston (UH), Baylor College of Medicine, and the University of Texas Health Science Center at Houston.
To meet contemporary guidelines for vigorous activity (17), prescribed aerobic exercise training included three 30-minute exercise sessions/week at 65%–85% of age- and gender-predicted maximum heart rate reserve (HRR) for 15 weeks using the subject’s choice of treadmill, elliptical trainer, stair stepper, or exercise bike. Participants were permitted to exercise more frequently and for longer durations (up to 60 minutes) than the prescribed 30 minutes. During each exercise session, participants wore portable heart rate monitors (Polar Electro, Lake Success, NY), and mode of exercise was documented. The monitors recorded minute-to-minute heart rate, date, time, and duration for each exercise session and have been shown to provide a valid measure of exercise heart rate (13). Data from the heart rate monitors for each participant were downloaded into the manufacturer’s software program (E-Series, Polar Electro, Lake Success, NY) and merged with attendance files to formulate a comprehensive database of exercise parameters. Participants were required to complete a minimum of 25 minutes within their target heart rate zone (THRZ) for an exercise session to be considered valid.
Physiological testing was completed at baseline and after 15 weeks of training. Stature was measured to the nearest centimeter using a free-standing stadiometer (SECA Road Rod, Snoqualmie, WA), and body mass was measured to the nearest 0.1 kg using a digital scale (SECA 770, Hanover, MD). Percent body fat (%Fat) was estimated using dual energy X-ray absorptiometry (DXA, Hologic, Bedford, MA), and body mass index (BMI) was calculated from stature and body mass (kg/m2). Resting blood pressure (BP) was measured three times using a digital blood pressure monitor (Omron HEM 907; Omron Healthcare, Inc., Bannockburn, IL) and calculated from the average of the second and third measures taken after the participant had been sitting quietly for at least 5 min. Phlebotomy was performed following an overnight fast, and blood samples were collected from a peripheral arm vein into evacuated tubes treated with EDTA. Plasma was separated from the packed cells by centrifugation, aliquoted, and frozen (− 80°C) until further analysis. Plasma was analyzed for total cholesterol using a portable analyzer (Cardio-Check, Brooklyn, NY) and standard chemistry based on the Trinder Method (23) and for glucose using a calibrated glucose analyzer (YSI 2300 Stat Plus; Yellow Spring, OH).
Calculation of Exercise Dose
Approximately 83.2% (27,883/33,473) of the attendance records documented during the semester had usable heart rate observations. The remaining 16.8% of attendance records had either missing or unusable heart rate data, due primarily to technical errors with the monitors. Because the participants were known to have exercised during the sessions that were missing heart rate data, values for the missing/excluded exercise data were imputed based on the within-participant distributions of duration and average heart rate across all non-missing exercise sessions. For each documented (based on attendance records) exercise session for which heart rate monitor data were unavailable, a randomly-generated z-score value was converted to an imputed parameter value based on the within-subject mean and standard deviation of the exercise parameter values (e.g., average heart rate, duration), under the assumption that the data were missing at random. Imputation of missing values required that valid data be available for at least 60% of all possible exercise sessions for each subject. Imputed values that were outliers from the original exercise parameter distributions across all participants were eliminated, and imputed values were re-calculated. Following imputation, the distributions of average heart rate and duration with and without imputed values were statistically compared; this imputation approach was demonstrated to produce unbiased values with respect to means, variances, homoscedasticity, and kurtosis.
To quantify total exercise dose, duration for each session was adjusted for average exercise intensity (percent HRR) to create a measure of intensity-minutes for each workout, which were summed over all exercise sessions to formulate the HRPAS. Exercise duration was recorded as the time the monitor was stopped minus the time the monitor was started. Because resting heart rate is difficult to measure accurately and consistently across subjects, percent of predicted heart rate reserve (%HRR) was estimated by dividing average exercise heart rate (ExHR) by each individual’s age- and gender-predicted maximum HRR, using gender-specific constants for resting heart rate, as described elsewhere (2, 11). The HRPAS was calculated in two steps. A workout heart rate physical activity score (W-HRPAS) was first calculated for each exercise session by adjusting exercise duration in minutes (ExMin) by exercise intensity:
W-HRPAS = %HRR * ExMin.
Exercise frequency was determined by the number of exercise sessions attended across 15 weeks, and the HRPAS was then calculated as the sum of each W-HRPAS across the entire 15-week program:
HRPAS = Σ W-HRPAS.
Total available sessions for each cohort varied due to differences in semester length and weather-related university closures and consisted of 34, 30, 36, and 37 sessions, respectively for each of the four cohorts examined in this study. These exercise sessions occurred over a period of 15 weeks. In order to compare values across cohorts, a normalized HRPAS, adjusted for the different numbers of possible workouts in each cohort, was also calculated.
HRPAS as a Measure of Compliance
Compliance was evaluated by comparing observed HRPAS values to prescribed HRPAS values based on a minimum %HRR of 65% for at least 30 minutes per session. For example, the prescribed HRPAS for a total of 34 sessions was equal to:
65%*30 min/session*34 sessions = 663
Compliance was defined as an observed HRPAS equal to or greater than this prescribed HRPAS.
In order to compare the HRPAS as a measure of compliance to a simple attendance criterion of adherence, participants who attended at least 80% of their scheduled exercise sessions were assigned as adherent and participants who attended less than 80% of their exercise sessions as non-adherent. Because the TIGER protocol is administered within the structure of a college course for credit, this attendance criterion was based on the minimum class participation needed in order to pass the course.
Statistical Analysis
All statistical analyses were performed using STATA version 11.1 (Statacorp Inc., College Station, Texas). Histograms, normal probability plots, central tendency and variability measures, and zero-order product-moment correlation coefficients were used to examine the distributions and bivariate associations, respectively, of exercise frequency (i.e., attendance), ExHR, %HRR, ExMin, and HRPAS. Using HRPAS as the dependent variable, exercise frequency, %HRR, and ExMin were included in multiple linear regression analysis adjusted for age, gender, race/ethnicity, and BMI to determine the variance in HRPAS accounted for by the exercise components independent of the covariates. Multiple regression was also used to examine the association between HRPAS and changes in physiological outcomes, including BMI, %Fat, waist and hip circumferences, resting systolic and diastolic BP, resting heart rate, estimated aerobic capacity, fasting glucose, and fasting total cholesterol. Each dependent variable was analyzed using a separate model adjusted for age, gender, race/ethnicity, and baseline value of the measure. The tests of the respective regression coefficients were evaluated to determine whether HRPAS was associated with changes in the outcome variables independent of baseline values and the other covariates. Logistic regression was used to examine predictors of exercise compliance and adherence. For all tests, statistical significance was set at p<0.05.
Results
Heart Rate Monitor Data
Participants were excluded from analysis if no exercise sessions were completed (n = 132) or if more than 40% of heart rate observations were missing (n = 147). The final sample consisted of 1,150 participants (447 men, 703 women) whose ages ranged from 18 to 35 years (Table 1). The racial/ethnic groups most frequently represented by the majority of participants in this study were non-Hispanic white (28.5%), African American (27.3%), Hispanic (23.7%), and Asian (7.4%). Participants completed an average of 29.1 (SD = 6.9) exercise sessions at an average duration of 38.4 (SD = 3.7) min. Average heart rate was 156 (SD = 8) b·min−1, and mean %HRR was 67.9% (SD = 5.8%).
Table 1.
Participants’ baseline characteristics.
| Women (n = 703) |
Men (n = 447) |
|
|---|---|---|
| Age (y) | 21.0 ± 2.8 | 21.5 ± 2.8 |
| Height (cm) | 161.6 ± 6.8 | 175.0 ± 7.0 |
| Weight (kg) | 67.2 ± 17.8 | 83.1 ± 20.5 |
| Body mass index (kg/m2) | 25.7 ± 6.2 | 27.1 ± 5.8 |
| DXA body fat (%) | 31.8 ± 7.3 | 20.2 ± 7.8 |
| Resting heart rate (bpm) | 76.5 ± 11.3 | 70.5 ± 12.1 |
| Systolic blood pressure (mmHg) | 108.9 ± 10.8 | 122.9 ± 11.6 |
| Diastolic blood pressure (mmHg) | 66.6 ± 9.1 | 66.9 ± 10.1 |
| Fasting glucose (mg/dL) | 79.5 ± 12.9 | 84.2 ± 20.2 |
| Fasting cholesterol (mg/dL) | 164.5 ± 30.6 | 150.8 ± 30.7 |
The mean calculated normalized HRPAS was 739 (SD = 202) intensity-minutes. The HRPAS was positively related to all three components of exercise, most strongly to frequency (r = 0.87, p < 0.001) but also significantly to duration (r = 0.34, p < 0.001) and intensity (r = 0.38, p < 0.001). The three components together explained 98% of the variability in the HRPAS (i.e., R2 = 0.98, p < 0.001). After accounting for these components, the HRPAS was unassociated with age (p = 0.570), gender (p = 0.220), race/ethnicity (p = 0.395), or BMI (p = 0.156).
Based on HRPAS, a total of 868 participants (75.5%) were identified as compliant, and 282 (24.5%) were identified as non-compliant, while 885 participants (77.0%) were defined as adherent and 265 (23.0%) were defined as non-adherent, based on attendance. Concordance between adherence defined by attendance and compliance defined by HRPAS is depicted in Table 2. The HRPAS classified 9.1% (n=105) of the participants differently for the adherence criterion than for the compliance criterion. Forty-four participants (3.8%) who were identified as compliant by the HRPAS criterion were classified as non-adherent by attendance alone. These participants exceeded the prescribed HRPAS despite attending fewer sessions by exercising for a longer duration per session (40.5 ± 2.8 min) and/or at a higher relative intensity (70.1% ± 4.2%) than prescribed. By contrast, 61 participants (5.3%) identified as non-compliant by the HRPAS criterion were classified as adherent by attendance records alone. These participants failed to meet their prescribed HRPAS despite attending most of the sessions, primarily because of non-compliance with the exercise intensity prescription (i.e., average relative intensity was lower (60.0 ± 5.5%) than the prescribed intensity). After controlling for age, gender, race, and BMI, both mean duration and average intensity (%HRR) were significantly predictive of both non-compliance (p<0.001) and non-adherence (p<0.01).
Table 2.
Concordance between adherence defined by attendance and compliance defined by HRPAS.
| HRPAS | ||||
|---|---|---|---|---|
| Compliant | Non-compliant | Total | ||
| Attendance | Adherent | 824 | 61 | 885 |
| Non-adherent | 44 | 221 | 265 | |
| Total | 868 | 282 | 1150 | |
HRPAS and Health-Related Risk Factors
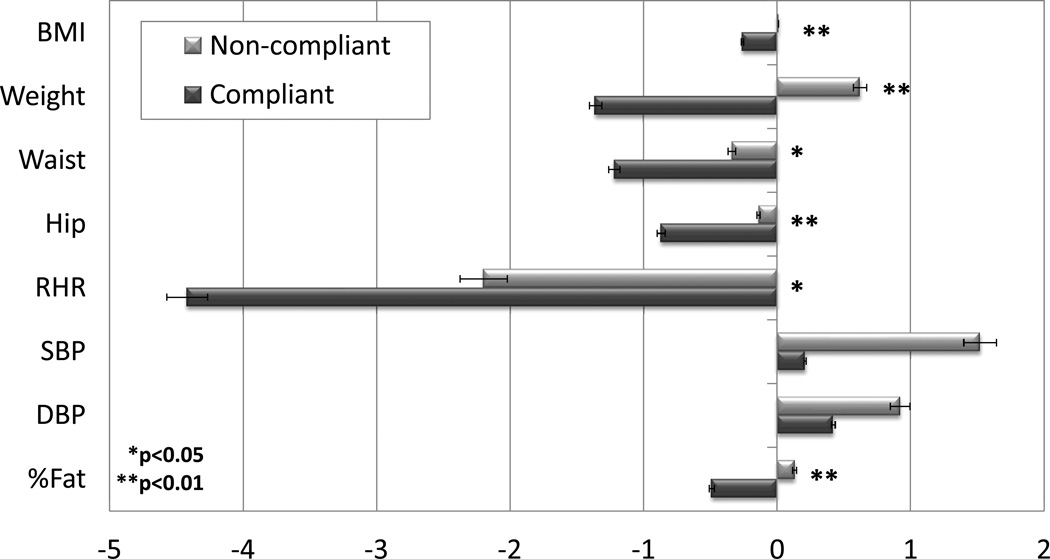
After adjusting for age, gender, race, and baseline values of each measure, HRPAS exercise dose was significantly associated with positive change in BMI, body mass, waist and hip circumferences, resting heart rate (RHR), %Fat, systolic blood pressure, and fasting glucose and cholesterol (Table 3). Standardized regression coefficients, which represent the amount of change in each physiologic variable associated with change in each of the measures of compliance/adherence in standard deviation units, allow for comparison across analyses (see Table, Supplemental Digital Content: Regression analyses for absolute change in health-related outcomes for HRPAS, HRPAS-based compliance, and attendance-based adherence). Only change in diastolic blood pressure was not associated with HRPAS, possibly due to the narrow range of this variable in this young, healthy cohort. Conversely, compliance (defined by HRPAS) and adherence (defined by attendance) cut-points were only associated with changes in body mass, hip circumference, %Fat, and RHR. HRPAS-based compliance was also associated with BMI and waist circumference, while attendance-based adherence was associated with cholesterol change (Table 3). Unadjusted absolute differences in health-related outcomes by compliance status are summarized in Figure 1. Compliance with the prescribed protocol across 15 weeks was associated with an average decrease of 1.4 kg in body mass, a mean 4.5 beats/min 1 decrease in resting HR, and approximately 1 cm decrease in waist and hip circumferences independent of age, gender and race. Mean changes in physiological parameters by combined compliance/adherence cut-points are summarized in Table 4. Standardized mean differences and confidence intervals, along with effect sizes (Hedges’ d), by compliance/adherence cut-points are provided in Supplemental Tables 1 and 2. Combined non-compliance and non-adherence was associated with the poorest 15-week outcomes (Table 4). Individuals who were compliant with the exercise protocol but non-adherent based on attendance did not differ significantly for any physiologic parameter measured from those who were classified as both adherent and compliant by their attendance and HRPAS.
Table 3.
Regression analyses for absolute change in health-related outcomes for HRPAS, HRPAS-based compliance, and attendance-based adherence*
| HRPAS | HRPAS-based Compliance |
Attendance-based Adherence |
||||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) |
p | Coefficient (95% CI) |
p | Coefficient (95% CI) |
p | |
| Body mass (kg) | −0.006 (−0.008 ± −0.004) |
0.001 | 2.14 (1.16 ± 3.12) |
0.001 | 1.37 (0.32 ± 2.42) |
0.011 |
| BMI (kg/m2) | −.001 (−0.001 ± −0.000) |
0.001 | 0.29 (0.10 ± 0.49) |
0.004 | 0.17 (−0.04 ± 0.38) |
0.110 |
| Waist (cm) | −0.003 (−.005 ± −0.001) |
0.001 | 0.97 (0.30 ± 1.64) |
0.004 | 0.66 (−0.05 ± 1.36) |
0.070 |
| Hip (cm) | −0.003 (−0.005 ± −0.001) |
0.001 | 0.81 (0.10 ± 1.51) |
0.025 | 0.89 (0.15 ± 1.64) |
0.019 |
| DXA Fat (%) | −0.002 (−0.003 ± −0.001) |
0.001 | 0.59 (0.18 ± 1.01) |
0.005 | 0.45 (0.06 ± 0.84) |
0.023 |
| Resting heart rate (bpm) | −0.006 (−.010 ± −0.002) |
0.003 | 1.88 (0.33 ± 3.43) |
0.018 | 2.07 (0.42 ± 3.71) |
0.014 |
| Systolic blood pressure (mmHg) | −0.005 (−0.008 ± −0.001) |
0.011 | 0.74 (−0.75 ± 2.22) |
0.331 | −0.19 (−1.76 ± 1.38) |
0.816 |
| Diastolic blood pressure (mmHg) | −0.0002 (−0.003 ± 0.003) |
0.885 | 0.21 (−1.03 ± 1.44) |
0.742 | 0.31 (−1.00 ± 1.62) |
0.664 |
| Fasting glucose (mg/dL) | −0.010 (−0.015 ± −0.005) |
0.001 | 0.94 (−1.12 ± 3.00) |
0.370 | 0.98 (−0.93 ± 2.87) |
0.405 |
| Fasting cholesterol (mg/dL) | −0.014 (−0.026 ± −0.003) |
0.012 | 3.91 (−0.73 ± 8.55) |
0.098 | 7.55 (2.63 ± 12.48) |
0.003 |
All models adjusted for age, gender, race, and baseline values of each measure.
Figure 1.
Unadjusted absolute change by exercise compliance based on HRPAS (Heart Rate Physical Activity Score). Average absolute change in individuals who were compliant or non-compliant with the prescribed exercise protocol based on HRPAS. Error bars are based on standard error. BMI=body mass index (kg/m2); RHR=resting heart rate (bpm); SBP=systolic blood pressure (mm Hg); DBP=diastolic blood pressure (mm Hg); %Fat=percent fat determined by dual x-ray absorptiometry (DXA); Glucose (mg/dL); Cholesterol (mg/dL). P-values based on regression adjusted for age, gender, race, and baseline value.
Table 4.
Baseline to final changes in health-related risk factors based on compliance (heart rate physical activity score; HRPAS) and adherence (attendance) status.
| Compliant/ Adherent |
Non-compliant/ Non-adherent |
Compliant/ Non- Adherent, |
Non- compliant/ Adherent |
|
|---|---|---|---|---|
| (N = 824) | (N = 221) | (N = 44) | (N = 61) | |
| Body weight (kg) | −1.35 ± 6.2 | 0.4 ± 6.0* | −1.5 ± 6.5 | 1.0 ± 4.1* |
| BMI (kg/m2) | −0.3 ± 1.3 | −0.03 ± 1.0 | −0.3 ± 1.0 | 0.1 ± 0.7* |
| Waist (cm) | −1.2 ± 4.4 | −0.4 ± 3.4 | −1.3 ± 3.7 | −0.2 ± 2.3 |
| Hip (cm) | −0.9 ± 4.7 | 0.1 ± 3.1* | −0.4 ± 3.6 | −0.6 ± 3.3 |
| DXA Fat (%) | −0.5 ± 1.7 | 0.2 ± 2.0* | −0.6 ± 1.8 | −0.2 ± 1.7 |
| Resting heart rate (bpm) | −4.5 ± 10.8 | −1.4 ± 11.1* | −3.3 ± 12.3 | −3.7 ± 9.7 |
| Systolic blood pressure (mmHg) | 0.2 ± 10.1 | 1.2 ± 12.0 | −0.9 ± 10.2 | 1.9 ± 9.8 |
| Diastolic blood pressure (mmHg) | 0.4 ± 8.2 | 1.6 ± 9.0 | −0.4 ± .6 | −0.3 ± 7.6 |
| Fasting glucose (mg/dL) | 2.9 ± 10.8 | 3.0 ± 11.3 | 7.2 ± 12.5 | 4.9 ± 10.4 |
| Fasting cholesterol (mg/dL) | 1.9 ± 29.6 | 7.7 ± 30.4 | 16.8 ± 26.8* | 5.9 ± 27.3 |
| Heart rate physical activity score (HRPAS) | 832.0 ± 114.7 | 436.1 ± 173.5* | 731.0 ± 81.5* | 586.3 ± 61.8* |
| Mean duration (min) | 38.8 ± 3.7 | 37.5 ± 3.7* | 40.5 ± 2.8* | 35.4 ± 3.2* |
| Mean intensity (%HRR) | 68.7 ± 5.3 | 66.6 ± 5.9* | 70.1 ± 4.2 | 60.0 ± 5.5* |
P < 0.05 compared to the Compliant/Adherent group.
Compliant = Achieved or exceeded prescribed HRPAS.
Non-compliant = Did not achieve prescribed HRPAS.
Adherent = Attended ≥81% of prescribed exercise sessions.
Non-adherent = Attended 81% of prescribed exercise sessions.
Discussion
In this study, exercise dose was quantified using objective heart rate monitoring as a measure of exercise intensity, duration and frequency. Effects of HRPAS on biomarkers of health risk were compared with effects when adherence was defined based on either compliance or attendance cut-points. Larger values of HRPAS were significantly associated with improvements in multiple physiologic parameters, regardless of whether participants met a definition of adherence based only on attendance. The positive association between HRPAS and these health-related measures is consistent with the expected effect of greater amounts of physical activity improving health and fitness (10).
Based on an empirical measure of exercise dose, compliance to an exercise prescription can be achieved by modifying any of the components of the prescription, including frequency, duration, and intensity. In addition to the direction (i.e., adoption of an exercise program) and persistence (e.g., attendance or completion of a program) of behavior, motivation theory incorporates the intensity of behavior as an important component of physical activity. Individuals in this study who were compliant but non-adherent based on attendance did so by increasing the intensity and/or duration of each session performed. Though average duration of each session was similar in compliant and non-compliant participants (38.8 ± 3.6 min versus 37.0 ± 3.7 min, respectively), exercise intensity was substantially higher in compliant participants compared to those who were non-compliant (68.8 ± 5.2% versus 65.2 ± 6.4%, p<0.001). Intensity has often been neglected in clinical trials of the determinants and outcomes of exercise training, which are generally limited to activity type in most population surveys (6). Importantly, compliant individuals who were non-adherent based on attendance did not differ significantly on any physiologic response parameter measured from those who were classified as both adherent and compliant, suggesting that total exercise dose may be more informative and predictive of change in health-related outcome than cut-point measures.
Exercise dose is a complex stimulus involving not only attendance but actual duration and intensity of exercise in each exercise session accumulated across all sessions of an intervention. By using session attendance as a proxy for exercise exposure, the true effect of exercise may be over- or underestimated because of unknown exposure to the active feature of the exercise stimulus. Here we quantified exercise exposure by adjusting the duration of each session by the intensity of the exercise performed. Thus, qualitatively-different 30-min exercise bouts performed at 50% and 70% intensity can be quantified using this approach (i.e., W-HRPAS for these sessions would be 15 and 21, respectively, while attendance measures would give equal credit to the exercise bouts).
There has been continued interest in the relative merits of 1) accumulation of total volume, 2) plausible differences between short exercise bouts versus long and 3) continuous exercise bouts. Recently, Glazer et al. reported that total minutes of moderate to vigorous physical activity was significantly related to blood lipids, BMI, waist circumference, and Framingham risk score (p<0.0001), regardless of whether the physical activity was accumulated in bouts shorter or longer than 10 minutes (9). A wide range of durations may provide equivalent benefits when similar total daily and weekly volumes are accumulated (18). The results reported here confirm that objective assessment of exercise dose using heart rate monitoring provides unique associations with health-related outcomes beyond those observed when adherence is defined only by session attendance. As long as the product of intensity and duration is at least the prescribed value (for each session and total across sessions), the health benefits appear to be similar. In other words, an individual can choose to exercise at a lower intensity for a longer duration or for a shorter duration but higher intensity and get similar health benefits. One could even “skip” sessions (frequency) and “make it up” by going longer and/or harder the next time – from a public health perspective, this is an important message.
Heart rate monitoring allows for calculation of HRPAS as both a measure of total exercise dose and a measure of exercise compliance over the course of an intervention. In addition, most heart rate monitors provide audible feedback to the participants when they are in their target training zone, serving as an excellent tool for teaching participants how to exercise in a heart rate range most likely to elicit change. Compliant participants in this study spent significantly more time each session in their target heart rate zone (i.e., 65–85% maximum HRR) compared to non-compliant participants (28.5 ± 4.1 min versus 25.1± 6.6 min, respectively, p<0.001), despite exercising for similar total duration. The ability to efficiently reach one’s target heart rate zone may play an important role in compliance to the exercise prescription. Given expert opinions that “just showing up” to exercise is not enough (18, 26), it is particularly noteworthy that HRPAS provided a conceptually more comprehensive measure of exercise response than using only attendance records, the most common method of evaluating exercise adherence.
Though a defined exercise prescription naturally creates a cut-point for compliance, our results demonstrate that increasing levels of total exercise dose are associated with greater health and fitness benefits, as outlined by contemporary guidelines (10, 17, 18), beyond simply achieving the minimum prescribed exercise dose. These results also suggest that healthy young adults are willing and able to exercise at higher levels than those currently recommended and that higher intensity and/or longer duration of each exercise session are both associated with better exercise adherence.
This study had several methodological and conceptual strengths that represent improvements over previous exercise adherence research. These include: 1) the recruitment of a large, ethnically diverse cohort of young adults; 2) the use of a standardized, supervised exercise program designed in accordance with guidelines for vigorous physical activity (17); 3) the use of objective measures of frequency, intensity, and duration of physical activity; 4) the use of individualized target heart prescriptions; and 5) the ability to download data from the heart rate monitors to a computer database. Future studies that include a full assessment of HRPAS over a broader range of exercise intensities and durations will provide more complete information regarding the role of the components of exercise dose in adherence and compliance.
Conclusions
Heart rate monitoring is an objective, practical measure of physical activity and presents low interference with normal activities. Importantly, heart rate monitors can be used to teach individuals how to exercise at a level most likely to elicit physiologic change. The HRPAS is a quantifiable measure of exercise dose that was associated with improvement in health indicators beyond that observed when adherence is defined as session attendance.
Supplementary Material
Acknowledgments
Support for this work was provided by the National Institute of Diabetes and Digestive and Kidney Diseases/National Institutes of Health grant DK062148. Results of the present study do not constitute endorsement by ACSM.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement
The authors have the following conflicts to disclose: FLM (none); DPO (Nimbic, Inc., Centers for Disease Control and Prevention, NASA, JW King Orthopedic Institute, SLACK, Inc., Association of Bone and Joint Surgeons); MPH (None); MHS (None); ASJ (None); RKD (None); MSB (None).
Supplemental Digital Content
Table S1. Regression analyses for absolute change in health-related outcomes for HRPAS, HRPAS-based compliance, and attendance-based adherence
References
- 1.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Jr., Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS. Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 2.Astrand P, Ryhming I. A nomogram for calculation of aerobic capacity (physical fitness) from pulse rate during sub-maximal work. J Appl Physiol. 1954;7(2):218–221. doi: 10.1152/jappl.1954.7.2.218. [DOI] [PubMed] [Google Scholar]
- 3.Bouchard C, Blair SN, Church TS, Earnest CP, Hagberg JM, Hakkinen K, Jenkins NT, Karavirta L, Kraus WE, Leon AS, Rao DC, Sarzynski MA, Skinner JS, Slentz CA, Rankinen T. Adverse metabolic response to regular exercise: is it a rare or common occurrence? PLoS One. 2012;7(5):e37887. doi: 10.1371/journal.pone.0037887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bray MS, Hagberg JM, Perusse L, Rankinen T, Roth SM, Wolfarth B, Bouchard C. The human gene map for performance and health-related fitness phenotypes: the 2006–2007 update. Med Sci Sports Exerc. 2009;41(1):35–73. doi: 10.1249/mss.0b013e3181844179. [DOI] [PubMed] [Google Scholar]
- 5.Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA. 2007;297(19):2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- 6.Dishman R. In: Psychological factors and physical activity level. In: Physical Activity and Obesity. Bouchard C, Katzmarzyk P, editors. Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- 7.Dishman RK. In: Psychological factors and physical activity level. In: Physical Activity and Obesity. Bouchard C, Katzmarzyk P, editors. Champaign, IL: Human Kinetics; 2010. pp. 89–93. [Google Scholar]
- 8.Duncan GE, Anton SD, Sydeman SJ, Newton RL, Jr., Corsica JA, Durning PE, Ketterson TU, Martin AD, Limacher MC, Perri MG. Prescribing exercise at varied levels of intensity and frequency: a randomized trial. Arch Intern Med. 2005;165(20):2362–2369. doi: 10.1001/archinte.165.20.2362. [DOI] [PubMed] [Google Scholar]
- 9.Glazer NL, Lyass A, Esliger DW, Blease SJ, Freedson PS, Massaro JM, Murabito JM, Vasan RS. Sustained and Shorter Bouts of Physical Activity Are Related to Cardiovascular Health. Med Sci Sports Exerc. 2013;45(1):109–115. doi: 10.1249/MSS.0b013e31826beae5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 11.Jackson AS, Blair SN, Mahar MT, Wier LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22(6):863–870. doi: 10.1249/00005768-199012000-00021. [DOI] [PubMed] [Google Scholar]
- 12.King AC, Haskell WL, Taylor CB, Kraemer HC, DeBusk RF. Group-vs home-based exercise training in healthy older men and women. A community-based clinical trial. JAMA. 1991;266(11):1535–1542. [PubMed] [Google Scholar]
- 13.Laukkanen RM, Virtanen PK. Heart rate monitors: state of the art. J Sports Sci. 1998;16(Suppl):S3–S7. doi: 10.1080/026404198366920. [DOI] [PubMed] [Google Scholar]
- 14.Lee IM, Paffenbarger RS., Jr. Associations of light, moderate, and vigorous intensity physical activity with longevity. The Harvard Alumni Health Study. Am J Epidemiol. 2000;151(3):293–299. doi: 10.1093/oxfordjournals.aje.a010205. [DOI] [PubMed] [Google Scholar]
- 15.Martin JE, Dubbert PM. Adherence to exercise. Exerc Sport Sci Rev. 1985;13:137–167. [PubMed] [Google Scholar]
- 16.Oldridge NB. Compliance and exercise in primary and secondary prevention of coronary heart disease: a review. Prev Med. 1982;11(1):56–70. doi: 10.1016/0091-7435(82)90005-6. [DOI] [PubMed] [Google Scholar]
- 17.Physical AGAC. Physical Activity Guidelines for Americans. Washington, DC: Department of Health and Human Services; 2008. [Google Scholar]
- 18.Powell KE, Paluch AE, Blair SN. Physical activity for health: What kind? How much? How intense? On top of what? Annu Rev Public Health. 2011;32:349–365. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 19.Sallis J, Owen N. Physical activity and behavioral medicine. Thousand Oaks, Calif: Sage Publications; 1999. pp. 110–134. [Google Scholar]
- 20.Schnohr P, Scharling H, Jensen JS. Intensity versus duration of walking, impact on mortality: the Copenhagen City Heart Study. Eur J Cardiovasc Prev Rehabil. 2007;14(1):72–78. doi: 10.1097/HJR.0b013e3280144470. [DOI] [PubMed] [Google Scholar]
- 21.Sigal RJ, Kenny GP, Boule NG, Wells GA, Prud'homme D, Fortier M, Reid RD, Tulloch H, Coyle D, Phillips P, Jennings A, Jaffey J. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. 2007;147(6):357–369. doi: 10.7326/0003-4819-147-6-200709180-00005. [DOI] [PubMed] [Google Scholar]
- 22.Thompson D, Batterham AM, Markovitch D, Dixon NC, Lund AJ, Walhin JP. Confusion and conflict in assessing the physical activity status of middle-aged men. PLoS One. 2009;4(2):e4337. doi: 10.1371/journal.pone.0004337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trinder P. Oxidase determination of plasma cholesterol as cholest-4-en-3-one using iso-octane extraction. Ann Clin Biochem. 1981;18(Pt 2):64–70. doi: 10.1177/000456328101800202. [DOI] [PubMed] [Google Scholar]
- 24.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 25.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40(4):454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Wilmore JH. Aerobic exercise and endurance: improving fitness for health benefits. Phys Sportsmed. 2003;31(5):45–51. doi: 10.3810/psm.2003.05.367. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.