Abstract
Background and Purpose
The recording of fall events is usually subjective and imprecise, which limits clinical practice and falls-related research. We sought to develop and validate a scale to grade near-fall and fall events based on their severity represented by the use of healthcare resources, with the goal of standardizing fall reporting in the clinical and research settings.
Methods
Qualitative instrument development was based on a literature review and semi-structured interviews to assess face and content validity. We queried older individuals and healthcare professionals with expertise in the care of patients at risk of falling about clinically important differences to detect and how to optimize the scale's ease of use. To assess the scale's inter-rater reliability, we created 30 video-vignettes of falls and compared how healthcare professionals and volunteers rated each of the falls according to our grading scale.
Results
We developed the illustrated 4-point Hopkins Falls Grading Scale (HFGS). The grades distinguish a near-fall (Grade 1) from a fall for which an individual did not receive medical attention (Grade 2), a fall associated with medical attention but not hospital admission (Grade 3), and a fall associated with hospital admission (Grade 4). Overall, the HFGS exhibited good face and content validity, and had an intraclass correlation coefficient of 0.998.
Conclusion
The 4-point HFGS demonstrates good face and content validity and high inter-rater reliability. We predict this tool will facilitate the standardization of falls reporting in both the clinical and research settings.
Keywords: Falls definition, falls classification, falls reporting
Introduction
Falls are a common and dangerous event among older individuals.1-4 One of the strongest established risk factors for a fall is a history of a prior fall.5;6 As such, accurate identification of a fall event is critical to the risk-stratification of patients in the clinical setting.7;8 Moreover, the rigorous reporting of fall events is central to the development and assessment of strategies to reduce the risk of falls in the research setting.9;10
The reporting of fall events has numerous shortcomings. First, definitions of a fall used in both the clinical and research settings are ambiguous.9-13 Efforts have been made to consolidate the disparate definitions:14;15 for example, the Prevention of Falls Network Europe (PROFANE) has promulgated the definition of a fall as “an unexpected event in which the participants come to rest on the ground, floor, or lower level.”16 However, not all research trials have adopted this definition. 11 Furthermore, specific definitions of a fall are typically not offered in the screening and reporting tools used in the clinical inpatient and outpatient settings.5;10;12 An additional limitation in the current reporting of falls is that a near-fall, which may be important in presaging a future fall, is not uniformly contained in existing fall definitions. 17-20 Finally, the clinical and functional significance of each fall event is not captured by most current definitions.9;13;21;22 These limitations in the reporting of a fall event make the ascertainment and reduction of fall risk difficult in the clinical and research settings.
In this report we develop and validate a falls grading scale supported by illustrations intended to standardize the reporting of near-fall and fall events based on their impact to the patient. We performed initial validation studies in a group of older individuals and healthcare professionals, and assessed the reliability of the scale in the same healthcare professionals and volunteers throughout the age range. The use of a validated falls scale may help standardize the reporting of falls, with potential benefits for clinical decision-making and for research.
Methods
Development of the Hopkins Falls Grading Scale
The Hopkins Falls Grading Scale (HFGS) was developed to enhance the accuracy of falls reporting in the clinical and research settings. The initial development of a qualitative instrument was based on a literature review, using the keywords “falls grading scale”, “fall definition”, “falling definition”, “falls recording”, “history of falls”, “falls severity” and “falls self-report” in PubMed. Twenty-nine manuscripts were reviewed, although none described an instrument for standardized falls reporting. Various definitions of near-falls and falls were considered, and measures of fall severity were reviewed, including distinctions based on the extent of injury or on the use of healthcare resources. We developed a candidate grading scale as well as several variations whereby we altered the number of grades (4 vs. 5 grades) and the basis for distinguishing among grades (based on minor vs. major injury or healthcare resource utilization). The accompanying illustrations were created by a member of the Arts as Applied to Medicine Department at the Johns Hopkins University.
Face and Content Validity
The HFGS was assessed for its face and content validity. Face validity evaluates the extent to which a scale makes intrinsic sense to potential users of the scale. Content validity assesses the value of the scale based on a priori theoretical and empirical considerations.23 We measured face and content validity by conducting semi-structured interviews with 4 older individuals and 12 healthcare professionals. The older individuals were aged 70 years and older and were recruited from a geriatrics ambulatory care center. Two of them were fallers (reported a fall in the previous year) and 2 were non-fallers. The group of healthcare professionals was larger given that a diversity of experts in treating older patients at risk of falls were surveyed (including 1geriatrician, 2 otolaryngologists, 1 neurologist, 1 ophthalmologist, 1 orthopedic surgeon, 3 physical therapists, 1 occupational therapist, 1 nurse, and 1 geriatrics clinical researcher). Each of these healthcare professionals routinely saw older patients at risk of falls or following a fall in their clinical practices, and had recently convened to form a Multidisciplinary Falls Clinic and Board.
The semi-structured interviews consisted of 7 open-ended questions that fostered additional discussion. The first 3 questions assessed face validity, and addressed the scale's ease of use, the need for additional explanations on a back page, and the quality of the accompanying illustrations. The next 3 questions assessed content validity based on a priori theoretical considerations, and related to whether the distinctions among grades were clinically significant and could be accurately determined, whether any of the severity grades were equivalent and should be combined, , and the need for additional considerations. The 7th question allowed for any additional comments or suggestions (Table 1). Modifications to the HFGS were implemented iteratively as the older individuals and healthcare professionals were interviewed.
Table 1. Questions Asked During the Semi-structured Interviews.
| Validity | Question |
|---|---|
| Face validity | 1. Do you think the scale would be easy to use by patients and providers? |
| 2. Are the definitions in the back of the scale useful for its application? Would you add anything to them? | |
| 3. Are the images representative of each of the grades? | |
| Content validity | 4. Do you think the different grades correspond to clinically significant differences? |
| 5. Would you combine any of the grades? | |
| 6. Would you include other factors/considerations in the grading scale? | |
| Both | 7. Do you have other comments regarding the scale's structure or its application? |
Reliability
Once the final HFGS was developed through iterative refinement based on the semi-structured interviews, the inter-rater reliability of the HFGS was assessed. We developed 30 brief video-vignettes with actors depicting examples of each of the HFGS' grades. We then evaluated the scale's inter-rater reliability among the 12 healthcare professionals listed above and 4 others who joined the Falls Board (including another geriatrician, ophthalmologist, and 2 physical therapists), and volunteers (who varied in age and profession and included office assistants and family members of patients). We recruited sufficient volunteers to obtain a wide age range between 23-95 years, representative of a cross-section of the population and of potential users of the scale (given that the scale was not specifically designed for a certain age or demographic group). We taught the HFGS to the healthcare professionals and volunteers and then asked them to grade the fall events shown in the videos (the videos are available in the Supplemental Materials). The study was approved by the institutional review board at the Johns Hopkins Hospital. The overall process by which we developed and validated our instrument is outlined in Table 2.24
Table 2. Process of Falls Grading Scale Development and Validation.
| Step | Purpose | Number | Product |
|---|---|---|---|
| Phase 1: Qualitative Development | |||
| Literature review | Data generation | 29 articles; 3 standarized falls definitionsa | |
| Candidate falls severity grades | Data synthesis | Hopkins Falls Grading Scale study investigators | Draft Hopkins Falls Grading Scale and several variations (4-5 grades) |
| Illustration development | Illustrative aid to the grading system | Member of Arts as Applied to Medicine Department at the Johns Hopkins University | Draft illustrated Hopkins Falls Grading Scale and several variations (4-5 grades) |
| Phase 2: Scale Validation | |||
| Semi-structured interviews | Face and content validity | Older individuals (n=4) and providers (n = 12) with diverse expertise in treating older patients at risk of falls | Hopkins Falls Grading Scale (4 grades) with strong face and content validity |
| Phase 3: Reliability Assessment | |||
| Scoring of 30 sample falls shown in video-vignettes based on the Hopkins Falls Grading Scale | Inter-rater reliability | 46 participants: 16 healthcare professionals and 30 volunteers | Intraclass correlation coefficient (ICC) of 0.998 (ICC of 0.995 for healthcare professionals and 0.996 for volunteers.) |
Statistical Analysis
Inter-rater reliability was assessed using the intraclass correlation coefficient (ICC), calculated using a 2-way random effects model of the consistency type. The ICC for single measures was computed along with 95% confidence intervals. SPSS Statistics release version 19.0 (Chicago, IL) was used for all analyses.
Results
Development and validation of the Hopkins Falls Grading Scale
During the semi-structured interviews, most of the volunteers and healthcare professionals believed that classifying injury severity as minor or major would be ambiguous, and an exhaustive list of conditions (e.g. abrasion, laceration, fracture, etc) could not be practicably provided with each grade on the HFGS. The interview responses showed that the requirement for varying degrees of medical assistance would best capture the severity of a fall event. The participants also agreed on four clinically separable grades, and felt that the details of the grades should be contained in the HFGS without additional explanations. Both groups judged that the illustrations represented each grade adequately.
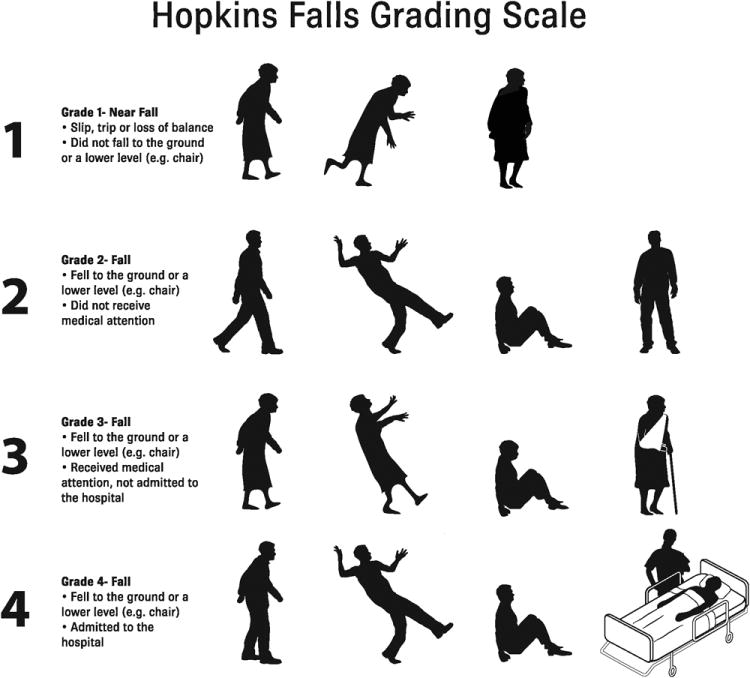
Based on the responses to the interviews, we developed the 4-point HFGS (Figure 1). Grade 1 is defined as a near-fall, when an individual slips, trips or loses their balance without falling to the ground or to a lower level. A Grade 2 fall is defined as a fall to the ground or to a lower level without obtaining medical assistance. A Grade 3 fall is defined as a fall to the ground or to a lower level when medical assistance was obtained but the individual was not admitted to the hospital. A Grade 4 fall was defined as a fall to the ground or to a lower level with hospitalization. The final product of this iterative process demonstrated good face and content validity.
Figure 1. Hopkins Falls Grading Scale. © Johns Hopkins University.
Reliability
In the reliability analysis using the 30 video-vignettes depicting near-fall and fall events, we observed a high inter-rater reliability for application of the HFGS, with an ICC of 0.998 for the complete sample with a 95% confidence interval (CI) of 0.997, 0.999 (p<0.001). When calculating the ICC among healthcare professionals and volunteers separately, both subgroups had a high ICC of 0.995 (CI 0.992, 0.997) and 0.996 (CI 0.994, 0.998), respectively (p<0.001).
Discussion
We developed the illustrated 4-point Hopkins Falls Grading Scale to standardize reporting of the nature and severity of a fall event. The need for standardization is well-recognized, given that the case definition of a fall influences clinical decision-making and the results of research studies.17 Use of the HFGS to characterize each index fall event should be supplemented by measuring the frequency of falls, the rate of falls per person-year and the time to a fall event; a prospective daily calendar with monthly reporting is considered the gold standard for collecting this data. 9;16;25;26 Additional outcomes to consider include fear of falling, physical activity level, and health-related quality of life.16
The HFGS, which distinguishes between near-falls and falls and classifies fall severity based on the use of healthcare resources, exhibited good face and content validity and high inter-rater reliability, even given the small sample sizes used in the validity and reliability analyses. One group previously suggested classifying falls based on etiology into extrinsic falls (caused by factors external to the individual) and intrinsic falls (due to biologic characteristics of the individual),27 although a limitation of this grading system is that falls are frequently multifactorial and cannot be accurately or reproducibly attributed to one factor. 6;27 The focus of the HFGS on healthcare utilization after a fall is supported by other studies that have found that both healthcare professionals and patients usually focus on the consequences of the fall.12 It should be noted that the HFGS relies on self-report, which is subject to the individual's physical and cognitive state and has been associated with under- as well as over-reporting of falls in several studies.21;22;28;29
A few authors have suggested that grading falls based on utilization of resources reflects geographic differences in patterns of practice rather than severity of falls.9 Other authors suggest that the presence or absence of a radiologically-confirmed peripheral fracture may be a good way to capture the severity of injuries from falls.16 Our semi-structured interviews with volunteers and healthcare professionals suggested that patients are much less likely to report a medical diagnosis (e.g., a radiologically-confirmed fracture) accurately than a visit to the emergency room or a stay in the hospital. The classification of injuries is difficult, and some studies suggest that the self-report of injuries is less accurate than the self-report of fall events.16;28 As an initial application, the HFGS may be used longitudinally to assess fall events within single individuals (ensuring high internal consistency) or cross-sectionally to compare fall rates and severity across populations with relatively homogeneous healthcare systems (e.g., individual US states). Further studies of the criterion validity of the HFGS, in which the individual grades are correlated with factors that contribute to fall risk (such as vision and balance control) as well as for their ability to predict morbidity and mortality, will be required to corroborate the validity of this scale.23
Conclusion
The Hopkins Falls Grading Scale is a simple, valid and reliable method designed to standardize fall reporting among patients, clinicians and researchers. A more uniform and objective grading system will allow for improved risk stratification of patients and better decision-making in the clinical setting. Additionally, a standardized scale could facilitate a more rigorous assessment of strategies to reduce the risk of falls and the development of evidence-based clinical guidelines in the research setting.
Supplementary Material
Acknowledgments
The authors thank the members of the Falls Board at the Johns Hopkins Hospital for their contribution to the development of the falls grading scale. They also thank Carolina Trevino and Richard T. Penninger for helping with the creation of the falls video-vignettes.
Footnotes
Conflict of Interest and Source of Funding: None declared.
Scientific Meeting Presentations: 4th Pan-American Congress, International Association of Gerontology and Geriatrics. Falls Session. October 22, 2011. Ottawa, Canada.
Contributor Information
Marcela Davalos-Bichara, Email: mdavalo1@jhmi.edu, Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, USA.; Escuela de Medicina Ignacio A. Santos del Tecnológico de Monterrey, Monterrey, México, 601 N. Caroline St., 6th Floor, Room 6030D, Baltimore, MD 21287-0910, 410-955-7876.
Frank R. Lin, Email: flin@jhmi.edu, Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, USA., 601 N. Caroline St., 6th Floor Room, 6163 Baltimore, MD 21287-0910, 443-287-6509.
John P. Carey, Email: jcarey@jhmi.edu, Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, USA., 601 N. Caroline St., 6th Floor, Room 6255, Baltimore, MD 21287-0910, Phone: 410-955-7381, Fax: 410-955-0035.
Jeremy D. Walston, Email: jwalston@jhmi.edu, Division of Geriatric Medicine and Gerontology, The Johns Hopkins University School of Medicine, Baltimore, USA., 5501 Hopkins Bayview Circle, JHAAC:1A:62 Baltimore, MD 21224-6801, 410-550-1003.
Jennifer E. Fairman, Email: fairman@jhmi.edu, Department of Art as Applied to Medicine, The Johns Hopkins University School of Medicine, Baltimore, USA., 1830 E Monument St., Suite 7000. Baltimore, MD 21287, 410-955-3213.
Michael C. Schubert, Email: mschube1@jhmi.edu, Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, USA., 601 N. Caroline St., 6th Floor, Room 6245, Baltimore, MD 21287-0910, 410-955-7381.
Jeremy S. Barron, Email: jbarron5@jhmi.edu, Division of Geriatric Medicine and Gerontology, The Johns Hopkins University School of Medicine, Baltimore, USA., 5505 Hopkins Bayview Circle, Baltimore, MD 21224, 410-550-0925.
Jennifer Hughes, Email: jhughe39@jhmi.edu, Division of Geriatric Medicine and Gerontology, The Johns Hopkins University School of Medicine, Baltimore, USA., 5501 Hopkins Bayview Circle, JHAAC:1B:84 Baltimore, MD 21224-6801, 410-550-9016.
Jennifer Millar, Email: jmillar@jhmi.edu, Physical Medicine and Rehabilitation, The Johns Hopkins University School of Medicine, Baltimore, USA., 600 N. Wolfe Street, Meyer 1-130. Baltimore, MD 21287, 410-614-3234.
Anne Spar, Email: aspar@jhmi.edu, Physical Medicine and Rehabilitation, The Johns Hopkins University School of Medicine, Baltimore, USA., 600 N. Wolfe Street, Meyer 1-130. Baltimore, MD 21287, 410-614-3234.
Kristy L. Weber, Email: kweber6@jhmi.edu, Department of Orthopedic Surgery, The Johns Hopkins University School of Medicine, Baltimore, USA., 601 N. Caroline St., 5th Floor, Room 5251, Baltimore, MD 21287-0910, 410-955-2888.
Howard S. Ying, Email: hying1@jhmi.edu, Ophthalmology, The Johns Hopkins University School of Medicine, Baltimore, USA., Maumenee 721 - Ophthalmology, 600 North Wolfe Street, Baltimore, MD 21287, 410-502-5383.
Kathleen M. Zackowski, Email: zackowski@kennedykrieger.org, Physical Medicine and Rehabilitation, The Johns Hopkins University School of Medicine, Baltimore, USA.; Kennedy Krieger Institute, Johns Hopkins Medical Institutions, 707 N Broadway, Baltimore, MD 21205, 443-923-2715.
David Zee, Email: dzee@dizzy.med.jhu.edu, Department of Neurology, The Johns Hopkins University School of Medicine, Baltimore, USA., Pathology 2-210, 600 N. Wolfe Street, Baltimore, MD 21287-7247, Phone: 410-955-3319, Fax: 410-614-1746.
Yuri Agrawal, Email: yagrawa1@jhmi.edu, Department of Otolaryngology-Head and Neck Surgery, The Johns Hopkins University School of Medicine, Baltimore, USA., 601 N. Caroline St., 6th Floor, Room 6260, Baltimore, MD 21287-0910, Phone: 410-955-1932, Fax: 410-955-0035.
Reference List
- 1.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 1998;53:M112–M119. doi: 10.1093/gerona/53a.2.m112. [DOI] [PubMed] [Google Scholar]
- 2.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 3.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 4.Sattin RW, Lambert Huber DA, DeVito CA, et al. The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol. 1990;131:1028–1037. doi: 10.1093/oxfordjournals.aje.a115594. [DOI] [PubMed] [Google Scholar]
- 5.Freiberger E, De Vreede P. Falls recall—limitations of the most used inclusion criteria. Eur Rev Aging Phys Act. 2011 [Google Scholar]
- 6.Tinetti ME, Kumar C. The patient who falls: “It's always a trade-off”. JAMA. 2010;303:258–266. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamb SE, McCabe C, Becker C, Fried LP, Guralnik JM. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: the Women's Health and Aging Study. J Gerontol A Biol Sci Med Sci. 2008;63:1082–1088. doi: 10.1093/gerona/63.10.1082. [DOI] [PubMed] [Google Scholar]
- 8.Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 9.Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing. 2006;35:5–10. doi: 10.1093/ageing/afi218. [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Clinical Excellence. London: Royal College of Nursing; 2004. Clinical practice guideline for the assessmetn and prevention of falls in older people. [PubMed] [Google Scholar]
- 11.Skelton DA, Hauer K, Lamb S. Re: ‘falls definition validation’. Age Ageing. 2007;36:111–112. doi: 10.1093/ageing/afl138. [DOI] [PubMed] [Google Scholar]
- 12.Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a fall and reasons for falling: comparisons among the views of seniors, health care providers, and the research literature. Gerontologist. 2006;46:367–376. doi: 10.1093/geront/46.3.367. [DOI] [PubMed] [Google Scholar]
- 13.Dickens J, Jones M, Johansen A. Falls definition--reliability of patients' own reports. Age Ageing. 2006;35:450–451. doi: 10.1093/ageing/afl016. [DOI] [PubMed] [Google Scholar]
- 14.The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull. 1987;34(4):1–24. [PubMed] [Google Scholar]
- 15.Buchner DM, Hornbrook MC, Kutner NG, et al. Development of the common data base for the FICSIT trials. J Am Geriatr Soc. 1993;41:297–308. doi: 10.1111/j.1532-5415.1993.tb06708.x. [DOI] [PubMed] [Google Scholar]
- 16.Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. doi: 10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 17.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 18.Teno J, Kiel DP, Mor V. Multiple stumbles: a risk factor for falls in community-dwelling elderly. A prospective study. J Am Geriatr Soc. 1990;38:1321–1325. doi: 10.1111/j.1532-5415.1990.tb03455.x. [DOI] [PubMed] [Google Scholar]
- 19.Srygley JM, Herman T, Giladi N, Hausdorff JM. Self-report of missteps in older adults: a valid proxy of fall risk? Arch Phys Med Rehabil. 2009;90:786–792. doi: 10.1016/j.apmr.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arnold CM, Faulkner RA. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007;7:17. doi: 10.1186/1471-2318-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53:2190–2194. doi: 10.1111/j.1532-5415.2005.00509.x. [DOI] [PubMed] [Google Scholar]
- 22.Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36:613–616. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- 23.Netemeyer R, Bearden W, Sharma S. Scaling Procedures: Issues and Applications. Thousand Oaks, CA: Sage Publications, Inc; 2003. [Google Scholar]
- 24.Lin FR, Ceh K, Bervinchak D, Riley A, Miech R, Niparko JK. Development of a communicative performance scale for pediatric cochlear implantation. Ear Hear. 2007;28:703–712. doi: 10.1097/AUD.0b013e31812f71f4. [DOI] [PubMed] [Google Scholar]
- 25.Peel N. Validating recall of falls by older people. Accid Anal Prev. 2000;32:371–372. doi: 10.1016/s0001-4575(99)00066-4. [DOI] [PubMed] [Google Scholar]
- 26.Hannan MT, Gagnon MM, Aneja J, et al. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the MOBILIZE Boston Study. Am J Epidemiol. 2010;171:1031–1036. doi: 10.1093/aje/kwq024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lach HW, Reed AT, Arfken CL, et al. Falls in the elderly: reliability of a classification system. J Am Geriatr Soc. 1991;39:197–202. doi: 10.1111/j.1532-5415.1991.tb01626.x. [DOI] [PubMed] [Google Scholar]
- 28.Mackenzie L, Byles J, D'Este C. Validation of self-reported fall events in intervention studies. Clin Rehabil. 2006;20:331–339. doi: 10.1191/0269215506cr947oa. [DOI] [PubMed] [Google Scholar]
- 29.Cumming RG, Kelsey JL, Nevitt MC. Methodologic issues in the study of frequent and recurrent health problems. Falls in the elderly. Ann Epidemiol. 1990;1:49–56. doi: 10.1016/1047-2797(90)90018-n. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


