Abstract
Objective
The National Survey of Family Growth has been a primary data source for trends in US women’s contraceptive use. However, national-level data may mask differences in contraceptive practice resulting from variation in local policies and norms.
Study Design
We used the Pregnancy Risk Assessment Monitoring System), a survey of women who are 2–4 months postpartum. Information on women’s current method was available for 18 reporting areas from 2000–2009. Using the two most recent years of data, we computed the weighted proportion of women using specific contraceptive methods according to payment for delivery (Medicaid or private insurance) and examined differences across states. We used log binomial regression to assess trends in method use in 8 areas with consecutive years of data.
Results
Across states, there was a wide range of use of female sterilization (7.0–22.6%) and long-acting reversible contraception (LARC; 1.9–25.5%). Other methods, like vasectomy and the patch/ring, had a narrower range of use. Women with Medicaid-paid deliveries were more likely to report female sterilization, LARC and injectables as their method compared to women with private insurance. LARC use increased ≥18% per year, while use of injectables and oral contraceptives declined by 2.5%–10.6% annually.
Conclusions
The correlation in method-specific prevalence within states suggests shared social and medical norms, while the larger variation across states may reflect both differences in norms and access to contraception for low-income women. Surveys of postpartum women, who are beginning a new segment of contraceptive use, may better capture emerging trends in US contraceptive method mix.
Implications
There is considerable variation in contraceptive method use across states, which may result from differences in state policies and funding for family planning services, local medical norms surrounding contraceptive practice, and women’s and couples’ demand or preference for different methods.
Keywords: postpartum contraception, long-acting reversible contraception, PRAMS, contraceptive method mix
1. Introduction
Approximately half of pregnancies in the United States (US) are unintended, a figure that has changed little over the last several years [1,2]. One of the reasons for the persistently high rates of unintended pregnancy is that a large percentage of reproductive aged women rely on methods with relatively high typical-use failure rates, such as oral contraceptives (OCs) and condoms [3,4]. Although there has been a recent increase in the use of long-acting reversible contraceptive (LARC) methods, the overall prevalence remains low; among women at risk of unintended pregnancy, 8.5% are using LARC and 50% rely on other non-permanent contraceptive methods [5].
These figures and much of what is known about trends in US women’s contraceptive use comes from one large nationally representative data set: the National Survey of Family Growth (NSFG). However, national-level data may mask differences in women’s contraceptive practice that result from a variety of factors operating at the state and local levels. For example, the availability of programs that provide women, and particularly low-income women, with access to contraception varies across states, as does the income eligibility criterion for these programs [6,7]. Additionally, women’s use of specific methods may vary across communities as a result of differences in medical norms [8–10] or local initiatives, such as the Contraceptive CHOICE project [11]. Furthermore, it is difficult to identify emerging trends in the NSFG since many respondents are long-time users of a specific method, particularly sterilization, and cannot be expected to change. In contrast, surveys conducted postpartum, when women are beginning a new segment of contraceptive use, are better positioned to capture change in the acceptance of new methods.
Authors of a recent study on postpartum teens’ contraceptive use found substantial geographic variation in method use following delivery [12]. Use of the most effective methods, like LARC, ranged from 7.2% of contracepting teens in New York to 50.3% among teens in Colorado, where a state-wide family planning initiative was created to increase use of highly effective methods [13]. However, this study did not include women’s insurance status, which is associated with variation in method use and likely reflects differential patterns of contraceptive access [3,14,15]. Although the authors analyzed several years of data, they did not examine temporal trends, and therefore did not identify how women’s contraceptive use may have changed across both time and place.
In the current study, we address these issues by conducting a further exploration of the variation and trends in US women’s contraceptive use. We use state-level data on postpartum women’s method use collected as part of the Pregnancy Risk Assessment Monitoring System (PRAMS), which until recently, has been a little-used data source to examine women’s contraceptive practice and risk of unintended pregnancy [12,16–18]. In addition to examining variation across states in method use for all women (versus teens only) and changes in method-specific prevalence over time, we assess the extent to which women’s postpartum method use is patterned by insurance status. Although women with Medicaid or who live in certain regions are more likely to rely on particular methods, like female sterilization [14,15,19,20], it is not well-known whether method prevalence among women with Medicaid is related to the prevalence among those with private insurance in the same area.
2. Materials and Methods
2.1. Data
The PRAMS is a survey of postpartum women conducted annually in 40 participating states and New York City through a collaboration between state health departments and the Centers for Disease Control and Prevention (CDC). A representative sample of 1,300 – 3,400 women who gave birth in each reporting area are surveyed by mail two to four months following delivery, and mail non-respondents are contacted via telephone; the sample is stratified by infants’ birth weight (low vs normal) and women’s race/ethnicity in many reporting areas [21]. The survey includes a core set of questions about women’s sociodemographic characteristics and health behaviors before, during and after pregnancy. The core question on contraceptive use asks, “Are you or your husband or partner doing anything now to keep from getting pregnant?” Reporting areas also can include a supplemental question about specific methods used: “What kind of birth control are you or your husband or partner using now to keep from getting pregnant?” Women can select multiple methods.
For this analysis, we requested data from the CDC on PRAMS reporting areas that collected information on women’s specific postpartum contraceptive method between 2000 and 2009 (the most recent year available at the time of our request) and that had achieved the minimum overall response rate required for public release of the data; the minimum response rate was ≥70% between 2000–2006 and ≥65% from 2007–2009. We obtained data from 18 reporting areas (Table 1) for a total sample of 185,436 postpartum women.
Table 1.
PRAMS reporting areas that collected information on specific postpartum contraceptive methods and years of publicly available data
| Alabama | 2000–2003 |
| Arkansas | 2000–2009 |
| Colorado | 2000–2003, 2009 |
| Florida | 2000–2005 |
| Louisiana | 2000–2004 |
| Michigan | 2004–2009 |
| Mississippi | 2003, 2004, 2006, 2008 |
| Nebraska | 2000–2009 |
| New York | 2000–2008 |
| New York City | 2004–2007 |
| North Carolina | 2000–2005, 2007–2008 |
| Ohio | 2000–2003 |
| Oklahoma | 2000–2003 |
| Oregon | 2003–2009 |
| Rhode Island | 2002–2009 |
| South Carolina | 2000–2007 |
| Vermont | 2001–2003 |
| West Virginia | 2000–2008 |
We categorized women’s current method use as: female sterilization; vasectomy; LARC (i.e., IUDs/implants); injectables; OCs; patch/ring; and other methods (condoms, diaphragm, cervical cap, sponge, rhythm method, natural family planning, withdrawal). If a woman selected more than one method, we used her most effective method. Women who were missing information on their postpartum method (n=2,754) were excluded.
Women also reported their payment source for delivery, which we categorized women’s as private insurance, Medicaid (or other public insurance program) and other. We used payment source as an indicator of access to services since publicly insured women may have less consistent access to contraception due to program eligibility criteria and constraints faced by publicly funded clinics where many low-income women seek care [22,23]. After restricting our sample to women with private insurance or Medicaid-paid deliveries, 174,781 postpartum women were included in the analysis.
2.2. Statistical analyses
As a first step, we examined the percentage of women using specific methods in each reporting area, overall and by payment source for delivery. We combined the two most recent years of data available in each reporting area to obtain an adequate sample size within each method category. In Colorado, information on method use was only available between 2000–2003 and in 2009. Since the distribution of methods may have changed considerably between 2003 and 2009, we analyzed data for 2009 only; examination of these data revealed that there was a sufficient sample size for each method (≥5 respondents) to permit analyses of this year alone. We report our results for New York state and New York City separately since local norms and initiatives may affect women’s contraceptive use.
Arkansas, Nebraska, New York, Oregon, Rhode Island, South Carolina and West Virginia had at least seven consecutive years of data available on specific methods – a time series long enough to permit an analysis of trends in method use. Although North Carolina collected information on specific methods used between 2000–2008, it did not meet the minimum response rate in 2006. However, we included the state in our trend analysis using the years of data available. To analyze change in the method-specific prevalence over time, we estimated log binomial regression models for each of these eight PRAMS reporting areas in which we included survey year as a continuous covariate. We estimated separate models for female sterilization, LARC, injectables and OCs since these were the most commonly used methods. The beta coefficient for survey year in the log binomial models, when multiplied by 100, can be interpreted as the annual percent change in the use of each method. Here, we present the percentage of women using each method during the first year under study along with the annual percent change and 95% confidence interval.
All analyses were conducted in Stata 11.0 and weighted to account for the complex sampling design and non-response in the PRAMS. Use of these publicly accessible data was not considered human subjects research by the first author’s university Institutional Review Board.
3. Results
Across these 18 reporting areas, there is substantial variation in the percentage of postpartum women using specific methods (Table 2). There is a wide range of use for female sterilization (7.0–22.6%) and LARC (1.9–25.5%). Other methods, like vasectomy and the patch/ring, have a narrower range of use (1.0–5.4% and 2.2–8.5%, respectively). OCs are commonly used in all reporting areas with 22.0–34.2% of women relying on this method. The percentage of women using other, less effective methods, like condoms and withdrawal, ranged from 13.7% (Mississippi) to 45.8% (New York City), but 20–30% of women in most reporting areas use these methods.
Table 2.
Distribution of contraceptive method use, by PRAMS reporting area
| n in sample | Female Sterilization | Vasectomy | LARC | Injectables | Patch/Ring | OCs | Other Methods | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| %* | %* | %* | %* | %* | %* | %* | ||
| Alabama | 2,563 | 19.9 | 4.2 | 2.4 | 16.0 | 4.2 | 33.0 | 20.3 |
| Arkansas | 2,076 | 16.5 | 3.3 | 17.4 | 9.8 | 3.6 | 26.1 | 23.3 |
| Colorado | 1,453 | 10.2 | 3.2 | 23.8 | 7.7 | 3.0 | 22.0 | 30.0 |
| Florida | 2,903 | 16.5 | 3.4 | 5.8 | 10.4 | 6.1 | 28.0 | 29.8 |
| Louisiana | 2,556 | 18.8 | 2.5 | 1.9 | 13.7 | 8.5 | 33.7 | 20.9 |
| Michigan | 2,409 | 11.1 | 4.8 | 15.6 | 9.0 | 2.3 | 27.4 | 29.7 |
| Mississippi | 1,885 | 22.6 | 2.0 | 9.4 | 14.0 | 4.3 | 33.9 | 13.7 |
| Nebraska | 2,408 | 11.5 | 3.0 | 18.4 | 6.0 | 2.7 | 27.3 | 31.0 |
| New York | 1,573 | 9.0 | 2.8 | 10.7 | 8.3 | 3.2 | 32.1 | 34.0 |
| New York City | 1,941 | 7.0 | 1.0 | 8.5 | 8.9 | 2.8 | 26.0 | 45.8 |
| North Carolina | 2,316 | 12.5 | 3.0 | 19.7 | 9.8 | 2.8 | 27.3 | 24.9 |
| Ohio | 2,240 | 13.1 | 4.7 | 2.1 | 10.7 | 8.2 | 32.7 | 28.5 |
| Oklahoma | 2,725 | 16.5 | 3.5 | 3.2 | 14.9 | 5.0 | 32.2 | 24.7 |
| Oregon | 2,353 | 11.7 | 4.0 | 24.4 | 7.1 | 2.4 | 23.1 | 27.3 |
| Rhode Island | 1,879 | 11.3 | 3.3 | 25.5 | 6.6 | 3.5 | 24.4 | 25.3 |
| South Carolina | 1,602 | 16.9 | 2.3 | 8.9 | 11.1 | 4.9 | 34.2 | 21.7 |
| Vermont | 2,023 | 10.5 | 5.4 | 6.1 | 8.6 | 3.8 | 31.0 | 34.7 |
| West Virginia | 2,571 | 20.8 | 3.3 | 10.2 | 8.1 | 2.2 | 34.0 | 21.4 |
Data source: AL 2002–2003; AR 2008–2009; CO 2009; FL 2004–2005; LA 2003–2004; MI 2008–2009; MS 2006, 2008; NE 2008–2009; NY 2007–2008; NYC 2006–2007;
NC 2007–2008; OH 2002–2003; OK 2002–2003; OR 2008–2009; RI 2008–2009; SC 2006–2007; VT 2002–2003; WV 2007–2008
Percentages are weighted to reflect the sampling design and non-response in the PRAMS.
LARC: long-acting reversible contraception (IUDs, implants); OCs: Oral contraceptives
Other methods included: condoms, diaphragm, cervical cap, sponge, rhythm method, natural family planning, and withdrawal
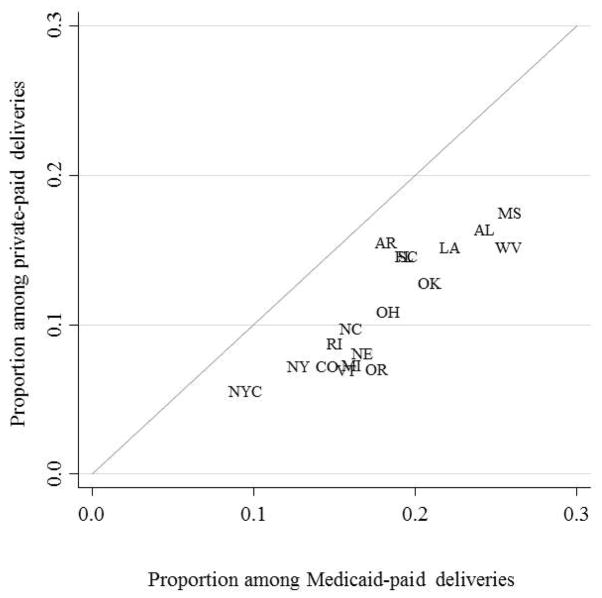
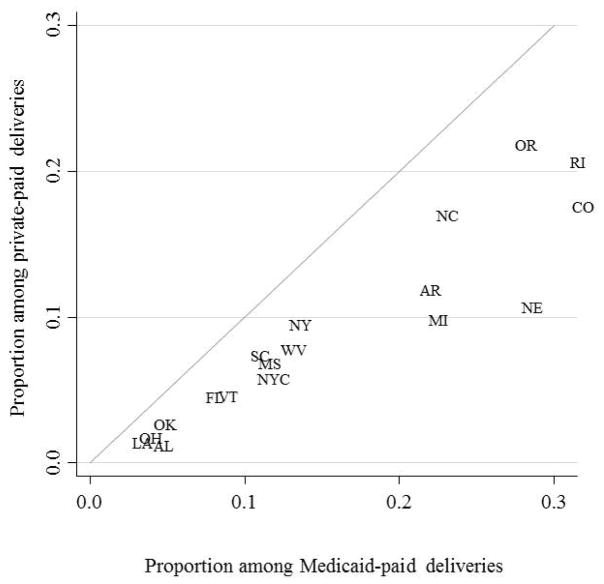
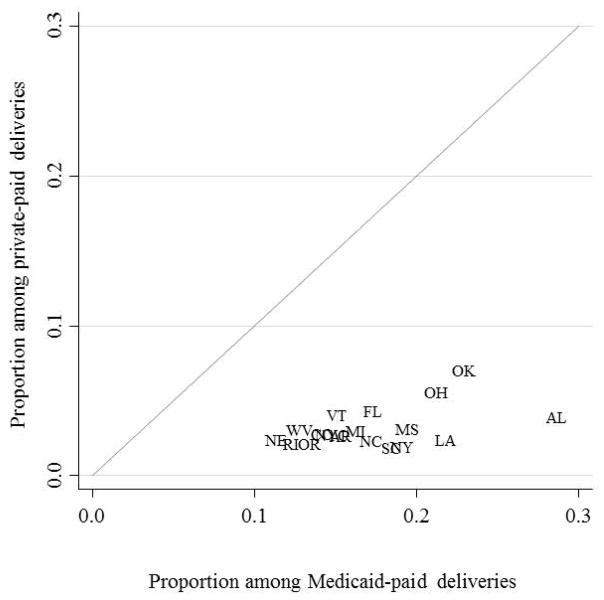
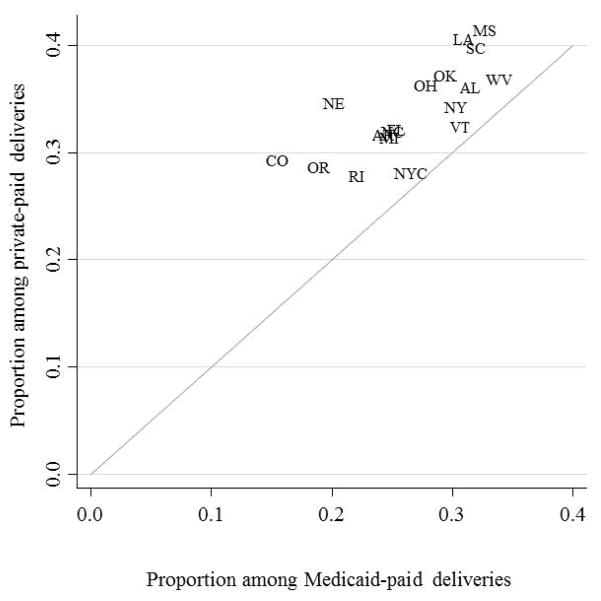
Figure 1 shows scatter plots of the proportion of women with Medicaid-paid deliveries (x-axis) and private insurance (y-axis) using specific methods. For female sterilization (Figure 1a), all points lie slightly below the diagonal, indicating somewhat greater use of the method among publicly insured women compared to those with private insurance. A similar pattern is observed for LARC (Figure 1b). Additionally, there is a clear correlation between the use of these methods in each insurance category across a very wide range of prevalence. In contrast to female sterilization and LARC, points for injectables lie far below the diagonal (Figure 1c), and those for OCs are above the diagonal (Figure 1d). Correlation across insurance status is less evident for these two methods.
Figure 1.
Proportion of women using contraception, by payment source for delivery and PRAMS reporting area
Figure 1a. Female sterilization
Figure 1b. LARC
Figure 1c. Injectables
Figure 1d. OCs
NOTES: LARC: long-acting reversible contraception (IUDs, implants); OCs: Oral contraceptive pills
For five of the eight reporting areas with consecutive years of data on postpartum method use, there has been relatively little change in female sterilization use over time, despite large differences in the baseline prevalence of women relying on this method (Table 3). There has been a significant decrease in the percentage of women in Arkansas who rely on female sterilization postpartum, while the percentage using this method has increased in Nebraska and West Virginia. Use of LARC has increased significantly over time for women in all eight reporting areas, with the annual percent increase ranging from 18% in Oregon to 33.5% in West Virginia. Additionally, there have been significant decreases in the prevalence of injectable use in all reporting areas, except New York state. The prevalence of OC use also has decreased slightly but significantly over time.
Table 3.
Baseline and annual percent change in postpartum contraceptive use by PRAMS reporting area
| Female sterilization | LARC | Injectables | OCs | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Baseline % | Annual % change* (95% CI) | Baseline % | Annual % change* (95% CI) | Baseline % | Annual % change* (95% CI) | Baseline % | Annual % change* (95% CI) | |
| Arkansas (2000–2009) | 20.0 | −1.9 (−3.6, −0.2) | 1.2 | 32.8 (29.2, 36.4) | 14.0 | −6.4 (−8.8, −4.1) | 37.6 | −3.6 (−4.9, −2.4) |
| Nebraska (2000–2009) | 8.8 | 2.2 (0.3, 4.2) | 1.5 | 28.6 (26.1, 31.0) | 15.6 | −10.6 (−12.6, −8.6) | 40.0 | −4.2 (−5.2, −3.2) |
| New York (2000–2008) | 9.1 | 0.3 (−2.8, 3.3) | 2.2 | 29.9 (23.8, 36.0) | 10.7 | −2.5 (−6.2, 1.2) | 38.1 | −2.7 (−4.4, −1.0) |
| North Carolina (2000–2008) | 13.7 | −1.8 (−4.0, 0.4) | 3.0 | 31.3 (27.8, 34.8) | 16.8 | −7.7 (−10.2, −5.2) | 40.5 | −5.4 (−6.8, −4.1) |
| Oregon (2003–2009) | 10.2 | 3.3 (−1.4, 7.9) | 7.8 | 18.0 (14.6, 21.4) | 9.4 | −6.3 (−11.4, −1.3) | 30.1 | −5.9 (−8.5, −3.3) |
| Rhode Island (2002–2009) | 9.9 | 1.4 (−1.6, 4.4) | 5.1 | 24.2 (21.2, 27.2) | 9.7 | −5.6 (−9.3, −1.8) | 36.0 | −5.0 (−6.7, −3.3) |
| South Carolina (2000–2007) | 13.4 | 1.0 (−2.3, 4.3) | 2.1 | 22.2 (14.5, 29.9) | 19.3 | −10.0 (−13.9, −6.2) | 42.6 | −3.2 (−5.2, −1.1) |
| West Virginia (2000–2008) | 16.9 | 2.6 (0.7, 4.6) | 0.8 | 33.5 (28.5, 38.6) | 12.6 | −7.5 (−10.3, −4.7) | 43.5 | −3.1 (−4.4, −1.8) |
LARC: long-acting reversible contraception (IUDs, implants); OCs: Oral contraceptives; CI: Confidence interval
Annual percent change estimated using survey weighted log binomial regression models.
4. Discussion
We found striking variation in the specific methods used across the 18 reporting areas. The most notable differences were observed for female sterilization and LARC. Certainly some of this variation is due to the fact that in a few states, like Louisiana, Ohio and Vermont, data were only available from the early 2000’s. In these states, the prevalence of LARC use was low and the prevalence of injectables was high relative to other states. It is possible that the distribution of method use in these states today may look quite different. However, even across areas with more recent data, there were large differences in the percentage of women using specific methods. Less than 10% of postpartum women in New York, Mississippi and South Carolina were using LARC, while more than 20% of women in Colorado, Oregon and Rhode Island were using an IUD or implant.
There are several possible explanations for the variation across states: state policies and funding for family planning services; local medical norms surrounding contraceptive practice; and women’s and couples’ demand or preference for different methods. There is well-known variation in state-level funding and programs for family planning services, particularly for low-income women, which may affect access to contraception postpartum [17,23]. For example, women with Medicaid-paid deliveries may have a higher prevalence of female sterilization and LARC use in some states than others because they have inconsistent contraceptive coverage starting several months after delivery; their state may not have a Medicaid family planning waiver, or they may have to recertify their eligibility and possibly lose coverage due to modest fluctuations in their income in states with more stringent eligibility criteria. As a result, women may be more likely to choose methods that do not require regular contact with the health care system [19].
However, it is unlikely that state programs and funding alone account for such large variation in method use. Both New York and Oregon have Medicaid family planning waivers for women with incomes ≤200% and 250% of the Federal Poverty Level, respectively [6], but quite different prevalence of LARC use. Additionally, there is a close correlation in the proportion of women using specific methods across insurance groups. This finding could reflect the fact that the contraceptive choices being made in these two sectors are closely connected. Whether this is due to overlap and communication among providers, or communication between contraceptive users cannot be ascertained from the PRAMS data, but raises interesting questions for future research.
In addition to state-level variation, our analyses demonstrated that there has been an extremely rapid uptake in LARC among postpartum women over the last decade. Even in the state with the lowest estimated growth rate, Oregon – which also had the highest baseline prevalence, LARC use increased six-fold over a six-year period. This rapid increase lies in marked contrast to previous results on LARC trends reported from the NSFG and California [5,24]. The likely explanation for this difference is that studies of contraceptive use in the general population of reproductive aged women may not be the best sources of data to examine emerging trends, and that postpartum method use is a leading indicator of future patterns in contraceptive method mix, since the postpartum period is when women begin a new segment of use.
Based on the observed trends in postpartum LARC use in these eight states, it would seem that appreciation of and interest in these methods is diffusing rapidly among women and providers. As in other studies [5], it appears that the increase in LARC use is mainly replacing use of injectables and OCs. Use of female sterilization, on the other hand, has been relatively stable, and the wide variation we found across reporting areas cannot be interpreted as resulting from early versus late adoption in the diffusion process, and seems to result from well-entrenched differences in medical norms and users’ preferences.
This study has several limitations. First, our analysis is limited to states that chose to include the question on the specific postpartum method women used. Although our findings are representative of women giving birth in each state, they are not generalizable to other states, which accounted for 67% of US births in 2009 [25]. Additionally, the question about postpartum method use focuses on women’s use at the time of the survey (two to four months postpartum) and therefore does not offer a complete view of the dynamic process of adopting methods that women may go through following delivery. Finally, the PRAMS does not include questions about the nature of contraceptive counseling women received during and after their pregnancy, what methods they were offered (but did not accept), or their preferred method, which could illuminate whether the variation in method use reflects women’s preferences, medical norms or access to services.
Despite these limitations, our results show surprising differences in contraceptive method use across states and offer a new perspective on major shifts in women’s contraceptive practice. Additionally, they point to the PRAMS as a potentially valuable, but relatively underutilized, resource for studying contraceptive adoption in the US. PRAMS would be an even more valuable resource if all participating states included the optional question on specific method use.
Acknowledgments
Infrastructural support for the study was provided by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R24 042849) to the Population Research Center, University of Texas at Austin. We would like to acknowledge the CDC PRAMS Team, Applied Sciences Branch, Division of Reproductive Health and PRAMS Working Group. We would also like to thank the PRAMS state coordinators who assisted us with the preliminary analyses of these data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 2.Finer LB, Zolna MR. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception. 2011;84:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones J, Mosher W, Daniel K. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 4.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the U.S 2007–2009. Fertil Steril. 2012;98:893–97. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guttmacher Institute. Medicaid family planning eligibility expansions. New York: Guttmacher Institute; Apr 1, 2013. [PubMed] [Google Scholar]
- 7.Kaiser Family Foundation, The George Washington University Medical Center School of Public Health and Health Services. State medicaid coverage of family planning services: Summary of state findings. Menlo Park: Henry J. Kaiser Family Foundation; 2009. [Accessed May 2013]. Available from: http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8015.pdf. [Google Scholar]
- 8.Potter JE. The persistence of outmoded contraceptive regimes: The cases of Mexico and Brazil. Population and Development Review. 1999;25:703–739. [Google Scholar]
- 9.Birkmeyer JD, Sharp SM, Finlayson SRG, et al. Variation profiles of common surgical procedures. Surgery. 1998;124:917–23. [PubMed] [Google Scholar]
- 10.Wennberg J, Gittelson A. Small area variations in health care delivery. Science. 1973;182:1102–08. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- 11.Secura GM, Allsworth JE, Madden T, et al. The contraceptive CHOICE project: Reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010:203. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gavin L, Warner L, O’Neil ME, et al. Vital signs: Repeat births among teens - United States, 2007–2010. Morbidity and Mortality Weekly Report. 2013;62:1–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Philliber Research Associates, Bixby Center for Global Reproductive Health. Evaluating the Colorado initiative to reduce unintended pregnancies. New York: Philliber Research Associates; 2010. [Accessed August 2013]. Available from: http://bixbycenter.ucsf.edu/publications/files/Brief_2_Colorado%28Feb2010%29.pdf. [Google Scholar]
- 14.Baldwin MK, Rodriguez MI, Edelman AB. Lack of insurance and parity influence choice between long-acting reversible contraception and sterilization in women postpregnancy. Contraception. 2012;86:42–7. doi: 10.1016/j.contraception.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Whiteman MK, Cox S, Tepper NK, et al. Postpartum intrauterine device insertion and postpartum tubal sterilization in the United States. Am J Obstet Gynecol. 2012;206:127, e1–7. doi: 10.1016/j.ajog.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Finer LB, Kost K. Unintended pregnancy rates at the state level. Perspect Sex Reprod Health. 2011;43:78–87. doi: 10.1363/4307811. [DOI] [PubMed] [Google Scholar]
- 17.Kost K, Finer LB. Explaining variation in state unintended pregnancy rates in the United States. Perspect Sex Reprod Health. 2012;44:57–64. doi: 10.1363/4405712. [DOI] [PubMed] [Google Scholar]
- 18.Wilson EK, Fowler CI, Koo HP. Postpartum contraceptive use among adolescent mothers in seven states. J Adolesc Health. 2013;52:278–83. doi: 10.1016/j.jadohealth.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 19.Borrero S, Schwarz EB, Reeves MF, et al. Race, insurance status, and tubal sterilization. Obstet Gynecol. 2007;109:94–100. doi: 10.1097/01.AOG.0000249604.78234.d3. [DOI] [PubMed] [Google Scholar]
- 20.Chan LM, Westhoff CL. Tubal sterilization trends in the US. Fertil Steril. 2010;94:1–6. doi: 10.1016/j.fertnstert.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention, Division of Reproductive Health. [Accessed April 2013];PRAMS methodology: Centers for Disease Control and Prevention. 2012 Available from: http://www.cdc.gov/prams/Methodology.htm.
- 22.Lindberg LD, Frost JJ, Sten C, Dailard C. Provision of contraceptive and related services by publicly funded family planning clinics, 2003. Perspect Sex Reprod Health. 2006;38:139–47. doi: 10.1363/psrh.38.139.06. [DOI] [PubMed] [Google Scholar]
- 23.Wood S, Goldberg D, Beeson T, et al. Health centers and family planning: Results from a nationwide survey. Washington, D.C: The George Washington University School of Public Health and Health Services; 2013. [Google Scholar]
- 24.Thompson KM, Foster DG, Harper CC. Increased use of intrauterine contraception in California, 1997 to 2007. Women’s Health Issues. 2011;21:425–30. doi: 10.1016/j.whi.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 25.Martin JA, Hamilton BE, Ventura SJ, et al. Births: Final data for 2009. National vital Statistics Reports. 2011;60:1. [PubMed] [Google Scholar]