Abstract
OBJECTIVE
To examine the longitudinal effects of comorbid anxiety disorders in youth with bipolar spectrum disorder (BP).
METHOD
As part of the Course and Outcome of Bipolar Youth study, 413 youth, ages 7 to 17 years who met criteria for DSM-IV BP-I (n=244), BP-II (n=28), and operationally defined bipolar disorder not otherwise specified (BP-NOS) (n=141) were included. Subjects were followed on average 5 years using the Longitudinal Interval Follow-up Evaluation. Effects of anxiety on the time to mood recovery and recurrence and percentage of time with syndromal and subsyndromal mood symptomatology during the follow-up period were analyzed.
RESULTS
At intake and during the follow-up, 62% of youth with BP met criteria for at least one anxiety disorder. About 50% of the BP youth with anxiety had ≥ 2 anxiety disorders. Compared to BP youth without anxiety, those with anxiety had significantly more depressive recurrences and significantly longer median time to recovery. The effects of anxiety on recovery disappeared when the severity of depression at intake was taken into account. After adjusting for confounding factors, BP youth with anxiety, particularly those with ≥ 2 anxiety disorders, spent significantly less follow-up time asymptomatic and more time with syndromal mixed/cycling and subsyndromal depressive symptomatology compared to those without anxiety.
CONCLUSIONS
Anxiety disorders are common and adversely affect the course of BP in youth, as characterized by more mood recurrences, longer time to recovery, less time euthymic, more time in mixed/cycling and depressive episodes. Prompt recognition and the development of treatments for BP youth with anxiety are warranted.
Keywords: anxiety disorders, bipolar disorders, longitudinal study
INTRODUCTION
The frequency with which anxiety symptoms accompany manic and depressive states was originally noted by Kraepelin, 1 and modern clinical and epidemiological studies also confirm the presence of anxiety disorders in youth with bipolar disorders (BP). 2–5
While comorbid anxiety disorders have been linked to poorer prognosis and an increased risk of suicide in youth with BP, 6 these observations are primarily cross-sectional in nature. 2, 5 To our knowledge only 2 studies have investigated the effect of comorbid anxiety disorders in youth with BP longitudinally. Masi et al. (2007)7 followed a sample of 224 youth with BP spectrum disorders for a minimum of 6 months, noting that those with concurrent panic disorder (PD) showed less mood severity at baseline but greater persistence of illness during the follow-up compared to those without PD. Similarly, DelBello et al., (2007) 4 followed a group of 71 adolescents with BP-I for 1 year after discharge from the hospital and observed more severe mood symptoms and lower rates of recovery amongst those with comorbid anxiety disorders compared to those without anxiety.
Longitudinal studies in adults report similar associations; namely, that comorbid anxiety confers greater affective morbidity, including less time spent with euthymic mood, 8–10 more severe depressive symptoms and more follow-up time in depression, 10, 11 more rapid cycling, 8 increased time to episode remission, 8 and earlier relapse. 9 Comorbid anxiety has also been associated with greater substance use, 8 poorer psychosocial functioning,8, 9 and poorer response to pharmacological treatments. 10
In a prior publication, 12 we reported that anxiety disorders that were ascertained at intake persisted in 50% of the youth with BP; persistence of anxiety disorders over the follow-up period was defined as at least 50% of follow-up time meeting full-threshold DSM-IV anxiety disorders criteria. Moreover, during approximately 5 years, 25% of the youth with BP who did not have anxiety disorders at intake developed new onset anxiety disorders. In comparison with youth who had anxiety disorders at intake, those who developed anxiety disorders during the follow-up showed significantly more substance abuse (10/92, 40% vs. 5/162, 33%, χ2=6.4, p=0.01). There were no other between-group demographic or clinical differences. Given the clinical implications and the existence of few longitudinal studies examining the longitudinal effects of comorbid anxiety disorders in BP youth, we sought to extend our prior findings and examine the impact of anxiety on the 5-year prospective course and outcome of youth with bipolar spectrum disorders. Based on the literature, we hypothesized that in comparison with BP youth without anxiety disorders, those with anxiety disorders will have: 1) less recovery and more recurrences, and 2) less percentage of follow-up time spent asymptomatic and more with syndromal and subsyndromal mood symptomatology.
METHOD
Subjects
The original sample of Course and Outcome of Bipolar Youth study (COBY) consisted of 446 youth (BP-I=260, BP-II =32, BP-NOS; n=154). In comparison with the 413 who participated in this study, those who did not participate (n=33) showed significantly less any anxiety disorders (39, 2% vs. 69.6%, χ2= 7.5, p=0.006). There were no other between-group demographic or clinical differences. The present study included 413 youth, ages 7 to 17 years 11 months (12.6 ± 3.3 years old) who met criteria for Diagnostic and Statistical Manual IV (DSM-IV) BP-I (n=244), BP-II (n=28), and operationally defined BP-NOS (n=141) and were recruited primarily through clinical referrals from 3 academic medical centers (University of Pittsburgh Medical Center, Brown University, and University of California at Los Angeles). 13 To date, subjects have been prospectively interviewed on average every 37.13 ± 20.4 weeks for a mean of 261.7 ± 94.1 weeks (approximately 5 years). At present, subject retention rate is 84.8%.
Because the DSM-IV criteria for BP-NOS are vague, the COBY study investigators set the minimum inclusion threshold for the BP-NOS group as subjects who did not meet the DSM-IV criteria for BP-I or BP-II but had a distinct period of abnormally elevated, expansive, or irritable mood plus the following: (1) 2 DSM-IV manic symptoms (3 if the mood is irritability only) that were clearly associated with the onset of abnormal mood, (2) a clear change in functioning, (3) mood and symptom duration of a minimum of 4 hours within a 24-hour period for a day to be considered meeting the diagnostic threshold, and (4) a minimum of 4 days (not necessarily consecutive) meeting the mood, symptom, duration, and functional change criteria over the subject's lifetime, which could be two 2-day episodes, four 1-day episodes, or another variation 14.
Institutional review board approval was obtained at each site prior to subject enrollment. After the Institutional Review Board approval, consent or assent was obtained from all participants by project staff prior to administering study instruments.
Procedures
The methods used to evaluate the subjects were reported in detail elsewhere. 15 In summary, at intake children and parents were interviewed for the presence of current and lifetime psychiatric disorders using the Schedule for Affective Disorders and Schizophrenia for School Age Children, Present and Lifetime Version (K-SADS-PL), 16 the Kiddie Mania Rating Scale (K-MRS) 17 and the Depression Rating Scale (DRS) which was derived from the respective sections of the KSADS-P. The index episode was defined as the current or most recent episode assessed at intake. To ascertain the episode duration, time to recovery was calculated from the onset of the index episode. Therefore, for some subjects the duration of episode exceeds the length of prospective follow-up.
Parents were also interviewed at intake about their personal psychiatric history using the Structured Clinical interview for DSM-IV Axis I Disorder (SCID), 18 and about first- and second-degree psychiatric family history using a modified version of the Family History Screen (FHS). 19 Socioeconomic status (SES) was measured using the Hollingshead 4-factor scale. 20 Functional impairment was assessed using the Child Global Assessment Scale (CGAS). 21 The child and parent Screen for Child Anxiety Related Emotional Disorder (SCARED) 22 was used to evaluate severity of anxiety symptoms. Pubertal status and equivalent Tanner Stage was assessed with the Petersen Pubertal Developmental Scale (PDS). 23
Longitudinal change in psychiatric symptoms, functioning, and treatment exposure since the previous evaluation were assessed using the Longitudinal Interval Follow-up Evaluation (LIFE). 24 The LIFE was administered to adolescents and parents separately. When younger children had problems timing their symptoms, they were interviewed with their parents. Any discrepancies between the informants' responses were discussed and a summary score based on all available information was determined. The LIFE evaluates the course of symptoms by identifying change points, frequently anchored by memorable dates for the subject (e.g., holidays and beginning of school). The severity of ongoing symptoms, onset of new symptoms, and episode polarity for BP since the last appointment are tracked using weekly LIFE Psychiatric Status Rating (PSR) scores. Symptoms for each disorder were not double counted.15 For DSM-IV mood disorders, the PSR scores range from 1 for no symptoms, 2 to 4 for varying levels of subthreshold symptoms and impairment, to 5 or 6 for full criteria with different degrees of severity or impairment. 15 Most of the anxiety disorders were rated on a 6-point scale of 1 to 6, where 5 and 6 indicate presence of fulfilled DSM-IV symptoms criteria (including impairment). For anxiety disorder NOS and separation anxiety disorders (SAD), other comorbid disorders, and psychosis were assigned weekly scores on a 3-point scale of 1 to 3, where 2 indicates subthreshold level of symptoms and 3 indicates presence of full DSM-IV symptoms criteria (including impairment). Clinically relevant psychotic symptoms were assigned a PSR score of 3 (definitely present) for delusions and/or hallucinations. 15 Past and current pharmacological treatment was obtained using the Psychotropic Treatment Record of the LIFE. Using this instrument the lifetime exposure to antimanics (lithium, valproic acid, and atypical antipsychotics), antidepressants (mainly selective serotonin reuptake inhibitors [SSRIs]), and stimulants were evaluated. Youth with only specific phobia (e.g., fear of the dark) were excluded because simple phobias are ubiquitous. 2, 12
The percentage of follow-up weeks spent asymptomatic or symptomatic in the different mood symptom categories during the entire follow-up period were computed based on the PSR scores for each subject. Full recovery was defined as 8-consecutive weeks with a score of ≤2 (minimal or no mood symptoms). 15, 25 Time to recovery from the index episode was measured from the onset of the index episode. A recurrence (new episode) required a PSR ≥5, with duration of 1-week for mania/hypomania and 2-weeks for depression. 15 COBY used the DSM-IV definitions for rapid cycling and mixed episodes. 15 Subsyndromal mixed episodes were defined as not having full DSM-IV criteria for mixed episodes.
All assessments were conducted by research staff trained to reliably administer the interviews; interview results were presented to child psychiatrists or psychologists, who confirmed the diagnoses and the PSR scores. 15 The evaluators were not blind to diagnostic group.
Statistical Analyses
Demographic and clinical differences between BP youth with versus without anxiety disorders were evaluated using standard parametric and nonparametric statistics as appropriate. The percent of subjects with recovery from mood episodes and recurrence were compared using chi-square test and significant confounding variables were adjusted using step-wise regression analyses. Time to recovery and recurrence after the index mood episode were compared using survival analyses. Stepwise Cox proportional hazard regression, keeping anxiety into the model, were utilized to adjust for between group demographic and clinical variables with p-values< 0.1. Age onset of mood symptoms and duration of BP (r=−0.58; p<0.0001) and DRS at intake and DRS during the most severe lifetime (r=0.55; p<0.0001) were significantly correlated. Thus, for simplicity, only duration of BP and DRS at intake was included in the analyses. Finally, the proportion of follow-up time (% weeks) spent asymptomatic, with subsyndromal and syndromal mood symptomatology and psychosis as measured by the PSR were analyzed using general linear models and adjusting for any between group demographic and clinical differences. Given that the majority of subjects with obsessive-compulsive disorder (OCD) or posttraumatic stress disorder (PTSD) also met criteria for another anxiety disorder, 26 we analyzed the sample together. In addition, exploratory analyses examining the effects of specific anxiety disorders on the course of the mood symptomatology were done. All p-values are based on 2-tailed tests with p-value ≤0.05.
RESULTS
Prevalence and Demographics
Sixty-two percent (256/413) of youth with BP met criteria for an anxiety disorder at intake or at any time during the follow-up. Among those with any anxiety disorder, the prevalence of specific anxiety disorders was as follows: 19.53% panic disorder, 46.09% SAD, 28.13% social anxiety disorder, 43.36% generalized anxiety disorder (GAD), 23.44% OCD, 19.14% PTSD, 17.19% anxiety-NOS, 7.42% agoraphobia. Approximately 55% of anxious subjects had ≥ 2 anxiety disorders (50.8% excluding anxiety-NOS), particularly SAD and GAD. BP youth with anxiety had significantly lower SES, were less likely to live with both natural parents, and had greater length of follow-up compared to BP youth without anxiety (Table 1; all p-values ≤0.03). There were no other between-group demographic differences.
Table 1.
Demographic and Clinical Characteristics Among Youth With Bipolar Disorder With Versus Without Anxiety Disorders
| BP with Anxiety (n=256) |
BP without Anxiety (n=157) |
stats | p-value | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 12.6±3.3 | 12.7 ± 3.2 | |t| = 0.25 | 0.80 |
| Sex, female (%) | 48.4 | 43.3 | χ2 = 1.03 | 0.31 |
| Race, White (%) | 81.3 | 83.4 | χ2 = 0.32 | 0.57 |
| SES | 3.3 ± 1.2c | 3.6 ± 1.2 | |t| = 2.96 | 0.003 |
| Living with both natural parents (%) | 37.9 | 49.0 | χ2 = 4.97 | 0.03 |
| Pubertal Status | ||||
| I | 25.4 | 30.1 | ||
| II–III | 29.2 | 24.8 | χ2 = 1.12 | 0.6 |
| IV–V | 45.4 | 45.1 | ||
| Follow-up period (weeks) | 271.4±92.2 | 245.9±95.3 | |t| = 2.70 | 0.007 |
| Clinical Characteristics | ||||
| BP Subtype (%) | ||||
| BP-I | 57.0 | 62.4 | ||
| BP-II | 8.6 | 3.8 | χ2 =3.76 | 0.15 |
| BP-NOS | 34.4 | 33.8 | ||
| Age Onset of Mood Symptoms a | 8.0±3.8 | 9.0±4.3 | |t| = 2.54 | 0.01 |
| Duration of BP b | 4.8±3.2 | 3.7±2.5 | |t| = 3.88 | 0.0001 |
| Mania Rating Scale | ||||
| Intake | 23.3±11.8 | 22.2±12.6 | |t| = 0.83 | 0.41 |
| Most Severe Lifetime | 34.5±7.4 | 33.7±9.0 | |t| = 0.77 | 0.44 |
| Depression Rating Scale | ||||
| Intake | 17.0±9.9 | 10.8±9.5 | |t| = 6.28 | <.0001 |
| Most Severe Lifetime | 24.8±9.8 | 19.4±11.3 | |t| = 4.63 | <.0001 |
| Age of Onset of Anxiety Disorders | 8.9±5.1 | |||
| SCARED | ||||
| Child-Intake | 28.6±17.0 | 18.4±17.5 | |t| = 5.33 | <.0001 |
| Parent-Intake | 30.7±15.6 | 15.7±12.2 | |t| = 10.16 | <.0001 |
| ADHD (%) | 61.7 | 55.4 | χ2 = 1.60 | 0.21 |
| ODD (%) | 35.9 | 44.0 | χ2 = 2.63 | 0.11 |
| CD (%) | 12.9 | 10.2 | χ2 = 0.68 | 0.41 |
| SUD (%) | 10.2 | 5.7 | χ2 = 2.46 | 0.12 |
| Suicide Attempt (%) | 34.4 | 21.7 | χ2 = 7.57 | 0.006 |
| History of Physical or Sexual Abuse (%) | 25.0 | 10.8 | χ2 = 12.4 | 0.0004 |
| Psychotic Symptoms (%) | 23.8 | 19.8 | χ2 = 0.94 | 0.33 |
| CGAS | ||||
| Intake | 55.2±11.2 | 54.1±13.8 | |t| = 0.85 | 0.39 |
| Most Severe Lifetime | 37.6±11.4 | 37.4±9.0 | |t| = 0.12 | 0.91 |
| Lifetime Psychosocial Treatment (% Yes) | 99.6 | 98.7 | F=1.05 | 0.56 |
| Lifetime Pharmacological Treatment (% Yes) | ||||
| Any Psychotropics | 95.3 | 96.2 | χ2 = 0.18 | 0.68 |
| Antimanics | 79.3 | 84.7 | χ2 = 1.88 | 0.17 |
| Antidepressants | 63.3 | 42.7 | χ2 = 16.73 | <.0001 |
| Stimulants | 58.2 | 52.9 | χ2 = 1.13 | 0.29 |
| Psychiatric Family History (% of subjects with at least one 1st or 2nddegree relative) | ||||
| Mania/Hypomania | 55.9 | 42.7 | χ2 = 6.77 | 0.009 |
| Depression | 86.7 | 74.5 | χ2 = 9.84 | 0.002 |
| Anxiety Disorder | 68.4 | 57.3 | χ2 = 5.15 | 0.02 |
| Any Substance Use Disorder | 71.9 | 64.3 | χ2 = 2.59 | 0.11 |
| Suicide Attempt | 42.2 | 38.2 | χ2 = 0.64 | 0.43 |
Note: ADHD = attention-deficit/hyperactivity disorder; BP = bipolar disorder; BP-I = bipolar I disorder; BP-II = bipolar II disorder; BP-NOS = bipolar disorder not otherwise specified; CD = conduct disorder; CGAS = Child Global Assessment Scale; F = Fisher exact test; ODD = oppositional defiant disorder; SCARED = Screen for Child Anxiety Related Emotional Disorder; SES = socioeconomic status; SUD = substance use disorder.
Age 4 is set as the minimum value.
Calculated from age at onset of any DSM mood episode.
Equivalent to middle class.
Clinical Characteristics
As shown in Table 1, compared with BP youth without anxiety, BP youth with anxiety had significantly earlier age of onset of mood symptoms, longer duration of BP, higher self- and parent-rated depression and anxiety scores at intake and over follow-up, higher rates of past suicide attempts, and higher rates of physical or sexual abuse. In addition, BP youth with anxiety had significantly higher lifetime rates of treatment with antidepressants and had more family history of mania/hypomania, depression, and anxiety compared to BP youth without anxiety (for all above noted comparisons p-values ≤0.02). There were no significant differences in the history of lifetime psychosocial treatments between BP youth with and without anxiety disorders.
Of all the above demographic and clinical univariate differences only the following factors remained significant in the step-wise regression models: socioeconomic status, living with both natural parents, duration of BP, DRS at intake, history of physical and sexual abuse, family history of mania/hypomania, depression and anxiety, and follow-up time period. These variables were entered in all the analyses described below.
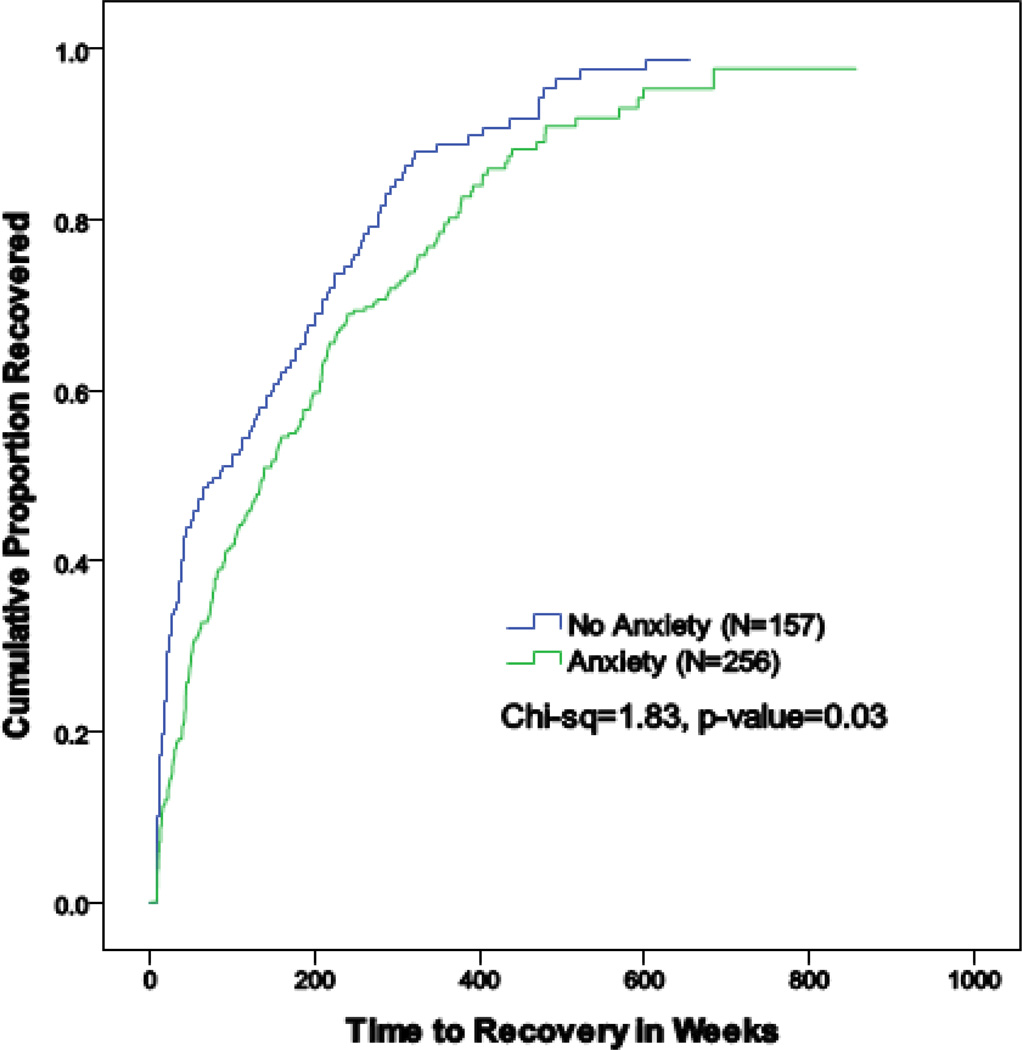
Recovery From the Index Episode (Table 2 and Figure 1)
Table 2.
Summary of Recovery and Recurrence Among Youth With Bipolar Disorder (BP) With Versus Without Anxiety Disorders
| BP with Anxiety (n=256) |
BP without Anxiety (n=157) |
Statistics | Unadjusted p-value |
|||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Rate of Recovery | 217/256 | 84.8 | 140/157 | 89.2 | χ2=1.61 | 0.20 |
| Rate of Recurrence a | 165/217 | 76.0 | 79/140 | 56.4 | χ2=15.12 | 0.0001 |
| Time to recovery from the index episode, weeks b | 138.29 | 86.57 | log-rank χ2= 8.88 | 0.003 | ||
| Time to recurrence, weeksc | 37.00 | 48.00 | log-rank χ2=3.23 | 0.07 | ||
Note:
Recurrence required either 1 week of Psychiatric Status Rating Scales scores ≥5 for mania/hypomania or 2 consecutive weeks of Psychiatric Status Rating Scales scores ≥5 for depression
The index episode was defined as the current or most recent episode assessed at intake. To ascertain the episode duration, time to recovery was calculated form the onset of the index episode. Therefore, for some subjects the duration of episode exceeds the length of prospective follow-up
Time to recurrence was calculated from the time participants fulfilled criteria for recovery until they met full criteria for a new episode.
Figure 1.
Recovery from index episode among youth with bipolar disorders with versus without anxiety disorders.
There were no between-group differences in the rates of recovery from the index mood episode.
However, using survival analyses, BP youth with anxiety showed significantly longer median time to recovery than those without anxiety (138.3 weeks vs. 86.6 weeks, χ2=8.88, p=0.003). After adjusting for the above-noted significant confounding factors, the effects of anxiety on time to recovery were no longer significant. However, when the DRS score at intake was removed from the model, anxiety remained significantly associated with recovery (p=0.02).
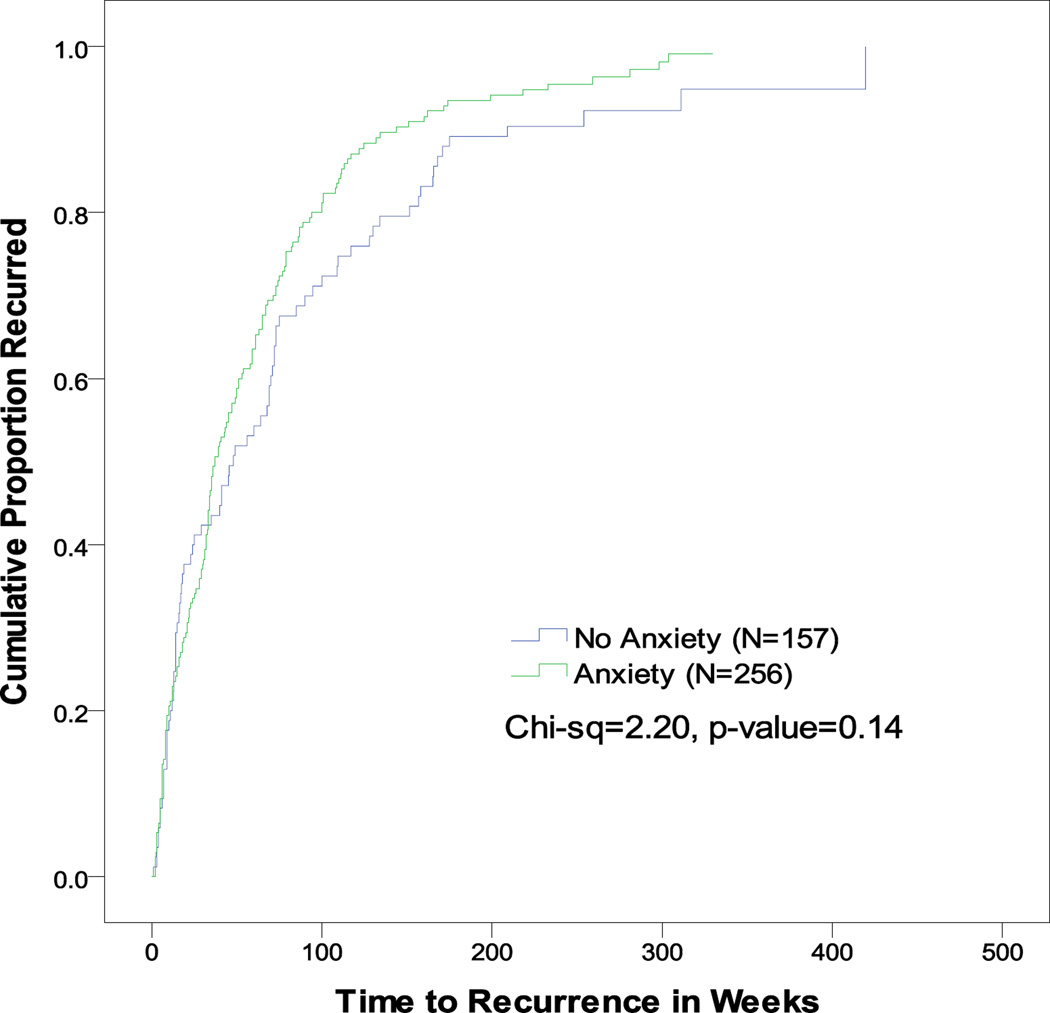
Recurrence After Recovery From the Index Episode (Table 2 and Figure 2)
Figure 2.
Recurrence after recovery from index episode among youth with bipolar disorder with versus without anxiety disorders.
Among youth who recovered from the index episode, those with anxiety were significantly more likely to experience any mood recurrences (76% vs. 56.4%, χ2=15.12, p=0.0001) and depression recurrences specifically (64.9% vs. 49.4%; F=5.33; p=0.02) when compared to those without anxiety disorders. Similar results were obtained after adjusting for the above-noted significant confounding factors. There were no between-group differences in the median time to recurrence and to other polarity recurrences.
Week-by-Week Mood Symptom Analyses (Table 3)
Table 3.
Weekly Symptomatic Status Among Youth With Bipolar Disorder (BP) With Versus Without Anxiety Disorders
| BP with Anxiety (n=256) |
BP without Anxiety (n=157) |
|t| | Unadjusted p-value |
Fa | Adjusted p- valuea |
|
|---|---|---|---|---|---|---|
| Asymptomatic (%) | 37.5±26.4 | 55.2±30.8 | 5.99 | <.0001 | 12.08 | 0.0006 |
| Syndromal (%) | ||||||
| Mania | 18.8±19.3 | 10.2±16.4 | 4.85 | <.0001 | 4.93 | 0.028 |
| Hypomania | 1.0±3.3 | 1.2±4.0 | 0.70 | 0.49 | 0.11 | 0.75 |
| Mixed/Cycling | 1.9±5.8 | 1.7±5.5 | 0.46 | 0.64 | 0.29 | 0.6 |
| MDD | 9.0±13.0 | 3.7±10.6 | 4.56 | <.0001 | 4.67 | 0.03 |
| 6.8±10.3 | 3.5±9.6 | 3.21 | 0.001 | 1.37 | 0.25 | |
| Subsyndromal (%) | 43.7±24.0 | 34.6±27.2 | 3.57 | 0.0004 | 4.75 | 0.03 |
| Mania | 11.6±12.9 | 13.9±18.4 | 1.41 | 0.16 | 0.82 | 0.36 |
| Mixed | 16.6±18.6 | 10.4±18.7 | 3.30 | 0.001 | 2.33 | 0.13 |
| Depression | 15.5±15.8 | 10.3±15.1 | 3.33 | 0.0009 | 6.84 | 0.01 |
| Psychosis (delusions and/or hallucinations) | 3.4±11.6 | 1.1±5.1 | 2.77 | 0.006 | 0.92 | 0.32 |
Note: Data from the Longitudinal Interval Follow-up Evaluation (LIFE) Psychiatric Status Rating cores. MDD = major depressive disorder.
Analyses adjusting for between-group demographic and clinical differences.
BP youth with anxiety spent significantly less follow-up time asymptomatic and more follow-up time with syndromal and subsyndromal mixed/cycling and depressive symptomatology, and psychosis compared to BP youth without anxiety (all p-values ≤0.006). After adjusting for the above-noted significant confounding factors, anxious BP youth continued to show significantly less time asymptomatic, more syndromal mixed/cycling, and more subsyndromal depression when compared with non-anxious BP youth (all p-values ≤0.03).
Within the anxious BP youth, in comparison with youth with one anxiety disorder, those with ≥2 anxiety disorders showed significantly less follow-up time asymptomatic (33.2±25.2 vs. 42.7±27; F=8.28; p=0.004) and more follow-up time with syndromal mood symptomatology (21.8±20 vs. 15.1±17.8; F=7.71; p=0.006), syndromal depression (8.7±11.5 vs. 4.5±8.1; F=10.50; p=0.001), and subsyndromal mixed/cycling (19.4±20.3 vs. 13.2±15.7; F=7.25; p=0.008). Exploratory analyses examining the effects of specific anxiety disorders on the course of the mood symptomatology showed that in comparison with youth with other anxiety disorders, those with social anxiety disorder or PTSD spent less follow-up time asymptomatic and more time with syndromal depression. In addition, those with PTSD spent more follow-up time with syndromal and subsyndromal mixed/cycling and psychosis, those with OCD more time with hypomanic symptomatology, and those with panic disorder more time with syndromal depression (for all comparisons p-values≤0.04).
DISCUSSION
At intake and during the follow-up, 62% of youth with BP had at least one anxiety disorder and about 50% of the anxious youth had ≥ 2 anxiety disorders, particularly SAD and GAD. Survival analyses showed that compared to BP youth without anxiety disorders, those with anxiety had significantly more depression episode recurrences and significantly longer median time to recovery. After adjusting for significant confounding factors, the effects of anxiety on recovery were significant when the severity of the depression at intake was removed from the model. Week-by week mood symptom analyses showed that after adjusting for confounding factors, BP youth with anxiety, particularly those with ≥2 anxiety disorders, spent significantly less time asymptomatic, more time with syndromal mixed/cycling and subsyndromal depressive symptomatology compared to those without anxiety. Preliminary analyses indicated that youth with social anxiety disorder or PTSD and to lesser degree panic disorder had worse mood outcome than youth with other anxiety disorders.
Our findings are consistent with prior clinical 5, 27 and epidemiologic studies 28 in which anxiety disorders have been reported at high rates among youth with BP. Also, similar to the adult BP literature, we found that BP youth with anxiety had significantly longer time to recovery from the index episode and more mood recurrences, particularly depression episodes, among those who recovered. 9
Consistent with evidence from the adult BP literature,9, 11 we found that BP youth with anxiety have longer time to recovery than those without anxiety. However, as expected this effect was confounded by the presence of depressive symptomatology. The Collaborative Depression Study follow-up 29 also showed that recovery one year after intake was much more likely for those BP patients whose index episode was purely manic than for those whose index episode was depressed or cycling.
Present findings also converge with the adult BP literature in showing that comorbid anxiety is associated with less time asymptomatic, 8–10, 30 more time with syndromal mixed/cycling, 8, 31, 32 and more depressive symptomatology. 8, 10 In addition, we found that having ≥2 anxiety disorders have a worse course of BP illness compared to those with only one anxiety disorder8, 9 with social anxiety disorder and PTSD, and to a lesser degree panic disorder, having the most negative impact on outcome. 8 Furthermore, those with OCD had more time with hypomanic symptomatology. 33 Interestingly, Otto et al. 9 documented a negative impact of anxiety disorders on BP course, even when anxiety was assessed during periods of relative euthymia, suggesting that a worse course of BP in adults with anxiety comorbidity may reflect a unique biological subtype of BP. The above noted findings are similar to those found in the large depression literature noting the deleterious effects of concomitant anxiety disorders in unipolar depression. 34 In a prior COBY article using the same sample as the present study, we reported that anxiety disorders predated the onset of BP. 26 In addition, in a second paper we found that about 80% of the anxiety disorders persist and tend to be of the same type during the follow-up.12
The continuity between anxiety comorbidity and depressive morbidity raises two notable questions. The first is whether anxiety phenotypes in these subjects are truly independent factors that confer risk of subsequent depressive episodes, or a variable expression of a single propensity. In line with this possibility, while evidence is substantial that genetic factors impact individual differences in liability to anxiety and depression—generalized anxiety disorder in particular—the 2 phenotypes co-occur frequently in clinical and epidemiological samples, 35 due largely to a sharing of common genes, 36 whereas individual specific environmental effects may account for the primacy of anxiety in some individuals versus depression in others. 36 Second, lower socioeconomic status, less likelihood of living with both natural parents, and higher rate of abuse may have an important role to play as well. 37, 38 The association of traumatic events (e.g., history of physical and sexual abuse) with anxiety comorbidity in this cohort is consistent with a voluminous literature on the role of early life adversity in the programming of anxiety proneness and other symptoms of poor control of affective arousal via neurotoxic, inflammatory, and epigenetic mechanisms. 39 But whether or not these associations are robust in the context of bipolar versus non-bipolar affective disorder remain unresolved.
Despite the high rates of comorbid anxiety and its association with negative course and outcome of BP, there are no studies regarding the pharmacological or psychosocial management of anxiety disorders in youth with BP. This is very relevant because currently the main pharmacological treatment for anxiety disorders in youth is the SSRIs. 40–42 However, the use of antidepressants may worsen the symptoms of patients with BP 43 and the presence of anxiety may be a predictor of treatment emergent mania. 44 At this time, there are no controlled trials and very few open trials examining the efficacy of pharmacotherapy or psychotherapy aimed at managing anxiety disorders in BP illness, 45 with an open study of divalproex sodium 46 and an open study of group cognitive-behavioral therapy 47 suggesting possible benefit. Therefore, given the absence of compelling efficacy data to guide clinical practice for this population, it is not surprising that often they receive inadequate treatment. 48 Furthermore, given the differential effects of individual anxiety disorders on the course of BP in youth, it might be helpful to incorporate specific treatment protocols, including CBT, specifically targeted for these comorbid conditions.
The above-noted results need to be taken in the context of the limitations of this study. First, despite the efforts to obtain precise longitudinal information the data collected were subject to retrospective recall bias. 4, 49 Second, the effect of psychosocial treatments on the course of BP youth with anxiety disorders was not examined. Third, no psychiatric control group was included. Fourth, we only collected information on the rates of overall psychosocial treatments and not specific types of psychotherapy, such as cognitive behavior therapy. Finally, as most subjects were Caucasian and were recruited primarily from outpatient clinics, and to a lesser extent, from inpatient settings, the generalizability of the observations to other populations remains uncertain. Nevertheless, a community-based study of non-referred adolescents with BP reported similarly high rates of comorbid anxiety disorders. 3
In summary, anxiety disorders are common and adversely affect the course of BP in youth, as characterized by more mood recurrences, longer time to recovery, less time asymptomatic, more syndromal mixed/cycling, and more subsyndromal depression compared to those without anxiety. Prompt recognition and the development of psychosocial and pharmacological treatments for anxious youth with BP are warranted.
Clinical Guidance.
62% of youth with bipolar disorder (BP) met criteria for at least one anxiety disorder and about 50% of the anxious BP youth had ≥ 2 anxiety disorders.
Anxiety disorders are adversely affect the course of BP in youth, as characterized by less time euthymic, more time in mixed/cycling and depressive episodes compared to BP youth without anxiety.
Prompt recognition and the development of treatments for anxious BP youth are warranted.
Acknowledgments
Funding for this study was provided by the National Institute of Mental Health (NIMH) grants MH59929 (B.B.), MH59977 (M.A.S.), and MH59691 (M.B.K.). Dr. Sala received support from a grant from the Alicia Koplowitz Foundation.
Drs. Ha and Iyengar served as the statistical experts for this research.
Dr. Strober has received grant or research support from the National Institute of Mental Health (NIMH). Dr. Axelson has received grant or research support from NIMH. Dr. T.R. Goldstein has received grant or research support from NIMH, the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, and the Pittsburgh Foundation; and has received royalties from Guilford Press. Dr. B.I. Goldstein has received grant or research support from the Canadian Institute of Health Research, the Depressive and Bipolar Disorder Alternative Treatment Foundation, the Heart and Stroke Foundation of Ontario, NIMH, and the Ontario Mental Health Foundation; has served as a consultant to Bristol-Myers Squibb; and has received honoraria from Purdue Pharma. Dr. Iyengar has received grant or research support from NIMH. Dr. Yen has received grant or research support from NIMH. Dr. Hunt has received grant or research support from NIMH and honoraria from Wiley Publishing. Dr. Dickstein has received grant or research support from NIMH. Dr. Ryan has received grant or research support from NIMH and the National Center for Complementary and Alternative Medicine. Dr. Keller has served as a consultant to or has received honoraria from Medtronic and has received grant or research support from NIMH and Pfizer. Dr. Birmaher has received grant or research support from NIMH and has received or will receive royalties from UpToDate, Random House, and Lippincott Williams and Wilkins. Drs. Sala, Castro-Fornieles, and Ha, and Ms. Gill, Ms. Liao, and Ms.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Preliminary findings were presented in poster form at the 58th Annual Meeting of the American Academy of Child and Adolescent Psychiatry, October 2011, Toronto, Canada.
Disclosure: Drs. Sala, Castro-Fornieles, and Ha, and Ms. Gill, Ms. Liao, and Ms. Hower report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Regina Sala, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine. Institute of Psychiatry, King's College London.
Michael A Strober, David Geffen School of Medicine, University of California at Los Angeles.
David A. Axelson, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
Mary Kay Gill, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
Josefina Castro-Fornieles, IDIBAPS, CIBERSAM, Neurosciences Institute, Hospital Clinic de Barcelona, Universitat de Barcelona.
Tina R. Goldstein, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
Benjamin I. Goldstein, Sunnybrook Health Sciences Centre, University of Toronto.
Wonho Ha, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
Fangzi Liao, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
Satish Iyengar, University of Pittsburgh.
Shirley Yen, Butler Hospital, Brown University School of Medicine.
Heather Hower, Butler Hospital, Brown University School of Medicine.
Jeffrey Hunt, Butler Hospital, Brown University School of Medicine.
Daniel P. Dickstein, Butler Hospital, Brown University School of Medicine.
Neal D. Ryan, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
Martin B. Keller, Butler Hospital, Brown University School of Medicine.
Boris Birmaher, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine.
References
- 1.Kraepelin E. Lectures on clinical psychiatry. Dr. Emil Kraepelin: Wood; 1917. [Google Scholar]
- 2.Sala R, Axelson DA, Castro-Fornieles J, et al. Comorbid anxiety in children and adolescents with bipolar spectrum disorders: prevalence and clinical correlates. J Clin Psychiatry. 2010 Oct;71(10):1344–1350. doi: 10.4088/JCP.09m05845gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord. 2000 Sep;2(3 Pt 2):281–293. doi: 10.1034/j.1399-5618.2000.20309.x. [DOI] [PubMed] [Google Scholar]
- 4.DelBello MP, Hanseman D, Adler CM, Fleck DE, Strakowski SM. Twelve-month outcome of adolescents with bipolar disorder following first hospitalization for a manic or mixed episode. Am J Psychiatry. 2007 Apr;164(4):582–590. doi: 10.1176/ajp.2007.164.4.582. [DOI] [PubMed] [Google Scholar]
- 5.Dickstein DP, Rich BA, Binstock AB, et al. Comorbid anxiety in phenotypes of pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2005 Aug;15(4):534–548. doi: 10.1089/cap.2005.15.534. [DOI] [PubMed] [Google Scholar]
- 6.Joshi G, Wilens T. Comorbidity in pediatric bipolar disorder. Child Adolesc Psychiatr Clin N Am. 2009 Apr;18(2):291–319. doi: 10.1016/j.chc.2008.12.005. vii–viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Masi G, Perugi G, Millepiedi S, et al. Clinical and research implications of panic-bipolar comorbidity in children and adolescents. Psychiatry Res. 2007 Sep 30;153(1):47–54. doi: 10.1016/j.psychres.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Boylan KR, Bieling PJ, Marriott M, Begin H, Young LT, MacQueen GM. Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J Clin Psychiatry. 2004 Aug;65(8):1106–1113. doi: 10.4088/jcp.v65n0813. [DOI] [PubMed] [Google Scholar]
- 9.Otto MW, Simon NM, Wisniewski SR, et al. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry. 2006 Jul;189:20–25. doi: 10.1192/bjp.bp.104.007773. [DOI] [PubMed] [Google Scholar]
- 10.Gaudiano BA, Miller IW. Anxiety disorder comobidity in Bipolar I Disorder: relationship to depression severity and treatment outcome. Depress Anxiety. 2005;21(2):71–77. doi: 10.1002/da.20053. [DOI] [PubMed] [Google Scholar]
- 11.Coryell W, Solomon DA, Fiedorowicz JG, Endicott J, Schettler PJ, Judd LL. Anxiety and outcome in bipolar disorder. Am J Psychiatry. 2009 Nov;166(11):1238–1243. doi: 10.1176/appi.ajp.2009.09020218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sala R, Axelson DA, Castro-Fornieles J, et al. Factors associated with the persistence and onset of new anxiety disorders in youth with bipolar spectrum disorders. J Clin Psychiatry. 2012 Jan;73(1):87–94. doi: 10.4088/JCP.10m06720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunt J, Birmaher B, Leonard H, et al. Irritability without elation in a large bipolar youth sample: frequency and clinical description. J Am Acad Child Adolesc Psychiatry. 2009 Jul;48(7):730–739. doi: 10.1097/CHI.0b013e3181a565db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Axelson DA, Birmaher B, Strober MA, et al. Course of subthreshold bipolar disorder in youth: diagnostic progression from bipolar disorder not otherwise specified. J Am Acad Child Adolesc Psychiatry. 2011 Oct;50(10):1001–1016. e1003. doi: 10.1016/j.jaac.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birmaher B, Axelson D, Goldstein B, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry. 2009 Jul;166(7):795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997 Jul;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 17.Axelson D, Birmaher BJ, Brent D, et al. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. J Child Adolesc Psychopharmacol. 2003 Winter;13(4):463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- 18.First MB, Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-IV (SCID) Washington, DC: American Psychiatric Association; 1995. [Google Scholar]
- 19.Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry. 2000 Jul;57(7):675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- 20.Hollingshead AB. Four-Factor Index of Social Status. New Haven, Conn: Sociology Dept, Yale University; 1975. [Google Scholar]
- 21.Shaffer D, Gould MS, Brasic J, et al. A children's global assessment scale (CGAS) Arch Gen Psychiatry. 1983 Nov;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 22.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999 Oct;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Petersen A, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity, and initial norms. J Youth Adolesc. 1988;17:117–133. doi: 10.1007/BF01537962. 1988. [DOI] [PubMed] [Google Scholar]
- 24.Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: an ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. J Psychiatr Res. 2001 Sep-Oct;35(5):297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- 25.Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002 Jun;59(6):530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 26.Sala R, Axelson DA, Castro-Fornieles J, et al. Comorbid anxiety in children and adolescents with bipolar spectrum disorders: prevalence and clinical correlates. J Clin Psychiatry. 2010 Oct;71(10):1344–1350. doi: 10.4088/JCP.09m05845gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vitiello B, Riddle MA, Yenokyan G, et al. Treatment moderators and predictors of outcome in the Treatment of Early Age Mania (TEAM) study. J Am Acad Child Adolesc Psychiatry. 2012 Sep;51(9):867–878. doi: 10.1016/j.jaac.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry. 1995 Apr;34(4):454–463. [PubMed] [Google Scholar]
- 29.Keller MB, Lavori PW, Klerman GL, et al. Low levels and lack of predictors of somatotherapy and psychotherapy received by depressed patients. Arch Gen Psychiatry. 1986 May;43(5):458–466. doi: 10.1001/archpsyc.1986.01800050064007. [DOI] [PubMed] [Google Scholar]
- 30.Simon NM, Otto MW, Wisniewski SR, et al. Anxiety disorder comorbidity in bipolar disorder patients: data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Am J Psychiatry. 2004 Dec;161(12):2222–2229. doi: 10.1176/appi.ajp.161.12.2222. [DOI] [PubMed] [Google Scholar]
- 31.Vieta E, Colom F, Corbella B, et al. Clinical correlates of psychiatric comorbidity in bipolar I patients. Bipolar Disord. 2001 Oct;3(5):253–258. [PubMed] [Google Scholar]
- 32.Kauer-Sant'Anna M, Frey BN, Andreazza AC, et al. Anxiety comorbidity and quality of life in bipolar disorder patients. Can J Psychiatry. 2007 Mar;52(3):175–181. doi: 10.1177/070674370705200309. [DOI] [PubMed] [Google Scholar]
- 33.Perugi G, Akiskal HS, Toni C, Simonini E, Gemignani A. The temporal relationship between anxiety disorders and (hypo)mania: a retrospective examination of 63 panic, social phobic and obsessive-compulsive patients with comorbid bipolar disorder. J Affect Disord. 2001 Dec;67(1–3):199–206. doi: 10.1016/s0165-0327(01)00433-5. [DOI] [PubMed] [Google Scholar]
- 34.Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Arch Gen Psychiatry. 2003 Oct;60(10):993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 35.Gorwood P. Generalized anxiety disorder and major depressive disorder comorbidity: an example of genetic pleiotropy? Eur Psychiatry. 2004 Feb;19(1):27–33. doi: 10.1016/j.eurpsy.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychol Med. 2007 Mar;37(3):453–462. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- 37.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009 Sep;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wittchen HU, Nelson CB, Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med. 1998 Jan;28(1):109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- 39.Bohacek J, Mansuy IM. Epigenetic inheritance of disease and disease risk. Neuropsychopharmacology. 2013 Jan;38(1):220–236. doi: 10.1038/npp.2012.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Birmaher B, Axelson DA, Monk K, et al. Fluoxetine for the treatment of childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2003 Apr;42(4):415–423. doi: 10.1097/01.CHI.0000037049.04952.9F. [DOI] [PubMed] [Google Scholar]
- 41.Allgulander C, Dahl AA, Austin C, et al. Efficacy of sertraline in a 12-week trial for generalized anxiety disorder. Am J Psychiatry. 2004 Sep;161(9):1642–1649. doi: 10.1176/appi.ajp.161.9.1642. [DOI] [PubMed] [Google Scholar]
- 42.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008 Dec 25;359(26):2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ghaemi SN, Hsu DJ, Soldani F, Goodwin FK. Antidepressants in bipolar disorder: the case for caution. Bipolar Disord. 2003 Dec;5(6):421–433. doi: 10.1046/j.1399-5618.2003.00074.x. [DOI] [PubMed] [Google Scholar]
- 44.Goldsmith M, Singh M, Chang K. Antidepressants and psychostimulants in pediatric populations: is there an association with mania? Paediatr Drugs. 2011 Aug 1;13(4):225–243. doi: 10.2165/11591660-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kauer-Sant'Anna M, Kapczinski F, Vieta E. Epidemiology and management of anxiety in patients with bipolar disorder. CNS Drugs. 2009 Nov 1;23(11):953–964. doi: 10.2165/11310850-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 46.Baetz M, Bowen RC. Efficacy of divalproex sodium in patients with panic disorder and mood instability who have not responded to conventional therapy. Can J Psychiatry. 1998 Feb;43(1):73–77. doi: 10.1177/070674379804300109. [DOI] [PubMed] [Google Scholar]
- 47.Bowen RC, D'Arcy C. Response of patients with panic disorder and symptoms of hypomania to cognitive behavior therapy for panic. Bipolar Disord. 2003 Apr;5(2):144–149. doi: 10.1034/j.1399-5618.2003.00023.x. [DOI] [PubMed] [Google Scholar]
- 48.Simon NM, Otto MW, Weiss RD, et al. Pharmacotherapy for bipolar disorder and comorbid conditions: baseline data from STEP-BD. J Clin Psychopharmacol. 2004 Oct;24(5):512–520. doi: 10.1097/01.jcp.0000138772.40515.70. [DOI] [PubMed] [Google Scholar]
- 49.Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006 Feb;63(2):175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]