Abstract
The Doppler-derived renal resistive index has been used for years in a variety of clinical settings such as the assessment of chronic renal allograft rejection, detection and management of renal artery stenosis, evaluation of progression risk in chronic kidney disease, differential diagnosis in acute and chronic obstructive renal disease, and more recently as a predictor of renal and global outcome in the critically ill patient. More recently, evidence has been accumulating showing that an increased renal resistive index not only reflects changes in intrarenal perfusion but is also related to systemic hemodynamics and the presence of subclinical atherosclerosis, and may thus provide useful prognostic information in patients with primary hypertension. On the basis of these results, the evaluation of renal resistive index has been proposed in the assessment and management of patients with primary hypertension to complement other signs of renal abnormalities.
Keywords: cardiovascular risk, hypertension, renal resistive index
INTRODUCTION
Detection of target organ damage plays a key role in the evaluation of overall risk, and therefore in the management of patients with primary hypertension. Looking for renal abnormalities such as increased albuminuria or mild reduction in glomerular filtration rate (GFR) has been proposed with growing emphasis as the initial step in the evaluation of cardiovascular risk, also thanks to its relatively low cost and feasibility [1].
Ultrasound and Doppler imaging has also traditionally been used in the assessment of chronic renal disease. Not only does Doppler ultrasonography detect renal macroscopic vascular abnormalities but it also identifies changes in blood flow at the microvascular level. Evaluation of vascular impedance at different sites of the renal parenchyma may suggest functional or structural changes within the kidneys and could provide useful diagnostic and prognostic information.
Although the functional and structural factors that contribute to renal blood flow patterns and changes are still not completely understood, intraparenchymal arterial waveform is believed to be the result of both vascular compliance and resistance. Doppler-derived indexes may thus reflect one or more pathogenetic mechanisms such as arteriolosclerosis and interstitial fibrosis, which contribute to determining vascular distensibility [2].
Indeed, the Doppler-derived renal resistive index (RRI) has been used for years in a variety of clinical settings such as the assessment of chronic renal allograft rejection [3], detection and management of renal artery stenosis [4,5], evaluation of progression risk in chronic kidney disease (CKD) [6], differential diagnosis in acute and chronic obstructive renal disease, and more recently as a predictor of renal and overall outcome in the critically ill patient [7,8].
Recent clinical and experimental evidence indicates that an increased RRI in patients with primary hypertension not only reflects changes in intrarenal perfusion, but that it is also associated with systemic hemodynamics and atherosclerosis, and may provide useful prognostic information and possibly have therapeutic implications [9,10].
This article will briefly review the main clinical applications of RRI and will discuss more recent data on its meaning and prognostic usefulness in the management of patients with hypertension.
TECHNIQUE AND THEORY
The need for meticulous, standardized techniques to obtain Doppler signals has been repeatedly emphasized [2]. A high frequency probe is recommended together with the use of color or power Doppler to help vessel localization. As resistance to blood flow progressively increases from the hilar arteries toward the more peripheral parenchymal vessels, it is generally recommended that sampling for RRI should be done at the level of the arcuate or interlobar arteries, adjacent to medullary pyramids (Fig. 1). Measurements should preferentially be repeated in different parts of both organs (superior, median, and lower) when at least three reproducible waveforms have been obtained. An RRI is calculated with the following formula: (peak systolic velocity – end diastolic velocity)/peak systolic velocity, and the mean value of three measurements at each kidney is usually considered. An RRI value 0.60 ± 0.01 (mean ± SD) is usually taken as normal with a value of 0.70 being considered the upper normal threshold by most authors [2]. In order to maximize waveform size, care should be taken in using the lowest pulse repetition frequency without aliasing, the highest possible gain without noise and the lowest wall filter.
FIGURE 1.
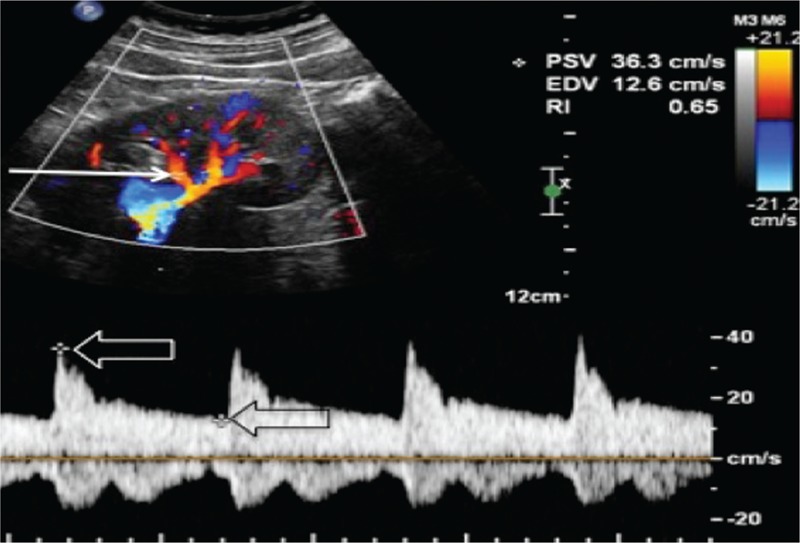
Renal RI measurement technique. A sample volume (arrow) is placed within an intrarenal artery (an arcuate or interlobar one) under Color Doppler guidance and spectral analysis of vascular signals is obtained. The measurement calipers are then set at the systolic peak (white open arrow) and end diastole (black open arrow) of a waveform, and the RI is calculated according to the formula (PSV-EDV)/PSV. EDV, end diastolic velocity; RI, resistive index; SV, peak systolic velocity.
There is a general agreement that 0.70 should be considered the upper limit of normality in adults, but not in children in whom RRIs typically show higher values, especially within the first year of life [11]. Furthermore, RRI has been reported to increase in the healthy elderly population, possibly because of age-related changes in vascular compliance [12].
An increased RRI has often been regarded solely as an indicator of renal vascular resistance, although other factors such as vascular compliance, systemic pulse pressure, and heart rate and rhythm have more recently been shown to influence it. In fact, RRI may be an unreliable indicator, and good quality waveforms could be difficult to obtain in the presence of cardiac arrhythmias such as atrial fibrillation [2]. Thus, various pathologic changes, such as tissue interstitial fibrosis and vascular stiffening, might substantially affect the RRI. Although the complex and rather aspecific nature of the involved mechanisms may account for the disappointing results obtained in differentiating specific renal diseases, it may also explain more recent encouraging studies exploring its usefulness in the assessment of cardiorenal risk.
DOPPLER-DERIVED RENAL RESISTIVE INDEX IN THE MANAGEMENT OF RENOVASCULAR HYPERTENSION
A complete ultrasound Doppler evaluation of the entire renal vasculature, which includes end-diastolic velocity, peak systolic velocity (PSV) from both proximal renal arteries, as well as the ratio between renal and aortic PSV, is a rather cost-efficient diagnostic tool in the diagnosis of renal artery disease [13], and remains a routine clinical approach to this disease in many centers worldwide. However, this may be impossible to obtain in all patients because of the difficulties in identification of the entire course of both renal arteries. Indirect criteria for renal artery stenosis, such as assessment of arterial waveforms at the renal hilum can be also employed, with known lower sensitivity. Although the sole evaluation of RRI is not considered a reliable tool in the screening for renal artery stenosis as compared to other imaging techniques such as magnetic resonance angiography, contrast-enhanced computed tomography (CT), or radioisotopic renal scan, the finding of a tardus-parvus waveform at the level of the interlobar arteries is almost pathognomonic of the condition and should prompt accurate color and duplex Doppler evaluation of the main renal artery to establish the diagnosis. Furthermore, the assessment of RRI may provide valuable prognostic insights into the management of this condition. Following the seminal work of Radermacher et al. [4], in 2001, which reported a series of 138 patients with unilateral or bilateral renal artery who underwent surgery or angioplasty, an RRI more than 0.80 has been considered a negative prognostic sign and a contraindication to surgery. On the contrary, lower resistance-index values are associated with an improvement in blood pressure, renal function, and kidney survival after the correction of renal-artery stenosis. A number of subsequent studies [14,15] later confirmed that increased RRI values indicate the presence of diffuse microvascular atherosclerotic abnormalities. This condition, often referred to as ‘small vessel disease’, is unlikely to benefit from changes in large vessel hemodynamics brought about by renal revascularization.
DOPPLER-DERIVED RENAL RESISTIVE INDEX IN PRIMARY HYPERTENSION
Early reports by our group [16], later confirmed by others [17], have shown that in untreated patients with primary hypertension and normal renal function an increase in RRI is associated with subclinical signs of renal organ damage (Fig. 2). An RRI shows a direct relationship with the amount of urine albumin excretion, thus the presence of microalbuminuria signals an increased likelihood of RRI above 0.7. An RRI is also reportedly inversely related to renal volume index. The relationship between RRI and renal function in primary hypertension was subsequently investigated in greater detail in a larger cohort of patients, and it was shown that increased impedance to blood flow at the parenchymal level is often associated with a mild reduction in GFR, increased albuminuria, or both [18].
FIGURE 2.
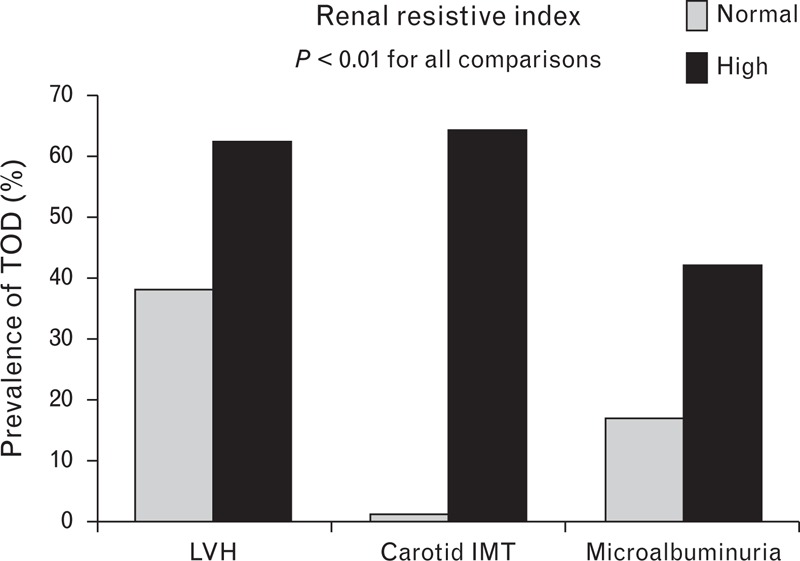
Renal resistive index and target organ damage in primary hypertension. IMT, intima–media thickness; LVH, left ventricular hypertrophy; PH, primary hypertension; TOD, indicates target organ damage [16,18].
Furthermore, increased RRI signals the presence of hypertensive and atherosclerotic organ damage such as left ventricular hypertrophy and carotid intima–media thickening (Fig. 2), and may therefore be taken as an indicator of an increased cardiovascular risk profile [19]. A relationship was found between aortic vascular stiffness, which was indirectly assessed by the ambulatory blood pressure measurements-derived ambulatory arterial stiffness index and the RRI. This intriguing finding may suggest that in the context of primary hypertension, changes in kidney impedance parallel those observed at the systemic level and thus, the increased RRI may be considered a marker of atherosclerotic vessel damage [19]. In a cohort of 870 elderly Americans from the Cardiovascular Health Study, Pearce et al.[10] examined associations between renal parenchyma Doppler-derived parameters and cardiovascular morbidity and mortality over a median follow-up of 7 years. These authors reported that Doppler signals indicating increased intrarenal stiffness and impedance to blood flow were significantly associated with subsequent cardiovascular events after checking for several confounders, such as renal function, hypertension, diabetes, and history of coronary artery or cerebrovascular events.
The role of RRI as a marker of subclinical renal damage and its relationship with abnormalities in central and renal hemodynamics has been further elucidated by the work of Hashimoto and Ito [9], who studied several measures of central and peripheral vascular stiffness in 136 patients with primary hypertension. They found that microalbuminuria is associated with increased RRIs and that these, in turn, depend on increased central pulse pressure and aortic stiffness as well as abnormal renal hemodynamics – namely increased peripheral resistance and/or increased flow pulsation. In keeping with this hypothesis and the multifactorial nature of this parameter, RRI has been shown to be influenced by age and pulse pressure [20], and has been associated with greater systemic 24-h blood pressure load and abnormal circadian patterns (i.e. nondipping) as well as with increased sympathetic activity and uric acid values.
In a recently published study, Doi et al. [21] investigated the prognostic role of RRI over a mean follow-up of 3.1 years in a group of 426 patients with primary hypertension and no previous cardiovascular disease. RRI proved to be an independent predictor of worse cardiovascular and renal outcomes, especially when combined with reduced GFR, thus providing a useful diagnostic complement to the assessment of renal function in these patients (Fig. 3).
FIGURE 3.
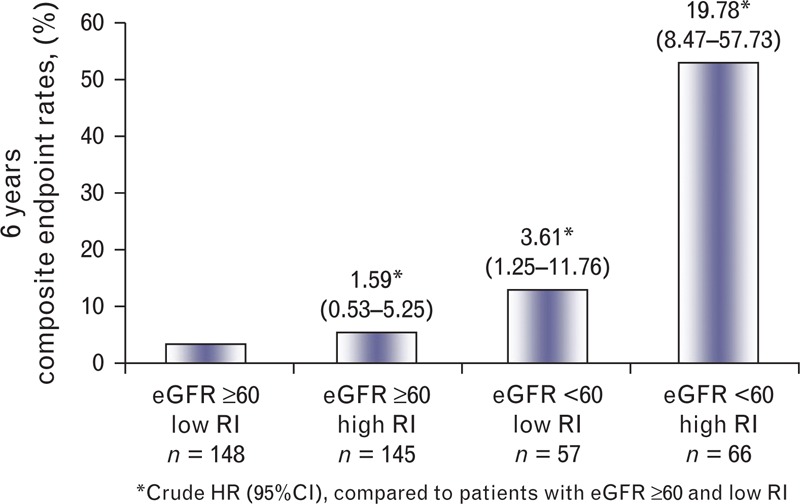
Renal resistive index and cardiovascular and renal outcomes in primary hypertension. Low and high resistive index were defined on the basis of sex-specific median values of RI (i.e. 0.62 for men and 0.67 for women in the group with GFR ≥60 ml/min; 0.73 for men and 0.72 for women in the group with GFR <60 ml/min). CIs, confidence intervals; HRs, indicates hazard ratios; GFR, estimated glomerular filtration rate; RI, resistive index [21].
Furthermore, an increased RRI has been demonstrated to predict the onset of diabetes mellitus in patients with primary hypertension, a finding which may stimulate further research into the recently developed hypothesis concerning a pathogenetic link between early signs of renal abnormalities and an unfavorable cardiovascular outcome [22].
Lastly, evaluating RRI may have therapeutic implications. Preliminary studies suggest that changes in RRI may parallel variations in urine albumin excretion under chronic antihypertensive treatment [23], although long-term studies are needed to assess the usefulness and clinical meaning of these findings. Furthermore, an increase in RRI may signal the presence of intrarenal stiffness and suggests caution in titrating renin–angiotensin–aldosterone system inhibitors, especially when added to diuretics, pending the risk of renal function worsening.
DOPPLER-DERIVED RENAL RESISTIVE INDEX IN CHRONIC RENAL DISEASE
Several studies on a variety of chronic renal diseases in native as well as in transplanted kidneys have reported the prognostic, independent value of an increased RRI. In a group of 137 patients with proteinuric chronic renal disease, Radermacher et al.[6] reported that RRI more than 0.80 was associated with faster decline of renal function over a 5-year median follow-up period, even after adjusting for several known risk factors including baseline GFR values and the degree of proteinuria. Using the very same cutoff value in a group of patients with type 2 diabetes and microalbuminuria, Nosadini et al.[24] described an unfavorable renal prognostic value of increased RRI even when GFR is still within normal values. More recently, Hamano et al.[25] reported that RRI was related to the severity of renal damage in diabetic patients, as it progressively increases in parallel with the amount of urine excretion. Furthermore, an increase in RRI was also associated with lower DBP and signs of vascular stiffness as evaluated by the ankle-brachial index. Other studies have confirmed a more rapid decline in renal function over time in the presence of increased RRI in CKD [26], and some have suggested that this abnormality may entail worse response to steroid treatment [27].
Recently, pathophysiological mechanisms underlying the association of increased RRIs and renal function have been further clarified by reports of pathological correlations with the severity and extension of tissue changes such as tubulointerstitial fibrosis and arteriosclerosis in CKD patients [28]. Many, although not all studies have reported that RRI is a predictor of future function worsening in transplanted kidneys [29–31]. Although RRI analysis is not considered useful for identifying specific causes of transplant dysfunction, it may generally indicate vascular complications and the need for further investigation.
Apart from its renal prognostic role, high RRIs (i.e., >0.80) have been reported to be predictive of all-cause mortality in CKD patients [6].
USE OF DOPPLER-DERIVED RENAL RESISTIVE INDEX IN OTHER RENAL CONDITIONS
There is a growing interest in the RRI and its broader application in various clinical areas and pathologic conditions, and recent studies have addressed its usefulness as a predictor of renal and global outcome in critically ill patients. Indeed, experimental work has suggested that cortical blood flow redistribution and an increase in renal vascular resistance may be early sensitive signs of an impending hemodynamic deterioration, even in apparently stable patients. Thus, RRI measurement may be usefully utilized in the management of various clinical conditions such as hemorrhagic, septic, or posttraumatic shock [32]. However, numerous confounding factors, including nonhemodynamic ones, have been shown to influence renal Doppler parameters in the acute setting, and the value of RRI in predicting both global outcome and the development of acute kidney injury in critically ill patients currently remains uncertain [33].
Given the well known diagnostic limitations of ultrasound scan in obstructive renal disease, great interest was initially placed on the possibility to gain more reliable insights into the presence of urinary obstruction by analyzing the intraparenchymal spectra. After initial enthusiasm in the early 1990s, several clinical trials [34] considerably reduced the expectations regarding the usefulness of Doppler-derived indices in this area as results showed that most patients with partial obstruction had normal RRIs [35]. These findings, together with the progressive acceptance of unenhanced CT as the gold standard for identifying ureteral calculi [36], have led to a decrease in interest over the usefulness of this parameter, except perhaps with regard to specific clinical conditions, such as the evaluation of the pregnant patient. More recently, several studies have addressed the potential clinical use of contrast-enhanced ultrasound in different vascular fields, although specific application for this method remains a matter of debate.
CONCLUSION
Despite its relatively low specificity in terms of clinical-pathological correlation and the still poorly understood pathogenesis, RRI has been fruitfully used to gain diagnostic and prognostic insights into a variety of clinical conditions from renal vascular disease to CKD and renal transplant.
In patients with renal artery stenosis, an RRI more than 0.80 has been shown to be a reliable indicator of poor therapeutic response to revascularization treatment and has gained considerable popularity in the clinical management of these patients.
In the presence of diabetic and nondiabetic CKD and in renal transplant, increased RRI has been shown to correlate with the severity of vascular and interstitial damage, and therefore is taken as a powerful predictor of disease progression.
More recently, an increased RRI has been shown to be a marker of renal and extrarenal organ damage in primary hypertension. Several studies indicate that this abnormality may in part reflect systemic vascular stiffness and entail a worse cardiovascular prognosis. On the basis of these results, the evaluation of RRI should be used to complement other signs of renal abnormalities in the assessment and management of patients with primary hypertension.
Finally, indirect preliminary evidence suggests that the evaluation of RRI may also carry therapeutic implications as far as the type of drug and, possibly, target blood pressure are concerned in order to optimize renal protection in the subgroups at greater risk such as the elderly and those with diabetes and CKD. This is an area that certainly deserves further investigation given the growing epidemiological weight of hypertensive renal disease in the cardiovascular arena.
ACKNOWLEDGEMENTS
This work was supported by grants from the Italian Ministero della Salute (Bando Giovane Ricercatore 2008, CUP G35J11000130001).
Conflicts of interest
There are no conflicts of interest.
Reviewers’ Summary Evaluations
Reviewer 1
Strengths: Increased renal resistive index (RRI) is a marker of atherosclerotic and hypertensive organ damage both at the renal and systemic level. It is a predictor of cardiovascular and renal outcome. Finally, measurements of RRI may have therapeutic implications in the management of hypertensive patients in particular.
Reviewer 2
The authors provide a comprehensive review of the studies relating renal resistive index to cardiovascular risk and outcomes. The review is inclusive of a large body of work in this area. The discussion is insightful and will be of value to researchers interested in vascular assessment and cardiovascular disease prediction.
Footnotes
Correspondence to Roberto Pontremoli, Universita‘ degli Studi e I.R.C.C.S. Azienda Ospedaliera Universitaria San Martino-IST, Istituto Nazionale per la Ricerca sul Cancro Viale Benedetto XV 6–16132 Genoa, Italy. Tel: +39 347 302 2987; fax: +39 010 8561237; e-mail: roberto.pontremoli@unige.it
Abbreviations: CKD, chronic kidney disease; GFR, glomerular filtration rate; RRI, Doppler-derived renal resistive index
REFERENCES
- 1.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. ESH-ESC Task Force on the Management of Arterial Hypertension 2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens 2007; 25:1751–1762Erratum in: J Hypertens 2007; 25:2184 [DOI] [PubMed] [Google Scholar]
- 2.Tublin ME, Bude RO, Platt JF. The resistive index in renal Doppler sonography: where do we stand? AJR Am J Roentgenol 2003; 180:885–892 [DOI] [PubMed] [Google Scholar]
- 3.Radermacher J, Mengel M, Ellis S, Stuht S, Hiss M, Schwarz A, et al. The renal arterial resistance index and renal allograft survival. N Engl J Med 2003; 349:115–124 [DOI] [PubMed] [Google Scholar]
- 4.Radermacher J, Chavan A, Bleck J, Vitzthum A, Stoess B, Gebel MJ, et al. Use of Doppler ultrasonography to predict the outcome of therapy for renal-artery stenosis. N Engl J Med 2001; 344:410–417 [DOI] [PubMed] [Google Scholar]
- 5.Crutchley TA, Pearce JD, Craven TE, Stafford JM, Edwards MS, Hansen KJ. Clinical utility of the resistive index in atherosclerotic renovascular disease. J Vasc Surg 2009; 49:148–155 [DOI] [PubMed] [Google Scholar]
- 6.Radermacher J, Ellis S, Haller H. Renal resistance index and progression of renal disease. Hypertension 2002; 39:699–703 [DOI] [PubMed] [Google Scholar]
- 7.Le Dorze M, Bouglé A, Deruddre S, Duranteau J. Renal Doppler ultrasound: a new tool to assess renal perfusion in critical illness. Shock 2012; 37:360–365 [DOI] [PubMed] [Google Scholar]
- 8.Darmon M, Schortgen F, Vargas F, Liazydi A, Schlemmer B, Brun-Buisson C, et al. Diagnostic accuracy of Doppler renal resistive index for reversibility of acute kidney injury in critically ill patients. Intensive Care Med 2011; 37:68–76 [DOI] [PubMed] [Google Scholar]
- 9.Hashimoto J, Ito S. Central pulse pressure and aortic stiffness determine renal hemodynamics: pathophysiological implication for microalbuminuria in hypertension. Hypertension 2011; 58:839–846 [DOI] [PubMed] [Google Scholar]
- 10.Pearce JD, Craven TE, Edwards MS, Corriere MA, Crutchley TA, Fleming SH, et al. Associations between renal duplex parameters and adverse cardiovascular events in the elderly: a prospective cohort study. Am J Kidney Dis 2010; 55:281–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bude RO, DiPietro MA, Platt JF, Rubin JM, Miesowicz S, Lundquist C. Age dependency of the renal resistive index in healthy children. Radiology 1992; 184:469–473 [DOI] [PubMed] [Google Scholar]
- 12.Kaiser C, Götzberger M, Landauer N, Dieterle C, Heldwein W, Schiemann U. Age dependency of intrarenal resistance index (RI) in healthy adults and patients with fatty liver disease. Eur J Med Res 2007; 12:191–195 [PubMed] [Google Scholar]
- 13.Bolduc JP, Oliva VL, Therasse E, Giroux MF, Bouchard L, Perreault P, et al. Diagnosis and treatment of renovascular hypertension: a cost-benefit analysis. AJR Am J Roentgenol 2005; 184:931–937 [DOI] [PubMed] [Google Scholar]
- 14.Soulez G, Therasse E, Qanadli SD, Froment D, Léveillé M, Nicolet V, et al. Prediction of clinical response after renal angioplasty: respective value of renal Doppler sonography and scintigraphy. AJR Am J Roentgenol 2003; 181:1029–1035 [DOI] [PubMed] [Google Scholar]
- 15.Davies MG, Saad WE, Bismuth J, Naoum JJ, Peden EK, Lumsden AB. Renal parenchymal preservation after percutaneous renal angioplasty and stenting. J Vasc Surg 2010; 51:1222–1229 [DOI] [PubMed] [Google Scholar]
- 16.Pontremoli R, Viazzi F, Martinoli C, Ravera M, Nicolella C, Berruti V, et al. Increased renal resistive index in patients with essential hypertension: a marker of organ damage. Nephrol Dial Transplant 1999; 14:360–365 [DOI] [PubMed] [Google Scholar]
- 17.Doi Y, Iwashima Y, Yoshihara F, Kamide K, Takata H, Fujii T, et al. Association of renal resistive index with target organ damage in essential hypertension. Am J Hypertens 2012; 25:1292–1298 [DOI] [PubMed] [Google Scholar]
- 18.Derchi LE, Leoncini G, Parodi D, Viazzi F, Martinoli C, Ratto E, et al. Mild renal dysfunction and renal vascular resistance in primary hypertension. Am J Hypertens 2005; 18:966–971 [DOI] [PubMed] [Google Scholar]
- 19.Ratto E, Leoncini G, Viazzi F, Vaccaro V, Falqui V, Parodi A, et al. Ambulatory arterial stiffness index and renal abnormalities in primary hypertension. J Hypertens 2006; 24:2033–2038 [DOI] [PubMed] [Google Scholar]
- 20.Afsar B, Ozdemir NF, Elsurer R, Sezer S. Renal resistive index and nocturnal nondipping: is there an association in essential hypertension? Int Urol Nephrol 2009; 41:383–391 [DOI] [PubMed] [Google Scholar]
- 21.Doi Y, Iwashima Y, Yoshihara F, Kamide K, Hayashi S, Kubota Y, et al. Renal resistive index and cardiovascular and renal outcomes in essential hypertension. Hypertension 2012; 60:770–777 [DOI] [PubMed] [Google Scholar]
- 22.Viazzi F, Leoncini G, Derchi LE, Baratto E, Storace G, Vercelli M, et al. Subclinical functional and structural renal abnormalities predict new onset type 2 diabetes in patients with primary hypertension. J Hum Hypertens 2013; 27:95–99 [DOI] [PubMed] [Google Scholar]
- 23.Leoncini G, Martinoli C, Viazzi F, Ravera M, Parodi D, Ratto E, et al. Changes in renal resistive index and urinary albumin excretion in hypertensive patients under long-term treatment with lisinopril or nifedipine GITS. Nephron 2002; 90:169–173 [DOI] [PubMed] [Google Scholar]
- 24.Nosadini R, Velussi M, Brocco E, Abaterusso C, Carraro A, Piarulli F, et al. Increased renal arterial resistance predicts the course of renal function in type 2 diabetes with microalbuminuria. Diabetes 2006; 55:234–239 [PubMed] [Google Scholar]
- 25.Hamano K, Nitta A, Ohtake T, Kobayashi S. Associations of renal vascular resistance with albuminuria and other macroangiopathy in type 2 diabetic patients. Diabetes Care 2008; 31:1853–1857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parolini C, Noce A, Staffolani E, Giarrizzo GF, Costanzi S, Splendiani G. Renal resistive index and long-term outcome in chronic nephropathies. Radiology 2009; 252:888–896 [DOI] [PubMed] [Google Scholar]
- 27.Hanamura K, Tojo A, Kinugasa S, Asaba K, Fujita T. The resistive index is a marker of renal function, pathology, prognosis, and responsiveness to steroid therapy in chronic kidney disease patients. Int J Nephrol 2012; 2012:139565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bigé N, Lévy PP, Callard P, Faintuch JM, Chigot V, Jousselin V, et al. Renal arterial resistive index is associated with severe histological changes and poor renal outcome during chronic kidney disease. BMC Nephrol 2012; 13:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Winther SO, Thiesson HC, Poulsen LN, Chehri M, Agerskov H, Tepel M. The renal arterial resistive index and stage of chronic kidney disease in patients with renal allograft. PLoS One 2012; 7:e51772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McArthur C, Geddes CC, Baxter GM. Early measurement of pulsatility and resistive indexes: correlation with long-term renal transplant function. Radiology 2011; 259:278–285 [DOI] [PubMed] [Google Scholar]
- 31.Saracino A, Santarsia G, Latorraca A, Gaudiano V. Early assessment of renal resistance index after kidney transplant can help predict long-term renal function. Nephrol Dial Transplant 2006; 21:2916–2920 [DOI] [PubMed] [Google Scholar]
- 32.Corradi F, Brusasco C, Vezzani A, Palermo S, Altomonte F, Moscatelli P, et al. Hemorrhagic shock in polytrauma patients: early detection with renal Doppler resistive index measurements. Radiology 2011; 260:112–118 [DOI] [PubMed] [Google Scholar]
- 33.Dewitte A, Coquin J, Meyssignac B, Joannès-Boyau O, Fleureau C, Roze H, et al. Doppler resistive index to reflect regulation of renal vascular tone during sepsis and acute kidney injury. Crit Care 2012; 16:R165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cronan JJ, Tublin ME. Role of the resistive index in the evaluation of acute renal obstruction. AJR Am J Roentgenol 1995; 164:377–378 [DOI] [PubMed] [Google Scholar]
- 35.Rodgers PM, Bates JA, Irving HG. Intrarenal Doppler ultrasound studies in normal and acutely obstructed kidneys. Br J Radiol 1992; 65:207–212 [DOI] [PubMed] [Google Scholar]
- 36.O’Connor OJ, Fitzgerald E, Maher MM. Imaging of hematuria. AJR Am J Roentgenol 2010; 195:W263–267 [DOI] [PubMed] [Google Scholar]


