Abstract
Hepatocyte growth factor (HGF) is a mitogen required for β-cell replication during pregnancy. To determine whether HGF/c-Met signaling is required for β-cell regeneration, we characterized mice with pancreatic deletion of the HGF receptor, c-Met (PancMet KO mice), in two models of reduced β-cell mass and regeneration: multiple low-dose streptozotocin (MLDS) and partial pancreatectomy (Ppx). We also analyzed whether HGF administration could accelerate β-cell regeneration in wild-type (WT) mice after Ppx. Mouse islets obtained 7 days post-Ppx displayed significantly increased c-Met, suggesting a potential role for HGF/c-Met in β-cell proliferation in situations of reduced β-cell mass. Indeed, adult PancMet KO mice displayed markedly reduced β-cell replication compared with WT mice 7 days post-Ppx. Similarly, β-cell proliferation was decreased in PancMet KO mice in the MLDS mouse model. The decrease in β-cell proliferation post-Ppx correlated with a striking decrease in D-cyclin levels. Importantly, PancMet KO mice showed significantly diminished β-cell mass, decreased glucose tolerance, and impaired insulin secretion compared with WT mice 28 days post-Ppx. Conversely, HGF administration in WT Ppx mice further accelerated β-cell regeneration. These results indicate that HGF/c-Met signaling is critical for β-cell proliferation in situations of diminished β-cell mass and suggest that activation of this pathway can enhance β-cell regeneration.
Introduction
Deficiency of functional β-cells ultimately leads to the development of diabetes. A potential future therapeutic approach to treat diabetes is to induce β-cell regeneration, but this requires deciphering the molecular mechanisms that control β-cell growth. In adult mice, β-cell replication is one of the main mechanisms to form new β-cells (1), but in basal conditions their proliferative capacity is very limited and further decreases with age (2). Several conditions, however, are known to stimulate β-cell replication including pregnancy, obesity, partial pancreatectomy (Ppx), and growth factor overexpression (3). Among these growth factors, we have shown that hepatocyte growth factor (HGF) overexpression increases β-cell replication, mass, and function in transgenic mice (4,5). Importantly, HGF regulates regeneration of multiple organs after injury (6–8). However, whether HGF plays a role in β-cell regeneration is unknown.
HGF binds with high affinity to and induces the dimerization of its tyrosine kinase receptor, c-Met (8). Both HGF and c-Met are expressed in the endocrine and nonendocrine pancreas, but conditional ablation of c-Met in adult mouse pancreas does not alter β-cell growth or function under basal conditions (9). However, we recently showed that pancreatic c-Met deficiency accelerates the onset of diabetes in a mouse model of multiple low-dose streptozotocin (MLDS) administration (9). Moreover, HGF is also required for maternal β-cell proliferation during pregnancy (10). Taken together, these studies indicate that HGF/c-Met signaling is required for β-cell adaptation to inflammatory and metabolic situations. They also suggest that HGF/c-Met signaling might participate in the regenerative response of β-cells after β-cell ablation. To address this issue, we analyzed β-cell regeneration in PancMet KO mice under situations of Ppx and MLDS treatment. Here, we report that c-Met is critically important for complete β-cell regeneration and that HGF administration into normal mice further accelerates β-cell regeneration post-Ppx. These observations underscore a therapeutic opportunity for the HGF/c-Met signaling pathway in diabetes.
Research Design and Methods
Generation of Conditional KO Mice With Pancreas Deletion of c-Met
PancMet KO mice were generated as previously described (9). Male mice (8–10 weeks old) were used in these studies. All studies were performed with the approval of, and in accordance with, guidelines established by the Icahn School of Medicine at Mount Sinai and the University of Pittsburgh institutional animal care and use committees.
MLDS-Induced Diabetes and Ppx Mouse Models
In the MLDS model, mice were injected with streptozotocin (40 mg/kg i.p.) for five consecutive days (9). For the Ppx model, the splenic portion of the pancreas was surgically removed (∼50–60% pancreatectomy) (11–13). Sham (SH) operation was performed by opening the abdomen while leaving the pancreas intact.
HGF Administration
Human recombinant HGF (Fitzgerald Industries International, Acton, MA) was administered in conjunction with dextran sulfate (DS), since DS enhances the effect and stability of HGF (14). DS (200 µg/mouse) was dissolved in saline and mixed with HGF (20 µg/mouse), and the mixture was injected intraperitoneally daily after Ppx. Control SH or Ppx mice were injected with an identical volume of saline.
Glucose Homeostasis
Blood was analyzed for glucose by a portable glucometer and plasma insulin by radioimmunoassay (Millipore, Bedford, MA) (4).
Immunohistochemistry
β-Cell mass and islet number were measured in four insulin-stained pancreas sections per mouse using ImageJ (National Institutes of Health, Bethesda, MD) (9,10). BrdU incorporation in β-cells was measured in pancreatic sections from mice injected intraperitoneally with BrdU (Amersham, Piscataway, NJ), killed 6 h later, and stained for insulin and BrdU (10). Sections were also stained for Ki67, phospho–histone-H3 (pHH3), and insulin (15). At least 2,000 β-cells/pancreas were counted.
Islet Isolation and mRNA Expression Analysis
Mouse islets were isolated after collagenase P injection through the pancreatic duct (4). Analysis of c-Met and HGF mRNA expression in isolated islets was performed by real-time PCR using specific primers and conditions previously described (9,10).
Glucose-Stimulated Insulin Secretion
Insulin release from 10–15 islets isolated from Ppx mice at 25 days postsurgery was measured after incubation with 2.8 or 22.2 mmol/L glucose for 30 min (12). Insulin secretion is expressed as percentage of total islet insulin content.
Western Blot Analysis
Mouse islet extracts were analyzed by Western blotting with antibodies against c-Met and cyclin-dependent kinase-4 (cdk-4) (Santa Cruz Biotechnology, Santa Cruz, CA), tubulin and HGF (Calbiochem, La Jolla, CA), and cyclin D1 and D2 (Thermo Fisher Scientific, Fremont, CA). After several washes, blots were incubated with peroxidase-conjugated secondary antibodies followed by chemiluminescence detection (9,10).
Statistical Analysis
The data are presented as means ± SE. Statistical analysis was performed using unpaired two-tailed Student t test. P < 0.05 was considered statistically significant.
Results
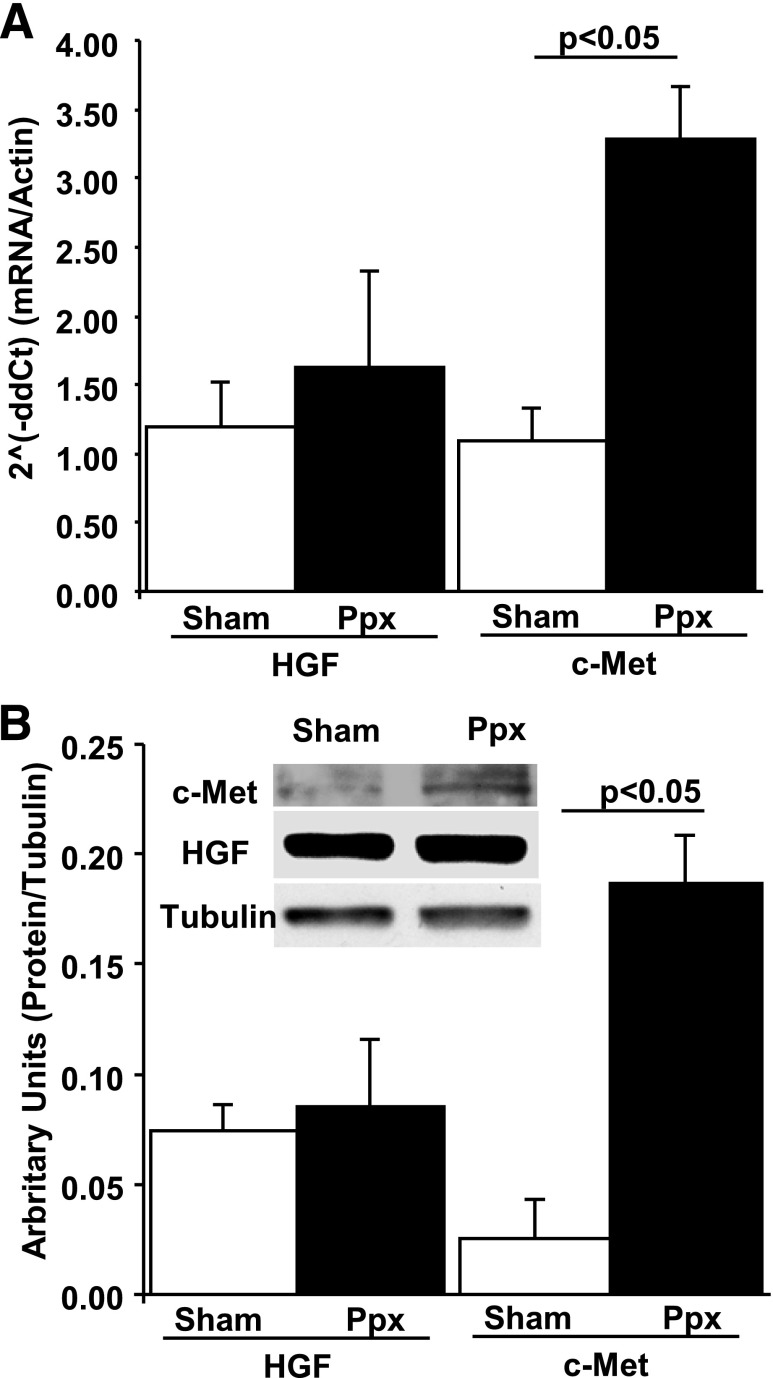
c-Met Expression Increases in Mouse Islets After Ppx
Analysis of c-Met expression in mouse islets obtained 7 days (7 days) after Ppx indicate that both c-Met mRNA (Fig. 1A) and protein (Fig. 1B) are increased in this model of β-cell regeneration. On the other hand, HGF mRNA and protein expression remained unchanged in these islets (Fig. 1). Collectively, these data and previous data in the MLDS model (9) suggest that reduction of β-cell mass is associated with an increase in c-Met expression in the remnant islets.
Figure 1.
Analysis of HGF and c-Met expression in islets from SH-operated or Ppx WT mice at 7 days postsurgery. A: Real-time PCR analysis of HGF and c-Met mRNA expression in total RNA extracted from islets obtained from WT mice 7 days after surgery. Results are means ± SEM of SH-operated (n = 4) and Ppx (n = 3) mice. P < 0.05 vs. SH-operated mouse islets. Actin was used as a housekeeping gene. B: Western blot analysis of c-Met and HGF expression in protein extracts of islets isolated from WT mice 7 days after surgery. Results are means ± SEM of SH-operated (n = 4) and Ppx (n = 4) mice. P < 0.05 vs. SH-operated mouse islets. Inset: Representative Western blot. Tubulin was used as housekeeping protein. 2ˆ(−ddCt) = 2(−delta delta Cycle threshold).
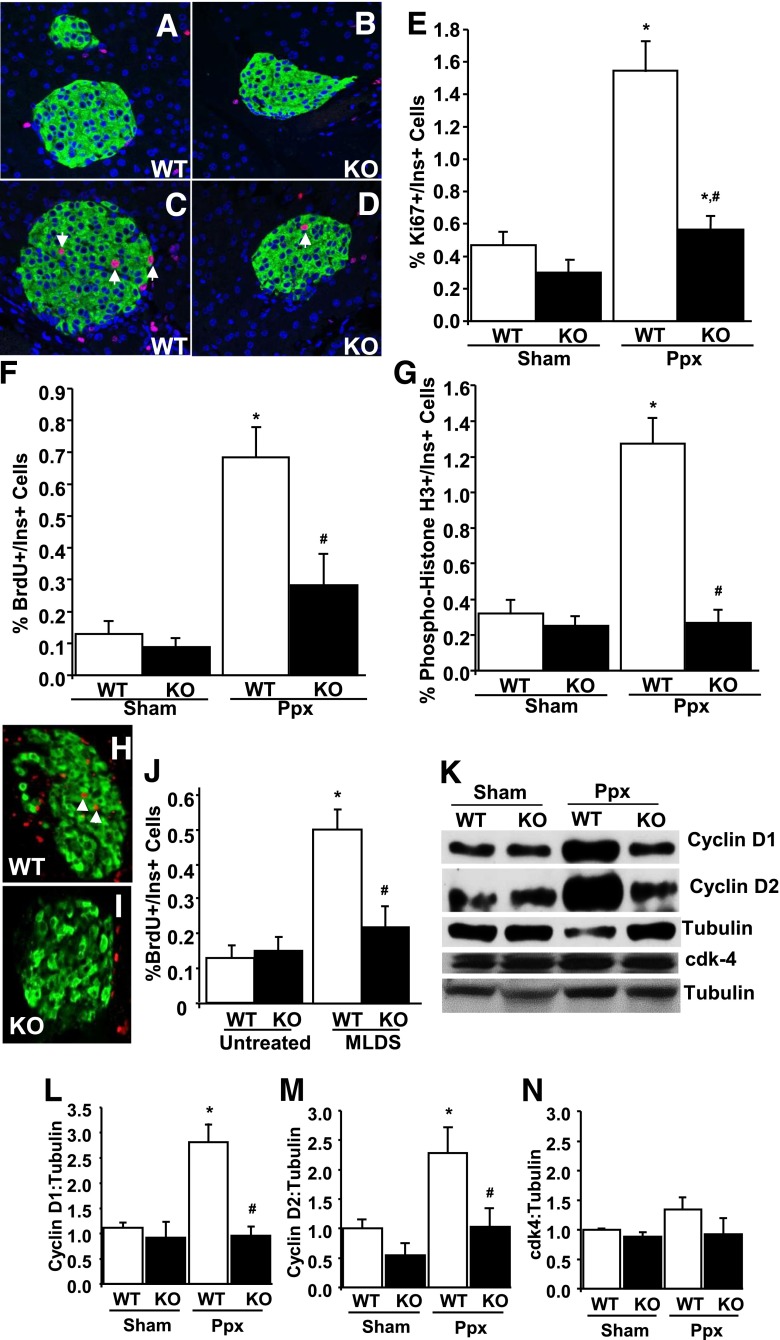
β-Cell Proliferation Does Not Increase in PancMet KO Mice After Both Ppx and MLDS Treatment
Since islet c-Met is upregulated after Ppx and MLDS treatments (Fig. 1) (9) and HGF increases β-cell proliferation (4), we sought to address the importance of c-Met in β-cell replication in these two mouse models of decreased β-cell mass. Pancreatic mass removed after Ppx was not different in both types of mice (Supplementary Fig. 1A). Body weight was not significantly different among these mice postsurgery (Supplementary Fig. 1B). As expected, β-cell mass was significantly diminished 7 days post-Ppx compared with SH-operated mice, but it was not significantly different between wild-type (WT) and PancMet KO mice in either surgical group (Supplementary Fig. 1C). In contrast, as shown in the representative images (Fig. 2A–D) and the corresponding quantitation (Fig. 2E–G), the number of proliferating β-cells (Ki67-, pHH3-, and BrdU-positive) was markedly and significantly decreased in PancMet KO mice compared with WT littermates 7 days post-Ppx. No evident alterations in vimentin staining were observed in pancreatic sections of WT and PancMet KO mice post-Ppx (not shown), suggesting that changes in epithelial-to-mesenchymal transition might not be involved in the proliferative changes observed in PancMet KO mice after Ppx.
Figure 2.
β-Cell proliferation in Ppx and MLDS-treated PancMet KO mice. A–D: Representative photomicrographs of SH-operated (A and B) and Ppx (C and D) WT (A and C) and PancMet KO (B and D) mouse pancreatic sections obtained at 7 days postsurgery and stained for insulin (green) and Ki67 (red). Arrows indicate Ki67-positive β-cell nuclei. Magnification of the images is ×630. E–G: Quantification of the percentage of Ki67-positive (E), BrdU-positive (F), and pHH3-positive (G) β-cells in SH-operated (n = 3) and Ppx (n = 7) WT and PancMet KO (n = 3 and n = 9, respectively) mice 7 days after surgery. Results are means ± SEM. *P < 0.05 vs. their corresponding SH-operated mice; #P < 0.05 vs. Ppx-WT mice. Values are not significantly different except where indicated. H and I: Representative photomicrographs of MLDS-treated WT (H) and PancMet KO (I) mouse pancreatic sections obtained at 20 days post-MLDS treatment and stained for insulin (green) and BrdU (red). Arrows indicate BrdU-positive β-cell nuclei. Magnification of the images is ×630. J: Quantification of the percentage of BrdU-positive β-cells in untreated (n = 5) and MLDS-treated (n = 10) WT and PancMet KO (n = 5 and n = 5, respectively) mice 20 days after treatment. Results are means ± SEM. *P < 0.05 vs. corresponding untreated mice; #P < 0.05 vs. MLDS-WT mice. Values are not significantly different except where indicated. K: Representative Western blot displaying cyclin D1, D2, cdk-4, and tubulin expression in protein extracts from SH-operated or Ppx PancMet KO and WT islets obtained at 7 days postsurgery. L–N: Densitometric quantitation of cyclin D1 (L), cyclin D2 (M), and cdk-4 (N) in five Western blots performed with five different protein extracts per condition. Results are means ± SEM. *P < 0.05 vs. SH-operated WT or PancMet KO mice; #P < 0.05 vs. Ppx WT mice. Values are not significantly different except where indicated. Ins, insulin.
The number of BrdU-positive β-cells was also significantly decreased in PancMet KO mice 20 days post-MLDS treatment (Fig. 2H–J). These results indicate that intact HGF/c-Met signaling is required for β-cell proliferation in situations of diminished β-cell mass accompanied by islet inflammation and diabetes (MLDS model) (9) or without islet inflammation and normal glucose homeostasis (Ppx model) (Supplementary Fig. 1D and E).
Ppx-Induced Upregulation of D Cyclins Is Diminished in PancMet KO Mouse Islets
D cyclins are upregulated in rodent islets when maximal proliferation occurs after Ppx (11,16). To determine whether the decrease in β-cell proliferation in PancMet KO mice after Ppx was associated with changes in G1/S transition activators, we analyzed D-cyclin and cdk-4 levels in PancMet KO and WT mouse islets 7 days post-Ppx. PancMet KO islets post-Ppx displayed a remarkable and significant decrease in cyclins D1 and D2, with no alteration in cdk-4 (Fig. 2K–N), suggesting an association between lower D cyclins and diminished β-cell replication in PancMet KO mice post-Ppx.
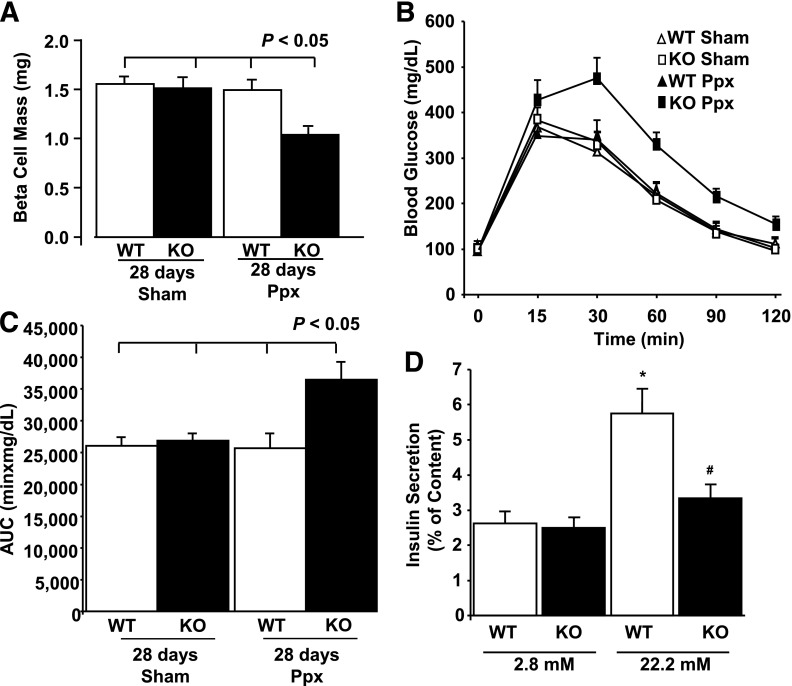
PancMet KO Mice Have Incomplete β-Cell Mass Regeneration and Diminished Glucose Tolerance
We assessed the impact of HGF/c-Met signaling on β-cell regeneration in PancMet KO and WT mice at 28 days after Ppx. β-Cell mass was increased in WT mice post-Ppx, reaching similar levels to SH-operated mice (Fig. 3A). Importantly, β-cell mass in PancMet KO mice was significantly decreased post-Ppx compared with WT mice and SH-operated mice (Fig. 3A), indicating incomplete β-cell regeneration. Islet number was not different between PancMet KO and WT littermates at 28 days post-Ppx (not shown), suggesting that the early decrease in β-cell proliferation was potentially responsible for the incomplete β-cell regeneration in c-Met–deficient mice. Furthermore, PancMet KO mice displayed decreased glucose tolerance at 25 days post-Ppx, suggesting that the incomplete β-cell mass and perhaps defective insulin secretion might have an impact on glucose homeostasis in c-Met–deficient mice (Fig. 3B and C). Indeed, glucose-stimulated insulin secretion (GSIS) is decreased in isolated islets from PancMet KO mice 25 days post-Ppx compared with WT mice (Fig. 3D). Taken together, these results indicate that HGF/c-Met signaling is required for full β-cell mass recovery and normal GSIS and glucose homeostasis in a model of surgically reduced β-cell mass.
Figure 3.
Incomplete β-cell mass regeneration in PancMet KO mice after Ppx. A: Quantification of β-cell mass in SH-operated (n = 5) and Ppx (n = 7) WT and PancMet KO (n = 5 and n = 10, respectively) mice 28 days after surgery. Results are means ± SEM. P < 0.05 vs. sham-operated WT or PancMet KO mice and Ppx WT mice. B: Intraperitoneal glucose tolerance test (3 g glucose/kg body wt) in sham-operated (n = 5) and Ppx (n = 7) WT and PancMet KO (n = 5 and n = 10, respectively) mice 25 days after surgery. Results are means ± SEM. C: Area under the curve (AUC) calculated from the intraperitoneal glucose tolerance test experiments in which sham-operated and Ppx WT and PancMet KO mice 25 days after surgery were examined. Results are means ± SEM. P < 0.05 vs. sham-operated WT or PancMet KO mice and Ppx WT mice. D: Quantitation of insulin secretion in islets isolated from WT (n = 6) and PancMet KO (n = 4) Ppx mice at 25 days postsurgery and incubated with 2.8 and 22.2 mmol/L glucose for 30 min. Results are means ± SEM. *P < 0.05 vs. islets at 2.8 mmol/L;#P < 0.05 vs. Ppx WT islets at the same glucose concentration.
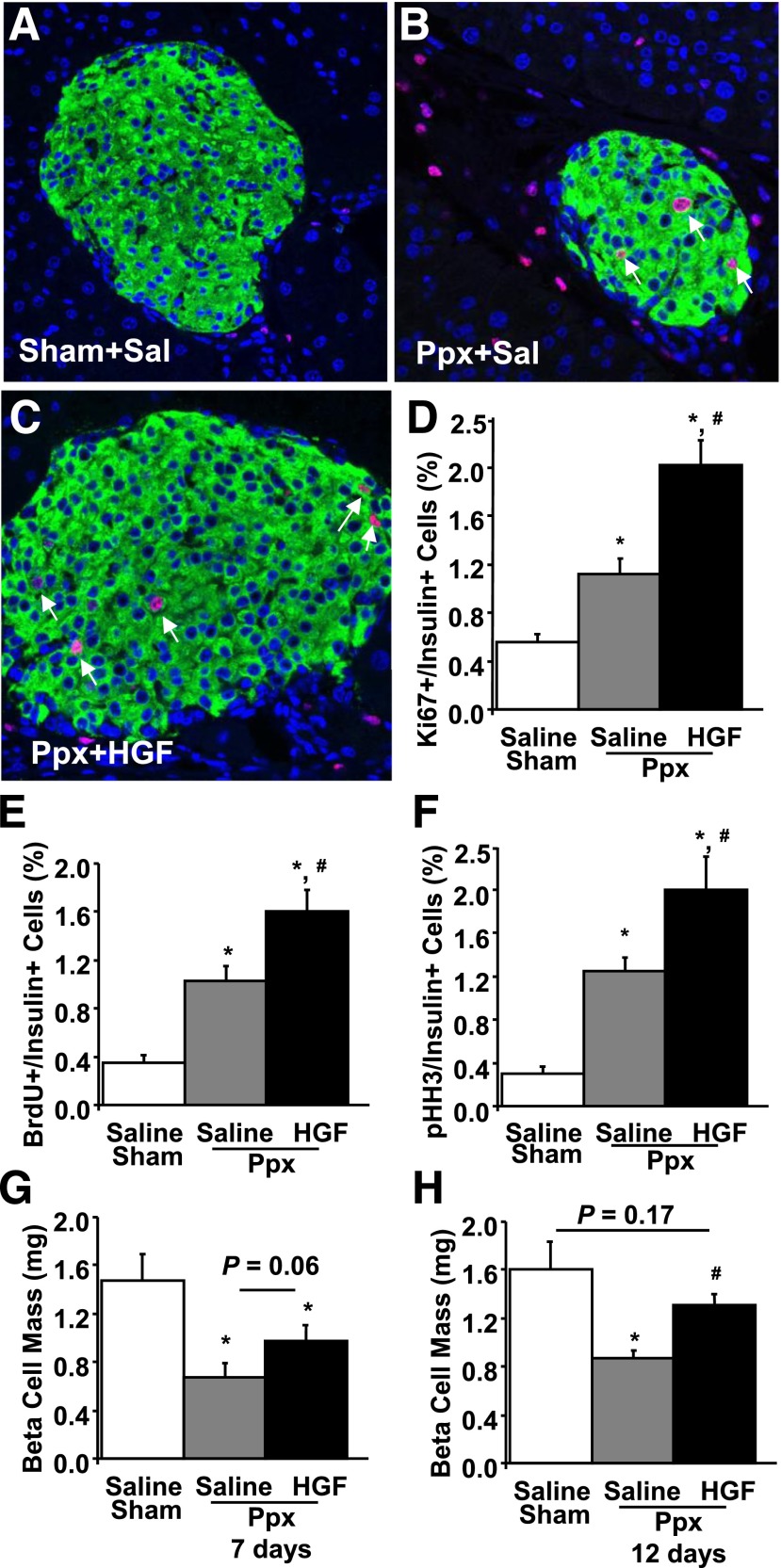
HGF Administration Further Enhances β-Cell Proliferation After Ppx
HGF increases β-cell proliferation in adult transgenic mice in basal conditions (4). Since islet c-Met is upregulated post-Ppx, we examined whether HGF administration could further enhance β-cell regeneration after Ppx. Daily HGF administration increased β-cell proliferation compared with saline-treated controls 7 days post-Ppx (Fig. 4A–F), suggesting that HGF could further accelerate β-cell regeneration. Indeed, HGF increased β-cell mass in Ppx mice at 7 days (P = 0.06) and 12 days (P < 0.05) compared with saline-treated Ppx mice (Fig. 4G and H). This highlights the therapeutic potential of HGF for increasing β-cell regeneration in diabetes.
Figure 4.
β-Cell proliferation in Ppx WT mice treated with saline or HGF. A–C: Representative photomicrographs of pancreatic sections from SH-operated saline (Sal)-treated (A) and Ppx saline-treated (B) or HGF-treated (C) WT mice at 7 days postsurgery and stained for insulin (green) and Ki67 (red). Arrows indicate Ki67-positive β-cell nuclei. Magnification of the images is ×630. Mice were treated daily with 20 μg/mouse HGF and 200 μg/mouse DS in saline or an identical volume of saline for 7 days. D–G: Quantification of the percentage of Ki67-positive (D), BrdU-positive (E), and pHH3-positive (F) β-cells and β-cell mass (G) in SH-operated saline-treated (n = 4) and Ppx saline-treated (n = 7) or HGF-treated (n = 4) WT mice 7 days after surgery. H: β-Cell mass in mice treated with HGF (n = 4) or saline (sham, n = 3; Ppx, n = 3) for 12 days as indicated above. Results are means ± SEM. *P < 0.05 vs. saline-injected SH-operated mice; #P < 0.05 vs. saline-injected Ppx-operated mice.
Discussion
The current study provides the first direct evidence that endogenous pancreatic HGF/c-Met signaling is required for β-cell regeneration in situations of diminished β-cell mass. On one hand, c-Met absence in the mouse pancreas diminishes β-cell replication leading to incomplete β-cell mass expansion after Ppx and MLDS treatment (9). On the other hand, HGF administration further enhances mouse β-cell regeneration after Ppx. Therefore, activation of HGF/c-Met signaling is needed for full β-cell regeneration and truly highlights this pathway as a potential therapeutic target for β-cell regeneration in diabetes.
The role of growth factors in the adaptive β-cell proliferative response in situations of diminished β-cell mass has been understudied. Multiple growth factors have been shown to increase β-cell proliferation in vivo in basal conditions; however, only GLP-1 has been shown to be required for β-cell regeneration after Ppx (12). GLP-1 receptor−/− mice displayed markedly diminished β-cell mass 5 weeks post-Ppx. Importantly, as in the GLP-1 studies, mice with pancreatic c-Met deletion displayed decreased β-cell proliferation and incomplete β-cell mass recovery after Ppx. This would suggest that at least in mice, both GLP-1 and HGF are required for complete β-cell regeneration after Ppx. It is important to note that both HGF and GLP-1 activate protein kinase C-ζ, and this activation is required for increasing proliferation in rodent β-cells (17,18). It is important to note that c-Met deletion in islets also led to decreased GSIS and glucose intolerance 25 days post-Ppx, aspects not present in PancMet KO mice in basal conditions (9). Similarly, pregnant PancMet KO mice display incomplete maternal β-cell expansion and defective GSIS (10). Taken together, these observations suggest that c-Met deficiency in pancreas is associated not only with incomplete β-cell expansion in physiological and pathological models but also with defective insulin secretion.
Interestingly, c-Met–null islets did not display the upregulation of cyclin D1 and D2 observed in WT mouse islets after Ppx. D cyclins are essential for postnatal β-cell growth, and their overexpression leads to increased β-cell proliferation (19,20). Therefore, it is likely that the diminished levels of islet D cyclins in PancMet KO mice might compromise the accelerated cell cycle progression and regeneration after Ppx.
It has been suggested that β-cell regeneration, in the face of immune destruction, occurs in patients with recent-onset type 1 diabetes (21,22). To further assess the regenerative role of HGF/c-Met signaling, we analyzed β-cell replication in PancMet KO mice in a surrogate model of islet inflammation with features of type 1 diabetes: the MLDS model (9). In this model, the enhanced β-cell proliferation observed in WT mice was impaired in c-Met–null islets, further confirming that HGF/c-Met signaling is essential for β-cell regeneration, even in a setting with cytotoxic- and immune-mediated reduction of β-cells. Taken together, these and previous studies indicate that although endogenous HGF/c-Met signaling is dispensable for normal adult β-cell growth in basal conditions, it is required for β-cell proliferation in situations of diminished β-cell mass such as Ppx and MLDS administration (current studies) and increased metabolic demand such as pregnancy and obesity/insulin resistance (10,23). This highlights HGF as a key growth factor for β-cell proliferation and expansion in pathophysiologic situations.
Since HGF/c-Met signaling is required for β-cell proliferation after Ppx, islet c-Met is increased after Ppx, and HGF is a mitogen for rodent β-cells (4), we wondered whether HGF administration in vivo could lead to further enhanced β-cell regeneration. Daily HGF administration further accelerated the already high levels of β-cell proliferation found in mice after Ppx. Importantly, this increase in β-cell proliferation in HGF-treated Ppx mice led to a further increase in β-cell mass compared with saline-treated mice. This indicates that HGF could be used as a regenerative factor for the treatment of diabetes. Nevertheless, it is clear that unwanted proliferation of non–β-cells might be a concern when administration of growth factors/hormones is suggested as a potential therapy for regenerative purposes. It is important to note that circulating HGF levels are increased not only in situations related to uncontrolled cell replication but also in situations such as pregnancy (10,24) and obesity (25). In addition, future approaches targeting specifically the β-cell could further facilitate the use of activators of the HGF/c-Met signaling pathway without potential worrisome uncontrolled proliferation of non-β-cells.
In summary, these studies clearly indicate that HGF is required for β-cell regeneration in situations of diminished β-cell mass. Importantly, HGF administration can further increase β-cell regeneration in mice with diminished β-cell mass, highlighting HGF/c-met signaling as a potential therapeutic target for enhancing β-cell regeneration in diabetes.
Article Information
Acknowledgments. The authors thank Drs. Andrew F. Stewart (Icahn School of Medicine at Mount Sinai) and Laura C. Alonso (University of Massachusetts) for helpful comments during the development of these studies and Shelley Valle and Taylor Rosa (University of Pittsburgh) for technical help.
Funding. This work was supported in part by grants from the National Institutes of Health (DK-067351 and DK-077096) and the Juvenile Diabetes Research Foundation (1-2007-3) to A.G.-O. S.E. was the recipient of a postdoctoral fellowship from the National Institutes of Health T32 Research Training grant (T32DK-07052-32). C.D. was the recipient of a research fellowship from the Lawson Wilkins Pediatric Endocrine Society.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.C.A.-P., S.E., and C.D. researched data, contributed to discussion, and reviewed and edited the manuscript. G.P.C., J.M.D.M.-G., and F.R.-P. researched data. R.C.V. contributed to discussion and reviewed and edited the manuscript. A.G.-O. researched data, contributed to discussion, and wrote the manuscript. A.G.-O. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db13-0333/-/DC1.
C.D. is currently affiliated with Pediatric Endocrinology, Connecticut Children’s Medical Center, Hartford, CT, and J.M.D.M.-G. is currently affiliated with Centro Andaluz de Biología Molecular y Medicina Regenerativa, Sevilla, Spain.
References
- 1.Dor Y, Brown J, Martinez OI, Melton DA. Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature 2004;429:41–46 [DOI] [PubMed] [Google Scholar]
- 2.Rankin MM, Kushner JA. Adaptive beta-cell proliferation is severely restricted with advanced age. Diabetes 2009;58:1365–1372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ackermann AM, Gannon M. Molecular regulation of pancreatic beta-cell mass development, maintenance, and expansion. J Mol Endocrinol 2007;38:193–206 [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Ocaña A, Takane KK, Syed MA, Philbrick WM, Vasavada RC, Stewart AF. Hepatocyte growth factor overexpression in the islet of transgenic mice increases beta cell proliferation, enhances islet mass, and induces mild hypoglycemia. J Biol Chem 2000;275:1226–1232 [DOI] [PubMed] [Google Scholar]
- 5.García-Ocaña A, Vasavada RC, Cebrian A, et al. Transgenic overexpression of hepatocyte growth factor in the beta-cell markedly improves islet function and islet transplant outcomes in mice. Diabetes 2001;50:2752–2762 [DOI] [PubMed] [Google Scholar]
- 6.Huh CG, Factor VM, Sánchez A, Uchida K, Conner EA, Thorgeirsson SS. Hepatocyte growth factor/c-met signaling pathway is required for efficient liver regeneration and repair. Proc Natl Acad Sci USA 2004;101:4477–4482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohmichi H, Matsumoto K, Nakamura T. In vivo mitogenic action of HGF on lung epithelial cells: pulmotrophic role in lung regeneration. Am J Physiol 1996;270:L1031–L1039 [DOI] [PubMed] [Google Scholar]
- 8.Nakamura T, Sakai K, Nakamura T, Matsumoto K. Hepatocyte growth factor twenty years on: Much more than a growth factor. J Gastroenterol Hepatol 2011;26(Suppl 1):188–202 [DOI] [PubMed] [Google Scholar]
- 9.Mellado-Gil J, Rosa TC, Demirci C, et al. Disruption of hepatocyte growth factor/c-Met signaling enhances pancreatic beta-cell death and accelerates the onset of diabetes. Diabetes 2011;60:525–536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Demirci C, Ernst S, Alvarez-Perez JC, et al. Loss of HGF/c-Met signaling in pancreatic β-cells leads to incomplete maternal β-cell adaptation and gestational diabetes mellitus. Diabetes 2012;61:1143–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He LM, Sartori DJ, Teta M, et al. Cyclin D2 protein stability is regulated in pancreatic beta-cells. Mol Endocrinol 2009;23:1865–1875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De León DD, Deng S, Madani R, Ahima RS, Drucker DJ, Stoffers DA. Role of endogenous glucagon-like peptide-1 in islet regeneration after partial pancreatectomy. Diabetes 2003;52:365–371 [DOI] [PubMed] [Google Scholar]
- 13.Peshavaria M, Larmie BL, Lausier J, et al. Regulation of pancreatic beta-cell regeneration in the normoglycemic 60% partial-pancreatectomy mouse. Diabetes 2006;55:3289–3298 [DOI] [PubMed] [Google Scholar]
- 14.Nakano M, Yasunami Y, Maki T, et al. Hepatocyte growth factor is essential for amelioration of hyperglycemia in streptozotocin-induced diabetic mice receiving a marginal mass of intrahepatic islet grafts. Transplantation 2000;69:214–221 [DOI] [PubMed] [Google Scholar]
- 15.Harb G, Vasavada RC, Cobrinik D, Stewart AF. The retinoblastoma protein and its homolog p130 regulate the G1/S transition in pancreatic beta-cells. Diabetes 2009;58:1852–1862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morisset J, Aliaga JC, Calvo EL, Bourassa J, Rivard N. Expression and modulation of p42/p44 MAPKs and cell cycle regulatory proteins in rat pancreas regeneration. Am J Physiol 1999;277:G953–G959 [DOI] [PubMed] [Google Scholar]
- 17.Vasavada RC, Wang L, Fujinaka Y, et al. Protein kinase C-zeta activation markedly enhances beta-cell proliferation: an essential role in growth factor mediated beta-cell mitogenesis. Diabetes 2007;56:2732–2743 [DOI] [PubMed] [Google Scholar]
- 18.Buteau J, Foisy S, Rhodes CJ, Carpenter L, Biden TJ, Prentki M. Protein kinase Czeta activation mediates glucagon-like peptide-1-induced pancreatic beta-cell proliferation. Diabetes 2001;50:2237–2243 [DOI] [PubMed] [Google Scholar]
- 19.Kushner JA, Ciemerych MA, Sicinska E, et al. Cyclins D2 and D1 are essential for postnatal pancreatic beta-cell growth. Mol Cell Biol 2005;25:3752–3762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang X, Gaspard JP, Mizukami Y, Li J, Graeme-Cook F, Chung DC. Overexpression of cyclin D1 in pancreatic beta-cells in vivo results in islet hyperplasia without hypoglycemia. Diabetes 2005;54:712–719 [DOI] [PubMed] [Google Scholar]
- 21.Willcox A, Richardson SJ, Bone AJ, Foulis AK, Morgan NG. Evidence of increased islet cell proliferation in patients with recent-onset type 1 diabetes. Diabetologia 2010;53:2020–2028 [DOI] [PubMed] [Google Scholar]
- 22.Meier JJ, Bhushan A, Butler AE, Rizza RA, Butler PC. Sustained beta cell apoptosis in patients with long-standing type 1 diabetes: indirect evidence for islet regeneration? Diabetologia 2005;48:2221–2228 [DOI] [PubMed] [Google Scholar]
- 23.Araújo TG, Oliveira AG, Carvalho BM, et al. Hepatocyte growth factor plays a key role in insulin resistance-associated compensatory mechanisms. Endocrinology 2012;153:5760–5769 [DOI] [PubMed] [Google Scholar]
- 24.Horibe N, Okamoto T, Itakura A, et al. Levels of hepatocyte growth factor in maternal serum and amniotic fluid. Am J Obstet Gynecol 1995;173:937–942 [DOI] [PubMed] [Google Scholar]
- 25.Rehman J, Considine RV, Bovenkerk JE, et al. Obesity is associated with increased levels of circulating hepatocyte growth factor. J Am Coll Cardiol 2003;41:1408–1413 [DOI] [PubMed] [Google Scholar]