Abstract
Background:
District mental health program (DMHP) is the flagship program of Government of India to deliver mental health-care throughout the country. Being an out-reach program, it is likely that elderly people with mental health programs are accessing it more frequently. If this is the case, there is potential for including additional components in this program so that something more than the generic service is offered to them.
Aim:
This study aims to find out whether the elderly are accessing the DMHP services frequently.
Materials and Methods:
We compared the proportion of elderly people attending two mental health-care facilities: - A Government Medical College Out-patient Department and the clinics run by the DMHP of the same department.
Results:
A significantly higher number of elderly people are attending the clinics of the DMHP compared to the outpatient service of a teaching hospital.
Conclusion and Implication:
It is concluded that DMHP can be further strengthened by adding additional components like service for the elderly. This is important in view of the increasing number of older people who may need these services in future.
Keywords: Aged with mental disorders, delivery of health care, community based care, mental health program
INTRODUCTION
District mental health program (DMHP) is an approach to decentralize mental health-care in the community using the existing public health infrastructure and additional resources. This model has been pilot tested in Bellary district of Karnataka State and found to be useful in addressing the basic mental health needs of the population. Later on, this model was developed as a program, which was thought fit to be applied to the whole of India. The central government funded DMHP in a few districts in the first phase. More districts were added subsequently. Currently, 126 districts have running programs.
In most districts where the program is in operation, a team of the DMHP, consisting of a Psychiatrist, Psychologist, social worker, and nurse visits designated peripheral health centers. They deliver diagnostic and therapeutic services. Medicines and services are provided free of cost to the patients attending the clinic. Services are geared to provide general adult psychiatric care. There are no special services for special populations such as women, children, elderly, and those with substance misuse, though persons with such problems could also be approaching these clinics.
Being a decentralized program, DMHP may be more accessible to older people with mental health problems and their families. Is this presumption true? If older people tend to access DMHP more than the traditional service, then there is a strong case to suitably modify DMHP to meet the mental health needs of the rapidly growing number of older people in our country. This would then open up an avenue for scaling up geriatric mental health services across the country.
AIM
This study aims to examine whether there is an increased attendance of elderly persons at DMHP clinics, compared to a traditional tertiary care facility (Psychiatry Out-patient Department of a Government Medical College Hospital (MCH)) by examining records available at these two setting.
MATERIALS AND METHODS
The out-patient records maintained by the Department of Psychiatry at a Government MCH, and the office of the DMHP at the nearby district and run by the same department were analyzed to find out the number and socio demographic details of out-patients seen at these two facilities during a period of 1 year. All subjects who attended the out-patient services during the study at these two facilities period were identified from the records. They were categorized into two groups based on the recorded age. Patients 60 years and older formed the geriatric group and the others formed the second group.
The proportions of geriatric subgroup in two centers were estimated. Sex ratio was also examined. The sample from these two centers were compared to see if there was any significant difference in the proportion of older people seen at these two care facilities. We also made sex-wise comparison of the older patients from both the settings to see if there was any difference between these two in terms of the proportion of women getting care.
RESULTS
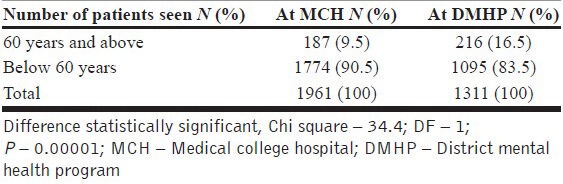
The data in Table 1 shows that elderly account for only 9.5% of out-patient attendance at the MCH while they account for 16.5% in the clinics of DMHP. This difference was statistically significant (Chi-square test; P<0.0001).
Table 1.
Comparison of patients attending a MCH and community outreach clinics of DMHP (1st May 2007 and 30th April 2008)
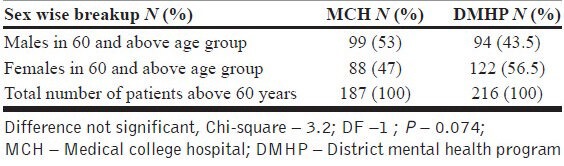
Proportion of women in the geriatric age group seen at the DMHP clinics were more, compared to the sample from the MCH. It was 56.5% versus 47% respectively. However, this difference was not statistically significant [Table 2].
Table 2.
Older people seeking care at MCH and community outreach clinics of DMHP (1st May 2007 and 30th April 2008)
DISCUSSION
Our results show that a significant proportion of people who receive mental health-care through the community outreach clinics of DMHP are people above the age of 60 years. In fact, every sixth person seen at these clinics is an older person. The proportion of older people among the users was DMHP clinics is 16.5%, whereas the proportion of people above the age of 60 years in the general population in the state of study is less than 11%. It is no big surprise to note that the decentralized services provided by the DMHP are more accessible to older people. This implies that the provision of care through community outreach clinics by the DMHP is a step in the right direction. However, the services currently provided through the DMHP are generic, and not tailored to meet special needs of the elderly. While planning decentralized programs, planners should understand that its users are likely to include special populations and provide additional services.
There are no government funded specialized services for elderly in India and the outreach services generally do not include health-care for older people as part of their work.[1,2,3] Our study shows that DMHP clinics are more accessible for older people. Improving access is important, but that is not enough. We need to ensure that the services provided do meet the needs of older people who seek help. For example, an attempt will have to be made to cater to the special needs of people with medical illness and depression. People with disabling conditions like dementia and their caregivers may need to be provided specialized care and support. There has to be a strong link with the existing outreach services. DMHP should take up the task of supporting and guiding community based initiatives as well as other out reach services. Community clinics run by DMHP can support and supervise other community based initiatives.[4] Collaboration with palliative care initiatives has the potential for wider application in the community.
Primary care as well as outreach services can play a crucial role in scaling up services for older people with mental health needs. We need to develop a strategy to link the community clinics of the DMHP with primary care and outreach services. These links should provide a two way support. Primary care need to receive continuous support and guidance from the mental health expertise available with the DMHP. Health workers could be trained to identify cases of dementia in the community.[5] They may be able to identify older individuals with unmet mental health needs and bring them to the notice of the services. Service providers then could think of strategies to bring them into the service network. Once this is possible, clinicians will be in a better position to identify and manage common mental health problems of late life such as depression and dementia. Outreach services can facilitate case identification and support home based care. They can play a huge role in providing information and education to the caregivers and could be entrusted to deliver simple caregiver interventions.[4,6] Support to home based care is particularly important in conditions such as dementia and various other disabling conditions affecting older people.
CONCLUSION
DMHP should reorient itself by deciding to focus on the special needs of the older people. This need will become more evident in the future as we anticipate gradual increase in the number of older people in the population. It is time that we reevaluate the potential for DMHP to provide better mental health-care for older people. This will help to scale up the services for older people with mental health needs in India. Our findings support this view. We need to convince the governments and policy makers to make such changes in the DMHP.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Patel V, Prince M. Ageing and mental health in a developing country: Who cares? Qualitative studies from Goa, India. Psychol Med. 2001;31:29–38. doi: 10.1017/s0033291799003098. [DOI] [PubMed] [Google Scholar]
- 2.Sathyanarayana Rao TS, Shaji KS. Demographic aging: Implications for mental health. Indian J Psychiatry. 2007;49:78–80. doi: 10.4103/0019-5545.33251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaji KS, Kishore NR, Lal KP, Pinto C, Trivedi JK. Better mental health care for older people in India. Indian J Psychiatry. 2004;46:367–72. [PMC free article] [PubMed] [Google Scholar]
- 4.Shaji KS. Dementia care in developing countries: The road ahead. Indian J Psychiatry. 2009;51:S5–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Shaji KS, Arun Kishore NR, Lal KP, Prince M. Revealing a hidden problem. An evaluation of a community dementia case-finding program from the Indian 10/66 dementia research network. Int J Geriatr Psychiatry. 2002;17:222–5. doi: 10.1002/gps.553. [DOI] [PubMed] [Google Scholar]
- 6.Dias A, Dewey ME, D’Souza J, Dhume R, Motghare DD, Shaji KS, et al. The effectiveness of a home care program for supporting caregivers of persons with dementia in developing countries: A randomised controlled trial from Goa, India. PLoS One. 2008;3:e2333. doi: 10.1371/journal.pone.0002333. [DOI] [PMC free article] [PubMed] [Google Scholar]


