Abstract
Background:
Post-traumatic stress disorder (PTSD) is the one of the most commonly observed psychiatric disorder in veterans. The condition can lead to considerable social, occupational, and interpersonal dysfunction. PTSD occurring after combat injury appears to be strongly correlated with the extent of injury, and develops over several months. Present study was designed for assessing the cognitive behavioral therapy in the quality of life (QOL) of war-related PTSD in veterans compared to control group and compare applied treatments with each other.
Materials and Methods:
In the present study, we assessment effects of cognitive behavioral therapy such as problem solving, exposure therapy and their combination on QOL in 120 Iranian PTSD patients veterans after Iran-Iraq war. They were randomly allocated to one of four equal interventional groups: (a) Problem solving therapy (b) exposure therapy (c) combined therapy (exposure therapy plus problem solving) (d) control group. Before and after study intervention, patients were evaluated by short form-36 (SF-36) questionnaire.
Results:
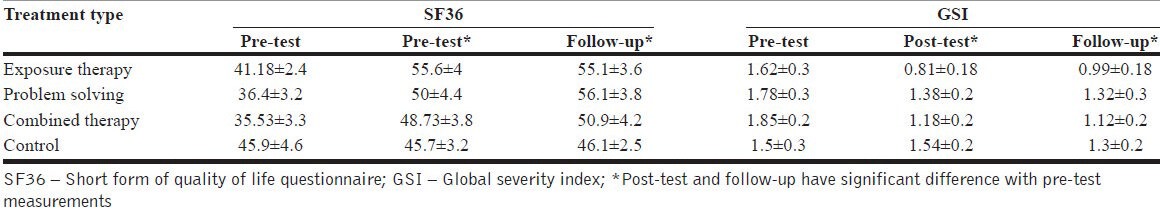
Post-test and follow-up SF-36 scores were 55.6±4 and 55.1±3.6 in exposure therapy, 50±4.4 and 56.1±3.8 in problem solving, and 48.73±3.8 and 50.9±4.2 in combined therapy. In comparing to control group, all intervention showed significant improvement in QOL in PTSD patients.
Conclusion:
According to the results of the present study, behavioral therapy can improve QOL in PTSD patients.
Keywords: Exposure therapy, post-traumatic stress disorder, problem solving skills, quality of life, short form-36
INTRODUCTION
War veterans were exposed frequently to a variety of traumatic events and stressors due to their special condition. Post-traumatic stress disorder (PTSD) is the most commonly observed psychiatric disorder in communities affected by disasters and mass violence.[1] PTSD has been described as “the complex somatic, cognitive, affective, and behavioral effects of psychological trauma.”[2] PTSD is characterized by intrusive thoughts, nightmares and flashbacks of past traumatic events, avoidance of reminders of trauma, hypervigilance and sleep disturbance, all of which lead to considerable social, occupational, and interpersonal dysfunction. About 27% of people, who experienced an awful trauma and have been injured physically, would suffer from the PTSD in future.[3] The pathophysiology of PTSD reflects long-lasting changes in the biological stress response systems that underlie many of the symptoms of PTSD and other trauma related disorders.[4]
In the overall, PTSD imparts substantial functional impairment in the exposed and is often comorbid with conditions such as depression, generalized anxiety disorder, and substance abuse.[5] PTSD occurring after combat NZ injury appears to be strongly correlated with the extent of injury and develops over several months.[6] Evidence suggests that the severity of PTSD is related to the degree of combat exposure and war duration.[7,8,9] Since, Iran-Iraq war lasted for 8 years (1982-1989) it has been presumed to burden a variety of uncompensated psychological damages such as PTSD, on both sides.
Cognitive-behavioral treatment (CBT) comprising interactive psycho education, cognitive restructuring and anxiety management training, offers the best outcome supported by Randomized Clinical Trial (RCT) studies for PTSD patients.[10,11,12] Generally, controlled research studies have indicated that behavioral and CBTs are effective in reducing symptoms of PTSD and depression.[13] Problem solving therapy, a short-term cognitive behavioral intervention teaches a systematic method for solving current, and future problems. Exposure-based behavioral treatments utilize gradual, systematic, repeated exposure to the feared object or situation to allow patients with anxiety disorders to become desensitized to the feared stimulus. The exposures are predictable and under the patient's control. The patient is taught a variety of adaptive coping strategies to utilize throughout treatment.
Present study was designed for assessing the efficacy of problem solving, exposure therapy and combined therapy (both of them) in quality of life (QOL) of war-related PTSD in veterans compared to control group and compare applied treatments with each other.
MATERIALS AND METHODS
Study samples
The sample of present randomized control study was comprised of Iranian veterans in 8 years consecutive Iraq-Iran War combat, who presented with a variety of concerns to the Deployment Health Clinic of Bonyad-e-Shahid and Sepah Pasdaran between 2005 and 2006 in Tehran. The Deployment Health Clinic is structured to screen for PTSD purely or PTSD with concomitant depression by Diagnostic and Statistical Manual of Mental Disorder, 4th Edition, Text Revision diagnosis criteria and psychological interview. Participants were a random sample of men, ages 25-50 years, diagnosed with PTSD merely or PTSD with concomitant depression, who had a recorded profile in Hazrat Abolfazl clinic, Sani Khani clinic, and psychiatric Sadr Bonyad center.
In the first stage, 150 PTSD patients were selected among patient's dossiers of clinical centers belonging to Islamic Revolution Guards Corp and Bonyad in Tehran. Of 150 patients invited after sending written invitation and making phone contact, 92 participated in the explaining session and 85 volunteered to participate in the study. They were informed about the reason of the invitation, study conditions, procedures, and treatments. To make up the deficit, the dossiers were checked again, and those absent in the session were invited again. Finally, 120 patients included to the study.
Before the beginning of the study, all participants filled demographic questionnaires and gave written informed consent. According to the participant's answers, it has been programmed that patients attend therapeutically sessions twice weekly. They were randomly allocated to one of four equal interventional groups: (a) Problem solving therapy (b) exposure therapy (c) combined therapy (exposure therapy plus problem solving) (d) control group.
Study interventions
Problem solving therapy
Fifteen therapy sessions were held containing seven group sessions each lasting 2 h, and eight individual sessions each lasting 45 min. Patients were trained five steps of problem solving therapy by an expert therapist, throughout seven group sessions. At the end of the first session, patients were assessed by the questionnaires as pre-therapy tests. Individual sessions were devoted to recognizing the exact stressor situations and memories of each case. Then patients were asked to perform their learning on their own virtual problems and trying to go through each step by therapist assistance. Post-therapy tests were held at the end of 15 session and 3 months later.
Exposure therapy
This program contained 13 therapy sessions and two sessions dedicated to prior and post-therapy tests. The aim of individual sessions was to achieve annoying memories, images, and situations by focusing on and describing the details of that traumatic experience. Then relaxation is trained by the therapist and the patients were asked to repeat recalling arousing memories by some relaxation intervals. Here, again we held post-therapy tests at the end of 15 sessions and in subsequent 3 months.
Combined therapy
Seven group sessions were held to train problem solving and relaxation skills. Further individual eight sessions are devoted to learning implementation on problem solving and stressors recalling.
Study outcome variable measurement tools
QOL questionnaire
It is measured by SF-36 as a multi-purpose, short-form health survey with only 36 questions. It yields an eight-scale profile of functional health and well-being scores as well as psychometrically-based physical and mental health summary measures and a preference-based health utility index.
Global severity index
We used Symptom Checklist 90-Revised (SCL90-R) to assess the rate of psychological disorders. The SCL-90-R instrument from Pearson Assessments helps evaluate a broad range of psychological problems and symptoms of psychopathology. The instrument is also useful in measuring patient progress or treatment outcomes. This is a self-assessment test and is answered by subjects themselves. It has 90 questions and 9 scales in the following aspects: Somatization (SOM), Obsessive-Compulsive (O-C), Interpersonal Sensitivity (I-S), Depression (DEP), Anxiety (ANX), Hostility (HOS), Phobic Anxiety (PHOB), Paranoid Ideation (PAR) and Psychoticism (PSY) for assessing psychological symptoms. This checklist is widely used self-report instrument for assessing psychiatric problems and a wide range of psychopathic comorbid problems and is brief enough to be taken in only 15-20 min. The checklist has many archival databases. It is possible to measure PTSD by this instrument in a wide range of clinical and research settings. We applied GSI of this checklist in this study.
Statistical analysis
Data were analyzed using the SPSS for Windows version 16. Quantitative variables were presented by central indices (Mean and Standard error of mean) and qualities variables were presented by frequencies tables (frequency and Percentages). Independent sample t tests for comparison of quantities variables between two groups and analysis of variance for comparing quantities in more than two groups. Chi-square was used for detecting significant association between qualities variables. Two-tailed significance level of 0.05 was used to detect a difference between variables.
RESULTS
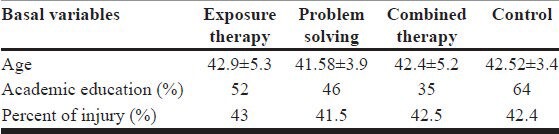
Each of four study groups was composed of 25 individuals. Overall mean age was 42.37±4.55 (34-57). Mean of age in patients of each of study groups had no significant difference [Table 1].
Table 1.
Baseline characteristics of individuals enrolled in the study
QOL and GSI between study groups before and after intervention
Mean of SF36 scores in patients in baseline was 36.4±3.2 in the group (a), 41.18±2.4 in group (b), 35.53±3.3 in group (c) and 45.9±4.6 in group (d). After study intervention mean of SF36 scores were significantly improved. Same significant improvement was seen in the mean of SF36 scores after a follow-up period.
Mean of GSI in patients in baseline was 1.78±0.3 in the group (a) 1.62±0.3 in group (b) 1.85±0.2 in group (c) and 1.5±0.3 in group (d). After study intervention mean of GSI were significantly improved. Same significant improvement was seen in the mean of GSI after a follow-up period [Table 2].
Table 2.
SF36 and GSI score in pre, post-test and follow-up period
DISCUSSION
Present study was designed for assessment of effects of cognitive behavioral therapy such as exposure therapy and problem solving on QOL of PTSD patients in veterans of Iraq-Iran war. In our study, these therapeutic modalities significantly improved both of QOL and global severity scores in them.
Pharmacotherapy and psychotherapy for treatment of PTSD patients are the focus in different studies. Among psychotherapy method, cognitive-behavioral therapy appeared to be the first line of treatment especially in chronic cases of combat-related PTSD and several studies use that for treatment of PTSD.[14] Cognitive behavioral therapy presented as an effective therapy for PTSD patients[14,15] and can cause accelerated symptoms removing.[16,17] Foa et al. believed that highest results of cognitive therapy was presented during 1st 2 months of treatment of PTSD patients.[16]
QOL suggested as one the important parts of human health.[18,19] There are some studies that discussed on QOL in mental disorders.[20,21] QOL in veterans and nonveterans of PTSD might impaired due to their disorders and in recent meta-analysis on QOL in patients with anxiety disorders, found that PTSD had main effects on QOL in them among several causes.[20] In social-material condition, studies showed that PTSD increased rate of unemployment and homelessness.[22,23,24,25] PTSD either can increase marital instability.[26]
In functioning part of QOL, PTSD accompanying with some problems such as social and interpersonal functioning,[27,28] marital function,[29] family function,[30] and occupational functioning.[28] Most of the published evidence in the literature showed that PTSD might be related to impair QOL of veterans. However, one main question was remained: How PTSD treatment can improve QOL? Some evidences showed that psychotherapy can improve psychosocial QOL.[31,32,33] Researchers work on psychosocial and physical health related QOL.[34,35,36] They showed different and even opposite findings in their research. In one of them Malik et al. reported that PTSD treatment can improved psychosocial function and had no effects on physical functioning,[34] against of this results was presented by Mueser et al.[35] and in another study by Schnurr et al. PTSD treatment did not improve physical and psychological function of health related QOL.[36]
Finally, we had another question: How we can apply evidences of cognitive behavioral therapy effects on QOL to design treatment modalities for PTSD patients? We need a large sample studies for psychological assessment of PTSD patients to providing basic data. Clinicians may need to collaboration with a group of specialist including, rehabilitation specialists, social workers to present better treatment for PTSD patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- 2.van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: The complexity of adaptation of trauma. Am J Psychiatry. 1996;153:83–93. doi: 10.1176/ajp.153.7.83. [DOI] [PubMed] [Google Scholar]
- 3.Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: A prospective study. Am J Psychiatry. 1996;153:219–25. doi: 10.1176/ajp.153.2.219. [DOI] [PubMed] [Google Scholar]
- 4.Vermetten E, Bremner JD. Circuits and systems in stress. II. Applications to neurobiology and treatment in posttraumatic stress disorder. Depress Anxiety. 2002;16:14–38. doi: 10.1002/da.10017. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Breslau N. Epidemiological risk factors for trauma and PTSD. In: Yehuda R, editor. Washington, DC: American Psychiatric Press, Inc; 1999. [Google Scholar]
- 6.Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC, et al. Posttraumatic stress disorder and depression in battle-injured soldiers. Am J Psychiatry. 2006;163:1777–83. doi: 10.1176/ajp.2006.163.10.1777. [DOI] [PubMed] [Google Scholar]
- 7.Spiro A, 3rd, Schnurr PP, Aldwin CM. Combat-related posttraumatic stress disorder symptoms in older men. Psychol Aging. 1994;9:17–26. doi: 10.1037//0882-7974.9.1.17. [DOI] [PubMed] [Google Scholar]
- 8.Sutker P, Madeline U, NA A. Clinical and research assessment of posttraumatic stress disorder: A conceptual overview. Psychol Assess. 1991;3:520–30. [Google Scholar]
- 9.Herrmann N, Eryavec G. Posttraumatic stress disorder in institutionalized World war II veterans. Am J Geriatr Psychiatry. 1999;2:324–31. doi: 10.1097/00019442-199402040-00007. [DOI] [PubMed] [Google Scholar]
- 10.Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, et al. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. J Consult Clin Psychol. 1999;67:13–8. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- 11.Rothbaum BO, Meadows EA, Resick P, Foy DW. Cognitive – Behavioral therapy. In: Foa EB, Keane TM, Friedman M, editors. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. New York: Guilford Press; 2000. [Google Scholar]
- 12.Harvey AG, Bryant RA, Tarrier N. Cognitive behaviour therapy for posttraumatic stress disorder. Clin Psychol Rev. 2003;23:501–22. doi: 10.1016/s0272-7358(03)00035-7. [DOI] [PubMed] [Google Scholar]
- 13.Sherman JJ. Effects of psychotherapeutic treatments for PTSD: A meta-analysis of controlled clinical trials. J Trauma Stress. 1998;11:413–35. doi: 10.1023/A:1024444410595. [DOI] [PubMed] [Google Scholar]
- 14.Foa EB, Meadows EA. Psychosocial treatments for posttraumatic stress disorder: A critical review. Annu Rev Psychol. 1997;48:449–80. doi: 10.1146/annurev.psych.48.1.449. [DOI] [PubMed] [Google Scholar]
- 15.Harkins K, Tartter PI, Hermann G, Squitieri R, Brower ST, Keller RJ. Multivariate analysis of roentgenologic characteristics and risk factors for nonpalpable carcinoma of the breast. J Am Coll Surg. 1994;178:149–54. [PubMed] [Google Scholar]
- 16.Foa EB, Hearst-Ikeda D, Perry KJ. Evaluation of a brief cognitive-behavioral program for the prevention of chronic PTSD in recent assault victims. J Consult Clin Psychol. 1995;63:948–55. doi: 10.1037//0022-006x.63.6.948. [DOI] [PubMed] [Google Scholar]
- 17.Foa EB, Zoellner LA, Feeny NC. An evaluation of three brief programs for facilitating recovery after assault. J Trauma Stress. 2006;19:29–43. doi: 10.1002/jts.20096. [DOI] [PubMed] [Google Scholar]
- 18.Gladis MM, Gosch EA, Dishuk NM, Crits-Christoph P. Quality of life: Expanding the scope of clinical significance. J Consult Clin Psychol. 1999;67:320–31. doi: 10.1037//0022-006x.67.3.320. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan RM. The significance of quality of life in health care. Qual Life Res. 2003;12(Suppl 1):3–16. doi: 10.1023/a:1023547632545. [DOI] [PubMed] [Google Scholar]
- 20.Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clin Psychol Rev. 2007;27:572–81. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Quilty LC, Van Ameringen M, Mancini C, Oakman J, Farvolden P. Quality of life and the anxiety disorders. J Anxiety Disord. 2003;17:405–26. doi: 10.1016/s0887-6185(02)00225-6. [DOI] [PubMed] [Google Scholar]
- 22.Magruder KM, Frueh BC, Knapp RG, Johnson MR, Vaughan JA, 3rd, Carson TC, et al. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. J Trauma Stress. 2004;17:293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- 23.Savoca E, Rosenheck R. The civilian labor market experiences of Vietnam-era veterans: The influence of psychiatric disorders. J Ment Health Policy Econ. 2000;3:199–207. doi: 10.1002/mhp.102. [DOI] [PubMed] [Google Scholar]
- 24.Smith MW, Schnurr PP, Rosenheck RA. Employment outcomes and PTSD symptom severity. Ment Health Serv Res. 2005;7:89–101. doi: 10.1007/s11020-005-3780-2. [DOI] [PubMed] [Google Scholar]
- 25.O’Connell MJ, Kasprow W, Rosenheck RA. Rates and risk factors for homelessness after successful housing in a sample of formerly homeless veterans. Psychiatr Serv. 2008;59:268–75. doi: 10.1176/ps.2008.59.3.268. [DOI] [PubMed] [Google Scholar]
- 26.Riggs DS, Byrne CA, Weathers FW, Litz BT. The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. J Trauma Stress. 1998;11:87–101. doi: 10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]
- 27.Amaya-Jackson L, Davidson JR, Hughes DC, Swartz M, Reynolds V, George LK, et al. Functional impairment and utilization of services associated with posttraumatic stress in the community. J Trauma Stress. 1999;12:709–24. doi: 10.1023/A:1024781504756. [DOI] [PubMed] [Google Scholar]
- 28.Norman SB, Stein MB, Davidson JR. Profiling posttraumatic functional impairment. J Nerv Ment Dis. 2007;195:48–53. doi: 10.1097/01.nmd.0000252135.25114.02. [DOI] [PubMed] [Google Scholar]
- 29.Dekel R, Solomon Z. Marital relations among former prisoners of war: Contribution of posttraumatic stress disorder, aggression, and sexual satisfaction. J Fam Psychol. 2006;20:709–12. doi: 10.1037/0893-3200.20.4.709. [DOI] [PubMed] [Google Scholar]
- 30.Cohen LR, Hien DA, Batchelder S. The impact of cumulative maternal trauma and diagnosis on parenting behavior. Child Maltreat. 2008;13:27–38. doi: 10.1177/1077559507310045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. J Consult Clin Psychol. 2002;70:1067–74. doi: 10.1037//0022-006x.70.5.1067. [DOI] [PubMed] [Google Scholar]
- 32.Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M, Herbert C, et al. A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Arch Gen Psychiatry. 2003;60:1024–32. doi: 10.1001/archpsyc.60.10.1024. [DOI] [PubMed] [Google Scholar]
- 33.Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. J Consult Clin Psychol. 2005;73:953–64. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- 34.Malik ML, Connor KM, Sutherland SM, Smith RD, Davison RM, Davidson JR. Quality of life and posttraumatic stress disorder: A pilot study assessing changes in SF-36 scores before and after treatment in a placebo-controlled trial of fluoxetine. J Trauma Stress. 1999;12:387–93. doi: 10.1023/A:1024745030140. [DOI] [PubMed] [Google Scholar]
- 35.Mueser KT, Rosenberg SD, Xie H, Jankowski MK, Bolton EE, Lu W, et al. A randomized controlled trial of cognitive-behavioral treatment for posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 2008;76:259–71. doi: 10.1037/0022-006X.76.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, et al. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: Results from a department of veterans affairs cooperative study. Arch Gen Psychiatry. 2003;60:481–9. doi: 10.1001/archpsyc.60.5.481. [DOI] [PubMed] [Google Scholar]


