Abstract
Background:
The presence of intestinal parasites in a population group is indicative of lack of proper sanitation, low economic standards and poor educational background.
Aim:
To determine the prevalence of intestinal parasites in primary school children of Mthatha, South Africa and relate this to their socio-economic status.
Subjects and Methods:
The study population was randomly selected from four governmental schools, rural and urban, from April 2009 to September 2009. A total of 162 learners (85 boys and 77 girls) participated in this survey. Parasitological data were collected by analyzing stool samples using Formalin ethyl-acetate concentration technique. Socio-economic and epidemiologic data were collected by means of a pre-tested structured questionnaire, covering the important relevant aspects, in this descriptive, cross sectional and analytical study. Data were analyzed descriptively and inferentially with SPSS satistical software, and P values of <0.05 were considered as significant.
Results:
Out of 162 learners analyzed, 64.8% (105/162) stool samples were positive for ova and cysts of which 57.4% (93/162) were known pathogenic parasites. The most common parasite was Ascaris lumbricoides 29.0% (47/162), followed by Giardia lamblia 9.9% (16/162) and Entamoeba histolytica/dispar 6.8% (11/162) (Other parasites observed but at lower rates of occurrence were Iodamoeba butschlii, Trichuris trichiura, Hymenolepis nana, Taenia spp, Chilomastix mesnili, and Fasciola spp. Our findings showed no significant difference in parasitic infections between urban and rural learners, gender and the age of these learners. Significant associations between parasitic infections and parents’ unemployment and lower education were observed.
Conclusion:
Prevalence of worm infestation was more than 50%; therefore, there was a need for mass de-worming of school children in these communities and also a need for other public health interventions like health education programs and improvement of sanitation.
Keywords: Children, Intestinal parasites, Parasite infection, Prevalence
Introduction
Intestinal parasitic infections are amongst the most common infections throughout the world. It is estimated that some 3.5 billion people are affected, and that 450 million are ill as a result of these infections, the majority being children.[1] These infections are regarded as a serious public health problem, as they can cause iron deficiency anemia, growth retardation in children and other physical and mental health conditions.[1,2,3,4,5] The high prevalence of these infections is closely correlated with poverty, poor environmental hygiene and impoverished health services.[6,7,8]
The fecal oral route is significant in the transmission of parasitic infections to human via poor personal hygiene and environmental conditions such as contaminated soil and water sources.[9] Worm infection is believed to be imposing an unnecessary burden on many South African children and on the overall cost of health-care.[10] Disadvantaged children are the most affected, especially those who live in densely populated and under-serviced urban informal settlements as well as in some rural areas.[10] World Health Assembly (WHA) member states, including South Africa, were urged to implement regular, non-selective de-worming of school-age children and young women by 2010 in areas where the prevalence of worm infestation is 50% or more.[11]
Currently, there is scarcity of available literature regarding the prevalence of parasitic infections from the Province; therefore, little is known about intestinal parasitic infections in the inhabitants of the Eastern Cape, in particular those of Mthatha. The study was carried out to fill that gap. Therefore, the aim of this study was to determine the prevalence of intestinal parasites in urban and rural primary school children of Mthatha and relate this to their socio-economic status.
Subjects and Methods
Study design and setting
This descriptive, analytical, cross-sectional study was carried out from April 2009 to September 2009 in Mthatha. Mthatha (formerly Umtata), is the main town of the King Sabata Dalindyebo Local Municipality in the Oliver Reginald Tambo District of the Eastern Cape Province in South Africa [Figure 1]. The Eastern Cape Province is divided into a metropolitan city, six districts, and 38 local municipalities. Local municipalities cover both towns and rural areas. OR Tambo district municipality lies in the North-East region of the Eastern Cape. Its boundaries stretch from the Indian Ocean in the east to the rolling hills of the former Transkei in the west, to the Mbhashe River in the south and KwaZulu-Natal in the north. It has the second-highest population, estimated at 1.5-million and a population density of 90/km2. The district covers an area of about 16 000 km2, about 9% of the province. Mthatha, in the King Sabata Dalindyebo Local Municipality is mostly surrounded by rural areas and some informal settlements.
Figure 1.

Map of Mthatha, Eastern cape province, South Africa. http://www/routes.co.za/maps/rsa.ipg
Ethical clearance and informed consent
The research project was approved by the Ethics Committee of Walter Sisulu University with ethical approval number 0005/08. Written informed consent was received from parents or guardians as all of our participants were young.
Study population and sample
Four schools (MKT, MHL, NCA and TPN) were randomly selected from urban and rural schools of Mthatha. They were all governmental schools. Learners were randomly selected from the four schools, using the random numbers. A total of 162 learners completed the questionnaire and provided stool samples. In order to inform schools and parents about the survey, principals of the relevant schools were approached and they called meetings where the relevant grade teachers and parents were present. The subject information sheet as well as the consent form were discussed and explained. Instructions on how to collect the stool samples were also explained to the parents and copies were given to them.
Questionnaire forms
Both socio-economic and epidemiological data were collected by means of a questionnaire.
The questionnaire was designed to address three areas: (i) socio-demographic data: Age, sex and residence; (ii) environmental factors: Occupation and education level of the parent's, number of rooms and people in the house, if there was any toilet in the house, type of toilet, household water source and hygiene practices (washing of hands after using toilet); (iii) personal complaints of the learner: Lack of appetite, abdominal pain/distention, peri-anal itching and history of parasitic infections and treatment. Teachers assisted learners whose parents could not read or write in filling the forms and answering the questionnaire. P values were determined using Chi Square method.
Stool specimen collection and investigation
A universal specimen jar with no preservative, labeled with a unique identification number and the name of the learner was distributed to each participating learner. All mothers of participants were asked to collect an early morning stool sample from their child. The samples were then transported in cooler bags to the Medical Microbiology Laboratory at the Walter Sisulu University, within 2 h of collection. Stool samples were processed using Formalin ethyl-acetate concentration technique. After concentration a drop of sediment was placed onto a microscope slide and covered with a cover-slip. The entire cover-slip was examined with a ×10 objective for large parasites and ×40 objective for smaller parasites and to study the morphology of the organism. Results were recorded on a corresponding learner survey form and quantified as +; ++ or +++ according to the parasite load (1-5 parasites/100 hpf = +; 1-5 parasites/10 hpf = ++ and 1−≥ 5parasites/hpf as +++), (hpf means high power field). We cannot give any reference for this but we may state that this grading was arbitrarily decided by us. Specimen examination was performed by a technologist and a microbiologist. Quality control was carried out by split sampling and parallel staining of known positive samples of fecal parasites.
Statistical analysis
Statistical significance between the prevalence of intestinal parasites and socioeconomic status determined using the Chi square test and P value less than 0.05 with the help of SPSS software, South Africa.
Results
Characteristics of study participants
Out of 200 learners registered to participate in the survey, 38 (21 girls and 17 boys) did not take part, (23 did not return the questionnaire and 15 did not provide stool samples). Consequently, a total of 162 learners were examined for intestinal parasites (85 boys and 77 girls) between 4 years and 11 years of age, mean = 7(1). The response rate of boys was 52.5% and a 47.5% rate was seen in girls.
Prevalence by socio-demography
There was no significant difference in the prevalence of intestinal parasites between urban and rural learners (P = 0.30). No significant difference was observed in gender between urban (P = 0.30) and rural (P = 0.20) learners as well as between age groups in urban (P = 0.90) and rural (P = 0.40) learners. Prevalence of intestinal parasites by demographic characteristics is given in Table 1.
Table 1.
Prevalence of intestinal parasites by socio-demographic characteristics
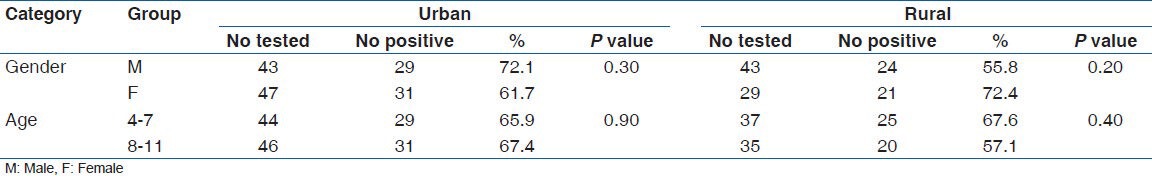
Out of 90 learners from an urban area 66.7% (60/90) were positive for intestinal parasites and 33.3% (30/90) negative. From 72 rural learner participants 62.5% (45/72) were positive for parasites and 37.5% (27/72) negative.
Distribution of parasites
Ascaris lumbricoides was the most common pathogen observed and it was found in 29.0% (47/162) learners, followed by Giardia lamblia 9.9% (16/162) and Entamoeba histolytica/dispar 6.8% (11/162). Other pathogens isolated, though in lower numbers, were Hymenolepis nana 4.9% (8/162), Iodamoeba butschlii 3.1% (5/162), Trichuris trichiura 3.7% (6/162), Taenia spp 1.6% (3/162), Chilomastix mesnili 1.2% (2/162) and Fasciola spp 0.6% (1/162). There were 26.0% (42/162) cases of Entamoeba coli, 19.1% (31/162) of Endolimax nana and 13.0% (21/162) of Blastocystis hominis. Eggs of Schistosoma haematobium were observed in one case. As far as the distribution of both pathogenic and non-pathogenic parasites among the learners of the four primary schools there was no significant statistical difference.
Correlations between parasites and socio-economic status
Statistical significance between intestinal parasites and socio-economic status of the learners are given in Table 2. The survey revealed a very high rate of unemployment among the parents in these communities, urban (76.7%) and rural (65.3%). A statistically significant correlation between unemployment and incidence of parasites was observed in urban learners (P = 0.03). The level of education of the mother was also taken into consideration since it is the mother who looks after the children. A higher prevalence of infection was noted in learners whose mothers had primary school education and the prevalence rate was higher in rural learners (79.5%) than urban (69.0%). There was a significant relation between a mother's level of education and parasite infection (P < 0.01) among rural learners.
Table 2.
Statistical significance between intestinal parasites and socio-economic status
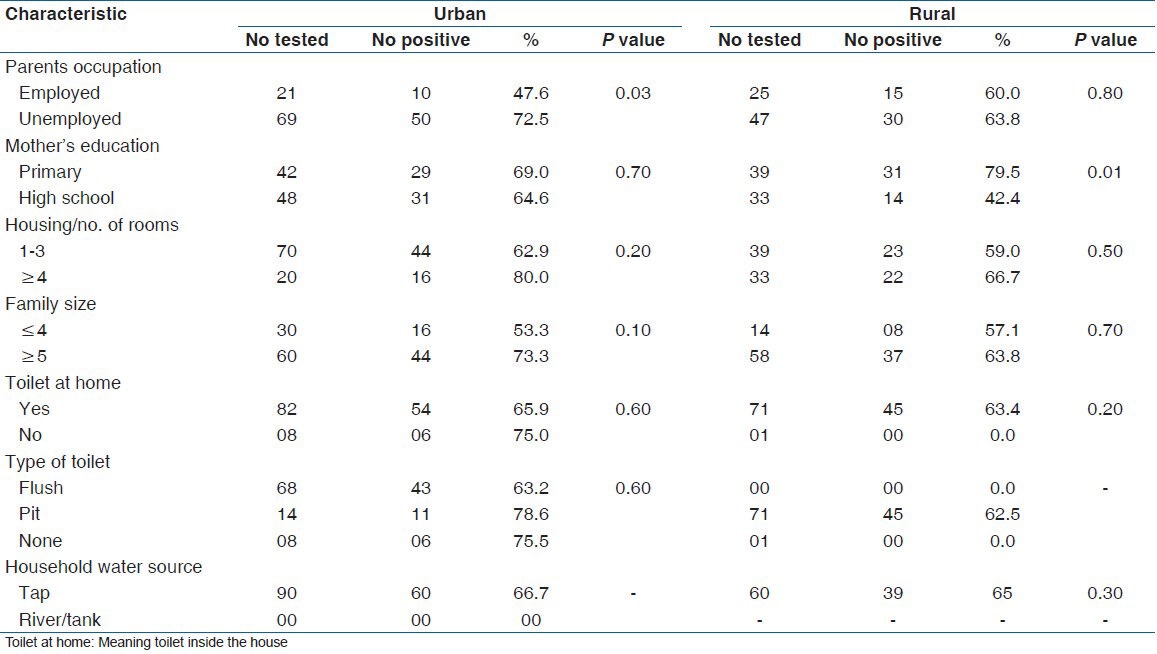
There was no statistical significant difference in parasitic infection between urban and rural learners in the following areas: Number of rooms in the house, family size, type of toilet, and the water source. The most frequent complaint related to any parasite infection was a loss of appetite (60.4%) in urban and (62.5%) in rural learners followed by perianal itching (urban - 57.7%) and (rural - 64.7%) and abdominal pain/distension (urban - 67.7%) and (rural - 48.7%). Learners who said they were previously treated for worms, 71.4% of urban and 62.7% of rural learners were still positive for intestinal parasites.
Polyparasitism
Among the infected school children, 43.8% (46/105) were infected by a single intestinal parasite and 56.2% (59/105) had multiple infections. In the multiple infection groups, the most common combinations were those of A. lumbricoides/E. coli and E. coli/E. nana both at 8.5%; followed by A. lumbricoides/E. coli/E. nana at 6.8%.
Discussion
The study revealed that more than 60% of the learners in four primary schools of Mthatha were positive for intestinal parasitic infections. The demographic data indicated no significant difference between the incidence of parasites and the residing area, i.e. urban and rural. This may be due to the fact that there were two schools from urban areas, one was mainly attended by children from a nearby village and the other one by children from a nearby informal settlement; hence, we observed no significant difference in the infection rate between urban and rural learners. The study also revealed a very high rate of unemployment among the parents in these communities. We observed that there was a relation between unemployment and incidence of parasites as more learners whose parents were unemployed tested positive for parasites and a more significant correlation was observed in urban learners. This was also true for those pupils whose parents had a primary school level of education and where there was overcrowding.
Urban males had a higher prevalence than females, whereas in rural participants females were more infected than males. There was no significant relation detected between the parasitic infections and the age of the learners in both urban and rural areas.
A. lumbricoides and T. trichiura were the most common geohelminths observed. A. lumbricoides had the highest prevalence rate. Similarly, in a study conducted in Lesotho, a neighboring country of South Africa in the northern part of Mthatha, a high prevalence rate of A. lumbricoides was reported among patients attending Tebellong hospital, in Qacha's Nek.[12] Samie et al.,[13] also reported higher rates of infection by Ascaris in Cape Town, South Africa. Ekpo et al., found that A. lumbricoides was the most common infecting species in the three schools they surveyed.[14]
We found the pathogenic protozoan, G. lamblia to be more prevalent in rural learners than urban which correlate with Ouattara et al.,[14] We could not distinguish E. histolytica from E. dispar as it is only electron microscope that can show the difference. H. nana was encountered in urban schools, which is similar to what Adams et al.,[11] in Cape Town reported.
No hookworms were observed in our study, which is consistent with the findings of Mehraj et al.,[8] E. coli and E. nana were the most commonly observed protozoan parasites. This finding correlates with what Kwitshana et al.,[3] found in KwaZulu Natal Province.
Geohelminth infections with Trichuris were of low prevalence in all four schools, which is contrary to the findings of Ekpo et al.,[6] where prevalence of T. trichiura was higher among school children in both rural and urban government schools except for private schools.
An interesting finding of S. haematobium egg was encountered in one urban learner. This parasite is normally found in the urine of infected persons and observed in urine analysis.
Charcot-Leyden crystals were seen in a few stool specimens. These crystals may also occur in sputum and in tissues.[15]
As this is the first study in the region to provide comprehensive information related to prevalence of intestinal parasites in primary school children, recommendations from the study will assist government health officials in policy development, interventions such as deworming and health education programs. Public health awareness campaigns will also be recommended as a high rate of re-infection was observed.
Limitation of the study: One limitation of this study was that the sample size was not very large and we could cover only four schools in Mthatha. A larger sample from more schools is necessary before generalizing the results to the whole population. Another limitation of the study was that we did not perform the direct stool examination or collect swabs from children with perianal itching, which may have resulted in some underreporting of parasites.
Conclusion
Prevalence of worm infestation among our school children is high. Geohelminths were most common parasites found in Mthatha school children.
Recommendations: WHA member states, including South Africa, were urged to implement regular, non-selective de-worming of school-age children and young women by 2010 in areas where the prevalence of worm infestation is 50% or more. Therefore, there is a need for mass de-worming of school children in these communities. There is also a need for public health awareness programs and adequate treatment of food to reduce the incidence of intestinal parasitic infections. More work still needs to be carried out to reach more of these communities.
Acknowledgments
The authors would like to thank the principals, educators, and learners of the four schools for their participation in the survey. We are grateful to Parasitology Unit of the National Institute for Communicable diseases (NICD) for their assistance especially in the identification of protozoan cysts. Many thanks also go to Mr. Hoyi, an NHLS-Mthatha Medical Technologist, for co-reading our samples. We also thank the faculty of Health Sciences, Walter Sisulu University and the National Health laboratory Services (NHLS), South Africa.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Okyay P, Ertug S, Gultekin B, Onen O, Beser E. Intestinal parasites prevalence and related factors in school children, a western city sample – Turkey. BMC Public Health. 2004;4:64. doi: 10.1186/1471-2458-4-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ostan I, Kilimcioğlu AA, Girginkardeşler N, Ozyurt BC, Limoncu ME, Ok UZ. Health inequities: Lower socio-economic conditions and higher incidences of intestinal parasites. BMC Public Health. 2007;7:342. doi: 10.1186/1471-2458-7-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwitshana ZL, Tsoka JM, Mabaso ML. Intestinal parasitic infections in adult patients in KwaZulu-Natal. S Afr Med J. 2008;98(Suppl 9):709–11. [PubMed] [Google Scholar]
- 4.Alaofè H, Zee J, Dossa R, O’Brien HT. Intestinal parasitic infections in adolescent girls from two boarding schools in southern Benin. Trans R Soc Trop Med Hyg. 2008;102:653–61. doi: 10.1016/j.trstmh.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Elliott AM, Kizza M, Quigley MA, Ndibazza J, Nampijja M, Muhangi L, et al. The impact of helminths on the response to immunization and on the incidence of infection and disease in childhood in Uganda: Design of a randomized, double-blind, placebo-controlled, factorial trial of deworming interventions delivered in pregnancy and early childhood ISRCTN32849447. Clin Trials. 2007;4(Suppl 1):42–57. doi: 10.1177/1740774506075248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekpo UF, Odoemene SN, Mafiana CF, Sam-Wobo SO. Helminthiasis and hygiene conditions of schools in Ikenne, Ogun State, Nigeria. PLoS Negl Trop Dis. 2008;2(Suppl 1):e146. doi: 10.1371/journal.pntd.0000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uga S, Rai SK, Kimura K, Ganesh R, Kimura D, Wakasugi M, et al. Parasites detected from diarrheal stool samples collected in Nepal. Southeast Asian J Trop Med Public Health. 2004;35(Suppl 1):19–23. [PubMed] [Google Scholar]
- 8.Mehraj V, Hatcher J, Akhtar S, Rafique G, Beg MA. Prevalence and factors associated with intestinal parasitic infection among children in an urban slum of Karachi. PLoS One. 2008;3(Suppl 11):e3680. doi: 10.1371/journal.pone.0003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyarango RM, Aloo PA, Kabiru EW, Nyanchongi BO. The risk of pathogenic intestinal parasite infections in Kisii Municipality, Kenya. BMC Public Health. 2008;8:237. doi: 10.1186/1471-2458-8-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fincham J, Dhansay A. Worms in SA's Children. MRC Policy Brief. 2006. [Accessed 2012 Jul 28]. p. 2. Available from: http://www.mrc.ac.za/policybriefs/worms.pdf .
- 11.Adams VJ, Markus MB, Adams JF, Jordaan E, Curtis B, Dhansay MA, et al. Paradoxical helminthiasis and giardiasis in Cape Town, South Africa: Epidemiology and control. Afr Health Sci. 2005;5:276–80. doi: 10.5555/afhs.2005.5.3.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oguntibeju OO. Parasitic infestation and anaemia: The prevalence in a rural hospital setting. West Indian Med J. 2003;4:210–2. [Google Scholar]
- 13.Samie A, Guerrant RL, Barrett L, Bessong PO, Igumbor EO, Obi CL. Prevalence of intestinal parasitic and bacterial pathogens in diarrhoeal and non-diarroeal human stools from Vhembe district, South Africa. J Health Popul Nutr. 2009;27(Suppl 6):739–45. doi: 10.3329/jhpn.v27i6.4325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ouattara M, N’guéssan NA, Yapi A, N’goran EK. Prevalence and spatial distribution of Entamoeba histolytica/dispar and Giardia lamblia among schoolchildren in Agboville area (Côte d’Ivoire) PLoS Negl Trop Dis. 2010;4(Suppl 1):e574. doi: 10.1371/journal.pntd.0000574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.John DT, Petri WA., Jr . 9th ed. Missouri: Elsevier Sabre Foundation; 2006. Markell and Voge's Medical Parasitology. [Google Scholar]


