Abstract
Background:
The amount of time a patient waits to be seen is one factor which affects utilization of healthcare services. Patients perceive long waiting times as barrier to actually obtaining services and keeping patients waiting unnecessarily can be a cause of stress for both patient and doctor.
Aim:
This study was aimed at assessing the determinants of patients’ waiting time in the general outpatient department (GOPD) of a tertiary health institution in northern Nigeria.
Subjects and Methods:
This descriptive cross-sectional study was carried out among new patients attending the GOPD of the Usmanu Danfodiyo University Teaching Hospital, Sokoto, North Western Nigeria. A structured questionnaire was used to elicit information from 100 patients who were recruited into the study using a convenience sampling method. Data collected were entered and analyzed using Statistical Package for Social Sciences version 17; Chi-square test was used to compare differences between proportions with the level of statistical significance set at 5% (P < 0.05).
Results:
Sixty-one percent (59/96) of the respondents waited for 90-180 min in the clinic, whereas 36.1% (35/96) of the patients spent less than 5 min with the doctor in the consulting room. The commonest reason for the long waiting time in the GOPD was the large number of patients with few healthcare workers.
Conclusion:
There is an urgent need to increase the number of health workers in the GOPDs which serves as the gate way to the hospital if the aims of the Millennium Development Goals are to be realized.
Keywords: General outpatient department, Patients, Waiting time
Introduction
Patients spend substantial amount of time in the clinics waiting for services to be delivered by physicians and other allied health professionals. The degree to which health consumers are satisfied with the care received is strongly related to the quality of the waiting experience. Healthcare organizations that strive to deliver exceptional services must effectively manage their clinic wait.[1] Failure to incorporate consumer-driven features into the design of wait experience could lead to patient and provider dissatisfaction.
Waiting time refers to the time a patient waits in the clinic before being seen by one of the clinic medical staff.[2] Patient clinic waiting time is an important indicator of quality of services offered by hospitals.[3] The amount of time a patient waits to be seen is one factor which affects utilization of healthcare services. Patients perceive long waiting times as a barrier to actually obtaining services.[4] Keeping patients waiting unnecessarily can be a cause of stress for both patient and doctor. Waiting time is a tangible aspect of practice that patients will use to judge health personnel, even more than their knowledge and skill.
The Institute of Medicine (IOM) recommends that, at least 90% of patients should be seen within 30 min of their scheduled appointment time.[5] This is, however, not the case in most developing countries, as several studies have shown that patients spend 2-4 h in the outpatient departments before seeing the doctor.[6,7,8] A source of dissatisfaction with health care reported by patients is having to wait a long period of time in the clinic,[9] and several studies have documented the negative association between increased waiting time and patient satisfaction with primary care.[10,11]
The duration of waiting time varies from country to country, and even within country it varies from center to center. Long waiting times have been reported in both developed and developing countries. In the USA, an average waiting time of about 60 min was found in Atlanta,[12] and an average of 188 min in Michigan.[13]
In Nigeria, an average waiting time of about 173 min was found in Benin,[9] while in University College Hospital Ibadan, a mean waiting time of 1 h 13 min was observed.[14]
Time spent waiting is a resource investment by the patient for the desired goal of being seen by the physician and therefore may be moderated by the outcome. This study aimed at assessing the determinants of patients’ waiting time in the general outpatient department (GOPD) of a tertiary health institution in northern Nigeria.
Subjects and Methods
Study area
This study was carried out between February 2011 and July 2011 at the GOPD of Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria. The teaching hospital is one of the tertiary health institutions in the state and acts as a referral for patients in the north western part of Nigeria and from neighboring Niger Republic.
Sample size estimation
The minimum sample size was determined using the formula for estimating required sample size in a population less than 10,000.[15]
Nf = n/1+ (n/N)
Value of n was calculated using the formula n = Z2pq/d2
where n = sample size, Z = standard normal deviate at 95% confidence level = 1.96, P = prevalence of the factor under study, 84% (0.84) from a previous study,[7] q = complementary factor for q = 1 – p, N = average number of targeted population (i.e., average number of patients attending GOPD daily) =150, nf = minimum required sample size (for population less than 10,000), d = precision/tolerable margin of error = 5% (0.05).
Therefore, minimum required sample size was calculated to be 96; however, the sample size was increased to 100 for the study.
Subjects and methods
The study was descriptive cross-sectional in design involving all new patients seen at the GOPD. Structured questionnaire and waiting time assessment card were used to elicit information on socio-demographic characteristics of patients, time spent before registration, time spent in the waiting area, and time spent with a doctor. Trained health personnel assisted respondents who could not read or write in completing the questionnaire.
The questionnaire was pre-tested at the GOPD of a specialist hospital located some distance from the hospital. Only new patients presenting to the GOPD for the first time and who gave their consent to participate in the study were selected (inclusion criteria) while critically ill patients were excluded from the study. Approval to carry out the study was also obtained from the ethical committee of the teaching hospital.
A total of 100 consenting patients were recruited into the study using a systematic sampling technique after calculating the sampling interval:
where K is the sampling interval,
K = 150/100
K = 1.50
This was, however, approximated to 2.
Based on the above sampling interval, the systematic sampling technique was carried out as follows:
Simple random sampling was done for the first two patients to get the starting point.
Thereafter, every other new patient that came to the clinic was enrolled in the study until the required sample size was obtained.
Four respondents however, opted out of the study, giving a response rate of 96%.
Data analysis
The data generated were entered and analyzed using statistical package for social sciences version 17.0 (Chicago, IL, USA) and Microsoft Excel 2007. Quantitative and qualitative statistical variables were cross tabulated; Chi-square test was used to compare proportions, whereas the Student t-test was used to compare means. The level of statistical significance was set at 95% confidence interval.
Results
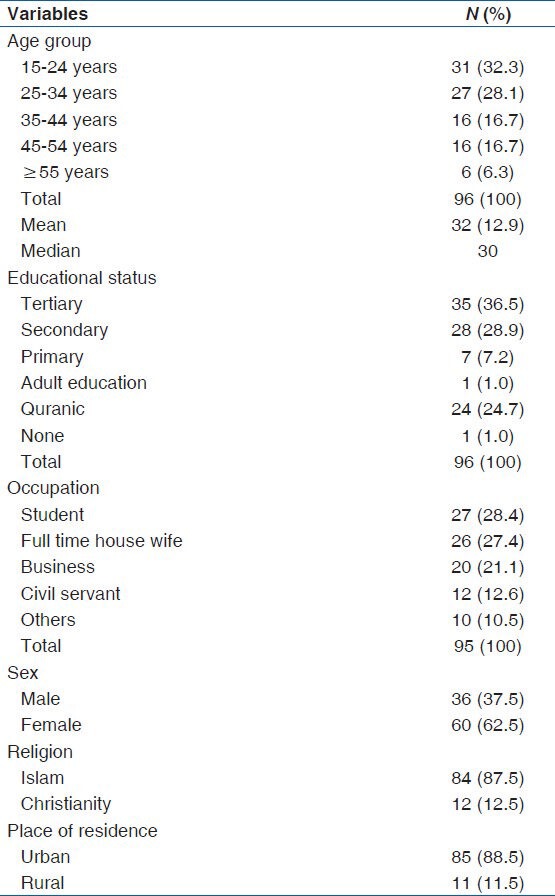
The ages of the respondents (N = 96) ranged from 15 to 70 years, with a mean age of 33 (13) years. Female respondents accounted for 62.5% (60/96) whereas males accounted for 37.5% (36/96) of those surveyed. Twenty-eight point one percent the respondents (28.1%) (27/96) were students, whereas 12.6% (12/96) of them were civil servants; 12.5% (12/96) of the respondents were engaged in one business or the other, 36.5% (35/96) had up to tertiary education while only one subject had no form of education [Table 1].
Table 1.
Socio-demographic characteristics of study subjects
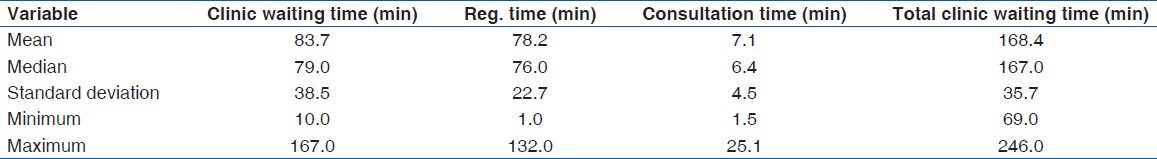
Sixty-one percent (59/96) respondents waited between 90 and 180 min in the clinic (from entry to exit), whereas 36.5% (35/96) waited for more than 180 min with a mean total clinic waiting time (TCWT) of 168 (35) min. Seventy-four percent (71/96) of the respondents waited between 60 and 120 min to be registered, whereas 10.3% (10/96) waited for more than 120 min with a mean (SD) registration time of 78.22 (22) min. With regards the consultation time, 36.1% (35/96) respondents spent less than 5 min with the doctor, whereas only 19.6% (19/96) spent more than 10 min with the doctor. The mean consultation time with the doctor was 7 (4) min.
Out of the 96 respondents, 76 (79%) of them felt they had waited for too long and reasons adduced for the long waiting period included too many patients as revealed by 44.7% (34/76) of the respondents, availability of few doctors in the clinic to attend the numerous patients (36% [27/76]), few filing and record clerks (12% [9/76]), and jumping of queue by patients or staff members (8% [6/76]) [Table 2].
Table 2.
Duration of waiting time
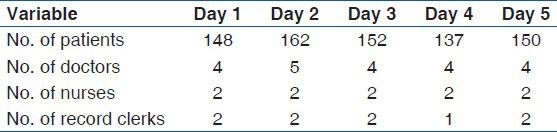
In terms of personnel attending to patients in the clinic, there were only 4 doctors, 2 nurses, and 2 record clerks who attended to 148 patients on day 1, while on the 2nd day, the number of patients who were seen at the clinic was even higher (162). On an average, only 4 doctors and 2 record clerks attended to about 150 patients on each day [Table 3].
Table 3.
Distribution of personnel in the clinic
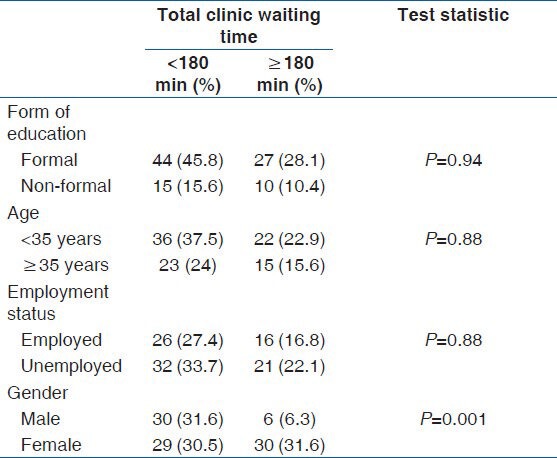
Cross tabulation between TCWT and form of education (whether formal or non-formal) showed that there was no statistically significant association between TCWT and form of education (P = 0.94).
Similarly, age and employment status of the respondents had no statistical association with TCWT (P = 0.88), whereas there was a significant association between TCWT and gender of respondents (P = 0.001) [Table 4]. While waiting to be attended to, 65.6% (63/96) of the respondents engaged in chatting with each other, while a few others (7.3%) engaged in reading newspapers or magazines. Among the study subjects, 43.8% (42/96) would have preferred listening to health talks on important health issues, while 33.3% (32/96) would have preferred watching television if available. About 65% (62/96) of the respondents said they would recommend the center to others.
Table 4.
Relationship between total clinic waiting time and some socio-demographic factors
Discussion
The mean (SD) age of respondents was 33 (12.9) years, which is low compared to 38 years and 45 years obtained in similar studies.[5,16] The lower mean age observed in this study could be related to the fact that 56.3% (54/96) of the respondents were below the age of 35 years.
Sixty-one percent of the patients waited between 90 and 180 min in the clinic, in contrast to the observation made in a previous study, where 61.2% of the patients were seen within 61-300 min.[8] The mean TCWT from entry to time of leaving the clinic was found to be 168 (35.7) minutes. This finding is similar to the findings in a Teaching hospital in Nigeria, where an average waiting time of 173 min was observed,[8] and in Trinidad and Tobago, where waiting time of 160 min was recorded.[7] These long waiting times could be a reflection of what happens in most developing countries, where there is a dearth of medical doctors, resulting in low doctor – patient ratio. Patients in developing countries experience long waiting times because of the imbalance in the doctor – patient ratio; thus, health facilities are unable to meet the recommendations of the IOM, that at least 90% of patients should be seen within 30 min of their scheduled appointment time.[5] The finding is, however, at variance with the waiting time of 74 min found in Ibadan, Nigeria,[14] in a nurse managed clinic in the USA,[18] and in a Community hospital in China.[19] Regarding respondents’ perceived waiting time, 70% (67/100) of the respondents felt they had waited for more than 2 h in the clinic, which is similar to the observation made in a previous study, where 71.8% of the respondents felt their waiting time was prolonged.[20]
The consultation time ranged from 1 to 25 min, which is similar to the findings from a previous study, where a range of 1-26 min was observed.[21] The mean consultation time was 7 min, with 43.3% (42/96) of the respondents spending 5-10 min. The mean consultation time observed in this study is much higher than the 3.4 min observed in a previous study.[21] The reason for this higher consultation time may not be unconnected to the fact that the study area is a tertiary teaching hospital where the doctors use the opportunity of their interaction with patients to teach medical students undergoing various trainings, thus increasing the consultation time. This study also observed a mean (SD) registration time of 78 (22) min, with majority 74% (71/96) of the respondents spending between 60 and 120 min to be registered. This long registration time could be explained by the shortage of manpower, as evidenced in this study, where only two record clerks attended to an average of 150 patients daily.
The three most common factors leading to long waiting time observed in this study were high patient load, few doctors, and record clerks. Similar observations were made in Malaysia where four major elements were found to cause long waiting time, namely human resources, availability of equipment, registration process, and too many patients.[22] Majority of the respondents (80.2%) pointed to the presence of too many patients with few doctors to be the reason for their long stay in the clinic. This is not surprising because over the years, population has increased several folds without commensurate increase in the number of healthcare providers. Throughout the period of the data collection, only four doctors attended to an average of 150 patients on daily basis. Nigeria is one of the countries with a very low doctor – patient ratio, reaching up 1 per 25,000,[23] which is far lower than the World Health Organization target of 1 per 1000 population. This will continue to cause long waiting times in the clinics as long as the trend remains unchecked. Gender was also found to be associated with duration of waiting time, as 31.6% (30/96) of the respondents that waited for more than 3 h were females, while only 6.3% (6/96) of the male respondents waited that long (P = 0.001). A study conducted by Arnesen, however, did not observe any association between gender and duration of waiting time.[24] This difference could be explained by the fact that 62.5% (60/96) of the respondents in this study were females. Other socio-demographic characteristics such as age, education, and employment status did not have any significant effect on the waiting time (P > 0.05).
Majority of the respondents in this study would have preferred listening to health talks or watching television during the time spent waiting. Similar findings were observed by Bamgboye and Jarallah in their study. Health personnel providing health education in the form of health talks could therefore be a useful way of utilizing the long waiting times in the outpatient clinics. Despite the long waiting times experienced by the majority of respondents in this study, 64.58% (62/96) of them still said they would recommend the center to others. This may not be unrelated to the fact that the study center is a tertiary health center, thus patients still prefer to utilize the services offered in the clinic despite the long waiting times associated with it, because they anticipate better services.
Conclusion
Findings from this study have showed varying degrees of waiting time in the GOPD of the study area. More than half of the patients waited for more than 1 h, with high patient load coupled with few doctors and nurses being the main causes of this long waiting time. If the aims of the Millennium Development Goals and recommendations of the IOM are to be realized, there is an urgent need for our health facilities to increase the number of health workers in the GOPDs which are the gate way to the hospital. This will go a long way in reducing the long waiting time experienced by patients and thus increase the rating of satisfaction with services. Healthcare providers also need training on the various ways by which waiting time can be reduced such as the application of computer simulation to assist in allotting appointment time to patients and triage system to sort out patients with urgent need of attention.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Rondeau KV. Managing the clinic wait: An important quality of care challenge. J Nurs Care Qual. 1998;13:11–20. doi: 10.1097/00001786-199812000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Rossiter CE, Raynolds FA. Automatic monitoring of the time waited in an outpatient clinic. [Last accessed 2010 Oct 07];Journal Storage: Med Care. 1968 1:218–25. [Google Scholar]
- 3.Maxwell RJ. Quality assessment in health. Br Med J (Clin Res Ed) 1984;288:1470–2. doi: 10.1136/bmj.288.6428.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernandes CM, Daya MR, Barry S, Palmer N. Emergency Department patients who leave without seeing a physician: The Toronto Hospital experience. Ann Emerg Med. 1994;24:1092–6. doi: 10.1016/s0196-0644(94)70238-1. [DOI] [PubMed] [Google Scholar]
- 5.O’Malley MS, Fletcher SW, Fletcher RH, Earp JA. Measuring patient waiting time in a practice setting: A comparison of methods. J Ambul Care Manage. 1983;6:20–7. doi: 10.1097/00004479-198308000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Singh H, Haqq ED, Mustapha N. Patients’ perception and satisfaction with health care professionals at primary care facilities in Trinidad and Tobago. Bull World Health Organ. 1999;77:356–60. [PMC free article] [PubMed] [Google Scholar]
- 7.Ofilli AN, Ofowve CE. Patient's assessment of efficiency of services at a teaching hospital in a developing country. Ann Afr Med. 2005;4:150–3. [Google Scholar]
- 8.Ofilli AN, Ofowve CE. What patients want: A content analysis of key qualities that influence patient satisfaction. J Med Pract Manage. 2007;22:255–61. [PubMed] [Google Scholar]
- 9.Dansky KH, Miles J. Patient satisfaction with ambulatory healthcare services: Waiting time and filling time. Hosp Health Serv Adm. 1997;42:165–77. [PubMed] [Google Scholar]
- 10.Huang XM. Patient attitude towards waiting in an outpatient clinic and its applications. Health Serv Manage Res. 1994;7:2–8. doi: 10.1177/095148489400700101. [DOI] [PubMed] [Google Scholar]
- 11.Average ER. Reported by Associated Press; 2008. [Accessed on 7/4/110]. Waiting Time Nears 1 h, CDC Says. Available at: www.oregonlive.com/kiddo/index.../average_er_waiting_time_nears_1h . [Google Scholar]
- 12.dos Santos LM, Stewart G, Rosenberg NM. Pediatric emergency department walk-outs. Pediatr Emerg Care. 1994;10:76–8. doi: 10.1097/00006565-199404000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Dos Santos LM, Stewart G, Rosenberg NM. Pediatric emergency department walk-outs. Pediatr Emerg Care. 1994;10:76–8. doi: 10.1097/00006565-199404000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Bamgboye EO, Erinoso HO, Ogunlesi AO. The waiting time at the children's emergency room, University College Hospital, Ibadan. Nig J Pediatr. 1994;19:9–14. [Google Scholar]
- 15.Araoye MA. Research methodology with statistics for health and social sciences. 1st ed. Illorin: Nathadex Publishers; 2003. Sample size determination; pp. 115–21. [Google Scholar]
- 16.Jawaid M, Ahmed N, Nadeem AL, Rizvi BH, Hina AR. Patients experiences and satisfaction from surgical out-patient department of a tertiary care teaching hospital. Pak J Med Sci. 2009;25:439–42. [Google Scholar]
- 17.Mackey TA, Cole FL. Patient waiting time in a nurse managed clinic. [Last accessed 2010 Nov 12];The Int J Adv Nur Practice. 1997 1(1) ISSN: 1523-6064. [Google Scholar]
- 18.Chen BL, Li ED, Yamawuchi K, Kato K, Naganawa S, Miao WJ. Impact of adjustment measures on reducing outpatient waiting time in a community hospital: Application of a computer simulation. Chin Med J (Engl) 2010;123:574–80. [PubMed] [Google Scholar]
- 19.Ademola-Popoola DS, Akande TM, Idris A. Patients’ assessment of quality of eye care in a nigerian teaching hospital. Niger Postgrad Med J. 2005;12:145–8. [PubMed] [Google Scholar]
- 20.Assefzadeh S. Patient flow analysis in a children's clinic. East Mediterr Health J. 1996;2:412–7. doi: 10.1093/intqhc/9.2.143. [DOI] [PubMed] [Google Scholar]
- 21.Hannafi MA. Department of Statistics Malaysia; 2004. [Last accessed 2010 Nov 12]. Study on outpatients’ waiting time in Hospital University Kebangsaan Malaysia (HUKM) through the six sigma approach. Available at: http://www.statistics.gov.my/portal/download_journals/files/2005/Volume1/Contents_Article_Hanaffi.pdf . [Google Scholar]
- 22.Labonte RN, Labonte R, Sanders D, Schrecker T. Illustrated ed. The University of Cape Town Press; 2004. Brain Drain, Fatal Indifference: The G8 Africa and global health, IDRC. [Google Scholar]
- 23.Arnesen KE, Erikssen J, Stavem K. Gender and socioeconomic status as determinants of waiting time for inpatient surgery in a system with implicit queue management. Health Policy. 2002;62:329–41. doi: 10.1016/s0168-8510(02)00052-0. [DOI] [PubMed] [Google Scholar]
- 24.Bamgboye EA, Jarallah JS. Long-waiting outpatients: Target audience for health education. Patient Educ Couns. 1994;23:49–54. doi: 10.1016/s0738-3991(05)80021-7. [DOI] [PubMed] [Google Scholar]


