Abstract
Habitual dislocation of the patella (HDP) is a common presentation in pediatric age unlike adults. Many surgical procedures using proximal realignment and distal realignment have been reported to treat HDP in children with satisfactory results. However, late presentation of habitual patellar dislocation with osteoarthritis is rare and treatment plan has not yet been established. We present a case of neglected iatrogenic habitual patellar dislocation with osteoarthritis in a 50-year-old woman. Two-staged procedure was planned, first with patellar realignment and later with definitive total knee arthroplasty. Quadricepsplasty, medial patello-femoral ligament reconstruction, lateral release and tibial tuberosity transfer was done as primary procedure and total knee arthroplasty, which was planned as secondary procedure, was deferred as the patient improved functionally.
Keywords: Habitual dislocation of patella, lateral release, medial patello-femoral ligament, reconstruction, quadricepsplasty, tibial tuberosity transfer
INTRODUCTION
Habitual dislocation of the patella is a rare condition among adults, where the patella dislocates during flexion and relocates during extension without pain and swelling unlike the recurrent patellar dislocation. Various surgical techniques have been reported to treat pediatric population. These techniques are all designed to relocate the patella and regain alignment of the extensor mechanism.[1,2,3,4] Late presentation of neglected habitual patellar dislocation with gonarthrosis is rare.[5]
The etiology of patellar instability is multifactorial. Determination of the factors permits an effective elective treatment plan and it has been known that satisfactory or significant treatment results can be obtained with combined procedures,[6] not with a single procedure.
We report a case of iatrogenic habitual dislocation of patella with osteoarthritis of left knee in a 50-year-old female patient, who was treated with lateral release quadricepsplasty, medial patello femoral ligament (MPFL) reconstruction and tibial tuberosity transfer.
CASE REPORT
A 50-year-old woman presented with iatrogenic habitual dislocation of left patella from childhood and pain from past 3 years. She recalled a childhood surgery over middle third of left thigh (incision and drainage). Few years after the surgery, she started noticing the giving way of patella and lived for 38 years without much disability. She was carrying out her daily activities without much pain or symptoms, but she was never symptom free during this period.
Physical examination did not reveal general joint laxity or malalignment of the lower extremity. There was a healed surgical scar over middle and lower third lateral aspect of the left thigh. Although the patella was in the femoral trochlear groove in extension, it dislocated laterally with 25 degrees of knee flexion. She complained slight discomfort by an apprehension test, but was not very painful even when dislocated. The passive lateral patellar tilt test was negative since the soft tissue attachment to the lateral border of the patella was diffusely stiff and tight. Radiological examination revealed evidence of patella alta as defined by Insall and Salvati,[7] and Q angle was 18 degrees. Clinically and radiologically (Grade III Kellgren and Lawrence classification[8]) tricompartmental degenerative knee arthritis was appreciated [Figure 1]. Preoperative Kujala score[9] was 49.
Figure 1.
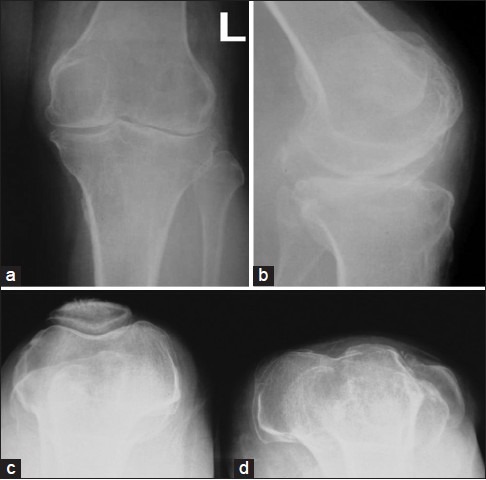
Preoperative radiographs anteroposterior (a) and lateral view (b) of left knee joint showing degenerative changes. (c) Skyline view of normal knee (Right); (d) Skyline view of affected left knee showing lateral subluxation of patella
Operative procedure
With patient in supine position under epidural anesthesia, an anterior midline knee incision was used with paramedian arthrotomy. The lateral retinaculum was thickened while the medial retinaculum was thinned. The lateral tether is released by dividing the fibrous adhesions, which extended along the lateral intermuscular septum. The lateral patellar retinaculum and the synovium were divided and vastus lateralis was detached from the quadriceps tendon, leaving a rim of tendon for suturing.
Due to shortening of the extensor mechanism, the patella could not be reduced. Quadriceps tendon was lengthened using V Y plasty at aponeurotic junction. Tracking was augmented with MPFL reconstruction using semi-tendinosus tendon and patellar end was fixed with 2.8 mm FASTak titanium anchor on the medial border of patella and over near isometric point on medial epicondyle of femur, which was checked under fluoroscopy. Patellar maltracking was persistent and so, it was decided to proceed with medial and distal transfer of tibial tuberosity.
A long-leg hinged knee brace was applied with the knee in 20° of flexion and partial weight bearing with crutches for four weeks was advised, during which the patient was encouraged to do vigorous static quadriceps strengthening exercises. Knee mobilization and full weight bearing was started after four weeks. Initially patient had extensor lag of 15 degrees as she was immobilized in flexion. But after vigorous quadriceps exercises, patient improved without any extensor lag.
At final followup two years postoperatively, the patient was pain-free. There was no evidence of patellar maltracking or instability on detailed physical examination. Radiographs showed well reduced patella in both lateral, anteroposterior view and skyline view [Figure 2]. The patient's kujala knee society score 89 [Figure 3] and range of motion was 0° to 90° on the left side [Figure 4]. Quadriceps strength was rated 4 (MRC grade).
Figure 2.
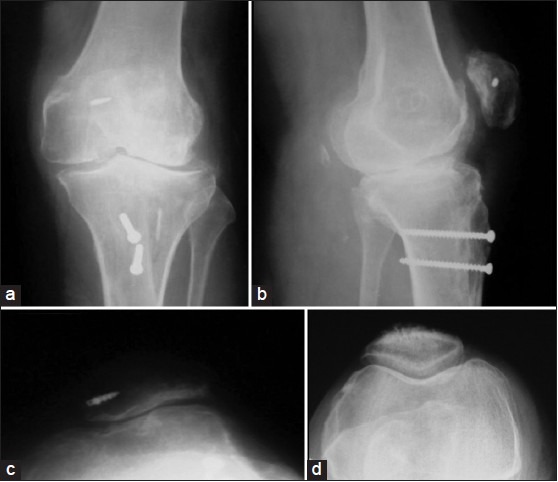
Postoperative radiographs anteroposterior (a) and lateral views (b) of left knee showing tibial tuberosity transfer fixed with screws and 2.8 mm FASTak titanium anchor on the medial border of patella (c) Skylinr view of left side showing FASTak titanium anchor (d) Skyline vfiew of normal knee (right)
Figure 3.

Clinical photographs showing functional outcome (a) walking down the stairs (b) sitting cross legged
Figure 4.
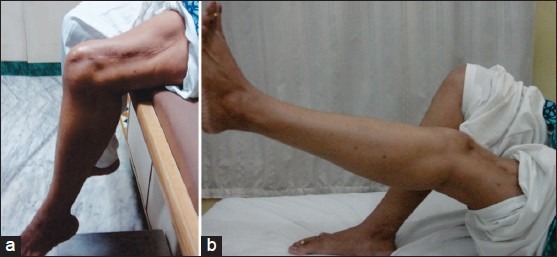
Clinical photographs showing range of motion (a) Flexion of 90 degrees and (b) extension at left knee (postoperatively)
DISCUSSION
Habitual or recurrent dislocation of the patella is common in children unlike adults. Predisposing factors include ligamentous laxity, contracture of the lateral patellar soft tissues, patella alta, quadriceps contractures, hypoplasia of the lateral femoral condyle and genu valgum (bony factors).[10] The soft tissue and bony structures mentioned above give an active and passive stability, which allow the patella to be located within the trochlea during knee movements.[11]
Permanent patellar dislocation, either congenital or acquired, is diagnosed at an early age in childhood and numerous surgical techniques have been introduced for its treatment. This is not the same for adult patellar dislocation with arthritis, where no specific treatment protocols are established. However, it has been known that combined procedures, not one single procedure, should be performed to achieve relatively satisfying treatment results. In our case, the patient was a 50-year-old female with moderate degeneration and an active lifestyle. Hence, TKR was an option and we had decided to go for staged procedures - initially getting the normal patellar tracking and later TKR.
When patellar realignment is selected for habitual dislocation of the patella with quadriceps contracture in adults, the gold standard of management has not yet been established. Proximal realignment includes lateral release, reconstruction of the MPFL and quadriceps plasty. Distal realignment comprises partial medialization of the ligamentum patella and/or tibial tuberosity transfer. Successful results require combination of these procedures, depending on clinical and intraoperative findings on an individual basis.[12]
Habitual dislocation is associated with shortening of the quadriceps muscles and considering that lengthening of the tendon is an essential part of the procedure to allow the patella to remain reduced after realignment.[13] In our case, as a result of childhood surgery and long term dislocation, the patient had quadriceps contracture and lateral soft tissue contractures, hence we decided to proceed with lateral release and quadriceps plasty as initial procedure.
Medial vector augmentation and patellar tendon alignment procedures should be included depending on the degree of quadriceps dysfunction.[14] Many times in neglected dislocations, even after lateral release, the patella may lie in trochlea in extension. Once the knee joint flexion starts, patella tends to dislocate laterally. To prevent this, always lateral release is combined with medial augmentation. In our case, we have done medial patello-femoral ligament reconstruction using semi-tendinosus tendon.[15] Medial transfer of tibial tuberosity was decided intraoperatively after doing above mentioned three procedures, because the patellar tracking was not satisfactory although the Q angle was near-normal. The diagnostic relevance of Q angle as an indication for distal realignment was not established in our case and we recommend tibial tuberosity-trochlear groove distance (TTTG) as measured by CT scan as a better tool.[16] Although standard procedures of patellar realignment include simple lateral release, proximal realignment, distal patellar tendon realignment or combination of them, addressing the pathoanatomy which is unique for every individual and careful pre-operative evaluation would give a better treatment algorithm.
Contradictory reports are present in the relevant literature. Marmor was the first to perform TKA in an adult patient with congenital dislocation of the patella without reconstructing the extensor mechanism. He reported replacement of the patella be avoided in adult patients with congenital dislocation of the patella if they can function reasonably well.[17] Pradhan et al. reported TKA for bilateral congenital dislocation of patella performed on the basis of Marmor's report. Unconstrained TKA with extensive soft tissue release in the right knee failed after 14 months. The failed TKA was revised by using constrained-type prosthesis.[18]
Total knee arthroplasty in middle-aged patient with habitual dislocation is not a permanent solution. Though the initial plan was to subject the patient for total knee replacement after soft tissue surgery, the procedure was deferred as there was significant improvement in function (kujala score) after the soft tissue surgery and the patient herself denied the second procedure. We believe that the soft tissue surgery as primary procedure will buy additional time for patient to delay the TKA and proper soft tissue balancing will improve the longevity and clinical outcome of the definitive procedures.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85:6. [PubMed] [Google Scholar]
- 2.Gao GX, Lee EH, Bose K. Surgical management of congenital and habitual dislocation of the patella. J Pediatr Orthop. 1990;10:255–60. [PubMed] [Google Scholar]
- 3.Marcacci M, Zaffagnini S, Lo Presti M, Vascellari A, Iacono F, Russo A. Treatment of chronic patellar dislocation with a modified Elmslie-Trillat procedure. Arch Orthop Trauma Surg. 2004;124:250–7. doi: 10.1007/s00402-003-0511-2. [DOI] [PubMed] [Google Scholar]
- 4.Raghuveerreddy K, Somasekharreddy N. trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Indian J Orthop. 2012;46:242–5. doi: 10.4103/0019-5413.93691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sato H, Ishibashi Y, Tsuda E, Sasaki K, Toh S. Total knee arthroplasty for gonarthrosis with patellar dislocation. J Orthop Sci. 2005;10:656–60. doi: 10.1007/s00776-005-0948-y. [DOI] [PubMed] [Google Scholar]
- 6.Shen HC, Chao KH, Huang GS, Pan RY, Lee CH. Combined proximal and distal realignment procedures to treat the habitual dislocation of the patella in adults. Am J Sports Med. 2007;35:2101–8. doi: 10.1177/0363546507305014. [DOI] [PubMed] [Google Scholar]
- 7.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101–4. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 8.Petersson IF, Boegård T, Saxne T, Silman AJ, Svensson B. Radiographic osteoarthritis of the knee classified by the Ahlbäck and Kellgren and Lawrence systems for the tibiofemoral joint in people aged 35-54 years with chronic knee pain. Ann Rheum Dis. 1997;56:493–6. doi: 10.1136/ard.56.8.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–63. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 10.Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 11.Heegaard J, Leyvraz PF, Van Kampen A, Rakotomanana L, Rubin PJ, Blankevoort L. Influence of soft tissue structures on patellar three dimensional tracking. Clin Orthop Relat Res. 1994;299:235–43. [PubMed] [Google Scholar]
- 12.Aglietti P, Giron F, Cuomo P. Disorders of patellofemoral joint. In: Scott WN, editor. Surgery the Knee. 4th ed. Philadelphia, PA: Elsevier; 2006. pp. 807–936. [Google Scholar]
- 13.Bergmann NR, Williams PF. Habitual dislocation of the patella in flexion. J Bone Joint Surg Br. 1988;70:415–9. doi: 10.1302/0301-620X.70B3.3372563. [DOI] [PubMed] [Google Scholar]
- 14.Hughston JC, Walsh WM. Proximal and distal reconstruction of the extensor mechanism for patellar subluxation. Clin Orthop Relat Res. 1979;144:36–42. [PubMed] [Google Scholar]
- 15.Raghuveer RK, Mishra CB. Reconstruction of medial patellofemoral ligament for chronic patellar instability. Indian J Orthop. 2012;46:447–54. doi: 10.4103/0019-5413.97259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abbas M, Alireza PS, Ali Y, Gholamreza S. The correlation between Q-angle (clinical) and TTTG distance (axial computed thomography) in Firuzgar Hospital. MJIRI. 2010;23:189–99. [Google Scholar]
- 17.Marmor L. Total knee arthroplasty in a patient with congenital dislocation of the patella: Case report. Clin Orthop Relat Res. 1988;226:129–33. [PubMed] [Google Scholar]
- 18.Pradhan RL, Watanabe W, Itoi E, Yamada S, Shimada Y, Sato K. Total knee arthroplasty in bilateral congenital dislocation of the patella: A case report. Acta Orthop Scand. 2001;72:422–4. doi: 10.1080/000164701753542113. [DOI] [PubMed] [Google Scholar]


