Abstract
Objective
In 2005 a definition for medication therapy management services (MTM) was developed by eleven pharmacy organizations. That year the American Medical Association introduced three temporary Current Procedural Terminology (CPT) codes for MTM. In 2008 these codes were made permanent making billing for outpatient MTM services possible. In 2010 our institution implemented a MTM program to augment services already provided. Clinical pharmacy specialists documented within the electronic medical record (EMR) upon completion of service and submitted a charge for MTM. The primary objective was to determine the effect of formal MTM services on pharmacist workload. Secondary objectives included describing the population receiving MTM, describing services provided, and determining the reimbursement rate for billed MTM services.
Data Sources
MTM CPT code claims, EMR, pharmacist MTM log
Study Selection
Not applicable
Data Synthesis
A retrospective review of all MTM charges from 1/1/2010-3/31/2010 was performed. Data collected included: location of MTM visit, age, gender, insurance, primary malignancy, comorbidities, home medications, time completing and documenting MTM visit, and rate of reimbursement.
Results
In the three month period 239 MTM visits were completed. It took pharmacists a median of 20 minutes (range: 15–127 minutes) of face-to-face time and 18 minutes (range: 5–90 minutes) for documentation per visit. To date no claims for MTM have been rejected and reimbursement rates range from 47–79% depending on the insurance provider.
Conclusions
MTM in the ambulatory clinic is feasible despite the increase in pharmacist work load from documenting and billing. Increased visibility of clinical pharmacy services justify the extra time required for formal MTM.
Keywords: Medication therapy management, clinical pharmacy, reimbursement, ambulatory clinic, CPT codes
Background
In late 2003 the Medicare Prescription Drug Improvement and Modernization Act was signed into law. Within this legislation was a mandate for the provision of medication therapy management (MTM) for patients with multiple chronic disease states, taking multiple medications, and with annual drug costs greater than 4000 dollars.1 In 2005 a consensus definition of MTM services was developed and stated that the provision of MTM services includes nine criteria previously described by Bluml.2 The essential function of MTM is that all of a patients medications are evaluated. More recently the Patient Protection and Affordable Care Act of 2010 has made pharmacist provided medication management services for chronic illness a centerpiece of health care reform.3
Currently outpatient clinical pharmacists at our institution, a comprehensive cancer center, provide MTM services to patients visiting the ambulatory care clinics through integration with the multidisciplinary team. Often these services are provided in conjunction with patient education including, but not limited to: chemotherapy teaching, chemotherapy supportive care and toxicity evaluations, and low molecular weight heparin (LMWH) teaching. Despite the fact that MTM services are well established, the ability to obtain compensation has only become a possibility since the passage of the 2003 legislation.4
The recognition of pharmacist provided cognitive services by the Centers for Medicare and Medicaid Services in 2003 paved the way for new billing opportunities. In 2005 the American Medical Association introduced three Current Procedural Terminology (CPT) codes for billing of MTM services. In 2008 these codes were made permanent after lobbying by professional organizations and evidence of substantial use.4 The current codes are 99605 for the first 15 minutes spent with a new patient, 99606 for the first 15 minutes spent with an established patient and 99607 for every additional 15 minutes spent with the patient. These codes make it possible to bill patients’ medical insurance for MTM services provided to patients in an outpatient setting. Despite this progress, billing for MTM services has been slow to develop.5–8 Once the CPT codes were made permanent, our institution began evaluating how to best implement a MTM program. Members from pharmacy, billing and reimbursement and hospital administration were involved in the development of the program which began January 2010. The decision was made that the first 15 minutes would be charged a standard flat fee. Every additional 15 minute interval would be charged a smaller flat fee. These charges are always the same amount and do not change based upon which oncology service provides them or the primary reason for the MTM visit. The amount of the charges was based upon similar charges utilized by various allied health professionals. Our institutions clinical pharmacy practice model allows for the clinical pharmacy specialists to evaluate and counsel patients each day in their respective clinics. The implementation of MTM billing does not change the patient care activities that are carried out in the ambulatory care clinics; it simply formalizes the process. The purpose of this study was to evaluate the feasibility of documenting and billing for MTM services and the effect on pharmacists’ workload. Secondary objectives included describing the patient population receiving MTM services, describing the services provided, and determining the rate of reimbursement for billed MTM services.
Methods
The formal MTM process consists of completion of a patient visit with a pharmacist in the ambulatory clinic, creation of a note within the EMR to document the visit, and submission of a charge. There was no disclosure of billing made to the patient prior to completion of the MTM visit. A template which includes all of the components required for billing is used for the EMR clinic note. In addition to serving as documentation of the visit, the note also provides valuable patient information for other healthcare providers, such as the complete medication list, any recommended dose adjustments due to organ dysfunction, drug interactions or toxicities, and the final plan of treatment as designated by the multidisciplinary team. The pharmacist submits a bill electronically using pharmacy order entry software (Centricity, Version 8.2, GE Healthcare). Clinical pharmacy specialists were educated on which patients might benefit most from MTM and were encouraged to complete an MTM visit for as many patients as possible. Ultimately, the patient selection was left to the discretion of the clinical pharmacy specialists. A review of all MTM CPT code (99605, 99606, 99607) claims submitted and completed from 1 January 2010 to 31 March 2010 was conducted. The EMR was used to collect the MTM visit location, MTM visit type, amount of face-to-face time, patient age, gender, primary disease, co-morbidities/adverse effects, insurance type, and number of home medications. In addition to completion of a note in the EMR, during the first two months of MTM billing the pharmacists completed a log recording the amount of time required to complete the note and bill for every MTM visit. Billing and reimbursement information were obtained from our institution’s department of clinical revenue and reimbursement. Data collected was analyzed using descriptive statistics to determine the impact of MTM provision and documentation on pharmacist workload, and to define the patient population receiving MTM services.
Results
During the three month research period, 239 MTM visits were completed by 24 pharmacists in 13 outpatient clinics. During the study period there were only 4 MTM visits for established patients thus 235 unique patients were included. The average age of patients receiving MTM services was 56 years (SD ± 13) and 46% were male. In addition to having at least one malignancy, the median number of co-morbidities was two (range 0–9). The median number of medications (not including intravenously administered chemotherapy) was ten (range: 1–30). Forty-five patients were taking oral chemotherapy. Thirty-one different malignancies were represented from 10 different cancer subspecialties the most common being gastrointestinal cancer (60 patients, 26%) the other types are listed in Table 1. While evaluation of patients’ complete medication list was always provided the impetus for the majority of MTM visits, 143 (60%), was chemotherapy teaching and management of potential toxicities (, followed by post stem cell transplant follow up 50 (21%), and symptom management 39 (16%) with 7 (3%) consisting of LMWH education, hormone therapy teaching, and herbal supplement counseling. Of the 239 MTM visits 159 (66.5%) were provided to patients with commercial insurance, 69 (28.9%) to those with government insurance, and 11 (4.6%) classified as either self-pay or indigent. Pharmacists charged all patients regardless of insurance status. Pharmacists took a median of 20 minutes (range 15–127 minutes) of face-to-face time and 18 minutes (range 5–90 minutes) to document each visit. The median time needed to complete the entire MTM process was 38 minutes (range 20–170 minutes). Comparing January to February, the mean amount of face-to-face time was not significantly different. The average amount of time spent documenting and billing decreased by seven minutes from January to February (Figure 1). Reimbursement rates for these charges ranged from 47–79% depending on the insurance provider.
Table 1.
Malignancies
| Type | Patients |
|---|---|
| Gastrointestinal Cancers | 60 |
| Breast Cancer | 54 |
| Leukemias | 36 |
| Lymphoma/Myeloma | 25 |
| Thoracic/Head and Neck Cancers | 21 |
| Sarcomas | 16 |
| Gynecologic Cancers | 10 |
| Unknown Primary | 6 |
| Genitourinary Cancers | 4 |
| Anaplastic Anemia post Stem Cell Transplant | 3 |
Figure 1.
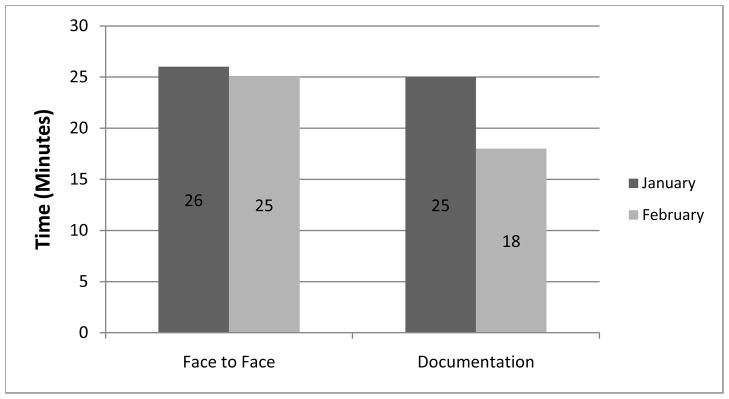
Mean Time to Complete Per Month
Discussion
Since the implementation of clinical pharmacy services at our institution in 1985 our clinical pharmacists have been working in a capacity that meets the consensus definition for MTM. The challenge that has faced pharmacists since the inception of clinical pharmacy is how to distinguish cognitive services from dispensing services in terms of reimbursment.7 This distinction is vital to establish ourselves as integral practitioners who provide valuable services to our patients, not just providing a product. The opportunity to develop a formal MTM process and bill for MTM services has afforded us a means to increase our patient visibility as collaborative healthcare professionals providing formal cognitive services, and to improve documentation of patient care while maintaining our role as medication experts.
During the three months of our study 24 clinical pharmacists were able to document 239 MTM visits for complex patients due to the nature of their malignancies, active treatment with chemotherapy or biotherapy, additional co-morbidities, and numerous medications. Variability in patient selection was the product of a variety of patient, clinic and pharmacist factors. The factors ranged from number of patients medications to clinic patient volume. These patients’ medication issues were able to be addressed with less than 30 minutes of face-to-face time. Given the fact that MTM-like services have been provided for many years at our institution, it is not surprising that the visits were efficient. When considering the feasibility of MTM at our center the time spent with patients is not the main concern. For us the amount of time that is required to document and bill for MTM is the primary concern. At institutions where clinical pharmacy specialists are not able to spend as much time with individual patients due to staffing constraints the overall time to complete the formal MTM process including the face-to-face time would be more of a concern. We found that MTM documentation was able to be completed with a median time less than 20 minutes per encounter. This time is likely to improve with experience considering most pharmacists were not familiar with the process of billing and type of documentation required. Our finding that the time required to document and bill decreased by an average of 7 minutes from January to February clearly suggests that as familiarity increased, the amount of time required decreased (Figure 1). The ability to complete the entire MTM process in a median of 38 minutes shows that it is possible to successfully implement an MTM billing program within the context of a clinical pharmacist’s role in the outpatient clinic setting. Unfortunately at our institution payments are posted by encounter not by individual charge making detailed analysis difficult. To date we have had no specific MTM denials and in fact all payers have been reimbursing the total encounter charge at rates ranging from 47–79% depending on the contractual agreement.
In an attempt to compare our experience to that of other pharmacists conducting MTM in ambulatory clinics a literature search was conducted using Pubmed, Ovid, and SCOPUS. Multiple searches were conducted using the following terms: medication therapy management, MTM, billing, reimbursement, CPT codes, ambulatory care, pharmaceutical care and clinical pharmacy. There were a number of articles describing the value of MTM on patient outcomes and billing to prescription insurances primarily Medicare part D. Based on are searches there are only a limited number of studies billing to primary medical insurance. We believe this to be the first study focusing on the oncology ambulatory setting which allows few direct comparisons to be made with previously published literature.
Despite the progress that has been made there are a number of barriers to the process of MTM documentation and billing were discovered during the initial implementation. Resistance by pharmacists to the MTM billing process was encountered due to a variety of different issues, the primary of which was perceived time constraints. Many pharmacists believed that their other duties would keep them from completing the required MTM documentation and billing. The perception of not having enough time to complete MTM has been a barrier since its inception.6 To overcome this we provided further education and training using patient cases and demonstration on how to efficiently carry out the process. One-on-one training was also provided to those with continued difficulty. Even without further education, documentation and billing time decreased as pharmacists’ experience increased. Evaluation of methods to capture the impact on patient outcomes is also ongoing in hopes of further solidifying the value of these services. Additional perceived benefits of MTM such as improved awareness of patients’ non-oncologic issues and improved coordination of care for patients could increase the willingness to participate in the MTM program.
A second obstacle involves discrepancies that were observed between the pharmacists’ log that were kept during January and February and the amount of MTM claims submitted via the billing software. It is most likely that these claims were lost due to user error while completing the charge. During additional training sessions we have addressed these issues in the hope they will be resolved. We continue to monitor for problems with the computer software used for billing and are developing an internal auditing process.
The pharmacist log used to determine the amount of time required to complete the billing process proved to be an ineffective method of evaluation. Despite thorough instruction and education there was variability in the way this log was kept by each individual. This specifically affected our ability to determine the amount of time pharmacists spent preparing and documenting a MTM visit. In an attempt to evaluate the feasibility of the MTM process and not further increase the workload placed on already busy pharmacists, the log was only kept for a portion of the study period. In the future a log may be beneficial to evaluate whether the amount of time spent documenting and billing for MTM is decreasing. To limit the impact on pharmacists’ workload, it may be beneficial to only include a sample of pharmacists and document over a shorter period of time.
Moving forward it is essential for us to ensure that we provide quality services and to determine the value of MTM provided at our facility. To monitor quality as well as encourage participation, MTM has been incorporated in to all eligible pharmacists’ yearly evaluation. A recurring peer-to-peer audit process of all MTM notes and charges has been developed and instituted. This audit will ensure that we are compliant with all billing requirements and assess the MTM notes for quality. Another aspect of quality that we plan to assess in the future is the effect of MTM on patient outcomes. While there have been many studies demonstrating the positive effect of pharmaceutical care and MTM on patient outcomes for a variety of chronic conditions such as diabetes and hypertension it has not been demonstrated in the oncology setting.7,8 Once the formal MTM process has been firmly integrated into the workflow of our institutions clinical pharmacy specialists we will determine the impact on patient outcomes.
Ultimately we believe that this program has increased recognition of the value of pharmacists in the ambulatory clinic setting. As a profession these types of activities may help further distinguish ourselves as healthcare providers vital to high quality patient care.7 Through documenting and billing for cognitive services we have taken another step to demonstrate to physicians, advanced practice nurses, physician assistants, nurses and patients that pharmacists are integral providers within the multidisciplinary team. Our program shows that pharmacists are willing and capable to carry our profession into a new era where our contribution to patient care is recognized as having value. While many challenges remain unresolved and many more have yet to be discovered we will continue to press forward; in doing so we strive to better our profession, our institution and most of all the lives of our patients.
Acknowledgments
Supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant, CA016672.
Footnotes
Conflict of Interest: The authors of this paper have no potential or real conflicts of interest or financial interests in any of the products or services mentioned in this article.
Data previously presented as a poster at the Hematology/Oncology Pharmacy Association Annual Meeting 2010
Contributor Information
Jack L. Watkins, The University of Texas MD Anderson Cancer Center, Houston, Texas.
Andrea Landgraf, The University of Texas MD Anderson Cancer Center, Houston, Texas.
Chad M. Barnett, The University of Texas MD Anderson Cancer Center, Houston, Texas.
Laura Michaud, The University of Texas MD Anderson Cancer Center, Houston, Texas.
References
- 1.Centers of Medicare and Medicaid Services. [Accessed 2009 Aug 30];Medicare prescription drug, improvement, and modernization act of 2003. www.cms.hhs.gov/MMAUpdate/downloads/PL108-173summary.pdf.
- 2.Bluml BM. Definition of medication therapy management: development of profession-wide consensus. J Am Pharm Assoc. 2005;45:566–572. doi: 10.1331/1544345055001274. [DOI] [PubMed] [Google Scholar]
- 3. [Accessed May 1, 2010];Patient protection and affordable care act, HR 3590, 111th Cong. 2009 Available from http://democrats.senate.gov/reform/patient-protection-affordable-care-act-as-passed.pdf.
- 4.Lamb E. [Accessed 2009 Aug 30];CPT codes for MTM made permanent. http://www.pharmacist.com/AM/Template.cfm?Section=Pharmacy_News&template=/CM/ContentDisplay.cfm&ContentID=14126.
- 5.Thomas J, Zingone M, Smith J, et al. Feasibility of contracting for medication therapy management services in a physician’s office. Am J Health-Sys Pharm. 2009;66:1390–1393. doi: 10.2146/ajhp080464. [DOI] [PubMed] [Google Scholar]
- 6.Lounsbery JL, Green CG, Bennett MS, et al. Evaluation of pharmacists’ barriers to the implementation of medication therapy management services. J Am Pharm Assoc. 2009;49:51–58. doi: 10.1331/JAPhA.2009.017158. [DOI] [PubMed] [Google Scholar]
- 7.Ramalho OD, Brummel AR, Miller DB. Medication therapy management: 10 years experience in large integrated health care system. J manag care pharm. 2010;16(3):185–95. doi: 10.18553/jmcp.2010.16.3.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stubbings J, Nuescu E, Durley SF, Bauman JL. Payment for clinical pharmacy services revisited. Pharmacotherapy. 2011;31(1):1–8. doi: 10.1592/phco.31.1.1. [DOI] [PubMed] [Google Scholar]


