Abstract
Background: The present study aimed to assess parental perceptions of weight-based victimization (WBV) and its consequences for children's health as well as how perceptions of WBV vary by parental and child weight status.
Methods: A national sample of American parents with children ages 2–18 years (N=918) completed an online questionnaire to assess their perceptions of how common WBV is, compared to other forms of victimization among youth, their level of concern with this issue both generally and for their own child, and their perceptions of behavioral and psychological consequences of WBV. Descriptive statistics and censored regression models with standardized coefficients were used to analyze the data.
Results: Fifty-three percent of parents perceived “being overweight” to be the most common reason that youth are bullied, regardless of parental or child weight status. Parents, both with and without overweight children, endorsed similar levels of general concern about WBV and its psychological and behavioral consequences for youth. However, parents with overweight children were substantially more concerned about WBV affecting their child(ren) and perceived it to be more common, serious, and posed risks to their child(ren)'s health, compared to parents without overweight children.
Conclusions: The present study, to the best of the authors' knowledge, is the first to indicate that parents have substantial concerns about WBV and its health consequences for youth. These findings highlight the need for educators and pediatric healthcare providers to be aware that WBV is a common concern among families, and suggest that increased efforts are needed to address WBV.
Introduction
In recent years, bullying among youth has received increased attention as a public health issue. National antibullying campaigns, state and school policies, and even the White House have begun concerted efforts to address this problem.1,2 During adolescence, nearly half of youth are vulnerable to repeated bullying,3 and recent evidence indicates that adolescents report that being overweight is the most common reason their peers are teased and bullied at school.4 Given that almost one third of youth are either overweight or obese,5 millions are at risk of weight-based victimization (WBV) by peers in schools, athletic teams, extracurricular activities, and other settings involving peers.
WBV is associated with a range of negative outcomes for youth, such as increased depression, social isolation, lower self-esteem, poor body image, unhealthy eating behaviors, and suicidal ideation,6–8 as well as binge eating and avoidance of physical activity,9–11 which may exacerbate obesity in youth. In addition, WBV is associated with poorer school performance12 and increases the likelihood of youth avoiding school and reporting that their grades are harmed because of WBV incidents.13
Parents have an important role to play in efforts to address WBV. Parental support has been shown to protect youth from multiple forms of bullying.14 However, most research to date has focused on the experiences of victims, perpetrators, and bystanders, and the little research that has examined adults' perceptions regarding bullying has focused on perspectives of teachers, rather than parents.15 The few studies conducted with parents often assess family factors, such as attachment style or authoritative parenting approaches,16–18 or assess parents as informants reporting on their child's experiences of bullying.19,20
A recent qualitative study attempting to address this gap in the literature found that many parents are unclear about the definition of bullying, and that this affects their likelihood of recognizing bullying behaviors in youth.15 Nevertheless, several general surveys suggest that parents rate bullying as one of their main health concerns for their child, among other risk behaviors such as drug use and underage drinking.21,22 Parents of overweight and obese youth in particular rate bullying as their top health concern for their child.23
To the authors' knowledge, no research has yet examined parental perceptions of WBV in youth. Parental perceptions of WBV may affect how attentive and aware they are of their child's experiences of WBV, which, in turn, could affect the type and amount of parental support they give, their perceptions of the consequences of WBV for emotional and physical health for youth, and the services that parents seek to help their children cope with WBV. To examine this unstudied area, the present study aimed to assess parental concerns and beliefs about WBV and its consequences for health among youth who are targeted as well as how perceptions of WBV vary by parental and child weight status.
Methods
Participants
The study sample was comprised of adults recruited through a survey panel administered by Survey Sampling International (SSI) during April 2012. SSI is a global provider of sampling solutions for survey research, with headquarters in Connecticut. Online recruitment was derived from >3400 sources by use of targeted approaches (e.g., banner ads, key words, search links, e-mail, and online invitations) to achieve demographic and psychographic diversity within the online population. SSI data aggregators reach millions of users, carefully screen panelists, and employ validation processes that compare respondent demographic characteristics to multiple databases. SSI provides a variety of incentives (including research feedback, charitable donations, and monetary and points rewards) for participation, which is completely voluntary.24,25 For recruitment in the present study, panelists who identified themselves as parents, and who chose to participate, were directed to the online survey. All participants provided informed consent, and the study was approved by the Yale University Institutional Review Board (New Haven, CT).
Of 1168 participants who entered the survey, exclusions were made for participants who declined to participate (n=43), and for participants who did not have a child between the ages of 2–18 years living at home (n=88), yielding a sample of 1037 participants. In addition, observations with item-nonresponse missing data were excluded list-wise, yielding a final sample of 918 parents. Table 1 summarizes characteristics of the study participants. Parents' BMI was stratified by using clinical guidelines for the classification of overweight and obesity in adults by the National Heart, Lung, and Blood Institute of the National Institutes of Health.26 This stratification revealed that 2.4% of the parents were underweight, 33% were healthy weight (BMI, 18.5–24.9), 33% were overweight (BMI, 25.0–25.9), and 32% were obese (BMI, >30). This distribution of body weight is representative of the general population.27 The racial distribution of the sample closely resembled that of US Census data, and the household income distribution approximated national percentages.28,29 Parental reports of their child(ren)'s weight showed that 8.5% were underweight, 49% were healthy weight, 18% were overweight, and 24% were obese. Compared with recent US estimates, this sample contained a slightly higher percentage of youth who are overweight and obese.5
Table 1.
Sample Characteristics
| Characteristics | N | % |
|---|---|---|
| Gender | ||
| Male |
447 |
48.69 |
| Female |
471 |
51.31 |
| Highest educational degree | ||
| High school |
324 |
35.29 |
| Some college |
267 |
29.08 |
| College+ |
327 |
35.62 |
| Annual household income | ||
| Under $25,000 |
229 |
24.95 |
| $25,000–$49,999 |
221 |
24.07 |
| $50,000–$74,999 |
198 |
21.57 |
| $75,000–$99,999 |
132 |
14.38 |
| $100,000+ |
138 |
15.03 |
| Race/ethnicity | ||
| White |
652 |
71.02 |
| Black |
116 |
12.64 |
| Hispanic |
91 |
9.91 |
| Other |
59 |
6.43 |
| Political orientation | ||
| Conservative |
285 |
31.05 |
| Moderate |
446 |
48.58 |
| Liberal |
187 |
20.37 |
| Participant weight status | ||
| Underweight |
22 |
2.4 |
| Healthy weight |
300 |
32.68 |
| Overweight |
302 |
32.9 |
| Obese |
294 |
32.03 |
| Participant has at least one child that is overweight or obese | ||
| No |
447 |
48.69 |
| Yes |
471 |
51.31 |
| Participant children's weight status | ||
| Underweight |
127 |
8.49 |
| Healthy weight |
739 |
49.4 |
| Overweight |
264 |
17.65 |
| Obese | 366 | 24.47 |
| N | M | SD | |
|---|---|---|---|
| BMI (participants) |
918 |
28.30 |
7.04 |
| Age (years, participants) | 918 | 41.18 | 11.37 |
M, mean; SD, standard deviation.
Measures
Demographic and weight information
Participants reported their age, gender, ethnicity, highest level of education, annual household income, political affiliation, height, and weight. Parents were also asked the number of children they have, each child's age (year and month they were born), gender, and current height and weight. BMI percentiles for youth were calculated with respect to age and gender based on the CDC growth curves,30 then classified according to weight categories (e.g., healthy weight, overweight, or obese).31 Parents' perceptions of their child(ren)'s weight status were assessed by asking, “Are any of your children overweight (heavier than most children their age)?”
Parental perceptions of weight-based victimization
Before asking participants questions about WBV in youth, they were provided with a comprehensive definition of bullying, which stated: “Bullying is when a person or group of people intentionally and repeatedly hurt another individual during face-to-face interactions or through technology (i.e., a computer or cell phone). This may include being mean, spreading rumors, teasing, harassing, name-calling, insulting, ignoring, excluding, embarrassing, threatening, making fun of someone, or even being physically aggressive.”4,13 They were then instructed to answer the survey questions with this definition in mind.
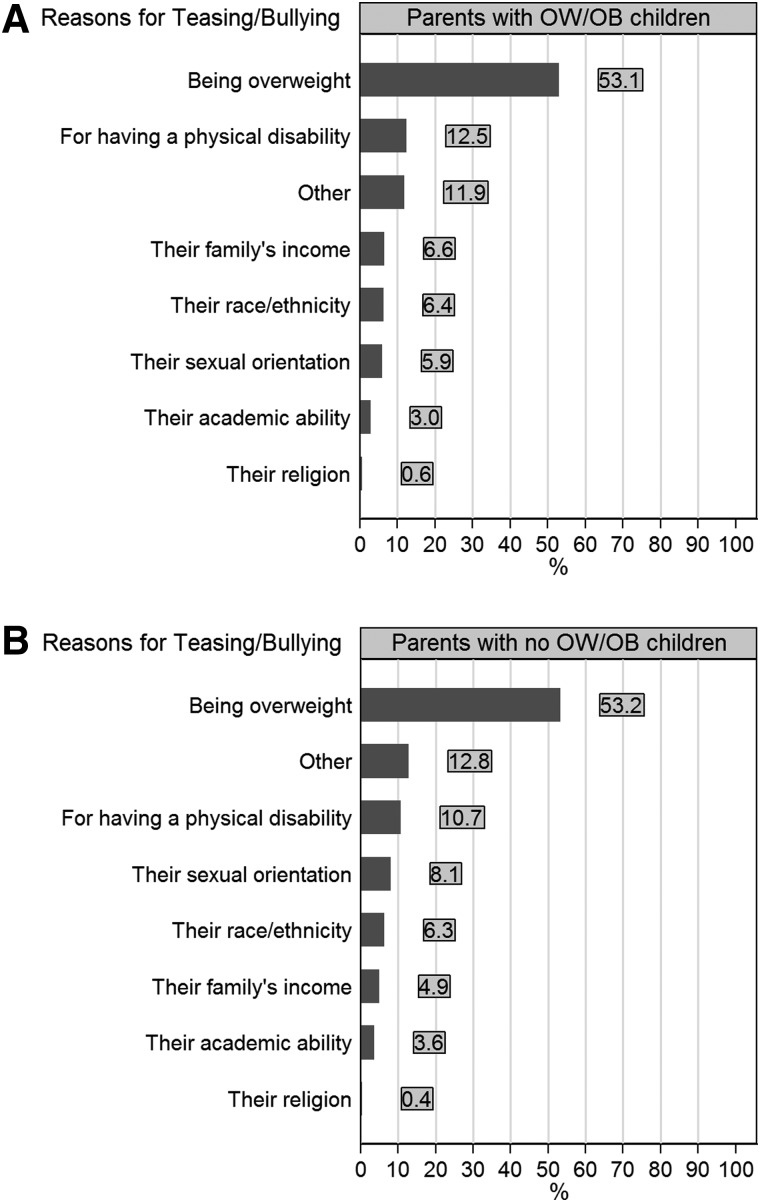
To assess parental perceptions of how common WBV is compared to other forms of victimization among youth, parents were first asked, “In your opinion, why are children most often called names, teased, or bullied?” Participants had to choose one of eight response options, which are presented in Figure 1. Subsequently, participants were asked eight questions about their perceptions of how common and serious WBV is, how concerned they are about it, and the extent to which they perceive WBV to be harmful to children's health. These questions were asked both for perceptions of WBV among youth in general and in regard to participants' own children (e.g. “How common do you think the problem of weight-related bullying and teasing is in general?” and “How common do you think the problem of weight-related bullying and teasing is at your child's school?”). Responses were measured on 5-point Likert scales [coded from 1 (for “very uncommon”) to 5 (for “very common”)]. Based on principal component factor analysis with orthogonal varimax rotation, two mean scales were constructed from the eight items: one scale for general concern about WBV [4 items; mean (M), 4.28; standard deviation (SD), 0.75; Cronbach's α=0.85] and the other for personal concern about WBV for their own child (4 items; M, 3.25; SD, 1.09; Cronbach's α=0.84).
Figure 1.
Parents' perceptions of the most common reason that youth are teased or bullied. Original questionnaire item was: “In your opinion, why are children most often called names, teased, or bullied?”, with response options as shown in the graph; bars in the graphs appear in descending order; OW/OB is overweight or obese, based on parents' self-report about height and weight of their children and subsequent classification based on BMI-for-age z-scores; weight status of children based on the CDC classification; using parent's perceived weight status of their children revealed that 65% of parents who perceived their child(ren) as either overweight or obese reported “being overweight” as the most important reason for bullying; N=918.
Parental concerns about consequences of weight-based victimization
Participants were asked 12 questions to assess their level of concern with potential behavioral and psychological consequences of WBV. Specifically, parents were asked how concerned they are that WBV will lead to behavioral consequences in youth, including avoidance of group-based physical activities and social activities, skipping class or school, increasing food consumption, engaging in unhealthy eating behaviors, and exercise avoidance, as well as psychological consequences, including depression, poor body esteem, low self-esteem, obsession about weight, and suicidal thoughts. These items were selected because they are well-documented correlates of weight-related bullying (see Introduction). Five-point Likert scales were used for all items [coded 1 for (“not at all concerned”) to 5 (for “extremely concerned”)]. Based on principal component factor analysis with orthogonal varimax rotation, two mean scales were constructed, including concern about behavioral consequences of WBV (6 items; M, 3.91; SD, 0.99; Cronbach's α=0.94) and psychological consequences (6 items; M, 4.12; SD, 1; Cronbach's α=0.96).
History of weight-based victimization
Finally, participants were asked four forced-choice questions to assess whether they or their child had ever been bullied because of their weight. This measure has been used in previous studies of weight bias.25
Statistical Analysis
All four scales that are used as outcome variables are characterized with a mean that is close to a scale's maximum value. The reason for this is that a number of respondents selected the highest response category from the Likert scales. As a result, the data for these scales are negatively skewed, illustrating a clumping at their highest values. Therefore, a regression model was used for censored data (the Tobit model). Data are regarded as censored from above at maximum values of the outcome variables. Estimated coefficients from a Tobit model are interpreted similarly to linear regression estimates. Estimated coefficients were standardized by dividing raw coefficients by the (unconditional) standard deviation estimate of the latent outcome variable and thus can be interpreted in terms of standard deviation units.
Results
Descriptive Findings
Figure 1 shows percentages pertaining to parents' perceptions of the reason why youth are most often bullied. These percentages are reported both for parents with and without children who are overweight or obese. In both groups of parents, “being overweight” was perceived to be the most common reason that youth are bullied. Over 50% of parents perceived “being overweight” to be the most common reason for youth bullying. Other reasons for bullying (e.g., physical disability, sexual orientation, and so on) were rated as most common by 13% or less of parents. Participants could also select an “other” category and provide open responses, which were subsequently coded into nine categories and included the following: all reasons listed (3.05%); “child is different” (2.07%); personality of victim (1.63%); physical appearance (1.42%); social reasons (0.98%); “kids are mean” (0.87%); personality of perpetrators (0.65%); unknown reasons (0.65%); and other reasons (0.76%). Responses did not differ substantially across parents with and without overweight or obese children.
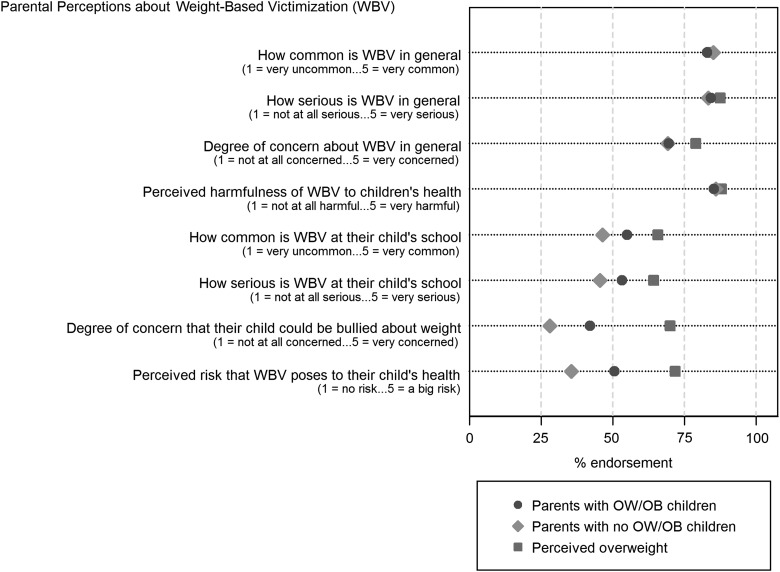
Figure 2 shows the percentage of item endorsement for parents' general perceptions about WBV among youth (first four items in the graph) and with respect to their own child(ren) (last four items). Endorsement was defined as selection of the top two response categories of the 5-point Likert scales (a “4” or “5” on the scale). As Figure 2 indicates, both parents with and without overweight youth endorsed similar levels of general concern about WBV as a problem among youth. However, with regard to their own children, parents with overweight children were substantially more concerned about WBV and perceived it to be more common, serious, and posing risks to their child(ren)'s health, compared to parents without overweight children. These differences were even more pronounced when analyses were conducted using parents' perceptions of children's weight status, rather than CDC classifications of BMI (see Fig. 2). Of note, of the 468 parents (51% of total sample) who had at least one overweight or obese child based on the CDC classification, 156 (33%) correctly perceived their child(ren) to be overweight, whereas 28 (6% of parents) without overweight or obese child(ren) based on the CDC classification regarded their child(ren) as overweight or obese.
Figure 2.
Parents' perceptions of weight-based victimization among youth in general and with regard to own children. Dots represent percentages of item endorsement, with endorsement being defined as the top two categories (4 and 5) of 5-point Likert scales. “Parents with OW/OB children” refers to youth who were overweight or obese using BMI percentiles according to CDC classifications. “Perceived overweight” is based on the perceived weight status of participant's children, questionnaire wording was: “Are any of your children overweight (heavier than most children their age)?”, with response options “Yes” (20%) and “No” (80%); percentages in the graph only refer to parents who answered the question with “yes”; parents who answered “no” had similar endorsement percentages as parents without overweight or obese children, based on the CDC classification; N=918.
Table 2 shows response percentages for the original Likert scales assessing parents' degree of concern about psychological and behavioral consequences of WBV in youth. Table 2(A) presents the degree of parental concern about potential psychological consequences of WBV. Parents with overweight children reported being “quite” or “extremely” concerned that WBV in youth would lead to low self-esteem and poor body esteem (80%), depression (78%), suicidality (71%), and impaired academic achievement (68%). Percentages were very similar for parents without overweight or obese children, suggesting that there is considerable concern among parents that WBV poses adverse outcomes for psychological functioning, regardless of their child's weight status. Table 2(B) shows the degree of parental concern with respect to potential behavioral consequences of WBV. Again, response patterns were fairly similar for parents with and without overweight or obese children, with the majority of parents in each group indicating that they were “quite” or “extremely” concerned about potential behavioral consequences of WBV for their children, with percentages ranging from 64% (e.g., skipping class or school) to approximately 70% (e.g., avoiding physical and social activities or eating more food).
Table 2.
Percentage of Parents Who Express Concern about Psychological and Behavioral Consequences of Weight-Based Victimization
| |
Parents of overweight/obese children Degree of concern (%) |
Parents with no overweight/obese children Degree of concern (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| None | Little | Somewhat | Quite | Extreme | None | Little | Somewhat | Quite | Extreme | |
| A. Potential psychological consequences of WBV | ||||||||||
| Depression |
4 |
5 |
14 |
25 |
53 |
3 |
4 |
14 |
24 |
54 |
| Poor body esteem |
3 |
4 |
13 |
30 |
50 |
3 |
5 |
13 |
27 |
51 |
| Low self-esteem |
2 |
4 |
13 |
27 |
54 |
3 |
4 |
12 |
26 |
55 |
| Obsession with weight |
3 |
7 |
18 |
24 |
48 |
3 |
6 |
16 |
28 |
47 |
| Suicidal thoughts |
6 |
7 |
15 |
20 |
51 |
4 |
6 |
13 |
23 |
54 |
| Impaired academic achievement |
5 |
10 |
17 |
26 |
42 |
5 |
10 |
18 |
27 |
41 |
| B. Potential behavioral consequences of WBV | ||||||||||
| Avoidance of physical activities |
5 |
6 |
20 |
33 |
36 |
3 |
8 |
19 |
33 |
36 |
| Avoidance of social activities |
4 |
7 |
20 |
31 |
38 |
3 |
7 |
21 |
32 |
38 |
| Skip class or school |
9 |
8 |
19 |
24 |
40 |
6 |
10 |
24 |
24 |
37 |
| Eat more food |
4 |
7 |
19 |
27 |
44 |
3 |
5 |
20 |
30 |
42 |
| Unhealthy weight loss behaviors |
5 |
7 |
19 |
23 |
45 |
2 |
6 |
17 |
27 |
47 |
| Avoidance of exercise | 5 | 10 | 21 | 27 | 36 | 4 | 9 | 24 | 29 | 33 |
Questionnaire wording asked participants how concerned they were that weight-related bullying would lead children to experience various psychological consequences (A) and behavioral consequences (B). Response options were rated on a 5-point Likert scale from 1 (not at all concerned) to 5 (extremely concerned); weight status of children was based on the CDC classification; using parent's perceived weight status of their children yielded similar results; N=918.
WBV, weight-based victimization.
Model Results
Table 3 summarizes results from four separate Tobit regression models. All coefficients are standardized and indicate differences in the outcome variables in terms of standard deviation units. Participants with overweight or obese children expressed more concern about bullying with regard to their own children (Table 3, column 2, small effect of ∼20% of a standard deviation), compared to participants with no overweight children. However, whether or not parents had an overweight child made no difference in the degree of their general concern about WBV and its potential to lead to behavioral or psychological consequences for youth. Using parents' perceptions of children's weight status revealed comparable results, except that the effect on concerns about bullying with regard to their own children was twice as large (0.40; p<0.001), and the negative effect on the potential of WBV to lead to psychological consequences was larger and statistically significant (–0.23; p=0.015).
Table 3.
Parental Concern about Weight-Based Bullying and Its Consequences among Youth, Censored Regression Models
| Concerned about WBV in youth—in general | Concerned about WBV—their own child(ren) | Concerned about psychological consequences of WBV | Concerned about behavioral consequences of WBV | |
|---|---|---|---|---|
| Any child overweight or obese?a (ref. no.) |
— |
— |
— |
— |
| Yes |
−0.078 |
0.204** |
−0.132 |
−0.107 |
| Child reported WBV (ref. no.) |
— |
— |
— |
— |
| Yes |
0.503** |
1.073*** |
0.528** |
0.310* |
| Don't know |
0.100 |
0.558** |
0.044 |
0.002 |
| Respondent experienced WBV in the past (ref. no.) |
— |
— |
— |
— |
| Yes |
0.454*** |
0.343*** |
0.405*** |
0.419*** |
| Parents' weight status (ref. healthy weight) |
— |
— |
— |
— |
| Parents' weight status: underweight |
0.566 |
−0.227 |
0.840* |
0.729** |
| Parents' weight status: overweight |
0.186 |
0.139 |
0.069 |
0.116 |
| Parents' weight status: obese |
−0.042 |
0.082 |
−0.066 |
−0.050 |
| Gender composition of children [ref.: only boy(s)] |
— |
— |
— |
— |
| Only girl(s) |
−0.044 |
0.050 |
−0.006 |
−0.049 |
| Boy(s) and girl(s) |
0.203 |
0.069 |
0.185 |
0.235 |
| Number of children |
−0.084 |
−0.028 |
−0.019 |
−0.068 |
| Gender (ref. male) |
— |
— |
— |
— |
| Female |
0.346*** |
0.088 |
0.400*** |
0.257** |
| Race/ethnicity (ref. Caucasian) |
— |
— |
— |
— |
| African American |
0.042 |
0.100 |
0.034 |
0.049 |
| Hispanic |
0.229 |
0.305** |
0.274 |
0.186 |
| Other |
−0.031 |
0.121 |
0.004 |
−0.013 |
| Highest level of education (ref. high school or less) |
— |
— |
— |
— |
| Some college |
−0.053 |
−0.100 |
0.124 |
0.059 |
| College+ |
−0.356** |
−0.203* |
−0.148 |
−0.145 |
| Household income (ref. under $25,000) |
— |
— |
— |
— |
| $25,000–$49,999 |
−0.019 |
0.165 |
0.126 |
0.067 |
| $50,000–$74,999 |
−0.212 |
0.054 |
−0.012 |
0.083 |
| $75,000–$99,999 |
−0.257 |
−0.025 |
−0.130 |
−0.064 |
| $100,000+ |
−0.003 |
0.063 |
0.142 |
0.180 |
| Political orientation (ref. conservative) |
— |
— |
— |
— |
| Moderate |
0.134 |
0.133 |
0.202 |
0.093 |
| Liberal |
0.063 |
0.186 |
0.151 |
0.028 |
| Age (in years) |
0.006 |
0.003 |
−0.001 |
−0.004 |
| Constant |
−0.204 |
−0.682*** |
−0.248 |
−0.046 |
|
N |
918 |
918 |
918 |
918 |
|
N uncensored |
634 |
824 |
616 |
727 |
| N right censored | 284 | 94 | 302 | 191 |
Displayed results are estimated using regression models for censored data (Tobit). All outcome variables are regarded as right censored (i.e., censored from above) at their highest values; all coefficients are standardized with respect to the estimated standard deviation of the latent outcome variable, thus the effects can be interpreted along the standard deviation metric; ref. indicates reference category; significance levels: *p<0.05; **p<0.01; ***p<0.001.
Based on BMI-for-age classification (CDC).
WBV, weight-based victimization.
Several additional findings emerged. Parents whose children had reported that they were bullied about their weight scored higher on all four scales (with moderate to strong effects; Table 3). This was also the case for parents who reported that they themselves had experienced WBV. In addition, mothers were more concerned than fathers with respect to general concern about WBV and its potential psychological and behavioral consequences for youth. There were no gender differences with regard to degree of concern about WBV for their own child(ren), and no consistent effects were observed for gender of youth or weight status of parents. Parents with the highest educational attainment expressed less concern about WBV than parents with the lowest educational attainment.
Discussion
To the best of the authors' knowledge, this is the first study to provide a comprehensive assessment of parental perceptions of WBV in youth. Results indicate that parents perceive being overweight to be the most common reason that youth are bullied and view it to be substantially more common than other reasons for bullying, such as race, sexual orientation, physical disability, religion, and others. These findings were consistent regardless of parental and child weight status. These parental perceptions are similar to those expressed by youth, who also report that WBV is the most common form of teasing that they observe in the school setting.4
Parents with overweight or obese children expressed higher levels of concern about WBV affecting their own children, compared to parents with no overweight children. Given recent evidence suggesting that the heaviest youth are most vulnerable to WBV, compared to peers of lower weights,32,33 it would be expected that parents of these youth might voice the strongest concerns about WBV. However, it is noteworthy that parental concerns remained substantial even among those without overweight children, suggesting that parents may perceive their children to be vulnerable to WBV even if they do not have excess weight. This explanation seems plausible in light of recent research showing that youth report experiencing WBV at different weight categories, including those who are underweight and at a healthy weight,34 and among youth who were formerly overweight, but, through weight loss, have obtained a healthy weight.35
The finding that parents both with and without overweight children expressed substantial, and similar, levels of concern about WBV among youth and its effect on psychological and behavioral functioning of youth is important. These parental perspectives are in line with current evidence demonstrating the negative influence of WBV on the emotional, social, and physical well-being of youth (see review by Puhl and Latner, 2007).36 However, whereas parents in the present study certainly acknowledged their concerns about the consequences that WBV may pose for youths' health, they may not be aware of (or have access to) services available to help youth cope with WBV or be equipped with other tools to assist their child in effectively coping with these experiences. Thus, these findings further highlight the need for educators and healthcare providers to be aware that WBV may be a common concern among families. In schools, there may be a need for increased vigilance and responsiveness to WBV from educators, teachers, guidance counselors, social workers, and administrators to ensure that weight-based bullying is treated as seriously as other forms of bullying in the school setting. Schools and educators can also help parents support their children who may be vulnerable to WBV, such as efforts to teach youth help-seeking behaviors, reinforce appropriate social skills, or provide assistance in obtaining supportive mental health services, if needed.
In the healthcare setting, providers can also address this issue by looking for signs that youth may be experiencing WBV, such as associated psychological distress among those who are overweight or obese. For example, providers can use empirically validated measures to assess for depression, anxiety, and other psychological symptoms that may be present for overweight or obese youth. By discussing WBV with parents during patient visits with youth, providers can encourage parents to help their child use adaptive coping strategies to deal with WBV. Strategies such as offering emotional support to children at home, helping their child practice positive self-talk strategies to help buffer against low self-esteem, and assisting their child to implement problem-focused coping strategies (e.g., developing concrete plans to avoid bullies or enlist support of teachers at school) are examples of approaches that parents can implement to help foster their child's well-being in the face of bullying.
Finally, in light of the present findings, which demonstrate substantial parental concern about WBV and its consequences for youth, it is concerning that weight-based bullying has remained primarily absent in recent initiatives to address youth bullying on both the state and national level. For example, despite widely publicized national campaigns to address bullying in youth, such as the “Born This Way” campaign and the “It Gets Better” campaign, which aim to reduce victimization of lesbian, gay, bisexual, and transgender youth, there has been an absence of discourse about WBV in antibullying campaigns and the popular media,37 as well as a lack of research to develop and test interventions to reduce WBV in youth. This is an important and needed area for future research and policy initiatives.
Several limitations should be noted. Recruitment of participants was limited to those who had access to a computer with an Internet connection, and it is not known whether parents in the study had children who had sought treatment for their weight or WBV. This study also relied on self-report data for parental perceptions of their child, as well as body weight and height for parents and children. However, evidence has demonstrated fairly high concordance between parent and child reports of victimization,38 as well as measured versus self-reported values for height and weight.39 Although the racial distribution of the sample resembled that of US Census data, it will be important for future work to more closely examine parental perspectives of WBV among ethnic minorities whose vulnerability and experiences may be different. Similarly, future studies should investigate urban versus rural settings, as well as specific regions of the country, to identify whether there are differences in parental perceptions of WBV and resources available to address this problem.
Conclusions
In light of recent evidence documenting that both nonclinical and treatment-seeking youth experience pervasive WBV,34,35 the present study indicates that parents, too, have substantial concerns about WBV and its health consequences for youth. This has important implications for both educators in schools and clinical intervention and treatment by health providers, who can play a valuable role in helping families by looking for signs of teasing and bullying in youth, identifying psychological distress that may be related to WBV, and talking to parents about their concerns of WBV and ways to provide support to help their child adaptively cope with WBV. Though these efforts seem particularly warranted for parents of youth who are overweight or obese, the present findings suggest that WBV is a common concern among parents even if their child is not struggling with weight and is, potentially, a broader problem for youth. Thus, it may be important for increased awareness of WBV to promote efforts to identify these experiences among youth and associated concerns among parents, regardless of their body size.
Acknowledgment
Research and project support were provided by the Rudd Center for Food Policy & Obesity.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Shepherd S. White house conference tackles bullying. CNN Politics. 2011. Available at www.cnn.com/2011/POLITICS/03/10/obama.bullying/index.html Last accessed July17, 2013
- 2.Hu W. Bullying law puts New Jersey schools on spot. The New York Times. 2011. Available at www.nytimes.com/2011/08/31/nyregion/bullying-law-puts-new-jersey-schools-on-spot.html?pagewanted=all&_r=0 Last accessed February2, 2013
- 3.Pepler D, Craig W, Jiang D, et al. . Developmental trajectories of bullying and associated factors. Child Dev 2008;79:325–338 [DOI] [PubMed] [Google Scholar]
- 4.Puhl RM, Luedicke J, Heuer C. Weight-based victimization toward overweight adolescents: Observations and reactions of peers. J School Health 2011;81:696–703 [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, et al. . Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:E1–E8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eisenberg ME, Neumark-Sztainer D, Story M. Associations of weight-based teasing and emotional well-being among adolescents. Arch Pediatr Adolesc Med 2003;157:733–738 [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg ME, Neumark-Sztainer D, Haines J, et al. . Weight-teasing and emotional well-being in adolescents: Longitudinal findings from Project EAT. J Adolesc Health 2006;38:675–683 [DOI] [PubMed] [Google Scholar]
- 8.Haines J, Neumark-Sztainer D, Eisenberg ME, et al. . Weight teasing and disordered eating behaviors in adolescents: Longitudinal findings from Project EAT (Eating Among Teens). Pediatrics 2006;117:209–215 [DOI] [PubMed] [Google Scholar]
- 9.Faith MS, Leone MA, Ayers TS, et al. . Weight criticism during physical activity, coping skills, and reported physical activity in children. Pediatrics 2002;110:e23–e31 [DOI] [PubMed] [Google Scholar]
- 10.Neumark-Sztainer D, Falkner N, Story M, et al. . Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. Int J Obes (Lond) 2002;26:123–131 [DOI] [PubMed] [Google Scholar]
- 11.Jensen CD, Steele RG. Brief report: Body dissatisfaction, weight criticism, and self-reported physical activity in preadolescent children. J Pediatr Psychol 2009;34:822–826 [DOI] [PubMed] [Google Scholar]
- 12.Krukowski RA, West DS, Perez AP, et al. . Overweight children, weight-based teasing and academic performance. Int J Pediatr Obes 2009;4:274–280 [DOI] [PubMed] [Google Scholar]
- 13.Puhl RM, Luedicke J. Weight-based victimization among adolescents in the school setting: Emotional reactions and coping behaviors. J Youth Adolesc 2012;41:27–40 [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Iannotti RJ, Nansel TR. School bullying among adolescents in the United States: Physical, verbal, relational and cyber. J Adolescent Health 2009;45:368–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sawyer JL, Mishna F, Pepler D, et al. . The missing voice: Parents' perspectives of bullying. Childr Youth Serv Rev 2011;33:1795–1803 [Google Scholar]
- 16.Baldry AC, Farrington DP. Bullies and delinquents: Personal characteristics and parental styles. J Community Appl Soc 2000;10:17–31 [Google Scholar]
- 17.Kaufmann D, Gesten E, Santa Lucia RC, et al. . The relationship between parenting style and children's adjustment: The parents' perspective. J Child Fam Stud 2000;9:231–245 [Google Scholar]
- 18.Smith PK, Myron-Wilson R. Parenting and school bullying. Clin Child Psychol Psychiatry 1998;3:405–417 [Google Scholar]
- 19.Nordhagen R, Nielsen A, Stigum H, et al. . Parental reported bullying among Nordic children: A population-based study. Child Care Health Dev 2005;31:693–701 [DOI] [PubMed] [Google Scholar]
- 20.Stockdale MS, Hangaduambo S, Duys D, et al. . Rural elementary students', parents', and teachers' perceptions of bullying. Am J Health Behav 2002;26:266–277 [DOI] [PubMed] [Google Scholar]
- 21.Glover M, Kira A, Scragg R, et al. . Smoking is rank! But, not as rank as other drugs and bullying say New Zealand parents of pre-adolescent children. Health Promot J Austr 2011;22:223–227 [DOI] [PubMed] [Google Scholar]
- 22.Davis MM, Clark SJ, Singer DC, et al. . Drug abuse now equals childhood obesity as top health concern for kids. The C.S. Mott Children's Hospital National Poll on Children's Health. 2011. Available at http://mottnpch.org/sites/default/files/documents/081511toptenreport.pdf Last accessed January25, 2013
- 23.Davis MM, Clark SJ, Singer DC, et al. . Bullying worries parents of overweight and obese children. The C.S. Mott Children's Hospital National Poll on Children's Health. 2008. Available at http://mottnpch.org/sites/default/files/documents/090808_bully_report_0.pdf Last accessed February10, 2013
- 24.Survey Sampling International The science of sampling. 2011. Available at www.surveysampling.com/ Last accessed July30, 2013
- 25.Puhl RM, Peterson JL, Luedicke J. Parental perceptions of weight terminology that providers use with youth. Pediatrics 2011;128:e786–e793 [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Division of Nutrition, Physical Activity, and Obesity Defining overweight and obesity. Overweight and obesity. 2012. Available at www.cdc.gov/nccdphp/dnpa/obesity/defining.htm Last accessed July30, 2013
- 27.Ogden C, Carroll MD, Curtin LR, et al. . Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295:1549–1555 [DOI] [PubMed] [Google Scholar]
- 28.Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010 Census briefs. 2011. Available at www.census.gov/prod/cen2010/briefs/c2010br-02.pdf Last accessed July17, 2013
- 29.United States Census Bureau. Money income of households-percent distribution by income level, race, and hispanic origin in constant (2008) dollars: 1980–2008. Income, Expenditures, Poverty, and Wealth, US Census Bureau Statistical Abstract of the United States. 2011. Available at www.census.gov/compendia/statab/2011/tables/11s0689.pdf Last accessed July31, 2013
- 30.Ogden CL, Kuczmarski RJ, Flegal KM, et al. . Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002;109:45–60 [DOI] [PubMed] [Google Scholar]
- 31.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007;120:s164–s192 [DOI] [PubMed] [Google Scholar]
- 32.Janssen I, Craig WM, Boyce WF, et al. . Associations between overweight and obesity and bullying behaviors in school-aged children. Pediatrics 2004;113:1187–1193 [DOI] [PubMed] [Google Scholar]
- 33.Griffiths LJ, Wolke D, Page AS, et al. . Obesity and bullying: Different effects for boys and girls. Arch Dis Child 2006;91:121–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Puhl RM, Peterson JL, Luedicke J. Strategies to address weight-based victimization: Youths' preferred support interventions from classmates, teachers, and parents. J Youth Adolesc 2012:1–13 [DOI] [PubMed] [Google Scholar]
- 35.Puhl RM, Peterson JL, Luedicke J. Weight-based victimization: Bullying experiences of weight-loss treatment-seeking youth. Pediatrics 2013;131:e1–e9 [DOI] [PubMed] [Google Scholar]
- 36.Puhl RM, Latner JD. Stigma, obesity, and the health of the nation's children. Psychol Bull 2007;133:557–580 [DOI] [PubMed] [Google Scholar]
- 37.Puhl RM.A glaring omission in efforts to address youth bullying. Sizable issues.2011. Available at http://boards.medscape.com/forums/?128@@.2a0e7528!comment=1 Last accessed February14, 2013
- 38.Shakoor S, Jaffee SR, Andreou P, et al. . Mothers and children as informants of bullying victimization: Results from an epidemiological cohort of children. J Abnorm Child Psychol 2011;39:379–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stommel M, Osier N. Temporal changes in bias of body mass index scores based on self-reported height and weight. Int J Obes (Lond) 2012;37:461–467 [DOI] [PMC free article] [PubMed] [Google Scholar]