Abstract
Individuals 65 years of age and over have the highest rates of traumatic brain injury (TBI)-related hospitalizations and deaths, and older adults (defined variably across studies) have particularly poor outcomes after TBI. The factors predicting these outcomes remain poorly understood, and age-specific care guidelines for TBI do not exist. This study provides an overview of TBI in older adults using data from the National Trauma Data Bank (NTDB) gathered between 2007 and 2010, evaluates age group-specific trends in rates of TBI over time using U.S. Census data, and examines whether routinely collected information is able to predict hospital discharge status among older adults with TBI in the NTDB. Results showed a 20–25% increase in trauma center admissions for TBI among the oldest age groups (those >=75 years), relative to the general population, between 2007 and 2010. Older adults (>=65 years) with TBI tended to be white females who have incurred an injury from a fall resulting in a “severe” Abbreviated Injury Scale (AIS) score of the head. Older adults had more in-hospital procedures, such as neuroimaging and neurosurgery, tended to experience longer hospital stays, and were more likely to require continued medical care than younger adults. Older age, injury severity, and hypotension increased the odds of in-hospital death. The public health burden of TBI among older adults will likely increase as the Baby Boom generation ages. Improved primary and secondary prevention of TBI in this cohort is needed.
Key words: : adult brain injury, epidemiology, geriatric brain injury, traumatic brain injury
Introduction
Traumatic brain injury (TBI) is a leading cause of death and disability in the United States. Individuals over the age of 65 years have the highest rates of TBI-related hospitalizations and deaths,1–3 and in 2010, annual hospital charges for treating TBI patients 65 years and older exceed $2 billion.4 Relative to younger people, older adults who sustain a TBI tend to have particularly poor outcomes5,6 and slower recovery,7 even after milder injuries.8,9 Rates of TBI-related emergency department (ED) visits and hospitalizations begin to increase dramatically as early as age 50 among females, and rates of injury increase even earlier among males.1 Though the size of the older adult population is increasing rapidly, some evidence suggests that TBI-related trauma visits among older adults are increasing at a rate that exceeds population growth.1
The poor postinjury outcomes often observed among older adults5,6,8,10 suggest that TBI in older adults may represent a clinical condition that is distinct from that observed in younger adults. Unlike younger adults who most commonly incur TBI in accidents that are unlikely to be related to, or reflective of, their overall health status (e.g., motor vehicle crashes), the majority of TBIs among older adults are the result of falls.1 Several aspects of aging may contribute to fall risk, including imbalance, frailty, joint disorders, chronic medical conditions, and medication interactions.11 It is therefore possible that falls are actually a symptom of age-related decline. In aging, the brain undergoes widespread atrophy or brain shrinking, neuronal shrinkage, reduced synaptic density, and decreased neural plasticity.12,13 The effects of a TBI are then overlaid upon the age-related structural and functional changes known to occur in the aging brain, which likely affects the course of recovery after injury. Thus, the aging brain may be more vulnerable to damage, such that significant injury can result from a milder blow, and there is less “reserve” with which to recover. The presence of multiple pre-existing medical comobidities and the polypharmacy required to manage comorbid conditions may make TBI harder to diagnose and treat in older adults and may increase the risk for secondary complications. Anticoagulant therapy, in particular, has been associated with poorer outcomes after TBI, including increased incidence of intracranial hemorrhage (even among individuals with an initial Glasgow Coma Scale [GCS] score of 15),14 longer lengths of hospital stay, and greater in-hospital mortality.14,15 The possibility that older adults are more vulnerable to more secondary complications after TBI is consistent with research indicating that younger people are more frequently seen in EDs and discharged, whereas older adults more often require hospital admission for TBIs of similar severity.12
Although ambulatory guidelines provide for special considerations for the transport of older adults to a trauma center in the event of a TBI,16 existing guidelines for the treatment of severe TBI do not address any special needs of the older adult population.17 Relatedly, specific risk factors for poor TBI outcomes among older adults are poorly understood. A preliminary step in establishing standards for the care of older adults with TBI is identifying the demographic, injury, and care-related factors that account for poor outcomes in this population. Several studies have evaluated general trauma outcomes (e.g., extracranial injury) in older adults, and findings indicate that, in addition to factors such as age, race, gender, and mechanism of injury,18,19 pre-existing medical conditions and in-hospital complications can have a significant effect on outcomes.20,21 To date, the affect of many of these factors on TBI outcomes among older adults have not been comprehensively examined.
The current article endeavors to (1) provide an updated overview of TBI in older adults using data from the National Trauma Data Bank (NTDB) gathered between 2007 and 2010, (2) evaluate age group-specific trends in rates of TBI over time using U.S. Census data, and (3) identify demographic, injury, and care-related factors that predict hospital discharge status among older adults with TBI in the NTDB.
Methods
Inclusion/exclusion criteria
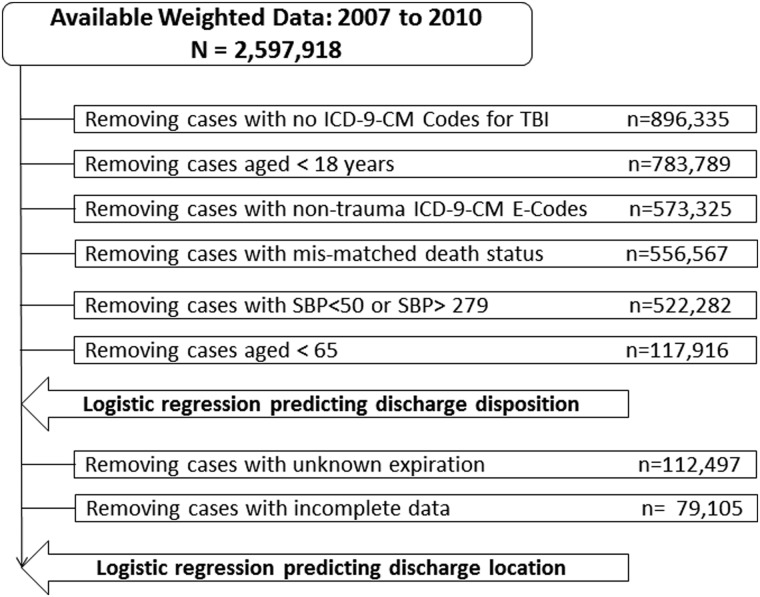
The NTDB National Sample Program (NTDB-NSP) is maintained by the American College of Surgeons and contains records voluntarily submitted by over 80 level I or II trauma centers in the United States.22 For the current study, 4 years of population-weighted data sets from the NTDB-NSP (2007–2010) were acquired and merged for analysis. Information on the sampling design can be found in Goble and colleagues.23 Inclusion criteria were (1) at least one diagnosis code that met the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), case definition of TBI established by the Centers for Disease Control and Prevention (CDC; 800.0–801.9, 803.0–804.9, 850.0–854.1, 950.1–950.3, and 959.01).24 Rules for inclusions and exclusions, as shown in Figure 1, were (1) 995.55 was not included, because it was not expected that adults would incur TBI as a result of shaken baby syndrome, (2) cases where age was known and was 18 years or older were included, (3) cases where the initial admission was to a trauma facility were included (transfers were excluded), (4) cases with an etiology of injury that could logically result in a TBI were included (e.g., cases with etiology codes of asphyxiation, poisoning, drug or medication overdose, and so on, were removed), (5) cases where the ED and hospital dispositions did not follow a logical order were excluded (e.g., cases coded as expired at ED discharge and alive at hospital discharge represented clear data entry or coding errors and were removed), and (6) cases with extreme values (<50 or >279) for systolic blood pressure (SBP) were removed. A total of 522,882 cases were retained for analysis.
FIG. 1.
Data reduction steps. ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; TBI, traumatic brain injury; SBP, systolic blood pressure.
For subanalysis examining characteristics of TBI in older adults, these data (described below) included various data limitations, including removal of cases that were younger than 65, had an unknown expiration status or had expired, or had incomplete data for at least one injury-related or demographic variable. Figure 1 provides a representation of all data limitation steps invoked, including the number of cases retained after each step and the number of cases available for each analysis. Two subanalyses of these data that included cases from NTDB facilities with a minimum of 80% complete data for procedure coding and complication data entry resulted in samples sizes of 46,645 and 25,037, respectively.
Variables of interest
Demographics
Demographic variables of interest included age, gender, and race or ethnicity. Age was grouped into six categories to allow for closer investigation of older (age 55+) and mature adulthood (45–54), which is when rates of TBI begin to increase1 and some vulnerability to negative outcomes may be present;25 these categories are as follows: 18–44, 45–54, 55–64, 65–74, 75–84, and 85 years and older. Race and ethnicity was categorized by condensing all race and ethnic variables in the NTDB data sets into the following groups: white, black, Hispanic, Asian, Native American/Alaskan/Hawaiian, and other.
Injury etiology
Injury etiology was determined by reviewing the primary and additional ICD-9-CM external cause of injury codes (E-codes) attached to each case. A schema was applied to condense the E-codes into meaningful categories and distinguish those that could reasonably cause a TBI (i.e., falls, natural or environmental [e.g., accident resulting from cataclysmic earth movements and eruptions] or mechanical [e.g., accident caused by machinery], cut or pierce, sports, struck by or against [e.g., struck by falling object], suicide attempt [involving physical trauma], motor vehicle incident, and violence or unintentional explosions) and those that could not result in a TBI (fire, burn, or scald, hypoxia or anoxia, late effects of traumatic injury, leisure, poison, medication or surgical, and environmental or weather [fires, floods, or droughts]). For all cases included in these analyses, either the primary or additional E-code was one that could reasonably cause a TBI. If neither the primary nor additional E-code was also considered to be TBI related, or if the case was missing an E-code, the case was excluded from analysis.
Injury severity
TBI severity was characterized using the GCS score26 taken at admission to the ED and also by using the maximum Abbreviated Injury Scale (AIS) score of the head27 derived from the ICDMAP algorithm (calculated AIS scores are included in the NTDB database).28 Additional indices of overall injury severity included total hospital length of stay (LOS) and SBP at admission to the ED. GCS scores were collapsed into the categories of mild (13–15), moderate (9–12), and severe (3–8). Maximum AIS score for the head region was retained in its original format, using the following scale: minor (1); moderate (2); serious (3); severe (4); critical (5); and unsurvivable (6). Total hospital LOS in the NTDB is entered in days, so the following categories were used in the current study: 1 day; 2 days to 1 week; more than 1 week to 2 weeks; more than 2 weeks to 3 weeks; more than 3 weeks to 1 month; and more than 1 month to 1 year. SBP was categorized using schema recommended by the American Heart Association29: (1) 50–89, hypotension; (2) 90–119, normal; (3) 120–139, prehypertension; (4) 140–159, stage 1 hypertension; (5) 160–179, stage 2 hypertension; and (6) ≥180, hypertensive crisis. SBP measures of less than 50 and 280 or greater were removed, because these were assumed to be data entry errors.
Pre-existing medical conditions
Extensive missing data for pre-existing conditions indicates that these are very rarely reported in the NTDB, preventing their inclusion in the current study.
In-hospital complications
The NTDB allows for entry of a large number of in-hospital complications, so, for the purposes of the current project, we limited our focus to the 10 most commonly occurring complications (identified by complication codes used in the NTDB that are based primarily on ICD-9-CM codes) among patients with TBI over the age of 64. These included acute renal failure, acute respiratory distress syndrome (ARDS), cardiac arrest with cardiopulmonary resuscitation (CPR), decubitus ulcer, drug or alcohol withdrawal syndrome, increased intracranial pressure (ICP), myocardial infarction, pneumonia, stroke or cerebral vascular accident (CVA), and systemic sepsis. As indicated above, analyses using complications only used data from those facilities that had 80% or greater completion rates for complication code entry, which included 24 facilities.
Procedures
Before identifying the 10 most commonly occurring procedures (based on ICD-9-CM procedure codes abstracted from patient medical records and entered into the NTDB) among patients with TBI over the age of 64, procedures deemed similar in technique were condensed into one-procedure code categories. For example, codes for “closed reduction of fracture” for all extremities were condensed into one category. The 10 most commonly occurring procedure code categories included application of an external fixation device, closed reduction of a fracture, computerized axial tomography (CT) of the head, incision of the cerebral meninges, insertion of tracheostomy tube, insertion of indwelling urinary catheter, ICP monitoring, magnetic resonance imaging (MRI) of the brain or brainstem, open reduction of a fracture, other craniotomy, other CT, other X-ray, routine chest X-ray, transfusion, and venous catheterization. Analyses including procedures used data from those facilities that had 80% or greater completion rates for procedure code entry, which included 39 facilities.
Discharge disposition
Discharge status was characterized by using data from both ED discharge and hospital discharge, when applicable. Overall discharge disposition was categorized as alive or expired, accounting for expiration at ED or hospital discharge. Cases that did not expire during hospitalization were further grouped into categories according to discharge destination; these categories included home with no assistance, home with health aid, intermediate care facility (ICF) or hospice care, acute hospital or some other type of hospital (e.g., short-term general hospital), skilled nursing facility (SNF), leaving against medical advice (AMA), and inpatient rehabilitation. To identify factors that predict discharge outcomes among survivors, we further grouped these categories for use in logistic regression (described below) to distinguish between community settings (in this case, discharge home with no assistance or home with health aid) and institutional settings (continued medical care, comprising all other discharge categories), as is commonly noted in the rehabilitation literature.30
Statistical analysis
The first series of analyses conducted were descriptive. The distribution of demographic, injury, and discharge disposition characteristics were calculated for each of the age groups defined above; distributions of most commonly reported procedures and complications were also calculated for each age group.
Rates of TBI-related admissions relative to population characteristics provided by the U.S. Census were also calculated for each year from 2007 through 2010. Change in TBI-related admissions relative to population growth was also calculated for this 4-year period. The 2010 Bridged Census data were used to calculate rates.31
Cross-tabulations of injury etiology and age groups were completed for all cases age 65 and older meeting inclusion criteria, as were cross-tabulations of injury etiology and GCS score. Two series of backward stepwise logistic regressions were conducted to identify variables that were predictive of discharge outcomes among individuals who were 65 years and older at the time of injury: (1) discharge status (expired or alive) and (2) discharge location (continued medical care or home with or without health aid) for those patients discharged alive. Variables were entered into models in progressive categorical blocks. The first block included the demographic variables age group, gender, and race. The second block included injury etiology, whereas the third block included the severity-related variables, ED GCS score, maximum AIS of the head, LOS, and SBP. The fourth block included independently entered interaction terms of interest (age group by injury etiology, age group by GCS, and age group by AIS score of the head). An additional series of backward stepwise logistic regressions was computed, including only those cases that had 80% or greater in-hospital complication and procedure code data entry, respectively, with variables from each of these categories entered as a final (fifth) block. For all models, categories of each included variable were evaluated for confounding by comparing the results of models that included each variable independently (not presented here) with those that included multiple variables. If confounding was discovered, the variable providing the least predictive power was removed from the final models. All analyses were completed with SPSS statistical software (19.0; SPSS, Inc., Chicago, IL).32 Study methods were approved by an independent institutional review board (HCA-Health ONE).
Results
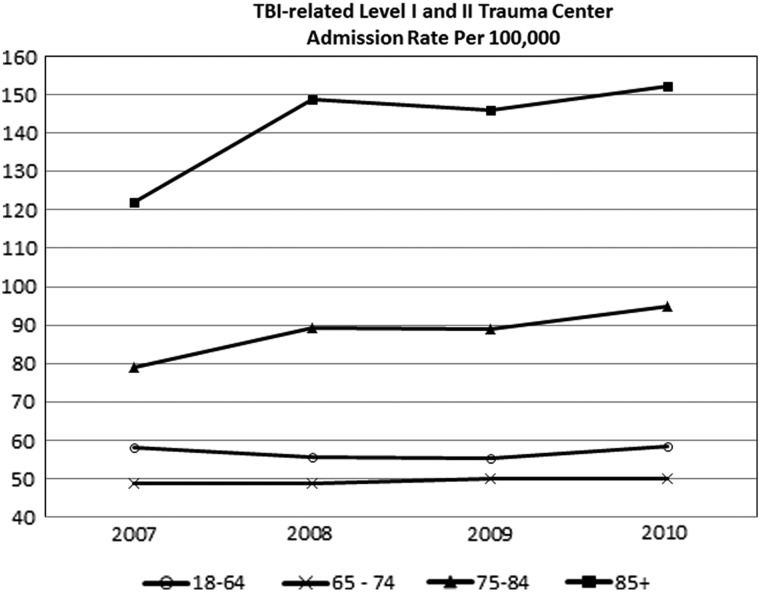
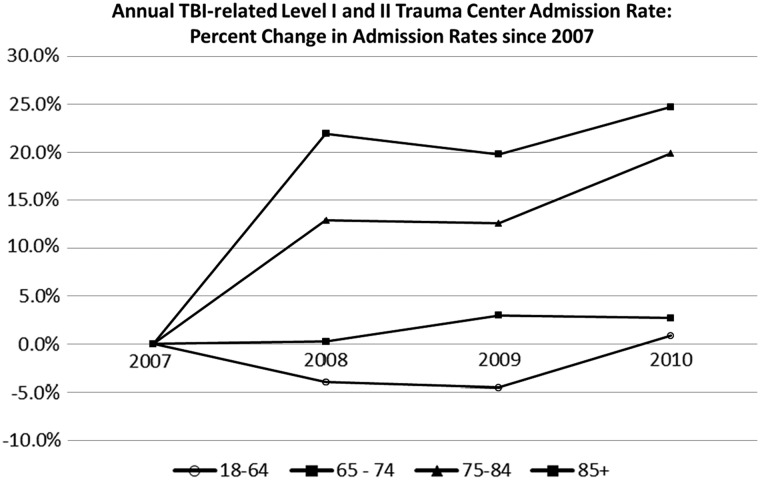
The rate of TBI-related admissions at level I or II trauma centers was highest for adults 85 years of age and older, with an increase from 122 per 100,000 to 152 per 100,000 population between 2007 and 2010 (see Fig. 2). It should be noted that the most marked increase is apparent between the years 2007 and 2008. As shown in Figure 3, this equates to a 25% increase in admissions among the 85 and older group, relative to the general adult population, between 2007 and 2010. The next highest rates of TBI-related trauma admissions are for adults 75–84 years of age, with rates starting at 79 per 100,000 in 2007 and ending at 94 per 100,000 population in 2010 (see Fig. 2), which equates to a 20% increase over the 4-year period (see Fig. 3). Rates for adults 18–64 and 65–74 were lowest, with little change over the years reviewed.
FIG. 2.
TBI-related level I and II trauma center admission rate (per 100,000). TBI, traumatic brain injury.
FIG. 3.
Percent change in annual TBI-related level I and II trauma center admission rates since 2007. TBI, traumatic brain injury.
Demographic, injury, and discharge-related descriptive characteristics are summarized in Table 1. There were many descriptive differences in the data between age groups that were not statistically tested. Most comparisons would likely be statistically significant given the large sample size in the current study; here, we highlight key findings. Younger adults (<65 years of age) with TBI tended to be white males who have incurred an injury in a motor vehicle incident resulting in “minor” AIS of the head severity scores. Older adults (>=65 years) with TBI tended to be white females who have incurred an injury from a fall resulting in a “severe” AIS score of the head. The proportion of people who sustained more severe injuries (as measured by Head AIS) and who expired in the hospital appears to increase with age, but the patterns of missing data for these outcomes (namely, less missing data as age increases) raised the concern that missing data may reflect more severe injuries and initially limited our confidence in this finding. However, the vast majority of cases with missing Head AIS scores were discharged home with no assistance (63%) or home with assistance (an additional 4%), suggesting that many cases with missing Head AIS scores actually sustained milder injuries.
Table 1.
Level I and II Trauma Centers: Weighted Age Group Characteristics of Patients Included in the 2007, 2008, 2009, and 2010 NTDB-NSP Data Sets with a Diagnosis of TBIa
| |
Age groups (in years) |
|||||
|---|---|---|---|---|---|---|
| Characteristics | 18–44 (%) (n=266,836) | 45–54 (%) (n=87,781) | 55–64 (%) (n=57,445) | 65–74 (%) (n=37,503) | 75–84 (%) (n=43,717) | 85 and older (%) (n=29,600) |
| Gender | ||||||
| Female |
25.5 |
26.6 |
30.4 |
38.5 |
50.4 |
62.2 |
| Male |
74.1 |
73.0 |
69.1 |
61.1 |
49.0 |
37.5 |
| Missing |
0.4 |
0.4 |
0.5 |
0.5 |
0.6 |
0.4 |
| Race/ethnicity | ||||||
| White |
57.8 |
65.2 |
69.1 |
73.2 |
79.2 |
82.7 |
| Black |
15.3 |
15.5 |
11.8 |
8.5 |
4.6 |
3.8 |
| Hispanic |
13.1 |
7.9 |
6.7 |
7.3 |
5.6 |
4.6 |
| Asian |
1.8 |
1.6 |
2.4 |
3.0 |
2.7 |
2.5 |
| Native American, Alaskan, or Hawaiian |
0.9 |
0.9 |
0.8 |
0.4 |
0.4 |
0.3 |
| Other |
4.1 |
3.1 |
2.9 |
2.8 |
1.9 |
1.2 |
| Missing |
7.0 |
5.8 |
6.3 |
4.7 |
5.5 |
4.9 |
| TBI etiology | ||||||
| Falls |
13.4 |
25.9 |
37.0 |
54.8 |
72.9 |
84.9 |
| Natural/environmental/mechanical |
4.5 |
4.4 |
4.5 |
3.0 |
1.6 |
0.7 |
| Cut/pierce |
0.1 |
0.1 |
0.1 |
0.0 |
0.0 |
0.0 |
| Sports |
0.1 |
0.0 |
0.1 |
0.0 |
0.1 |
0.0 |
| Struck by/against |
1.9 |
1.6 |
1.6 |
1.7 |
0.7 |
0.6 |
| Suicide attempt |
1.3 |
1.2 |
1.0 |
0.8 |
0.8 |
0.5 |
| Motor vehicle crash |
61.9 |
51.2 |
49.6 |
36.7 |
23.1 |
12.5 |
| Violence or explosion |
16.8 |
15.5 |
6.1 |
3.0 |
0.9 |
0.7 |
| GCS at ED admission | ||||||
| Mild |
75.7 |
77.2 |
77.5 |
79.5 |
77.3 |
76.5 |
| Moderate |
4.8 |
4.9 |
4.8 |
3.7 |
4.5 |
6.0 |
| Severe |
16.3 |
14.4 |
12.9 |
10.6 |
8.7 |
7.2 |
| Missing |
3.2 |
3.6 |
4.9 |
6.3 |
9.4 |
10.3 |
| AIS of the head on admission | ||||||
| 1–minor |
2.3 |
2.5 |
1.9 |
1.7 |
1.9 |
1.9 |
| 2–moderate |
30.7 |
25.8 |
24.0 |
20.3 |
15.8 |
17.4 |
| 3–serious |
12.2 |
14.7 |
15.0 |
16.7 |
17.0 |
15.2 |
| 4–severe |
21.9 |
26.0 |
29.7 |
37.5 |
44.3 |
46.2 |
| 5–critical |
4.3 |
4.6 |
5.3 |
5.2 |
6.0 |
5.3 |
| 6–unsurvivable |
0.1 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
| Missing |
28.5 |
26.4 |
24.1 |
18.5 |
14.9 |
14.1 |
| Status at discharge | ||||||
| Alive |
85.1 |
86.1 |
86.2 |
86.0 |
82.9 |
81.4 |
| Expired |
4.8 |
6.2 |
7.6 |
9.5 |
13.7 |
15.0 |
| Missing |
10.1 |
7.7 |
6.2 |
4.5 |
3.4 |
3.6 |
| Final discharge disposition | ||||||
| Home with no assist |
68.5 |
64.2 |
58.0 |
47.9 |
35.2 |
24.1 |
| Home with home health |
2.3 |
3.1 |
3.4 |
5.6 |
6.6 |
6.7 |
| ICF or hospice |
2.5 |
2.7 |
3.6 |
4.3 |
4.2 |
3.1 |
| Acute and other hospital |
1.5 |
1.6 |
2.3 |
2.0 |
1.8 |
1.6 |
| SNF |
1.7 |
4.2 |
7.3 |
13.0 |
22.0 |
35.6 |
| Left AMA |
1.6 |
1.8 |
1.2 |
0.6 |
0.2 |
0.2 |
| Rehabilitation |
7.0 |
8.6 |
10.4 |
12.6 |
12.7 |
10.2 |
| Expired |
4.4 |
5.7 |
7.0 |
8.9 |
12.8 |
14.1 |
| Missing |
10.5 |
8.2 |
6.8 |
5.1 |
4.3 |
4.5 |
| Hospital LOS | ||||||
| 1 day |
0.6 |
0.7 |
0.9 |
0.5 |
0.6 |
0.1 |
| 2 days to 1 week |
59.1 |
64.8 |
65.4 |
69.5 |
76.7 |
81.5 |
| More than 1 week to 2 weeks |
4.0 |
4.7 |
6.6 |
6.5 |
5.0 |
3.5 |
| More than 2 weeks to 3 weeks |
3.0 |
3.8 |
4.2 |
3.9 |
3.3 |
1.8 |
| More than 3 weeks to 1 month |
2.7 |
3.5 |
3.4 |
3.1 |
2.2 |
0.9 |
| More than 1 month to 1 year |
30.4 |
22.5 |
19.3 |
16.5 |
12.3 |
12.1 |
| Missing |
0.6 |
0.7 |
0.9 |
0.5 |
0.6 |
0.1 |
| SBP | ||||||
| 50– 89 |
2.3 |
3.2 |
3.1 |
2.4 |
2.4 |
2.1 |
| 90–119 |
19.5 |
17.7 |
16.1 |
14.1 |
11.2 |
9.2 |
| 120–139 |
37.1 |
29.3 |
25.0 |
22.0 |
19.1 |
19.2 |
| 140–159 |
29.5 |
29.8 |
28.4 |
29.0 |
29.0 |
26.3 |
| 160–179 |
8.0 |
12.6 |
16.4 |
18.0 |
19.4 |
20.5 |
| 180–279 |
3.5 |
7.4 |
11.0 |
14.6 |
18.7 |
22.7 |
| Missing | 2.3 | 3.2 | 3.1 | 2.4 | 2.4 | 2.1 |
(n=522,882).
NTDB-NSP, National Trauma Data Bank National Sample Program; TBI, traumatic brain injury; GCS, Glasgow Coma Scale; ED, emergency department; AIS, Abbreviated Injury Score; ICF, intermediate care facility; SNF, skilled nursing facility; AMA, against medical advice; LOS, length of stay; SBP, systolic blood pressure.
In-hospital death occurred more frequently in older adults, 65 and over with TBI (9.5–15.0%), as compared to younger adults with TBI (4.8–7.6%). Older adults had progressively higher rates of elevated SBP (>120 mmHg) at admission to the ED. Younger adults with TBI were more likely to experience very long LOS (30.4% of individuals <45 years had LOS between 1 month and 1 year, as compared to 12.1–16.5% of those >=65 years), whereas older adults with TBI more commonly experienced shorter LOS (69.5–81.5% remained hospitalized for between 1 day and 1 week), as compared to those under 45 years of age (59.1%). Among those discharged alive, older adults were more frequently admitted to SNFs than younger adults. Younger adults were most frequently discharged to home with no assistance. Frequencies across all characteristics are presented in Table 1.
In-hospital complications are not widely reported in the NTDB. For those facilities that had 80% or greater rates of complication code completion, individuals with TBI experienced pneumonia, drug and alcohol withdrawal syndrome, and acute respiratory distress syndrome most frequently. Older adults had slightly higher rates of cardiac arrest and acute renal failure; however, these differences were minor. Rates of the 10 most frequently reported complications are presented for each age group in Table 2A.
Table 2A.
Level I and II Trauma Centers: Distribution of Most Common Complications of Patients with a Diagnosis of TBI by Age Group for Facilities With 80% or Greater Complication Data Entrya
| |
Age groups (in years) |
|||||
|---|---|---|---|---|---|---|
| Most frequently listed complications | 18–44 (%) (n=81,369) | 45–54 (%) (n=25,831) | 55–64 (%) (n=18,118) | 65–74 (%) (n=11,356) | 75–84 (%) (n=11,692) | 85 and older (%) (n=7945) |
| Acute renal failure | ||||||
| Present |
0.6 |
0.7 |
1.3 |
2.2 |
2.3 |
1.8 |
| Absent |
91.8 |
92.0 |
93.2 |
91.1 |
92.0 |
92.2 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| ARDS | ||||||
| Present |
2.1 |
2.3 |
2.9 |
3.2 |
2.7 |
1.9 |
| Absent |
90.4 |
90.4 |
91.5 |
90.1 |
91.6 |
92.1 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Cardiac arrest with CPR | ||||||
| Present |
0.6 |
1.0 |
1.2 |
1.4 |
2.1 |
1.8 |
| Absent |
91.8 |
91.7 |
93.3 |
91.8 |
92.2 |
92.3 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Decubitus ulcer | ||||||
| Present |
0.8 |
1.1 |
1.5 |
1.9 |
0.9 |
1.4 |
| Absent |
91.7 |
91.5 |
93.0 |
91.4 |
93.5 |
92.7 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Drug or alcohol withdrawal syndrome | ||||||
| Present |
1.7 |
2.0 |
3.2 |
3.7 |
2.6 |
2.0 |
| Absent |
90.8 |
90.7 |
91.3 |
89.5 |
91.7 |
92.1 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Increased ICP | ||||||
| Present |
0.3 |
0.4 |
0.4 |
0.1 |
0.5 |
0.3 |
| Absent |
92.2 |
92.3 |
94.1 |
93.2 |
93.8 |
93.7 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Myocardial infarction | ||||||
| Present |
0.1 |
0.2 |
0.4 |
0.8 |
1.0 |
0.9 |
| Absent |
92.4 |
92.5 |
94.0 |
92.5 |
93.3 |
93.1 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Pneumonia | ||||||
| Present |
5.6 |
6.1 |
8.2 |
8.2 |
6.4 |
5.7 |
| Absent |
86.9 |
86.6 |
86.3 |
85.1 |
87.9 |
88.3 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Stroke or CVA | ||||||
| Present |
0.2 |
0.6 |
0.8 |
0.8 |
0.7 |
0.1 |
| Absent |
92.2 |
92.1 |
93.7 |
92.4 |
93.6 |
93.9 |
| Unknown |
7.5 |
7.3 |
5.5 |
6.7 |
5.7 |
6.0 |
| Systemic sepsis | ||||||
| Present |
1.3 |
1.5 |
2.0 |
1.9 |
1.7 |
0.7 |
| Absent |
91.2 |
91.2 |
92.4 |
91.4 |
92.6 |
93.4 |
| Unknown | 7.5 | 7.3 | 5.5 | 6.7 | 5.7 | 6.0 |
(n=156,311).
TBI, traumatic brain injury; ARDS, acute respiratory distress syndrome; CPR, cardiopulmonary resuscitation; ICP, intracranial pressure; CVA, cerebral vascular accident.
In-hospital procedures were more commonly reported in the NTDB than were complications. For those facilities that had 80% or greater rates of procedure code completion, older adults were found to have higher rates of CT scans of the head, incisions of the cerebral meninges, MRIs of the brain and brainstem, routine chest X-rays, transfusions, and venous catheterizations. Younger adults were found to have higher proportions of many common procedures, compared to older adults, such as the application of external fixation devices to stabilize fractures (10.4–11.3%, compared to 6.5–10.5% for older adults), closed reduction of fracture (4.3–6.1%, compared to 2.1–4.1% for older adults), and open reductions of fractures (7.58.9%, compared to 2.4–4.6%) and insertion of tracheostomy tubes (13.7–15.6%, compared to 3.7–9.2% for older adults). However, CT scans were less common for younger than older adults (74.8–77.3%, compared to 79.4–83.2% for older adults). Full descriptive data for these variables are listed in Table 2B.
Table 2B.
Level I and II Trauma Centers: Distribution of Most Common Procedures by Age Group for Facilities With 80% or Greater Complication Data Entrya
| |
Age groups (in years) |
|||||
|---|---|---|---|---|---|---|
| Most common procedures | 18–44 (%) (n=102,820) | 45–54 (%) (n=36,280) | 55–64 (%) (n=21,542) | 65–74 (%) (n=13,404) | 75–84 (%) (n=16,142) | 85 and older (%) (n=10,216) |
| Application of an external fixation device | ||||||
| Present |
10.4 |
11.3 |
10.6 |
10.5 |
6.5 |
6.6 |
| Absent |
84.1 |
83.1 |
83.6 |
83.7 |
87.1 |
86.2 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Closed reduction of fracture | ||||||
| Present |
6.1 |
4.3 |
5.5 |
4.1 |
2.6 |
2.1 |
| Absent |
88.3 |
90.2 |
88.6 |
90.1 |
91.1 |
90.8 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| CT of head | ||||||
| Present |
74.8 |
77.3 |
76.8 |
79.4 |
81.8 |
83.2 |
| Absent |
19.6 |
17.2 |
17.4 |
14.8 |
11.9 |
9.6 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Incision of cerebral meninges | ||||||
| Present |
1.4 |
2.2 |
3.5 |
4.2 |
6.0 |
2.1 |
| Absent |
93.1 |
92.3 |
90.7 |
90.0 |
87.6 |
90.7 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Insertion of a tracheostomy tube | ||||||
| Present |
15.6 |
13.7 |
14.6 |
9.2 |
7.5 |
3.7 |
| Absent |
78.9 |
80.8 |
79.6 |
85.0 |
86.1 |
89.2 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Insertion of indwelling catheter | ||||||
| Present |
15.2 |
14.6 |
17.1 |
16.6 |
17.1 |
19.1 |
| Absent |
79.3 |
79.8 |
77.1 |
77.6 |
76.5 |
73.8 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| ICP monitoring | ||||||
| Present |
1.2 |
1.2 |
1.2 |
0.3 |
0.1 |
0.1 |
| Absent |
93.3 |
93.3 |
93.0 |
93.9 |
93.5 |
92.7 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| MRI of the brain | ||||||
| Present |
1.9 |
2.4 |
4.7 |
6.4 |
7.1 |
5.9 |
| Absent |
92.5 |
92.1 |
89.5 |
87.8 |
86.6 |
86.9 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Open reduction of fracture | ||||||
| Present |
8.9 |
7.9 |
7.5 |
4.6 |
4.6 |
2.4 |
| Absent |
85.5 |
86.5 |
86.7 |
89.6 |
89.1 |
90.5 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Other craniotomy | ||||||
| Present |
2.3 |
2.7 |
2.7 |
2.9 |
3.5 |
1.6 |
| Absent |
92.1 |
91.8 |
91.5 |
91.3 |
90.2 |
91.2 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Other CT | ||||||
| Present |
50.7 |
51.5 |
51.9 |
51.7 |
45.0 |
45.6 |
| Absent |
43.8 |
42.9 |
42.2 |
42.5 |
48.7 |
47.3 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Other X-ray | ||||||
| Present |
8.7 |
9.1 |
9.3 |
8.1 |
6.6 |
6.6 |
| Absent |
85.8 |
85.4 |
84.9 |
86.0 |
87.1 |
86.3 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Routine chest X-ray | ||||||
| Present |
15.7 |
16.4 |
19.1 |
20.3 |
18.5 |
20.0 |
| Absent |
78.8 |
78.0 |
75.0 |
73.8 |
75.2 |
72.8 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Transfusion | ||||||
| Present |
4.0 |
4.8 |
6.1 |
8.0 |
10.8 |
9.1 |
| Absent |
90.5 |
89.6 |
88.0 |
86.2 |
82.9 |
83.8 |
| Unknown |
5.5 |
5.5 |
5.8 |
5.8 |
6.3 |
7.1 |
| Venous catheterization | ||||||
| Present |
12.4 |
15.1 |
18.3 |
22.6 |
22.3 |
20.6 |
| Absent |
82.1 |
79.4 |
75.9 |
71.5 |
71.3 |
72.3 |
| Unknown | 5.5 | 5.5 | 5.8 | 5.8 | 6.3 | 7.1 |
(n=200,404).
CT, computed tomography; ICP, intracranial pressure; MRI, magnetic resonance imaging.
Cross-tabulations of discharge status and injury etiology (Table 3) and of GCS score and injury etiology (Table 4) were calculated for adults 65 years of age and older. Among older adults receiving ED care, those who had an etiology of attempted suicide were most likely to expire in hospital (80.6%). The other most fatal injury etiologies among older adults were natural, environmental, or mechanical (18.4%) and sports (18.2%), followed by motor vehicle crashes (13.1%). Consistent with the gravity of injuries resulting from attempted suicide, 82.4% of older adults with an injury etiology of suicide attempt had a severe GCS score on admission to the ED. Etiologies of natural, environmental, or mechanical and sports were the next most likely to result in severe GCS (17.9 and 13.0%, respectively), with the remaining etiologies resulting in severe GCS in 0–10.3% of cases.
Table 3.
Level I and II Trauma Centers: Expiration Status by Injury Etiology of Patients 65 Years of Age and Older Included in the 2007, 2008, 2009, and 2010 NTDB-NSP Data Sets with a Diagnosis of TBIa
| |
|
Hospital discharge status |
||
|---|---|---|---|---|
| Injury etiology | n | Expired (%) | Alive (%) | Missing (%) |
| Falls |
77,533 |
11.7 |
85.0 |
3.3 |
| Natural/environmentalb/mechanicalc |
2038 |
18.4 |
76.3 |
5.3 |
| Cut/pierce |
29 |
0.0 |
93.3 |
6.7 |
| Sports |
54 |
18.2 |
81.8 |
0.0 |
| Struck by/againstd |
1130 |
11.0 |
85.4 |
3.6 |
| Suicide attempt |
787 |
80.6 |
17.2 |
2.3 |
| Motor vehicle crash |
27,552 |
13.1 |
81.7 |
5.2 |
| Violence or explosion | 1693 | 8.4 | 88.1 | 3.4 |
(n=110,816).
For example, accident resulting from cataclysmic earth movements and eruptions.
For example, accident caused by machinery.
For example, struck by falling object.
NTBD-NSP, National Trauma Data Bank National Sample Program; TBI, traumatic brain injury.
Table 4.
Level I and II Trauma Centers: GCS Score Category by Injury Etiology of Patients 65 Years of Age and Older Included in the 2007, 2008, 2009, and 2010 NTDB-NSP Data Sets with a Diagnosis of TBIa
| |
|
GCS score on admission |
|||
|---|---|---|---|---|---|
| Injury etiology | n | Mild (%) | Moderate (%) | Severe (%) | Missing (%) |
| Falls |
77,533 |
76.5 |
5.1 |
7.5 |
11.0 |
| Natural/environmentalb/mechanicalc |
2038 |
73.4 |
5.4 |
17.9 |
3.3 |
| Cut/pierce |
29 |
69.0 |
0.0 |
0.0 |
31.0 |
| Sports |
54 |
70.4 |
7.4 |
13.0 |
9.3 |
| Struck by/againstd |
1130 |
72.0 |
2.4 |
10.3 |
15.3 |
| Suicide attempt |
787 |
11.3 |
4.3 |
82.4 |
2.0 |
| Motor vehicle crash |
27,552 |
84.0 |
3.3 |
10.3 |
2.5 |
| Violence or explosion | 1693 | 82.2 | 4.8 | 10.3 | 2.7 |
(n=110,816).
For example, accident resulting from cataclysmic earth movements and eruptions.
For example, accident caused by machinery.
For example, struck by falling object.
GCS, Glasgow Coma Scale; NTDB-NSP, National Trauma Data Bank National Sample Program; TBI, traumatic brain injury.
In older adults, progressive backward stepwise logistic regressions predicting discharge status (expired or alive) were able to predict 47% of the variance in this outcome. Demographic and injury etiology categorical blocks provided little explanatory power, with the progressive model that contained both of these categories having a Nagelkerke value of 0.04. Injury severity, however, was shown to greatly improve this model. Within the final model, a critical AIS of the head score and a severe GCS score was shown to greatly increase the odds of death, with odds ratios (ORs) and 95% confidence intervals (CIs) ranging from 9.9 (95% CI, 9.2–10.6) to 120.4 (95% CI, 73.2–198.1). Hypotension (SBP between 50 and 89 mmHg) was also associated with increased risk for death (OR, 2.9; 95% CI, 2.4–3.3). Older age was also a significant predictor of death, with those 85 and older most likely to expire (OR, 3.1; 95% CI, 2.8–3.3). Female patients and patients who had a progressively longer LOS had a decrease in the odds of death (OR, 0.66; 95% CI, 0.63–0.70; and OR, 0.28; 95% CI, 0.26–0.30, respectively). Early in-hospital death did not explain the apparent protective effect of longer LOS, but post-hoc investigation of discharge locations indicated that the majority (71%) of cases with extreme (>90 days) LOS went on to receive extended medical care: 34.7% went to rehabilitation, 21.5% went to SNFs, and 11.8% went to hospice. Thus, it may be that although longer length of stay predicts survival to hospital discharge, for many cases it is associated with great medical need and likely postdischarge death (particularly among cases discharged to hospice). Interactions investigating the relationships between age, severity, and LOS were not retained, because no interactive terms were found to improve the overall model prediction and estimates for these variables were found to be largely unstable. Full results of the progressive regressions predicting discharge status are presented in Table 5.
Table 5.
Level I and II Trauma Centers: Progressive Backward Stepwise Logistic Regressions Predicting In-Hospital Deaths for Adults Age 65 and Older with a Diagnosis of TBI
| |
Predicting death (N = 79,105) 0.600.03 |
Predicting death (N = 79,105) 0.610.04 |
Predicting death (N = 79,105)0.87 0.47 |
|||
|---|---|---|---|---|---|---|
| Model informationC-statisticNagelkerkeCharacteristic | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) |
| Age group: 65–74 |
Reference |
|
Reference |
|
Reference |
|
| Age group: 75–84 |
1.53 |
(1.46 1.61) |
1.65 |
(1.56 1.73) |
2.16 |
(2.02 2.32) |
| Age group: 85 and older |
1.83 |
(1.73 1.93) |
2.02 |
(1.91 2.14) |
3.06 |
(2.84 3.30) |
| Gender: male |
Reference |
|
Reference |
|
Reference |
|
| Gender: female |
0.57 |
(0.55 0.59) |
0.60 |
(0.57 0.63) |
0.66 |
(0.63 0.70) |
| Race: white |
Reference |
|
Reference |
|
Reference |
|
| Race: black |
0.90 |
(0.82 0.98) |
0.82 |
(0.75 0.89) |
0.90 |
(0.81 1.01) |
| Race: Hispanic |
0.75 |
(0.69 0.82) |
0.72 |
(0.66 0.79) |
0.65 |
(0.58 0.73) |
| Race: Asian |
1.08 |
(0.96 1.21) |
1.06 |
(0.94 1.19) |
0.97 |
(0.84 1.12) |
| Race: Native Alaskan, Hawaiian, American |
0.51 |
(0.35 0.75) |
0.49 |
(0.33 0.71) |
0.70 |
(0.46 1.07) |
| Race: Other |
0.94 |
(0.81 1.08) |
0.95 |
(0.83 1.10) |
1.28 |
(1.07 1.52) |
| Injury etiology: fall |
|
|
Reference |
|
Reference |
|
| Injury etiology :natural/environmental/mechanical |
|
2.01 |
(1.76 2.29) |
1.35 |
(1.12 1.64) |
|
| Injury etiology: cut/pierce |
|
|
*** |
****** |
*** |
****** |
| Injury etiology: sports |
|
|
0.97 |
(0.38 2.47) |
0.16 |
(0.03 0.79) |
| Injury etiology: struck by/against |
|
|
1.11 |
(0.90 1.37) |
1.29 |
(0.99 1.68) |
| Injury etiology: suicide |
|
|
*** |
****** |
*** |
****** |
| Injury etiology: violence or explosion |
|
|
3.43 |
(3.09 3.81) |
0.90 |
(0.76 1.08) |
| Injury etiology: motor vehicle incidents |
|
|
1.19 |
(1.13 1.25) |
1.31 |
(1.23 1.40) |
| GCS admission total: mild |
|
|
|
|
Reference |
|
| GCS admission total: moderate |
|
|
|
|
3.85 |
(3.54 4.19) |
| GCS admission total: severe |
|
|
|
|
9.86 |
(9.19 10.58) |
| AIS Head: minor |
|
|
|
|
Reference |
|
| AIS Head: moderate |
|
|
|
|
2.70 |
(1.64 4.45) |
| AIS Head: serious |
|
|
|
|
6.17 |
(3.76 10.14) |
| AIS Head: severe |
|
|
|
|
11.85 |
(7.24 19.38) |
| AIS Head: critical |
|
|
|
|
120.38 |
(73.17 198.05) |
| AIS Head: unsurvivable |
|
|
|
|
53.52 |
(14.88 192.47) |
| LOS group: 1 day |
|
|
|
|
Reference |
|
| LOS group: 2 days to 1 week |
|
|
|
|
0.28 |
(0.26 0.30) |
| LOS group: up to 2 weeks |
|
|
|
|
0.32 |
(0.28 0.36) |
| LOS group: up to 3 weeks |
|
|
|
|
0.22 |
(0.19 0.25) |
| LOS group: up to 1 month |
|
|
|
|
0.20 |
(0.17 0.23) |
| LOS group: up to 1 year |
|
|
|
|
0.22 |
(0.16 0.30) |
| SBP: 90 thru 119 |
|
|
|
|
Reference |
|
| SBP: 50 thru 89 |
|
|
|
|
2.85 |
(2.43 3.34) |
| SBP: 90 thru 119 |
|
|
|
|
0.84 |
(0.76 0.92) |
| SBP: 140 thru 159 |
|
|
|
|
0.74 |
(0.68 0.81) |
| SBP: 160 thru 179 |
|
|
|
|
0.73 |
(0.66 0.80) |
| SBP: 180 thru 279 | 0.84 | (0.77 0.92) | ||||
Unreliable estimate as a result of small cell sizes.
TBI, traumatic brain injury; OR, odds ratio; CI, confidence interval; GCS, Glasgow Coma Scale; AIS, Abbreviated Injury Scale; LOS, length of hospital stay; SBP, systolic blood pressure.
The progressive backward stepwise logistic regressions predicting older adult discharge location (continued medical care or discharge to home) were less successful than those predicting death, accounting for only 25% of variance in this outcome. Again, demographic and injury etiology information were found to have little predictive power (Nagelkerke value of 0.06). The final model, which included injury severity indices (presented in Table 6) had the highest predictive power. LOS was shown to have the highest ORs, with LOS between 3 weeks to 1 month most strongly predicting discharge to continued care (OR, 112.8; 95% CI, 86.9–146.4). More severe GCS and AIS of the head scores, older age, and female gender were also predictive of continued care. Nonwhite race was the only variable found to be consistently predictive of a discharge to home. As with the previous models, interactive terms were not retained because these variables did not improve overall model prediction and estimates were largely unstable.
Table 6.
Level I and II Trauma Centers: Progressive Backward Stepwise Logistic Regressions Predicting Continued Medical Carea of Those Who Survive to Discharge for Adults Age 65 and Older with a Primary Diagnosis of TBI
| |
Predicting continued care(N = 67,929)0.620.06 |
Predicting continued care(N = 67,929)0.620.06 |
Predicting continued care(N = 67,929)0.750.25 |
|||
|---|---|---|---|---|---|---|
| Model informationC-statisticNagelkerkeCharacteristic | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) |
| Age group: 65–74 |
Reference |
|
Reference |
|
Reference |
|
| Age group: 75–84 |
1.73 |
(1.67 1.80) |
1.69 |
(1.63 1.75) |
1.78 |
(1.71 1.85) |
| Age group: 85 and older |
2.80 |
(2.69 2.92) |
2.70 |
(2.59 2.81) |
3.16 |
(3.01 3.31) |
| Gender: male |
Reference |
|
Reference |
|
Reference |
|
| Gender: female |
1.03 |
(1.00 1.07) |
### |
### ### |
1.15 |
(1.11 1.19) |
| Race: white |
Reference |
|
Reference |
|
Reference |
|
| Race: black |
0.78 |
(0.73 0.83) |
0.79 |
(0.74 0.84) |
0.74 |
(0.69 0.80) |
| Race: Hispanic |
1.06 |
(0.99 1.12) |
1.06 |
(1.00 1.13) |
0.95 |
(0.88 1.01) |
| Race: Asian |
0.76 |
(0.70 0.84) |
0.77 |
(0.71 0.85) |
0.71 |
(0.64 0.78) |
| Race: Native Alaskan, Hawaiian, American |
0.51 |
(0.41 0.63) |
0.52 |
(0.42 0.65) |
0.49 |
(0.39 0.62) |
| Race: Other |
0.76 |
(0.68 0.84) |
0.75 |
(0.68 0.84) |
0.64 |
(0.57 0.72) |
| Injury etiology: fall |
|
|
Reference |
|
Reference |
|
| Injury etiology: natural/environmental/mechanical |
|
1.03 |
(0.92 1.17) |
0.73 |
(0.63 0.84) |
|
| Injury etiology: cut/pierce |
|
|
*** |
****** |
*** |
****** |
| Injury etiology: sports |
|
|
8.72 |
(2.81 27.03) |
8.52 |
(2.74 26.43) |
| Injury etiology: struck by/against |
|
|
0.50 |
(0.42 0.59) |
0.40 |
(0.33 0.48) |
| Injury etiology: suicide |
|
|
*** |
****** |
*** |
****** |
| Injury etiology: violence or explosion |
|
|
0.77 |
(0.68 0.86) |
0.64 |
(0.56 0.74) |
| Injury etiology: motor vehicle incidents |
|
|
0.86 |
(0.83 0.89) |
0.78 |
(0.75 0.82) |
| GCS admission total: mild |
|
|
|
|
Reference |
|
| GCS admission total: moderate |
|
|
|
|
2.04 |
(1.85 2.25) |
| GCS admission total: severe |
|
|
|
|
2.21 |
(1.98 2.48) |
| AIS Head: minor |
|
|
|
|
Reference |
|
| AIS Head: moderate |
|
|
|
|
1.08 |
(0.96 1.21) |
| AIS Head: serious |
|
|
|
|
1.36 |
(1.21 1.52) |
| AIS Head: severe |
|
|
|
|
1.77 |
(1.58 1.98) |
| AIS Head: critical |
|
|
|
|
4.43 |
(3.56 5.51) |
| AIS Head: unsurvivable |
|
|
|
|
1.30 |
(0.25 6.68) |
| LOS group: 1 day |
|
|
|
|
Reference |
|
| LOS group: 2 days to 1 week |
|
|
|
|
5.30 |
(4.91 5.73) |
| LOS group: up to 2 weeks |
|
|
|
|
39.43 |
(34.65 44.88) |
| LOS group: up to 3 weeks |
|
|
|
|
49.96 |
(42.29 59.02) |
| LOS group: up to 1 month |
|
|
|
|
112.85 |
(86.94 146.49) |
| LOS group: up to 1 year |
|
|
|
|
32.96 |
(22.65 47.96) |
| SBP: 90 thru 119 |
|
|
|
|
Reference |
|
| SBP: 50 thru 89 |
|
|
|
|
0.83 |
(0.71 0.99) |
| SBP: 90 thru 119 |
|
|
|
|
0.79 |
(0.74 0.84) |
| SBP: 140 thru 159 |
|
|
|
|
0.84 |
(0.79 0.89) |
| SBP: 160 thru 179 |
|
|
|
|
0.80 |
(0.75 0.85) |
| SBP: 180 thru 279 | 0.78 | (0.73 0.83) | ||||
Unreliable estimate resulting from small cell sizes.
###Variable not retained in by backward stepwise procedure.
Continued medical care includes the following discharge locations: intermediate care facility (ICF) or hospice care; acute hospital or some other type of hospital (e.g., short-term general hospital); skilled nursing facility (SNF); leaving against medical advice (AMA); and inpatient rehabilitation.
TBI, traumatic brain injury; OR, odds ratio; CI, confidence interval; GCS, Glasgow Coma Scale; AIS, Abbreviated Injury Scale; LOS, length of hospital stay; SBP, systolic blood pressure.
Supplemental progressive backward stepwise logistic regressions were conducted to evaluate whether in-hospital complications and procedures account for additional variance in discharge disposition and discharge location. Results of these analyses (not presented here) indicated that neither in-hospital complications nor procedures account for additional variance in discharge disposition or discharge location over previous models. Models that included only facilities with 80% procedure code entry resulted in Nagelkerke values of 0.55 and 0.26 for prediction of in-hospital death and home discharge, respectively, whereas those that included only facilities with 80% complication entry resulted in Nagelkerke values of 0.59 and 0.29. It should be noted that limiting the sample to facilities with 80% or higher rates of completion on these variables resulted in a substantially reduced sample size.
Discussion
Main findings
The aims of this study were to provide an updated overview of TBI in older adults using data from the NTDB, evaluate changes in the rates of TBI among older adults over a 4-year period, and verify important predictors of outcomes (e.g., death and hospital discharge status). The most striking finding in this study was the substantial increase in TBI-related trauma admissions between 2007 and 2010 among the oldest age groups: those >=75 (20% increase in admissions relative to the general population) and those >=85 (25% increase). These results indicate that the rate of TBI-related hospital visits among the oldest segment of the U.S. population has actually exceeded population growth in recent years. It is important to note that these numbers on older adults do not include the vast majority of 76 million Baby Boomers (born between 1946 and 1964), who have not yet reached the ages of greatest injury risk. Baby Boomers have more chronic medical conditions and report more limitations in physical mobility than previous generations,33 suggesting they may be at even greater risk for injury as they age. The implications of TBI rates continuing to exceed population growth are far reaching because Baby Boomers may enter older adulthood with greater rates of disability, morbidity, and associated medical and social service needs.
The findings from this study provide support for the notion that TBI in older adults differs in multiple ways from these injuries experienced by other adult age groups and may be associated with additional recovery challenges, when compared to younger adults. The majority of TBIs among older adults occur as a result of falls and are mild in severity. Yet, compared to younger adults, older people tend to have more severe TBIs (as measured by AIS), longer lengths of hospital stay, are more likely to be discharged to subacute nursing facilities, and are more likely to die in the hospital. In other words, these data are consistent with previous research in indicating that older adults tend to sustain lower-impact injuries (e.g., falls, as opposed to motor vehicle crashes, which cause the majority of TBIs in younger adults), and yet they suffer more consequential brain injuries and poorer outcomes than younger adults.8,9 Older adults appear to sustain fewer extracranial injuries than younger adults with TBI, as indicated by far lower numbers of nonhead CT scans and fewer fractures treated in the older age groups. These findings are consistent with a previous study,8 particularly those that have reported high rates of mortality after low-impact injuries, such as ground-level falls among adults>=65.34,35 However, results of the current study indicate that falls do not result in the most consequential injuries among older adults. Instead, injuries resulting from suicide attempt, natural, environmental, or mechanical events, and sports are more fatal and are more likely to result in severe TBI, although the base rates of these injuries were quite low in the NTDB.
There were some discrepancies in age-related trends in injury severity, as measured by the GCS and AIS. As age increased, a greater proportion of injuries fell in the more severe ranges of AIS scores, but a smaller proportion of injuries fell in the severe range of GCS scores. This divergence may reflect age-related differences in the progression of TBI symptoms among older adults, who are at greater risk for postinjury complications such as intracranial hemorrhage, hematoma, and other complications related to age-related frailty, pre-existing medical conditions, and polypharmacy.14,36 Older adults may sustain injuries that initially appear mild and then become more significant over the subsequent hours and days.14 In the NTDB, GCS scores are taken at the ED and may be affected by alcohol intoxication and other extracranial etiologies that effect sensorium (i.e., sepsis, cardiogenic shock, and so on). AIS scores are calculated using ICD-9-CM codes entered throughout the hospital stay, so it may be the case that AIS scores more accurately reflect injury severity in cases where postinjury complications result in worsening. Moreover, given the higher rates of CT scans in older adults, it is possible that abnormal scan findings (which may or may not be clinically significant) may influence AIS scores, which reflect the presence of intracranial pathology.
Data on in-hospital complications in the NTDB are not routinely reported by all facilities, but older adults experience slightly higher incidence of serious complications, such as cardiac arrest and acute renal failure, compared to younger adults. Older adults also undergo higher incidence of certain in-hospital procedures, such as transfusions, venous catheterization, and chest X-rays, which further reflect the complexity of treating TBI in this older age group. It is likely that pre-existing disease burden and the polypharmacy required to manage multiple chronic conditions would place older adults with TBI at a higher risk for in-hospital complications and necessitate a greater number of procedures. Previous literature clearly indicates that the overall burden of multiple chronic medical conditions increases with age: Approximately two thirds of Medicare beneficiaries 65 years of age or older are diagnosed with at least two chronic conditions, and approximately one quarter have been diagnosed with four or more chronic conditions.37 Unfortunately, pre-existing conditions are rarely reported in the NTDB, and so it was not possible to evaluate the direct effect of comorbid medical conditions on outcomes after TBI in the current study.
Given the number of studies that have demonstrated poorer post-TBI outcomes among older adults, it is reasonable to question whether potentially serious injuries are unrecognized by emergency medical responders38 and whether older adults receive appropriately aggressive care upon arrival to the hospital.39,40 Several studies have suggested that adults over the age of 65 years have higher undertriage rates41,42 and are less likely to have trauma team involvement43 than their younger counterparts, suggesting that they are less likely to be transported to a hospital that is equipped to provide trauma care, such as a level I or II trauma center.39,44
An important and indirect finding in this study is that a much smaller proportion of older adults are treated in a level I or II trauma center for TBI than would be expected based on hospital admissions for older adults with TBI. To evaluate this, we calculated the cumulative number of cases with TBI noted in the nationally weighted NTDB data sets (2007 thru 2010) who were 75 years of age and older that met our inclusion characteristics and divided this value by the cumulative number of adults 75 and older living in the United States between 2007 and 2010 according to U.S. Census data. The current study found rates to be much lower for the group 75 and older (104 per 100,000), compared to the published rate data on trauma center and nontrauma center admissions (339 per 100,000).1 Thus, only approximately one third of older adults who sustain a TBI are observed in a trauma center. As noted, the rate trend is increasing, but it is unclear whether the increase is the result of an aging population that is being treated more often, in general, or more often in a level I or II trauma center, or if there are improvements in adherence to the special considerations section on older adults in the field triage guidelines.16
Some previous studies have suggested that older adults are given more conservative acute care after traumatic injuries, compared to their younger counterparts. One study using data from the National Study on the Costs and Outcomes of Trauma database found that as age increased, older adults were less likely to receive ICP monitoring, specialty care, and intensive care unit admission.40 In contrast to this study, which includes nondesignated trauma centers, data from the current study indicated that among adults who are treated at level I or II trauma centers (i.e., those included in the NTDB), older adults underwent a greater number of TBI-related procedures, compared to younger adults, such as head CT, MRI of the brain, and neurosurgical interventions. These findings may reflect the effect of large-scale efforts to improve acute care for geriatric patients (e.g., as previously reported16,46). The National Expert Panel on Field Triage released updated guidelines in 2011 that recognize the increased risk for injury and death among individuals over the age of 55 years and specifically identify low SBP and ground-level falls as factors that may indicate severe injury among older adults.45 In 2009, the American College of Emergency Physicians updated its 2002 clinical policy on the management of mild TBI46 to recommend head CT for adults over the age of 60 presenting with TBI with loss of consciousness or post-traumatic amnesia as well as for adults over the age of 65 presenting with TBI regardless their altered consciousness. Given the amount of missing data on in-hospital complications and procedures from many NTDB hospitals, however, the findings based on these data should be interpreted with caution. It is not clear whether these data are representative of all U.S. trauma centers, because many older adults with TBI may be taken to a level III or IV trauma center or nontrauma centers.39,44
Consistent with prior studies,47–50 results presented here indicate that injury severity, older age, and hypotension at admission are strong predictors of in-hospital death among older adults with TBI. It should be noted that the ORs by age increase when injury severity is added to the model predicting death, which suggests that, even after milder injuries, older people may still be at increased risk for death, compared to younger people. Age and injury severity are independent predictors of mortality, and it is clear that injury severity alone does not explain the poor outcomes observed among older adults with TBI. A recent study that evaluated effect measure modification of the relationship between TBI severity and mortality by age found that GCS is a better predictor of mortality among younger people and is more weakly associated with mortality among older people.48 Further research is necessary to identify precise factors that moderate the relationship between injury severity and mortality among older adults.
Models predicting discharge location were not as successful as those predicting disposition; this likely reflects the complexity of factors at play in discharge decision making. The strongest predictor of discharge to continued medical care versus home among older adults in the current study was length of hospital stay. It is probable that factors such as the extent of injury-related impairment, number of in-hospital complications and procedures, and even pre-existing conditions may all influence LOS and discharge location, making these constructs strong indices of the gravity of injury-related consequences. As expected, older age and greater injury severity were also identified as significant predictors of discharge to continued medical care. It is prudent to consider the possibility that length of hospital stay and discharge location reflect sociocultural and socioeconomic factors in addition to injury severity-related factors. In the current study, for example, female gender was associated with reduced odds of death, but was associated with greater likelihood of being discharged to a continued medical care facility. It is possible that females, who tend to outlive their male counterparts, may not have the social support (e.g., a spouse capable of assisting) or financial resources that would be necessary for a discharge to home. Consistent with a previous study,51 nonwhite race was associated with greater likelihood of being discharged home, further underscoring the potential effect of sociocultural and other factors in determining discharge location.
Limitations
This study has several limitations. The NTDB includes data from hospitals that are designated by the American College of Surgeons as trauma centers, and we excluded from these analyses any cases that were transferred in, so findings presented here may not reflect the care provided to older adults with TBI who are treated in other facilities, such as urgent care centers and community hospitals. There is some evidence that older adults are less likely to be treated at a designated trauma center than younger adults,39,44 so the generalizability of these findings to all older adults with a diagnosis of TBI is not clear. Several variables that may be essential in predicting TBI outcomes among older adults were unavailable (e.g., pre-existing medical conditions) or were not commonly recorded across NTDB hospitals (e.g., in-hospital procedures and complications). As described in the Methods section, analyses were limited by missing data. Some variables were unavailable for analysis because of low rates of completion, and rates of missing data for some variables varied systematically by age, undermining confidence in the proportion of subjects rated in other categories. Finally, The finding that the rate of TBI-related admissions at level I or II trauma centers increased between 2007 and 2010 among older adults may have been an artifact of the years chosen for analysis, because the most marked increase occurred between 2007 and 2008 and this may not represent the true change observed over a longer period of time. Replication of this finding is warranted as more data become available.
Conclusions
Data from the current study indicate that the rate of older adult TBI-related trauma visits is increasing at a rate faster than the population itself is expanding. Older adults primarily incurred injuries in falls and motor vehicle incidents, with increasing rates of moderate to severe TBI as age increased, based on head AIS scores. Older adults not only present with different injury characteristics than their younger counterparts, but also have different discharge dispositions than younger cohorts—importantly, they require more ongoing care. The potential public health burden of TBI among older adults over the next two decades as the Baby Boom generation ages to older adulthood will be significant. Initiatives to improve primary and secondary prevention of TBI in this cohort are clearly warranted.
Our research suggests that factors that were not systematically measured in the NTDB may be important in predicting favorable discharge (i.e., home with or without assistance). This is consistent with previous studies that demonstrate the limited prognostic significance of injury severity indices among older adults, relative to younger adults,47 and indicates that confounding features, such as pre-existing medical conditions, overall frailty, and hospital course, play a critical role in predicting injury outcomes in older adults. It may be difficult to systematically collect data on these variables given the time and cost required, but this information is necessary to identify age-appropriate care guidelines and maximize injury outcomes for older adults.
Acknowledgment
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Faul M., Xu L., Wald M.M., and Coronado V.G. (2010). Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA [Google Scholar]
- 2.Langlois J.A., Rutland-Brown W., Thomas K.E., and Xi Y.L. (2006). Incidence of traumatic brain injury in the United States, 2003. J. Head Trauma Rehabil. 21, 544–548 [DOI] [PubMed] [Google Scholar]
- 3.Colantonio A., Saverino C., Zagorski B., Swaine B., Lewko J., Jaglal S. and Vernich L. (2010). Hospitalizations and emergency department visits for TBI in Ontario. Can J Neurol Sci 37, 783–790 [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Quality and Research (2013). H-CUPnet, healthcare cost and utilization project. Available at: www.ahrq.gov/HCUPnet/ (last accessed March28, 2013)
- 5.Ponsford J., Cameron P., Fitzgerald M., Grant M., and Mikocka-Walus A. (2011). Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J. Neurotrauma 28, 937–946 [DOI] [PubMed] [Google Scholar]
- 6.Marquez de la Plata C.D., Hart T., Hammond F.M., Frol A.B., Hudak A., Harper C.R., O'Neil-Pirozzi T.M., Whyte J., Carlile M., and Diaz-Arrastia R. (2008). Impact of age on long-term recovery from traumatic brain injury. Arch. Phys. Med. Rehabil. 89, 896–903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mosenthal A.C., Livingston D.H., Lavery R.F., Knudson M.M., Lee S., Morabito D., Manley G.T., Nathens A., Jurkovich G., Hoyt D.B., and Coimbra R. (2004). The effect of age on functional outcome in mild traumatic brain injury: 6-month report of a prospective multicenter trial. J. Trauma 56, 1042–1048 [DOI] [PubMed] [Google Scholar]
- 8.Susman M., DiRusso S.M., Sullivan T., Risucci D., Nealon P., Cuff S., Haider A., and Benzil D. (2002). Traumatic brain injury in the elderly: increased mortality and worse functional outcome at discharge despite lower injury severity. J. Trauma 53, 219–223; discussion, 223–214. [DOI] [PubMed] [Google Scholar]
- 9.Livingston D.H., Lavery R.F., Mosenthal A.C., Knudson M.M., Lee S., Morabito D., Manley G.T., Nathens A., Jurkovich G., Hoyt D.B., and Coimbra R. (2005). Recovery at one year following isolated traumatic brain injury: a Western Trauma Association prospective multicenter trial. J. Trauma 59, 1298–1304; discussion, 1304. [DOI] [PubMed] [Google Scholar]
- 10.Dams-O'Connor K., Gibbons L.E., Bowen J.D., McCurry S.M., Larson E.B., and Crane P.K. (2013). Risk for late-life re-injury, dementia and death among individuals with traumatic brain injury: a population-based study. J. Neurol. Neurosurg. Psychiatry 84, 177–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cefalu C.A. (2011). Theories and mechanisms of aging. Clin. Geriatr. Med. 27, 491–506 [DOI] [PubMed] [Google Scholar]
- 12.Dijkers M., Cantor J., Hibbard M., Belkonen S., Warshowsky A., and Layman D. (2008). The consequences of TBI in the elderly: a systematic review. Brain Inj. Professional 5, 14–18 [Google Scholar]
- 13.Fjell A.M., and Walhovd K.B. (2010). Structural brain changes in aging: courses, causes and cognitive consequences. Rev. Neurosci. 21, 187–221 [DOI] [PubMed] [Google Scholar]
- 14.Brewer E.S., Reznikov B., Liberman R.F., Baker R.A., Rosenblatt M.S., David C.A., and Flacke S. (2011). Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. J. Trauma Acute Care Surg. 70, e1–e5 [DOI] [PubMed] [Google Scholar]
- 15.Ott M.M., Eriksson E., Vanderkolk W., Christianson D., Davis A., and Scholten D. (2010). Antiplatelet and anticoagulation therapies do not increase mortality in the absence of traumatic brain injury. J. Trauma 68, 560–563 [DOI] [PubMed] [Google Scholar]
- 16.Sasser S.M., Hunt R.C., Faul M., Sugerman D., Pearson W.S., Dulski T., Wald M.M., Jurkovich G.J., Newgard C.D., and Lerner E.B. (2012). Guidelines for field triage of injured patients: recommendations of the national expert panel on field triage, 2011. MMWR Recomm. Rep. 61, 1–20 [PubMed] [Google Scholar]
- 17.AANS (2007). Brain Trauma Foundation, guidelines for the management of severe traumatic brain injury. J. Neurotrauma 24, Suppl. 1, S1–106 [DOI] [PubMed] [Google Scholar]
- 18.Evans L. (1988). Risk of fatality from physical trauma versus sex and age. J. Trauma 28, 368–378 [DOI] [PubMed] [Google Scholar]
- 19.Thomas K.E., Stevens J.A., Sarmiento K., and Wald M.M. (2008). Fall-related traumatic brain injury deaths and hospitalizations among older adults—United States, 2005. J. Safety Res. 39, 269–272 [DOI] [PubMed] [Google Scholar]
- 20.Grossman M.D., Miller D., Scaff D.W., and Arcona S. (2002). When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J. Trauma 52, 242–246 [DOI] [PubMed] [Google Scholar]
- 21.George R.L., McGwin G., Jr., Metzger J., Chaudry I.H., and Rue L.W., 3rd (2003). The association between gender and mortality among trauma patients as modified by age. J. Trauma 54, 464–471 [DOI] [PubMed] [Google Scholar]
- 22.Neal M. (2005). National Trauma Data Bank. NTDB National Sample Program. American College of Surgeons: Chicago, IL [Google Scholar]
- 23.Goble S., Neal M., Clark D.E., Nathens A.B., Annest J.L., Faul M., Sattin R.W., Li L., Levy P.S., Mann N.C., Guice K., Cassidy L.D., and Fildes J.J. (2009). Creating a nationally representative sample of patients from trauma centers. J. Trauma 67, 637–642; discussion, 642–634. [DOI] [PubMed] [Google Scholar]
- 24.Marr A.L., Coronado, Victor G. (2002). Central nervous system injury surveillance data submission standards—2002. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention: Atlanta, GA [Google Scholar]
- 25.Harrison-Felix C., Kolakowsky-Hayner S.A., Hammond F.M., Wang R., Englander J., Dams-O'Connor K., Kreider S.E., Novack T.A., and Diaz-Arrastia R. (2012). Mortality after surviving traumatic brain injury: risks based on age groups. J. Head Trauma Rehabil. 27, E45–E56 [DOI] [PubMed] [Google Scholar]
- 26.Teasdale G., and Jennett B. (1974). Assessment of coma and impaired consciousness. A practical scale. Lancet 2, 81–84 [DOI] [PubMed] [Google Scholar]
- 27.Baker S.P., O'Neill B., Haddon W., Jr., and Long W.B. (1974). The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 14, 187–196 [PubMed] [Google Scholar]
- 28.Tri-Analytics (1997). ICDMAP-90 Injury severity coding software. John Hopkins University and Tri-Analytics Inc.: Baltimore, MD [Google Scholar]
- 29.AHA (2011). Understanding blood pressure readings. American Heart Association: Dallas, TX [Google Scholar]
- 30.Reistetter T.A., Graham J.E., Deutsch A., Granger C.V., Markello S., and Ottenbacher K.J. (2010). Utility of functional status for classifying community versus institutional discharges after inpatient rehabilitation for stroke. Arch. Phys. Med. Rehabil. 91, 345–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.CDC (2010). U.S. Census bridged race population estimates: data files and documentation. Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD [Google Scholar]
- 32.IBM (Released 2010). IBM SPSS statistics for windows, version 19.0. IBM Corp.: Armonk, NY [Google Scholar]
- 33.Farrer S.R. (2007). Growing older in america, the health and retirement study. National Institute on Aging, National Institutes of Health: Bethesda, MD [Google Scholar]
- 34.Spaniolas K., Cheng J.D., Gestring M.L., Sangosanya A., Stassen N.A., and Bankey P.E. (2010). Ground level falls are associated with significant mortality in elderly patients. J. Trauma 69, 821–825 [DOI] [PubMed] [Google Scholar]
- 35.Chisholm K.M., and Harruff R.C. (2010). Elderly deaths due to ground-level falls. Am. J. Forensic Med. Pathol. 31, 350–354 [DOI] [PubMed] [Google Scholar]
- 36.Pearson W.S., Sugerman D.E., McGuire L.C., and Coronado V.G. (2012). Emergency department visits for traumatic brain injury in older adults in the United States: 2006–08. West J. Emerg. Med. 13, 289–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolff J.L., Starfield B., and Anderson G. (2002). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 162, 2269–2276 [DOI] [PubMed] [Google Scholar]
- 38.Phillips S., Rond P.C., 3rd, Kelly S.M., and Swartz P.D. (1996). The failure of triage criteria to identify geriatric patients with trauma: results from the Florida Trauma Triage Study. J. Trauma 40, 278–283 [DOI] [PubMed] [Google Scholar]
- 39.Lane P., Sorondo B., and Kelly J.J. (2003). Geriatric trauma patients-are they receiving trauma center care? Acad. Emerg. Med. 10, 244–250 [DOI] [PubMed] [Google Scholar]
- 40.Thompson H.J., Rivara F.P., Jurkovich G.J., Wang J., Nathens A.B., and MacKenzie E.J. (2008). Evaluation of the effect of intensity of care on mortality after traumatic brain injury. Crit. Care Med. 36, 282–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang D.C., Bass R.R., Cornwell E.E., and Mackenzie E.J. (2008). Undertriage of elderly trauma patients to state-designated trauma centers. Arch. Surg. 143, 776–781; discussion, 782. [DOI] [PubMed] [Google Scholar]
- 42.Scheetz L.J. (2011). Trends in the accuracy of older person trauma triage from 2004 to 2008. Prehsp. Emerg. Care 15, 83–87 [DOI] [PubMed] [Google Scholar]
- 43.Lehmann R., Beekley A., Casey L., Salim A., and Martin M. (2009). The impact of advanced age on trauma triage decisions and outcomes: a statewide analysis. Am. J. Surg. 197, 571–574; discussion, 574–575. [DOI] [PubMed] [Google Scholar]
- 44.Ryb G.E., and Dischinger P.C. (2011). Disparities in trauma center access of older injured motor vehicular crash occupants. J. Trauma 71, 742–747 [DOI] [PubMed] [Google Scholar]
- 45.Sasser S. M., Hunt R. C., Sullivent E. E., Wald M. M., Mitchko J., Jurovich G. J., and Sattin R. W. (2009). Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention: Washington, DC [Google Scholar]
- 46.Jagoda A.S., Bazarian J.J., Bruns J.J., Cantrill S.V., Gean A.D., Howard P.K., Ghajar J., Riggio S., Wright D.W.>, Wears R.L., Bakshy A., Burgess P., Wald M.M., and Whitson R.R. (2009). Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. J. Emerg. Nursing 35, e5–e40 [DOI] [PubMed] [Google Scholar]
- 47.DuBose J.J., Browder T., Inaba K., Teixeira P.G., Chan L.S., and Demetriades D. (2008). Effect of trauma center designation on outcome in patients with severe traumatic brain injury. Arch. Surg. 143, 1213–1217; discussion, 1217. [DOI] [PubMed] [Google Scholar]
- 48.Linn S., Levi L., Grunau P.D., Zaidise I., and Zarka S. (2007). Effect measure modification and confounding of severe head injury mortality by age and multiple organ injury severity. Ann. Epidemiol. 17, 142–147 [DOI] [PubMed] [Google Scholar]
- 49.Utomo W.K., Gabbe B.J., Simpson P.M., and Cameron P.A. (2009). Predictors of in-hospital mortality and 6-month functional outcomes in older adults after moderate to severe traumatic brain injury. Injury 40, 973–977 [DOI] [PubMed] [Google Scholar]
- 50.Stocchetti N., Paterno R., Citerio G., Beretta L., and Colombo A. (2012). Traumatic brain injury in an aging population. J. Neurotrauma 29, 1119–1125 [DOI] [PubMed] [Google Scholar]
- 51.Cuthbert J.P., Corrigan J.D., Harrison-Felix C., Coronado V., Dijkers M.P., Heinemann A.W., and Whiteneck G.G. (2011). Factors that predict acute hospitalization discharge disposition for adults with moderate to severe traumatic brain injury. Arch. Phys. Med. Rehabil. 92, 721–730 [DOI] [PubMed] [Google Scholar]