Abstract
Purpose
Laparoscopic techniques have allowed surgeons to perform complicated intra-abdominal surgery with minimal trauma. Single incision laparoscopic surgery (SILS) was developed with the aim of reducing the invasiveness of conventional laparoscopy. In this study we aimed to compare results of SILS cholecystectomy and three port conventional laparoscopic (TPCL) cholecystectomy prospectively.
Methods
In this prospective study, 100 patients who underwent laparoscopic cholecystectomy for gallbladder disease were randomly allocated to SILS cholecystectomy (group 1) or TPCL cholecystectomy (group 2). Demographics, pathologic diagnosis, operating time, blood loss, length of hospital stay, complications, pain score, conversion rate, and satisfaction of cosmetic outcome were recorded.
Results
Forty-four SILS cholesystectomies (88%) and 42 TPCL cholecystectomies (84%) were completed successfully. Conversion to open surgery was required for 4 cases in group 1 and 6 cases in group 2. Operating time was significantly longer in group 1 compared with group 2 (73 minutes vs. 48 minutes; P < 0.05). Higher pain scores were observed in group 1 versus group 2 in postoperative day 1 (P < 0.05). There was higher cosmetic satisfaction in group 1 (P < 0.05).
Conclusion
SILS cholecystectomy performed by experienced surgeons is at least as successful, feasible, effective and safe as a TPCL cholecystectomy. Surgeons performing SILS should have a firm foundation of advanced minimal access surgical skills and a cautious, gradated approach to attempt the various procedures. Prospective randomized studies comparing single access versus conventional multiport laparoscopic cholecystectomy, with large volumes and long-term follow-up, are needed to confirm our initial experience. (ClinicalTrials.gov Identifier: NCT01772745.)
Keywords: Surgery, Laparoscopy, Cholecystectomy
INTRODUCTION
Single-incision laparoscopic procedures have evolved gradually to include a multitude of various surgical procedures. The current literature documents the use of a single-incision or single-port access surgery for cholecystectomy, adrenalectomy, splenectomy, appendectomy, herniorrhaphy, bariatric, and colon surgery [1,2]. Improved optics, roticulating instruments, and specially designed ports have facilitated single-incision surgery.
The advent of laparoscopy in the 1980s has made laparoscopic cholecystectomy one of the most common procedures in general surgery with improved overall recovery and shortened length of hospital stay compared with conventional open cholecystectomy [3]. The first video-laparoscopic cholecystectomy was performed by Phillipe Mouret in 1987 (quoted from [4]). Single incision laparoscopic surgery (SILS), also known as laparoendoscopic single-site surgery or single-port access surgery, is an area of active investigation for abdominal surgery. In 1987, Navarra et al. [5] performed the first single-port cholecystectomy. Since that time, the idea of "scarless" surgery has gained increasing popularity among patients as well as surgeons.
Patients' demand for better cosmetic outcomes and minimally invasive interventions plays a significant role in increasing the popularity of this technique. A better cosmetic result makes it possible for the patient to prefer this operation. The advantages of SILS cholecystectomy are not yet clearly defined. Decreased postoperative pain, faster return to normal activity, and improved cosmetic outcome are a few of the proposed advantages over conventional laparoscopy but have yet to be compared prospectively. Recent reports demonstrate large series of SILS cholecystectomies [6,7] but the number of prospective randomized study is insufficient. This study compares SILS cholecystectomy and three port conventional laparoscopic (TPCL) cholecystectomy prospectively.
METHODS
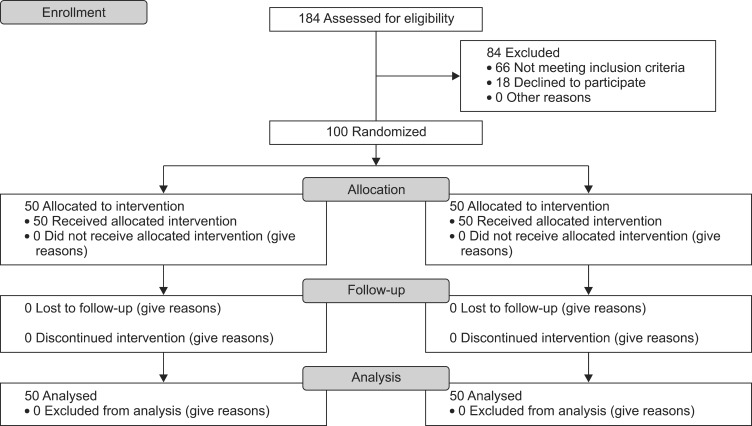
From January 2010 through January 2012, patients with gallbladder disease were evaluated. The study was approved by the local Ethical Committee at the Turkish Ministry of Health. All interventions were only performed by two surgeons (U.D. and U.B.). These two surgeons were specialized in laparoscopic surgery. Written informed consent was obtained from all the participants. One hundred patients (88 women and 12 men) aged from 21 to 68 years (mean, 41.5 ± 12.16 years) were randomly assigned to undergo SILS cholecystectomy (group 1, n=50) or TPCL cholecystectomy (group 2, n=50) according to a computer-generated table of random numbers. Exclusion criteria were 1) American Society of Anesthesiologists score (ASA) of more than III, 2) patients with prior abdominal surgery, 3) patients with choledocolithiasis and/or abnormal cholestasis enzymes values, 4) pregnancy, 5) ongoing peritoneal dialysis, and 6) the presence of pancreatitis. Primary outcome measures were pain score and intra-abdominal complications. Secondary outcome measures were operating time and cosmetic outcomes. The flow diagram displays the progress of all participants through the study (Fig. 1).
Fig. 1.
Flow diagram of the study.
Preoperative preparation, anesthesia, and preoperative antibiotics were performed similarly for all patients. Preoperative cefazolin 1 g. was administered intravenously half an hour before skin incision. Demographics, body mass index (BMI), ASA score, indication for operation, operative morbidity, operative time, pain score, length of hospital stay, need for conversion to three or four port laparoscopic cholecystectomy, need for conversion to open cholecystectomy and satisfaction of cosmetic outcome were recorded. A standard analgesia protocol was used with intravenous nonsteroid anti-inflammatory drug (tenoxicam 20 mg) twice a day. An opioid (tramadol 50 mg) was added when required. Postoperative pain was assessed according to a visual analogue scale (VAS) from 0 (no pain) to 10 (worst pain imaginable) on the postoperative sixth hour (POSH-VAS) and postoperative day 1 (POFD-VAS) [8]. Morbidity was evaluated by rates of bile leak, wound infection, hospital readmission, and hernia. Six months after surgery we recorded satisfaction of cosmetic outcome through face-to-face interviews with all patients. Cosmetic outcome was assessed on a scale from 1 (worst satisfaction) to 5 (best satisfaction) on postoperative month 6.
Operative technique
All procedures were performed under general anesthesia and orotracheal intubation. All patients were placed in reverse Trendelenburg position (30 degrees) with the table tilted downward to the patient's left in order to bring the operative field toward the surgeon and displace intra-abdominal organs away from the gallbladder. In both groups, during laparoscopy the gas used was CO2 and intra-abdominal pressure was maintained at 12-14 mmHg. In all patients a nasogastric tube was inserted at the beginning and removed after the intervention. The incision site was infiltrated with 10 mL of 0.25% Marcaine (AstraZeneca Global, London, UK) before skin closure.
SILS cholecystectomy
Two stay sutures are inserted either side of the intended incision line and a vertical incision is made between the two stay sutures in the umbilicus. A 1.5 cm vertical skin incision and 2 cm vertical fascial incision is made directly through the umbilicus. SILS port (Covidien Inc., Norwalk, CT, USA) placement phases are shown in Fig. 2. During operation, the surgeon and assistant both stand on the left side of the patient. For some cases, transabdominal 2/0 polypropylene suture retractors were used due to the challenging anatomy of Callot's triangle. Simultaneous palpation of the abdominal wall demonstrates the optimum site for insertion of the suture, which should be placed as high as possible while avoiding the pleura. Fundal retraction is critical in safely completing dissection in the triangle of Callot. The gallbladder is elevated over the liver edge to identify the cystic duct infundibular junction (Fig. 3). Articulated Endograsper and endodissector instruments are moved with inward and outward rather than side-to-side motions (Fig. 4). A cholecystectomy is then performed in the standard fashion. The gallbladder is extracted from the abdominal cavity with the use of an EndoCatch (Covidien Inc., Norwalk, CT, USA). The fascia is closed with no:0 polypropylene sutures. Dermis of umbilicus is closed subcuticular with 4/0 poliglecaprone 25 to ensure cosmesis. Drain is not used routinely. Subhepatic closed drain was placed in two patients with difficult dissection of the bed of the gallbladder and drains were taken out from the umbilicus. Drains were withdrawn on the first postoperative day. View of the third day after surgery is shown Fig. 5.
Fig. 2.

Intraumbilical incision and gelport insertion.
Fig. 3.
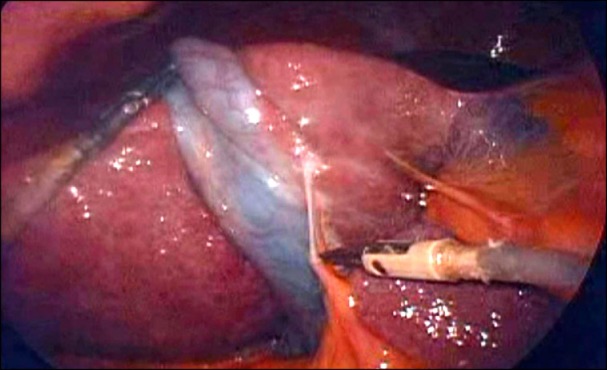
Gallbladder dissection with articulated instruments in group 1.
Fig. 4.
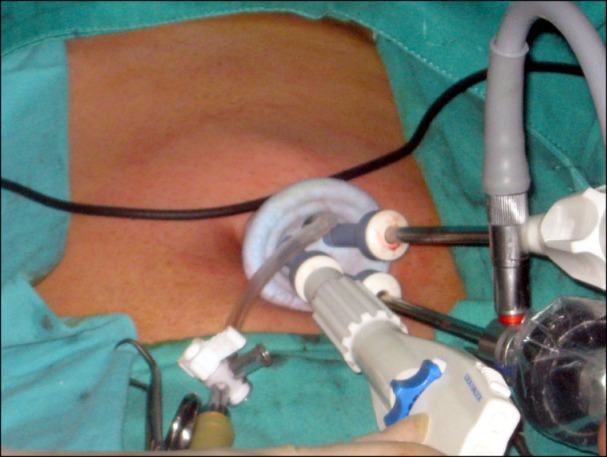
Instruments in the gelport.
Fig. 5.

Postoperative view of patient in group 1.
TPCL cholecystectomy
Pneumoperitoneum was created with Veress needle and a 10-mm trocar was placed in the umbilicus. Another 10-mm trocar was placed in the midepigastrium just to the right of the falciform ligament, and 5-mm trocars were placed in the right upper abdomen two fingerbreadths below the right coastal margin in the midclavicular line. A cholecystectomy is then performed in the standard fashion. The specimen is then removed and only umbilical fascia is closed with no:0 polypropylene sutures. Trocar wounds were sutured with 4/0 poliglecaprone 25. Subhepatic closed drain was placed in seven patients with difficult dissection of the bed of the gallbladder. Drains were withdrawn first postoperative day except in one patient with bile leakage.
Patient demographic data were compared using the parametric t-test. Nonparametric Mann-Whitney U test was performed for comparison of pain scores and cosmetic outcomes. Operating time, and hospital stay were compared using the t test. Fisher exact test was done for the complications. All statistical analyses were conducted by using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). The level of significance was set at 0.05.
RESULTS
One hundred patients enrolled in this study. The patients characteristics are presented in Table 1. There was no significant difference in the age, gender, diagnosis, ASA score and BMI between the groups. Forty-four SILS cholesystectomies (88%) and 42 TPCL cholecystectomies (84%) were completed successfully. Due to difficult dissection, four SILS cases and two TPCL cases were converted to open surgery. Two SILS cases and two TPCL cases were converted to conventional four port laparoscopic surgery due to inadequate visualization. Correlation between diagnosis and conversion was not determined (P > 0.05). We observed SILS cholecystectomy to be safe and feasible for acute cholecystitis. Two patients in group 1 and one of patient in group 2 were morbidly obese. We demonstared no correlation between BMI and conversion rate (P > 0.05).
Table 1.
Patients characteristics
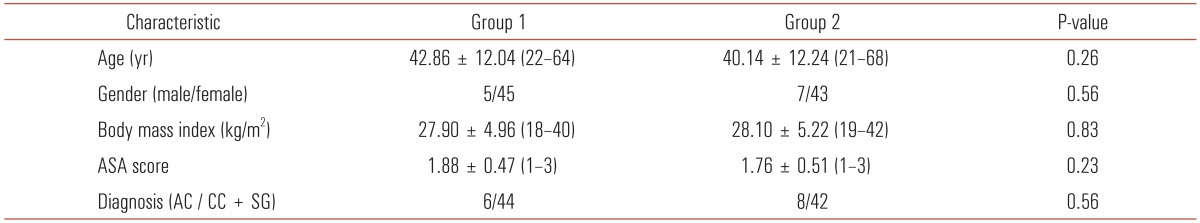
Values are presented as mean ± standard deviation (range).
ASA, American Society of Anesthesiology; AC, acute cholecystitis; CC, chronic cholecystitis; SG, symptomatic gallstone.
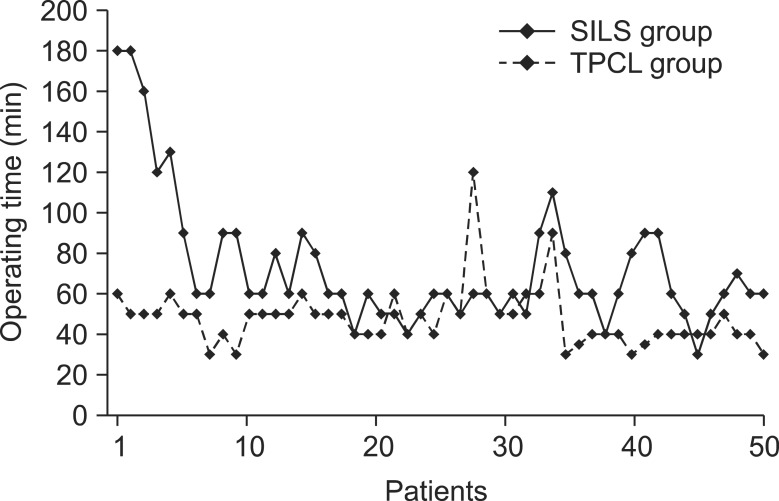
There were no complications during surgery such as bleeding and injury. Average blood loss was similar between the groups. Operating data are shown in Table 2. Operating time was significantly longer for group 1 versus group 2 (73 minutes vs. 48 minutes, P < 0.001). This difference is based on significant lack of experience in SILS procedure. A learning curve was noticed with respect to operating time in the SILS cholecystectomies. The mean operating time of the first 10 cases compared with the remainder of the series was 116 ± 45 minutes versus 62.2 ± 16 minutes. This decrease in operative time after the first 10 cases was statistically significant (P = 0.005) (Fig. 6).
Table 2.
Operative data
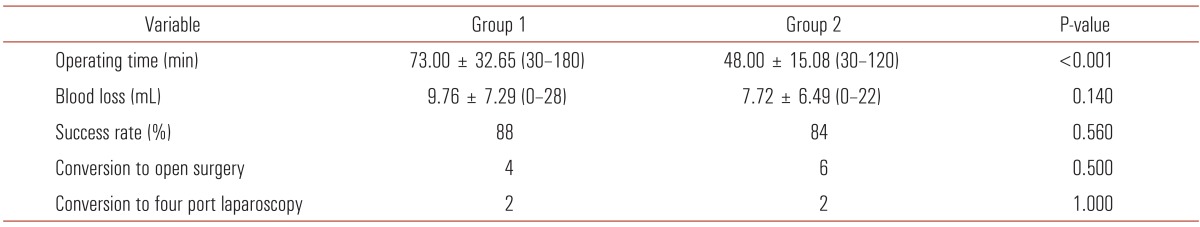
Values are presented as mean ± standard deviation (range).
Fig. 6.
Operating time. SILS group, single incision laparoscopic surgery cholecystectomy group; TPCL group, three port conventional laparoscopic cholecystectomy group.
We tabulated the pain score in both groups. POSH-VAS was more in the group 1 compared to the group 2 but that difference was not stastically significant. POFD-VAS was higher in group 1 than in group 2 (2.32 vs. 3.32, P < 0,001). Correlation between operative time and POFD-VAS was examined. Pearson correlation test demonstrated that the pain score correlated with operative time (P < 0.001). POFD-VAS was compared between groups excluding the first 10 cases. No statistical difference was determined between the groups excluding the first 10 cases (P = 0.42). Postoperative data are shown in Table 3.
Table 3.
Postoperative data
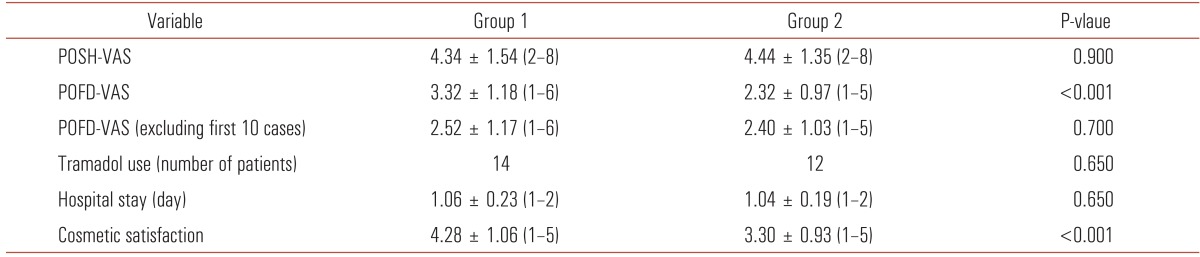
Values are presented as mean ± standard deviation (range).
POSH-VAS, sixth postoperative hour visual anologue scale; POFD-VAS, first postoperative day visual analogue scale.
One of the patients in group 2 had mild bile leakage for 2 days and was treated conservatively through a closed subhepatic drain placed in this patient because of difficult dissection of the bed of the gallbladder. None of the patients had indication for intraoperative cholangiography. Length of hospital stay was similar between the groups. Two patients in both groups were readmitted to hospital because of wound infection. These patients with wound infections were treated with local wound dressing and antibiotherapy. Complications rates are shown in Table 4. Mean follow-up was 24.0 ± 7.51 months (range, 12-36 months). At the time of submission of this manuscript, no patients had developed a postoperative port site hernia in both groups. Wound satisfaction score showed statistically significant differences between the groups (P < 0.001). SILS cholecystectomy patients were more satisfied with the umbilical scarless incision as expected (Table 3).
Table 4.
Complications
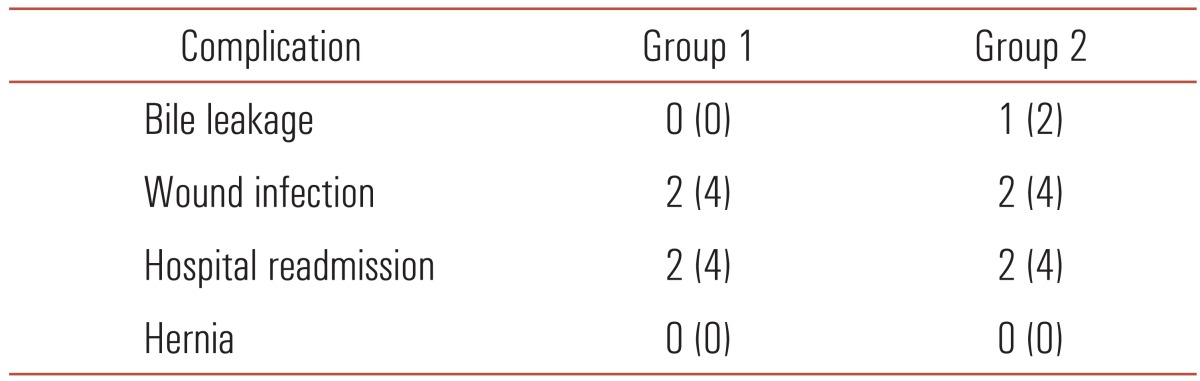
Values are presented as number (%). Fisher exact test was done for assessment.
P > 0.05.
DISCUSSION
Nowadays, four-trocar conventional cholecystectomy is the gold standard for symptomatic cholelithiasis. Notwithstanding the well-established advantages of four-port laparoscopic cholecystectomy over laparotomy, surgeons have continued to investigate less invasive procedures. Mini-laparoscopic cholecystectomy (MLC) was conceived in the 1990s under the name "needlescopic cholecystectomy" [9,10]. Two recent meta-analyses have shown that the only real advantage of MLC was the cosmetic outcome, although duration of operation was longer and the technique more difficult to perform because of the fragility of the microinstruments [11,12]. In reality, this technique has not been widely adopted.
The evolution to a decreased number of ports to complete laparoscopic procedures including cholecystectomy is not surprising in a field known as "minimal access surgery" [6]. The latest development, natural orifice translumenal endoscopic surgery (NOTES), is in its early stages, and there is little consensus about its safety and value to patients at this time [4,13]. The NOTES technique requires multidisciplinary cooperation, is often long and difficult, has created ethical problems as the transvaginal route, the most often employed, has been criticized. Moreover, with the inconvenience associated with NOTES, single site surgery has gained greater interest and diffusion. The umbilicus is considered by some as an embryological natural orifice [9]. It was therefore quite natural to see the development of laparoscopic surgery through a unique umbilical incision. This technique can be performed with conventional surgical instruments and the attending benefits are similar to those of NOTES [9].
The use of three trocars instead of four is definitely a step in this direction [14]. Single incision laparoscopic cholecystectomy is a step towards an even less invasive surgical procedure [15]. In our clinic, laparoscopic cholecystectomy is performed by three port for five years, except in a few patients. The umbilical access we use is a well-known and standardized site for access to the abdominal cavity for laparoscopy. It does not add new risks and results in the same operative view as in standard laparoscopic cholecystectomy [15]. SILS cholecystectomy is technically more challenging than conventional laparoscopic cholecystectomy. The major difficulty with SILS stems from the need for the surgeon to adapt to the new method of instrumentation. The SILS technique is not a naturally ergonomic technique because the traditional laparoscopic principles of triangulation are lost. Naturally, this situation leads to a long operation time at initial learning period. Our study confirms the feasibility of the technique although operative times were relatively long. Mean operation durations of more than 75 minutes have been reported in several publications [5,9,16-19]. Despite the long duration of surgery, surgeons should be patient. Our experience has shown that in subsequent cases, the operative time is shortened with increasing experience. Despite the long operative time (116 minutes) in the first ten cases, in the following cases, the mean operative time was 62 minutes in this study. With additional experience and improved instrumentation, SILS and conventional cholecystectomy can be of similar duration [7].
There are potential benefits of decreasing the number of ports to complete laparoscopic procedures as compared with the traditional multiport approach. These include less pain in the abdominal wall, less need for narcotic analgesics, earlier discharge from the hospital, quicker recovery and of course, fewer scars [6,7,16,20]. In a prospective randomized study, Tsimoyiannis et al. [14] compared four-port laparoscopic cholecystectomy and single access technique. They observed lower pain scores in SILS group than conventional laparoscopy. In fact, less pain and less need of narcotics for SILS is controversial. Ostlie et al. [21] compared, prospectively, SILS and four-port laparoscopic cholecystectomy and they observed pain scores, requirement of analgesics and length of hospital stay were not stastically different between the groups. In another prospective randomized study, Marks et al. [22] showed no statistical difference in average pain scores in all time points. Similarly, Luna et al. [23] determined SILS does not significantly reduce systemic inflammatory response, postoperative pain or analgesic use compared with conventional laparoscopy. On the other hand, in our study, we observed first postoperative day pain scores as higher in SILS group than conventional laparoscopy group. Similarly, Jung at al. [24] demonstrated pain score and analgesic requirement were higher in SILS group than conventional laparoscopy. In our study, analgesic requirement was not different between the groups.
Several authors have reported on SILS. Most of them used a variation of Navarra et al. described technique, using a straight transabdominal suture to pull the fundus of the gallbladder, and the use of retractable curved instruments in the dissection, while using different umbilical ports [5-7,9,22]. We believe that the use of percutaneously placed transfascial sutures is not essential but the transfascial sutures is very useful in difficult cases. On the other hand, in case of difficult dissection or inadequate visualization, transfascial sutures should be used. Transfascial sutures were used in 17 patients (34%) owing to difficult dissection or inadequate visualization in this study. In difficult cases, this was usually successful with one suture placed in the fundus, although in a minority of patients, additional sutures placed in the body and infundibulum were necessary for adequate exposure of the triangle of Callot. Hawasli et al. [25] demonstrated the benefit of EndoClose and Veress needle use. The use of the EndoClose to push the fundus of the gallbladder and the Veress needle to push the liver or duodenum allows the exposure of the triangle of Callot, according to them. EndoClose or Veress needle were not used for exposure in our study. Intraoperative cholangiograms (IOCs) have not always been performed routinely [15,17,18,26]. In a study by Curcillo 2nd et al. [27], IOC prolonged the operation by 19 minutes. Bokobza et al. [9] and Bucher et al. [28] recommend that cholangiograms should be performed routinely. In our study, there was no indication to perform IOC. We believe that IOC should not be performed routinely.
Khambaty et al. [2] showed that BMI was a risk factor for conversion to a traditional or multiport cholecystectomy. They suggested that morbidly obese patients with a BMI greater than 35 may not be candidates for single incision cholecystectomies. In our series, we observed no correlation of BMI conversion rate in SILS group. Acute cholecystitis has been exclusion criterion in many studies. We observed no correlation between acute cholecystitis and conversion to open surgery. We experienced no major additional difficulties in cases of morbid obesity or acute cholecystitis. Should any issue arise, a SILS procedure can always be converted to a standard laparoscopic cholecystectomy easily, with no need for a change in operative position or additional instruments.
In many trials, no significant difference in complication rate (intraoperative and postoperative) was found between SILS and conventional laparoscopic cholecystectomy [29]. The readmission rate of 4% in our study is similar to that of 5% reported in the literature [25]. Only two patients in both groups were readmitted to hospital because of wound infection. There were no late complications. Cosmetic satisfaction is significantly higher in SILS cholecystectomy [21,29]. Another study reported that the cosmetic outcomes were similar in SILS and conventional laparoscopic cholecystectomy [30]. Our study also demonstrated a high level of satisfaction in SILS group.
Single incision laparoscopic cholecystectomy is feasible and safe. The technique and technology for this are still in their infancy but rapidly catching up. Operative outcomes are acceptable. It provides superior cosmetic results by hiding the incision in the umbilicus, which is particularly important to younger female patients. In conclusion, a SILS cholecystectomy performed by experienced surgeons is at least as successful and safe as a traditional laparoscopic cholecystectomy.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Barbaros U, Dinccag A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg. 2009;13:1520–1523. doi: 10.1007/s11605-009-0869-8. [DOI] [PubMed] [Google Scholar]
- 2.Khambaty F, Brody F, Vaziri K, Edwards C. Laparoscopic versus single-incision cholecystectomy. World J Surg. 2011;35:967–972. doi: 10.1007/s00268-011-0998-6. [DOI] [PubMed] [Google Scholar]
- 3.Kaiser AM, Corman ML. History of laparoscopy. Surg Oncol Clin N Am. 2001;10:483–492. [PubMed] [Google Scholar]
- 4.Chamberlain RS, Sakpal SV. A comprehensive review of single-incision laparoscopic surgery (SILS) and natural orifice transluminal endoscopic surgery (NOTES) techniques for cholecystectomy. J Gastrointest Surg. 2009;13:1733–1740. doi: 10.1007/s11605-009-0902-y. [DOI] [PubMed] [Google Scholar]
- 5.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. [PubMed] [Google Scholar]
- 6.Elsey JK, Feliciano DV. Initial experience with single-incision laparoscopic cholecystectomy. J Am Coll Surg. 2010;210:620–624. doi: 10.1016/j.jamcollsurg.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 7.Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009;209:632–637. doi: 10.1016/j.jamcollsurg.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 9.Bokobza B, Valverde A, Magne E, Delaby J, Rubay R, Bellouard A, et al. Single umbilical incision laparoscopic cholecystectomy: initial experience of the Coelio Club. J Visc Surg. 2010;147:e253–e257. doi: 10.1016/j.jviscsurg.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Bittner R. The standard of laparoscopic cholecystectomy. Langenbecks Arch Surg. 2004;389:157–163. doi: 10.1007/s00423-004-0471-1. [DOI] [PubMed] [Google Scholar]
- 11.McCloy R, Randall D, Schug SA, Kehlet H, Simanski C, Bonnet F, et al. Is smaller necessarily better? A systematic review comparing the effects of minilaparoscopic and conventional laparoscopic cholecystectomy on patient outcomes. Surg Endosc. 2008;22:2541–2553. doi: 10.1007/s00464-008-0055-1. [DOI] [PubMed] [Google Scholar]
- 12.Hosono S, Osaka H. Minilaparoscopic versus conventional laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. J Laparoendosc Adv Surg Tech A. 2007;17:191–199. doi: 10.1089/lap.2006.0051. [DOI] [PubMed] [Google Scholar]
- 13.Auyang ED, Hungness ES, Vaziri K, Martin JA, Soper NJ. Human NOTES cholecystectomy: transgastric hybrid technique. J Gastrointest Surg. 2009;13:1149–1150. doi: 10.1007/s11605-009-0813-y. [DOI] [PubMed] [Google Scholar]
- 14.Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2010;24:1842–1848. doi: 10.1007/s00464-010-0887-3. [DOI] [PubMed] [Google Scholar]
- 15.Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009;23:896–899. doi: 10.1007/s00464-008-0147-y. [DOI] [PubMed] [Google Scholar]
- 16.Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg. 2009;75:681–685. [PubMed] [Google Scholar]
- 17.Romanelli JR, Roshek TB, 3rd, Lynn DC, Earle DB. Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc. 2010;24:1374–1379. doi: 10.1007/s00464-009-0781-z. [DOI] [PubMed] [Google Scholar]
- 18.Ersin S, Firat O, Sozbilen M. Single-incision laparoscopic cholecystectomy: is it more than a challenge? Surg Endosc. 2010;24:68–71. doi: 10.1007/s00464-009-0543-y. [DOI] [PubMed] [Google Scholar]
- 19.Lee SK, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech A. 2009;19:495–499. doi: 10.1089/lap.2008.0424. [DOI] [PubMed] [Google Scholar]
- 20.Vilallonga R, Barbaros U, Sumer A, Demirel T, Fort JM, Gonzalez O, et al. Single-port transumbilical laparoscopic cholecystectomy: a prospective randomised comparison of clinical results of 140 cases. J Minim Access Surg. 2012;8:74–78. doi: 10.4103/0972-9941.97586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ostlie DJ, Juang OO, Iqbal CW, Sharp SW, Snyder CL, Andrews WS, et al. Single incision versus standard 4-port laparoscopic cholecystectomy: a prospective randomized trial. J Pediatr Surg. 2013;48:209–214. doi: 10.1016/j.jpedsurg.2012.10.039. [DOI] [PubMed] [Google Scholar]
- 22.Marks J, Tacchino R, Roberts K, Onders R, Denoto G, Paraskeva P, et al. Prospective randomized controlled trial of traditional laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy: report of preliminary data. Am J Surg. 2011;201:369–372. doi: 10.1016/j.amjsurg.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Luna RA, Nogueira DB, Varela PS, Rodrigues Neto Ede O, Norton MJ, Ribeiro Ldo C, et al. A prospective, randomized comparison of pain, inflammatory response, and short-term outcomes between single port and laparoscopic cholecystectomy. Surg Endosc. 2013;27:1254–1259. doi: 10.1007/s00464-012-2589-5. [DOI] [PubMed] [Google Scholar]
- 24.Jung GO, Park DE, Chae KM. Clinical results between single incision laparoscopic cholecystectomy and conventional 3-port laparoscopic cholecystectomy: prospective case-matched analysis in single institution. J Korean Surg Soc. 2012;83:374–380. doi: 10.4174/jkss.2012.83.6.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hawasli A, Kandeel A, Meguid A. Single-incision laparoscopic cholecystectomy (SILC): a refined technique. Am J Surg. 2010;199:289–293. doi: 10.1016/j.amjsurg.2009.08.037. [DOI] [PubMed] [Google Scholar]
- 26.Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009;23:1138–1141. doi: 10.1007/s00464-009-0389-3. [DOI] [PubMed] [Google Scholar]
- 27.Curcillo PG, 2nd, Wu AS, Podolsky ER, Graybeal C, Katkhouda N, Saenz A, et al. Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc. 2010;24:1854–1860. doi: 10.1007/s00464-009-0856-x. [DOI] [PubMed] [Google Scholar]
- 28.Bucher P, Pugin F, Morel P. From single-port access to laparoendoscopic single-site cholecystectomy. Surg Endosc. 2010;24:234–235. doi: 10.1007/s00464-009-0626-9. [DOI] [PubMed] [Google Scholar]
- 29.Aprea G, Coppola Bottazzi E, Guida F, Masone S, Persico G. Laparoendoscopic single site (LESS) versus classic videolaparoscopic cholecystectomy: a randomized prospective study. J Surg Res. 2011;166:e109–e112. doi: 10.1016/j.jss.2010.11.885. [DOI] [PubMed] [Google Scholar]
- 30.Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg. 2011;254:22–27. doi: 10.1097/SLA.0b013e3182192f89. [DOI] [PubMed] [Google Scholar]