Abstract
Extrauterine epithelioid trophoblastic tumors constitute an extremely rare gestational trophoblastic disease. We report the case of an extrauterine trophoblastic tumor that was incidentally detected in the left lung. Squamous cell carcinoma was suspected after microscopically examining the specimen obtained upon preoperative needle biopsy. After surgery, the tumor was confirmed by microscopic findings and immunohistochemical features.
Keywords: Epithelioid trophoblastic tumor, Lung neoplasms
CASE REPORT
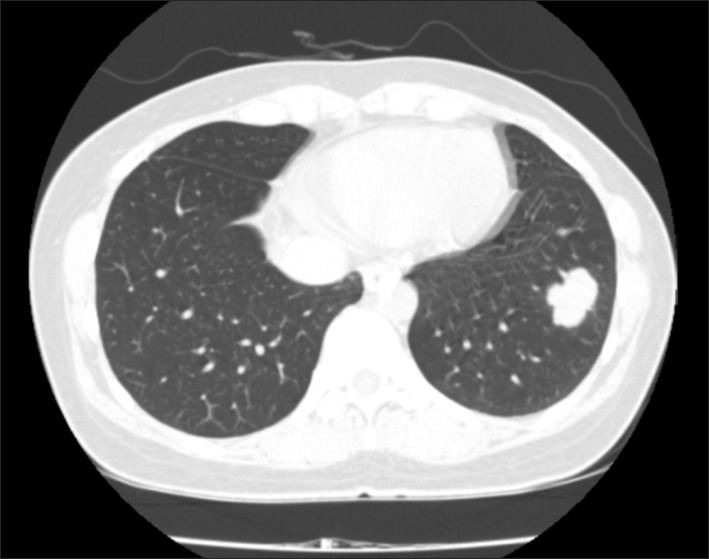
A 35-year-old multiparous woman was transferred to Asan Medical Center because of abnormal findings on lung imaging. She was admitted to the regional tertiary hospital because of abdominal pain, nausea, and vomiting 10 days prior to presentation to Asan Medical Center. During a work-up for evaluating the cause of her abdominal pain, a 2.7-cm pulmonary nodule was incidentally discovered in an abdominal computed tomography (CT) scan. Subsequently, a chest CT scan revealed that the nodule was located in the basal segment of the left lower lobe. The nodule had a well-defined lobule, whereas no other definite nodules or active lesions were found in the lungs (Fig. 1). For further evaluation, the patient was referred to Asan Medical Center. At the time of admission, the patient's vital signs were stable and her physical examination was unremarkable. The results of all laboratory tests were within normal limits.
Fig. 1.
A 2.7-cm well-defined lobulated nodule observed in the basal segment of the left lower lobe in chest computed tomography.
A lung needle biopsy was performed, the results of which indicated a few atypical cells that were positive for p63 and cytokeratin in a necrotic background. We believed that the characteristics of the nodule indicated squamous cell carcinoma. In 18-fluorodeoxyglucose positron emission tomography, the nodule showed a maximum standardized uptake value of 1.6 in the basal segment of the left lower lobe that indicated low metabolic activity. No other significant hypermetabolic lesions were found.
The follow-up chest CT performed after 1 month indicated that the mass had enlarged to 3.3×3.0 cm. No definite evidence of lymphadenopathy was seen in the hilar mediastinum. Because distant metastasis was not evident in brain magnetic resonance imaging or a bone scan, we performed video-assisted left lower lobectomy in addition to mediastinal lymph node dissection.
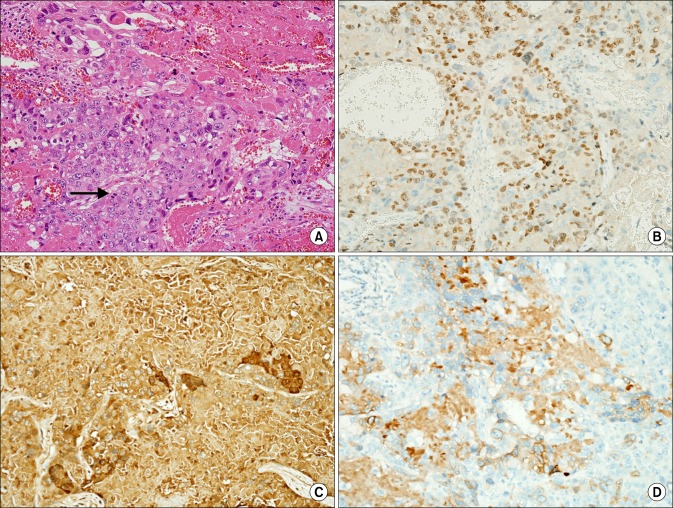
On gross examination, an ill-defined firm mass measuring 3.2×2.5×2 cm was observed. The mass was yellowish gray, firm, and granular with necrosis and an anthracotic pigment at the cut surface. Microscopic examination indicated that the mass was well-circumscribed and had replaced the normal pulmonary parenchyma. The tumor cells had a relatively uniform, mononuclear epithelioid appearance and were arranged in nests or cords. They had eosinophilic cytoplasm and irregular nuclei with prominent nucleoli. Hyaline-like materials were observed surrounding the tumor nest. Mitoses were occasionally observed (Fig. 2A). Tumor cells had positive immunoreactivity for p63 (Fig. 2B), beta-human chorionic gonadotropin (β-hCG) (Fig. 2C), cytokeratin, inhibin (Fig. 2D), sal-like protein 4, and placental alkaline phosphatase. Immunohistochemical staining for human placental lactogen, alpha-fetoprotein, and CD30 was negative.
Fig. 2.
(A) Epithelioid trophoblastic tumor predominantly composed of mononuclear epithelioid cells in nests. The tumor cells have eosinophilic cytoplasm and large, irregular nuclei with prominent nucleoli. Eosinophilic, hyaline-like materials, and necrotic debris surround the tumor nests. Mitoses are observed occasionally (→) (×200). (B) Immunohistochemical staining for p63: tumor cells are diffusely positive in the nucleus (×200). (C) Immunohistochemical staining of tumor cells indicates that the cells are diffusely positive for β-hCG in the cytoplasm (×200). (D) Immunohistochemical staining of the tumor cells indicates that the cells are focally positive for inhibin in the cytoplasm (×200).
We consulted the department of gynecology for pelvic examination ultrasonography, the findings of which were unremarkable. Endometrial curettage revealed normal menstrual-phase endometrium. The results of the postoperative serial serum β-hCG and carbohydrate antigen 19-9 tests were within normal limits at that time.
On postoperative day 3, the patient was discharged without complications. She received conservative treatment after that and underwent regular follow-ups in the outpatient clinic. After 15 months, a follow-up chest CT did not show any evidence of recurrence.
DISCUSSION
Epithelioid trophoblastic tumors constitute a rare gestational trophoblastic neoplasm first reported by Shih and Kurman [1] in 1998. In particular, extrauterine epithelioid trophoblastic tumors are extremely rare, and their diagnosis and treatment guidelines are not conclusive. Previous studies have reported that microscopic findings and immunohistochemical features are important because epithelioid trophoblastic tumors can be misdiagnosed as squamous cell carcinoma. In these cases, the tumors show nodular expansile lesions that grow in nests and cords composed of mononulcear trophoblastic cells with eosinophilic, hyaline-like materials and necrotic debris; these tumor cells are positive for p63, inhibin, cytokeratin, β-hCG, and/or human placental lactogen [1-3].
For the diagnosis of pulmonary extrauterine epithelioid trophoblastic tumors, several criteria should be met. First, the woman should be of reproductive age and should be primiparous or multiparous or have a history of antecedent uterine epithelioid trophoblastic tumor. Second, mildly elevated serum β-hCG levels should be detected. Third, an isolated pulmonary lesion should be detected with unusual pathologic features [2]. Our case meets these conditions except for the normal level of serum β-hCG.
Because epithelioid trophoblastic tumors are rare, their prognosis and clinical course are not well known. However, a high mitotic index should be considered a marker for malignancy, and the mass should be completely removed for a precise diagnosis and the prevention of recurrence [3]. In other previously reported cases, adjuvant chemotherapy was administered although the regimen was not well defined. Adjuvant chemotherapy regimens in previous reports have varied depending on the institution or the patient's condition. Ahn et al. [2] used 6 cycles of etoposide, methotrexate, dactinomycin, cyclophosphamide, and vincristine; Macdonald et al. [4] used 6 cycles of cyclophosphamide, etoposide, and cisplatin for 1 patient, and 8 cycles of etoposide and cisplatin for another case; and Lewin et al. [5] used 3.5 cycles of cisplatin and etoposide for 1 patient, and 3 cycles of etoposide, methotrexate, and dactinomycin alternating with cisplatin and etoposide for another patient.
We did not perform additional adjuvant chemotherapy because the mitotic index of the tumor was low, the β-hCG serum level was normal, and the tumor was completely removed by lobectomy. We plan to closely observe the patient and conduct serial follow-ups, and if the tumor recurs, we will consider adjuvant chemotherapy.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Shih IM, Kurman RJ. Epithelioid trophoblastic tumor: a neoplasm distinct from choriocarcinoma and placental site trophoblastic tumor simulating carcinoma. Am J Surg Pathol. 1998;22:1393–1403. doi: 10.1097/00000478-199811000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Ahn HY, Hoseok I, Lee CH, et al. Pulmonary mass diagnosed as extrauterine epithelioid trophoblastic tumor. Thorac Cardiovasc Surg. 2013;61:97–100. doi: 10.1055/s-0032-1331264. [DOI] [PubMed] [Google Scholar]
- 3.Fadare O, Parkash V, Carcangiu ML, Hui P. Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement. Mod Pathol. 2006;19:75–82. doi: 10.1038/modpathol.3800485. [DOI] [PubMed] [Google Scholar]
- 4.Macdonald MC, Palmer JE, Hancock BW, Tidy JA. Diagnostic challenges in extrauterine epithelioid trophoblastic tumours: a report of two cases. Gynecol Oncol. 2008;108:452–454. doi: 10.1016/j.ygyno.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Lewin SN, Aghajanian C, Moreira AL, Soslow RA. Extrauterine epithelioid trophoblastic tumors presenting as primary lung carcinomas: morphologic and immunohistochemical features to resolve a diagnostic dilemma. Am J Surg Pathol. 2009;33:1809–1814. doi: 10.1097/PAS.0b013e3181b9cd67. [DOI] [PubMed] [Google Scholar]