Abstract
Plasmacytoma is a plasma cell neoplasm that locally infiltrates a bone or spreads to extramedullary areas. A new World Health Organization criterion defines solitary plasmacytoma of bone as a localized bone tumor consisting of plasma cells identical to those seen in plasma cell myeloma, which is manifested as a solitary osteolytic lesion in a radiological evaluation. Primary tumors of the sternum are generally malignant, and solitary plasmacytomas of the sternum are very rare tumors. We present herein the case of a patient who had a primary sternal tumor with solitary plasmacytoma and no evidence of multiple myeloma.
Keywords: Plasmacytoma, Sternum, Multiple myeloma
CASE REPORT
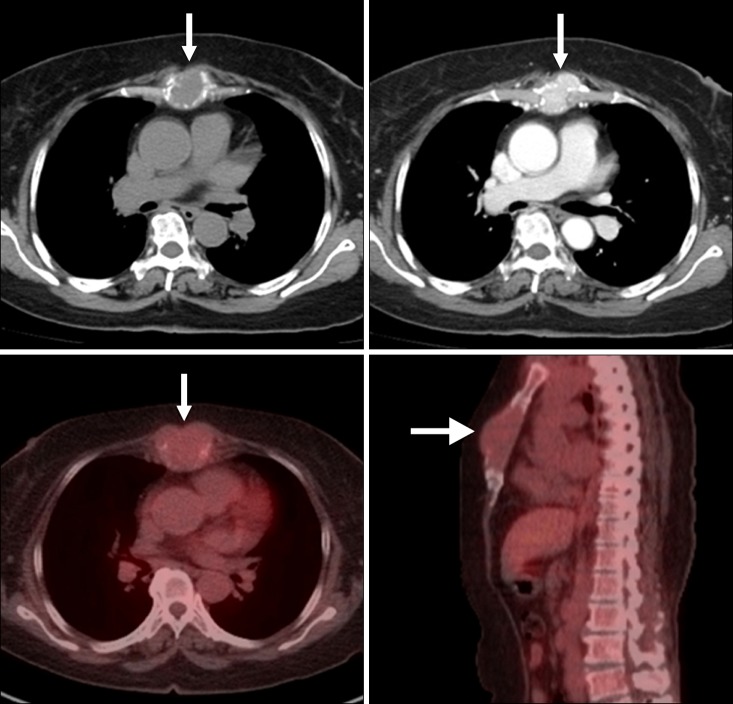
A 62-year-old female patient was referred by a regional hospital to department of thoracic and cardiovascular surgery because of a mass in her sternum. At presentation, the patient had no disease other than hypertension. She had received calcium channel blocker therapy for her hypertension at a regional hospital for >3 years prior to this presentation, and her blood pressure was well controlled. She was a housewife by occupation and did not have any specific family history of cancer. Her blood pressure was 118/72 mmHg; pulse rate, 64 beats/min; respiratory rate, 16/min; and body temperature, 36.7℃. A physical examination revealed a bulging mass in the mid-sternum and mild tenderness around the mass. Laboratory tests revealed white blood cell, 7,800/µL and hemoglobin, 13.2 g/dL. However, other initial laboratory test results were noted to be within the normal range. Plain chest radiographs, including the sternum lateral view, revealed a sternal mass. Chest computed tomography (CT) revealed a sternal mass 4×4 cm in size containing an osteoclastic lesion in the body of the sternum. A further evaluation using whole body bone scintigraphy revealed a focus of mild increased uptake in the sternum with a bone-to-soft tissue ratio of 2.34:1, and no evidence of a hot uptake lesion was noted in the other bony areas. Positron emission tomography-CT (PET-CT) with 18-fluro-deoxyglucose showed a mildly hypermetabolic mass in the body of the sternum with a standard uptake value of 4.6 but did not detect any other lesions or distant metastasis other than a sternal lesion (Fig. 1). Under localized anesthesia, an incisional biopsy was performed, which showed atypical plasma cells having centrally or eccentrically located ovoid nuclei and eosinophilic cytoplasm. These histological findings indicated a plasma cell neoplasm suggestive of solitary plasmacytoma of the sternum (Fig. 2). Immunohistochemical studies of the specimen showed positive lambda chains and negative kappa chains, but the results were all negative for the clusters of differentiation 99, neuron specific enolase, S-100, cytokeratin, and desmin. Further studies were performed to differentiate solitary plasmacytoma of sternum from multiple myeloma (MM). Complete skeletal radiographs, including the humerus and femur, revealed negative results and no evidence of other osteolytic lesions. In addition, laboratory studies, including complete blood cell count, serum electrophoresis, 24-hour urine protein electrophoresis, alkaline phosphatase, lactic dehydrogenase, C-reacting protein, serum calcium, and phosphate showed normal values and no evidence of anemia, hypercalcemia, or renal involvement suggestive of systemic myeloma. Immunofixation of serum and concentrated urine exhibited no monoclonal proteins.
Fig. 1.
Chest computed tomography (CT) and positron emission tomography-CT scans of a sternal bulging mass. The white arrow indicates a solitary plasmacytoma of the sternum.
Fig. 2.
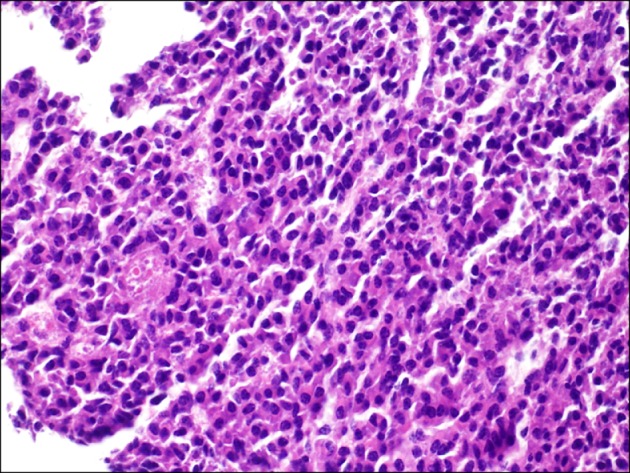
Pathological features of an incisional biopsy specimen from the sternum. Atypical plasma cells having centrally or eccentrically located ovoid nuclei and eosinophilic cytoplasm indicate plasma cell neoplasms suggestive of solitary plasmacytoma of the sternum (H&E, ×400).
Multidisplinary approaches for further management, including radiotherapy, surgical management with wide resection, and chemotherapy, were discussed, and radiation therapy was determined to be the best choice for the patient. The patient was transferred to the department of hemato-oncology and radiation oncology.
DISCUSSION
Solitary bone plasmacytoma (SBP) is defined as the clonal proliferation of plasma cells identical to those of plasma cell myeloma, which manifests itself as a localized osseous growth. Plasma cell neoplasms account for approximately 1% to 2% of all human malignancies and occur at a rate of about 3.5/100,000 per year. SBP is composed of monoclonal plasma cells, which are cytologically, immunophenotypically, and genetically identical to those seen in MM [1]. MM is a multi-focal plasma cell proliferation in the bone marrow, produces excess immunoglobulin, and infiltrates bone. Free light chains are also produced along with intact proteins; these light chains are detected by urine protein electrophoresis and are designated as Bence-Jones proteins. Excess cytokines activate osteoclasts, leading to bone destruction and subsequently to discrete lytic lesions or diffuse osteopenia. Increased bone resorption also leads to hypercalcemia associated with neurologic manifestations. Patients are susceptible to recurrent bacterial infections due to the suppression of normal humoral immunity, which is frequently the cause of death. Bence-Jones proteins are toxic to renal tubular cells and thus may contribute to renal insufficiency or failure [2]. Chondrosarcoma is the most common tumor among primary malignant tumors of the sternum, although its incidence is extremely low. Of the 11,087 bone tumors in the Dahlin tumor series at the Mayo Clinic, only 66 (0.6%) were primary malignant tumors of the sternum. Of these 66 tumors, 22 (33%) were chondrosarcomas; 20 (30%) were myelomas, including plasmacytomas; 14 (21%) were lymphomas; 8 (12%) were osteosarcomas; 1 (1.5%) was a fibrosarcoma; and 1 (1.5%) was a Ewing tumor [3]. Zehani et al. [4] in a study of primary malignant tumors of the sternum observed for 16 years between 1993 and 2009, reported that primary tumors of the sternum were very rare and accounted for only 0.5% of all of the primary bone tumors they encountered and that these tumors were often malignant, osteolytic, and aggressive. They also described 6 cases of primary malignant tumors of the sternum, of which 3 were plasmacytomas, 1 was a chondrosarcoma, 1 was an osteosarcoma, and 1 was a large B-cell lymphoma. Plasmacytoma arises in bone or soft tissue. SBP is defined as a tumor confined to a bone with no multiple osteolytic lesions, while extramedullary plasmacytoma (EMP) is defined as a tumor that occurs only in a soft tissue with no multiple osteolytic lesions. EMP mainly involves the head, neck, and lungs [2]. SBP is relatively rare and accounts for 3% to 5% of all plasma cell neoplasms [1]. The median age at the diagnosis of SBP is 55 years, and SBP occurs 10 years earlier than MM. Males are more frequently affected than females, and one study reported that two-thirds of all patients were male [2]. SBP more commonly involves the axial skeleton, and distal appendicular diseases are extremely rare. As in MM, marrow areas with active hematopoiesis are targeted, including the vertebrae, ribs, skull, pelvis, femur, clavicle, and scapula, in order of decreasing frequency [1]. The thoracic vertebrae are more frequently involved than the lumbar, sacral, and cervical spines. SBP originates in the medullary cavity and erodes through cancellous and cortical bone. Thus, punched-out defects are seen on radiographs and usually measure 1 to 4 cm. Patients may present with pathologic fractures or skeletal pain. Further, cord compression may be the presenting feature of solitary plasmacytoma involving the vertebrae. Soft tissue extension of the tumors may result in palpable masses, particularly when the rib is involved. Therefore, SBP should be distinguished from MM. The International Myeloma Working Group has established the following criteria for the diagnosis of SBP [5]. The diagnosis of SBP requires a solitary bone lesion; a biopsy which shows histological evidence of bony involvement by plasma cells; negative results of complete skeletal radiographs, including the humerus and femur, that show no lytic lesions; absence of clonal plasma cells in a random sample of bone marrow; no evidence of anemia, hypercalcemia, or renal involvement suggestive of systemic myeloma; and immunofixation of serum and concentrated urine that shows no monoclonal proteins [6]. Like MM, SBP has a lytic appearance on plain radiographs. CT and particularly, magnetic resonance imaging (MRI) depict the extent of SBP more clearly. MRI is useful for identifying additional unsuspected plasma cell lesions that do not appear in a skeletal survey. Some recent studies have emphasized the necessity of CT and MRI along with 99m Tc-MIBI scintigraphy, while others have mentioned the increased diagnostic sensitivity of fluorine-18 fluorodeoxyglucose PET. Electrophoresis of serum and urine samples reveals monoclonal proteins in 24% to 72% of SBP patients, although protein levels are considerably lower in SBP patients than in MM patients. All SBP patients should undergo serum and urine immunofixation even when electrophoresis results are normal because monoclonal proteins may not be detected in approximately one-third of all patients [1,6]. SBP can be definitively diagnosed by a biopsy. The gross and microscopic features of solitary plasmacytoma are identical to those of MM. Histologically, plasmacytoma appears as sheets of plasma cells. These are small round blue cells with 'clock-face' nuclei and abundant cytoplasm with a perinuclear clearing or 'halo.' Plasmacytoma exhibits monoclonal kappa or lambda light chains, whereas plasma cells of reactive chronic osteomyelitis are polyclonal [3,4]. Radiotherapy is the treatment of choice for SBP; however, there exists controversy regarding extensive wide resection. Treatment fields should be designed to encompass all diseases shown by MRI or CT scanning and should include a margin of normal tissue. Localized radiotherapy should be administered even if the tumor is completely removed for diagnostic purposes. The local response rate has been shown to be 80% to 90%, and there is no clinical evidence that adjuvant or prophylactic chemotherapy prevents the ultimate development of MM. Approximately 55% of patients with SPB develop MM within 10 years of successful treatment; 10% develop local recurrences or solitary plasmacytomas at different locations [7]. Although solitary plasmacytoma occurs less commonly in the sternum than MM, it must be considered in the differential diagnosis of bone and soft tissue tumors, particularly in the absence of lytic lesions in a skeletal survey and in the presence of clinical evidence of end organ damage. Unfortunately, more than half of the patients with solitary plasmacytoma develop MM during their lifetime.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Pezzella AT, Fall SM, Pauling FW, Sadler TR. Solitary plasmacytoma of the sternum: surgical resection with long-term follow-up. Ann Thorac Surg. 1989;48:859–862. doi: 10.1016/0003-4975(89)90688-7. [DOI] [PubMed] [Google Scholar]
- 2.Shih LY, Dunn P, Leung WM, Chen WJ, Wang PN. Localised plasmacytomas in Taiwan: comparison between extramedullary plasmacytoma and solitary plasmacytoma of bone. Br J Cancer. 1995;71:128–133. doi: 10.1038/bjc.1995.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Unni KK, Dahlin DC. Dahlin's bone tumors: general aspects and data on 11,087 cases. Philadelphia: Lippincott-Raven; 1996. [Google Scholar]
- 4.Zehani A, Ayadi-Kaddour A, Marghli A, et al. Primary malignant tumors of the sternum. Tunis Med. 2012;90:824–828. [PubMed] [Google Scholar]
- 5.International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol. 2003;121:749–757. [PubMed] [Google Scholar]
- 6.Dimopoulos MA, Moulopoulos LA, Maniatis A, Alexanian R. Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood. 2000;96:2037–2044. [PubMed] [Google Scholar]
- 7.Kyle RA. "Benign" monoclonal gammopathy: after 20 to 35 years of follow-up. Mayo Clin Proc. 1993;68:26–36. doi: 10.1016/s0025-6196(12)60015-9. [DOI] [PubMed] [Google Scholar]