Abstract
Background
Adults over age 40 are increasing their use of email and social media, raising interest in use of peer-to-peer Internet-based messaging to promote cancer screening.
Objective
The objective of our study was to assess current practices and attitudes toward use of email and other e-communication for peer-to-peer dialogues on cancer screening.
Methods
We conducted in-person interviews with 438 insured adults ages 42-73 in Georgia, Hawaii, and Massachusetts. Participants reported on use of email and other e-communication including social media to discuss with peers routine health topics including breast and colorectal cancer (CRC). We ascertained willingness to share personal CRC screening experiences via conversation, postcard, email, or other e-communication. Health literacy scores were measured.
Results
Email had been used by one-third (33.8%, 148/438) to discuss routine health topics, by 14.6% (64/438) to discuss breast cancer screening, and by 12.6% (55/438) to discuss CRC screening. Other e-communication was used to discuss routine health topics (11.6%, 51/438), screening for breast cancer (3.9%, 17/438), and CRC (2.3%, 10/438). In the preceding week, 84.5% (370/438) of participants had used email, 55.9% (245/438) had used e-communication of some type; 44.3% (194/438) text, 32.9% (144/438) Facebook, 12.3% (54/438) instant message, 7.1% (31/438) video chat, and 4.8% (21/438) Twitter. Many participants were willing to share their CRC screening experiences via email (32.4%, 142/438 might be willing; 36.3%, 159/438 very willing) and via other e-communication (15.8%, 69/438 might be willing; 14.4%, 63/438 very willing). Individuals willing to send CRC screening emails scored significantly higher on tests of health literacy compared to those willing to send only postcards (P<.001).
Conclusions
Many adults are willing to use email and e-communication to promote cancer screening to peers. Optimal approaches for encouraging peer-to-peer transmission of accurate and appropriate cancer screening messages must be studied.
Keywords: colorectal neoplasms, electronic mail, social media, breast neoplasms, early detection of cancer, communication, health promotion, Internet, peer group, social support
Introduction
Electronic Peer Communication
The rise in use of email and social media among Americans over age 40 presents a unique opportunity for the development of novel health care interventions [1-6]. Electronic peer communication has been shown to influence political [7], consumer [8], and health-related behavior [9,10]. Internet-based peer-to-peer communication has the potential to act via a number of mechanisms, including information exchange, social support (eg, emotional and instrumental), and establishment of group norms [11]. Encouraging peer-to-peer promotion of healthy lifestyles and of cancer screening may be an effective way to further cancer prevention efforts in today’s rapidly changing and collaborative Web 2.0 environment [5,6,12,13].
Web 2.0
Web 2.0 is a term used to describe the interactive experience of the Internet (in the form of blogs, wikis, Internet-based forums, etc.) [14], which has been made possible by technological advances that allow for and encourage open sharing of information. Increasingly, adults over age 50 share information using social media platforms that enable the interactive Web by engaging users who create content and communicate with their social network members (eg, Facebook, Twitter, and LinkedIn) [1,4,15]. Adults of all ages now go online to share their own experiences and to seek advice from friends and family on issues such as chronic disease caregiver roles and medical crises [12]. While medical illness may pose a more urgent prompt for peer-to-peer communication, a recent study indicates that several hundred breast cancer and colorectal cancer groups exist on Facebook and Twitter, and that cancer prevention is the main objective in over one-quarter of these groups [16]. We were interested in assessing the feasibility of a peer-to-peer intervention in which individuals who had completed cancer screening tests were invited to share their experiences with unscreened peers in order to promote completion of recommended screening behavior. We identified understanding current practices in Internet-based cancer screening discussion and gauging acceptability of such discussions as a necessary first step in developing our intervention.
In a diverse group of HMO-insured patients across three states (Georgia, Hawaii, and Massachusetts), we sought to document current practices and attitudes toward Internet-based email and social media cancer screening discussions. We also explored willingness to use these avenues for future peer communication and the association between health literacy and likely mode of communication.
Methods
Study Population and Setting
This study was conducted within the Cancer Research Network (CRN), a consortium of research organizations affiliated with 14 community-based nonprofit integrated health care delivery systems and the National Cancer Institute. Participants were recruited from three health plans–Kaiser Permanente Georgia (KPGA), Kaiser Permanente Hawaii (KPHI), and Fallon Community Health Plan (FCHP). This study was reviewed and approved by the Institutional Review Boards at each of the plans.
Participants in the present study had previously completed a two-hour study session for a larger study focused on communication of cancer information [17]. One CRN site—Kaiser Permanente Colorado—participated in the previous larger study, but not in the present study. All participants were 40-70 years of age at the time of recruitment for the larger study (some were 71 by the time the interviews occurred), all had been a member of one of the participating health plans for a minimum of 5 years, were able to understand English, and had no physical or mental limitation that would preclude participating in a two-hour in-person interview. We targeted this age range because these adults are most likely to face cancer screening decisions and to be at elevated risk for most cancers compared to younger adults. To optimize sampling across educational levels, at FCHP, KPGA and KPHI, sampling was stratified by United States Census-based estimates of educational level defined by the percentage of residents with a high school education or less in the census tract in which participants lived. At KPGA, sampling was further stratified according to the percent of African-American residents, to ensure that African-American and white members were invited in equal numbers within each educational strata. A variety of recruitment techniques were used, including mailings, telephone follow-up, and offering sessions at multiple locations. Interested participants were screened to confirm ability to communicate in English, adequate corrected hearing and vision, and the absence of physical or psychological limitations that would preclude participation. Study sessions lasted approximately 2 hours, and were conducted in-person by a trained research assistant. All items (except reading items) were administered orally. A total of 1074 participants completed interviews between June 22, 2009 and April 19, 2010.
For the present study, 3 sites participated (KPGA, KPHI, and FCHP). There were 789 participants from the initial study that were contacted by mail; approximately one week later, individuals who did not respond were contacted via telephone to again extend the invitation to participate. There were 438 (56% of the 789 people invited) people who agreed to participate. For budgetary reasons, participants from FCHP were recruited more aggressively and made up a higher proportion of this current study population (46.3%, 203/438 of the present study sample was from FCHP as compared to 28.86%, 310/1074 of the previous larger study). This higher proportion of FCHP participants resulted in a higher proportion of white participants. There were no significant differences in age, educational level, health literacy scores, numeracy scores, or self-reported health status for current study participants from the 3 sites as compared to previous participants at these 3 sites.
Interviews were conducted for the present study between August 4, 2011 and January 27, 2012. Sessions lasted approximately 1 to 1.5 hours (see Multimedia Appendix 1).
Data Collection
Health literacy assessments were conducted during the previous study’s sessions. Comprehension of spoken health messages (sometimes referred to as verbal health literacy) was assessed using the Cancer Message Literacy Test-Listening (CMLT-Listening). This test is administered via computer and requires no reading. Development of this test is described in further detail elsewhere [18]; results of reliability and validity studies are described by Mazor et al [17]. Print literacy was assessed using the Cancer Message Literacy Test-Reading (CMLT-Reading) [17,18]. Numeracy was assessed using the Lipkus numeracy scale [19]. Self-efficacy was assessed using the Perceived Efficacy in Patient-Physician Interactions (PEPPI) [20]. Aside from the CMLT-Reading, research staff administered the measures verbally.
During in-person interviews, 438 returning participants engaged in the current study reported on their recent use of email and other electronic communication. E-communication included texting, Facebook, instant messaging, Internet-based and video chatting, Twitter, and LinkedIn. We queried participants on their use of these media: (1) for any purpose, (2) to discuss routine health-related topics (including cancer screening, vaccines, diet, or exercise), and (3) for specific types of cancer screening; colorectal cancer (CRC) and breast cancer. Participants were also questioned regarding their willingness to communicate about such topics using email and other forms of e-communication.
In order to explore the role of user-generated content, participants were provided with the following hypothetical situation–“Imagine that you completed colon cancer screening. Everything went OK and your results were fine. The doctor asked you to help educate friends and family members over age 50 about colon cancer screening. We are trying to design a message to be sent out by people who have completed colonoscopies, so that they can explain to friends and family why screening is important. Please help us design a message you’d be willing to pass along to friends and family members over age 50.”
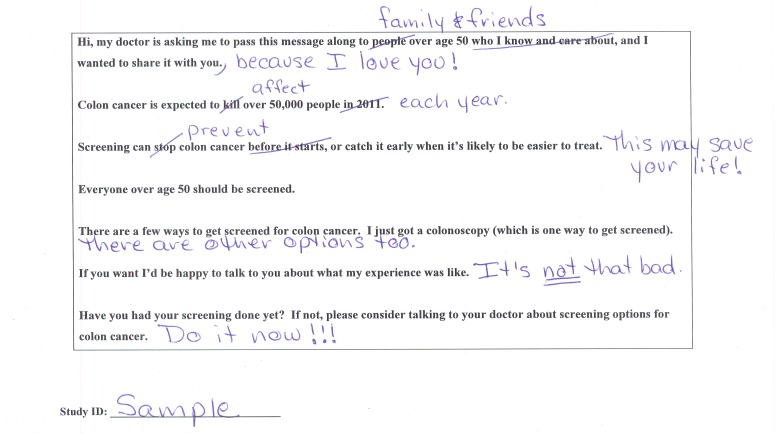
We then provided participants with a sample message in which the sender shares the fact that he or she has completed a colonoscopy and urges readers to discuss CRC screening with their doctor (Figure 1 shows the sample message). We encouraged participants to edit the message as they wished, then asked whether they would be willing to send the edited message to friends and family by either email or postcard. No messages were actually sent. Those who indicated they would not be willing to pass along their message (“nonsenders”) were asked to explain why and their answers were transcribed and categorized.
Figure 1.
Colorectal cancer screening message template with edits (example).
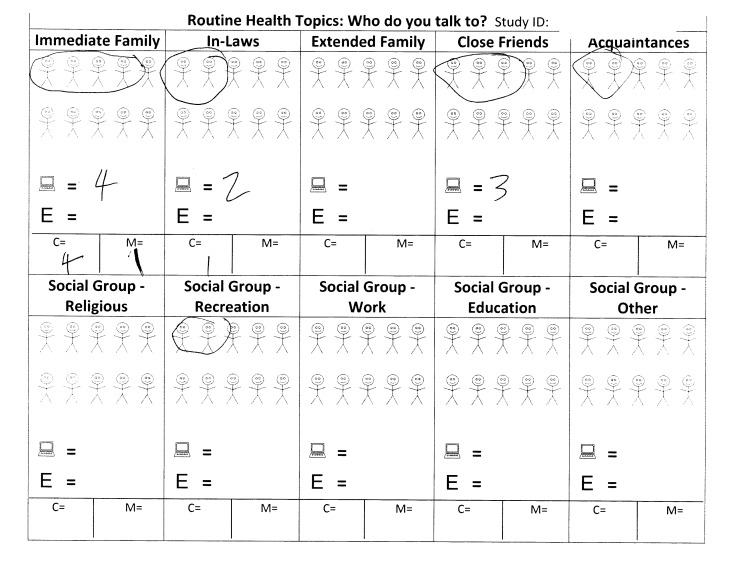
Participants who indicated that they would be willing to pass along messages were asked to estimate the number of emails or postcards they would send. To facilitate this estimation, participants were offered a worksheet (Figure 2 shows this worksheet) and encouraged to circle stick figures in each of 10 social group categories in order to visually designate members of their social network with whom they communicate about routine health topics and cancer screening.
Figure 2.
Health communication network tool. Study participants were provided with blank worksheets and asked: “Please mark one stick figure for each person you can think of that you communicate with about routine health topics…these are people you would communicate with about routine health topics like cancer screening, vaccine shots, diet, or exercise.” The worksheet was used to facilitate the estimation of the number of emails or postcards promoting colorectal cancer screening that they would send to members of their social network.
Analysis
We calculated the number of people who reported using email and e-communication for: (1) any use, and (2) discussion of routine health topics including cancer screening. We used χ2 to analyze bivariate associations between age group and use of email or e-communication. Then, focusing on CRC (since this screening is applicable to both men and women), we analyzed willingness to share CRC screening experience via various modes (through general conversation, email, or other e-communication; or through a specific self-edited message via email or postcard). For this analysis we again used χ2 to analyze bivariate associations between age and willingness to share via various modes. Finally, we sought to understand whether sociodemographic factors or measures of health literacy, numeracy, or self-efficacy were associated with willingness to share CRC screening experience via email or postcard. We conducted a multinomial logistic regression model (generalized logistic regression) using SAS 9.2 (SAS Institute, Inc, Cary, NC), modeling the odds of being: (1) an email sender, or (2) a postcard sender, as compared to (3) being a nonsender. We then conducted a logistic regression modeling the odds of being a sender of either email or postcard. We included in the model variables identified a priori as being of interest.
Results
Study Participants
The majority of our study participants (52.3%, 229/438) were 60 years or older and there were slightly more women (56.4%, 247/438) than men (See Table 1). There were three-quarters (75.6%, 331/438) reporting educational levels above a high school degree. Almost 90% (382/438) of all participants reported ever having completed any type of CRC screening and 72.6% (318/438) reported having had a colonoscopy.
Table 1.
Participant characteristics. χ2 used to derive P values shown for age, gender, race/ethnicity, education, marital status, ever had friends/family diagnosed with CRC, and ever had a colonoscopy. Analysis of variance–ANOVA used to derive P values for health literacy scores, numeracy, and self-efficacy.
| Characteristic | n | % | |
| Study sample |
|
438 | 100.0 |
| Study site |
|
|
|
|
|
Georgia | 130 | 29.7 |
|
|
Hawaii | 105 | 24.0 |
|
|
Massachusetts | 203 | 46.3 |
| Race/ethnicity |
|
|
|
|
|
Black/African-American | 65 | 14.8 |
|
|
Asian/Pacific Islander | 45 | 10.3 |
|
|
White/Caucasian | 286 | 65.3 |
|
|
Other or not reported | 42 | 9.6 |
| Language spoken at home |
|
|
|
|
|
English | 419 | 95.7 |
|
|
English and other | 9 | 2.1 |
|
|
Other | 7 | 1.6 |
| Education |
|
|
|
|
|
High School degree or less (includes technical school) | 104 | 23.7 |
|
|
At least some college | 331 | 75.6 |
| Age (in years) |
|
|
|
|
|
40-49 | 52 | 11.9 |
|
|
50-59 | 157 | 35.8 |
|
|
60-73 | 229 | 52.3 |
| Gender |
|
|
|
|
|
Male | 191 | 43.6 |
|
|
Female | 247 | 56.4 |
| Marital status |
|
|
|
|
|
Married | 282 | 64.4 |
|
|
Unmarried | 153 | 34.9 |
| Work status |
|
|
|
|
|
Working for pay | 260 | 59.4 |
|
|
Retired | 126 | 28.8 |
|
|
Disabled | 17 | 3.9 |
|
|
Other | 35 | 8.0 |
| Self-reported health status |
|
|
|
|
|
Excellent/very good | 240 | 54.8 |
|
|
Good/fair/poor | 197 | 45.0 |
| Number of comorbidities |
|
|
|
|
|
0/1 | 336 | 76.7 |
|
|
2+ | 99 | 22.6 |
| Current smoking status |
|
|
|
|
|
Current smoker | 27 | 6.2 |
|
|
Current nonsmoker | 410 | 93.6 |
| Has doctor ever recommended that you be screened for CRC cancer? |
|
|
|
|
|
Yes | 385 | 87.9 |
|
|
No | 48 | 11.0 |
| Completed any type of CRC screening? |
|
|
|
|
|
Yes | 382 | 87.2 |
|
|
No | 50 | 11.4 |
| Ever had a colonoscopy? |
|
|
|
|
|
Yes | 318 | 72.6 |
|
|
No | 114 | 26.0 |
| Health literacy, numeracy, and efficacy measures, mean (SD) | |||
| Verbal health literacy (CMLT-Listening) | 79.9 | (14.1) | |
| Print health literacy (CMLT-Reading) | 84.8 | (14.6) | |
| Numeracy | 78.5 | (21.9) | |
|
|
Self-efficacy (PEPPI) | 8.1 | (1.3) |
Use of Email for Discussions of Routine Health Topics and Cancer Screening
A high percentage of participants (84.5%, 370/438) had used email in the past week with no significant variation across age categories (Table 2). Only one-third of the participants (33.8%, 148/438) had ever used email to discuss routine health topics, and more than one in ten had used email to discuss CRC screening (12.6%, 55/438) or breast cancer screening (14.6%, 64/438). There was no significant variation by age category for these measures.
Table 2.
Use of email and social media to discuss health-related topics and to discuss cancer screening.
|
|
Total sample (N=438) |
Age 40-49 | Age 50-59 | Age 60-73 | P | |||||
|
|
n | % | n | % | n | % | n | % |
|
|
| Used email | ||||||||||
|
|
Ever | 387 | 88.4 | 49 | 94.2 | 144 | 91.7 | 194 | 85.5 | .067 |
|
|
In past week | 370 | 84.5 | 47 | 90.4 | 135 | 86.0 | 188 | 82.8 | .345 |
|
|
For 5-7 days in past week | 303 | 69.2 | 39 | 75.0 | 120 | 76.4 | 144 | 63.4 | .016 |
|
|
To discuss routine health topics | 148 | 33.8 | 14 | 26.9 | 62 | 39.5 | 72 | 31.4 | .180 |
|
|
To discuss CRC screeninga | 55 | 12.6 | 6 | 11.5 | 24 | 15.3 | 25 | 10.9 | .683 |
|
|
To discuss breast cancer screeninga | 64 | 14.6 | 9 | 17.3 | 26 | 16.6 | 29 | 12.7 | .176 |
| Used other e-communication b | ||||||||||
|
|
Ever | 247 | 56.4 | 43 | 82.7 | 107 | 68.2 | 97 | 42.4 | <.001 |
|
|
In past week | 245 | 55.9 | 43 | 82.7 | 105 | 67.7 | 97 | 42.4 | <.001 |
|
|
For 5-7 days in past week | 148 | 33.8 | 30 | 57.7 | 70 | 45.2 | 48 | 21.0 | <.001 |
| Type of e-communication used | ||||||||||
|
|
Texting | 194 | 44.3 | 41 | 78.8 | 88 | 56.1 | 65 | 28.4 | <.001 |
|
|
144 | 32.9 | 24 | 46.2 | 59 | 37.6 | 61 | 26.6 | .008 | |
|
|
Instant messaging/Internet-based chatting | 54 | 12.3 | 10 | 19.2 | 28 | 17.8 | 16 | 7.0 | .002 |
|
|
Video chatting | 31 | 7.1 | 5 | 9.6 | 16 | 10.2 | 10 | 4.4 | .068 |
|
|
21 | 4.8 | 4 | 7.7 | 13 | 8.3 | 4 | 1.7 | .007 | |
|
|
3 | 0.6 | 0 | 0.0 | 3 | 1.9 | 0 | 0.0 | .067 | |
|
|
Other | 3 | 0.7 | 1 | 1.9 | 1 | 0.6 | 1 | 0.4 | .500 |
| Used other e-communication to discuss routine health topics | 51 | 11.6 | 16 | 30.8 | 25 | 15.9 | 10 | 4.4 | .000 | |
| Used other e-communication to discuss CRC screeningc | 10 | 2.3 | 3 | 5.8 | 7 | 4.5 | 0 | 0.0 | .168 | |
| Used other e-communication to discuss breast cancer screeningc | 17 | 3.9 | 7 | 13.5 | 9 | 5.7 | 1 | 0.4 | .244 | |
| Type of e-communication used to discuss routine health topics | ||||||||||
|
|
Texting | 31 | 7.1 | 11 | 21.2 | 16 | 10.2 | 4 | 1.7 | .000 |
|
|
21 | 4.8 | 5 | 9.6 | 10 | 6.4 | 6 | 2.6 | .053 | |
|
|
Instant messaging/ Internet-based chatting | 6 | 1.4 | 3 | 5.8 | 2 | 1.3 | 1 | 0.4 | .011 |
|
|
Video chatting | 3 | 0.7 | 0 | 0.0 | 2 | 1.3 | 1 | 0.4 | .505 |
|
|
1 | 0.2 | 0 | 0.0 | 1 | 0.6 | 0 | 0.0 | .408 | |
|
|
Other | 2 | 0.5 | 1 | 1.9 | 1 | 0.6 | 0 | 0.0 | .163 |
| Uses cell phone to access Internet | 122 | 27.9 | 23 | 44.2 | 55 | 35.3 | 44 | 19.2 | .000 | |
aOnly asked of those who use email to discuss routine health topics.
bIncludes texting, Facebook, instant messaging, Internet-based or video chatting, Twitter, LinkedIn or other.
cOnly asked of those who use e-communication to discuss routine health topics.
Use of Electronic Communication for Discussions of Routine Health Topics and Cancer Screening
In the previous week, just over half of all participants (55.9%, 245/438) had used some other form of electronic communication (including texting, Facebook, instant messaging, Internet-based or video chatting, Twitter, LinkedIn, or other), there was significant variation by age with the youngest age group (40-49 year olds) being most likely to report use (Table 2). Approximately one in ten respondents (11.6%, 51/438) had ever used electronic communication (other than email) to discuss routine health topics, as expected from trends in overall use, youngest respondents were most likely to report such behavior. Similarly, close to one in ten participants under age 60 (8.6%, 18/209) had used electronic communication to discuss CRC screening or breast cancer screening. Texting and Facebook were the two most commonly mentioned forms of electronic communication across all age categories both for general use and specifically for discussion of routine health topics.
Attitudes Toward Discussing CRC Screening via Email and Electronic Communication
When asked whether they would be willing to share their CRC screening experience with friends or family in order to educate and encourage screening, close to three-quarters of all participants (73.3%, 321/438) were “very willing” to share through conversation, with almost all of the remaining stating that they “might be willing” to share in this way (Table 3). Email and other electronic communication showed lower proportions of users who were “very willing” to share (41.3%, 159/385 email users; and 25.1%, 63/251 e-communication users), but over half of both user groups would at least consider sharing their CRC experience in this way (“might be willing” or “very willing” to share–78.2%, 301/385 of email users; and 52.6%, 132/251 of e-communication users).
Table 3.
Willingness to share personal CRC screening experience with friends and family and preferred mode.
| Mode by which CRC screening experience would be shared | Total sample | Age 40-49 | Age 50-59 | Age 60-73 | P | |||||||
| n=433 | % | n=52 | % | n=156 | % | n=225 | % |
|
||||
| Through conversation asked of everyone (n=433) | .620 | |||||||||||
|
|
Not willing | 10 | 2.3 | 0 | 0.0 | 4 | 2.6 | 6 | 2.7 |
|
||
|
|
Might be willing | 102 | 23.6 | 13 | 25.0 | 32 | 20.5 | 57 | 25.3 |
|
||
|
|
Very willing | 321 | 74.1 | 39 | 75.0 | 120 | 76.9 | 162 | 72.0 |
|
||
| By email asked only of those who use email (n=385) | .393 | |||||||||||
|
|
Not willing | 84 | 21.8 | 8 | 16.3 | 30 | 21.1 | 46 | 23.7 |
|
||
|
|
Might be willing | 142 | 36.9 | 18 | 36.7 | 47 | 33.1 | 77 | 39.7 |
|
||
|
|
Very willing | 159 | 41.3 | 23 | 46.9 | 65 | 45.8 | 71 | 36.6 |
|
||
| By other electronic communication asked only of those who use e-communication (n=251) | .029 | |||||||||||
|
|
Not willing | 119 | 47.4 | 13 | 30.2 | 48 | 45.3 | 58 | 56.9 |
|
||
|
|
Might be willing | 69 | 27.5 | 18 | 41.9 | 27 | 25.5 | 24 | 23.5 |
|
||
|
|
Very willing | 63 | 25.1 | 12 | 27.9 | 31 | 29.2 | 20 | 19.6 |
|
||
When offered the opportunity to create their own content, adding, deleting, or rearranging text according to their own preferences (Figure 1), the vast majority of participants (85.4%, 374/438) were willing to send a message encouraging CRC screening; 68.5% (300/438) indicated that they would use either email or a combination of email and postcard (Table 3). Across all age groups, those who would send emails were in the majority and those who would send only postcards were the next largest group (Table 4). Older participants were least likely to send any message and men were more likely than women to indicate that they would not send. Those with a higher educational level were more likely to choose email, but education was not associated with overall willingness to send (Table 4).
Table 4.
Characteristics of respondents who are willing to pass along self-edited email or postcard messages sharing CRC screening experience (n=432).
|
|
|
Emaila | Postcard only | Would not send | P | |||||||||||||
|
|
n=300 | % | n=74 | % | n=58 | % |
|
|||||||||||
| Age, n % | .010 | |||||||||||||||||
|
|
40-49 | 42 | 82.4 | 5 | 9.8 | 4 | 7.8 |
|
||||||||||
|
|
50-59 | 118 | 76.1 | 20 | 12.9 | 17 | 11.0 |
|
||||||||||
|
|
60-73 | 140 | 61.9 | 49 | 21.7 | 37 | 16.4 |
|
||||||||||
| Gender, n % | .010 | |||||||||||||||||
|
|
Male | 117 | 62.2 | 37 | 19.7 | 34 | 18.1 |
|
||||||||||
|
|
Female | 183 | 75.0 | 37 | 15.2 | 24 | 9.8 |
|
||||||||||
| Race/ethnicity, n % | .365 | |||||||||||||||||
|
|
Black/African-American | 46 | 70.8 | 15 | 23.1 | 4 | 6.2 |
|
||||||||||
|
|
Asian/Pacific Islander | 35 | 77.8 | 5 | 11.1 | 5 | 11.1 |
|
||||||||||
|
|
White/Caucasian | 192 | 68.3 | 47 | 16.7 | 42 | 14.9 |
|
||||||||||
|
|
Other or not reported | 27 | 65.9 | 7 | 17.1 | 7 | 17.1 |
|
||||||||||
| Education, n % | <.001 | |||||||||||||||||
|
|
High School degree or less (includes technical school) | 55 |
53.9 |
33 |
32.4 |
14 |
13.7 |
|
||||||||||
|
|
At least some college | 243 | 74.3 | 41 | 12.5 | 43 | 13.1 |
|
||||||||||
| Marital status, n % | .561 | |||||||||||||||||
|
|
Married | 198 | 71.2 | 45 | 16.2 | 35 | 12.6 |
|
||||||||||
|
|
Unmarried | 100 | 66.2 | 29 | 19.2 | 22 | 14.6 |
|
||||||||||
| Ever had friends/family diagnosed with CRC?, n % | .063 | |||||||||||||||||
|
|
Yes | 103 | 76.9 | 19 | 14.2 | 12 | 9.0 |
|
||||||||||
|
|
No | 196 | 66.0 | 55 | 18.5 | 46 | 15.5 |
|
||||||||||
| Ever had a colonoscopy?, n % | .039 | |||||||||||||||||
|
|
Yes | 221 | 70.4 | 58 | 18.5 | 35 | 11.1 |
|
||||||||||
|
|
No | 73 | 65.2 | 16 | 14.3 | 23 | 20.5 |
|
||||||||||
| Verbal health literacy “CMLT-Listening”, mean (SD) | 81.24 (13.50) | 73.96 (15.11) | 81.26 (13.46) | <.001 | ||||||||||||||
| Print health literacy “CMLT-Reading”, mean (SD) | 86.23 (13.72) | 78.51 (15.60) | 85.39 (15.85) | <.001 | ||||||||||||||
| Numeracy, mean (SD) | 79.72 (20.18) | 71.62 (27.63) | 80.82 (21.99) | .012 | ||||||||||||||
| Self-efficacy “PEPPI”, mean (SD) | 8.18 (1.21) | 8.22 (1.51) | 7.56 (1.67) | .004 | ||||||||||||||
aThose indicated in the email column would send out either only emails or would send a mix of emails and postcards.
CRC Screening Email Messages: Role of Health Literacy and Self-Efficacy
Using ANOVA tests, mean measures of health literacy (print and verbal) and numeracy were compared across email senders, postcard senders, and those who wouldn’t send (Table 4). We found a consistent pattern across these three categories, with postcard senders scoring significantly lower than the other 2 groups on all three measures. For measures of self-efficacy, senders (both email and postcard) scored significantly higher than those who wouldn’t send.
On multivariate analysis (Table 5, Model 1), those with lower education were significantly more likely to be postcard senders than to be nonsenders. When we modeled the odds of sending any message at all (Table 5, Model 2), neither education nor health literacy level was significant. Those with higher self-efficacy scores were more likely to send messages in both models.
Table 5.
Willingness to send messages sharing CRC screening experience with peers.
|
|
|
Model 1a | Model 2b | ||||
|
|
|
Odds of being an email sender | Odds of being a postcard sender | Odds of sending either email or postcard | |||
|
|
|
OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Age | |||||||
|
|
40-49 | 2.21 | 0.73-6.73 | 0.77 | 0.19-3.22 | 1.83 | 0.61-5.53 |
|
|
50-59 | 1.72 | 0.89-3.29 | 1.06 | 0.47-2.41 | 1.57 | 0.83-2.97 |
|
|
60 and upc | - | - | - | - | - | - |
| Gender | |||||||
|
|
Male | 0.50 | 0.27-0.90 | 0.80 | 0.38-1.67 | 0.55 | 0.31-0.99 |
|
|
Femalec | - | - | - | - | - | - |
| Race/ethnicity | |||||||
|
|
Black/African American | 2.55 | 0.70-9.26 | 2.70 | 0.66-11.07 | 2.50 | 0.70-8.92 |
|
|
Asian/Pacific Islander | 1.19 | 0.46-3.12 | 0.59 | 0.15-2.32 | 1.05 | 0.41-2.72 |
|
|
Other or not reported | 0.85 | 0.31-2.30 | 0.93 | 0.28-3.14 | 0.84 | 0.32-2.20 |
|
|
White/Caucasianc | - | - | - | - | - | - |
| Education | |||||||
| High School degree or less (includes technical school) | 0.88 |
0.42-1.88 |
2.39 |
1.02-5.59 |
1.17 |
0.56-2.45 |
|
| At least some collegec | - | - | - | - | - | - | |
| Print health literacy scored (CMLT-Reading) | 1.01 | 0.99-1.03 |
0.99 | 0.96-1.01 | 1.00 |
0.98-1.03 |
|
| Self-efficacy (PEPPI)d | 1.25 | 1.03-1.53 | 1.35 | 1.04-1.74 | 1.28 | 1.06-1.55 | |
aModel 1–Odds of being an email sender or a postcard sender as compared to being a nonsender.
bModel 2–Odds of being a sender, either email or postcard, as compared to being a nonsender.
creference
dper unit increase in score
CRC Screening Email Messages: How Many Would Be Sent?
Those who indicated they would be willing to send emails estimated that they would send, on average, 15.9 emails per sender; those who indicated they would be willing to send postcards estimated they would send, on average 14.3 postcards per sender.
CRC Screening Email Messages: Expected Impact
Close to three-quarters of all participants thought that the self-edited message could have a positive impact; 71.5% (313/438) thought receiving the edited message would make their friends and family more likely to discuss CRC screening with a health care provider, and 73.1% (320/438) would be more likely to discuss screening if they themselves received such a message.
CRC Screening Email Messages: Reasons for Not Sending
While many participants in our study expressed willingness to share cancer-screening messages via email or e-communication, there are also important lessons to be learned from the 58/438 (13.2% of all participants) who were unwilling to send messages. Asked about their reasons for not sending this message, 43.1% (25/58) of those unwilling said they felt emails were inappropriate, 62.1% (36/58) expressed willingness to discuss the issue verbally. Additionally, 22.4% (13/58) cited their own limitations (lacked expertise) and 20.7% (12/58) felt their social network would not receive the message well (some felt their network members would be offended, while others said their network had already been screened). Equal percents (12.1%, 7/58) found the message unappealing and stated that they were already discussing this within their social network (and therefore didn’t need to send such a message). (Participants could provide more than one reason for not sending messages).
Discussion
Study Participants and Electronic Communication
When given both a template and an opportunity to create their own content, most study participants expressed willingness to pass along a personalized CRC screening message to members of their social network, and most thought the message would have a positive impact. Adults in this 40-70 year old age group were willing to share their cancer screening experience with peers and to promote screening using a variety of modes. Approximately one in ten had already used either email or electronic communication to discuss a cancer screening test. Most were regular email users and over one-third had discussed routine health topics via email. The majority had used another form of electronic communication such as text messaging or social media in the preceding week, with one in ten having used these modes for communication about routine health topics. Many adults expressed a willingness to use email and electronic communication to share cancer screening experiences.
Our findings are consistent with recent surveys [1,2,4] that reflect already high rates of email use and rising rates of social media use among adults in this age group. Data from the 2007 Health Information National Trends Survey (HINTS) showed that approximately one-quarter of Internet users had used social networking sites in the preceding year, but that relatively few older adults had done so (5.5% of those 65 years and over) [3]. By 2012, a Pew Internet poll showed 57% of Internet users 50-64 years old and 38% of those 65 years and older using social networking sites [1].
Our findings also align with recent studies demonstrating use of electronic communication to discuss health topics. Cycle 1 of HINTS 4, collected in 2011-2012, asked specifically about visiting a social networking site such as Facebook or LinkedIn “to read and share about medical topics” and found that 17.0% of Internet users had done this (12.9% of Internet users 50-64 years old, and 7.6% of Internet users 65-74 years old, unpublished data) [21].
Recent work indicates that Internet users may be receptive to the use of narratives to promote CRC screening within an online community [22]. While participation in Facebook support groups for breast cancer has been described among younger users [23], there is little documentation in the literature of older adults using Facebook or Twitter to discuss cancer or cancer screening. Social groups for prevention as well as support in CRC and breast cancer have been described in a recent content analysis [16], which identified 216 breast cancer groups and 171 CRC groups on Facebook and Twitter, but did not provide information on the age of participants.
Our study addresses the intersection of two distinct evolutions. The first is the spread of innovative and Internet-based technologies among older adults who are becoming increasingly comfortable both with text messaging and with social media platforms. The second is patients’ growing expectation that they will engage in collaborative and interactive dialogues around health.
Adults Spreading the CRC Screening Message
As our next step, we plan to recruit insured patients 50-70 years old at the time of CRC screening completion, and invite them to spread messages promoting screening to network members via the pathway of their choice (eg, postcard, email, text messaging, and social media). We hypothesize that this approach would take advantage of new technologies [6], while remaining inclusive of motivated, but less technologically savvy adults. In addition to prompting Internet-based conversations, this approach might also encourage face-to-face or telephone discussions.
We found that adults with less education were just as willing to pass along a CRC screening message to friends and family members, but were more likely to favor postcards. Mean health literacy scores for those who would send messages via postcard were significantly lower than both email senders and those who chose not to send. Adults with less education and lower health literacy may have social networks with higher numbers of unscreened individuals; efforts to include this group in peer-recruiting interventions are therefore particularly important.
Exploring a participatory intervention with multiple choices for network communication might also allow for future adaptation as new technologies supersede those of today. Interventions should capitalize on increased connectivity among social network members, facilitating exchanges of support, and information around cancer screening. Caution must also be taken. At times, social network members may communicate unhelpful or even harmful information [24,25]; interventions encouraging user-generated health content must include provisions to address this issue.
Potential Study Limitations
There are potential limitations to our study. Participants all had health insurance. Study participants may therefore not be representative of uninsured populations. Participants were asked to report whether they would be willing to forward messages to friends and family, but since they were not actually requested to send messages, it is possible that they overestimated their willingness to do so. Future studies are needed to assess whether these results are generalizable to the population at large, and whether people are in fact willing to forward personalized messages.
Conclusions
In conclusion, the majority of adults 42-73 years old in our study were willing to promote cancer screening to peers, and many were willing to use email and e-communication to do so. As the use of Web 2.0 participative technologies continues to rise in this age group, email, text messaging, and social media may offer cost-effective ways to disseminate peer-to-peer cancer screening messages. Our study indicates, however, that interventions relying exclusively on newer technologies may miss adults with lower education and lower health literacy levels who would otherwise be willing to engage in peer-to-peer screening promotion. This is a critical moment for further research.
Acknowledgments
The authors would like to thank those who assisted with coordination and collection of data for this round of interviews including–Brandi Robinson, Vinutha Vijayadeva, Roslin Nelson, Akeba Mitchell, Melody Fo, Dana Yamashiro, Jennifer Morita, Cassandra Firneno, Christopher Malone, Mark Mooradian, Mallory Thomas, and Jacquelyn Hyde. We also thank Mary Ellen Stansky for assistance with transcription and data entry, and Hassan Fouayzi for assistance with data analysis. Further, we thank Heather Richardson for assistance with editing and formatting. This work was supported by the National Cancer Institute at the National Institutes of Health via the Cancer Research Network (grant number U19 CA079689). This work was also supported by the National Center for Research Resources at the National Institutes of Health (grant number KL2RR031981). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
Abbreviations
- ANOVA
analysis of variance
- CMLT-Listening
Cancer Message Literacy Test-Listening
- CMLT-Reading
Cancer Message Literacy Test-Reading
- CRC
colorectal cancer
- CRN
Cancer Research Network
- FCHP
Fallon Community Health Plan
- HINTS
Health Information National Trends Survey
- KPGA
Kaiser Permanente Georgia
- KPHI
Kaiser Permanente Hawaii
- PEPPI
Perceived Efficacy in Patient-Physician Interactions
Multimedia Appendix 1
Willingness to use email and social media for peer-to-peer cancer screening communication.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Brenner J. Pew Research Center. Washington, DC: Pew Internet & Life Project; 2012. Pew Internet: Social networking (full detail) http://pewinternet.org/Commentary/2012/March/Pew-Internet-Social-Networking-full-detail.aspx. [Google Scholar]
- 2.Zickuhr K, Madden M. Pew Research Center. Washington, DC: Pew Internet & American Life Project; 2012. Jun 06, [2013-11-07]. Older adults and Internet use http://www.pewinternet.org/~/media//Files/Reports/2012/PIP_Older_adults_and_internet_use.pdf. [Google Scholar]
- 3.Chou WY, Hunt YM, Beckjord EB, Moser RP, Hesse BW. Social media use in the United States: Implications for health communication. J Med Internet Res. 2009;11(4):e48. doi: 10.2196/jmir.1249. http://www.jmir.org/2009/4/e48/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madden M. Pew Internet & American Life Project. Washington, DC: Pew Research Center; 2010. Aug 27, [2013-11-11]. Older adults and social media: Social networking use among those ages 50 and older nearly doubled over the past year http://pewinternet.org/Reports/2010/Older-Adults-and-Social-Media.aspx. [Google Scholar]
- 5.Cobb NK, Graham AL, Byron MJ, Niaura RS, Abrams DB, Workshop Participants Online social networks and smoking cessation: A scientific research agenda. J Med Internet Res. 2011;13(4):e119. doi: 10.2196/jmir.1911. http://www.jmir.org/2011/4/e119/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cobb NK, Graham AL. Health behavior interventions in the age of Facebook. Am J Prev Med. 2012 Nov;43(5):571–572. doi: 10.1016/j.amepre.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Bond RM, Fariss CJ, Jones JJ, Kramer AD, Marlow C, Settle JE, Fowler JH. A 61-million-person experiment in social influence and political mobilization. Nature. 2012 Sep 13;489(7415):295–298. doi: 10.1038/nature11421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aral S, Walker D. Creating social contagion through viral product design: A randomized trial of peer influence in networks. Management Science. 2011 Sep;57(9):1623–1639. doi: 10.1287/mnsc.1110.1421. [DOI] [Google Scholar]
- 9.Bull SS, Levine DK, Black SR, Schmiege SJ, Santelli J. Social media-delivered sexual health intervention: A cluster randomized controlled trial. Am J Prev Med. 2012 Nov;43(5):467–474. doi: 10.1016/j.amepre.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centola D. The spread of behavior in an online social network experiment. Science. 2010 Sep 3;329(5996):1194–1197. doi: 10.1126/science.1185231. http://www.sciencemag.org/cgi/pmidlookup?view=long&pmid=20813952. [DOI] [PubMed] [Google Scholar]
- 11.Ancker JS, Carpenter KM, Greene P, Hoffman R, Kukafka R, Marlow LA, Prigerson HG, Quillin JM. Peer-to-peer communication, cancer prevention, and the internet. J Health Commun. 2009;14 Suppl 1:38–46. doi: 10.1080/10810730902806760. http://europepmc.org/abstract/MED/19449267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fox S. Pew Internet & American Life Project. Washington, DC: Pew Research Center; 2011. May 12, [2013-11-08]. The social life of health information http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx. [Google Scholar]
- 13.Hesse BW, O'Connell M, Augustson EM, Chou WY, Shaikh AR, Rutten LJ. Realizing the promise of Web 2.0: Engaging community intelligence. J Health Commun. 2011;16 Suppl 1:10–31. doi: 10.1080/10810730.2011.589882. http://europepmc.org/abstract/MED/21843093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collins Dictionary, English, online. 2013. [2013-11-11]. Definition of “Web 2.0" http://www.collinsdictionary.com/dictionary/english/web-2-0?showCookiePolicy=true.
- 15.Cohen H. Heidi Cohen: Actionable marketing expert. 2011. May 09, [2013-11-08]. 30 Social media definitions http://heidicohen.com/social-media-definition/
- 16.De la Torre-Díez I, Díaz-Pernas FJ, Antón-Rodríguez M. A content analysis of chronic diseases social groups on Facebook and Twitter. Telemed J E Health. 2012;18(6):404–408. doi: 10.1089/tmj.2011.0227. [DOI] [PubMed] [Google Scholar]
- 17.Mazor KM, Rogers HJ, Williams AE, Roblin DW, Gaglio B, Field TS, Greene SM, Han PK, Costanza ME. The Cancer Message Literacy Tests: Psychometric analyses and validity studies. Patient Educ Couns. 2012 Oct;89(1):69–75. doi: 10.1016/j.pec.2012.06.018. http://europepmc.org/abstract/MED/22789147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazor KM, Roblin DW, Williams AE, Greene SM, Gaglio B, Field TS, Costanza ME, Han PK, Saccoccio L, Calvi J, Cove E, Cowan R. Health literacy and cancer prevention: Two new instruments to assess comprehension. Patient Educ Couns. 2012 Jul;88(1):54–60. doi: 10.1016/j.pec.2011.12.009. http://europepmc.org/abstract/MED/22244323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 20.Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient-physician interactions (PEPPI): Validation of an instrument in older persons. J Am Geriatr Soc. 1998 Jul;46(7):889–894. doi: 10.1111/j.1532-5415.1998.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 21.HINTS: Health Information National Trends Survey. 2012. [2013-11-08]. HINTS is a national survey uniquely dedicated to learning how people find, use, and understand health information (unpublished data-cycle 1) http://hints.cancer.gov/Default.aspx.
- 22.Hwang KO, Trickey AW, Graham AL, Thomas EJ, Street RL, Kraschnewski JL, Vernon SW. Acceptability of narratives to promote colorectal cancer screening in an online community. Prev Med. 2012 Jun;54(6):405–407. doi: 10.1016/j.ypmed.2012.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bender JL, Jimenez-Marroquin MC, Jadad AR. Seeking support on Facebook: A content analysis of breast cancer groups. J Med Internet Res. 2011;13(1):e16. doi: 10.2196/jmir.1560. http://www.jmir.org/2011/1/e16/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steinberg PL, Wason S, Stern JM, Deters L, Kowal B, Seigne J. YouTube as source of prostate cancer information. Urology. 2010 Mar;75(3):619–622. doi: 10.1016/j.urology.2008.07.059. [DOI] [PubMed] [Google Scholar]
- 25.Syed-Abdul S, Fernandez-Luque L, Jian WS, Li YC, Crain S, Hsu MH, Wang YC, Khandregzen D, Chuluunbaatar E, Nguyen PA, Liou DM. Misleading health-related information promoted through video-based social media: Anorexia on YouTube. J Med Internet Res. 2013;15(2):e30. doi: 10.2196/jmir.2237. http://www.jmir.org/2013/2/e30/ [DOI] [PMC free article] [PubMed] [Google Scholar]