Abstract
Background
Fear of childbirth and mode of delivery are two known factors that affect birth experience. The interactions between these two factors are unknown. The aim of this study was to estimate the effects of different levels of fear of birth and mode of delivery on birth experience 1 month after birth.
Methods
As part of an ongoing prospective study, we interviewed 3006 women in their third trimester and 1 month after first childbirth to assess fear of birth and birth experience. Logistic regression was performed to examine the interactions and associations between fear of birth, mode of delivery and birth experience.
Results
Compared to women with low levels of fear of birth, women with intermediate levels of fear and women with high levels of fear had a more negative birth experience and were more affected by an unplanned cesarean section or instrumental vaginal delivery. Compared to women with low levels of fears with a non-instrumental vaginal delivery, women with high levels of fear who were delivered by unplanned cesarean section had a 12-fold increased risk of reporting a negative birth experience (odds ratio 12.25; 95% confidence intervals 7.19-20.86). A non-instrumental vaginal delivery was associated with the most positive birth experience among the women in this study.
Conclusions
This study shows that both levels of prenatal fear of childbirth and mode of delivery are important for birth experience. Women with low fear of childbirth who had a non-instrumental vaginal delivery reported the most positive birth experience.
Keywords: fear of birth, mode of delivery, birth experience
Introduction
A positive maternal birth experience can have long lasting benefits by potentially strengthening self-confidence and improving bonding between mother and child (1). The birth experience can affect a woman's desire to have another child(2) and her mode of delivery preference for subsequent childbirth (3, 4). In contrast, women with a negative birth experience have an overall lower fertility rate, tend to wait longer until next pregnancy and are more likely to request a cesarean delivery(4, 5). Birth experience is a multidimensional concept, and factors associated with how the birth process is perceived include antenatal fear of childbirth (3, 6, 7) and mode of delivery(8-10).
Between 10 to 20% of all women have negative birth experiences (11-15). Reported prevalence rates of fear of childbirth range from 5% to 40%, and rates vary by study populations, cultural perspectives, and the instrument used to estimate fear (16-21). Compared with women with low levels of fear, women with high levels of fear tend to be younger, have unplanned pregnancies, low social support, and a worse economic status (22, 23).
Research has been inconclusive as to whether fear of childbirth predicts mode of delivery. A British study found no association between fear of childbirth and mode of delivery (24) whereas a Swedish study reported an increased risk of unplanned cesarean section among women with a high level of fear (25). A Norwegian study reported that women with high levels of fear were more likely to request and undergo anplanned cesarean section (26).
There is a lack of research how birth experience is influenced by mode of (non-operative and operative) delivery among women with low, intermediate or high levels of prenatal fear of childbirth. Using prospectively collected data including 3, 006 nulliparous women whose first birth was in 2009-2011 in Pennsylvania, USA, we studied associations between level of fear of birth, mode of delivery and birth experience.
Material and methods
The study was based on data from the First Baby Study (FBS), which included 3,006 English and Spanish speaking, nulliparous women aged 18 to 35 years in Pennsylvania, who were enrolled in the third trimester from 2009 to 2011.The FBS is a study of the effect of mode of first childbirth on subsequent childbearing and is following the study participants for a 3 year period post-partum. Because women who have their first child prior to the age of 18 or after the age of 35 are less likely to have a subsequent child within 3 years, this study excluded women younger than 18 or older than 35 at the time of the baseline interview. Participants were recruited from a variety of settings including childbirth education classes, hospital tours, health fares, targeted mailings to potentially eligible women throughout the State of Pennsylvania, Newspaper ads, and recruitment materials posted in low-income clinics and ultrasound centers throughout the State. Information about the study design, participant recruitment, and sample representativeness can be seen in Kjerulff et al.(27). All participants carried a singleton fetus and delivered past 34 completed gestational weeks. Information was prospectively collected by telephone interviews, the first survey (the baseline interview),occurred within 10 weeks before birth and the second at one month postpartum.The baseline interviews occurred when women were between 30 and 42 weeks gestation, with a median gestational age of 35 weeks. The 1-month postpartum interviews occurred between 3 and 80 days postpartum, with a median of 32 days postpartum.
The baseline survey included a 6-item scale to measure fear of upcoming birth, developed by the First Baby Study investigatorsand pilot-tested prior to deployment. The participants were asked to what extent they felt nervous, worried, fearful, relaxed, terrified, and calm about the upcoming delivery, using extremely, quite a bit, moderately, a little and not at all as response alternatives. A total score was created by summing participant responses to the items; the higher the score the more fearful the woman was about the upcoming delivery (the score of item “calm” was reversed). Total score could range from 6 (no fear) to 30 (extreme fear) and the overall Cronbach's Alpha for this scale (called the FBS Birth Anticipation Scale) was 0.82.We categorized the total scores into quintiles as follows: 6-13, 14-15, 16-17, 18-20 and 21 to 30. We then categorized the scores into 3 categories: 6-13 (the lowest quintile), 14-20 (the three middle quintiles) and 21-30 (the highest quintile). These categories were labeled “low fear”, “intermediate fear” and “high fear”. Previous research has shown that it is fair to believe that about 20% of all women who are pregnant have a fear of birth (11-15) so by letting only the top quintile represent the women with a real fear of birth we hoped to avoid the inclusion of women in this group who scored high on the scale but did not actually have a fear of birth. There was no information available on whether or not women received counseling for their potential fear, sought support or advice or explored other methods to cope with anxiety or fear related to their upcoming birth.
The primary outcome was birth experience, which was based on a 16-item scale administered in the one month postpartum survey, called the FBS Birth Experience Scale, which was developed by the FBS investigatorsand pilot-tested prior to use. The participants were asked to think back to right after they had their baby and report the extent to which they felt exhausted, on cloud nine, disappointed, in pain, sick, delighted, upset, excited, worried, calm, like a failure, thankful, traumatized, sad or proud of myself, using the response alternatives extremely, quite a bit, moderately, a little and not at all. A summated score was created, again with some items reversed, such that the higher the score the more positive women were about their birth experience. Scores could range from 16 to 80 and the Cronbach's Alpha was 0.73. For analytic purposes, the quintile of women with the lowest scores on the scale represents those having a negative birth experience.
Body mass index (BMI) was calculated using the mother's weight just prior to becoming pregnant, which was reported in the baseline survey and was categorized according to the World Health Organization as: underweight or normal weight (BMI <25), overweight (BMI 25.0-29.9) and obese (BMI ≥30.0). Social support was measured in the baseline survey, using 5 items from the MOS Social Support Survey(27). The participants were asked to tell how often each of the following kinds of support were available when needed: someone to confide in or talk to about your problems, someone to get together with for relaxation, someone to help you with daily chores if you are sick, someone to turn to for suggestions about how to handle a personal problem and someone to love and make you feel wanted, using the answers none of the time, a little of the time, some of the time, most of the time or all of the time. The 50% of women with the lowest scores were considered having low support and the 50% with the highest scores were considered having high support. Level of poverty was calculated using a formula that takes family income (from all sources) and number of children and adults living in the household into account (28). Race, marital status, education and whether pregnancy was intentional or not was reported in the baseline survey.Unplanned cesarean section was defined as a cesarean section performed after labor had started, either spontaneously or by induction.
The First Baby Study was approved by the Penn State College of Medicine Institutional Review Board (IRB) as well as the IRB's of participating hospitals located throughout the State of Pennsylvania.
Statistical methods
Chi-square tests were used to measure the association between maternal characteristics and fear of childbirth in three categories. Odds ratios (OR's) were estimated with 95% confidence intervals (CI's) using multiple logistic regression analyses. Odds ratios in Table 2 were adjusted for all other variables included in that table. Odds ratios in Table 3 were adjusted for social support, education and planned pregnancy. The covariates were categorized according to Table 1. We investigated interactions between level of fear of birth (low/intermediate/high) and mode of delivery (non-instrumental vaginal/instrumental vaginal/ /unplanned cesarean section/planned cesarean section) and risk of negative birth experience (yes/no) in a multivariate model.
Table 2.
Rates and adjusted odds ratios for a negative birth experience
| Variable |
Negative birth experience* |
|||
|---|---|---|---|---|
| Total | ||||
| N | Rate | Adjusted** | ||
| (n= 3005) | N (%) | OR | 95% CI | |
| Mode of delivery | ||||
| Non-instrumental vaginal delivery | 1 882 | 262 (13.9) | ref | |
| Planned cesarean section | 261 | 68 (26.1) | 1.62 | 1.04-2.53 |
| Instrumental vaginal delivery | 155 | 30 (19.4) | 2.19 | 1.57-3.06 |
| Unplanned cesarean section | 708 | 229 (32.3) | 3.14 | 2.50-3.95 |
| Fear of childbirth | ||||
| Low | 692 | 57 (8.2) | ref | |
| Intermediate | 1702 | 348 (20.4) | 2.85 | 2.08-3.92 |
| High | 611 | 184 (30.1) | 4.88 | 3.44-6.92 |
| Age (years) | ||||
| Prepregnancy BMI | ||||
| <25.0 | 1 709 | 351 (20.5) | ref | |
| 25-29.9 | 656 | 130 (19.8) | 0.88 | 0.69-1.13 |
| ≥30 | 607 | 102 (16.8) | 0.66 | 0.50-0.87 |
| Race/Ethnicity | ||||
| White | 2 502 | 491 (19.6) | ref | |
| Black | 221 | 43 (19.5) | 1.14 | 0.71-1.84 |
| Hispanic | 166 | 21 (12.7) | 0.60 | 0.34-1.06 |
| Other | 116 | 33 (28.4) | 1.34 | 0.84-2.15 |
| Social support | ||||
| Low | 1 428 | 365 (25.6) | 1.75 | 1.43-2.15 |
| High | 1 577 | 224 (14.2) | ref | |
| Marital status | ||||
| Married | 2 117 | 438 (20.7) | ref | |
| Living with partner | 544 | 102 (18.8) | 0.94 | 0.68-1.31 |
| Not living with partner | 187 | 19 (10.2) | 0.42 | 0.22-0.81 |
| Unattached | 157 | 30 (19.1) | 1.04 | 0.60-1.80 |
| Education | ||||
| High school degree or less | 501 | 73 (14.6) | ref | |
| Some technical college | 804 | 130 (16.2) | 1.24 | 0.84-1.82 |
| College graduate or higher | 1 701 | 386 (22.7) | 1.83 | 1.21-2.76 |
| Poverty | ||||
| Poverty | 246 | 41 (16.7) | 1.06 | 0.69-1.63 |
| Near poverty | 248 | 51 (20.6) | 1.27 | 0.86-1.87 |
| Not poverty | 2 332 | 467 (20.0) | ref | |
| Planned pregnancy | ||||
| Yes | 1 899 | 358 (18.9) | ref | |
| No | 1 098 | 226 (20.6) | 1.38 | 1.16-1.63 |
Includes the quintile (20%) of women with the most negative birth experience
Adjusted for all other variables in table.
Table 3.
Maternal fear of birth and mode of delivery and risk of having a negative birth experience*
|
Fear of childbirth |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mode of delivery | Low |
Intermediate |
High |
||||||
| Noa | ORb | (95% CI) | Noa | ORb | (95% CI) | Noa | ORb | (95% CI) | |
| Non-instrumental vaginal delivery | 443 | 1.00c | 1060 | 2.52 | (1.62-3.92) | 378 | 5.13 | (3.20-8.23) | |
| Planned cesarean section | 27 | 1.30 | (0.29-5.83) | 92 | 3.80 | (1.96-7.36) | 36 | 5.99 | (2.57-13.95) |
| Instrumental vaginal delivery | 66 | 1.96 | (0.81-4.76) | 136 | 6.11 | (3.50-10.65) | 59 | 10.35 | (5.25-20.39) |
| Unplanned cesarean section | 156 | 2.99 | (1.63-5.46) | 414 | 8.48 | (5.38-13.37) | 138 | 12.25 | (7.19-20.86) |
Includes the quintile (20%) of women with the most negative birth experience
Abbreviations: CI, confidence interval.
No. Denotes number of women included in the analyses
OR denotes odds rations, which are adjusted for social support, education and planned pregnancy.
The women in this group served as the reference group.
Table 1.
Maternal characteristics by level of fear
| Characteristic |
Level of fear* |
|||
|---|---|---|---|---|
| Low | Intermediate | High | ||
| N=692 | N=1702 | N=611 | ||
| N (%) | N (%) | N (%) | p-value | |
| Mode of delivery | ||||
| Non-instrumental vaginal delivery | 443 (64.0) | 1060 (62.3) | 378 (61.9) | |
| Planned cesarean section | 27 (3.9) | 92 (5.4) | 36 (5.9) | |
| Instrumental vaginal delivery | 66 (9.5) | 136 (8.0) | 59 (9.7) | |
| Unplanned cesarean section | 156 (22.5) | 414 (24.3) | 138 (22.6) | 0.378 |
| Age | ||||
| Prepregnancy BMI kg/m2 | ||||
| <25.0 | 409 (59.7) | 960 (57.0) | 340 (56.4) | |
| 25-29.9 | 142 (20.7) | 380 (22.6) | 134 (22.2) | |
| ≥30 | 134 (19.6) | 343 (20.4) | 129 (21.4) | 0.725 |
| Race/Ethnicity | ||||
| White | 565 (81.6) | 1455 (85.5) | 481 (78.7) | |
| Black | 51 (7.4) | 102 (6.0) | 68 (11.1) | |
| Hispanic | 48 (6.9) | 82 (4.8) | 36 (5.9) | |
| Other | 28 (4.0) | 62 (3.6) | 26 (4.3) | 0.001 |
| Social support | ||||
| Low | 270 (39.0) | 844 (49.6) | 314 (51.5) | |
| High | 422 (61.0) | 858 (50.4) | 296 (48.5) | <0.001 |
| Marital status | ||||
| Married | 491 (71.0) | 1259 (74.0) | 366 (60.0) | |
| Living with partner | 120 (17.3) | 278 (16.3) | 146 (23.9) | |
| Not living with partner | 42 (6.1) | 97 (5.7) | 48 (7.9) | |
| Unattached | 39 (5.6) | 68 (4.0) | 50 (8.2) | <0.001 |
| Education | ||||
| High school degree or less | 112 (16.2) | 250 (14.7) | 139 (22.7) | |
| Some technical college | 198 (28.6) | 437 (25.7) | 168 (27.5) | |
| College graduate or higher | 382 (55.2) | 1015 (59.6) | 304 (49.8) | <0.001 |
| Poverty | ||||
| Poverty | 61 (9.4) | 129 (8.0) | 56 (10.0) | |
| Near poverty | 45 (6.9) | 124 (7.7) | 78 (13.9) | |
| Not poverty | 545 (83.7) | 1 359 (84.3) | 428 (76.2) | <0.001 |
| Pregnancy was planned | ||||
| Yes | 455 (65.8) | 1136 (66.7) | 308 (50.4) | |
| No | 236 (34.1) | 560 (32.9) | 301 (49.3) | <0.001 |
Low= lowest quintile, intermediate= 2nd to 4th quintiles; high= highest quintile
The statistical software package SPSS 20.0 (SPSS Inc., Chicago, IL) was used for all data analyses.
Results
Scores on the FBS Birth Anticipation Scaleranged from a low of 6 (the minimum possible score) to a high of 30 (the maximum possible score). The mean score was 16.9 (standard deviation = 4.6) and the median score was 17. A larger proportion of women with high level of fear (highest score quintile) of the upcoming birth were young (18-24 years), black, had low social support, were unattached (to the father to be or partner), were living in poverty or near poverty, and had unplanned pregnancies (Table 1). The association between level of fear and mode of delivery was not significant (p = 0.710). There was no interaction between level of fear and mode of delivery (p= 0.971).
Scores on the FBS Birth Experience Scale (FBS-BES) ranged from a low of 28 to a maximum of 80. The mean on this scale was 68.7 and the median was 70. Those in the lowest quintile (19.8% of the study population) had scores ranging from 28 to 64. Table 2 presents associations with maternal factors and risks of having a negative birth experience (the lowest score quintile). Compared with women who had a non-instrumental vaginal delivery, risks of a negative birth experience were increased among women with planned cesarean section (OR = 1.62), vaginal instrumental delivery (OR = 2.19), and unplanned cesarean section (OR= 3.14). Compared with women reporting low fear of childbirth before delivery, women with high fear and women with intermediate fear had analmost five-fold and an almost three-fold increased risk of a negative birth experience, respectively. Low social support, having a college degree or higher education, and having an unplanned pregnancy were other factors independently associated with increased risks of having a negative birth experience. Compared with normal weight women, obese women had a reduced risk of a negative birth experience (Table 2).
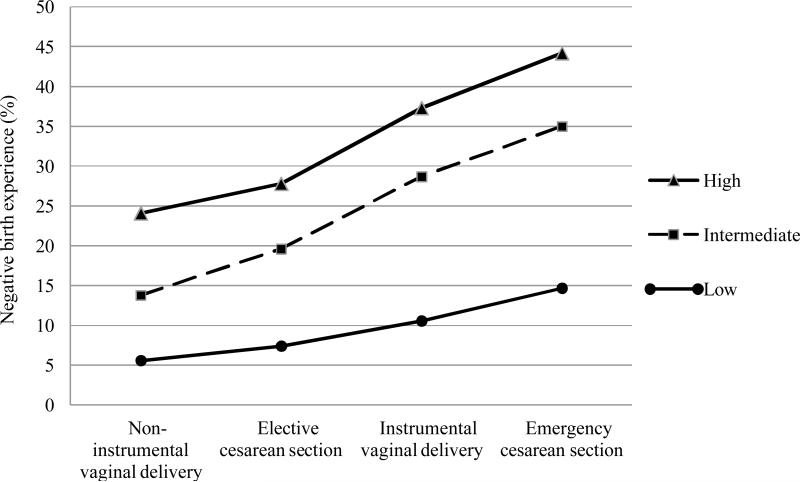
In Figure 1, we present crude rates of a negative birth experience by mode of delivery and antenatal fear of childbirth. In women with high fear, rates of a negative birth experience increased from 24% among women with a non-instrumental vaginal delivery to 44% among women with unplanned cesarean section. A slightly larger rate difference in negative birth experience was observed among women with intermediate fear: from 14% among women with a non-instrumental vaginal delivery to 36% among women delivered by unplannedcesarean section, thus an increase of a negative birth experience by 22%. Among women with low level of fear, corresponding rates were 6% and 15%, and the rate difference was only 9%.
Fig 1.
Unadjusted rates of a negative birth experience (highest quintile) by level of fear of labor and mode of delivery
In Table 3, we present risks of negative birth experience by combinations of antepartal fear of childbirth and mode of delivery, using women with no fear of upcoming birth having a non-instrumental vaginal delivery as the reference category. In each strata of level of fear, the risk of having a negative birth experience increased gradually with planned cesarean section, vaginal instrumentaldelivery and unplanned cesarean section. In each strata of mode of delivery, the risk of having a negativebirth experience increased with level of fear of childbirth before delivery. Compared with the women with low level of fear having a non-instrumental vaginal delivery, women with high level of fear had at least a 12-fold risk of having a negative birth experience if delivered by unplanned cesarean section and a 10-fold increase in risk if having an instrumental vaginal delivery.
Discussion
We found that rates and risks of a negative birth experience were influenced both by level of antenatal fear of childbirth and mode of delivery. Women with low levels of fear with non-instrumental vaginal delivery experienced the lowest risk of a negative birth experience, and women with high levels of fear delivered by unplanned cesarean section or instrumental vaginal deliverywere to a higher extent represented in the quintile of women with the most negative birth experience.
This study is unique because it shows the interplay between the different combinations of level of fear and mode of delivery and birth experience. For example, we were able to show that compared to women with intermediate and high levels of fear, women with low levels of fear rarely have a negative birth experience, disregarding mode of delivery. In congruence with previous research (22, 23), women with low levels of fear were characterized by having high levels of social support, they were well educated, were more often married, older and had planned pregnancies. As previously reported in another study (29), ahigher education was associated with both lower levels of fear but also an increased risk of a negative birth experience. We speculate that these findingsmay be explained by differences in expectations of the upcoming birth. Women with higher education were also generally older, and an age-related increased risk of a more complicated delivery may lead to a more negative birth experience (29). The youngest women were more exposed to social and psychological problems, which may have affected their expectations and experiences during labor.A previous study reported that women with low levels of fear of childbirth are generally less anxiety-prone, less irritable and have lower levels of somatic anxiety (30). Specific personality traits among these women such as high emotional stability and being extraverted can be associated with less risk of complications during childbirth and a more positive birth experience (31). Interestingly, the theory about the importance of preoperative fear or anxiety as a factor in postoperative emotional responses and recovery was proposed by Irving Janis in 1958 (32).
We were also able to show that birth experience among women with intermediate or high levels of fear were to a greater extent affected by an instrumental vaginal delivery or unplanned cesarean section. Problematically, it has been shown that women with high levels of fear are more likely to use epidural analgesia which in turn is associated with increased levels of intervention and cesarean section (33). Women with high levels of fear of birth have been given much attention in previous research (34-36) and should be continued to be given much focus due to the high risk of a negative birth experience. As it seems in our study, a non-instrumental vaginal delivery is the mode of delivery which is least likely to contribute to a negative experience among all women.
A non-instrumental vaginal delivery can never be guaranteed, and women undergoing anplanned cesarean section were nearly as satisfied as those having a non-instrumental vaginal delivery. Anplanned cesarean section for women with high fears could then seem like a good alternative. However, whether or not anplanned cesarean section should be carried out on maternal request is a controversial issue (37, 38). In a study with the aim toinvestigate maternal satisfaction following vaginal delivery after cesarean section and cesarean section after previous vaginal delivery, maternal satisfaction with vaginal delivery was high. Those that had experienced both modes of delivery would prefer vaginal births in future pregnancies(40).
In this study we used several newly developed instruments, the FBS Birth Anticipation Scaleand the FBS Childbirth Experience Scale,to define levels offear of birth and birth experience. Although these are newly developed instruments, they exhibited good levels of internal consistency reliability, and evidence of validity via the associations with the other variables in this study. We categorized women into three levels of fear (low, intermediate and high), using the lowest and highest quintiles to identify those with low and high levels of fear of childbirth. In addition, we defined women in the lowest quintile on the birth experience scale as having a negative birth experience, relative to the other women in the study. Converting continuous scales into categories using quintiles is a common strategy in social science and epidemiologic research and provided us with a way of measuring and visualizing the associations between fear of childbirth, mode of delivery and childbirth experience in a unique way. However, categories based on quintiles are based on the distribution of scores in the study population and the cut-off values would likely be different in other populations – limiting the external validity of this study.
In spite of the limitations in this study, our results clearly demonstrate that both antenatal fear of birth and mode of delivery have a significant impact on women's birth experience. For the past 25 years women with antenatal fear in Sweden have been receiving counseling in order to lower their fear and prepare for the upcoming birth. But even though a lot of women report the counseling to be helpful (42), the evidence in favor of such treatment is not overwhelming (36,42). There is far more evidence to show the benefits of one-to-one care and continuous support in labor. In a systematic review by Hodnett et al (43), it was concluded that women who received continuous labor support were more likely to have a positive birth experience, they were less likely to use pain medications, were more likely to give birth non-instrumentally and had slightly shorter labors. It was statedthat all women should have continuous support during labor.
It can be concluded that women's antenatal feelings of the upcoming birth are of high importance, just as the actual birthing process itself. As women's experiences of birth is a complex but important issue, health care providers should have an holistic view of the birth and inquire about the psychological well-being when evaluating care and not only the medical outcomes.
Acknowledgments
This paper reports on a study which was supported by grant (R01-HD052990) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, USA. Charlotte Elvander is supported by the National Doctoral School in Health Care Sciences, Sweden.
References
- 1.Beech BLP. Normal Childbirth Evidence and Debate churchill Livingstone. London: 2004. B. Normal birth: women's stories. pp. 59–83. [Google Scholar]
- 2.Bahl R, Strachan B, Murphy DJ. Outcome of subsequent pregnancy three years after previous operative delivery in the second stage of labour: cohort study. BMJ. 2004;328(7435):311. doi: 10.1136/bmj.37942.546076.44. Epub 2004/01/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waldenstrom U, Hildingsson I, Rubertsson C, Radestad I. A negative birth experience: prevalence and risk factors in a national sample. Birth. 2004;31(1):17–27. doi: 10.1111/j.0730-7659.2004.0270.x. Epub 2004/03/16. [DOI] [PubMed] [Google Scholar]
- 4.Hildingsson I, Radestad I, Rubertsson C, Waldenstrom U. Few women wish to be delivered by caesarean section. BJOG. 2002;109(6):618–23. Epub 2002/07/18. [PubMed] [Google Scholar]
- 5.Karlstrom A, Nystedt A, Hildingsson I. A comparative study of the experience of childbirth between women who preferred and had a caesarean section and women who preferred and had a vaginal birth. Sex Reprod Healthc. 2011;2(3):93–9. doi: 10.1016/j.srhc.2011.03.002. Epub 2011/07/12. [DOI] [PubMed] [Google Scholar]
- 6.Areskog B, Uddenberg N, Kjessler B. Experience of delivery in women with and without antenatal fear of childbirth. Gynecol Obstet Invest. 1983;16(1):1–12. doi: 10.1159/000299205. Epub 1983/01/01. [DOI] [PubMed] [Google Scholar]
- 7.Wijma K, Ryding EL, Wijma B. Predicting psychological well-being after emergency caesarean section: a preliminary study. Journal of Reproductive and Infant Psychology. 2002;20(1):25–36. [Google Scholar]
- 8.Wiklund I, Edman G, Andolf E. Cesarean section on maternal request: reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. 2007;86(4):451–6. doi: 10.1080/00016340701217913. Epub 2007/05/09. [DOI] [PubMed] [Google Scholar]
- 9.Ryding EL, Wijma K, Wijma B. Experiences of emergency cesarean section: A phenomenological study of 53 women. Birth. 1998;25(4):246–51. doi: 10.1046/j.1523-536x.1998.00246.x. Epub 1999/01/20. [DOI] [PubMed] [Google Scholar]
- 10.Ryding EL, Wijma B, Wijma K. Posttraumatic stress reactions after emergency cesarean section. Acta Obstet Gynecol Scand. 1997;76(9):856–61. doi: 10.3109/00016349709024365. Epub 1997/11/14. [DOI] [PubMed] [Google Scholar]
- 11.Waldenstrom U. Experience of labor and birth in 1111 women. J Psychosom Res. 1999;47(5):471–82. doi: 10.1016/s0022-3999(99)00043-4. Epub 2000/01/07. [DOI] [PubMed] [Google Scholar]
- 12.Green JM. Expectations and experiences of pain in labor: findings from a large prospective study. Birth. 1993;20(2):65–72. doi: 10.1111/j.1523-536x.1993.tb00419.x. Epub 1993/06/01. [DOI] [PubMed] [Google Scholar]
- 13.Green JM, Coupland VA, Kitzinger JV. Expectations, experiences, and psychological outcomes of childbirth: a prospective study of 825 women. Birth. 1990;17(1):15–24. doi: 10.1111/j.1523-536x.1990.tb00004.x. Epub 1990/03/01. [DOI] [PubMed] [Google Scholar]
- 14.Rijnders M, Baston H, Schonbeck Y, van der Pal K, Prins M, Green J, et al. Perinatal factors related to negative or positive recall of birth experience in women 3 years postpartumin the Netherlands. Birth. 2008;35(2):107–16. doi: 10.1111/j.1523-536X.2008.00223.x. Epub 2008/05/30. [DOI] [PubMed] [Google Scholar]
- 15.Larsson C, Saltvedt S, Edman G, Wiklund I, Andolf E. Factors independently related to a negative birth experience in first-time mothers. Sex Reprod Healthc. 2011;2(2):83–9. doi: 10.1016/j.srhc.2010.11.003. Epub 2011/03/29. [DOI] [PubMed] [Google Scholar]
- 16.Fenwick J, Gamble J, Nathan E, Bayes S, Hauck Y. Pre- and postpartum levels of childbirth fear and the relationship to birth outcomes in a cohort of Australian women. J Clin Nurs. 2009;18(5):667–77. doi: 10.1111/j.1365-2702.2008.02568.x. Epub 2009/02/26. [DOI] [PubMed] [Google Scholar]
- 17.Hall WA, Hauck YL, Carty EM, Hutton EK, Fenwick J, Stoll K. Childbirth fear, anxiety, fatigue, and sleep deprivation in pregnant women. J Obstetric Gynecol Neonat Nurs. 2009;38(5):567–76. doi: 10.1111/j.1552-6909.2009.01054.x. Epub 2009/11/04. [DOI] [PubMed] [Google Scholar]
- 18.Rouhe H, Salmela-Aro K, Halmesmaki E, Saisto T. Fear of childbirth according to parity, gestational age, and obstetric history. BJOG. 2009;116(1):67–73. doi: 10.1111/j.1471-0528.2008.02002.x. Epub 2008/12/06. [DOI] [PubMed] [Google Scholar]
- 19.Waldenstrom U, Hildingsson I, Ryding EL. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. 2006;113(6):638–46. doi: 10.1111/j.1471-0528.2006.00950.x. Epub 2006/05/20. [DOI] [PubMed] [Google Scholar]
- 20.Haines H, Pallant JF, Karlstrom A, Hildingsson I. Cross-cultural comparison of levels of childbirth-related fear in an Australian and Swedish sample. Midwifery. 2011;27(4):560–7. doi: 10.1016/j.midw.2010.05.004. Epub 2010/07/06. [DOI] [PubMed] [Google Scholar]
- 21.Geissbuehler V, Eberhard J. Fear of childbirth during pregnancy: a study of more than 8000 pregnant women. J Psychosom Obstet Gynaecol. 2002;23(4):229–35. doi: 10.3109/01674820209074677. Epub 2003/01/11. [DOI] [PubMed] [Google Scholar]
- 22.Saisto T, Salmela-Aro K, Nurmi JE, Halmesmaki E. Psychosocial predictors of disappointment with delivery and puerperal depression. A longitudinal study. Acta Obstet Gynecol Scand. 2001;80(1):39–45. doi: 10.1034/j.1600-0412.2001.800108.x. Epub 2001/02/13. [DOI] [PubMed] [Google Scholar]
- 23.Laursen M, Johansen C, Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish National Birth Cohort. BJOG. 2009;116(10):1350–5. doi: 10.1111/j.1471-0528.2009.02250.x. Epub 2009/06/23. [DOI] [PubMed] [Google Scholar]
- 24.Johnson R, Slade P. Does fear of childbirth during pregnancy predict emergency caesarean section? BJOG. 2002;109(11):1213–21. doi: 10.1046/j.1471-0528.2002.01351.x. Epub 2002/11/28. [DOI] [PubMed] [Google Scholar]
- 25.Ryding EL, Wijma B, Wijma K, Rydhstrom H. Fear of childbirth during pregnancy may increase the risk of emergency cesarean section. Acta Obstet Gynecol Scand. 1998;77(5):542–7. Epub 1998/07/08. [PubMed] [Google Scholar]
- 26.Kolas T, Saugstad OD, Daltveit AK, Nilsen ST, Oian P. Planned cesarean versus planned vaginal delivery at term: comparison of newborn infant outcomes. Am Journal Obstet Gyn. 2006;195(6):1538–43. doi: 10.1016/j.ajog.2006.05.005. Epub 2006/07/19. [DOI] [PubMed] [Google Scholar]
- 27.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. doi: 10.1016/0277-9536(91)90150-b. Epub 1991/01/01. [DOI] [PubMed] [Google Scholar]
- 28.United States Census Bureau [April 2013];How the Census Bureau Measures Poverty. [Internet]. Available from http://www.census.gov/hhes/www/poverty/about/overview/measure.html.
- 29.Zasloff E, Schytt E, Waldenstrom U. First time mothers’ pregnancy and birth experiences varying by age. Acta Obstet Gynecol Scand. 2007;86:1328–36. doi: 10.1080/00016340701657209. [DOI] [PubMed] [Google Scholar]
- 30.Ryding EL, Wirfelt E, Wangborg IB, Sjogren B, Edman G. Personality and fear of childbirth. Acta Obstet Gynecol Scand. 2007;86(7):814–20. doi: 10.1080/00016340701415079. Epub 2007/07/06. [DOI] [PubMed] [Google Scholar]
- 31.Johnston RG, Brown AE. Maternal trait personality and childbirth: The role of extraversion and neuroticism. Midwifery. 2012 doi: 10.1016/j.midw.2012.08.005. Epub 2012/10/09. [DOI] [PubMed] [Google Scholar]
- 32.Janis IL. Psychological stress: Psychoanalytic and behavioral studies of surgical patients. Wiley; New York: 1958. [Google Scholar]
- 33.Johanson R, Newburn M, Macfarlane A. Has the medicalisation of childbirth gone too far? BMJ. 2002;324(7342):892–5. doi: 10.1136/bmj.324.7342.892. Epub 2002/04/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nilsson C, Lundgren I. Women's lived experience of fear of childbirth. Midwifery. 2009;25(2):e1–9. doi: 10.1016/j.midw.2007.01.017. Epub 2007/05/22. [DOI] [PubMed] [Google Scholar]
- 35.Zar M, Wijma K, Wijma B. Pre- and postpartum fear of childbirth in nulliparous and parous women. Scand J Behaviour Therapy. 2001;30(2):75–84. [Google Scholar]
- 36.Hildingsson I, Nilsson C, Karlstrom A, Lundgren I. A longitudinal survey of childbirth-related fear and associated factors. J Obstet Gynecol Neonatal Nurs. 2011;40(5):532–43. doi: 10.1111/j.1552-6909.2011.01274.x. Epub 2012/01/26. [DOI] [PubMed] [Google Scholar]
- 37.Amu O, Rajendran S, Bolaji II. Maternal choice alone should not determine method of delivery. Brit Med J. 1998;317(7156):463–5. [PubMed] [Google Scholar]
- 38.Controversies in management - Should doctors perform an elective caesarean section on request? Brit Med J. 1998;317(7156):462. doi: 10.1136/bmj.317.7156.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dunn EA, O'Herlihy C. Comparison of maternal satisfaction following vaginal delivery after caesarean section and caesarean section after previous vaginal delivery. Eur J Obstet Gynecol Reprod Biol. 2005;121(1):56–60. doi: 10.1016/j.ejogrb.2004.11.010. Epub 2005/06/14. [DOI] [PubMed] [Google Scholar]
- 40.Saisto T, Salmela-Aro K, Nurmi JE, Kononen T, Halmesmaki E. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol. 2001;98(5 Pt 1):820–6. doi: 10.1016/s0029-7844(01)01552-6. Epub 2001/11/13. [DOI] [PubMed] [Google Scholar]
- 41.Wiklund I, Edman G, Ryding EL, Andolf E. Expectation and experiences of childbirth in primiparae with caesarean section. BJOG. 2008;115(3):324–31. doi: 10.1111/j.1471-0528.2007.01564.x. Epub 2008/01/15. [DOI] [PubMed] [Google Scholar]
- 42.Ryding EL, Persson A, Onell C, Kvist L. An evaluation of midwives’ counseling of pregnant women in fear of childbirth. Acta Obstet Gynecol Scand. 2003;82:10–7. doi: 10.1034/j.1600-0412.2003.820102.x. [DOI] [PubMed] [Google Scholar]
- 43.Hodnett ED, Lowe NK, Hannah ME, Willan AR, Stevens B, Weston JA, et al. Effectiveness of nurses as providers of birth labor support in North American hospitals. A randomized controlled trial. JAMA. 2002;288(11):1373–81. doi: 10.1001/jama.288.11.1373. [DOI] [PubMed] [Google Scholar]